Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
-
Upload
liliani-tjikoe -
Category
Documents
-
view
218 -
download
0
Transcript of Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
-
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
1/16
Indoor air pollution in developing countries andacute lower respiratory infections in children
Kirk R Smith, Jonathan M Samet, Isabelle Romieu, Nigel Bruce
AbstractBackgroundA critical review was con-
ducted of the quantitative literature link-ing indoor air pollution from householduse of biomass fuels with acute respira-tory infections in young children, which is
focused on, but not confined to, acutelower respiratory infection and pneumo-nia in children under two years in less
developed countries. Biomass in the formof wood, crop residues, and animal dung isused in more than two fifths of the worlds
households as the principal fuel.MethodsMedline and other electronicdatabases were used, but it was also
necessary to secure literature from col-leagues in less developed countries wherenot all publications are yet internationally
indexed.ResultsThe studies of indoor air pollu-tion from household biomass fuels are
reasonably consistent and, as a group,show a strong significant increase in riskfor exposed young children compared
with those living in households usingcleaner fuels or being otherwise lessexposed. Not all studies were able to adjust
for confounders, but most of those that didso found that strong and significant risksremained.
ConclusionsIt seems that the relativerisks are likely to be significant for theexposures considered here. Since acute
lower respiratory infection is the chiefcause of death in children in less developedcountries, and exacts a larger burden of
disease than any other disease category forthe world population, even small addi-tional risks due to such a ubiquitous expo-
sure as air pollution have important publichealth implications. In the case of indoorair pollution in households using biomass
fuels, the risks also seem to be fairlystrong, presumably because of the highdaily concentrations of pollutants found in
such settings and the large amount of time
young children spend with their mothersdoing household cooking. Given the largevulnerable populations at risk, there is anurgent need to conduct randomised trialsto increase confidence in the cause-eVectrelationship, to quantify the risk moreprecisely, to determine the degree ofreduction in exposure required to signifi-cantly improve health, and to establish theeVectiveness of interventions.(Thorax 2000;55:518532)
Keywords: acute respiratory infections; indoor airpollution; biomass fuels; developing countries; children
Acute respiratory infection (ARI) is the mostcommon cause of illness in children and amajor cause of death in the world. Among chil-dren under five years of age, three to fivemillion deaths annually have been attributed toARI, of which 75% are from pneumonia.1 TheWorld Health Organization estimates thatapproximately three million children under fivedied from ARI in 1993, exclusive of measles,pertussis, and diphtheria, and another 1.1 mil-lion died from conditions in association withthese diseases (table 1).2 As shown in table 2,ARI is one of the leading causes of death in theworld, smaller only than heart disease, cancer,and cerebrovascular disease. In terms of lost
healthy life years (measured as disabilityadjusted life years, DALYs), however, table 2shows that ARI is the chief cause of global illhealth today because its biggest impact is inyoung children.3 ARI is also a significant causeof death at other ages, particularly in the veryold.
Early in the 20th century ARI, in the form ofpneumonia, was also a major cause of death inthe currently developed countries, but itsimportance diminished dramatically during thecentury, partly due to the development of vac-cines and antibiotics.4 A large decline hadalready occurred before these medical inter-ventions became available, however, probablylargely reflecting improvements in housing
environments and nutrition.This report on indoor air pollution is part of
a series of reviews of the major determinants ofchildhood pneumonia in developing countriesthat were initiated by the World HealthOrganization in association with the LondonSchool of Hygiene and Tropical Medicine.5
There are a number of risk factors that aVect
Table 1 Annual mortality in children aged under fiveyears from developing countries in 1993
ARI related: 4.1 millionARI alone 3.0ARI with measles 0.64ARI with pertussis 0.26ARI with malar ia or HIV 0.23
Neonatal or perinatal 3.1 million(many involving ARI)
Diarrhoea related: 3.0 millionDiarrhoea alone 2.7Diarrhoea with measles or HIV 0.27
Measles/TB/tetanus/pertussis alone 1.2 millionMalaria alone 0.68 millionOther 0.2 millionTotal 12.2 million
ARI = acute respiratory infection.Source: World Health Organization.2
Other ARI information:ARIaccounts for33% ofall deathsfrominfectious disease in theworld and for 27% of the entire burden of infectious diseases.80% of the ARI burden occurs in children under five years fromless developed countries, accounting for about 6.7% of the glo-bal burden of disease from all causes.
Thorax 2000;55:518532518
Environmental Health
Sciences, University ofCalifornia, Berkeley,California 94720-7360,USAK R Smith
Department ofEpidemiology, Johns
Hopkins University,Baltimore, Maryland,
USAJ M Samet
Pan-American HealthOrganization, MexicoCity, MexicoI Romieu
Public HealthMedicine, Universityof Liverpool, UK
N Bruce
Correspondence to:Dr K R [email protected]
group.bmj.comon February 11, 2013 - Published bythorax.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://thorax.bmj.com/http://thorax.bmj.com/http://group.bmj.com/http://thorax.bmj.com/ -
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
2/16
ARI rates in young children, including malnu-trition, lack of breast feeding, and the incidenceof other diseases that aVect susceptibility. Thechilds environment also aVects risk throughsuch factors as crowding, chilling, and air pol-lution. This review explores what is knownabout the contribution of household air pollu-tion to the risk of ARI in young children world-wide, with particular focus on less developedcountries. When possible, we concentrate onpneumonia, which causes the highest casefatality rate. The review does not comprehen-
sively address the sources and concentrationsof indoor air pollutants in less developed coun-tries; rather, in the course of examining thestrength of air pollution as a risk factor, it oVersan overview. More details can be found inChen et al6 and Smith.7
Introduction to ARI and air pollutionEarly in the 20th century dramatic episodes ofoutdoor air pollution in developed countriesshowed that air pollution could cause excessdeaths and that children might be at particu-larly increased risk during the times of highpollution.8 For example, during the Londonfog of 1952, which was due mainly to smoke
from coal burning household stoves,
9
severalthousand excess deaths occurred. Infants andyoung children as well as the elderly were notedto be at higher risk than others and theproportion of deaths attributed to respiratorycauses was increased in comparison with theweeks before and after the fog.10 Outdoor airpollution has now been examined as a risk fac-tor for respiratory morbidity and mortality innumerous epidemiological studies and the evi-dence continues to indicate that infants andyoung children are at risk for adverseeVects.8 1114 Even though ambient pollutionlevels have now declined in developed coun-
tries,the epidemiological evidence continues toindicate adverse eVects on both respiratorymorbidity and mortality.12 13 Indeed, new stud-ies are indicating adverse eVects of inhaledparticles at levels that were previously consid-ered to be safe and are now frequently reachedin many urban areas.12 1517
During the last two decades the potentialsignificance for child health of exposures to airpollutants in indoor environments has also
been recognised.6 7 1820 The worlds childrenare exposed to inhaled pollutants as theybreathe air in diverse indoor and outdoor loca-tions. In considering risk to health, totalpersonal exposurewhich encompasses allexposures received to an agent, regardless ofthe locations and the mediumis the relevantexposure measure.21 Total personal exposure toan air pollutant can be estimated as theweighted average of the pollutant concentra-tions in the environments where a child spendstime; the weights are proportional to the timespent in each of these environments havingdistinct pollutant concentrations.22 This con-cept of pollution exposure, termed the micro-
environmental model, makes clear the healthrelevance of both indoor and outdoor pollutionexposures and the potential for widely varyingcontributions of indoor and outdoor exposuresto total personal exposures for children livingin diVerent countries throughout the world,depending on sources and time-activity pat-terns. It emphasises that one must be sure toexamine pollution where the people spendmost time, as well as in places where ambientlevels are high.2325
Using particulates as the indicator pollutant,for example, total population exposure globallyhas been estimated to be dominated by house-hold environments in developing countrieswhere solid fuels are used for cooking and
heating.25 26 This is because of confluence ofexposure factorsthat is, large populationsadjacent to frequently used devices with largeemission factors. Crop residues, dung, wood,and coal are widely used globally, perhapsaccounting for about half of all fuels used dailyto cook meals.27 From the standpoint of parti-cle levels, the most polluted urban outdoorenvironments in the world are also in develop-ing countriesnotably, but not exclusively, inthe coal using cities of Asia.26 28 Exposures toenvironmental tobacco smoke (ETS) tracktobacco consumption; this has been dominatedby developed countries but rates in these coun-tries are now static or declining while in the
developing world they are growing steadily.
26
This review focuses on indoor exposures ofthe worlds children to pollution from combus-tion of biomass fuels. (Companion reviewshave also been done on ARI risks to childrenfrom indoor air pollution due to tobaccosmoking and outdoor air pollution fromcombustion of fossil fuels.) The review doesnot address indoor air pollution by nitrogendioxide from cooking stoves and space heaters.In spite of intense investigation, this indoorpollutant has not been convincingly linked toARI, but has been inconsistently related to res-piratory symptoms.2931 For example, a cohort
Table 2 Global burden of death and diseases in 1990(%). Those categories causing at least 1% of lost DALYs
World LDCs MDCs
Acute respirator y infections 8.5 9.4 1.6Diarrhoea 7.2 8.1 0.3Perinatal eVects 6.7 7.3 1.9Child cluster (measles, pertussis,
polio, tetanus, diphtheria)5.2 5.8 0.008
Cancer 5.1 4.0 13.7Depression 4.7 4.4 8.5Malnutrition/anaemia (direct
eVects)
3.7 4.1 0.9
Heart (ischaemic) 3.4 2.5 9.9Tuberculosis 2.8 3.1 0.3Cerebrovascular (stroke) 2.8 2.4 5.9Motor vehicle accidents 2.5 2.2 4.4Congenital (birth defects) 2.4 2.4 2.2Malaria 2.3 2.6 0.003Maternal 2.2 2.4 0.6Sexually transmitted w/HIV 2.2 2.3 1.3C hr oni c obs tr uc ti ve l ung d is eas e 2 .1 2 .1 2. 1Falls 1.9 2.0 1.5War 1.5 1.5 0.7Suicide 1.4 1.2 2.3Violence 1.3 1.3 1.1Alcohol (direct eVects) 1.2 0.8 4.0Drowning 1.1 1.2 0.5Total (%) 72 73 64Population (million) 5260 4120 1 140Lost DALYs (million) 1380 1220 160Deaths (million) 50.5 10.9 36.6
Source: Murray and Lopez.3
DALYs = disability adjusted life years; MDCs = moredeveloped countries; LDCs = less developed countries.
Indoor air pollution in developing countries 519
group.bmj.comon February 11, 2013 - Published bythorax.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://thorax.bmj.com/http://thorax.bmj.com/http://group.bmj.com/http://thorax.bmj.com/ -
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
3/16
study of nitrogen dioxide exposure and respira-tory illness during the first 18 months of lifefound no evidence of increased risk withexposure.32 Ackermann-Liebrich and Rap33
have recently reviewed the evidence on indoorexposure to nitrogen dioxide.
A brief discussion of mechanismsARI comprise a set of clinical conditions ofvarious aetiologies and severities that aregenerally divided into two main forms: upperrespiratory tract infections (URI) and lower
respiratory tract infections (ALRI). The risk ofsevere ARI, which can be fatal, is highest invery young children and in the elderly. Clinicaland epidemiological criteria are available forseparating URI from ALRI but, unfortunately,worldwide there are no uniformly accepted cri-teria and the definitions in use are not fullyconsistent. For research and case managementunder field conditions in less developed coun-tries the WHO defines URI to include anycombination of the following symptoms: coughwith or without fever, blocked or runny nose,sore throat, and/or ear discharge. URI can usu-ally be treated successfully with supportivetherapy at home. ALRI include severe ARIinvolving infection of the lungs, with pneumo-
nia being the most serious form.34 Seriousinfections are most commonly caused bybacteria, although they may sometimes beviral. Clinical signs of ALRI include any of theabove symptoms of URI with the addition ofrapid breathing and/or chest indrawing and/orstridor. Severe ALRI caused by bacteria aretreated with antimicrobial therapy, withoutwhich they can sometimes be fatal.35
Air pollutants could increase the incidenceof ARI by adversely aVecting specific and non-specific host defences of the respiratory tractagainst pathogens (table 3).36 The non-specificmechanisms include filtration and removal ofparticles by the upper airway, the mucociliary
apparatus of the trachea and bronchi, phago-cytosis promoting components of the epitheliallining fluid, and phagocytosis and killing ofinfecting organisms by cells in the airways andalveolar macrophages. The specific mecha-nisms involve various components of humoraland cellular immunity. Organism specificimmunoglobulins promote phagocytosis; cellmediated immunity is required to kill organ-isms capable of living within alveolar macro-phages.
Smoke from household solid fuels is a com-plex mixture which contains many potentiallyrelevant components from a toxicologic per-
spective. These mixtures are inherently highlyvariable with characteristics determined bysources, materials burned, time since genera-tion, and other factors. The chemical andphysical characteristics of these mixtures havebeen characterised to some extent,7 37 38 par-ticularly in the form of wood smoke from metalheating stoves used in developed countries.Thus, only generalisations can be oVered con-cerning mechanisms by which particular air
pollutants could increase the risk for ARI andmixture-specific arguments cannot readily bedeveloped. On the other hand, there is a suY-cient basis of understanding of the toxicologi-cal properties of these mixtures to concludethat they could plausibly increase the risk ofARI.
A number of pollutants commonly found inindoor and outdoor air have been shown toadversely aVect components of the defencemechanisms against infectious organisms. Forexample, the particulate phase of cigarettesmoke and gas phase components adverselyaVect ciliary function in in vitro models. Gase-ous components that appear to be important
include nitrogen dioxide, ammonia, cyanides,aldehydes, ketones, acrolein, and acids.39 Nitro-gen dioxide has been shown to adversely aVectboth the mucociliary apparatus and humoraland cellular immune defences.40 The complexmixture of sulphur dioxide and particulatesmay reduce the eYcacy of host defencesagainst microbial agents and respiratory tractinflammation.13 Ozone has been shown tocause respiratory tract inflammation, increasedbronchoalveolar permeability, and to impairmacrophage functions.41 In animal studies die-sel exhaust has been related to chronic inflam-mation of the respiratory tract, epithelial cellhyperplasia, impaired alveolar clearance, pul-monary fibrosis, and compromised pulmonary
function.42Exposure to air pollutants might also act to
increase the severity of respiratory infectionsand thereby increase the proportion of illnessesconsidered clinically to involve the lower respi-ratory tract, and even to increase morbidity andmortality. The increased severity might bemediated by inflammation of the epithelial sur-face of the tracheobronchial tree caused by theirritant pollutants. If sustained exposure to airpollutants produces chronic inflammation,then infections might become more severe asthe infecting organisms further damage alreadyinflamed and possibly narrowed airways. Re-cently, Thomas and ZelikoV43 have shown that
exposure of animals to wood smoke signifi-cantly altered both the local and systemicimmune response associated with bacterialinfection.
INDOOR AIR POLLUTION
In addition to the strength of sources, theimpact of indoor emissions on air qualitydepends directly on ventilation and air mixingof the space. Most housing in developed coun-tries lies at temperate latitudes and has relativelylow exchange rates of indoor with outdoor air,typically one air change per hour or less.44 Evenlow emission rates in such housing can result in
Table 3 Host defences against respiratory infections
+ Anatomical barriers+ Angulation of airways+ Mucociliary clearance+ Secretory IgA+ Surfactant+ Opsonising IgG, fibronectin+ Complement+ Alveolar macrophages+ Polymorphonuclear leucocytes+ Plasma components+ Vasoactive mediators
Based on Reynolds and Elias.36
520 Smith, Samet, Romieu, et al
group.bmj.comon February 11, 2013 - Published bythorax.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://thorax.bmj.com/http://thorax.bmj.com/http://group.bmj.com/http://thorax.bmj.com/ -
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
4/16
indoor pollutant concentrations at levels ofpublic health significance. Ventilation rates forhouses in developing countries, which lieprimarily in tropical and subtropical regions ofthe world and are often open to the outdoors,are likely to be greater. Strong sources can bereadily identified in developing countries, how-ever, including biomass (wood, crop residues,and dung) and coal burning for cooking andheating.
Indoor pollutants can be grouped by sourceinto four principal classes: combustion prod-ucts; semi-volatile and volatile organic com-pounds released by building materials, furnish-
ings, and chemical products; pollutants in soilgas; and pollutants generated by biologicalprocesses.45 The principal combustion pollut-ants include carbon monoxide, nitrogen andsulphur oxides, particles, and volatile organics.The complex mixture in indoor air producedby tobacco smoking has been referred to asenvironmental tobacco smoke (ETS). A widevariety of semi-volatile and volatile organiccompounds can be found in indoor air; thereare diverse sources of these compounds. Thegas from the ground beneath a home may con-tain pollutants such as radon and termidicides
that may adversely aVect health. There aremany biological agents in indoor environmentsincluding, for example, pollens and moulds,insects, viruses, and bacteria.
Although systematically collected data areunavailable, it is likely that the relativeimportance of the four types of indoor air pol-lution varies throughout the world with climateand level of development. For combustionsources, the focus of this review, some generali-
sations can be made. After tobacco smoking,gas stoves have been the most common indoorpollution source of concern in studies in devel-oped countries.20 In the global context, how-ever, gas stoves are near the upper end of a his-torical evolution in the quality of householdfuels, sometimes called the energy ladder.46 Onthe lowest rungs are dried animal dung andscavenged twigs and grass as cooking fuels (fig1). The next rungs in the sequence are cropresidues, wood, and charcoal. The first non-biomass fuel on the ladder is kerosene or coal,and bottled and piped gases and electricity arehighest. In general, each successive rung on thisladder is associated with increases in the tech-
nology of the cooking system, cleanliness, eY
-ciency, and cost.
Biomass fuelNearly half the worlds households are thoughtto cook daily with unprocessed solid fuelsthat is, biomass fuels or coal (fig 2). In asignificant proportion of the households usingbiomass fuels, the bulk of the emissions isreleased into the living area.7 Although rates ofexchange of indoor with outdoor air arerelatively high in most housing in developingcountries, the pollutant emission rates for suchfuels are also high, and indoor concentrationsand associated exposures can be high as aresult. Compared with gas stoves, even stoves
using wood, one of the cleaner biofuels, canrelease 50 times more pollution during cooking(fig 1). In addition, unvented space heatingwith biomass fuels is common in much ofSouth Asia and in the highland areas of devel-oping countries of Asia, Africa, Latin Americaand Oceania.25 Large populations in China areexposed to smoke from coal fuels burned insimple stoves, which also have high emissionrates.
Incomplete combustion of unprocessed solidfuels produces hundreds of chemical com-pounds under the operating conditions of sim-ple cooking stoves. Such complex mixtures areproduced by burning of both coal and biomass
fuels, although the blends of compounds in thesmokes are diVerent.Unlike coal, biomass fuelsgenerally contain few intrinsic contaminants(sulphur, trace metals, and ash) and, underproper conditions, they can be burned withoutreleases other than the products of completecombustion (carbon dioxide and water). Un-fortunately, optimum conditions for completecombustion are diYcult to create with inexpen-sive household devices.
Smoke from cooking stoves is a complicatedand unstable mixture.7 47 Biomass fuel smokecontains significant quantities of several pollut-ants for which many countries have set outdoor
Figure 1 Emissions along the household fuel ladder. Reproduced with permission fromSmith et al.38
Dung Crop
residues
Wood Kerosene Gas Electricity0
5
10
15
20
25
30
35
40 1.8
1.6
1.4
1.2
1.0
0.8
0.6
0.4
0.2
0
g/meal
g/meal
CO
PM10
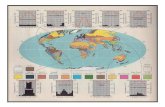
Figure 2 World distribution of household fuel use. Reproduced with permission from
Reddy et al.27
Subsaharan Africa
India
South-east Asia and Islands
China
North Africa and Middle East
Latin America and Caribbean
Former Soviet Union and East Europe
Established Market Economies
0 200 400 600
Population in 1990 (million)800 1000 1200
Non-solid fuel
Solid fuels (biomass and coal)
Indoor air pollution in developing countries 521
group.bmj.comon February 11, 2013 - Published bythorax.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://thorax.bmj.com/http://thorax.bmj.com/http://group.bmj.com/http://thorax.bmj.com/ -
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
5/16
air quality standardsfor example, carbonmonoxide, particles, hydrocarbons, and nitro-gen oxides. In addition, the aerosol containsmany organic compounds considered to be
toxic or carcinogenic, such as formaldehyde,benzene, and polyaromatic hydrocarbons. Thecomposition of the smoke varies with evenminor changes in fuel quality, cooking stoveconfiguration, or combustion characteristics.There is ample evidence that particles are gen-erally of the small sizes thought to be mostdamaging to health.7 48
Although a large scale worldwide survey ofsmoke concentrations has not been conducted,the findings of studies from diVerent parts ofthe world provide an indication of typicalindoor concentrations of the major pollutants.Table 4 lists studies that have measuredparticles, either total (TSP) or respirable.49
Compared with various national standards,WHO recommendations, or even outdoor con-centrations typical of the most polluted ofcities, these indoor levels are dramatically high.We cannot presently derive an accurate esti-mate of the total population in developingcountries exposed to indoor concentrationsthat would be considered unacceptable, norcan we readily apportion the contributions tototal personal exposure of indoor and outdoorsources. Additionally, in some rural areasoutdoor pollution penetrates indoors to asignificant extent and fuel burning indoors maybe a prominent contributor to outdoor pollu-
tion. Furthermore, there are no internationallyrecognised standards for pollutant concentra-tions indoors. Assuming that indoor standardsshould be at least as stringent as outdoor
standards, the number of people exposed atunacceptable levels indoors is expected to rivalor exceed the number exposed to unacceptableambient concentrations in all of the worldscities.50 Consideration of time-activity patterns,with far more time spent indoors thanoutdoors, suggests that the total global doseequivalent (amount actually inhaled) for in-door pollution could be an order of magnitudegreater than from ambient pollution.25
EPIDEMIOLOGY
(For an annotated bibliography of ARI andindoor air quality (non-ETS) see McCrackenand Smith.51)
The first report in the biomedical literatureto describe an association between indoorcooking smoke and childhood pneumonia indeveloping countries reported measurementsof indoor pollution levels in the homes ofinfants diagnosed with bronchiolitis and bron-chopneumonia at Lagos University TeachingHospital.52 Extremely high mean levels of vari-ous gaseous pollutants were measured and amean exposure time of 3.1 hours per day wasestimated but, unfortunately, the diVerences inexposure levels among households using wood,kerosene, coal, and gas were not reported andthere was no control group of infants. It is thus
Table 4 Indoor air pollution from biofuel combustion in developing countries
Location and year Description nParticulate concentration(g/m3) Reference
Kitchen area concentrationPapua New Guinea
1968 Overnight at floor level 9 2004900 Cleary & Blackburn101
1974 Overnight at sitting level 6 2 009000 Anderson102
Kenya197172 Overnight - highlands 5 27007900 Hofmann & Wynder103
- lowlands 3 3001500 CliVord104
1988 24 hours 64 12001900 (RSP) Boleij et al105
India1982 15 min cooking - wood 22 15 800 Aggarwal et al106
- dung 32 18 300 Patel et al107
- charcoal 10 55001988 Cooking (0.7 m to ceiling) 390 400021 000 Menon108
Nepal1986 Cooking - wood (geometric mean) 17 4700 Davidson et al109
China1987 All day - wood ? 2600 (RSP) Mumford et al110
The Gambia1988 24 hours 36 10002500 (RSP) Boleij et al105
Exposures during cooking (25 hours per day)India
1983 4 villages 65 6800 Smith et al111
1987 8 villages 165 3700 Ramakrishna et al66
1987 2 villages 44 3600 Ramakrishna112
1988 5 villages 129 4700 Menon108
1991 3 villages - winter 95 6800 Saksena et al113
- summer 5400- monsoon 4800
Nepal1986 2 villagesa 49 2000 Reid et al114
1990 1 village - beforeb 20 8200 (RSP) Pandey et al115
- after 20 3000 (RSP)
aApproximately half improved cookstoves.bCooks exposures measure before and after introduction of improved stoves.The studies are not completely comparable because of diVerent measurement protocols and equipment but, nevertheless, are fairlyconsistent. Area concentrations are measured with stationary instruments placed indoors at breathing height. Exposure rates weremeasured with instruments worn by the cook during food preparation. For comparisons, the US 24-hour standard, not to beexceeded more than once per year, has been 260 g/m3 and the Japanese one-hour standard is 200 g/m3. Some of the studies listedhere also measured other pollutants, including carbon monoxide and benzo(a)pyrene, which were sometimes found in concentra-tions well above those found in public settings in developed countries, as well as nitrogen and sulfur oxides and formaldehyde,whichwere found in concentrations roughly equal to the high end of those measured in indoor developed country conditions.Modified from Pandey et al.49
522 Smith, Samet, Romieu, et al
group.bmj.comon February 11, 2013 - Published bythorax.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://thorax.bmj.com/http://thorax.bmj.com/http://group.bmj.com/http://thorax.bmj.com/ -
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
6/16
diYcult to draw any quantitative conclusionsabout the relationship between exposure andthe incidence of pneumonia.
For focused attention in this review we wereable to identify 13 more recently publishedstudies which quantitatively addressed therelationship between exposure to householdbiomass smoke and ALRI in young children indeveloping countries (table 5) in which ALRIcase selection reasonably corresponded to
established WHO or other authoritative crite-ria in use at the time the study was done. Suchcriteria have evolved over time and thus, as dis-cussed below, have not been entirely consistentamong the studies. It is our judgement,however, that the protocols in these 13 studieshave been suYciently rigorous to warranttreating them as part of the same evidencepool. Nine were conducted in Africa and oneeach in India, Brazil, Argentina, and Nepal.Only one dealt with case fatality and the othersdealt with morbidity. In addition, we found twostudies from a developed country (USA) of therelationship between household wood smokeand ALRI among Navaho children (table 6).
These 15 studies are chosen for particularattention because they address actual ALRI,although confirmed by diVerent means, inchildren under five years old and involve indoorexposures to biomass fuel smoke. Each is suY-ciently quantitative to allow calculation of oddsratios and confidence intervals. Table 7 sum-marises the results of these 15 studies.
Some related studies, although discussedbriefly below, are not examined in detail herebecause they only meet some of the criteriafor example, addressing risks to older children,addressing respiratory symptoms but notconfirmed ALRI, or not providing enoughinformation to calculate odds ratios.
Incidence of ALRI in young children of developingcountriesOutcome measures diVered among the 13studies (table 5). Two of the cohort studies 53 54
and the one prospective case-control study55
used reported shortness of breath to screen forchildren with lower respiratory disease. Thefirst two assessed severity by counting respira-tory rate and assessing for chest indrawing andsigns of cardiorespiratory failure. ODempseyet al55 confirmed cases by laboratory tests andradiography. Pandey et al53 presented analysesfor moderate and severe lower respiratoryinfections (grade II and grade III/IV ARI,respectively). In an expanded study of the same
region in the Gambia studied by Campbell etal54 pneumonia was confirmed radiologically in50% of children with symptoms and signs oflower respiratory disease.56 The remainingstudies were based on children with pneumo-nia, severe wheezy bronchitis, or bronchiolitisdiagnosed clinically or according to WHO rec-ommendations in a hospital setting, or by ver-bal autopsy. These outcome measures wouldtend to include children with more severeillness.
Exposure to household smoke pollution wasalso assessed using diVerent approaches.Broadly, the studies examined the relationship
of the outcome measure with cooking practicessuch as use of an open wood fire comparedwith cleaner fuels such as kerosene,57 behav-ioural practicesfor example, carriage onmothers back while cooking53 55 56 5861orpresence of sources.6264 Pandey et al ,53 forexample, used maternally reported time spent
near the cooking stove as a categorical exposuremeasure in exploring the dose-response rela-tionship of exposure to smoke with lowerrespiratory disease in children (fig 3). Only onestudy actually measured pollutant levels andonly in a subset of study households.57
Air pollution studies in Kenya and the Gam-bia suggested that conditions were not favour-able for detecting a relationship betweenconcentrations of pollutants and lower respira-tory disease in children because of thehomogeneity of levels among households.65
Collings et al,57 however, found a significantdiVerence in levels of total particles duringcooking in households of 20 children with
lower respiratory disease and 20 with upperrespiratory disease, but few details wereprovided. The possibility of using carboxyhae-moglobin as a marker of smoke exposure wasalso explored in one study, but proved unsatis-factory because of the diYculty of controllingfor time since exposure.57
All but one of the eight morbidity studiesfinding significant associations were in Africa.The data in the one non-African study(Nepal53) were consistent with larger relativerisks for more severe disease, but the numberswere too small to exclude chance as anexplanation. Age specific data available in the
Figure 3 Acute respiratory infections (ARI) and exposureto biomass smoke in Nepal.(A) Based on six months datain about 250 infants in early 1984. (B) Based on threemonths data in late 1984 and early 1985 in samepopulation but with separate teams diagnosing ARI anddetermining smoke exposure. Trends for moderate andsevere cases are significant in both studies. Reproduced withpermission from Pandey et al.53
00.9 11.9 23.9 4+
2.50
2.25
2.00
1.75
1.50
1.25
1.00
0.75
0.50
0.25
0.00
Episodes
perinfant
A
00.9 11.9 23.9 4+0
Episodes
perinfant
B
0.1
0.2
0.3
2.4
2.0
1.6
Reported hours per day near stove
Line = Mild cases (grade I)
Bar 1 = Moderate cases (grade II)
Bar 2 = Severe cases (grades III & IV)
Indoor air pollution in developing countries 523
group.bmj.comon February 11, 2013 - Published bythorax.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://thorax.bmj.com/http://thorax.bmj.com/http://group.bmj.com/http://thorax.bmj.com/ -
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
7/16
http://group.bmj.com/http://thorax.bmj.com/ -
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
8/16
http://group.bmj.com/http://thorax.bmj.com/ -
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
9/16
Nepal study did not show greater eVects ininfants than during the second year of life. In adetailed analysis of data from the Gambia,
Armstrong and Campbell
56
found that the riskof pneumonia in association with smoke expo-sure was increased in girls but not in boys. Theauthors suggested that this diVerence resultedfrom greater exposure of females and not frombiological diVerences between the sexes. The
studies variably considered potential con-founding in their design and analytical ap-proaches (tables 6 and 7). Inadequate controlof confounding is likely to result in an overesti-mate of the odds ratios, since the use of openfires and biomass fuels is associated withpoverty and associated risk factors for ALRI.
Other possible sources of bias includemisclassification of exposure through recall
bias. Case-control studies are more likely to besubject to recall bias, although such bias canalso occur in prospective studies when collec-
tion of exposure data follows the occurrence ofillness. For example, in the study of Zulu chil-dren in Natal by Kossove58 the reportedduration of smoke exposure was remarkablysimilar in cases and controls, though theproportion of women reporting exposure of the
child to smoke (determined by questionnaire)was much higher in cases.
Bias in case-control studies from diVerential use ofhealth servicesDiVerential use of health services could
introduce bias if the subjects who use healthservices for serious paediatric illnesses, but notfor mild illnesses or preventive care, are alsothose who use unprocessed biomass fuels forcooking and who take no measures to avoidexposing their young children to the smoke. Inone of the case-control studies from Africa, butnot the others, breast feeding patterns andsocioeconomic status of cases and controlsdiVered.57 In the case-control study byKossove58 it is not clear whether the clinic con-trols were less sick. This approach to controlselection could introduce bias if caretakerswhose children were more heavily exposed toindoor air pollution were less likely than othersto bring their children to these services when
they were only mildly unwell or for preventivecare, but were just as likely as others to bringtheir children when seriously ill. This wouldresult in heavily exposed children being under-represented in the control groups and bias ofthe odds ratio away from unity. This situationcould arise due to distance of such householdsfrom the clinics, inability to aVord the cost oftransport, or from other constraints associatedwith poverty. In principle, this scenario is quitepossible since those households with the high-est exposures are also those most likely to bepoor, with less access to transport, etc.
In practice it is diYcult to assess whether thisbias has contributed to the risk estimates in the
studies quoted since care seeking has not beenstudied directly. From information available onsocioeconomic circumstances in three studies,however, there appears to be little diVerencebetween cases and controls.57 58 62 This sourceof bias was discussed by Morris et al69 as in theirstudy there was some evidence that socioeco-nomic circumstances (dirt floor, lack of run-ning water) were poorer among cases. It wasreported, however, that over 90% of childrenborn in the catchment area of the hospitalcompleted routine immunisation, suggestingthat the control sample from the well babyclinic was likely to represent the population.
Table 6 Wood burning and ALRI in children under five in developed countries
Study Design Case definition ExposureConfoundingadjusted Comments OR (95% CI)
Navaho reservation(1988) Tuba City,Arizona, USA(Morris et al)69
Case-control024 monthsn=58+58
Hospital:Cases: ALRI,bronchiolitis,pneumonia clinicaland x rayControls: Age-sexmatched, well childclinic
Interview:Primary energy sourcefor heating andcooking
Family history ofasthma, recentexposure torespiratorydisease, dirt floor,presence ofrunning water.
Wood burning stoves withchimneys but exposurelevels not validated. Recentexposure to respiratorydisease only other factorremaining significant (OR1.4) after multivariateanalysis. Humidifiers, ETS,
pets, crowding, and housetype not significant.
4.8 (1.7 to 12.9)
Navaho reservation(1993) FortDefiance, Arizona,USA (Robin et al)70
Case-control124 monthsn=45+45
Hospital:Cases: ALRI,bronchiolitis,pneumoniaControls: Age-sexmatched, sought carenot for otherconditions
Interview: cook withwoodMeasured 15 h PM10levels (5 pm8 am)
Interview
+ children/hh+ running water+ electricity
+ diYculty oftransport to clinic+ ETS
+ house type
No variation in PM10 levelswith ETS, type of home,etc. Type of cooking/heatingonly explained 10% ofvariance. Median PM10levels 24 g/m3 (cases), 22g/m3 (controls). No eVectfor coal use or wood forheating, but sample sizessmall
Cook with wood5.0 (0.6 to 43)PM >65 g/m3 7.0(0.9 to 57)
As in table 5, this list is confined to those quantitative studies using standardised protocols for determining ALRI. Other studies have just looked at the relationshipof wood burning with respiratory symptoms, e.g. Honicky et al,71 Butterfield et al,72 and Browning et al73 which are discussed in the text.
Table 7 Summary of studies of ALRI in young children and indoor biomass smoke indeveloping countries
Case-control studies (n = 9)
(South Africa, Zimbabwe, Nigeria, Tanzania, Gambia (2), Brazil, India, Argentina)6 adjusted for confounder s n=43113 not significant Odds ratios = 2.29.9
Cohort studies (n = 4)(Nepal, Kenya, Gambia (2))
2 adjusted for confounders n=9101 not significant Odds ratios = 2.26.0
Case-fatality study (n = 1)(Nigeria)
Hospitalised patients n=103Odds ratio = 4.8
Developed countries (n = 2)(USA (2))
Case-control n=206Adjust ed for confounder s Odds ratios = 4.87.0
The dividing line between developed and developing countries = $1000 per capita purchasingpower in 1995 (UNDP, 1998).116
526 Smith, Samet, Romieu, et al
group.bmj.comon February 11, 2013 - Published bythorax.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://thorax.bmj.com/http://thorax.bmj.com/http://group.bmj.com/http://thorax.bmj.com/ -
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
10/16
The study by Shah et al 63 provided limitedinformation on socioeconomic circumstancesfor cases and controls, and in any case did notreport an increased odds ratio for smoke expo-sure. The study from urban Argentina by Cer-queiro et al67 matched on five factors includingsocioeconomic status and district of residence.Overall, it appears that this bias was probablynot important in this group of case-controlstudies, although without specific information
on care seeking it remains a possible source oferror.
The study by Cerqueiro et al67 found a largeodds ratio (9.9, 95% CI 1.8 to 31) for homeheating with charcoal in patients with hospi-tal diagnosed ALRI compared with controlsmatched by socioeconomic level, nutritionalstatus, and other factors often addressed onlyby multivariate analysis in other studies (table5). No pollution measurements were reportedand little information was provided about thetype of stove and fuel involved. Cooking withgas (rather than electricity) also produced asignificant odds ratio (2.2, 95% CI 1.2 to 3.9).
It is intriguing to note that the three studies
that found no significant association were theonly ones which relied on questionnaires todetermine what type of cooking stove or fuelwas used at home without additional infor-mation about family behaviour patterns. InKerala, India the measure of exposure was aquestion about the existence of a smokelessstove (with a flue) at home.63 Unfortunately,however, such stoves in India often do notactually lower indoor air pollution levels.66 TheBrazil study took place in a city where theprevalence of household cooking with woodwas quite low (6%).64 The case-control studyreported by Johnson and Aderele in Nigeriafound no significant association of ALRI mor-bidity with reported type of household fuel, but
did find a strong relationship of fuel type withcase fatality.62
Other studiesA study of ARI in infants aged less than oneyear in India,74 which did not qualify for table 5because of its broad definition of ALRI, foundsomewhat conflicting results in urban slumcommunities where some households usedbiomass fuels and others kerosene. This waspossibly due to strong interference by largescale urban outdoor pollution and localoutdoor neighbourhood pollution from thecooking stoves themselves and other neigh-bourhood sources. Another study not qualify-
ing for inclusion in table 5 because of its inclu-sive case definition was an observational studyof 650 randomly chosen pre-school childrenaged 159 months in Lucknow, India, 14.5%of whom were found to have respiratory diseaseas defined by runny nose, cough, sore throat,breathlessness, or noisy respiration.68 Afteradjusting for age, weight, sex, income, andhouse type, use of dung as cooking fuel (OR2.7, 95% CI 1.4 to 5.3) and crowding (OR 1.2,95% CI 1.1 to 1.4) were associated with one ormore of these respiratory symptoms. The loca-tion of the child during cooking, ETS, andcooking with coal, kerosene, or wood were not
associated with respiratory symptoms in thisstudy. Somewhat diVerent results were ob-tained in the previously discussed six monthprospective study of 650 children aged 153months in the same area. With fortnightlyhousehold visits, a significant association ofsymptoms and/or duration of symptoms wasfound with outdoor TSP measurements.75
After multivariate analysis, cooking with any ofthe solid fuels (ORs 1.3 (wood); 1.6 (coal); 1.5(dung)) or kerosene (OR 1.4) and beingindoors while cooking took place (OR 2.0, 95%CI 1.7 to 2.4) were also significantly associ-ated. Morbidity due to probable pneumoniawas also determined by cough and diYculty inbreathing and was found only to be weakly butsignificantly related to the use of dung fuel (OR1.01, 95% CI 1.00 to 1.02).
A study of 658 children aged 06 years inJakarta found that, although respiratory symp-tom rates were, after multivariate analysis,related to evidence of uncollected refusearound the house (OR 1.6), they were notrelated to the type of cooking fuel used.76 Theauthor speculates that the sample size of
households using wood burning stoves (notgiven) was too small to find an eVect, and thatthe impact of the refuse may be a result of thesmoke generated by its frequent burning.76
A large national household survey in Indiafound a statistically significant relationship(OR 1.3) between reported use of householdbiomass fuel and reported incidence of respira-tory infection in the previous week among chil-dren under five years.77 Since the survey did notdistinguish cases by ALRI, URI, or severity,however, it probably is not a good predictor ofthe risk of severe, life threatening ALRI.
Mortality from pneumonia in developing countr iesAn association between exposure to householdbiomass pollution and mortality from pneumo-nia has been shown in one study of ALRI inNigeria.62 Although a case-control study in thesame hospital did not reveal a relationshipbetween type of cooking fuel and hospitaladmissions for ALRI, the children with ALRIwho came from homes that burnt wood were12.2 times (p
-
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
11/16
Incidence of ALRI in young children fromdeveloped countriesStudies of the health eVects of biomass smokein developed countries have focused on house-holds using enclosed metal heating or cookingstoves with chimneys. The indoor pollutantconcentrations are normally substantially lessthan those found in village homes using openfires.47 Peak indoor particulate concentrationsresulting from leaky heating stoves in devel-
oped country homes are at most severalhundred g/m3 and are typically much less thanthe peak values of many thousand g/m3 in vil-lage homes cooking with biomass fuel.25
Nevertheless, the impact on ALRI has beenshown in the two studies summarised in table6.
Although not increased to the extent suf-fered by children from developing countries,the age adjusted ALRI mortality rate of NativeAmerican children has been some six timesthat of non-Hispanic white children. A study ofyoung Navaho children in Arizona found thathousehold cooking/heating with woodstoves(with flues) produced a significant odds ratio
(4.8, 95% CI 1.7 to 12.9) after multivariateanalysis for physician-confirmed ALRI in hos-pitalised patients using radiographs.69 Caseswere thus confirmed as bronchiolitis or pneu-monia, but no information was given on themix. A second study was designed to addressfactors not covered in the firstin particular,to include the diYculty of reaching the clinic inthe multivariate analysis and to actually meas-ure indoor air pollution levels.70 Cases includedLRI, pneumonia, and bronchiolitis, ascer-tained from the hospitals inpatient records. Inthis case a similar but non-significant oddsratio was found (5.0, 95% CI 0.6 to 43). Themedian 15 hour PM10 levels in both sets ofhouseholds (measured once), however, were
quite similar (table 6) and were much lowerthan those found in developing countries. Fur-ther analysis revealed that PM10 levels over65 g/m3 (90th percentile) were related toALRI, but with a broad confidence band (OR7.0, 95% CI 0.9 to 57), and that type ofcooking/heating only explained 10% of thevariance.
Three other US studies of respiratory symp-toms in young children exposed to wood smokedid not qualify for inclusion in table 6. Honickyet al71 performed a historical prospective studyof 68 preschool children, half of whom camefrom homes with wood heating stoves, andfound significantly more respiratory symptoms
in the exposed group. Careful matching wasdone to assure that the groups did not diVer byincome, ETS, residence, etc, but no multivari-ate analysis was reported. Butterfield et al 72
found a significant correlation between hoursof reported wood stove use and five of 10respiratory symptoms in 59 children aged lessthan 66 months. Browning et al,73 on the otherhand, found no significant relationship be-tween respiratory symptoms in 823 childrenaged over one year and location in high or lowwood smoke neighbourhoods. However, anon-significant trend was observed in thoseaged 15 years. Ambient monitoring showed
an approximate diVerence of 20 g/m3 in PM10levels between the two neighbourhoods.
Morbidity in school aged childrenExposure to pollution from wood stoves hasbeen associated with chronic respiratory symp-toms, changes in lung function, and/or hospitalvisits in studies of school aged children in theUSA exposed to wood smoke from stoves intheir own home and/or their neighbourhoods.
Larson and Koenig78 reviewed six such studiesin school aged children,two of which dealt withasthmatics and five of which found significantrisks. (An earlier review can be found in Hon-icky and Osborne.79) The one study lackingstatistical significance80 was based on telephoneinterviews with 399 households. In addition,the Harvard Six Cities study of air pollutionfound use of wood stoves to be associated witha 30% increase in respiratory illness (chroniccough, bronchitis, chest illness, wheeze orasthma) in a large sample of children aged 710years.81 Such studies suggest an adverse eVectof biomass pollution on lung function and areconsistent with irritation and inflammation of
airways and impaired host defences.Similar associations were not found in twostudies in Malaysia. In a study involving 1214712-year-old children the presence of a wood orkerosene stove in the home was inversely asso-ciated with the forced vital capacity (FVC) andforced expiratory volume in one second(FEV1), but in a multiple logistic regressionanalysis that included passive smoking theassociation with stove type was no longersignificant.82 A more detailed analysis of 1501712-year-old children found, after multivari-ate analysis, that use of mosquito coils was sig-nificantly related to maternally reportedwheeze (OR 1.4) and asthma (OR 1.4) andETS with chest illness (OR 1.7). No associ-
ation was found with type of cooking fuel.83In Papua New Guinea Anderson84 also failed
to show a diVerence in rates of respiratorysymptoms or lung function in studies compar-ing children exposed to diVerent levels ofsmoke. In the first study of 1650 highland andlowland children under 10 years, both groupswere found to have similar rates of loose cough,adventitia and past chest illness, despite higherlevels of smoke exposure in the highlands. Infact, higher rates of asthma and wheeze werefound in coastal children. In a much smallerstudy involving 112 highland children, thoseexposed to smoke in their village homes werefound to have the same prevalence of respira-
tory symptoms and similar lung function astheir counterparts living in nearby governmenthousing.
More recent studies in developing countries,however, have found eVects in school agedchildren. A study in Adana, Turkey found byquestionnaire in a group of 617 912-year-oldsthat those in homes heated with coal hadsignificantly more cough than those usingkerosene, oil, or electricity.85 The lowest statis-tically diVerent lung functions (FVC, FEV1,PEFR, FEF25) were in children from woodburning homes. A similar study of 1905 713-year-olds in Jordan found that open wood
528 Smith, Samet, Romieu, et al
group.bmj.comon February 11, 2013 - Published bythorax.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://thorax.bmj.com/http://thorax.bmj.com/http://group.bmj.com/http://thorax.bmj.com/ -
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
12/16
and/or kerosene burning was statistically re-lated to lower lung function with about twicethe negative impact of ETS.86 No multivariateanalyses were reported for these studies.
Impact on known precursors of ARIOne mechanism by which biomass smoke andother air pollution exposures could enhancethe risk of ARI in young children would be byin utero exposures via their mothers who, whencooking, can be heavily exposed. Adverse preg-nancy outcomes such as low birth weight are
known ARI risk factors
1
through reducedimmunocompetence and/or impaired lungfunction.87 As shown in fig 4, there are severalpathways by which low birth weight and otheradverse pregnancy outcomes may result fromheavy maternal air pollution exposures. Provid-ing evidence of such in utero eVects, acase-control study of 451 stillbirths inAhmedabad, India88 found after multivariateanalysis that cooking with biomass fuel wasassociated with a statistically significant in-creased chance of stillbirth (OR 1.5, 95% CI1.0 to 2.1). A study in Bohemia found signifi-cant intrauterine growth retardation in babies
born to women exposed to increased levels ofsmall particles.89 A recent cohort study ofnearly 75 000 births in Beijing90 found a 6.9 gdecrease in birth weight for each 100 g/m3 ofambient TSP, which translated to an odds ratioof 1.1 (95% CI 1.05 to 1.14) for lowbirthweight babies (
-
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
13/16
increased ALRI in infants and young children,an association that has been judged as causal.32
Similarly, a large literature, primarily basedon studies of various pollutants in outdoor airin urban settings, also shows adverse eVects ofparticles and gases on the respiratory health ofchildren. Existing studies are likely to under-estimate the size of the association betweenambient pollution and health as a result of mis-classification of the exposure status of individu-
als within populations.
ConclusionsIndoor and outdoor environments are widelycontaminated by complex mixtures of gasesand particles that are produced by combustion.Components of these mixtures have beenshown to adversely aVect host defences againstrespiratory infections and it is thus plausiblethat such pollutant mixtures increase theincidence of respiratory infections. Air pollut-ants might also increase the severity of respira-tory infections by causing inflammation of thelung airways and alveoli. Infants and youngchildren are particularly susceptible to these
adverse eV
ects because of the immaturity ofrespiratory defence mechanisms and the geo-metry of the airways. Patterns of time-activity,which place children near sources of pollutionsuch as cooking stoves, cigarettes, vehicleexhaust, or other contaminated environments,may contribute to the increased risk of ARIfrom airborne pollutants in young children.
This review documents the potential for pre-venting ARI in general, and pneumonia in par-ticular, in children by reducing exposures to airpollution. Combustion of household solid fuelsin developing countries produces exposures tosmoke components that are remarkably high bythe standards set for outdoor air in developedcountries. Adverse eVects of these exposures
would be anticipated on a toxicological basis.Although the epidemiological evidence onsmoke from biomass fuels and pneumonia isnot yet abundant, associations have been dem-onstrated between exposure measures andindicators of illnesses involving the lower respi-ratory tract.When interpreted within the broadframework of epidemiological and toxicologi-cal evidence on inhaled pollutants and ARI, theassociation of smoke from biomass fuels withARI should be considered as causal, althoughthe quantitative risk has not been fully charac-terised.
Risk estimates from individual studies areimprecise because of relatively small sample
sizes and misclassification of exposure andoutcome. Given the imprecision and uncer-tainty in characterising the risk of biomasssmoke exposure, quantitative risk assessmentscannot be oVered with great confidence. Onthe other hand, the large population of childrenexposed and even our limited database on lev-els of exposure implies a significant burden ofattributable ARI. The extent to which excessbiomass smoke can be prevented is uncertain,however, because of the lack of information onexposure-response relationships. We urge fur-ther research directed at the time-activitypatterns of children under the age of five years
as well as studies designed to characterise totalpersonal exposures and the contributions ofindoor and outdoor pollution sources tochildrens exposures in developing countries.The resulting data would facilitate the designof additional case-control and cohort studies tobetter quantify the relationship between smokeexposure and ARI and to identify the mosteVective intervention strategies.
Unlike most sources of ambient air pollu-
tion, however, household sources of exposuresuch as cooking and heating oVer the oppor-tunity for conducting randomised trials ofpotential interventions, both engineering andbehavioural. Thus, of even higher priority thanfurther observational studies is the promotionof well designed randomised intervention trialsin households in less developed countries inconjunction with careful exposure assessment.Data from intervention studies could quantifyexposure-response relationships for ARI, con-vincingly demonstrate to policy makers thehealth benefits of practical interventions suchas clean fuels, improved stoves, and house-holder education and, ironically, given past sci-
entific inattention to this particular problem,move air pollution epidemiology in generalcloser to the gold standard of randomisedclinical trials.
Globally, even though the attributable frac-tion of pneumonia/ARI mortality due to airpollution is not yet certain, it is probable thatthis disease outcome represents the largestclass of health impacts from air pollution expo-sure worldwide. This is likely to be the case interms of total morbidity and mortality but,because much of the burden falls on youngchildren, is almost certainly the case withregard to measures of ill health that considerthe lost life years involved. This is due to threefactors: (1) the relatively high odds ratios
apparently involved (table 5), (2) the seeminglyhigh and prevalent exposures in less developedcountries, particularly in households (fig 2),and (3) the high base rate of the disease in thesenations (table 2).
Relatively recently there has been a signifi-cant increase in attention in many developedcountries to issues related to environmentaljusticethat is, the unfortunate tendency forthe highest exposures to environmental pollut-ants to be experienced by some of the mostdisadvantaged populations.98 Globally, how-ever, even more egregious examples of thisinjustice prevail.Indeed, few if any large groupsare more disenfranchised and disadvantaged
than poor rural women in developing countriesand their young children, who experience thebulk of global airborne exposures to many pol-lutants.
Some readers may be surprised by our con-clusion that ARI in children represents one ofthe major health consequences of air pollutionglobally. This conclusion contrasts with thelimited epidemiological research on air pollu-tion and ARI in developed countries. Indeed,the evidence driving policy for air pollutioncontrol at present derives largely from studiesof elderly persons. We suggest that this seemingparadox reflects a failure to systematically
530 Smith, Samet, Romieu, et al
group.bmj.comon February 11, 2013 - Published bythorax.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://thorax.bmj.com/http://thorax.bmj.com/http://group.bmj.com/http://thorax.bmj.com/ -
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
14/16
focus studies of air pollution and health onthe populations receiving the highestexposures.99 100 These populations may notnecessarily correspond with the locationswhere the greatest pollutant emissions occur.We need an organised international eVort tomonitor, evaluate, and mitigate air pollution inthe places where people live and work. A prin-cipal goal of this eVort should be rapid reduc-tion of the alarming global burden of ARI.
We appreciate comments on early drafts by Sandy Gove, Anto-nio Pio, and Stephen Rogers and research assistance from RubyH-D Nguyen. Isabelle Romieus work on this paper was partlysupported by the National Center for Environmental Health,Centers of Disease Control and Prevention, Atlanta, Georgia,USA.
1 Stansfield S, Shepard D. Acute respiratory infection. In:Jameson D, Mosley W, Measham A, Bobadilla J, eds.Disease control priorities in developing countries. Oxford:Oxford University Press, 1993: 6790.
2 World Health Organization (WHO). World health report.Geneva: WHO, 1995.
3 Murray CJL, Lopez AD. Global burden of disease. Cam-bridge, Massachusetts: Harvard University Press, 1996.
4 Doyle R. US deaths from pneumonia. Scientific Am1997:29.
5 Kirkwood BR, Gove S, Lob-Levyt J, et al . Potentialinterventions for the prevention of childhood pneumonia in
developing countries: a systematic review. Bull WHO 1995;73:7938.6 Chen BH, Hong CJ, Pandey MR, et al. Indoor air pollution
in developing countries. World Health Stat Q 1990;43:12738.
7 Smith KR. Biofuels, air pollution, and health: a global review.New York: Plenum, 1987.
8 Shy CM, Goldsmith JR, Hackney JD, et al. Health eVects ofair pollution. ATS News 1978;6:163.
9 Brimblecombe P. The big smoke: a history of air pollution inLondon since medieval times. London: Methuen, 1987.
10 Logan WPD. Mortality in the London fog incident 1952.Lancet 1953;i:3368.
11 Graham NM. The epidemiology of acute respiratory infec-tions in children and adults: a global perspective. EpidemiolRev 1990;12:14978.
12 Dockery DW, Pope III CA. Acute respiratory eVects of par-ticulate air pollution.Annu Rev Public Health 1994;15:10732.
13 Bascom R, Bromberg PA, Costa DA, et al. Health eVects ofoutdoor air pollution.Am J Respir Crit Care Med1996;153:350, 47798.
14 WoodruV TJ, Grillo J, Schoendorf KG. The relationship
between selected causes of postneonatal infant mortalityand particulate air pollution in the United States. EnvironHealth Perspect1997;105:60812.
15 Pope III CA, Dockery DW, Schwartz J. Review of epidemio-logical evidence of health eVects of particulate airpollution. Inhalat Toxicol 1995;7:118.
16 Pope III CA, Bates DV, Raizenne ME. Health eVects of par-ticulate air pollution:time for reassessment. Environ HealthPerspect1995;103:47280.
17 Schwartz J, Dockery DW, Neas LM. Is daily mortality asso-ciated specifically with fine particles? J Air Waste Manage-ment Assoc 1996;46:92739.
18 US National Research Council (USNRC), Committee onIndoor Pollutants. Indoor pollutants. Washington, DC:National Academy Press, 1981.
19 Spengler JD, Sexton K. Indoor air pollution: a public healthperspective. Science 1983;221:917.
20 Samet JM, Spengler JD. Indoor air pollution: a health perspec-tive. Baltimore, Maryland: Johns Hopkins University Press,1991.
21 US National Research Council (USNRC). Human exposureassessment for airborne pollutants. Washington, DC: NationalAcademy of Science, 1991: 321.
22 Sexton K, Ryan PB, Watson AY, et al. Assessment of humanexposure to air pollution: methods, measurements, andmodels. In: Air pollution, the automobile, and public health.Washington, DC: National Academy Press, 1988: 20738.
23 Smith KR. Total exposure assessment. Part 1: Implicationsfor the US. Environment1988;30:1015, 338.
24 Smith KR. Total exposure assessment. Part 2: Implicationsfor developing countries. Environment 1988;30:1620,2835.
25 Smith KR. Fuel combustion, air pollution exposure, andhealth: the situation in developing countries. Ann RevEnviron Energy 1993;18:52966.
26 World Health Organization (WHO). Health and environmentin sustainable development. Geneva: WHO, 1997.
27 Reddy AKN, Williams RH, Johansson TB. Energy after Rio:prospects and challenges. New York: United NationsDevelopment Programme, 1997: 176.
28 World Health Organization/United Nations EnvironmentProgramme (WHO/UNEP). Urban air pollution in mega-cities of the world. Oxford: Blackwell, 1992.
29 Neas LM, Dockery DW, Ware JH, et al. Association ofindoor nitrogen dioxide with respiratory symptoms andpulmonary function in children. Am J Epidemiol 1991;134:20419.
30 Braun-Fahrlnder C, Ackermann-Liebrich U, Schwartz J, etal. Air pollution and resiratory symptoms in pre-schoolchildren. Am Rev Respir Dis 1992;145:427.
31 Hasselblad V, Eddy DM, Kotchmar DJ. Synthesis ofenvironmental evidence: nitrogen dioxide epidemiologystudies. J Air Waste Management Assoc 1992;42:66271.
32 Samet JM, Lambert WE, Skipper BJ, et al. A study of respi-ratory illnesses in infants and nitrogen dioxide exposure.
Arch Environ Health 1992;47:5763.33 Ackermann-Liebrich U, Rap R. Epidemiological eVects of
oxides of nitrogen, especially NO2. In: Holgate ST, SametJM, Koren HS, et al, eds. Air pollution and health. SanDiego: Academic Press, 1999.
34 Pasternack MS. Pneumonia in childhood. In: Fishman A,ed. Fishmans pulmonary diseases and disorders. 3rd ed. NewYork: McGraw-Hill, 1998:19972010.
35 World Health Organization (WHO). Technical bases for theWHO recommendations on the management of pneumonia inchildren at first-level health facilities. Geneva: WHO, 1991.
36 Reynolds HY, Elias JA. Pulmonary defense mechanismsagainst infections. In: Fishman A, ed. Fishmans pulmonarydiseases and disorders. 3rd ed. New York: McGraw-Hill,1998.
37 Cooper JA, Malek D. Residential solid fuels: environmentalimpacts and solutions. Beaverton: Oregon Graduate Insti-tute, 1982.
38 Smith KR, Uma R, Kishore VVN, et al. Greenhouse gasesfrom small-scale combustion in developing countries: householdstoves in India. Research Triangle Park, NC: US Environ-mental Protection Agency, 1999.
39 US Department of Health and Human Services (USD-HHS).A report of the Surgeon General:the health consequencesof smokingchronic obstructive lung disease. Washington,
DC: US Government Printing OYce, 1984.40 Morrow PW. Toxicological data on NOx: an overview. J
Toxicol Environ Health 1984;13:20527.41 Lippmann M. EVects of ozone on respiratory function and
structure. Annu Rev Public Health 1989;10:4967.42 Health EVects Institute. Diesel exhaust: a critical analysis of
emissions, exposure and health eVects. A special report of theInstitutes Diesel Working Group, April 1995.
43 Thomas PT, ZelikoV JT. Air pollutants: moderators of pul-monary host resistance against infection. In: Holgate ST,Samet JM,Koren HS, et al, eds.Air pollution and health. SanDiego: Academic Press, 1999, 3579.
44 Murray DM, Burmaster DE. Residential air exchange ratesin the United States: empirical and estimated parametricdistributions by season and climatic region. Risk Analysis1995;15:45965.
45 Spengler JD, Samet JM. A perspective on indoor andoutdoor air pollution. In: Samet J, Spengler J, eds. Indoor air
pollution: a health perspective. Baltimore: Johns HopkinsUniversity Press, 1991:129.
46 Smith KR. Indoor air pollution and the risk transition. In:Kasuga H, ed. Indoor air quality. Berlin: Springer-Verlag,1990: 44856.
47 Marbury M. Wood smoke. In: Samet J, Spengler J, eds.Indoor air pollution: a health perspective. Baltimore: JohnsHopkins University Press, 1991: 20922.
48 Kleeman MJ, Schauer JJ, Cass GR. Size and compositiondistribution of fine particulate matter emitted from woodburning, meat charbroiling, and cigarettes. Environ SciTechnol 1999;33:351623.
49 Pandey MR, Boleij JS, Smith KR, et al. Indoor air pollutionin developing countries and acute respiratory infection inchildren. Lancet1989;i:4279.
50 UN Environmental Program/World Health Organization(UNEP/WHO). Assessment of urban air quality. Geneva:World Health Organization, 1988.
51 McCracken JP,Smith KR.An annotated bibliography on acuterespiratory infections (ARI) and indoor air pollution: withemphasis on children under five in developing countries. Wash-ington, DC: Environmental Health Project, EnvironmentalHealth Division, OYce of Health and Nutrition, USAgency for International Development, 1997.
52 Sofoluwe GO. Smoke pollution in dwellings of infants withbronchopneumonia.Arch Environ Health 1968;16:6702.
53 Pandey M, Neupane R, Gautam A, et al. Domestic smoke
pollution and acute respiratory infections in a ruralcommunity of the hill region of Nepal. Environ Int1989;15:33740.
54 Campbell H, Armstrong JR, Byass P. Indoor air pollution indeveloping countries and acute respiratory infection inchildren. Lancet1989;i:1012.
55 ODempsey T, McArdle TF, Morris J, et al. A study of riskfactors for pneumococcal disease among children in a ruralarea of west Africa. Int J Epidemiol 1996;25:88593.
56 Armstrong JR, Campbell H. Indoor air pollution exposureand lower respiratory infections in young Gambianchildren. Int J Epidemiol 1991;20:4249.
57 Collings DA, Sithole SD, Martin KS. Indoor woodsmokepollution causing lower respiratory disease in children. TropDoctor1990;20:1515.
58 Kossove D. Smoke-filled rooms and lower respiratorydisease in infants. S Afr Med J1982;61:6224.
59 Campbell H, Byass P, Greenwood BM. Acute lower respira-tory infections in Gambian children: maternal perceptionof illness. Ann Trop Paediatr 1990;10:4551.
Indoor air pollution in developing countries 531
group.bmj.comon February 11, 2013 - Published bythorax.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://thorax.bmj.com/http://thorax.bmj.com/http://group.bmj.com/http://thorax.bmj.com/ -
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
15/16
60 Mtango FD, Neuvians D, Broome CV, et al. Risk factors fordeaths in children under 5 years old in Bagamoyo district,Tanzania. Trop Med Parasitol 1992;43:22933.
61 de Francisco A, Morris J,Hall AJ, et al. Risk factors for mor-tality from acute lower respiratory tract infections in youngGambian children (see comments). Int J Epidemiol1993;22:117482.
62 Johnson AW, Aderele WI. The association of household pol-lutants and socioeconomic risk factors with the short-termoutcome of acute lower respiratory infections in hospital-ized pre-school Nigerian children. Ann Trop Paediatr 1992;12:42132.
63 Shah N, Ramankutty V, Premila PG, et al. Risk factors forsevere pneumonia in children in south Kerala: a hospital-based case-control st udy. J Trop Pediatr 1994;40:2016.
64 Victora CG, Fuchs SC, Flores JA, et al. Risk factors forpneumonia among children in a Brazilian metropolitanarea. Pediatrics 1994;93:97785.
65 Boleij JS, Brunekreef B. Domestic pollution as a factorcausing respiratory health eVects. Chest 1989;96(Suppl3):36872S.
66 Ramakrishna J, Durgaprasad MB, Smith KR. Cooking inIndia: the impact of improved stoves on indoor air quality.Environ Int1989;15:34152.
67 Cerqueiro MC, Murtagh P, Halac A, et al. Epidemiologicrisk factors for children with acute lower respiratory tractinfection in Buenos Aires, Argentina: a matched case-control study. Rev Infect Dis 1990;12(Suppl 8):S10218.
68 Awasthi S, Glick HA, Fletcher RH. EVect of cooking fuelson respiratory diseases in preschool children in Lucknow,India. Am J Trop Med Hyg 1996;55:4851.
69 Morris K, Morgenlander M, Coulehan JL, et al. Wood-burning stoves and lower respiratory tract infection inAmerican Indian children.Am J Dis Child1990;144:1058;erratum 490.
70 Robin LF, Less PS, Winget M, et al. Wood-burning stovesand lower respiratory illnesses in Navajo children. PediatrInfect Dis J1996;15:85965.
71 Honicky RE, Osborne JSD, Akpom CA. Symptoms ofrespiratory illness in young children and the use ofwood-burning stoves for indoor heating. Pediatrics 1985;75:58793.
72 Butterfield P, Edmundson E, LaCava G, et al. Woodstovesand indoor air: the eVects on preschoolers upperrespiratory systems. J Environ Health 1989;52:1723.
73 Browning KG, Koenig J, Checkoway H, et al. A question-naire study of respiratory health in areas of high and lowambient wood smoke pollution. Pediatr Asthma AllergyImmunol1990;4:183191.
74 Sharma S, Sethi GR, Rohtagi A, et al. Indoor air quality andacute lower respiratory infection in Indian urban slums.Environ Health Perspect 1998;106:2917.
75 Awasthi S, Glick HA, Fletcher RH, et al. Ambient air pollu-tion and respiratory symptoms complex in preschoolchildren. Indian J Med Res 1996;104:25762.
76 Surjadi C. Respiratory diseases of mothers and children andenvironmental factors among households in Jakarta.Environment Urbanization 1993;5:7886.
77 Mishra V, Retherford RD. Cooking smoke increases the risk ofacute respiratory infections in children. National FamilyHealth Survey Bulletin #8. Mumbai and East-West Center,
Honolulu: International Institute for Population Sciences,1997.78 Larson TV, Koenig JQ. Wood smoke: emissions and
noncancer respiratory eVects. Annu Rev Public Health1994;15:13356.
79 Honicky RE, Osborne JSD. Respiratory eVects of woodheat: clinical observations and epidemiologic assessment.Environ Health Perspect 1991;95:1059.
80 Tuthill RW. Woodstoves, formaldehyde, and respiratory dis-ease. Am J Epidemiol1984;120:9525.
81 Dockery DW, Speizer FE, Stram DO, et al. EVects of inhal-able particles on respiratory health of children. Am RevRespir Dis 1989;139:58794.
82 Azizi BH, Henry RL. EVects of indoor air pollution on lungfunction of primary school children in Kuala Lumpur.Pediatr Pulmonol1990;9:249.
83 Azizi BH, Henry RL. The eVects of indoor environmentalfactors on respiratory illness in primary school children inKuala Lumpur. Int J Epidemiol 1991;20:14450.
84 Anderson HR. Respiratory abnormalities in Papua NewGuinea children: the eVects of locality and domestic woodsmoke pollution. Int J Epidemiol 1978;7:6372.
85 Guneser S, Atici A, Alparslan N, et al. EVects of indoorenvironmental factors on respiratory systems of children. JTrop Pediatr 1994;40:1146.
86 Gharaibeh NS. EVects of indoor air pollution on lung func-tion of primary school children in Jordan. Ann Trop Paedi-atr1996;16:97102.
87 Victora CG, Kirkwood BR, Ashorth A, et al. Potential inter-ventions for the prevention of childhood pneumonia indeveloping countries: improving nutrition. Am J Clin Natr1999;70:30920.
88 Mavalankar DV, Trivedi CR, Grah RH. Levels and risk fac-tors for perinatal mortality in Ahmedabad, India. BullWHO 1991;69:43542.
89 Dejmek J, Selevan SG, Benes I, et al. Fetal growth andmaternal exposure to particulate matter during pregnancy.Environ Health Perspect 1999;107:47580.
90 Wang X,Ding H, Ryan L, et al. Association between air pol-lution and low birth weight: a community-based study.Environ Health Perspect 1997;105:51420.
91 Boy E, Delgado H, Bruce N. Birth weight and exposure tokitchen wood smoke during pregnancy. In: Child andadolescent health Geneva: World Health Organization, 1999.
92 Ikeda K, Iwata T, eds. CO as a tracer for assessing exposures toparticulates in wood and gas cookstove households of highlandGuatemala.Indoor Air 96,Nagoya. Tokyo, Institute of Pub-
lic Health, 1996.93 Dunn A, Zeise L, eds. Health eVects of exposure to
environmental tobacco smoke. Sacramento: California Envi-ronmental Protection Agency (CalEPA), 1997.
94 Ritz B, Yu F. The eVect of ambient carbon monoxide on lowbirth weight among children born in Southern Californiabetween 1989 and 1993. Environ Health Perspect 1999;107:1725.
95 Pereira LAA, Loomis D, Conceicao GMS, et al. Associationbetween air pollution and intrauterine mortality in SaoPaulo, Brazil. Environ Health Perspect 1998;106:3259.
96 Smith KR, Rasmussen RA, Manegdeg F, et al. Greenhousegases from small-scale combustion in developing countries: a pilotstudy in Manila. Research Triangle Park,NC: Global Emis-sions and Control Division, USEPA, 1992.
97 Zhang J,Smith KR. Emissions of carbonyl compounds fromvarious cookstoves in China. Environ Sci Technol 1999;15:231120.
98 Nardell EA, Kent D. Respiratory infections in the economi-cally disadvantaged. In: Fishman A, ed. Fishmans pulmo-nary diseases and disorders. 3rd ed. New York:McGraw-Hill,1998: 218798.
99 Smith KR. Indoor air pollution in India (editorial). Natl
Med J India 1996;9:1034.100 McMichael AJ, Smith KR. Air pollution and health: seek-ing a global perspective (editorial). Epidemiology 1999;10:14.
101 Cleary G, Blackburn C. Air pollution in native huts in thehighlands of New Guinea. Arch Environ Health 1968;17:78594.
102 Anderson H. Chronic lung disease and asthma in HighlandNew Guinea. MD thesis. Melbourne University, 1974.
103 Hofmann D, Wynder EL. Respiratory carcinogens: theirnature and precursors. International Symposium on Identifi-cation and Measurement of Environmental Pollutants, 1417
June 1971. Ottawa: Natural Research Council of Canada.104 CliVord P. Carcinogens in the nose and throat: naso-
pharyngeal carcinoma in Kenya. Proc R Soc Med 1972;65:6826.
105 Boleij J, Campbell H, Wafula E, et al. Biomass fuelcombustion and indoor air quality in developing countries.In: Perry R, Kirk P, eds. Proceedings of the Indoor and Ambi-ent Air Quality Symposium. London: Selper, 1988.
106 Aggarwal A, Raiyani C, Patel P, et al. Assessment of expo-sures to benzo(a)pyrene in air for various populationgroups in Ahmedabad. Atmos Environ 1982;16:86770.
107 Patel RS, Raiyani CV, Rao MN et al. Indoor air pollutionproblems: traditional versus modern fuels. In: Berglund B,Lindvall T,Sundall J, eds. Proceedings of the 3rd InternationalConference on Indoor Air Quality and Climate, Stockholm:Swedish Council for Building Research, 1984.
108 Menon P. Indoor spatial monitoring of combustion generatedpollutants (TSP, CO, and BaP) by Indian cookstoves.UHMET 88-01. Honolulu: Department of Meteorology,University of Hawaii, 1988.
109 Davidson C, Lin S, Osborn JF, et al. Indoor and outdoorair pollution in the Himalayas. Environ Sci Technol1986;20:5617.
110 Mumford J, He X, Chapman Rea. Lung cancer and indoorpollution in Xuan Wei, China. Science 1987;235:21735.
111 Smith K, Aggarwal A, Dave R. Air pollution and rural bio-mass fuels in developing countries: a pilot village study inIndia and implications for research and policy. Atmos Envi-ron 1983;17:234362.
112 Ramakrishna J. Patterns of domestic air pollution in India.PhD Dissertation, University of Hawaii, Honolulu, 1988.
113 Saksena S, Prasad R, Pal RC, et al. Patterns of daily expo-sure to TSP and CO in the Garhwal Himalaya. AtmosEnviron 1992;26A:212534.
114 Reid H, Smith K, Sherchand B. Indoor smoke exposuresfrom traditional and improved cookstoves: comparisonsamong rural Nepali women. J Mountain Res Dev 1986;6:293304.
115 Pandey M, Neupane R, Gautam A, et al. The eVectivenessof smokeless stoves in reducing indoor air pollution in arural region of Nepal.J Mountain Res Dev 1990;10:31320.
116 UNDP. Human Development Report. New York: UnitedNations Development Programme, 1998.
532 Smith, Samet, Romieu, et al
group.bmj.comon February 11, 2013 - Published bythorax.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://thorax.bmj.com/http://thorax.bmj.com/http://group.bmj.com/http://thorax.bmj.com/ -
7/29/2019 Indoor Air Polution in Developing Countries and Acute Lower Respiratory Infection in Children
16/16
doi: 10.1136/thorax.55.6.5182000 55: 518-532Thorax
Kirk R Smith, Jonathan M Samet, Isabelle Romieu, et al.childrenand acute lower respiratory infections inIndoor air pollution in developing countries
http://thorax.bmj.com/content/55/6/518.full.htmlUpdated information and services can be found at:
These include:
References
http://thorax.bmj.com/content/55/6/518.full.html#related-urlsArticle cited in:
http://thorax.bmj.com/content/55/6/518.full.html#ref-list-1This article cites 67 articles, 16 of which can be accessed free at:
serviceEmail alerting
box at the top right corner of the online article.Receive free email alerts when new articles cite this article. Sign up in the
CollectionsTopic
(384 articles)Pneumonia (respiratory medicine)(396 articles)Pneumonia (infectious disease)
(65 articles)Internet(904 articles)TB and other respiratory infections
(183 articles)Environmental issues(85 articles)Air pollution
Articles on similar topics can be found in the following collections
Notes
http://group.bmj.com/group/rights-licensing/permissionsTo request permissions go to:
http://journals.bmj.com/cgi/reprintformTo order reprints go to:
http://group.bmj.com/subscribe/To subscribe to BMJ go to:
group.bmj.comon February 11, 2013 - Published bythorax.bmj.comDownloaded from
http://thorax.bmj.com/content/55/6/518.full.htmlhttp://thorax.bmj.com/content/55/6/518.full.htmlhttp://thorax.bmj.com/content/55/6/518.full.html#related-urlshttp://thorax.bmj.com/content/55/6/518.full.html#related-urlshttp://thorax.bmj.com/content/55/6/518.full.html#ref-list-1http://thorax.bmj.com/cgi/collection/pneumonia2http://thorax.bmj.com/cgi/collection/pneumonia2http://thorax.bmj.com/cgi/collection/pneumonia2http://thorax.bmj.com/cgi/collection/pneumonia2http://thorax.bmj.com/cgi/collection/pneumonia2http://thorax.bmj.com/cgi/collection/pneumoniahttp://thorax.bmj.com/cgi/collection/pneumoniahttp://thorax.bmj.com/cgi/collection/pneumoniahttp://thorax.bmj.com/cgi/collection/internethttp://thorax.bmj.com/cgi/collection/tb_and_other_respiratory_infectionshttp://thorax.bmj.com/cgi/collection/internethttp://thorax.bmj.com/cgi/collection/tb_and_other_respiratory_infectionshttp://thorax.bmj.com/cgi/collection/tb_and_other_respiratory_infectionshttp://thorax.bmj.com/cgi/collection/tb_and_other_respiratory_infectionshttp://thorax.bmj.com/cgi/collection/environmental_issueshttp://thorax.bmj.com/cgi/collection/environmental_issueshttp://thorax.bmj.com/cgi/collection/environmental_issueshttp://group.bmj.com/group/rights-licensing/permissionshttp://group.bmj.com/group/rights-licensing/permissionshttp://journals.bmj.com/cgi/reprintformhttp://journals.bmj.com/cgi/reprintformhttp://group.bmj.com/subscribe/http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://thorax.bmj.com/http://thorax.bmj.com/http://group.bmj.com/http://thorax.bmj.com/http://group.bmj.com/subscribe/http://journals.bmj.com/cgi/reprintformhttp://group.bmj.com/group/rights-licensing/permissionshttp://thorax.bmj.com/cgi/collection/pneumonia2http://thorax.bmj.com/cgi/collection/pneumoniahttp://thorax.bmj.com/cgi/collection/internethttp://thorax.bmj.com/cgi/collection/tb_and_other_respiratory_infectionshttp://thorax.bmj.com/cgi/collection/environmental_issueshttp://thorax.bmj.com/cgi/collection/air_pollutionhttp://thorax.bmj.com/content/55/6/518.full.html#related-urlshttp://thorax.bmj.com/content/55/6/518.full.html#ref-list-1http://thorax.bmj.com/content/55/6/518.full.html