Lapjag Bangsal 27-08-2014
-
Upload
alvin-bernard -
Category
Documents
-
view
217 -
download
0
Transcript of Lapjag Bangsal 27-08-2014
-
8/11/2019 Lapjag Bangsal 27-08-2014
1/22
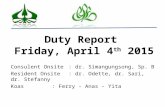
DUTY REPORT
27th
AUGUST 2014
GP on duty : dr. Ananita
Resident on duty : dr. Ardhestiro
Co-ass on duty : Alvin & Tedy
-
8/11/2019 Lapjag Bangsal 27-08-2014
2/22
PATIENTS RECAPITULATION
3rd floor :Mr. T > Myelodysplastic SyndromeMr. A > Anemia et causa hematoschezia
4th floor :
5th floor :Mrs. W > intraabdominal mass with anaemiaMrs. S > chronic diarrhea with HIVMrs. S> loss of consciousness et causa hypoglycaemia
6th floor :Mr. W > Dengue FeverMr. R > Hemorrhagic shockMr. A > anaemia with Carcinoma nasopharynx
-
8/11/2019 Lapjag Bangsal 27-08-2014
3/22
PATIENTS IDENTITY
Name : Mr. WSex : Male
Place, Date of Born : Jakarta, 21th November 1983Age : 30 years oldJob : ArmyReligion : Moslem
Marital Status : MarriedEthnic/Race : JavaneseAddress : Komplek Nagrag, Bogor
-
8/11/2019 Lapjag Bangsal 27-08-2014
4/22
Chief complaint : Patient came to ward with chiefcomplaint of fever 6 days before admission.
Additional complaint : headache, pain in his joint andmuscle, pain behind his eyeballs
4
-
8/11/2019 Lapjag Bangsal 27-08-2014
5/22
History of Present Illness
History of Present Illness:Patient came to the ward with the chief complaint of fever 6 daysbefore admission. The fever doesnt have a specific time, and it
goes fluctuating every day, had not given drugs for the fever butpatient went immediately to the hospital near his house. Hedidnthave a complain of his arm and leg with a red spots from 3days before admission. He complained about his pain in thejoint, muscle and behind his eye balls. He didnt have any
complained about spontaneous bleeding like gum bleeding ornose bleed or dark stool. He still wanted to eat and drink byhimself.
He didnthave any complain like palpitation, excessive sweating,abnormal breathing.
-
8/11/2019 Lapjag Bangsal 27-08-2014
6/22
Patient didnt have a history of sore throat, no cough, and no
symptoms of flu, no history of heavy breathing
No history of travelling, go to flood areas, no history of rat bite.
No history of diarrhea, he had no complaint in urinating and nocomplain in defecation.
He have a history of hypertension but it is not controlled by drugs
nor goes to the doctor or health care routine to check his bloodpressure
-
8/11/2019 Lapjag Bangsal 27-08-2014
7/22
History of Past Illness
He didnt have a history of diabetes, kidney and lungsdisease
He had underwent cardiac catheterisation et causaatherosclerosis
He never experienced these symptoms before
-
8/11/2019 Lapjag Bangsal 27-08-2014
8/22
History of family illness His mother suffered from hypertension
His father suffered from cardiac disease
No history of diabetes No family members have the similar symptoms
-
8/11/2019 Lapjag Bangsal 27-08-2014
9/22
History of Socio-Habits
He neither smokes, drinks alcohol, nor uses anyforbidden drug.
He could still eat and drink well
-
8/11/2019 Lapjag Bangsal 27-08-2014
10/22
Physical Examination
General State : Mildly sick Consciousness : Fully alert
Vital Signs
Blood Pressure : 120/70 mmHg Heart rate : 88 bpm (regular) Respiratory Rate : 18 times/minute Temperature : 36.7 oC
Body Weight : 75 kg Body Height : 173 cm BMI : 25.0 (Normoweight)
-
8/11/2019 Lapjag Bangsal 27-08-2014
11/22
General Examination
Head : Normocephal
Eye : anemic conjunctiva (-/-), icteric sclera (-/-)
Ears : discharge (-)
Nose : septum deviation (-), discharge (-)
Mouth : coated tongue (-), hyperemic pharynx (-), normal T1-T1,
pale mouth mucosa (-), dried mucosa (-)
Neck : lymph nodes enlargement (-)
-
8/11/2019 Lapjag Bangsal 27-08-2014
12/22
Thorax: symmetric, intercostals retraction (-)
COR
Inspection: Ictus cordis (-)
Palpation: heave (-), lift (-), thrill (-)
Percussion:
Right border:ICS V, linea midclavicularis dekstra
Left border : ICS V, linea midclavicularis sinistra
Heart waist: ICS IV, linea parasternal sinistra
Auscultation : regular 1stand 2ndheart sound, murmur (-),
gallop (-)
-
8/11/2019 Lapjag Bangsal 27-08-2014
13/22
PULMO
Inspection : chest within normal shape, symmetries on static and
dynamic state
Palpation : tactile vocal fremitus both lungs were symmetries, chest
expansion symmetries
Percussion : resonant both lungs
Auscultation : vesicular breathing sounds, rales (-/-), wheezing (-/-)
Abdomen : flat, not distended
timpani, no enlargement of liver & spleen
Extremities : warm, petechiae on extremities (-), CRT < 2 seconds, torniquet
test (-)
-
8/11/2019 Lapjag Bangsal 27-08-2014
14/22
Laboratory Results(27/08/2014)
Hemoglobin: 13.6 g/dL
Hematocrite : 38%
Erytrocyte : 5.0
Leukocyte : 4300 Platelet : 28.000
MCV : 76
MCH : 27
MCHC : 36
-
8/11/2019 Lapjag Bangsal 27-08-2014
15/22
RESUMEMr. W, 30 years old, came to ward with the chief complaint of fever 6
days before admission. The fever doesnthave a specific time, and itgoes fluctuating every day, had not given drugs for the fever butpatient went immediately to the hospital near his house. He didnt
have a complain of his arm and leg with a red spots from 3 daysbefore admission. He complained about his pain in the joint,muscle and behind his eye balls. He didnt have any complainedabout spontaneous bleeding like gum bleeding or nose bleed ordark stool. He still wanted to eat and drink by himself.
He didnt have any complain like palpitation, excessive sweating,abnormal breathing.
Physical examination showed normal sign
Laboratory results showed WBC 4300, Platelet 28.000/uL.
-
8/11/2019 Lapjag Bangsal 27-08-2014
16/22
Diagnosis
Working diagnosis
Dengue fever
Differential diagnosis
Dengue Hemorrhagic Fever
Malaria Urinary Tract Infection
Leptospirosis
-
8/11/2019 Lapjag Bangsal 27-08-2014
17/22
List of Problem
Dengue Fever
-
8/11/2019 Lapjag Bangsal 27-08-2014
18/22
Discussion Dengue Fever, Based on:
HT and PE:
history of sudden fever 2 7 days, biphasic with 2 or more of
this sign or symptoms:
headache
retro orbital pain
myalgia
athralgia
Lab: Thrombocytopenia ( < 100.000/mm3) 28.000/mm3
Leukopenia > 4300 with no sign of plasma leakage
-
8/11/2019 Lapjag Bangsal 27-08-2014
19/22
Dengue fever grading
Dengue Fever : Fever with 2 or more symptoms likeheadache, retro-orbital pain, myalgia, athralgia
Grade I: Fever with untypical constitutional symptoms,bleeding manifestation (+) by tourniquet test
Grade II: Grade I with spontaneous bleeding
Grade III: Compensated DSS (characterized by tachy- or
bradycardia or hypotension, with cold skin andagitated)
Grade IV:Uncompensated DSS (characterized by irregular bloodpressure and heart rate)
-
8/11/2019 Lapjag Bangsal 27-08-2014
20/22
Plan and Treatment Non-pharmacological
interventions:
Bed rest
Oral fluid intake max.2L/day
Diet calories 2168calories/day
Pharmacologicalinterventions:
IVFD RL 1800 cc / 24hours
Diagnostic plans:
IgM IgG antidengue
Monitoring plans:
CBC q12hrs
Urine output
-
8/11/2019 Lapjag Bangsal 27-08-2014
21/22
Prognosis
Quo ad Vitam : dubia ad bonam
Quo ad Functionam : ad bonam
Quo ad Sanationam : ad bonam
-
8/11/2019 Lapjag Bangsal 27-08-2014
22/22
THANK YOU