Disclosures New Antibiotics for Gram Negative...
Transcript of Disclosures New Antibiotics for Gram Negative...
4/5/16
1
New Antibiotics for Gram Negative Infections
April 16, 2016 Benjamin Colton, PharmD, BCPS Infectious Diseases Clinical Pharmacist, Antimicrobial Stewardship National Institutes of Health Clinical Center [email protected] 1
Disclosures • Grant/Research Support:
– None to disclose • Speakers Bureau:
– Cubist Pharmaceuticals • Advisory Board:
– None to disclose This continuing education activity is managed and accredited by Professional Education Services Group in cooperation with the NIH Pharmacy Department. PESG, NIH, and all accrediting organization do not support or endorse any product or service mentioned in this activity PESG and NIH staff has no financial interest to disclose.
2
Objectives At the conclusion of this activity, the participant will be able to: 1. Compare and contrast key aspects of the clinical pharmacology and
antimicrobial spectra of ceftazidime-avibactam and ceftolozane-tazobactam that guide their role in the treatment of multidrug-resistant gram-negative pathogens.
2. Illustrate key limitations in the current evidence supporting the use of ceftazidime-avibactam and ceftolozane-tazobactam for the treatment of multidrug-resistant gram-negative pathogens.
3. Recommend an appropriate antimicrobial regimen for an infection caused by a multi-drug resistant gram-negative pathogen.
4. Identify potential candidate antimicrobial agents with activity against drug-resistant gram-negative pathogens entering or nearing completion of Phase 3 clinical trials.
3
Antimicrobial Resistance Threats
CDC. Antibiotic resistance threats in the United States. 2013. 4
CDC. Antibiotic resistance threats in the United States. 2013. 5 CDC. Antibiotic resistance threats in the United States. 2013. 6
4/5/16
2
CDC. Antibiotic resistance threats in the United States. 2013. 7
Gram Negative HAIs Pathogen Overall
No. (%) CLABSI No. (%)
CAUTI No. (%)
VAP No. (%)
SSI No. (%)
Escherichia coli 9,351 (11.5%) 1,206 (4.0%) 5,660 (26.8%) 504 (5.9%) 1,981 (9.4%) Klebsiella pneumoniae & oxytoca
6,470 (8.0%) 2,407 (7.9%) 2,365 (11.2%) 854 (10.1%) 844 (4.0%)
Pseudomonas aeruginosa 6,111 (7.5%) 1,166 (3.8%) 2,381 (11.3%) 1,408 (16.6%) 1,156 (5.5%) Enterobacter species 3,821 (4.7%) 1,365 (4.5%) 880 (4.2%) 727 (8.6%) 849 (4.0%) Proteus spp. 2,031 (2.5%) 232 (0.8%) 1,013 (4.8%) 119 (1.4%) 667 (3.2%) Serratia spp. 1,737 (2.1%) 762 (2.5%) 204 (1.0%) 386 (4.6%) 385 (1.8%) Acinetobacter baumannii 1,490 (1.8%) 629 (2.1%) 185 (0.9%) 557 (6.6%) 119 (0.6%)
8 Sievert DM, et al. Infect Control Hosp Epidemiol. 2013
Expressed as percent of all infections. CLABSI, Catheter Line Associated Bloodstream Infection; CAUTI, Catheter-Associated Urinary Tract Infection; VAP, Ventilator-Associated Pneumonia; SSI, Surgical Site Infection
Gram Negative Resistance Pathogen and Resistance 2006 – 2007 2009 – 2010 Percent Change Escherichia coli Extended-Spectrum Cephalosporin Resistant Carbapenem Resistant
6.1 % 3.0 %
13.2 % 2.2 %
+ 7.1 % - 0.8 %
Klebsiella pneumoniae & oxytoca Extended-Spectrum Cephalosporin Resistant Carbapenem Resistant
22.5 % 7.6 %
25.4 % 11.9 %
+ 2.9 % + 4.3 %
Pseudomonas aeruginosa Extended-Spectrum Cephalosporin Resistant Carbapenem Resistant Fluoroquinolone Resistant
12.8 % 23.2 % 28.5 %
23.3 % 22.5 % 29.6 %
+ 10.5 % - 0.7 % + 1.1 %
9 Hidron AI, et al. Infect Control Hosp Epidemiol. 2010 Sievert DM, et al. Infect Control Hosp Epidemiol. 2013 CDC. Antibiotic Resistance Patient Safety Atlas. http://gis.cdc.gov/grasp/PSA/MapView.html. Accessed 04.2016.
Extended-Spectrum Cephalosporin Resistant: Resistance to 3rd-generation cephalosporins including ceftriaxone and ceftazidime
Systemic Antibacterial Approvals
0
2
4
6
8
10
12
14
16
18
1983-1987 1988-1992 1993-1997 1998-2002 2003-2007 2008-2012 2013-Present Modified from Boucher HW, et al. Clin Infect Dis. 2013 10
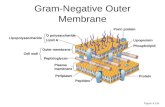
Gram-Negative Mechanisms of Resistance
Peleg A, Hooper D. N Engl J Med 2010;362:1804-1813
Ceftolozane-Tazobactam • Ceftolozane
– Broad-spectrum cephalosporin – Enhanced anti-psuedomonal
activity • Tazobactam
– Sulfone beta-lactamase inhibitor
– Irreversible inhibition
12
4/5/16
3
Structural Activity Relationships
Zhanel GG, et al. Drugs. 2014;74:31-51. 13
Antimicrobial Spectra Gram-Negatives Enterobacter cloacae Escherichia coli Klebsiella oxytoca Klebsiella pneumoniae Proteus mirabilis Pseudomonas aeruginosa
Acinetobacter baumannii Burkholderia cepacia Citrobacter freundii Citrobacter koseri Enterobacter aerogenes Enterobacter cloacae Haemophilus influenzae Moraxella catarrhalis Morganella morganii Pantoea agglomerans Proteus vulgaris Providencia rettgeri Providencia stuartii Serratia liquefacians Serratia marcescens
Gram-Positives Streptococcus anginosus Streptococcus constellatus Streptococcus salivarius Streptococcus agalactiae Streptococcus intermedius Streptococcus pyogenes Streptococcus pneumoniae
Zerbaxa™ (Ceftolozane-Tazobactam) Package Insert. Merck & Co., Inc. 2015. 14
Anaerobes Bacteroides fragilis Fusobacterium spp. Prevotella spp.
Pharmacokinetics Ceftolozane 2 gm IV infused over 1 hr Cmax (mcg/mL) Tmax (h) AUC (mcg*h/L) t1/2 (h)
Single Dose 69.1 1.02 172 2.77 Steady State 74.4 1.07 182 3.12
Zerbaxa™ (Ceftolozane-Tazobactam) Package Insert. Merck & Co., Inc. 2015. 15
Tazobactam 500 mg IV infused over 1 hr Cmax (mcg/mL) Tmax (h) AUC (mcg*h/L) t1/2 (h)
Single Dose 18.4 1.02 24.4 0.91 Steady State 18 1.01 25 1.03
Complicated Urinary Tract Infections • Randomised, double-blind, double-dummy, multi-
center, non-inferiority trial • Comparators
– Ceftolozane-Tazobactam 1.5 gm IV Q8H – Levofloxacin 750 mg IV Q24H
• Primary Outcome – Non-inferiority of composite cure rate at the test-of-cure
visit in the microbiological modified-intent-to-treat population.
Wagenlehner FM, et al. Lancet. 2015;385(9981):1949-56.
16
ASPECT-cUTI
Wagenlehner FM, et al. Lancet. 2015;385(9981):1949-56.
17
Outcomes with Resistant Pathogens
Wagenlehner FM, et al. Lancet. 2015;385(9981):1949-56. 18
4/5/16
4
ASPECT-cUTI Limitations • Inferior comparator • Lack of an option for de-escalation • Lack of an intravenous-to-oral switch • Inappropriate dose reductions for levofloxacin
19
ASPECT-cIAI • Multicenter, prospective, randomized, double-blind,
placebo-controlled trial • Comparators
– Ceftolozane-Tazobactam 1.5 gm IV Q8H PLUS Metronidazole 500 mg IV Q8H
– Meropenem 1 gm IV Q8H PLUS Placebo • Primary Outcome
– Noninferiority of ceftolozane-tazobactam plus metronidazole to meropenem
Solomkin J, et al. Clin Infect Dis. 2015;60:1462-71. 20
Key Eligability Criteria Inclusion Criteria • Adults • Clinical evidence of cIAI • Planned or performed drainage
Exclusion Criteria • Low likelihood of adequate
source control • CLCr < 30 mL/min
Solomkin J, et al. Clin Infect Dis. 2015;60:1462-71.
21
Primary & Secondary Outcomes
Solomkin J, et al. Clin Infect Dis. 2015;60:1462-71. 22
Per-Pathogen Clinical Cure
95.8% 100.0% 100.0% 100.0%
87.5%
100.0%
88.5%
72.7%
90.0%
77.8% 75.0%
0.0% 0.0%
20.0%
40.0%
60.0%
80.0%
100.0%
Enterobacteriaceae ESBL +
Enterobacteriaceae CTX-M-14/15
E. coli ESBL +
E. coli CTX-M-14/15
K. pneumoniae ESBL +
K. pneumoniae CTX-M-14/15
Ceftolozane-Tazobactam + Metronidazole Meropenem
Solomkin J, et al. Clin Infect Dis. 2015;60:1462-71. 23
23/24 23/26 13/13 8/11 14/14 18/20 9/9 7/9 7/8 3/4 5/5 0/1
Clinical Cure & Impaired Renal Function Ceftolozane-Tazobactam
plus Metronidazole, n/N (%) Meropenem, n/N (%)
Normal/mild impairment (CLCr > 50 mL/min)
312/366 (85.2%) 355/404 (87.9%)
Moderate Impairment (CLCr 30 to ≤ 50 mL/min)
11/23 (47.8%) 9/13 (69.2%)
Solomkin J, et al. Clin Infect Dis. 2015;60:1462-71. 24
4/5/16
5
Geographic Clinical Cures Region Ceftolozane-Tazobactam +
Metronidazole, (n = 275) Meropenem,
(n = 321) Percentage Difference
(95% CI) Eastern Europe 213/221 (96.4 %) 239/247 (96.8 %) – 0.4 (– 4.10 to 3.12) Western Europe 2/5 (40.0 %) 7/11 (63.6 %) – 23.6 (– 58.95 to 22.86) North America 8/11 (72.7 %) 10/11 (90.9 %) – 18.2 (– 48.41 to 15.40) South America 28/28 (100 %) 40/42 (95.2 %) 4.8 (– 7.78 to 15.79) Rest of world 8/10 (80.0 %) 8/10 (80.0 %) 0 (– 34.14 to 34.14)
Solomkin J, et al. Clin Infect Dis. 2015;60:1462-71. 25
Ceftazidime-Avibactam • Ceftazidime
– Broad-spectrum cephalosporin – Poor gram-positive activity
• Avibactam – Novel bridged diazabicyclooctane (DBO)
non-β-lactam β-lactamase inhibitor – Reversible inhibitor
Zhanel GG, et al. Drugs. 2013; 73:159-77. 26
Avibactam • Synthetic,non-β-lactam • Covalent, reversible inhibitor • Inhibits β-lactamases of
– Class A – Class C – Class D (some)
Ehmann DE, et al. Proc Natl Acad Sci USA. 2012;109:11663-8. 27
β-Lactamase Inhibition β-Lactamase Avibactam
IC50 (nM)
Clavulanic Acid IC50 (nM)
Tazobactam IC50 (nM)
Class A TEM-1 SHV-4 KPC-2 CTX-M-15
8 3
170 5
58 4
> 100,000 12
32 55
50,000 6
Class C P99 AmpC
100 128
> 100,000 > 100,000
1,300 4,600
Stachyra T, et al. Antimicrob Agents Chemother. 2010;54:5132-8.
28
IC50, half maximal inhibitor concentration
Antimicrobial Spectra Gram-Negatives Citrobacter freundii Citrobacter koseri Escherichia coli Enterobacter aerogenes Enterobacter cloacae Haemophilus influenzae Haemophilus parainfluenzae Klebsiella pneumoniae Klebsiella oxytoca Morganella morganii
Proteus spp. Providencia stuartii Pseudomonas aeruginosa Pseudomonas stutzeri Serratia marcescens
Gram-Positives Staphylococcus aureus (MSSA strains only)
Avycaz™ (Ceftazidime-Avibactam) Package Insert. Actavis, Inc. 2015. 29
Pharmacokinetics Ceftazidime 2 gm infused over 2 hours Cmax (mg/L) AUC (mg*h/L) t1/2 (h) CL (L/h) Vss (L) Single dose 88.1 289 3.27 6.93 18.1 Steady state 90.4 291 2.76 6.86 17.0
Avycaz™ (Ceftazidime-Avibactam) Package Insert. Actavis, Inc. 2015.
30
Avibactam 500 mg infused over 2 hours Cmax (mg/L) AUC (mg*h/L) t1/2 (h) CL (L/h) Vss (L) Single dose 15.2 42.1 2.22 11.9 23.2 Steady state 14.6 38.2 2.71 13.1 22.2
4/5/16
6
Complicated Urinary Tract Infections • Phase II, prospective, randomized, investigator- & patient-
blinded, multicenter study • Comparators
– Ceftazidime-Avibactam 625 mg IV Q8H – Imipenem-Cilastatin 500 mg IV Q8H
• De-escalation to oral ciprofloxacin was permitted after 4 days
• Primary Outcome – Favorable microbiological response at the test-of-cure in the
microbiologically evaluable population
Vazquez JA, et al. Curr Med Res Opin. 2012;28:1921-31. 31
Study Population
Vazquez JA, et al. Curr Med Res Opin. 2012;28:1921-31.
32
Patients Randomized (N = 137)
Ceftazidime-Avibactam, n = 69 Safety Population, n = 68
Completed, n = 49
Imipenem-Cilastatin, n = 68 Safety Population, n = 67
Completed, n = 54
MITT n = 46
ME n = 27
CE n = 28
MITT n = 49
ME n = 35
CE n = 36
Clinical and Microbiological Response Ceftazidime-Avibactam (n = 46)
Imipenem-Cilastatin (n = 49)
Observed Difference
Microbiological Response Eradication Persistance Indeterminate
31 (67.4%) 10 (21.7%) 5 (10.9%)
31 (63.3%) 14 (28.6%) 4 (8.2%)
4.1 (-16.1, 23.8)
Clinical Response Cure Failure Indeterminate
37 (80.4%) 5 (10.9%) 4 (8.7%)
36 (73.5%) 9 (18.4%) 4 (8.2%)
7.0 (-11.6, 24.7)
Clinical & Microbiological Response Cure + Eradication Failure + Persistance or Indeterminate
29 (63.0%) 17 (37.0%)
25 (51.0%) 24 (49.0%)
12 (-9.1, 31.7)
Center for Drug Evaluation and Research. AVYCAZ: Medical Review. 02.25.2015. Available at accessdata.fda.gov
33
Complicated Intra-Abdominal Infections • Prospective, randomized, multicenter, double-dummy,
double-blinded, comparative study • Comparators
– Ceftazidime-Avibactam 2.5 gm IV Q8H infused over 2 hours PLUS Metronidazole 500 mg IV Q8H
– Meropenem 1 gm IV Q8H infused over 30 minutes • Primary Outcome
– Non-inferiority of clinical cure at the test-of-cure visit Mazuski JE, et al. Clin Infect Dis. 2016. 34
Clinical Outcomes mMITT Population Ceftazidime-Avibactam +
Metronidazole (n = 413) Meropenem (n = 410)
Difference % (95% CI)
Cure at TOC 337 (81.6%) 349 (85.1%) - 3.5 % (-8.64, 1.58) Cure at EOT 361 (87.4%) 379 (92.4%) - 5.0 % (-9.24, -0.93) Cure at LFU 340 (82.3%) 347 (84.6%) - 2.3 % (-7.41, 2.79)
Mazuski JE, et al. Clin Infect Dis. 2016.
35
mMITT, microbiologically modified intent-to-treat; MITT, modified intent-to-treat; TOC, test-of-cure; EOT, end-of-treatment; LFU, late follow-up
MITT Population Ceftazidime-Avibactam + Metronidazole (n = 520)
Meropenem (n = 523)
Difference % (95% CI)
Cure at TOC 429 (82.5%) 444 (84.9%) - 2.4 % (-6.90, 2.10) Cure at EOT 459 (88.3%) 482 (92.2%) - 3.9 % (-7.57, -0.29) Cure at LFU 429 (82.5%) 436 (83.4%) - 0.9% (-5.45, 3.72)
Clinical Cure & Impaired Renal Function Ceftazidime-Avibactam + Metronidazole, n/N (%)
Meropenem, n/N (%)
Between Group Difference (95% CI)
mMITT CLCr > 50 mL/min CLCr 30 to ≤ 50 mL/min
322/379 (85.0%) 14/31 (45.2%)
321/373 (86.1%) 26/35 (74.3%)
-1.1 (-6.17, 3.97) -29.1 (-50.05, -5.36)
MITT CLCr > 50 mL/min CLCr 30 to ≤ 50 mL/min
407/476 (85.5%) 20/41 (48.8%)
410/478 (85.8%) 32/43 (74.4%)
-0.3 (-4.75, 4.21) -25.6 (-44.53, -4.78)
FDA. Ceftazidime-Avibactam – Summary Review. 2015; Mazuski JE, et al. Clin Infect Dis. 2016. 36
mMITT, microbiologically modified intent-to-treat; MITT, modified intent-to-treat
4/5/16
7
Poor Renal Function, Poor Outcomes Antibiotic Disease Study Drug, n/N (%) Comparator, n/N (%) Televancin cSSSI Mortality Mortality CLCr < 50 mL/min CLCr > 50 mL/min
58/86 (67.4%) 520/598 (87.0%)
67/81 (82.7%) 524/610 (85.9%)
Ceftolozane-Tazobactam cIAI Clinical Cure Clinical Cure CLCr 30 – 50 mL/min CLCr > 50 mL/min
11/23 (47.8%) 312/366 (85.2%)
9/13 (69.2%) 355/404 (87.9%)
Ceftazidime-Avibactam cIAI Clinical Cure Clinical Cure CLCr 30 – 50 mL/min CLCr > 50 mL/min
14/31 (45.2%) 322/379 (85.0%)
26/35 (74.3%) 321/373 (86.1%)
Telavancin. Prescribing Information. 2009. FDA. Ceftolozane-Tazobactam – Summary Review. 2014; Solomkin J, et al. Clin Infect Dis. 2015. FDA. Ceftazidime-Avibactam – Summary Review. 2015; Mazuski JE, et al. Clin Infect Dis. 2016.
37
cSSSI – complicated skin and skin structure infections; cIAI – complicated intra-abdominal infections
Conclusions
38
• Ceftolozane-tazobactam provides broad-spectrum activity against gram-positive and gram-negative pathogens, specifically Pseudomonas aeruginosa.
• Ceftazidime-avibactam provides broad-spectrum activity against gram-negative infections including some carbapenem-resistant Enterobacteriaceae.
Obtaining CME/CE Credit • If you would like to receive education credit for this
activity, please visit:
http://nih.cds.pesgce.com
39