Bronchial asthma (2)
-
Upload
vijay-prasad -
Category
Health & Medicine
-
view
86 -
download
0
Transcript of Bronchial asthma (2)

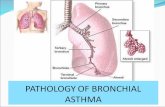
BRONCHIAL ASTHMA

Introducation
Asthma derived from Greek word- To stay awake in order to breath
ORDifficulty in breathing

Asthma is a chronic inflammatory disease in which patient suffers with reversible episodes of airway obstruction due to bronchial hyper responsiveness.

Early phase (Acute)
-Due to bronchial smooth muscle spasm.
- Excessive secretion of mucus.
Chronic phase Continuous
Inflammation, fibrosis, oedma, necrosis of bronchial epithelial cells.
It has 2phases

Clinical hallmarks
Recurrent episodic coughing Shortness of breathing Chest tightness Wheezing
Symptoms are worsening at night

Asthma described as two type Extrinsic(Atopic extrinsic asthma)It is associated with
exposure of specific allergen
Ex:- House dust, pollen It is episodic and less
prone to develop to status asthmaticus.
Intrinsic(Non atopic extrinsic asthma)It is associated with
some non specific stimulants
Ex:- chemical irritantsIt is perenial and prone
to develop to status asthmaticus.

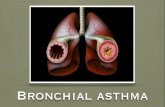
Pathophysiology Allergen enter (Foreign body)
Immunological reaction (AG:AB Complex formation)
Circulation in blood
Basophiles, Neutrophilis engulf
Cause neutralization contd..,

Whenever same allergen re exposed
Activation of AG:AB complex
Reacts with lung mast cells (Degranulation of mast cells)
Spasmogens release(Like Histamine,5HT,PGs,LT4, Cytokines)

Bronchial Tone
IgE-Antigen Complex
BasophilActivatio
n
Eosinophil
Activation
Chemical mediatorsHistamine, LTC4, LTD4, LTB4,Cytokines, Adenosine, PGD2, PAF,ECP and Neuropeptides
Cause inflammation, oedema, bronchospasm, muscus secretion, epithelial damage
Mast CellDegranulation
In early phase these mediators leads to bronchoconstriction
In late phase inflammation, pulmonary oedema, mucous secretion bronchial hypersensivity and epithelial damage

It divided into two categories
1. Short term relievers.( Bronchodilators)
2. Long term controllers.
Asthma therapy

Bronchial Tone
Bronchoconstriction
Bronchodilitation
Bronchial Smooth Muscle
β2
SALBUTAMOLβ2 AGONISTS 5AMP
AC
ATP
THEOPHYLLINE
M3
GTP
GC
cGMP
IPRA
TROPI
UM
M 3 A
GONI
STS
Adenosine
cAMPPDE

Bronchial Tone
Bronchoconstriction
Bronchodilitation
Bronchial Smooth Muscle
IgE-Antigen Complex
BasophilActivatio
n
Eosinophil
Activation
Chemical mediatorsHistamine, LTC4, LTD4, LTB4,Cytokines, Adenosine, PGD2, PAF,ECP and Neuropeptides
Cause inflammation, oedema, bronchospasm, muscus secretion, epithelial damage
CARTICOSTEROIDS
LT-ANTAGONISTLeukotrienes
SOD. CROMOGLYCATEStabilises Mast Cells
Mast CellDegranulation
INFECTION
NITRIC OXIDE
DONORS

Drugs Used in Bronchial Asthma
1. Selective β2– Agonists
Short acting Salbutamol, Terbutaline, Remiterol, Fenoterol, BitolterolLong-acting Salmeterol, Formoterol, Bambuterol
2. Non-Selective Sympathomimetics
Adrenaline, Ephedrine, Isoprenaline, Orciprenaline
(Metaproterenol), Isoetharine
BRONCHODILATORS

3. AnticholinergicsIpatropium, Tiotropium, Oxitropium
4. Methyl XanthinesTheophylline, Aminophylline, Diprophylline, Choline theophyllinate
Anti inflammatory Drugs (Controllers)Corticosteroids1. Oral : Prednisolone, Methylprednisolone2. Parenteral : Methyl prednisolone, Hydrocortisone3. Inhalational : Beclomethasome, Fluticasone, Triamcinolone, Budesonide, Flunisolide

Mast Cell StabilisersSodium Cromoglycate, Nedocromil, Ketotifen
Leukotriene Modulators:1. 5-Lipoxygenase Inhibitor : Zileuton2. LT – Receptor Antagonists : Zafirlukast, Montelukast, Iralukast, Pranlukast
Monoclonal Anti-IgE AntibodyOmalizumab
Miscellaneous: NO, Calcium channel blockers

Sympathomimetic agents ß2 receptors are present in the airway
smooth muscle. cause Bronchodilatation These are only provide relief M.O.A:
cAMP Bronchodilatation Release of broncho constricting mediators from mast cells Inhibit macrovascular leakage Mucociliary clearance

Epinephrine:
Rapid bronchodilator when SC/inhaled(320µg/puff) Onset of action 15min after inhalation Duration of action:60-90min.
ADR:- Acts on β1 receptor cause Tachycardia Arrhythmias Worsening angi So rarely prescribed.

Ephedrine: α,β1, β2
Ephedrine has a longer action
Oral activity
Lower potency
Pronounced central effects.

β2 Selective Short acting : Terbutaline, Salnutamol On inhalation they have rapid onset(1-5Min) Short duration of action preferred for acute attack Route: Inhalation 100-200µg/6hourly Other MDI, Oral, IM, IV
Terbutaline is the only one drug safely used during the pregnancy.

Long acting: Salmeterol, bambutarol
Long acting but slow onset of action Preferred for maintenance therapy Not useful in acute attack due to slow onset of
actionRoute: Inhalation 50µg twice daily.
Formoterol: Long acting Rapid onset Preferred for prophylaxis due to long actingRoute: Inhalation 12-24µg twice daily

ADR of Sympathomimetics By oral route stimulate β2 receptors in skeletal
muscle cause tremors, Orthostatic hypotension.
Tachycardia (High dos also stimulate β1 receptors in heart)
Restlessness
Tolarance occurs.

Antimuscurnic agent Less effective then β agonists
MOA: By blocking M3 receptors on air way smooth muscle and prevents Ach action.
-They acts by cGMP levels in bronchial smooth muscle.
Ipatropium:- -Poor absorption from bronchi into systemic
circulation -Do not cross BBB.-Also mucus secretion
Ipatropium + β2 (Salbutamol) work better in serve asthma and long duration of action

Methyl Xanthenes MOA:
i) Inhibition of PDE 3,4. These enzyme are responsible for metabolism of cAMP.
ii) Blockade of Adenosine receptors.
Actions: Theophyline exhibits bronchodilatory action Anti Inflammatory Immunomodulator Respiratory stimulation Diaphragmatic contractility Mucociliary clearance

Pharmaco Kinetics:
Oral/ParentalFood delay the rate of absorptionWell distributedCross placental & BBBMetabolized in LiverExcreted in urine

ADR: Low therapeutic window, CNS stimulant drugs Plasma levels 10-20µg/ml, Narrow safety
Restlessness, insomnia, headache, tremors
Nausea,VomitingPeptic ulcer
Tachycardia, palpitation, hypotension, arrythimiasTheophyline: potent vasodilator, reflex tachcardia, oral route Aminophyline: Slow IV infusion
XanthenesGIT Diuresis
Heart
CNS
20µg/ml40µg/ml
20µg/ml

Corticosteroids (Controllers) Glucocorticosteriods induce synthesis of lipocotrin
which inhibits pholipaseA2 there by preventing formation of mediators such as PGs,TAX2, LTand other mediators.
Actions: Anti allergic, anti inflammatory, immunosuppressant ( AG:AB reactions ), Mucosal oedema, bronchial hyperactivity, Enhance β adrenergic action by up regulation of β2 receptors in lung.

Inhalator glucocorticosteriods such as beclomethasone, budesonide and fluticasone are used as prophylactic agents in asthma.
PK: Well tolerated less systemic side effects.
Common side effects: Dryness of mouth Voice change Oropharangeal candidiats.Systemic are used in acute severe and chronic severe
asthma.

Mast cell stabilizers Non bronchodilating, Non steroid drugs, used for prophylactic
treat.MOA: Prevent degranulation and release of chemical mediators from
the mast cells. They stabilize the mast cells by preventing transmembarane
influx of Ca ions.PK: Highly ionized Least systemic absorption well tolerated.Uses: Allergic asthma, allergic conjunctivitis, allergic rhinitis,
allergic dermatitis.Ketotifen (Mast stab.+ Antihistamincs)

LT Modulators LT are powerful bronchoconstrictors. Action by preventing their synthesis or blocking
effect on cys LT receptors
Synthesis inhibitors (Lipooxygenase) Zafirlukast,Montelukast
PK: Well absorbed after oral administration Highly bound to plasma protein Metabolized by liver Effective for prophylactic treat of mild asthma.

ADR: Head ache skin rashes rarely eosinophilia Zileuton cause hepatic toxicity.

Monoclonal anti IgE antibody MOA:- AG:Ab complex formation by AB action Omalizumab: Recombinant humanized
monoclonal antibody. Inhibit the binding site of IgE to mast cells and
basophils PK: administered parentarally Uses: Moderate to severe asthma and allergic
disorders. Indicated for asthmatic patients who are not
adequately controlled by inhalational corticosteroids.
ADR: Inj site redness, itching, stinging.

Miscellaneous
NO: It dilate pulmonary blood vessels and relax airway smooth muscle.
Uses: For acute severe asthma and management of pulmonary hypertension.
Ca channel blockers: Broncho constriction ultimately involves
some degree of ca into cells Nefedpine / Verapamil should provide relief in asthma.

RX Status asthmatics (Acute severe asthma)
Status asthmatics a severe acute asthma, which is a life threatening condition involving exhaustion, cyanosis, bradicardia,hypotension, dehydration and metabolic acidosis.

Humidified O2 inhalation Neubulized β2 adrenergic agonist + anti
cholinergic agent Systemic glucocorticosteroids IV
(Hydrocortisone 200mgIV) IV fluids to correct dehydration. K supplements: To correct hypokalemia
produced by repeated administration of salbutamol.
NaHCo3 (Sodium bicarbonate) to treat acidosis.
Antibiotics to treat infection

DRUGS TO BE AVOIDED IN ASTHMA
β adrenergic blockers
Cholinergic agents
NSAIDS ( cause hyperapoenia) except paraceatamol.