2009 terni, università di medicina, i farmaci nel trattamento delle tachicardie ventricolari
-
Upload
centro-diagnostico-nardi -
Category
Health & Medicine
-
view
48 -
download
0
Transcript of 2009 terni, università di medicina, i farmaci nel trattamento delle tachicardie ventricolari
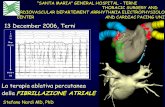
Drugs used to treat Ventricular
Tachyarrhythmias
Stefano Nardi MD, PhDStefano Nardi MD, PhDArrhythmia, EP Center and Cardiac Pacing Unit Arrhythmia, EP Center and Cardiac Pacing Unit
Thoracic Surgery and Cardiovascular Department Thoracic Surgery and Cardiovascular Department
S. Maria General Hospital, TerniS. Maria General Hospital, Terni
Definition: a variation in either the site or rate of cardiac impulse formation, and/or a variation in the sequence of cardiac impulse propagation.
Electrophysiology resting potential
• A transmembrane electrical gradient (potential) is maintained, with the interior of the cell negative with respect to outside the cell
• Caused by unequal distribution of ions inside vs. outside cell– Na+ higher outside than inside cell– Ca+ much higher “ “ “ “– K+ higher inside cell than outside
• Maintenance by ion selective channels, active pumps and exchangers
Cardiac Action Potential• Divided into five phases (0,1,2,3,4)
– Phase 4 - resting phase (resting membrane potential)• Phase cardiac cells remain in until stimulated• Associated with diastole portion of heart cycle
• Addition of current into cardiac muscle causes – Phase 0 – opening of fast Na channels and rapid
depolarization • Drives Na+ into cell (inward current), changing membrane
potential• Transient outward current due to movement of Cl- and K+
– Phase 1 – initial rapid repolarization• Closure of the fast Na+ channels• Phase 0 and 1 correspond to the R and S waves of the ECG
Cardiac Action Potential
• Phase 2 - plateau phase– sustained by the balance between the inward movement of
Ca+ and outward movement of K + – Has a long duration compared to other nerve and muscle
tissue– Normally blocks any premature stimulator signals (other
muscle tissue can accept additional stimulation and increase contractility in a summation effect)
– Corresponds to ST segment of the ECG.
• Phase 3 – repolarization – K+ channels remain open, – Allows K+ to build up outside the cell, causing the cell to
repolarize– K + channels finally close when membrane potential reaches
certain level– Corresponds to T wave on the ECG
Cell-Membrane Resting Potential
+
-
needle electrode
membrane
reference electrode outside of cell
Advance needle electrode across the cell membrane….
BIOPOTENTIALS
Cell-Membrane Resting Potential
+
-
0 mV
….a “resting” potential of -90 mV is observed inside the cell with respect to outside the cell
Advance needle electrode across the cell membrane….
Cell-Membrane Resting Potential
+
The resting potential is maintained by an ATP powered sodium-potassium “pump” within the membrane that transports Na+ ions outward and K+ ions inward (3 Na+ per 2 K+).
Na+
K+ Na+
Na+
The gradient of ion-concentration separates charge across the membrane with an equal and opposite electrical gradient of -90 mV.
-
K+
Advance needle electrode across the cell membrane….
-
--- -- ---
---
----
--- -
---
-
-- -
++++
++++
+++
+++++++
++++
++
Cell Membrane Action Potential (AP)
+
-
Stimulate the cell….
0 mV
….a transmembrane “AP” is observed with 5 characteristic
phases (Φ)
Cell Membrane Action Potential (AP)
+
-
Stimulate the cell….
Φ0 – Upstroke
Φ2 – Plateau (absolute
refractory)Φ3 – Recovery
(relative refractory)
Φ4 – Resting
Φ1 – Initial Recovery
0 mV
Cell Membrane Ion Channels
Voltage-gated, ion-selective channels open and close to generate the AP
Many types of channels are known, each selective to a specific species of Na+, K+, and Ca++ ions
Cell Membrane Ion Channels
Voltage-gated, ion-selective channels open and close to generate the AP
….with 4 “phases” of protein groups (I-IV)….
….including 1 “P-loop” polypeptide chain
….and 6 “sub-groups” within each phase….
All channels have a common structure that spans the membrane….
inside
outsidemembrane
Cell Membrane Ion Channels
Voltage-gated, ion-selective channels open and close to generate the AP
NH2
COOH
“unroll” channel....
Cell Membrane Ion Channels
Flattened view presents clearer view of the channel structure
NH2
COOH
membrane (phospholipid
bilayer)
amino-end
carboxy-end
IN OUT
IN OUT
Cell Membrane Ion Channels
NH2
COOH
….are repeated, forming each of the
4 phases (I-IV)
subgroups S1-S6….
Flattened view presents clearer view of the channel structure
IN OUT
IN OUT
Cell Membrane Ion Channels
NH2
COOH
“P-loops” form the narrowest part of
the channel responsible for gating ion-flow
Flattened view presents clearer view of the channel structure
IN OUT
IN OUT
Cell Membrane Ion Channels
Functional and structural evidence suggests that P-loops are central to….
NH2
COOH
• sensing voltage
• filtering ion species
• mechanical actuation
S6
S5
Cell Membrane Ion Channels
S6
S5
Functional and structural evidence suggests that P-loops are central to actuation
• P-loops extend (or twist) for channel activation
Cell Membrane Ion Channels
S6
S5
Functional and structural evidence suggests that P-loops are central to actuation
• P-loops retract (or twist) for channel inactivation
Na+
Cell Membrane Ion Channels
Transmembrane AP formation follows an organized sequence in response to stimulation:
Φ0 – Upstroke
1) Fast, inward Na+ channels open, rapidly depolarizing the membrane and triggering closure of the channels (Φ0 – upstroke and overshoot)
K+
Na+
Cell Membrane Ion Channels
Φ1 – Initial Recovery
Transmembrane AP formation follows an organized sequence in response to stimulation:
2) Slower, outward K+ channels sense the rising voltage and open, diminishing the overshoot (Φ1 – Initial Recovery)
Cell Membrane Ion Channels
Φ2 – Plateau (absolute refractory)
K+
Ca++
Transmembrane AP formation follows an organized sequence in response to stimulation:
3) Slower, inward Ca++ channels open, matching outward K+ and maintaining the membrane near 0 mV (Φ2 – Plateau)
Cell Membrane Ion Channels
Φ3 – Recovery (relative refractory)
K+
K+
Transmembrane AP formation follows an organized sequence in response to stimulation:
4) K+ conduction increases and Ca++ decreases, repolarizing the membrane (Φ3 – Recovery)
Ca+
+
Cell Membrane Ion Channels
Transmembrane AP formation follows an organized sequence in response to stimulation:
5) Na+– K+ pump helps converge and maintain resting potential near -90 mV (Φ4 – Resting)
Φ4 – Resting
Na+
K+ Na+
Na+
K+
Na +
Ca 2+
Ca 2+
K +
K +
4
0
12
3
4
K+
Na+
Na/K ATPase
The fast cardiac action potential
-90 mV
+55 mV
Na +
Refractory Period
Effect of local anesthetics on the fast cardiac action potential
Slope phase 0 = conduction velocity
Longer RP due to slower recovery from inactivation
Increased threshold
4
0
12
3
4
K +
K +
Refractory Period
Effect of drugs that block K channels
Increase action potential duration (APD)
4
0
2
3
4
Ca2+
Slope of phase 0 = Conduction velocity
Effect of Ca 2+ channel blockers
Refractory Period
• VAs are common in most people and are usually not a problem but…VA’s are most common cause of SCD
• Majority of SCD occurs in pts with neither a previously known HD nor history of VA’s
• AADs which decrease incidence of VA’s do not decrease (and may increase) the risk of SCD treatment may be worse then the disease!
Differences between non-PM and PM cell action potentials
• PCs - Slow, continuous depolarization during rest• Continuously moves potential towards threshold for a
new action potential (called a phase 4 depolarization)
Mechanisms of Cardiac Arrhythmias
• Result from disorders of impulse formation, conduction, or both
• Causes of arrhythmias– Cardiac ischemia– Excessive discharge or sensitivity to autonomic
transmitters– Exposure to toxic substances– Unknown etiology
Disorders of impulse formation
• No signal from the pacemaker site
• Development of an ectopic pacemaker– May arise from conduction cells (most are capable of
spontaneous activity)– Usually under control of SA node if it slows down too much
conduction cells could become dominant– Often a result of other injury (ischemia, hypoxia)
• Development of oscillatory afterdepolariztions– Can initiate spontaneous activity in nonpacemaker tissue– May be result of drugs (digitalis, norepinephrine) used to treat other
cardiopathologies
Disorders of impulse conduction• May result in
– Bradycardia (if have AV block)– Tachycardia (if reentrant circuit occurs)
Reentrant circuit
Antiarrhythmic drugs
• Biggest problem – AADs can cause arrhythmia!
– Example: Treatment of a non-life threatening tachycardia may cause fatal VTs
– Must be vigilant in determining dosing, blood levels, and in follow-up when prescribing AADs
Therapeutic overview
• Na+ channel blockade• β-adrenergic receptor blockade• Prolong repolarization• Ca2+ channel blockade
• Adenosine• Digitalis glycosides
Classification of AADs (based on mechanisms of action)
• Class I – blocker’s of fast Na+ channels – Subclass IA
• Cause moderate Phase 0 depression• Prolong repolarization• Increased duration of action potential• Includes
– Quinidine – 1st antiarrhythmic used, treat both atrial and ventricular arrhythmias, increases refractory period
– Procainamide - increases refractory period but side effects
– Disopyramide – extended duration of action, used only for treating ventricular arrthymias
Classification of AADs(based on mechanisms of action)
• Subclass IB– Weak Phase 0 depression– Shortened depolarization– Decreased action potential duration– Includes
• Lidocane (also acts as local anesthetic) – blocks Na+ channels mostly in ventricular cells, also good for digitalis-associated arrhythmias
• Mexiletine - oral lidocaine derivative, similar activity
• Phenytoin – anticonvulsant that also works as antiarrhythmic similar to lidocane
Classification of AADs(based on mechanisms of action)
– Subclass IC• Strong Phase 0 depression• No effect of depolarization• No effect on action potential duration
Includes– Flecainide (initially developed as a local
anesthetic)» Slows conduction in all parts of heart, » Also inhibits abnormal automaticity
– Propafenone» Also slows conduction» Weak β – blocker» Also some Ca2+ channel blockade
Classification of AADs(based on mechanisms of action)
• Class II – β–adrenergic blockers– Based on two major actions
1) blockade of myocardial β–adrenergic receptors2) Direct membrane-stabilizing effects related to Na+ channel
blockade
– Includes• Propranolol
– causes both myocardial β–adrenergic blockade and membrane-stabilizing effects
– Slows SA node and ectopic pacemaking– Can block arrhythmias induced by exercise or apprehension– Other β–adrenergic blockers have similar therapeutic effect
• Metoprolol• Nadolol• Atenolol• Acebutolol• Pindolol• Stalol• Timolol• Esmolol
Classification of AADs(based on mechanisms of action)
• Class III – K+ channel blockers – Developed because some patients negatively
sensitive to Na channel blockers (they died!)– Cause delay in repolarization and prolonged
refractory period– Includes
• Amiodarone – prolongs action potential by delaying K+ efflux but many other effects characteristic of other classes
• Ibutilide – slows inward movement of Na+ in addition to delaying K + influx.
• Bretylium – first developed to treat hypertension but found to also suppress ventricular fibrillation associated with myocardial infarction
• Dofetilide - prolongs action potential by delaying K+ efflux with no other effects