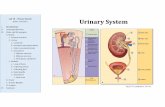
Urinary system. Urinary System Consist of: Kidneys Ureters Bladder Urethra.
Urinary System
description
Transcript of Urinary System

URINARY REVIEW

TUBULAR REABSORPTION

Tubular Reabsorption
• Occurs in the proximal convoluted tubule• Microvili of the epithelial cells account for
maximum reabsorption• It is the process by which nutrients are
absorbed after they’ve already been through the intestines

Transport Mechanisms
• Lipid-soluble substances – moving down a concentration gradient for that substance
• Sodium ions – active transport• Glucose – active transport through tubule walls• Water – osmosis through epithelium• Amino acids – active transport• Albumin – endocytosis• Lactic acid – active transport

WATER REABSORPTION

Water and Sodium
• Water is transported through osmosis, and so tends to follow sodium ions into the proximal convoluted tubule until osmotic equilibrium is reached
• Sodium transports water, because water diffuses passively but it carries the diffusion with its own active transport
• They are closely associated because if one increases or decreases, so does the other

ADH (Antidiuretic Hormone)
• ADH controls water absorption in the collecting duct and the distal convoluted tubule of the kidney
• It does this by stimulating the cells to insert “water channels” into the membrane, making the epithelium more permeable for water to diffuse through the cells

TUBULAR SECRETION

Tubular Secretion
• Process by which some substances move from the peritubular capillary into the renal tubule
• H+ Ions – actively secreted throughout the entire renal tubule– It regulates the pH balance, or acidity, of urine
• K+ Ions – passively transported through tubular epithelium into tubular fluid, then actively secreted

COUNTERCURRENT MECHANISM

Permeability of Limbs of the Nephron
• Ascending Limb:– Fairly permeable to water– Actively reabsorbs sodium and chloride ions– More hypotonic (less concentrated solutions in
osmosis)• Descending Limb:– Very permeable to water– Somewhat permeable to solutes– More hypertonic (more concentrated solutions in
osmosis)

Countercurrent
• Mechanism – the process by which the kidneys concentrate the urine
• Multiplier – the property where the urine becomes more concentrated each time a circuit is complete through the mechanism and filtration process

ADH – ANTIDIURETIC HORMONE

Antidiuretic Hormone
• ADH is produced in the pituitary gland• ADH prevents dehydration by stimulating the
collecting ducts and the distal convoluted tubule to be more permeable to water, increases osmosis and allowing more water back into the body
• When this happens, the sodium concentration in the medullary interstitial fluid increases as water leaves but sodium does not

Drinking Too Much Water
• On an incidental basis, drinking too much water simply dilutes the concentration of urine – too much causes water to seep out of the circulatory system and into the neighboring cells (causing headaches when this happens in the brain)
• On a regular basis, it can damage the glomeruli as they overwork to process the excess water in the circulatory system

RENIN-ANGIOTENSIN SYSTEM

Renin-Angiotensin
• Renin is an enzyme secreted by the juxtaglomerular cells of the afferent arteriole
• Renin – breaks down angiotensinogen– becomes Angiotensinogen I– converted into Angiotensinogen II– stimulates aldosterone formation, which reduces
the amount of sodium excreted in urine• Macula Densa cells are sensitive to the sodium
concentration in the distal convoluted tubule

URINARY SYSTEMTEXTBOOK NOTES
AND KIDNEYS

KIDNEYS

Kidneys
• Bean-shaped organs in the lower-middle back on either side of the spinal column, help in place by adipose and connective tissue
• Where urine is formed• Functions:– Remove metabolic wastes– Regulate blood pressure, red blood cell
production, and calcium ion absorption– Regulate volume, composition, and pH of blood

Nephrons
• Functional unit of the kidney– renal corpuscle• Glomerulus• Glomerular capsule
– renal tubule• proximal convoluted tubule• Nephron loop (ascending and descending limbs)• Distal convoluted tubule
• Joins a collecting duct

URINE FORMATION

Glomerular Filtration
• Urine formation begins when water and dissolved materials are filtered out of the glomerular capillary
• Secretes renin to stimulate formation of aldosterone to hold onto sodium when the concentration of sodium decreases

Filtration Rate and Pressure
• Pressure – powered by hydrostic pressure in the glomerular capillaries– Also affected by osmotic pressure– Blood vessels will constrict or relax when
necessary to keep up same pressure
• Rate – varies with pressure– Osmotic pressure increases, rate decreases– And vice-versa

Tubular Reabsorption
• Substances selectively reabsorbed from the glomerular filtrate
• Mostly happens in the proximal convoluted tubule, with help from microvili
• Different materials reabsorbed in different ways– Active transport – glucose, amino acids, sodium ions– Endocytosis – proteins– Osmosis – water (passively follows sodium)
• Excess substances released in urine

Tubular Secretion
• Transports some substances from plasma to tubular fluid– Substances are actively secreted– This includes various hydrogen ions
• Potassium secreted both actively and passively in distal convoluted tubule and collective duct

Urine Regulation(Concentration and Volume)
• Most of sodium is reabsorbed before urine is excreted, as they are concentrated in a renal medulla by the countercurrent mechanism– Water being reabsorbed helps it along, though it
increases the concentration of sodium in the tubular fluid
• Distal convoluted tubule and collecting duct impermeable to water, so any water left is excreted through urine– Unless ADH gets there, making them permeable to
water, promoting water absorption and controlling sodium concentration

Urea and Uric Acid Excretion
• Urea – byproduct of amino acid production– 50% is excreted through urine– Countercurrent mechanism involving urea helps
water absorption
• Uric Acid – result of metabolism of nucleic acids– Most reabsorbed by active transport• Some secreted into renal tubule

Urine
• Composition – 95% water, and contains:– Urea and uric acid– Creatinine– Trace amino acids– Varying electrolytes
• Renal Clearance – rate at which a chemical is removed from the plasma

NEPHRON COMPONENT FUNCTIONS
(Kind of a summary of Urine Formation)

Renal Corpuscle
• Glomerulus – filters water and substances from plasma
• Glomerular capsule – receives what’s filtered

Renal Tubule
• Proximal Convoluted Tubule – reabsorbs nutrients and substances
• Descending Limb of Nephron Loop – reabsorption of water by osmosis
• Ascending Limb of Nephron Loop – reabsorption of sodium, potassium, and chloride ions by active transport
• Distal Convoluted Tubule – reabsorption of sodium and water, secretion of hydrogen and potassium

Collecting Duct – reabsorbs water
Unrelated, but more on the Proximal Convoluted Tubule Reabsorption:
• Active transport: glucose; amino acids, creatine; lactic, citric, uric, and ascorbic acids; phosphate, sulfate, calcium, potassium, and sodium ions
• Endocytosis – proteins• Osmosis – water• Electrochemical Attraction – chloride and other
negatively charged ions

ELIMINATION OF URINE
(the Process of Peeing)

Ureters
• Tubes that extend from kidneys to bladder
• Wall as mucous, muscular, and fibrous layers
• Moves urine down through peristalsis

Urinary Bladder and Urethra
• Urinary Bladder– Organ that stores urine and forces it into urethra– Internal urethral sphincter formed by detrusor
muscle
• Urethra– Tube through which urine exits the body

Mincturition
• Process of expelling urine• Detrusor muscles contract, sphincter relaxes• Mincturition Reflex:– The more urine in the bladder, the more the stretch
receptors in it’s walls get stimulated, which send signals to the brain for you to do the pee-pee dance
– Eventually, the signals override the voluntary muscular clenching reflex, resulting in urine being forcibly expelled (and causing traumatizing memories of preschool in the process )