Salivary glands anatomy applied aspects 140608050047-phpapp01
-
Upload
abhishek-pt -
Category
Health & Medicine
-
view
69 -
download
1
Transcript of Salivary glands anatomy applied aspects 140608050047-phpapp01

SALIVARY GLANDS ANATOMYDR.ABHISHEK PT
Department of Oral & Maxillofacial Surgery


INTRODUCTIONThe salivary glands are exocrine glands, glands with ducts, that produce saliva and pour their secretion in the oral cavity
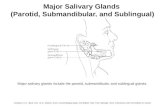
Major (Paired) Parotid Submandibular Sublingual
MinorThose in the Tongue, Palatine Tonsil, Palate, Lips and Cheeks

DEVELOPMENT


PAROTID GLAND
Largest Average Wt - 25gmIrregular lobulated mass lying mainly below the external acoustic meatus between mandible and sternomastoid.On the surface of the masseter, small detached part lies b/w zygomatic arch and parotid duct-accessory parotid gland or ‘socia parotidis’


External Features
• Resembles an inverted 3 sided pyramid
• Four surfaces• Superior(Base of the
Pyramid)• Superficial• Anteromedial• Posteromedial

Relations
• Superior Surface • Concave• Related to
• Cartilaginous part of ext acoustic meatus
• Post. Aspect of temperomandibular joint
• Auriculotemporal Nerve• Sup. Temporal vessels

•Separated by three borders
• Anterior• Posterior• Medial

• Apex• Overlaps posterior belly of
digastric and adjoining part of carotid triangle
• Superficial Surface• Covered by
• Skin• Superficial fascia containing
facial branches of great auricular N
• Superficial parotid lymph nodes and post fibers of platysma

• Anteromedial Surface• Grooved by posterior border of ramus of mandible
• Related to• Masseter• Lateral Surface of
temperomandibular joint• Medial pterygoid muscles• Emerging branches of Facial
N

• Posteromedial Surface
• Related • to mastoid process with
sternomastoid and posterior belly of digastric.
• Styloid process with structures attached to it.
• External Carotid A. which enters the gland through the surface
• Internal Carotid A. which lies deep to styloid process


BORDERS

• Anterior border
• Separates superficial surface from anteromedial surface.
• Structures which emerge at this border
• Parotid Duct• Terminal Branches of
facial nerve• Transverse facial
vessels

• Posterior Border
• Separates superficial surface from posteromedial surface
• Overlaps sternomastoid

• Medial Border
• Separates anteromedial surface from posteromedial surface
• Related to lateral wall of pharynx

Structures within the parotid gland

ARTERIES

VEINS

NERVES


• Facial Nerve trunk lies approximately 1 cm inferior and 1 cm medial to tragal cartilage pointer of external acoustic meatus.

Parotid Duct• ductus parotideus;
Stensen’s duct
• 5 cm in length
• Appears in the anterior border of the gland
• Runs anteriorly and downwards on the masseter b/w the upper and lower buccal branches of facial N.

• At the anterior border of masseter it pierces
• Buccal pad of fat• Buccopharyngeal fascia• Buccinator Muscle
• It opens into the vestibule of mouth opposite to the 2nd upper molar


Surface Anatomy of Parotid Duct
Tragus ofthe ear
Midway between the ala of the nose and the
angle of the mouth
Middle ⅓ of the horizontal line

Surface anatomy of Parotid Duct
• Corresponds to middle third of a line drawn from lower border of tragus to a point midway b/w nasal ala and upperlabial margin

SURFACE MARKINGA)UPPER BORDER OF HEAD OF MANDIBLE
B)JUST ABOVE CENTRE OF MASSETER MUSCLE
C)POSTEROINFERIOR TO THE ANGLE OF MAANDIBLE
D)UPPER PART OF ANGLE OF MANDIBLE

Head ofMandible
Middle ofMasseter m.
2 cm belowAngle of
Mandible
MastoidProcess

NERVE SUPPLY

•Parasymapthetic N• Secretomotor via
auriculotemporal N
•Symapathetic N• Vasomotor• Delivered from plexus
around the external carotid artery
•Sensory N• Reach through the Great
auricular and auriculotemporal N

Applied aspects
• Parotid swellings are very painful due to the unyeilding nature of the parotid fascia.
• Mumps is infection of salivary gland caused by paromyxovirus which will cause severe pain

Incision
• Lazy ‘S’ incision• Pre-auricular—mastoid-cervical incision• Blairs incision and modified blairs• Facelift incision



technique
• A modified Blair incision
• An alternative incision is a
modified face-lift incision.• A modified Blair incision is planned in a preauricular crease coursing around the ear lobule and then into an upper neck crease
Methylene blue can be used to mark points along the proposed incision, which facilitates proper wound alignment and closure.

Clin Otolaryngol. 2006 Dec;31(6):531-4.
An anatomical comparison of Blair and facelift incisions for parotid surgery.Nouraei SA1, Al-Yaghchi C, Ahmed J, Kirkpatrick N, Mansuri S, Singh A, Grant WE.Author informationAbstractBACKGROUND:The rhytidectomy approach for parotidectomy allows the incision to be hidden, and post-operative scarring minimised. Furthermore, separate elevation of the Superficial Musculo-Aponeurotic System (SMAS) reduces the incidence of Frey's syndrome, and provides vascularized soft tissue for contour reconstruction. The technique has gained popularity particularly with plastic surgeons, but concerns persist that with this approach, particularly with lesions located anteriorly, access to the gland may be inadequate, and facial nerve identification may be compromised.MATERIALS AND METHODS:We undertook an anatomical study to quantitatively compare the surgical access achieved using the facelift approach with the conventional Blair incision, by comparing the distances between the parotid edge and the retracted flaps.RESULTS:Despite reduced tissue elasticity due to formaldehyde fixation, it proved possible to demonstrate all regions of the parotid gland to the operating surgeon with either approach. There were no significant differences in the distance between the parotid edge and the retracted skin flaps (P > 0.1; paired t-test).CONCLUSIONS:The facelift approach provides at least equal access to all regions of the parotid gland when compared to a Blair's incision. It is a superior approach aesthetically and its more widespread use in parotid surgery is advocated.

Otolaryngol Head Neck Surg. 2013 Apr;148(4):548-56. doi: 10.1177/0194599812475221. Epub 2013 Feb 4.
Facelift approach for parotidectomy: an evolving aesthetic technique.Grover N1, D'Souza A.Author informationAbstractOBJECTIVE:To systematically review the literature on the modified facelift incision for parotidectomy and to identify the scope and safety of this approach, along with cosmetic outcomes. Where available, a direct comparison was made with Blair's incision (BI).DATA SOURCES:Medline, PubMed, Cochrane, and CINHAL databases for English-language studies published between 1960 and 2011 on the facelift approach for parotidectomy.REVIEW METHODS:Exclusion criteria were studies reporting on concurrent facelift, studies that used synthetic material for reconstruction of the surgical bed, descriptive studies, and studies with duplicate patient data. Outcome measures were candidacy for surgery, variations in incision, cosmetic outcomes, surgical time, complication rates, and limitations.

RESULTS:Of the initial 139 studies, 11 studies encompassing 628 patients were included. Male-to-female ratio was 0.49:1, and average age was 47.1 years. In total, 582 surgeries were performed for benign lesions. Only 10 studies specified the extent of surgery: 8 authors used it for performing superficial/partial parotidectomy, and 2 described 17 cases of total parotidectomy. Tumors up to 8 cm have been excised, with a median value of 4 cm. Operative time, formally analyzed in 3 studies, was not significantly different when compared with BI. Complication rates were not increased with this approach. Aesthetic outcomes pertaining to postoperative scar were good, as reported by the patients.
CONCLUSION:The facelift approach is a cosmetically superior approach to parotid tumors as proven by objective data. Most publications in the literature pertaining to the modified facelift incision for parotidectomy have been in the past decade, lending credence to its rising popularity

Cervicomastoidfacial versus modified facelift incision for parotid surgery: a patient feedback comparisonAnn R Coll Surg Engl. 2010 Jan; 92(1): 40–43.Joseph Wasson, Haider Karim, Justin Yeo, and Jaan PanesarAuthor information ► Copyright and License information ►See letter "Facial surgical incisions – role of maxillofacial surgeons" in volume 92 on page 267.Go to:AbstractINTRODUCTIONTraditionally, the cervicomastoidfacial (CMF) incision is used to excise benign tumours of the parotid gland. The rhytidectomy or modified facelift (MF) incision allows an alternative approach which leaves no visible neck scar. The objective of this study was to establish the frequency of each surgical approach used and identify any difference in complication and patient satisfaction between the two incisions for benign conditions of the parotid gland.


• PATIENTS AND METHODS• A retrospective analysis of 101 case notes for patients who underwent parotidectomy by both ENT and maxillofacial departments between January 2006 and February 2008 was undertaken. All histologically confirmed cases of malignancy were excluded. For each incision, immediate postoperative complications were obtained from the notes. A postal patient outcome evaluation questionnaire sought information regarding persistent and late complications as well as a visual analogue scar satisfaction score for both incisions.
• RESULTS• Overall, 79 parotidectomies were included (59 CMF incisions, 20 MF incisions). Of CMF incisions, 34% suffered facial weakness immediately postoperatively versus 20% of MF incisions. Of CMF incisions, 4% suffered postoperative haematomas versus none following MF incisions. In the study cohort, 47 (60%) responded to the postal feedback questionnaire (33 CMF versus 14 MF respondents). Information regarding immediate and late postoperative ipsilateral facial paraesthe-sia and gustatory sweating was obtained. Mean visual analogue scar satisfaction scores were 9.4 for CMF incisions and 8.9 for MF incisions.
• CONCLUSIONS• Immediate and late complications for CMF and MF approaches for benign disease parotidectomy were comparable, but scar satisfaction following MF incision was not greater than CMF incisions.

• During surgical removal of parotid gland for any tumour the facial nerve is preserved by removing the glands in two parts superficial and deep lobe separately.



1-1.5 cm deep and inferior to the pointer6-8 mm deep to the suture linejust superior and posterior to the cephalic margin



• When necessary, the
facial nerve can be
identified in the
mastoid bone by
mastoidectomy and
followed peripherally.

Facial Nerve injury

TEMPORARY PARALYSIS
TEMPRORARYDUE TO TRACTION
RECOVERS IN 6-8 WEEKSN0 ACTIVE TREATMENT IS REQUIRED


• A parotid abscess may be caused by the spread of infection from the oral cavity.
• An infection may also spread due to the parotid lymph node draining an infected area

• Parotid abscess is best drained by horizontal incision according to Hiltons method of incision and drainage.
Vertical incision on skin but transverse incision on the parotid fascia to safeguard facial nerve
and branches

• Frey's syndrome

Also called as auriculotemporal nerve syndrome or gustatory sweating
It is condition wherein sweating in the area of distribution of ATN occurs,which is caused by a stimulus to secretion of saliva.
It is thought to be the result damage to ATN post ganglionic parasympathetic fibres from otic ganglion become united to sympathetic fibres arising from superior cervical ganglion going to SUPPLY SWEAT GLAND

• The iodine test
administered by applying
an alcohol–iodine–oil
solution (3 g iodine, 20 mL
castor oil, and 200 mL
absolute alcohol) described
by Laage-Hellman
• The solution was applied on the lateral
portion of the face that had been surgically
treated and the upper region of the neck.

• The solution was allowed to
dry and was covered lightly
with starch powder.
• The patients received lemon
candy for a gustatory stimuli
for 10 minutes.
• Discoloration of the starch
iodine mixture was
interpreted as a positive
finding for Frey’s syndrome

• There is no effective treatment, but various options
are described:
i. Injection of Botulinum Toxin
ii. Surgical transection of the nerve fibers
iii. Application of an ointment containing
an anticholinergic drug such as scopolamine

• The lobule of the ear is often pushed up in parotid swelling
• For tumours of the parotid gland incision biopsy is not indicated as it will cause the seeding of the tumour

Inflamatory diseases of parotid
Acute suppurative parotitis
Acute parotitis (mumps parotitis)
Recurrent subacute parotitis / chronic parotitis

REFERENCES
• Oral anatomy- by Sicher and DuBruls• Gray’s anatomy• Oral and maxillofacial surgery-by Nilima Malik• Oral and maxillofacial surgery- Kruger• Ann R Coll Surg Engl 1994; 76: 108-109• Anatomy –BD Churasia



submandibular salivary gland

Submandibular Glands are….• Irregular in shape
• Large superficial and small deeper part continous with each other around the post. Border of mylohyoid


Superficial Part• Situated in the digastric triangle
• Wedged b/w body of mandible and mylohyoid
• 3 surfaces• Inferior, Medial, Lateral

Capsule
• Derived from deep cervical fascia
• Superficial Layer is attached to base of mandible
• Deep layer attached to mylohyoid line of mandible

Relations
• Inferior- covered by • Skin• Superficial fascia containing
platysma and cervical branches of facial N
• Deep Fascia• Facial Vein• Submandibular Nodes

0

• Lateral surface• Related to submandibluar
fossa on the mandible• Madibular attachment of
Medial pterygoid• Facial Artery

• Medial surface
• Anterior part is related to myelohyoid muscle, nerve and vessels
• Middle part - Hyoglossus, styloglossus, lingual nerve, submandibular ganglion, hypoglossal nerve and deep lingual vein.
• Posterior Part - Styloglossus, stylohyoid ligament,9th nerve and wall of pharynx

• Deep part• Small in size
• Lies deep to mylohyoid and superficial to hyoglossus and styloglossus
• Posteriorly continuous with superficial part around the posterior border of mylohyoid

Submandibular Duct• Whartons duct• 5 cm long• Emerges at the anterior end of deep
part of the gland• Runs forwards on hyoglossus b/w
lingual and hypoglossal N• At the ant. Border of hyoglossus it is
crossed by lingual nerve• Opens in the floor of mouth at the side
of frenulum of tongue


Blood supply and lymphatics

• Arteries• Branches of facial and lingual arteries
• Veins• Drains to the corresponding veins
• Lymphatics• Deep Cervical Nodes via submandibular
nodes

Nerve supply• Parasymapthetic fibers from chorda
tympani
• Sensory fibers from lingual branch of mandibular nerve
• Sympathetic fibers from plexus on facial A


Applied aspects
• The formation of calculus is more common in the submandibular gland than in the parotid.
• For excision of the submandibular salivary gland( for calculus or tumour), a skin crease incision is as a rule, given more than 1inch( 2.5cm) below the angle of the jaw
• A stone in the submandibular duct(wharton’s duct) can be palpated bimanually in the floor of the mouth and can even be seen if sufficiently large.

Tumors of submandibular glands• Tumors in this gland are uncommon• Enlargement is more due to calculus • Of all tumors, mixed tumor is most common• Swelling is hard but not stony hard and should be differentiated from submandibular lymph node



Submandibular gland excision• Indications :
• Chronic sialoadenitis• Stone in submandbular gland• Submandibular gland tumors

Incision
• Placed 2-4 cm below the mandible, parallel to it• Preserve :
• Marginal mandibular nerve• Lingual nerve• Hypoglossal nerve


Complications
• Hemorrhage• Infection• Injury to mandibular nerve, lingual nerve , hypoglossal nerve

APPROACH TO SUBMANDIBULAR GLAND:-
• INTRAORAL APPROACH
• EXTRAORAL APPROACH
• TRANSORAL APPROACH

EXTRAORAL APPROACH:-
- under la- supine position with moderate neck extention and chin rotated away.
- incision given-3cm below lower border of mandible to avoid damage to facial nerve
- 7cm long incision approx.- incision made directly down the platysma until gland reached using no.15 blade
- underlying investing layer of deep cervical fascia is divided.



- superior lobe of gland is mobilized and retracted to reveal post.belly of digastric.
- then posterosuperior part of gland is dissected
- facial vessels taken care of.
- facial vein ligated
- facial artery double ligated if needed
- then dissection of superior part of gland is done.



- then dissection of deep part of gland is done with downward retraction of gland
- then v-shaped lingual nerve is identified that is connected to submandibular gland
- this connection is cut off.
- then gland connected to duct anteriorly,duct has to be clamped,divided and tied as far as possible
- incision closed with interruped or subcuticular sutures


INTRAORAL APPROACH:-
• This procedure is anatomically safe and can be performed with minimal morbidity
• Infiltration with Xylocaine plus epinephrine with an adequate waiting period for hemostasis; The intraoral approach (IOA) consisted of an incision on the floor of mouth from the caruncle of Wharton's duct to the retromolar trigone
• careful identification of the submandibular duct/lingual nerve relationship; • Anterior retraction of the mylohyoid muscle to expose the superficial lobe; • superiorly directed, extraoral, manipulation of the submandibular gland; • close and blunt dissection to the gland laterally to avoid injury to the facial artery and vein.
(PMID: 10839409 [PubMed - indexed for MEDLINE]Division of Plastic and Reconstructive Surgery at the University of California, Los Angeles 90095-1665, USA.)

TRANSORAL APPROACH:-• The neck is prepared and marked in the standard fashion for transcervical submandibular gland excision.
• A Dingman mouth gag is placed in an inverted fashion into the oral cavity.
• The tongue is then retracted to the contralateral side of operation, and bimanual palpation of the floor of mouth identifies the position and size of the gland.
• This maneuver allows for delivery of the superior portion of the gland.
• After infiltration of lidocaine with epinephrine, the incision is created from the retromolar trigone to within 1 cm of the lingual surface of the alveolar ridge, at the caruncle of Wharton's duct.

• Dissection along Wharton's duct from the caruncle of the duct to the gland identifies the lingual nerve, located on the superior-posterior-lateral surface of the gland, which is carefully dissected away.
• Wharton's duct is circumferentially dissected, from the caruncle to the gland, so that it may be elevated and excised en bloc with the gland.
• The gland is then dissected off of the muscles of the tongue and floor of mouth. Posteriorly and laterally, dissection identifies the facial artery and vein branches involved in the gland, which are clipped and divided.
• After dissection of the anterior and lateral portions of the gland, the hypoglossal nerve should be identified inferior and lateral to the gland.
• The submandibular ganglion is identified and divided from the lingual nerve.
• The wound is then irrigated, inspected for hemostasis and closed with interrupted sutures.


Sublingual Salivary Glands

• smallest of the three glands
• weighs nearly 3-4 gm
• Lies beneath the oral mucosa in contact with the sublingual fossa on lingual aspect of mandible.

Relations
• Above• Mucosa of oral floor, raised as
sublingual fold
• Below • Myelohyoid Infront• Anterior end of its fellow
• Behind• Deep part of Submandibular gland

• Lateral• Mandible above the anterior part of mylohyoid line
• Medial• Genioglossus and separated from it by lingual nerve and submandibular duct

Duct
• Ducts of Rivinus• 8-20 ducts• Most of them open directly into
the floor of mouth• Few of them join the
submandibular duct

• Blood supply• Arterial from sublingual and
submental arteries• Venous drainage corresponds to
the arteries
• Nerve Supply• Similar to that of submandibular
glands( via lingual nerve , chorda tympani and sympathetic fibers)

Sublingual and minor salivary gland diseases
• Mucous cyst (retention cyst) : Ranula, sailoliths • Inflammatory salivary gland diseases • Tumors as described before but it rarely effects sublingual glands

Applied aspects
• The structures at risk during dissection of the gland are the submandibular duct and the lingual nerve.
• The duct lies superficially in the floor of the mouth medial to the sublingual fold, and is crossed inferiorly by the nerve which then enters the tongue
• The sublingual artery and vein also lie on the medial aspect of the gland close to the submandibular duct and lingual nerve.

Incision
Ann R Coll Surg Engl 1994; 76: 108-109

APPROACH TO SUBLINGUAL GLAND:-
• INTRAORAL APPROACH:-
- linear incision is made parellel and lateral to submandibular duct
- incision shouldn’t extend more posteriorly to 1st molar tooth to avoid damage to lingual nerve

- the submandibular duct is carefully identified and retracted medially
- stay sutures-passeing through margins of mucosa to aid in retention

-using blunt dissection(scissors) lingual nerve is identified-the sublingual gland lying adjacent to inner cortex of mandible is mobilized and its multiple ducts are divided carefully to avoid damage to it.

The anterolateral part of sublingual gland may be attached to periosteum of mandible by fibrous tissue which must be divided carefully.followed by removal of gland as and when necessary

REFERENCES
• Oral anatomy- by Sicher and DuBruls• Gray’s anatomy• Oral and maxillofacial surgery-by Neelima Malik• Oral and maxillofacial surgery- Kruger• Ann R Coll Surg Engl 1994; 76: 108-109• Anatomy –BD Churasia