Salivary Glands for BDS
Transcript of Salivary Glands for BDS
-
8/11/2019 Salivary Glands for BDS
1/47
Salivary GlandsDr. Y. Snigdha
-
8/11/2019 Salivary Glands for BDS
2/47
Anatomy
-
8/11/2019 Salivary Glands for BDS
3/47
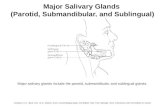
Salivary glands are divided into two groups as major
(90%) and minor glands (10%). There are three pairs of major salivary glands:
- Parotid (serous)
- Submandibular (mixed)
- Sublingual (mucous) 450 Minor glands (mucous) distributed in the lips,
cheeks, palate, floor of mouth, oropharynx, larynx,trachea and paranasal sinuses.
Total saliva secreted is 1500ml/day. It lubricates the
oral cavity and keeps it moist.
-
8/11/2019 Salivary Glands for BDS
4/47
Parotid Gland
Largest salivary gland. It is a serous type of gland.
Situated in the retromandibular fossa anterior and inferior
to acoustic meatus. It is enclosed by a capsule formed from deep cervical
fascia Parotid fascia.
It has a superficial part over the posterior part of ramusof mandible and deep part behind the mandible and medial
pterygoid muscle. Prolongates above the parotid duct (stensonsduct) to form
the accessory parotid.
The parotid duct opens into the oral mucosa opposite to thecrown of upper second molar tooth.
-
8/11/2019 Salivary Glands for BDS
5/47
There are three nerves in relationship to Parotid gland:
- Facial nerve along with retromandibular vein makes aplane named faciovenous plane of Patey in the substanceof parotid gland.
- Greater auricular nerve enters tail of parotid gland andit is sensory to tragus area and ear lobe.
- Auriculotemporal nerve is branch of mandibular divisionof 5th cranial nerve. It contains parasympathetic fiberssent to parotid by otic ganglion.
-
8/11/2019 Salivary Glands for BDS
6/47
FacialNerve
Facial nerve emerges through stylomastoid foramen.
The nerve enters the substance of parotid gland anddivides into two main branchesupper temporofacial andlower cervicofacial divisions.
The upper division further divides into zygomatic(orbicularis oculi), temporal (frontalis) and buccal
(orbicularis oris and buccinator) branches while thelower division divides into mandibular (lower lip muscles)and cervical (platysma) branches.
-
8/11/2019 Salivary Glands for BDS
7/47
-
8/11/2019 Salivary Glands for BDS
8/47
SubmandibularGland
Located deep in the digastric
triangle Has superficial and deep parts
Superficial part is located inthe submandibular space withinthe digastric triangle overlyingmylohyoid and hyoglossusmuscles.
Deep part is deep to mylohyoidmuscle.
The two parts join round theposterior free edge ofmylohyoid muscle
-
8/11/2019 Salivary Glands for BDS
9/47
Nerves related to submandibular gland are:
- Mandibular nerve- Sublingual nerve
- Hypoglossal nerve
The facial artery enters the posterior aspect of
the deep surface of the gland and grooves it. The Whartons duct runs from the deep lobe
and opens on the floor of the mouth lateral tothe frenulum of the tongue.
-
8/11/2019 Salivary Glands for BDS
10/47
Diseases of Salivary glands
-
8/11/2019 Salivary Glands for BDS
11/47
Mucous retention cyst
Develops from anobstructed minor salivarygland.
Painless, translucentswelling in oral mucosamostly in the lower lip orcheek.
Larger cysts need surgicalintervention. Smaller onesresolve spontaneously.
-
8/11/2019 Salivary Glands for BDS
12/47
Ranula Mucous extravasation cyst originating in sublingual salivary
gland.
Translucent cystic swelling with a bluish tinge situated onfloor of mouth on one side of fraenum linguae -characteristically described as frogs belly appearance.
Plunging ranula when the extravasation involves bothesubmandibular and sublingual gland, it extends into theneck and becomes bimanually palpable.
Similar to sublingual dermoid. Though dermoid containssebaceous content and is non transilluminant.
Treatment is excision of the cyst along with the involvedgland/glands. Simple excision leads to recurrence.Approach is usually trans oral unless its a plunging ranula
where the approach is cervical.
-
8/11/2019 Salivary Glands for BDS
13/47
-
8/11/2019 Salivary Glands for BDS
14/47
Sialography
Sialography is the radiographic examination ofthe salivary glands.
It usually involves the injection of a small amountof contrast dye (lipiodol or sodium diatrizoate) into thesalivary duct of a single gland, followed by routine X-ray projections
Indications:
- Salivary fistulas
- Sialectasis (abnormal dilation of the ducts)
- Congenital conditions
- Extra glandular masses
- Parotid duct stones
-
8/11/2019 Salivary Glands for BDS
15/47
Salivary Calculus
Submandibular Gland:
- 80% common
- 80% radiopaque
- Seen in xray
- Sialogram isnt needed.
Parotid gland
- 20% incidence
- Radioluscent
- Not seen in plain xray
- Identified by sialogram
Calculi are more common in submandibular gland because:- Viscous nature and mucin content- Calcium content- Non dependant drainage- Stasis- Hooking of the submandibular duct by the nerve.
-
8/11/2019 Salivary Glands for BDS
16/47
Sialadenitis Causes:
- Bacterial Most common, dueto obstruction and stasis
- Trauma over duct causingoedema and stasis
- Viral Mumps
Symptoms:
- Partial obstruction: Mildly
painful submandibular swelling.- Complete obstruction: painful
swelling appears during mealsand disappears after 1-2hours. Duct opening mayexude pus.
Types:
- Acute: Bacterial due to
obstruction/stasis. Canlead to abcess. Viral Mumps
- Chronic: Common afterpartial obstruction ofsubmandibular gland ductor hilum proximal to thelevel of crossing of thelingual nerve over theduct.
-
8/11/2019 Salivary Glands for BDS
17/47
Differential diagnosis
Submandibular Sialadenitis
Submandibular tumour
Submandibular lymphadenopathy
Plunging ranulaCystic hygroma
-
8/11/2019 Salivary Glands for BDS
18/47
Treatment
The stone lying in the duct can be removed by incising the duct over stonein floor of mouth. After stone removal, the opening in the duct should be
left unsutured for free drainage of saliva. If stone is palpable in proximal duct, it should not be removed through
intraoral route since there is risk of damage to lingual nerve that hooks theduct in this region. In such cases or in cases having stone in the gland,treatment is submandibular gland excision.
Complications
- Bleeding and hematoma formation.
- Infection.
- Injury to marginal mandibular nerve (drooping of angle of mouth).
- Injury to lingual nerve (anaesthesia of anterior 2/3rd of tongue).
- Injury to hypoglossal nerve (unilateral tongue paralysis).
-
8/11/2019 Salivary Glands for BDS
19/47
Acute parotitis
Acute painful swelling of parotid glanddue to inflammation.
Causes:
- Viral: Mumps most common inchildren of 4-6 years. Symptoms arefever with malaise and headachefollowed by painful swelling of one orboth parotids. Treatment is fluids andantibiotics.
- Obstructive causes :
- 1) Papillary obstruction due totrauma due to ill fitting denture.Presents with painful swelling duringmeal times. Teatment is papillotomyallowing free drainage of saliva.
- 2) Parotid calculi
-
8/11/2019 Salivary Glands for BDS
20/47
Granulomatous Sialadenitis
Tuberculosis: The organism usually gains access to thesalivary glands by a lesion in oral cavity, teeth or tonsiland presents as a painless mass in the gland. FNAC isthe investigation of choice and ATT helps in curing theailment.
Actinomycosis: Extension into the salivary glands occursfrom adjacent sites causing firm, indurated mass. Itleads to fistula formation producing yellow sulphurgranules. Treatment is with extended course ofpenicillin.
-
8/11/2019 Salivary Glands for BDS
21/47
Sarcoidosis
Sarcoidosis: It mostly affectsthe parotid gland producinglocalized tumor like swelling(sarcoid pseudotumor).
Heerfordt syndrome(uveoparotid fever) is a form ofsarcoidosis characterized by
fever, parotid swelling, uveitisand facial palsy. The diagnosis isconfirmed by biopsy revealingnoncaseating granulomas.Treatment is with steroids.
-
8/11/2019 Salivary Glands for BDS
22/47
Cat Scratch Disease
It usually affects children and
caused by Bartonella henselae.
A pustule forms at the site ofinfection following a scratch by a
cat.
It is followed by cervical
lymphadenopathy and parotidgland enlargement. It is a self-
limiting condition and resolveswithout treatment.
-
8/11/2019 Salivary Glands for BDS
23/47
Salivary gland tumours
-
8/11/2019 Salivary Glands for BDS
24/47
Etiology
Exact etiology is unknown.
Risk factors include:- Low dose ionizing radiation to head and neck (in dental
X-rays). High dose radiotherapy has no role.
- EB virus.
- Occupational hazard: Exposure to hard wood dust,nitrosamines (rubber industry).
- Tobacco: Warthinstumor is strongly associated withsmoking.
-
8/11/2019 Salivary Glands for BDS
25/47
Histological classification
A. Epithelial Tumours
Adenoma:
- Pleomorphic adenoma
- WarthinsTumour
Carcinoma
- Low grade: Acinic cellcarcinoma, Adenoid cystic
carcinoma, Low grademucoepidermoid carcinoma
- High grade: Squamous cellcarcinoma, Adenocarcinoma,Carcinoma in pleomorphic,Adenoma, High grademucoepidermoid carcinoma
B. Non-Epithelial Tumours
Angioma Lipoma
Neurofibroma
Lymphoma
Sarcoma
Metastatic tumors
-
8/11/2019 Salivary Glands for BDS
26/47
Parotid Gland Tumours
-
8/11/2019 Salivary Glands for BDS
27/47
Pleomorphic Adenoma
It is a mixed parotid tumour.
Pathologically it has the following features:
- Epithelial and myoepithelial cells proliferate in sheets and strands.
- Pseudocapsule (formed by compressed parotid tissue around thetumor).
- Pseudocartilage (mucoid material separating epithelial cells giveappearance of cartilage).
- Pseudopodia (strands of tumour cells project through thepseudocapsule into adjoining part of the parotid gland).
Due to presence of pseudopodia, simple enucleation of tumour willleave behind residual tumour leading to recurrence. Hence,superficial parotidectomy is the recommended treatment even fora benign tumour.
Cli i l f t
-
8/11/2019 Salivary Glands for BDS
28/47
Clinical features Clinically, it presents as a painless
slow growing mass that is rubberyand nodular in consistency.
The mass classically raises the earlobule and obliterates theretromandibular groove.
Even in big tumor, the mass is notadherent to overlying skin orunderlying masseter muscle andthere is no facial palsy.
Deep lobe tumors present withfullness in retromandibular areaalong with soft palate swelling.
Long standing pleomorphic adenomamay convert to carcinoma in 5%cases.
-
8/11/2019 Salivary Glands for BDS
29/47
Pleomorphic Adenoma
The signs of malignant change(Fig. 15.11) are:
- Sudden increase in tumor size.
- Facial nerve palsy.
- Tumor consistency becomes hard.
- Tumor becomes fixed to underlying
structures and invades overlyingskin.
- Cervical lymph node enlargement.
- Limited jaw movements due tomandibular invasion.
-
8/11/2019 Salivary Glands for BDS
30/47
WarthinsTumour
It is also called as adenolymphoma.
Not a true lymphoma but this name is given due topresence of lymphoid tissue in the tumor.
Consists of cystic spaces lined by double layeredepithelium.
Usually affects middle aged or elderly males.
Presents as a slow growing soft swelling at lower pole ofparotid gland
-
8/11/2019 Salivary Glands for BDS
31/47
-
8/11/2019 Salivary Glands for BDS
32/47
Other parotid tumours Acinic cell tumour: low grade tumor and is composed of serous acini. It is
soft and cystic. Rarely it may metastasize.
Mucoepidermoid Tumor: Composed of sheets and masses of epidermoidcells and cystic spaces lined by mucus secreting cells. Low grade tumor hamore cystic spaces and fewer cells, slow growing with rapid metastasis tolymph node while high grade tumor has more cells, less cystic spaces,metastasizes to lungs. It is most common salivary neoplasm in children.Clinically, patients present with a hard mass in the gland.
Adenoid Cystic Carcinoma: It is most common malignant salivary tumor. Itconsists of myoepithelial and duct cells, which are arranged in sheets andcords and give cribriform or lace like appearance. Its characteristicfeature is perineural invasion and bone invasion. Thus, tumor is alwaysmore extensive than seen clinically or on radiograph. Clinically, it presentas a hard fixed mass. Later, patient may complain of pain, anesthesia ofoverlying skin and muscle paralysis due to involvement of related nerves.
-
8/11/2019 Salivary Glands for BDS
33/47
Submandibular Gland Tumours
They are uncommon and usually present as a painlessslow growing swelling in submandibular triangle.
In 50% cases, they are benign in nature.
The submandibular gland tumor is bimanually palpable.
This clinical sign helps in differentiating it fromsubmandibular lymphadenopathy which is not palpablebimanually.
Treatment is submandibular gland excision with a cuffof normal tissue.
-
8/11/2019 Salivary Glands for BDS
34/47
-
8/11/2019 Salivary Glands for BDS
35/47
Investigations
-
8/11/2019 Salivary Glands for BDS
36/47
Radiological Investigations
CT scan and MRI are good for evaluation of malignant
masses that are deep seated and fixed.
CT scan and MRI help in defining location and extent oftumor, evaluation of neck nodes.
Bone destruction is best seen on CT scan.
MRI is useful in detecting perineural invasion,intracranial extension of tumor and detecting deep lobeparotid tumors.
PET scan is superior to CT and MRI in detecting localrecurrence and distinguishing it from past treatmentfibrosis.
Cytopathology
-
8/11/2019 Salivary Glands for BDS
37/47
Cytopathology
Preoperative tissue diagnosis is not required in discreet parotid swelling.
FNAC is done when there is high clinical suspicion of malignancy.
Surgery is modified if report is lymphoma. In suchcase, only incision biopis done instead of tumor excision so as to grade the tumor.
If report is Warthinstumor in an old patient, the treatment isconservative (no surgery).
FNAC is also useful in recurrent and inoperable tumors for planningradiotherapy as initial treatment.
Open biopsy is not done routinely due to risk of injury to facial nerve andspreading of tumor cells.
Biopsy is indicated in following conditions:
- Repeated FNAC inconclusive in a hard fixed mass.
- In case of lymphoma for tumor grading.
-
8/11/2019 Salivary Glands for BDS
38/47
Treatment
Benign and slow growing neoplasm confined to superficial lobe of
-
8/11/2019 Salivary Glands for BDS
39/47
Benign and slow growing neoplasm confined to superficial lobe ofparotid gland is treated with superficial parotidectomy with facialnerve conservation.
In deep lobe tumors, first superficial parotidectomy withidentification of facial nerve is completed. Then with blunt
dissection, deep lobe tumor is removed from in-between nervebranches.
Malignant and high grade parotid tumors requiresuperficial/total/radical parotidectomy with or without sacrifice offacial nerve depending on tumor extent.
- Radical parotidectomy may include removal of whole parotid gland
with facial nerve, adjoining muscles (masseter, pterygoids) andmandible.
- Most important aim of surgery in malignant tumor is To achieveclear margins of resection. Clearance of surgical margins can beconfirmed by intraoperative frozen section of the excisedspecimen
-
8/11/2019 Salivary Glands for BDS
40/47
Superficial Parotidectomy
Treatment for pleomorphic adenoma
Superficial lobe along with tumor is removed Facial nerve branches are identified and
preserved
Avoids tumor spillage and removes pseudopodia
Simple enucleation will leave behind residual
tumor leading to recurrence Complications: Flap necrosis, Fluid collection
(haematoma, infection), Facial Nerve palsy,Fistula (salivary), Freys syndrome, sensory lossto lower pinna.
-
8/11/2019 Salivary Glands for BDS
41/47
Facial Nerve Mgt.
Preoperative functional status of facial nerve should be assessed by physical
examination and look for any partial or total facial nerve palsy.
In case of absence of clinical nerve involvement and presence of surgicalplane between tumor and the nerve during operation, the facial nerve shouldbe preserved.
In case of preoperative facial palsy and operative findings of nerve invasionby the tumor, the involved area of nerve should be resected.
After nerve resection, immediate reconstruction by sural or greater auricularnerve should be done and its success rate is 75%.
Rehabilitation procedures should be performed simultaneously in form of:
- Gold weight upper eyelid implants.
- Lower lid tightening.
- Static facial slings.
-
8/11/2019 Salivary Glands for BDS
42/47
Mgt. Of Neck Nodes:
Neck dissection should be done in node positive casesonly.
Modified radial neck dissection is the preferredtechnique.
In high grade tumors with clinically negative neck nodes,
frozen section of suspicious nodes should be done. There is no benefit of elective node dissection in
clinically negative neck.
-
8/11/2019 Salivary Glands for BDS
43/47
-
8/11/2019 Salivary Glands for BDS
44/47
Radiotherapy
Area of radiotherapy includes preoperative extent with 2 cm margin.
In adenoid cystic carcinoma, radiotherapy is also given to named nerve roots
up to the base of skull.
In inoperable tumors, radiotherapy is given for palliation.
In case of recurrent malignant tumors, if resection is not possible, then highdose radiotherapy is given as:
- External beam RT
- Neutron RT or
- Brachytherapy
-
8/11/2019 Salivary Glands for BDS
45/47
Freys Syndrome Also known as gustatory sweating.
Occurs from damage to salivary innervation during dissection.
There is inappropriate regeneration of parasympathetic fibresleading to stimulation of sweat glands of overlying skin. As a result,sweating and skin flush occurs during salivary stimulation.
Freys syndrome can be prevented by inserting temporalis fascialflap between skin and parotid bed during parotidectomy.
Treatment is with
- Topical anticholenergic agent (1% Glycopyrrolate).
- Botulinum toxin injection into affected skin.
- Denervation by division of lesser superficial petrosal nerve.
Sj S d
-
8/11/2019 Salivary Glands for BDS
46/47
SjgrensSyndrome
It is an autoimmune syndrome causing progressive destruction ofsalivary and lacrimal glands.
Primary Sjgrenssyndrome is characterized by presence of dryeyes (keratoconjunctivitis sicca) and dry mouth (xerostomia). Ifassociated with some other disorder, its called secondary Sjgrenssyndrome.
Females are affected ten times more than males.
There is painful enlargement of salivary glands.
Sialography shows punctate sialectasis. Biopsy of minor salivary glands show focal lymphocytic infiltration.
Treatment is symptomatic in form of artificial tears for dry eyesand oral hydration along with salivary substitutes for dry mouth.
There is increased risk of developing lymphoma especially inprimary Sjgrenssyndrome.
-
8/11/2019 Salivary Glands for BDS
47/47