Imaging of salivary glands
-
Upload
walaa-mohamed-hamed -
Category
Documents
-
view
913 -
download
8
Transcript of Imaging of salivary glands
Imaging of salivary glandsPresented by:
Sara Mahanna
&
Soha Osama
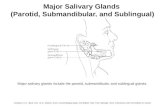
Introduction:Anatomy of salivary glands: there are three major salivary glands: parotid, submandibular and sublingual. These are paired glands that secrete a highly modified saliva through a branching duct system.
Parotid saliva is released through Stensons duct, the orifice of which is visible on the buccal mucosa adjacent to the maxillary 1st molars
Sublingual saliva may enter the floor of the mouth via a series of independent ducts, but will empty into the submandibular (Whartons) duct about half of the time. The orifice of whartons duct is located sublingually on either side of the lingual frenum.
There are also thousands of minor salivary glands throughout the mouth named for their location ( labial, buccal, palatal,etc) lie just below mucosal surface and communicate with oral cavity via short ducts.
They share basic anatomic structure composed of acinar and ductal cells arranged much like a cluster of grapes on stems. The acinar cells (the grapes) = secretory endpiece and are sole site of fluid transport into the duct. The ductal cells ( the stems) = branching system carries the saliva from the acini into the oral cavity
Salivary gland diseases:I II III IV functional disorders obstructive disorders non neoplastic disordes neoplastic disorders
I functional disorders:- sialorrhea ( increase in saliva flow)
I functional disorders:-xerostomia (decrease in saliva flow)
I functional disorders:-mucocele (mucous retention cyst)
I functional disorders:- ranula ( sublingual salivary gland mucocele)
I functional disorders:
II obstructive disorders:sialolithiasis: (formation of calcified obstruction within the duct) submandibular gland lithiasis
II obstructive diseases:Parotid lithiasis:
III Non neoplastic disorders:Acute Sialadenitis :viral( mumps)
bacterial (staph aureus, strept pyogenes)
III Non neoplastic disorders:Chronic sialadenitis( strept viridans)
III Non neoplastic disorders:Necrotizing sialometaplasis; Involves minor salivary glands in hard palate of no definite etiology
IV Neoplastic disorders:Epithelial: -adenomas e.g:pleomorphic adenoma
-mucoepidermoid tumor. -acinic cell tumor -carcinomas. E.g: adenocarcinoma
Non epithelial:Malignant lymphoma. Unclassified tumors.
Allied conditions:Benign lymphoepithelial lesions. Sialosis (hyperplasia) oncocytosis
Sjogrens syndrome :
Salivary gland imaging modalities:
[1] Plain RadiographyImportance : (1) It may identify unrelated pathoses in the areas of salivary gland that can be mistakenly identified as salivary gland disease. e.g. :- Resorptive or osteoblastic changes in adjacent bone causing periauricular swelling mimicking parotid tumor panoramic or posteroaterior view may demonstrate bony lesion, thus exclude salivary pathosis
(2) It is useful when patient history and clinical examination suggests prescence of sialolith
(3) Carcinomas can be apparent on plain radiography But when destructive changes occur to adjacent osseous structures.
Intraoral radiography : Submandibular sialolith [A] Anterior 2/3 of the whartons duct :- it can be imaged by To pographic mandibular occlusal projection
[B] Posterior part of duct :- can be demonstrated by posterior oblique view, where patients head is tilted back & inclined toward unaffected side. The central ray is parallel with mandible in area of submandibular fossa and posterior part of floor of mouth.
Parotid Saliolith :
In Ant part stensons duct anterior to masseter :- imaged by Intraoral film that is held by hemostate against the cheek as high as possible in buccal sulcus over the parotid papilla, the central ray is perpendicular to the film. The distal portion of the duct :- difficult to demonstrate on intraoral film because of tortuous course of the duct around anterior border of masseter muscle and buccinator muscle .
Extraoral RadiographySubmandibular Sialolith : Panorama demonstrate sialotith in posterior duct. demonstrate Intaraglandular sialolith . Lateral projection demonstrate Sialolith in the gland but the projection is modified by opening patient mouth, extending the chin, depressing the tongue with index finger this usually moves image of sialolith inferior to mandibular border where image is apparent.
Parotid Saliolith : Lateral projection difficult to demonstrate parotid sialolith or in distal part of duct because it is superimposed over ramus and body of mandible But it can be demonstrated by posteroanterior view. Posteroanterior projection made with check puffed out moving the image of sialolith free of bone making it visible on image. Also, this can demonstrate intraglandular sialolith.
Appearance of Sialolith in plain radiography:* Sialolith appears radiopaque object as it is calcified * Long standing stones appear more radiopaque than surrounding bone. * It is important to use about half the usual exposure to avoid over exposure of sialolith. * Some stones are not well calcified (of high organic content) , that appear radiolucent , these sialolith better demonstrated by sialography 20% of sialolith of submandibular gland 40% of Sialolith of parotid gland Rarely in sublingual gland
Sialography
Definition:Is radiographic visualization of salivary gland following retrograde instillation of radiopaque contrast medium into ductal system of salivary gland The film obtained is called sialogram
what is a contrast medium?!Def:Is a radiographic diagnostic agent of high opacification ( In dental field iodine compounds are mainly used ) Kinds : Water- soluble (ionic):urographin (diatrizoate) Soluble in saliva can diffuse to glandular tissue RG density = poor visualization. Oil based (non ionic) : lipidol Used only intraductal never intravenous ( can cause emboli ) Not diluted in saliva or across the mucosa maximum opacification Higher viscocity water soluble contrast agents or suspensions are also available
Requirements : 1- Inert pharmacologically 2- Non Toxic 3- Similar to saliva physiologically (PH & surface tension) 4- Easily evacuated through : Blood , oral cavity & Kidney .
Problem : iodine may induce allergic reaction or interfere with thyroid function or evaluation Symptoms : pain , flushing , headache or it may be fatal death To avoid : History , skin test, explanation, premedication (antihistaminic)
Uses of sialography:*Sialography provides clearest visualization of branching ducts & acinar end pieces *Chronic inflammatory diseases, ductal pathosis & localized sialolith or stricures (obstructions) are easily recognized. * When patients present history of rapidonset , acute painful swelling of a single gland (typically brought on by eating). * Whereas potential neoplasms are better visualized by CT or MRI. *Valuable tool in presurgical planning prior to the removal of salivary masses.
Mainly for:Parotid gland & submandibular gland although sublingual gland is difficult to infuse intentionally it may be opacified while infusing whartons duct to image the submandibular gland .
Method:[a] pateint preparation : 1- Scout film , is initial plain film for :- Use as a background for interpreting the sialogram -Visualizing radiopaque stones and potential bony destruction. 2- Antiseptic mouth wash to alleviate bacterial activity 3- Anatomical demarcation of duct orifice 4- Application of local anaesthesia around orifice to remove pain.
[b] Filling phase : 1- Successive graduated sizes of lacrimal probes are used for duct dilatation 2- Place the cannula or polyethylene catheter. 3- Use empty syringe for sucking the residual saliva present to avoid back pressure. 4- Hypodermic plastic syringe 2cm or 3cm loaded with contrast medium is applied. - Inject slowly till patient feels discomfort (usually between 0.2 and 1.5 ml depending on the gland being studied - Fluoroscopic monitoring is recommended by some otherwise static films monitoring . 0
[c] Taking the radiograph : N.B: ( Dont remove the cannula till the sialogram is processed) I- Parotid gland : oblique lateral true lateral-posteroanteior (occipitofrontal) puffed cheek II- Submandibular gland : best seen with mandibular occlusal view
Normal appearance :Normal ductal architecture is leafless tree appearance. The submandibular gland demonstrate more abrupt transition in ductal diameter whereas parotid demonstrate a gradual decrease in diameter .
What abnormalities can be detected ??* Ductal strictures , obstruction, dilatation ductal ruptures & stone can be visualized
Sausage appearance
* Sialectasis : is the appearance of focal collection of contrast medium within the gland, seen in sialadenitis, Sjogrens syndrome. The progression of severity is classified into punctate, globular and cavitary.
* Ball between two fingers benign tumors ( slowly growing well capsulated pressure on ductule)
Non opaque sialoliths appear as voids Bizzar or beading appearance malignant tumors.
[d] Emptying phase : (evacuation ): - The gland is allowed to empty for 5 minutes without stimulation. - Then sialogogue such as lemon juice or 2% citric acid, bubble gums or massage to the gland is done to encourage evacuation Post evacuation image after approximately 1 hour to assure complete evacuation . If substantial amount of contrast material remains follow up visits until completely emptying or fully resorption of it. Otherwise look for : obstruction of salivary flow extraductal or extravasated contrast collection of contrast material in abcess cavities or impaired secretory function .
Complication with sialography & contraindications:1- Allergic reaction against iodine 2- Perforation of duct during procedure (extraductal injection ) that may lead to granulomatous reaction 3- Acute exacerbation of chronic conditions If performed during active infection may further irritate & potentially rupture the already inflamed gland 4- Anticipitated thyroid function tests.
Ultrasonography:
Principle:x-ray equipment is replaced by a very high frequency (3.5- 10 MHZ) ultrasound beam which is directed in to body from a transducer placed in contact with the skin . US traveled through body and reflected back by tissue interfaces to produce echoes that is picked up by same transducer electrical signal black, white & grey visual echo picture which is displayed on screen
uses:Recently , it is reliable in demonstration of sialolith, 90% of stones larger than 2mm are detected as echo-dense spots with characteristic acoustic shadows. It can distinguish between diffuse inflammation (echo free light image ) and suppuration (less echo free-darker) image. Also it can detect abcess cavity if present.
It is of low diagnostic importance to sjogrens syndrom parenchymal inhomogencity only .
The primary application of US is differentiation of solid masses from cystic ones. Cystic lesions Sharply marginated & echo-free (dark area ) Benign masses less echogenic than parenchyma & well circumscribed . Malignant masses homogenous echo pattern with low reflectivity & attenuation, poorly defined margins.
N.B Sonography is unable to visualize deep lobe of parotid as it lies medial to the ascending ramus of the mandible
Nuclear medicine, (Scintigraphy ), Radioisotope scan
DefinitionA technique provide functional study of salivary gland taking advantage of selective concentration of specific radiopharmaceuticals in the glands.
Technique- Intravenous injection of 99m Tc pertechnetate , it is then concentrated in and excreted by glandular structures including salivary gland, thyroid, & mammory glands. - The radionuclide appear in ducts of salivary glands .within minutes and reaches maximal concentration within 30-45 minutes. - A Sialogogue is administred to evaluate secretory capacity . - Importance: Pathosis can be demonstrated by an increased, decreased or absence of radionuclide uptake.
Examples :Sjogrens syndrome Scintigraphy is useful for diagnosis & monitoring progression of syndrome. Impairment of parotid and submandibular is demonstrated by decreased uptake of 99m Tc as well as delay in its stimulated excretion. In cystic lesions decreased radioisotope uptake (cold spot )
But it doesnt give differential diagnosis because Benign and malignant tumors also appear as coldpot. So CT & MRI are preferable for evaluation of salivary masses. Also , scintigraphy demonstrates little morphology. Scintigraphy is advantageous in conditions in which sialography is contra indicated & in patients where ducts cant be cannulated.
Computerized Tomography
Principle:ct scanners use x-ray to produce sectional or slice image in which the receptor is a gas detector or sensitive crystal that measure the intensity of the x-ray beam emerging from the patient ( produce an attenuation or penetration profile) convert it into representing different tissue densities = visual image
Equipment:
Planes:
Types:Enhanced ct (contrast medium) Ultra fast ct Spiral ct
Thickness of the slice ( 1.5 ml 6 ml ) advantage of no superimposition Manipulation: - window level: bony level, soft tissue level differentiation between soft and bony lesions Window width:narrow; enable to see minute differences Wide
Reconstruction: to any other plane or production of 3D image without additional exposure to the patient
Applications in salivary gland:Normal CT scan after right submandibular sialogram
spiral ct
contrast enhanced ct of the neck demonstrate a stone (blue arrow) in the submandibular region of a dilated Whartons duct (red arrow)
Abscess of the submandibular salivary gland. Post contrast CT shows enlarged right submandibular gland with central low density (small arrow) and irregular peripheral contrast enhancement (arrowhead).
Abscess of the submandibular salivary gland. Post contrast axial CT image demonstrates a calcified stone (arrow) in the right submandibular gland. This is consistent with an abscess of the right submandibular gland secondary to an obstruction from a stone (calculus).
Magnetic Resonance Image :Idea: It uses electrical and magnetic fields and radiofrequency pulses rather than ionizing radiation. It involves the behaviour of Hydrogen protons in a magnetic field to produce the image.
Importance : * It is better than CT in demonstrating soft tissue image and vascular tumors . * It demonstrates the margins of salivary gland masses , Internal structures & regional extension of lesions in to adjacent spaces. * But it is non specific in demonstration of inflammatory duct disease or autoimmune salivary gland disorders
Normally :- Parotid gland appear in T1 weighted image & T2 weighted image having greater intensity than muscle & lower intensity than fat. - Structures that appear dark on both T1 & T2 weighted images include calcifications, rapid blood flow & fibrous tissue.
- In Benign tumors : may present as low intensity (dark) or high intensity (light) signal on T1 & T2 weighted image & proton density weighted format.
- In high grade malignancies : present as low intensity (dark) signal on T1 & T2 weighted MRIs. T1 Weighted image have low intensity (dark) than surrounding structures & are relatively homogenous. T2 Weighted image brighter than T1 Weighted image and are slightly darker than surrounding & are more heterogenous.
Examples:
MR Sialogram of the parotid gland
Conclusion
UltrasonographyIndication: Biopsy guidance; mass detection Advantage: Noninvasive; cost-effective Disadvantage: No quantification of function; observer variability; limited visibility of deeper portions of gland; no morphologic information
SialographyIndication: Stone, stricture; R/O autoimmune or radiation-induced sialadenitis Advantage: Visualizes ductal anatomy/blockage Disadvantage: Invasive: require iodine dye; no quantification
Radionuclide imagingIndication: Autoimmune sialadenitis, sialosis, tumor Advantage: Quantification of function Disadvantage: Radiation exposure; no morphologic information
Computerized tomographyIndication: R/O calcified structure; tumor Advantage: Differentiate osseous structures from soft tissue Disadvantage: No quantification; contrast dye injection ( in enhanced); radiation exposure
Magnetic resonance imagingIndication: R/O soft-tissue lesion Advantage: Soft-tissue resolution excellent, with ability to differentiate osseous structures from soft tissue; no radiation burden Disadvantage: No quantification; contraindicated with pacemaker or metal implant; dental scatter
References:Oral radiology and interpretation (White . Pharoh) Burkets oral medicine (diagnosis and treatment) Oral and maxillofacial diseases Websites (google,.)