Salivary glands
-
Upload
dushyantsinh-vala -
Category
Education
-
view
143 -
download
4
Transcript of Salivary glands
04/15/2023 1
Salivary glands
Presented by:Dr. Dushyantsinh Vala
Guided by:Dr. Nidhi DhakarDr. Rajat VarshneyDr. Vinayak KM
04/15/2023 2
Contents • Introduction • Composition of saliva • Functions of saliva • Anatomy of salivary glands • Development • Structure • Formation and secretion of saliva• Ductal modification of saliva • Histology of the major salivary glands• Histology of the minor salivary glands• Age changes • Clinical considerations
04/15/2023 3
Introduction
• The oral cavity is kept moist by a film of fluid called saliva that coats the teeth and the mucosa.
• Saliva is a complex fluid, produced by the salivary glands, the most important function of which is to maintain the well-being of mouth.
• Individuals with a deficiency of salivary secretion experience difficulty in eating, speaking, and swallowing and become prone to mucosal infections and rampant caries.
04/15/2023 4
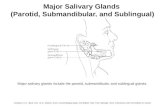
• In human beings, three pairs of major salivary glands- the parotid, submandibular, and sublingual.
• They are located outside the oral cavity, with extended duct systems through which the gland secretions reach the mouth.
• Numerous smaller minor salivary glands are located in various parts of the oral cavity- the labial, lingual palatal, buccal, glossopalatine, and retromolar glands- typically located in the submucosal layer, with short duct openings directly onto the mucosal surface.
04/15/2023 5
Saliva
• Is a clear, slightly acidic, mucoserous secretion.
• The whole saliva is a complex mixture of fluids, with contributions from major and minor salivary glands and the gingival crevicular fluid, containing a high population of normal oral bacteria, desquamated epithelial cells and transient residues of food or drink, following their ingestion.
04/15/2023 6
Composition of saliva Parameter Characteristics
Volume 600-1000ml/day
Electrolytes Na+, K+, Cl-, Ca2+, Mg2+and F-
Secretory proteins/peptides
Amylase, proline-rich proteins, mucins, histatin, cystatin, peroxidase, lysozyme, lactoferrin and defensis.
Immunoglobulins Secretory immunoglobulins A, immunoglobulins G and M
Small organic Glucose, amino acids, urea, uric acid, and lipid molecules
Other components Epidermal growth factor, insulin, cyclic adenosine monophosphate-binding proteins, and serum albumin
04/15/2023 7
Functions of saliva Function Effect Active constituents
Protection Clearance Water
Lubrication Mucins, glycoproteins
Thermal or chemical insulation
Mucins
Tannin binding Basic proline-rich proteins, histatins
Buffering pH maintenance Bicarbonate, phosphate, basic proteins, urea, ammonia
Neutralization of acids
04/15/2023 8
Function Effect Active constituents
Tooth integrity Enamel maturation, repair
Calcium, phosphate, fluoride, statherin, acidic proline-rich proteins
Antimicrobial activity
Physical barrier Mucins
Immune defense Seretory immunoglobulin A
Non-immune defense
Peroxidase, lysozyme, lectoferrin, histatin, mucins, agglutinins, secretory leukocyte protease inhibitor and defensins
Tissue repair Wound healing, epithelial regeneration
Growth factors, trefoil proteins
Digestion Bolus formation Water, mucins
04/15/2023 9
Function Effect Active constituents
Digestion Starch, triglyceride digestion
Amylase, lipase
Taste Solution of molecules Water and lipocalins
Maintenance of taste buds
Epidermal growth factor and carbonic anhydrase VI
04/15/2023 10
• Gland- An organized aggregation of cells functioning as a secretory or excretory organ.
04/15/2023 11
Classification of Glands
• Glands can be divided into two groups:
1. Endocrine glands- are glands that secrete their products onto a surface rather than through a duct. • e.g.- Adrenal gland, Pituitary gland.
04/15/2023 12
2) Exocrine glands- These glands secrete their products via a duct. e.g.- Salivary glands. It can be divided into three groups:-
a) Merocrine gland e.g.-Mucous and Serous glands b) Apocrine gland e.g.-Sweat glands c) Holocrine gland e.g.-Sebaceous glands
04/15/2023 13
Classification Of Salivary Glands
1) ACCORDING TO SIZE:
A) MAJOR B) MINOR Parotid Glands of Lips, Submandibular Cheeks , Hard Sublingual Palate, Soft palate, Von Ebners and Blandin & Nuhn.
04/15/2023 14
2) ACCORDING TO BRANCHING OF DUCTS: A) Compound- Major glands
B) Simple- Minor glands
3) ACCORDING TO SECRETION:
SEROUS MUCOUS MIXED a)Parotid a)Palatine a)Submandibular b)Von-ebner b)Post. lingual b)Sublingual c) Glossopalatine c)Buccal d)Labial.
04/15/2023 16
Parotid gland • Is the largest • Weight – 15gms
• Is situated below the External acoustic meatus, b/w the ramus of the mandible and the sternocleidomastoid and overlaps them.
• Secretion of parotid gland is serous. • Anteriorly , the gland overlaps the masseter muscle. A part of
this forward extension is often detached – Accessory Parotid which lies b/w the zygomatic arch and the parotid duct.
04/15/2023 18
Parotid Capsule• The investing layer of deep cervical fascia forms the capsule
for the gland.
• The fascia splits to enclose the gland.
• Superficial lamina – thick & adherent to the gland.
• Deep lamina – thin – attached to the styloid process, the mandible and tympanic plate.
• A portion of deep lamina, extending between the styloid process and the mandible – thickened to form Stylomandibular Ligament –separates the Parotid gland from the Submandibular salivary gland.
04/15/2023 19
External Features
• The glands has four surfaces
a) Superior
b) Superficial
c) Antero-medial
d) Postero-medial
• The surfaces are separated by three borders.
a) Anterior
b) Posterior
c) Medial
04/15/2023 20
Relations
1. Superior surface related to
External acoustic meatus
Superficial temporal vessels
Posterior surface of TMJ
Auriculotemporal nerve
2. Superficial surface (largest)
a) Skin
b) Superficial fasciai. Great auricular nerve
04/15/2023 21
ii) Pre-auricular lymph node
iii) Posterior fibers of platysma
c) Parotid fascia
d) Deep parotid lymph nodes
3. Anteromedial surfaceo Masseter o Lateral surface of TMJo Posterior border of the mandibleo Medial pterygoido Terminal branches of facial nerve
04/15/2023 23
3. Posteromedial surface
Mastoid process Sternocleidomastoid Posterior belly of the digastric Styloid process
04/15/2023 24
5. Anterior border :
– Separates the superficial surface from the Anteromedial surface
– Extends from –anterior part of the superior surface to the apex
– Structures emerging: Parotid duct Terminal branches of the facial nerve Transverse facial vessels
04/15/2023 26
6. Posterior border :
– Separated the superficial surface from the posteromedial surface
– Overlaps the sternomastoid.
7. Medial border :
– Separates the Anteromedial surface from the posteromedial surface.
– Related to the lateral wall of pharynx.
04/15/2023 27
Structures within the Parotid Gland
1. Arteries • ECA-external carotid
artery• Maxillary artery• Superficial temporal
vessels • Posterior auricular
artery
04/15/2023 28
2. Veins
• Retromandibular vein divides into:
1. Posterior division drains into external jugular vein
2. Anterior division drains into common facial vein
04/15/2023 29
3. Nerves • Terminal branches of facial
nervea) Temporal
b) Zygomaticc) Buccald) Mandibulare) cervical
• Parotid lymph nodes
04/15/2023 30
Nerve Supply:• Parasympathetic nerves are secretomotor.
-Reach the gland through the auriculotemporal nerve. • Sensory – auriculotemporal nerve.• Sympathetic nerves are vasomotor
–Derived from the plexus around the external carotid artery
Lymphatic Drainage
• Upper deep cervical nodes
Blood Supply :• ECA• Veins – drain into external jugular vein
04/15/2023 31
Parotid Duct
• Stensen’s duct-5cm long
• Emerges from the substance of the gland to course anteriorly until it reaches the anterior border of the masseter muscle at a point of the upper and middle third.
• When it crosses the masseter muscle it receives the duct of the accessory lobe.
04/15/2023 32
• Around the border of the masseter muscle-turns sharply medially, often embedded in the furrow of the protruding buccal fat pad.
• In its medial course ,the duct reaches the outer surface of the buccinator muscle, where it perforates in the oblique direction anteriorly and medially.
• Then runs for a short distance obliquely forward, between the buccinator and the mucous membrane –opens on the oral surface of the cheek
04/15/2023 33
Submandibular gland • Situated in the anterior part of the Digastric triangle
• Size that of a walnut
• Is J-shaped
• Secretion of submandibular gland is both serous and mucous.
• Divided by the posterior border of the Mylohyoid Muscle into
1. Larger part superficial to the muscle• Covers the inferior surface of the gland• Attached to the base of the mandible
04/15/2023 34
2. Small part lying deep to the muscle • Covers the medial surface of the gland• Attached to the mylohyoid line of the mandible
04/15/2023 36
Superficial part:
– Fills the digastric triangle– It has
a. Inferior surface-covered by- Skin Platysma Cervical branch of facial nerve Deep fascia Facial vein Submandibular lymph nodes.
04/15/2023 37
b. Lateral surface• Submandibular fossa on the mandible• Facial artery
c. Medial surface divided intoa) Anterior part – related to the – Mylohyoid muscle– Nerve – Vessels
04/15/2023 38
b) Middle part-• Hyoglossus• Styloglossus• Lingual nerve• Hypoglossal nerve
c) Posterior part-• Styloglossus• Stylohyoid ligament• IXth nerve• Wall of pharynx
04/15/2023 39
Submandibular Duct
• Called “WHARTONS” duct
• 5 cm long
• Emerges at the anterior end of deep part of the gland
• Runs forwards on the hyoglossus ,between the lingual and the hypoglossal nerves
• Opens in the floor of the mouth on the summit of the sublingual papilla, at the side of the frenum of the tongue
04/15/2023 41
BLOOD SUPPLY AND LYMPHATIC DRAINAGE :• Facial artery• Veins drain into common facial vein or lingual vein• Lymph passes into the Submandibular lymph nodes
NERVE SUPPLY :• Supplied by branches from• Submandibular ganglion• These convey
– Secretomotor fibers– Sensory fibers from lingual nerve– Vasomotor sympathetic fibers from facial artery.
04/15/2023 42
Sublingual gland• Is the smallest
• Almond shaped
• 3-4gm weight
• Secretion of sublingual gland is both serous and mucous.
• Lies above the mylohyoid, below the mucosa of the floor of the mouth
• Medial to the sublingual fossa
04/15/2023 43
• Lateral to genioglossus
• About 15 ducts emerge from the gland –
Called ducts of rivinus
BLOOD SUPPLY:• Lingual and submental
arteries.
04/15/2023 45
Minor Salivary Glands• Scattered & distributed in gaps beneath the epithelium having
small & narrow ducts
• Present almost on all parts of the oral cavity
• Absence of separate capsule on the glands
• They can be divided into:a) Labial & buccal glandsb) Palatine glandsc) Glands of tongue-anterior glands -posterior glands -Von ebners’ glands
04/15/2023 47
LABIAL & BUCCAL GLANDS
• Present under epithelium of lips & cheeks
• Mixed in nature
• Intercalated duct are variable in length.
04/15/2023 48
PALATINE GLANDS
• Present at glandular region of hard palate i.e. posterolateral part of hard palate.
• Pure mucous gland
04/15/2023 49
GLANDS OF TONGUE
Anterior Gland:
• Near apex of tongue anterior lingual gland are present. These are glands of Blandin & Nuhn.
• Mucous in nature
• Ducts of these gland open on ventral surface of tongue near lingual frenum.
04/15/2023 50
Posterior Glands:
• Present on posterior part of tongue near suclcus terminalis
• Mucous in nature
• Ducts open at dorsal surface of tongue
von Ebner’s gland:
• Serous gland
• Opening through vallate papilla.
04/15/2023 51
Development Of Salivary Glands
Development of salivary glands occurs in six stages:
1) Bud Formation 2) Formation And Growth Of Epithelial Cords 3) Branching Of Cords 4) Dichotomous Branching 5) Canalization 6) Cytodifferentation.
04/15/2023 52
Stage 1-Bud Formation
• Underlying mesenchyme induces the overlying epithelium to proliferate. The epithelium thus forms a bud.
04/15/2023 53
Stage 2 -Formation And Growth Of Epithelial Cord
• The epithelial bud proliferates to form a solid cord of cells.
• The underlying mesenchymal condensation also proliferates.
04/15/2023 54
Stage 3-Branching Of Cords
• The epithelial cord proliferates rapidly and branches into terminal bulbs. This stage donates the initiation of branching.
04/15/2023 55
Stage 4-Dichotomous Branching
• The terminal end branches extensively forms numerous bulbs.
• The connective tissue below the epithelial cord forms a capsule and surrounds the entire glandular structure.
04/15/2023 56
Stage 5-Canalization
• Extensive branching of the duct structure and growth of connective tissue septa continues at this stage of development.
• First in distal ends of main cord & in branch cords then in proximal part of main cord & finally in central portion of main cord
04/15/2023 57
Stage 6- Cytodifferentation
• At last there is cytodifferentation of the functional acini and intercalated ducts.
04/15/2023 58
Development Of Salivary Gland In Intrauterine Life
• Parotid Gland- 4th Week of intrauterine life
• Submandibular Gland- 6th Week of intrauterine life
• Sublingual Gland- 8th week of intrauterine life
• Minor glands- 12th week of intrauterine life.
04/15/2023 59
Molecular analysis
• The mechanism(s) by which tissues interact include "instructive" interactions in which the changes induced in the responding tissue are totally new and would not have occurred unless the specific interaction had taken place.
• The changes associated with the determination (the commitment to a specific function) of a cell's developmental pathway are usually induced by an "instructive“ type of interactive event.
04/15/2023 60
• Other types of heterotypic interactions are "permissive" in nature in that they facilitate the full expression of tissue characteristics that have already been determined.
• Thus, "instructive" interactions tend to restrict the cell's developmental options, while 'permissive'' interactions regulate or amplify the degree of expression or stabilization of the remaining developmental potential of the cell.
• Developmental, heterotypic tissue interactions between the mesenchyme and the epithelium play a significant role in inducing and controlling both the morphogenesis and the cytodifferentiation of developing salivary glands.
04/15/2023 61
Epithelial-mesenchymal interactions in salivary gland morphogenesis
• Epithelial mesenchymal interactions between the epithelium of the salivary gland anlage and its mesenchymal capsule directly control the development of the gland's characteristic branching pattern.
• The mesenchyme appears to exercise control over the behavior of the salivary epithelium through the selective production and destruction of specific extracellular matrix molecules
04/15/2023 62
• These extracellular matrix molecules are deposited in and near the basement membrane, which serves as the interface between the epithelial cells and their investing mesenchymal capsule.
• It consists of a complex mixture of molecules, including proteoglycans (heparan sulfate, chondroitin sulfate), laminin, type IV collagen, fibronectin, and entactin .
• The dynamic nature of the molecular composition of the basement membrane permits the structure to induce and maintain developmental changes in the encased epithelium.
04/15/2023 63
Role of collagen • Collagen, produced by the capsular mesenchyme, was the
important molecule in regulating and maintaining the branching pattern of the submandibular gland.
• Collagen serves as a stabilizing component that inhibits cell growth in specific areas of the growing salivary gland rudiment, while other areas are devoid of collagen and thus able to grow.
• The synthesis and deposition of both types I and III collagen appear to be required for salivary gland branching morphogenesis.
04/15/2023 64
• Types I and III collagen appear to prevent hyaluronidases and other enzymes from digesting the basement membrane by binding with heparan sulfate proteoglycan and other basement membrane components to stabilize the basal lamina.
• Deposition of type III collagen at the cleft or branch point areas seems to play a key role in regulating both assembly of basal lamina components and stabilizing these points so that branching may go forward.
04/15/2023 65
Role of fibronectin
• Fibronectin is expressed by the salivary gland epithelium, but also that it was expressed at much higher levels in cleft compared to bud epithelium.
• Fibronectin and fibronectin receptor function are needed for cleft formation, the initial stage of salivary gland branching morphogenesis.
04/15/2023 66
Other extracellular molecules
• Laminin γ2- it is expressed highly in the epithelial end bud regions of salivary glands.
• It might regulate the development of embryonic epithelium in various organs by stimulating cell motility ; in the salivary gland, it might be involved in outward bud expansion.
• Extracellular matrix proteins undergo degradation and turnover by matrix metalloproteinases (MMPs).
04/15/2023 67
Structure of Salivary Glands
• Is architecturally TUBULOACINAR
• Consists mainly of: 1.Terminal secretory units- Acini 2. Ductal system 3. Myoepithelial cells
04/15/2023 68
• General structure of salivary gland is compared with bunch of grapes with grapes represent the secretory acini while stalk represent ductal system.
04/15/2023 69
• Acini• The basic functional unit of salivary gland is the terminal
secretory unit called Acini.
• The cells in the acini rest on basement membrane and are arranged in single layer.
• The central lumen of each acini may have a star shaped morphology .
• The secretory terminal unit in serous acini is generally made up of 8-12 serous surrounding a central lumen.
04/15/2023 71
• Serous cells
• Cells are pyramidal in shape.
• Base resting on basal lamina & apex towards lumen
• Nucleus spherical in shape & located basal third of pyramid.
• Accumulation of secretory granules in apical cytoplasm
• That have many protein granules in their cytoplasm which secrete polysaccharides.
04/15/2023 73
• Plasma membrane of serous cells exhibit several specialization.
• Luminal Surface : contain intercellular canaliculi with few microvilli.
• Lateral surface: occasional folds
• Basal surface : regular folds .5µm deep( this folding increases surface area of cells)
• Basal cytoplasm contain cisternae of rough endoplasmic reticulum, golgi complex forming secretory granules of variable size & density.
04/15/2023 75
• These granules increase in density as their content condensed & forming mature secretory granules.
• This cells joined by each other or mucous gland by intercellular junction such as:
1. Tight junctions (zonula occludens)-->fusion of outer cell layer
2. Intermediate junction (zonula adherens)-->intercellular communication
3. Desmosomes-->firm adhesion
04/15/2023 77
• Mucous cells• Specialized for synthesis, storage, and secretion of secretory
proteins. Mucous secretion differs from secretion of serous in two respects:
a) have little or no enzymatic activity. b) ratio of carbohydrate to protein is greater.
• In cross section these tubules appear as round profile with mucous cell surrounding central lumen
• In electron microscope mucous secretory appear swollen, their membrane are disrupted & they often fused with one another.
04/15/2023 79
• Mucous end pieces in major salivary glands & some minor glands have serous cell associated with them in form of crescent covering the mucosa cells at end of tubules.
• Accumulation of apical cytoplasm of large amount of secretory product (mucous) which compress nucleus & endoplasmic reticulum against basal cell membrane.
• Have large golgi complex located mainly basal to mass of secretory granules.
04/15/2023 82
• Ductal system
• Comprises a varied network of ducts characterized by progressively narrow membranes.
• The network contains 3 classes of ducts:
a. Intercalated ductsb. Striated ductsc. Terminal excretory ducts
04/15/2023 83
INTERCALATED DUCTS
– The secretion of the terminal end piece first pass through the intercalated ducts.
– Are of small diameter
– Lined by short cuboidal cells with centrally placed nucleus and little cytoplasm
– Contains RER which is situated basally and golgi complex situated apically
04/15/2023 84
• Secretory granules are occasionally found.
• Prominent in glands with watery secretion
• Hence occur in parotid gland
04/15/2023 86
• Striated Ducts
• Receive saliva from intercalated ducts.
• The intercalated ducts pass into the striated ducts.
• Lined by columnar cells
• Have centrally placed nucleus and intense eosinophilic cytoplasm.
• Characteristic features – Prominent striations at the basal ends of the cell
04/15/2023 87
• Around the nucleus a few RER and golgi complex are found.
• Luminal surface is characterized by short, stubby microvilli
• Adjacent cells are united by junctional complexes and desmosomal attachments
• Are always surrounded by no. of longitudinally oriented blood vessels.
04/15/2023 89
• Excretory ducts
• The salivary fluid is secreted into oral cavity through the terminal excretory ducts.
• Near the striated ducts it is lined by a pseudo stratified epithelium consisting on tall, columnar cells.
• After passing through the striated ducts ,the salivary fluid is secreted through the terminal excretory ducts.
04/15/2023 90
• As the terminal secretory ducts approach the oral cavity, their epithelium changes to true stratified epithelium merging with that of the oral cavity.
04/15/2023 91
• Myoepethelial cells
• Stellate or spider-like with flattened nucleus, scanty perinuclear cytoplasm.
• Their appearance is reminiscent of a basket cradling the
secretory unit, hence the term BASKET CELL.
• These cells are contractile in nature like muscle. These cells contract causing pulsation & release of secretory product from end cell.
• These are also end piece cells but non secretory in nature.
04/15/2023 92
• These cells have octopus like structure having cell body present in intercalated duct region with processes extending onto parts of secretory end piece.
• In body of cell small flattened nucleus is present.
• From cell body 4 to 8 processes radiate.
• b/w myoepithelial cells & secretary cells desmosomal attachment present.
04/15/2023 93
• Cytoplasmic organism present in perinuclear region.
• Cells act as support for secretory cells by preventing their over distention, because secretory product accumulate within their cytoplasm.
• These cells also contract & widen the diameter of intercalated ducts. Thus they lower or increase their resistance to flow.
04/15/2023 95
• Primary saliva– Serous and mucous cells– Intercalated ducts
• Modified saliva– Striated and terminal ducts
• Production And Secretion Of Saliva
04/15/2023 96
• Saliva is formed in the secretory end pieces and consists of 2 components:
a) Macromolecular components: Derived from the Secretory and synthetic activity
of acinar cells.
b) Fluid component: derived from blood
04/15/2023 98
• In mechanism of salivary secretion, protein secretion occurs by exocytosis, that is, the fusion of secretory granules with the luminal membrane to release their content into the lumen.
• The binding of sympathetic transmitter norepinephrine (NE) to beta-adrenergic receptors on the basolateral membrance activates a heterotrimeric G-protein (Gs), which in turn activates adenylyl cyclase (AC), catalysing the formation of cyclic adenosine monophosphate (cAMP) from adenosin triphosphate (ATP).
04/15/2023 99
• Cyclic adenosine monophosphate activates protein kinase A (PKA), which phosphorylates other proteins in a cascade leading to exocytosis.
• Fluid and electrolyte secretion is stimulated mainly by the binding of the parasympathetic transmitter, acetylcholine (Ach) to muscarinic cholinergic (MC) receptors and also by norepinephrine binding to alpha-adrenergic receptors.
04/15/2023 100
• These receptors activate a heterotrimeric G-protein (Gq/11), causing activation of phopholipase C (PLC), which converts phophatidylinositol bisphosphate (PIP2) to inositol triphosphate (IP3) and diacylglycerol (DAG).
• Inositol triphosphate causes the release of Ca2+ from intracellular stores, probably the endoplasmic reticulum.
• The increased ca2+ concentration opens Cl- channels in the luminal membrance and K+ channels in the basolateral membrane and activates basolateral Na+/K+/2Cl- cotransporter.
04/15/2023 101
• The increased luminal cl- is balanced by the movement of extracellular Na+ across the tight junction, and resulting osmotic gradient pulls water into the lumen through the cell via water channel aquaporin 5 and through the tight junction.
• The basolateral Na+/K+/2Cle- cotransporter and the Na+/K+ adenosine triphophatase serve to maintain the intracellular electrolyte and osmotic balances.
04/15/2023 102
Ductal modification of saliva
• Striated duct cells resorb Na+ and Cl- mainly via channels in the luminal membrane; Na+/H+ and Cl-/Hco3- exchangers provide additional mechanisms for uptake of these ions.
04/15/2023 103
• Na+ exist at the basolateral surface maintain electroneutrality, and the Na+/H+ exchanger compensates for intracellular acidification.
• the tight junctions are relatively tight and the duct cells are impermeable to water.
04/15/2023 104
REGULATION OF SALIVA
2 varieties of salivary secretion:
1. Spontaneous : Occurs all the time, without any known
stimulus this keeps mouth moist all the time.
2. Stimulated : Occurs of known stimulus may be
1. Psychological
2. Visual
3. Taste
4. Others (during vomiting)
04/15/2023 105
Secretory Unit (salivon)
• The basic unit “salivon” consists of:
• Acinus -initial secretory process
• Intercalated duct -initial portion of duct
• Striated duct -modification of secretory product
• Myoepithelial cells surround acinus and intercalated duct contraction of which moves saliva and prevents development of back pressure
04/15/2023 106
Age changes
• Generalized loss of salivary gland parenchymal tissues occurs.
• Lost salivary cells often replaced by adipose tissues.
• Increase in fibrous connective tissue and vascular cells
• Gradual reduction in proportional acinar volume in major salivary glands.
• Decreased production of saliva
04/15/2023 107
ANOMALIES OF THE SALIVARY GLANDS
I. Developmental Aberrant Salivary Glands Aplasia and Hyperplasia Atresia
II. Obstructive conditions Sialolithiasis Mucocele Necrotizing Sialometaplasia
04/15/2023 108
.III. Inflammatory Diseases Viral Mumps H.I.V. Associated Bacterial Sialadenitis
V. Degenerative Conditions Sjogren’s Syndrome Ionizing Radiation
VI. Xerostomia
IV. Neoplastic Diseases Benign Malignant
Epithelial Mesenchymal
04/15/2023 110
Mikulicz’s disease
• Is a progressive autoimmune disease of the salivary gland characterised by replacement of gland acini by dense infiltrates of T lymphocyes along with squamous metaplasia of the dental epithelium.
• It’s a local benign lymphoepithelial lesion, which frequently involves the parotid and lacrimal glands.
• According to many investigators the disease is closely related to sjogren’s syndrome.
04/15/2023 111
• The exact etiology of the disease is not known, some people believe that genetic abnormality or defective cell-mediated immunity probably causes the disease.
• The disease can be associated with Xerostomia, which is sometimes very severe.
• The onset of disease is often marked with fevere, upper respiratory tract infection and any other oral and orofacial infections.
• However mikulicz’s disease should not be confused with mikulicz’s syndrome, which refers to parotid and lacrimal gland enlargement of lymphnodes.
• The mikulicz’s syndrome may represent some generalized specific diseases, e.g. lymphomas or tuberculosis, etc.
04/15/2023 112
Sjogren’s syndrome• Is a multi-system immune mediated chronic inflammatory disease,
characterized by lymphocytic infiltration and acinar destruction of salivary and lacrimal glands, with a marked predilection for women.
• It is believed that the disease is an autoimmune disorder.
• Rheumatoid factors, which are associated with many autoimmune disorders, are frequently present in sjogren’s syndrome.
• Presence of serum antinuclear antibodies (ANA) e.g. Anti Sjogren’s syndrome-A (anti-SS-A) and anti Sjogren’s syndrome-B (anti-SS-B) also further increase the probability of this disease.
04/15/2023 113
• Primary Sjogren’s syndrome is also reffered to as “sicca syndrome” in which dry mouth (xerostomia) and dry eyes (xerophthalmia or keratoconjuctivitis sicca) are the principal features.
• Secondary Sjogren’s syndromes characteristically have xerostomia, xerophthalmia and associated autoimmune CT diseases, usually the rheumatoid arthritis.
• The systemic disease can be any of following, lupus erythematous, systemic sclerosis, primary billiary cirrhosis, polymyositis, etc.
04/15/2023 115
Saliva in dental caries
• Decreased saliva flow rate, decreased buffer capacity, increased number of S. mutans and Lactobacilli in saliva are usually associated with increased caries prevalence.
• Similarly, decreased level of certain salivary proteins such as
proline-rich proteins (PRP1, PRP3), histatin 1, and statherin is associated with signifcantly higher caries-susceptibility
04/15/2023 116
Saliva and periodontal disorders
• Several marker proteins, saliva may be used for periodontal disorder screening.
• The levels of proteolytic granulocyte enzyme elastase,
protease inhibitor alpha1-antitrypsin,, and elastase inhibitor alpha2-macroglobulin may increase considerably under gingivitis and/or periodontitis.
04/15/2023 117
Saliva and xerostomia
• In xerostomia usually resting unstimulated whole saliva flow rate is less than 0.1.0.2 mL/min and stimulated flow rate is less than 0.4.0.7 mL/min.
• In serious cases, saliva demonstrates low pH and buffer capacity, increased total protein albumin and sodium concentration, decreased amylase/protein ratio, and high lactobacillus and yeast concentration.
04/15/2023 118
• Moreover, the level of alpha2-macroglobulin is also a good indicator of an individual’s periodontal status).
• Salivary level of 3-hydroxy-fatty acids (lipid constituent of lipopolysacharide endotoxin of several anaerobic bacteria) are also good indicators of chronic periodontitis.
• Albumin may also correlate with gingival inflammation.
04/15/2023 119
Salivary changes under medication
• Numerous kinds of medications such as anticholinergics, antide- pressants, antipsychotics, diuretics, benzodiazepines, antihypertensive agents, muscle relaxants, analgesics, and antihistamines have been reported to induce xerostomia, although some (antipsychotics, benzodiazepines, and antihypertensive drugs) may also induce siallorhea .
• Antiepileptic drugs also induce signifcant changes in saliva; however, in this case the level of flow rate and pH usually remains normal.
04/15/2023 120
• Phentoin, valproate, and carbamazepine medications increase the amylase and total protein concentration and decrease the cystatin S concentration (but not the cystatin C).
• However, it should also be considered that degradation and decreased bacterial aggregation was probably caused by poor oral hygiene in this group.
04/15/2023 121
The most important salivary changes in several systemic conditions
Condition Usual but not speciÞc changes in the saliva
Anxiety Decrease of flow rate
Depression Decrease of flow rate
Acute stress Decrease of sIgA,Increase of amylase, salivary chaperon Hsp70, stress hormonesPrompt changes of mucins. adhesive properties
Sj¨ogren.s syndrome Decrease of flow rate, phosphateIncrease of sodium, chloride and several salivary proteins
Cystic Þbrosis Increase of electrolytes, lipids, and prostaglandin E2Unusual form of EGF
04/15/2023 122
References • Tencate’s-Oral Histology. Antonio Nanci, Elsevier, seventh
edition.• Orban,s-oral histology and embryology. GS Kumar, Elsevier,
twelfth edition.• A colour atlas and textbook of oral anatomy histology and
embryology. B.K.B. Berkovitz, G.R. Holland, B.J. Moxham, Wolfe, second edition.
• B D Chaurasia; Human Anatomy; Volume 3 – Head, Neck & Brain, 4th edition
• Leslie S. Cutler and Waldemiro Gremski. Epithelial-mesenchymal Interactions In The Development Of Salivary Glands. Critical Reviews in Oral Biology and Medicine, (1991);2(1): 1—12.