Salivary Glands
description
Transcript of Salivary Glands

Page
45
Group 4 SALIVARY GLANDS Section B
THE CASE
A 48-year-old white female presented for evaluation of a neck mass. She first noted the mass 5 years earlier. She reported that it was larger at first but shrank slightly after a course of oral antibiotics. Since that time, its size had not changed. The mass was accompanied by tinnitus, impaired hearing and earache. Review of systems revealed no hoarseness, dysphagia, or weight loss. Past medical history was also positive for multiple medical problems, including diabetes and pulmonary tuberculosis. She was taking multiple medications, including anti Koch’s medications. Social history was positive for 15 pack-years of smoking, although the patient quit 7 years before the visit. Physical examination revealed a 3x3-cm non-tender mass below the angle of the left jaw. The consistency of the mass was soft. The mass was mobile and did not seem to be attached to either the skin or underlying structures. No other masses were noted in the head and neck. No adenopathy was noted in the groin, axilla, or extremities.
Clinical Findings:
MRI:
Histological Findings:
Low Power
High Power
OBJECTIVES

Page
45
Group 4 SALIVARY GLANDS Section B
General Objectives: To analyze the case and make a diagnosis To make a list of differential diagnosis based on the clinical findings, gross and
microscopic features.
Specific Objectives: To review the normal anatomy and histology of the salivary glands To identify the pertinent clinical information for the given case. To discuss the clinical features, gross and microscopic findings of the different
differential diagnosis. To discuss the management for the case presented.
THE SALIVARY GLANDS

Page
45
Group 4 SALIVARY GLANDS Section B
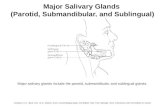
There are three major and innumerable minor pairs of salivary glands. The largest, on the cheek, is the parotid, where most neoplasms arise. The smaller major glands are the sublingual and submandibular, under the tongue and jaw. In general, the smaller the gland, the higher the proportion of its neoplasms that are malignant. Salivary neoplasms can arise in virtually any part of the sinonasopharyngeal system.
Figure 1. 1 = parotid gland; 2 = submandibular gland; 3 = sublingual gland.
Normal HistologyThe first major cell type is the secretory cell. The salivary glands are composed of serous and mucinous secretory units and ducts (Figure 1). Serous cells are wedge shaped (like pie slices) and arranged in acini around ducts. They are full of blue to purple granules. Mucinous cells have basal nuclei and apical mucin, like goblet cells; these are also arranged in acinar formations. The parotid is primarily serous, the submandibular is mixed, and the sublingual is primarily mucinous.
The second major cell type is the duct cell. The duct system has three types of ducts: the terminal, or intercalated ducts; the intermediate-sized striated ducts; and the interlobular large ducts. Each has a different epithelium and is theoretically associated with different tumor types. The intercalated ducts are small profiles with low cuboidal epithelium, similar to a bile ductule (Figure 2). Striated ducts are more proximal and are larger, with pink columnar cells full of mitochondria and striated basal borders (hard to see). Interlobular or excretory ducts have pseudostratified columnar epithelium with or without goblet and squamous metaplasia. Different tumors have some morphologic similarity to these different ducts, which may help you keep all of the neoplasms straight.
FIGURE 2 Normal salivary gland. In this example of mucinous salivary gland, the columnar secretory cells (arrowhead) form acini arranged around salivary
FIGURE 3. Types of ducts. (A) In the parotid, which has mainly serous glands, the terminal or intercalated ducts are visible as small tubules lined by cuboidal epithelium (arrowheads). The medium-sized striated ducts are more oncocytic in appearance, with abundant pink cytoplasm (arrow). (B) The large interlobular ducts have pseudostratified columnar epithelium (arrow), with occasional goblet cells, and become squamous at their junction with the gingival mucosa
The third cell major cell type is the myoepithelial cell. These cells, as in breast, surround acini and ducts. They are normally pale stellate cells with small nuclei and are very hard to identify in normal salivary gland. However, many neoplasms arise from the epithelial –myoepithelial cell line or, more specifically, from cells that can differentiate into either line. This creates a diagnostic nightmare, because the myoepithelial cells alone can take four different forms: spindled, plasmacytoid, epithelioid, or clear. Therefore, you must recognize any of these variants as

Page
45
Group 4 SALIVARY GLANDS Section B
myoepithelial (their immunologic profiles change with their form, unfortunately) and lump some very different-looking tumors into the same basket. Table 25.1 lists the most common neoplasms.
Note that, in general, benign lesions are encapsulated, whereas malignant tumors are infiltrative, either as pushing fronts or as tendrils of cells (although mucoepidermoid carcinoma and acinic cell carcinoma can be deceptively well circumscribed). The first thing you should do when evaluating a salivary neoplasm is to study the periphery or capsule.
AnatomyThe salivary glands are situated at the entrance to the gastrointestinal system to help begin the process of digestion.
a) Parotid GlandsThe parotid glands are a pair of glands located in the subcutaneous tissues of the face overlying the mandibular ramus and anterior and inferior to the external ear. The secretion produced by the parotid glands is serous in
nature, and enters the oral cavity through the Stensen's duct after passing through the intercalated ducts which are prominent in the gland. Despite being the largest pair of glands, only approximately 25%
of saliva is produced by the glands.
b) Submandibular GlandsThe submandibular glands are a pair of glands located beneath the floor of the
mouth, superior to the digastric muscles. The secretion produced is a mixture of both serous and mucous and enters the oral cavity via Wharton's ducts.
Approximately 70% of saliva in the oral cavity is produced by the submandibular glands, even though they are much smaller than the parotid glands.
c) Sublingual Gland
The sublingual glands are a pair of glands located beneath the floor of the mouth anterior to the submandibular glands. The secretion produced is mainly mucous in nature, however it is categorized as a mixed gland. Unlike the other two major glands, the ductal system of the subligual glands do not have striated ducts, and exit from 8-20 excretory ducts. Approximately 5% of saliva entering the oral cavity come from these glands.
d) Minor Salivary GlandsThere are over 600 minor salivary glands located throughout the oral cavity within the lamina propria of the oral mucosa. They are 1-2mm in diameter and unlike the other glands, they are not
encapsulated by connective tissue only surrounded by it. The gland is usually a number of acini connected in a tiny

Page
45
Group 4 SALIVARY GLANDS Section B
lobule. A minor salivary gland may have a common excretory duct with another gland, or may have its own excretory duct. Their secretion is mainly mucous in nature (except for Von Ebner's glands) and have many functions such as coating the oral cavity with saliva. Problems with dentures are usually associated with minor salivary glands.[1]
Glands located close to the oral cavity have mainly mucous secretions, whereas glands located further away from the oral cavity have mainly serous secretions. Following this general rule, the parotid glands contain almost exclusively serous acini, the submandibular glands contain both serous and mucous acini, and the sublingual glands contain mainly mucous acini or mucous acini with serous demilunes.
InnervationSalivary glands are innervated, either directly or indirectly, by the parasympathetic and sympathetic arms of the autonomic nervous system.
* Parasympathetic innervation to the salivary glands is carried via cranial nerves. The parotid gland receives its parasympathetic input from the glossopharyngeal nerve (CN IX) via the otic ganglion, while the submandibular and sublingual glands receive their parasympathetic input from the facial nerve (CN VII) via the submandibular ganglion.
* Direct sympathetic innervation of the salivary glands takes place via preganglionic nerves in the thoracic segments T1-T3 which synapse in the superior cervical ganglion with postganglionic neurons that release norepinephrine, which is then received by β-adrenergic receptors on the acinar and ductal cells of the salivary glands, leading to an increase in cyclic adenosine monophosphate (cAMP) levels and the corresponding increase of
saliva secretion. Note that in this regard both parasympathetic and sympathetic stimuli result in an increase in salivary gland secretions. The sympathetic nervous system also affects salivary gland secretions indirectly by innervating the blood vessels that supply the glands.

SIGNS & SYMPTOMSTinnitusImpaired hearingEarache
SIGNS & SYMPTOMSTinnitusImpaired hearingEarache
NO
MALIGNANT
Mucoepidermoid CAMucoepidermoid CA
Adenoid Cystic CAAdenoid Cystic CA
Acinic Cell CAAcinic Cell CA
Malignant Mixed Tumor
Malignant Mixed Tumor
AdenocarcinomaAdenocarcinoma
PAST MEDICAL HXPAST MEDICAL HX
Pulmonary TBPulmonary TBDiabetes MellitusDiabetes Mellitus Taking oral antibioticsTaking oral antibiotics
Anti-Kochs MedicationCiprofloxacinClarithromycinCycloserineDexamethasoneEthambutolIsoniazidPyridoximePyrazinamide Rifampicin
Streptomycin
Anti-Kochs MedicationCiprofloxacinClarithromycinCycloserineDexamethasoneEthambutolIsoniazidPyridoximePyrazinamide Rifampicin
Streptomycin
REVIEW OF SYSTEMS(-) Hoarseness(-) dysphagia(-) weight loss
REVIEW OF SYSTEMS(-) Hoarseness(-) dysphagia(-) weight loss
CHARACTERISTICS OF MASSSlow-growing (5yrs)3X3 cmNontenderMobileSoftNo Invasion
(Do not seem to be attached to either the skin/underlying structure)
CHARACTERISTICS OF MASSSlow-growing (5yrs)3X3 cmNontenderMobileSoftNo Invasion
(Do not seem to be attached to either the skin/underlying structure)
NECK MASSNECK MASS
LOCATION: Below the Angle of the left jaw
LOCATION: Below the Angle of the left jaw
Tail of the Parotid GlandSubmandibular GlandTail of the Parotid GlandSubmandibular Gland
NO
Oncocytoma>60y/o
Oncocytoma>60y/o
Monomorphic Adenoma
>60y/o
Monomorphic Adenoma
>60y/o
Myoepithelioma>50y/o
Myoepithelioma>50y/o
Warthins TumorM:F = 5:1race: WHITEbilateral
Warthins TumorM:F = 5:1race: WHITEbilateral
YES
BENIGN
AGE (48 years old)
AGE (48 years old) YES
FEMALEFEMALE
NO YES
PLEOMORPHIC ADENOMA
M:F = 1:3-4Race: white; unilateral
PLEOMORPHIC ADENOMA
M:F = 1:3-4Race: white; unilateral

DIFFERENTIAL DIAGNOSES
Trying to find an explanation for a mass found on the neck area is like trying to find a needle in a haystack. Masses in this area is a common sign of a myriad of clinical conditions that can involve pathologies in the head and the lungs, for example.
Starting from the simplest reason, a mass in the neck can a sign of an ongoing infection, particularly of the oral cavity. The cervical lymph nodes drain structures located in the mouth and in the lungs. The individual might have dental caries or even pulmonary tuberculosis. The presence of a painful, mobile and well-defined mass in the cervical region indicates an infection.
In contrast, malignant masses are painless, fixed, and its margins are not easily recognizable. But the assumption that painless, fixed masses should not immediately rule out malignancy. The definitive diagnosis of a malignant condition has to be supported by cytologic and imaging techniques to avoid making a false diagnosis and give undue fear and anxiety to the patient.
In the case, the patient is a 48-year-old female that presented with a mass at the angle of the jaw. The mass was first noticed 5 years prior to consultation, indicating that it is a slow-growing tumor. After intake of oral antibiotis, the mass reduced in size and the size did not change since. The mass was soft, mobile, non-tender, measuring 3x3 cm. The mass was accompanied by tinnitus, impaired hearing and earache. Hoarseness, dysphagia or weight loss was not encountered.
The following sections will discuss conditions of the salivary glands that are most likely to explain the patient’s condition. There are benign lesions as well as malignant ones. Lymphadenopathy and lymphomas are also considered as they can both cause swelling in the cervical area.
The age and gender of the patient was one of the factors that helped in narrowing the differential diagnoses. However, majority of the neoplasms seem to have preference for women so the differentials were still a lot. Slow growing tumors were also considered as the mass that the patient has was assumed to grow slowly because it took the patient five years before she consulted. The characteristics of the mass itself, also help to differentiate whether the lesion was benign or malignant. The painless presentation of the mass may indicate that it is a malignant tumor so malignant tumors are also considered. Soft consistency and mobility are characteristics of a benign lesion, therefore some benign neoplasms are considered.

DIFFERENTIAL DIAGNOSIS: PLEOMORPHIC ADENOMA(a.k.a. Benign Mixed Tumor)
Pleomorphic adenoma is the most common neoplasm of the salivary glands. It is about ten times more common in the parotid than in the submaxillary gland, and it is very rare in the sublingual gland. In the parotid gland, most tumors arise within the superficial lobe, from either the tail (50%) or the anterior portion (25%). The remaining 25% arise from the deep lobe and are often present as a pharyngeal mass without external evidence of tumor. Though it is classified as a benign tumor, pleomorphic adenomas have the capacity to grow to large proportions and may undergo malignant transformation, to form carcinoma ex pleomorphic adenoma, a risk that increases with time. Although it is "benign", the tumor can recur after resection, it invades normal adjacent tissue and distant metastases have been reported after long (+10 years) time intervals.
A. Etiology and EpidemiologyIt is most frequent in women, with a female-to-male ratio of 3:2, in the fourth decade of life, but it can be seen in children and in elderly persons of either sex. White persons have a slightly higher risk of pleomorphic adenomas than that of other races.
B. PathogenesisPleomorphic adenoma gene 1 (PLAG1), shown to be consistently rearranged in pleomorphic adenomas, is activated by chromosomal translocations involving 8q12, the chromosome region that is most frequently affected in these tumors. This causes PLAG1 to be juxtaposed to the gene for Beta-catenin. This activates the catenin pathway and leads to inappropriate cell division.
C. Clinical FeaturesPleomorphic adenoma is usually solitary and presents as a slow growing, painless, soft, nodular mass commonly located at the back of the jaw just below the earlobe. It is usually mobile unless found in the palate and can cause atrophy of the mandibular ramus when located in the parotid gland. When found in the parotid tail, it may present as an eversion of the ear lobe. Almost all are asymptomatic, and they are usually brought to the attention of the physician when routine physical examination is performed or when the patient feels or sees a mass. Typically, the signs and symptoms have been present for at least a year before patients seek medical attention.
D. Gross MorphologyThe tumor forms a rubbery, resilient mass, with a bosselated surface and may grow to a large size. Although the tumor tends to be well-circumscribed and is surrounded by a fibrous capsule of varying thickness, the tumor extends through normal glandular parenchyma in the form of finger-like pseudopodia, caused by the variability in the growth rates of the various cell types. This is not a sign of malignant transformation (fig.5).
Figure 4. Pleomorphic adenoma is usually situated at the back of the jaw just below ear lobe

Figure 5. A well-circumscribed, round to ovoid mass, surrounded by a fibrous capsule (left), Resected tumor. Note the glassy appearance of some areas reflecting the myxoid and chondromyxoid regions of a pleomorphic adenoma. (right)
E. HistologyHistologically, it is highly variable in appearance, even within individual tumors. Classically it is biphasic and is characterized by an admixture of polygonal epithelial and spindle-shaped myoepithelial elements in a variable background stroma that may be mucoid, myxoid, cartilaginous or hyaline. Epithelial elements may be arranged in duct-like structures, sheets, clumps and/or interlacing strands and consist of polygonal, spindle or stellate-shaped cells (hence pleiomorphism). Areas of squamous metaplasia and epithelial plugs may be present (fig. 6). The stroma may have non-specific fibromyxoid appearance, sometimes containing abundant elastic tissue, however, areas of clearcut cartilaginous differentiation are usually found (fig. 7).
Some pleomorphic adenomas are extremely cellular. These may be confused with malignant tumors; however, the rarity of mitotic figures and absence of necrosis are of help in the differential diagnosis with true malignant neoplasms.
Figure 6. Epithelial elements arranged in duct-like structures with epithelial plugs

Figure 7. Pleomorphic adenoma of the salivary gland consists of mixed epithelial (above) and mesenchymal cell components (below). The latter often exhibits myxofibrous appearance and in some instances shows chondromatous differention.
F. ImmunohistochemicalThe ductal epithelial component is positive for keratin, epithelial membrane antigen, secretory component, CEA, lysozyme, alpha-1-antitrypsin, alpha-1-antichymotrypsin, lactoferrin, and steroid C-21 hydroxylase. Conversely, amylase is usually absent. The myoepithelial component is immunoreactive for keratin, actin, myosin, fibronectin, laminin, and S-100 protein. The latter marker is also strongly expressed in the cartilaginous areas and in a subtype of the epithelial ductal cells. The immunohistochemical profile of the epithelial component is similar to that of the normal intercalated duct cells, particularly regarding the expression of lactoferrrin and secretory component. The demonstration in some of the tumors of glial fibrillary acidic protein and astroprotein two glial markers, is more difficult to explain.
G. PrognosisThe prevalence of carcinoma ex pleomorphic adenoma ranges from 2-25%. The rate is certainly high enough that resection is typically warranted when the lesions are diagnosed.
If the fibrous capsule can be completely removed, these tumors can be cured with surgery. Local recurrence can occur when portions of the capsule is left. The rate of successful cure after recurrence is less than 25%, and recurrence rates of up to 50% are reported with enucleation procedures. These tumors are now typically treated with partial parotidectomy. With appropriate surgery, the recurrence rate is 1-5%, and these recurrences may be due to capsular disruption during surgery. Most of these recurrences will appear during the first18 months following surgery, but others supervene over an exceedingly long period (50 years or more). Because of this, long- term follow up is essential.Facial nerve injury can occur during resection of these tumors, as the tumor may arise close to the nerve. One group reported that more than 50% of the tumors in their study contacted the facial nerve. The approximate risk of facial nerve injury is 1-2% during initial surgery, with an increased risk in operations on recurrent tumors.
H. Pleomorphic Adenoma of the Middle EarMiddle ear pleomorphic adenoma is an extremely rare disease. It might have three possible origins that is, the ceruminal glands of the external auditory canal , ectopic salivary gland or metaplasia of the middle ear mucosa. Since normal ceruminal glands have never been identified within the middle ear cleft; ectopic salivary gland tissue has been reported to be present in the middle ear, and mucosal epithelium metaplasia is less likely to account for the mixed tumor elements in pleomorphic adenoma, most authors inclined to the origination from ectopic salivary glands.
Pleomorphic adenoma of the middle ear is charactertized by tinnitus and loss of hearing. Histologically, the t umor shows adenomatous proliferation, comprised of gland, duct, and epithelial cord (fig. 8).

Figure 8. Histological appearance of the tumor, showing adenomatous proliferation, comprised of gland, duct, and epithelial cord. (H & E,. x 350)

DIFFERENTIAL DIAGNOSIS: WARTHIN’S TUMOR(ak.a. Papillary Cystadenoma Lymphomatosum, Cystic Papillary Adenoma, Adenolymphoma)
Albrecht first recognized this tumor in 1910, and Warthin later described it in 1929. Warthin tumors are considered as the second most common neoplasm of the parotid gland. In gross appearance, it is a smooth, soft, parotid mass. They tend to be firm or rubbery in texture and may be nodular. A minority of patients may report rapid enlargement of the tumor with associated pain or pressure. It is well encapsulated when located in the parotid gland and contains multiple cysts.
A. Etiology and EpidemiologyAlthough Warthin tumor can occur elsewhere, it is most commonly found within the parotid gland. In one series, essentially all were located in the parotid. Another series found 90% within the parotid, 7.6% in cervical lymph nodes, and 2.3% in the submandibular glandi.
The etiology of Warthin's tumors is controversial and whether they are true neoplasms or developmental malformations continues to be debated. Some clonal analysis claimed that 7 cases showed a polyclonal pattern using a PCR method based on the trinucleotide repeat polymorphism of the X-chromosome linked human androgen receptor gene (HUMARA) and on random gene inactivation of the gene by methylation ii. Radiation exposure has been also linked to the development of the benign Warthin tumor.
It accounts for 4-15% of salivary gland neoplasms iii and is more common in men during their 6-7th decades iv. There is slight male predominance but there has been an increased incidence in women. There is low incidence of this neoplasm in African Americans. Smokers have 8x increased risk of developing this neoplasm.
B. Pathogenesis Although the pathogenesis of Warthin's tumour is not fully understood, it is generally thought that the tumor arises from hetero-topic salivary ducts within pre-existing lymphoid tissue. Prolonged nitric oxide (NO) production by the enzyme type 2 nitric oxide synthase (NOS2) has been implicated in the pathogenesis of many solid tumors, but not in Warthin's tumor. Since NO and NOS2 are known to be associated with p53, the immunohistochemical expression of both NOS2 and p53 was investigated in 23 cases of Warthin's tumor. Widespread diffuse cytoplasmic immunostaining for NOS2 was found in tumor epithelial cells of all 23 cases studied, and it was additionally expressed in normal salivary duct epithelium. p53 staining was localized to the nuclei of tumor epithelium in 16 cases, with a similar pattern of distribution to tumor NOS2 expression. A significant correlation was found between NOS2 and p53 staining in the tumors (P<0.001). In contrast to NOS2, p53 was not expressed by normal salivary ductal cells in any of the cases studied. NOS2 is widely expressed by the tumor epithelium of Warthin's, and its association with p53 expression is discussed. The role of NO in the pathogenesis of Warthin's tumor remains to be established. v
C. Clinical Manifestations
i Eveson J, Cawson R. Warthin’s tumor (cystadenolymphoma) of salivary glands. A clinicopathologic investigation of 278 cases. Oral Surg Oral Med Oral Pathol 1986; 61: 256–2.
ii Hum Pathol 2000;31:1377-1380
iii Weedon D. Weedon's Skin Pathology Second Edition. Churchill Livingstone. 2002
iv Robbins Pathologic Basis of Disease. Seventh Edition. WB Saunders 2005.
v BRENNAN Peter A. ; UMAR Tijjani ; SMITH Graham I. ; MCCAULEY Philip ; PETERS Winston J. ; LANGDON John D. ; Expression of type 2 nitric oxide synthase and p53 in Warthin's tumour of the parotid

The clinical manifestations of Warthin’s tumor include: swollen salivary gland, lump near back of lower jaw, jaw pain, sensation of pressure, facial nerve paralysis, tinnitus, impaired hearing, and earache. However, the tumor is asymptomatic in 90% of patients,
D. Gross MorphologyMost Warthin tumors are round to oval, encapsulated masses, 2 to 5 cm in diameter, arising in most cases in the superficial parotid gland, where they are readily palpable. Transaction reveals a pale gray surface punctuated by narrow cystic or cleft-like spaces filled with a mucinous or serous secretion.
Figure 9. Gross appearance of Warthin’s tumor.
E. HistologyOn microscopic examination, these spaces are lined by a double layer of neoplastic epithelial cells resting on a dense lymphoid stroma sometimes bearing germinal centers. The spaces are frequently narrowed by polypoid projections of the lypmhoepithelial elements. The double layer ohf lining cells is distinctive, with a surface palisade of columnar cells having an abundant, finely granular, eosinophilic cytoplasm, imparting an oncocytic appearance, resting on a layer of cuboidal to polygonal cells. Oncocytes are epithelial cells stuffed with mitochondria that impart the granular appearance to the cytoplasm. Secretory cells are dispersed in the columnar cell layer, accounting for the secretion within the lumens.
Histologically, the Warthin tumor has a heavy lymphoid stroma and aciniform epithelial cells that line the cystic areas with papillary projections. Warthin tumor tends to be bilateral (10% of cases) and is usually found in the major glands, as are most other types.

Figure 10. The Warthin tumor has a heavy lymphoid stroma and aciniform epithelial cells that line the cystic areas with papillary projections
F. Radiographic FindingsBenign and malignant parotid tumors cannot be distinguished with PET-CT alone because of high false-positive rates. It is necessary to consider all available clinical information, including prior oncologic and surgical history, to make an accurate diagnosis. vi, vii
Figure 11. CT SCAN of the neck (axial view) showing a rounded tumor at the right parotid gland
F. DiagnosisThe diagnosis of Warthin’s tumor is often obvious, just by the appearance of the cut surface of the tumor. Multiple cysts of varying diameter and containing variably viscous fluid are seen. The lining of the cysts appears shaggy and irregular. The lymphoid component makes up the solid areas of the tumor and lymphoid follicles can occasionally be seen. The pathognomonic microscopic features are epithelial cells forming papillary projections into cystic spaces in a background of a lymphoid stroma. The epithelium is a double cell layer with tall columnar cells lining the cystic spaces and cuboidal cells along the basement membrane. The nuclei of the columnar cells is oriented toward the cystic space while the cuboidal cell nuclei is oriented toward the basement membrane.
G. Course and Prognosis

All patients with this tumor survive, and the recurrence rate is 5%. Malignant transformation has not been observed.
DIFFERENTIAL DIAGNOSIS: MONOMORPHIC ADENOMA
The term “monomorphic adenoma” refers to a group of rare salivary tumors that includes the basal cell adenoma, canalicular adenoma, sebaceous, glycogen-rich and clear cell adenoma. Of these, the basal cell adenoma is the most common.
The majority of basal cell adenomas occur in the parotid gland where they present as a slowly enlarging firm mass. They are well-encapsulated, smooth tumors on gross inspection and are divided into four subtypes based on their microscopic appearance—solid, trabecular, tubular and membranous. A. Etiology and Epidemiology Basal cell adenoma constitutes 1.8% of benign epithelial salivary gland tumors and typically occurs in the 6 th
decade of life. There are conflicting reports of gender predilection for this tumor but it does seem to occur more frequently among Caucasians than African Americans.
The presentation of canalicular adenoma peaks in the 7th decade of life and, like the basal cell adenoma, is more common in whites than blacks. There is a female predominance with a female-to-male ratio of occurrence of 1.8-1. This tumor most commonly involves the minor salivary glands of the upper lip (74%) or buccal mucosal (12%).
B. Clinical ManifestationsClinically it presents as a nonpainful submucosal nodule. viii The signs and symptoms are typically the same as that of Warthin’s tumor. It includes swollen salivary gland, lump near back of lower jaw, jaw pain, sensation of pressure, facial nerve paralysis, tinnitus, impaired hearing, and earache C. Histology An important distinguishing feature is the palisading at the periphery of the epithelial nests, giving the tumor a “basaloid” appearance (Figure 5).the pattern of growth may be predominantly tubular, trabecular, or solid.

Figure 12. Basal Cell Adenoma. Histological section of the parotid mass shows material resembling basal membrane surrounding an island of tumor cells. Note the trabecular pattern of tumour cells, some of which have formed palisades, with narrow cytoplasm and hyperchromatic nuclei (haematoxylin and eosin x 100).
Canalicular adenoma is characterized by the presence of bilayered strands or ribbons of columnar cells separated by a loose, well-vascularized stroma. On gross pathologic examination, canalicular adenomas may or may not possess a capsule and it is not unusual for there to be multifocal growth. Microscopically there are cords of single-layer columnar or cuboidal cells forming duct-like structures in a background of fibrous stroma.
Figure 13. Canalicular Adenoma. There long strands or cords of epithelial cells, arranged in a double row. There cystic spaces of varying sizes enclosed by these cords. The cystic spaces are filled with eosinophilic coagulum. The supporting stroma is loose and fibrillar with delicate vascularity.
D. Radiographic FindingsMRI Scan shows a hyperintense mass lesion surrounded by a hypointense capsule. Note the higher intensity in the right lateral aspect of the lesion (Figure 7).

E. Course and PrognosisThe majority of monomorphic adenomas display nonaggressive behavior and are adequately treated with surgical excision.
DIFFERENTIAL DIAGNOSIS: ONCOCYTOMA(a.k.a. Oxyphilic Adenoma)
Oncocytoma are monomorphic adenomas, which are benign salivary gland tumors accounting for 1% of all salivary gland tumors, the majority of which occurs in the parotid gland (84%). Monomorphic adenomas lack a stromal component.
A. Etiology and EpidemiologyOncocytoma are found to be evenly distributed between men and women, usually common in old age (>50). It is also said to have an association with previous radiation exposure, sometimes up to 40 years prior to discovery of the rumor.
B. Clinical ManifestationsMost cases are asymptomatic, discovered only incidentally by ultrasound.
C. Gross MorphologyOncocytoma are solid, well-circumscribed tumors with a brown lobular cut surface. They are firm, slowly growing, painless masses of < 4 cm. They may also be bilateral.

D. HistologyOncocytoma are composed of oncocytes, which are cells that have abundant eosinophilic staining cytoplasm with a slight granularity, and with centrally located nuclei. This appearance is caused by numerous mitochondria. Some of these mitochondria contain large amounts of glycogen, and others are partitioned, suggesting division. Mitotic figures are absent and cellular transition from normal lining cells of the duct may be seen. Occasionally, the cells undergo a clear change due to cystic dilatation of the mitochondria.
DIFFERENTIAL DIAGNOSIS: ADENOCARCINOMA
Adenocarcinomas of the salivary glands represent those malignancies that cannot otherwise be easily classified. These are rare but aggressive tumors. About half of these tumors present in the parotid glands. The minor salivary glands, particularly the palate, lip and tongue are the next most commonly affected sites.
A. Etiology and EpidemiologyAccording to the bicellular stem cell theory, adenocarcinoma of the salivary gland arises from intercalated stem cells. Risk factors include ionizing radiation and genetic or familial predisposition. Adenocarcinoma is the second most common malignancy of salivary gland tumors. It comprises 9 % of all salivary gland tumors and 16.8 % of all salivary gland malignancies. They tend to present in patients over 40 years of age (range: 10-93 years, average: 58 years) and occur with nearly equal frequency in men and women (almost 1:1 ratio) 46:54
B. PathogenesisNumerous studies have investigated the role that tumor suppressor genes, especially the p53 family, play in the development of salivary gland neoplasms. One study found p53 mutations to be important in the development of both benign and malignant salivary gland neoplasms and that most mutations occurred in the fifth and eighth exons of the gene.

The function of oncogenes is also being elucidated. Murine double minute 2 (MDM2), a cellular protooncogene, which is capable, if amplified, of causing tumorigenesis by inactivating the p53 tumor-suppressor gene, has been found to be overexpressed in varying types of benign and malignant salivary gland tumors. Overexpression of MDM2 along with high-mobility group protein gene (HMGIC) has also been shown to lead to malignant changes that cause carcinoma. Mutated K-ras has been shown in mouse models to activate cellular pathways that lead to increased truncated p63 expression that inhibits p53 transcriptional activity.
C. Clinical ManifestationClinical presentation most often involves an enlarging mass. Adenocarcinoma is different from other salivary gland neoplasms in that as many as 25% of patients will complain of pain or facial weakness at presentation.
D. Gross PathologyGross pathology reveals a firm mass with irregular borders and infiltration into surrounding tissue. It is generally a solid tumor without any cystic spaces. These malignancies can demonstrate a wide range of growth patterns and, for this reason, can be somewhat difficult to classify.
E. HistologyAll adenocarcinomas have in common the formation of glandular structures and they are described as grades I, II or III based upon the degree of cellular differentiation. Grade I lesions have well- formed ductal structures while Grade III lesions have a more solid growth pattern with few glandular characteristics. Neoplastic cells form cords, sheets, nests and islands. Clear cells and oncocytic cells may be present.

F. TreatmentBecause these are more aggressive tumors, treatment for adenocarcinoma is more aggressive. Complete local excision is the mainstay of therapy. In the parotid this may include facial nerve sacrifice. In the minor salivary glands, a portion of the maxilla or mandible may have to be resected with the tumor. Although the efficacy hasn’t been definitely proven, postoperative radiation therapy does seem to be of some benefit. Lymph node metastasis is not uncommon and in patients with palpable neck disease neck dissection is warranted. Elective neck dissection should probably be reserved for patients with extensive local disease or high-grade lesions.
G. PrognosisLocal recurrence rates vary in the literature but have been cited as high as 51%. Regional metastasis has been reported in 27% and distant metastasis in 26%--most often to the lung and bone. Survival is dependent on the disease stage, which takes into account the extent and location of disease as well as the histologic tumor grade. The overall cure rate at 15 years is 67% for stage I, 35% for stage II and 8% for stage III
DIFFERENTIAL DIAGNOSIS: ADENOID CYSTIC ADENOMA
Adenoid cystic carcinom is a rare form of adenocarcinoma, arising from within secretory glands, most commonly the major and minor salivary glands of the head and neck. AdCC is found mainly in the head and neck, but can occasionally occur in the uterus or other sites in the body. It most commonly occurs in the salivary glands, which consist of clusters of secretory cells scattered throughout the upper aerodigestive tract. Therefore, tumors may arise in areas such as the palate, nasopharynx, tongue base, or mucosal lining of the mouth, larynx, or trachea. It may also occur in the major salivary glands (parotid, submandibular, or sublingual).
Regardless of where it originates, AdCC has the same basic biologic behavior. AdCC tends to spread along nerves (perineural invasion) or through the bloodstream. It only spreads to the lymph nodes in about 5% to 10% of cases. The most common place of metastasis is the lung.
A. Etiology and Epidemiology AdCC is most often diagnosed in people in their 40s to 60s, but there are documented cases of pediatric AdCC. Women are slightly more likely to be diagnosed with AdCC than men (the female to male ratio is approximately 3 to 2).

No strong genetic or environmental risk factors have been identified. Damage to the DNA genome occurs in the development of ACC, as it does in all cancers studied to date. Various studies have shown chromosomal abnormalities and genetic deletions occurring in samples of ACC. Multiple genetic aberrations have been identified; one involves the loss of DNA copy number in chromosome 12q, and another involves deletion in 6q23 and 13q21 (6). Others show gain in chromosome 19 and deletion of chromosome 19q. Another study showed similarities in genetic abnormalities between adenoid cystic carcinoma and polymorphous low grade carcinoma involving chromosomes 12 and 6. Adenoid cystic carcinoma with mutations in CTNNB1 (b-catenin gene) was reported. Mutations that cause hypermethylation and downregulation of 14-3-3ó, a target gene for p53 in the Gap2/mitosis (G2/M) cell cycle checkpoint, was found to be extensive in adenoid cystic carcinoma (ACC). Allelic loss of chromosomal arm 19q has been reported to occur commonly in adenoid cystic carcinoma.
B. Clinical Manifestation:Signs and symptoms depend largely on the site of origin of the tumor. Early lesions of the salivary glands present as painless, usually slow-growing masses of the mouth or face. Advanced tumors may present with pain and/or nerve paralysis, for this neoplasm has a propensity to invade peripheral nerves. Because there are many salivary glands under the mucosal lining of the mouth, throat, and sinuses, lumps in these locations could be from this type of tumor. Other symptoms may include difficulties in swallowing, hoarseness, dull pain,a bump or nodule in front of the ear or underneath the jaw, paralysis of a facial nerve, numbness of the face or tongue, a lump under the tongue or on the palate (roof of the mouth).
C. Gross MorphologyGrossly, adenoid cystic carcinomas are usually monolobular and nonencapsulated. They have a gray-pink color and infiltrate the surrounding normal tissue.
D. HistologyHistologically, ACC is made up of infiltrative small, dark, uniform and basaloid cells with or without mitosis depending on the type. Three types have been described: cribriform pattern, solid pattern and tubular. Combinations of the three types are sometimes encountered in one neoplasm. Cribriform pattern is the most common type and is arranged in clusters and nests of epithelial cells with holes (spaces); thus, it is also known as a “Swiss cheese” pattern. The neoplastic cells are small, basaloid and uniform with little to no mitosis and no pleomorphism. It is clinically low-grade, behaving with multiple recurrences and a slow tendency for metastasis. The high-grade counterpart is also known as the solid type, where cells are arranged in nests with larger basaloid cells, pleomorphism and prevalent mitosis. Spaces within these clusters are usually scant or absent. This is a more aggressive type with a tendency for early metastasis. The tubular type is difficult to interpret since some believe is similar to the cribriform pattern in behavior. All three types have a tendency for perineural invasion.
Adenoid cystic carcinoma is the prototypical cribriform tumor. It is blue, very cellular, with high nuclear to cytoplasmic ratios and fairly dense nuclei. Visually, it is reminiscent of a basal cell carcinoma of skin. It can be solid or tubular, but cribriform is the classic presentation, which makes it often instantly identifiable. Another classic feature is the balls of hyaline material found in the cribriform lumens, which are basement membrane material. It is highly infiltrative and loves nerves. Although intermediate grade at baseline, if solid growth predominates, this is a high-grade tumor.

Figure 14. Histopathological image of adenoid cystic carcinoma of the salivary gland. Hematoxylin & eosin stain. ix
Figure 15. Histopathological image of adenoid cystic carcinoma of the salivary gland. Immunostain for S-100 protein. x
Figure 16. Adenoid cystic carcinoma. Although the nuclei are small, the nuclear to cytoplasmicratio is high, making the tumor appear blue at low power. The architecture is classically cribriform, with
sharply punched-out spaces full of pink secretions.
E. Radiographic Finding xi
The axial T2-weighted MR image (Figure 12) shows a hyperintense mass lesion (arrows) in the subglottis and distal hypopharynx. The mass is seen to infiltrate the larynx (upper arrowhead), proximal trachea (lower arrowhead), distal hypopharynx (upper arrow) and proximal esophagus (lower arrow).

Figure 17. Axial T2-weighted MRI image.
Figure 18. On the sagittal gadolinium-enhanced T1-weighted image

Figure 19. Recurrent adenoid cystic carcinoma. The axial T2-weighted MR image (a) shows a tumoral mass posteriorly in the maxillary sinus (arrow) extending into the pterygopalatine fossa and paranasopharyngeal tissues (arrowhead).
Figure 20. Recurrent adenoid cystic carcinoma. The coronal gadolinium-enhanced T1-weighted MR images also show perineural tumour extension towards the cavernous sinus structures (double arrows; compare with opposite side).
F. Course & prognosis: The five-year relative survival rate for AdCC is approximately 89%. The 15-year relative survival rate for AdCC is approximately 40%. Tumor progression for AdCC is often slow and patients may live a long time with metastatic disease; however, a late relapse of AdCC is common, and can occur many years after initial treatment.Cancer survival statistics should be interpreted with caution. These estimates are based on data from thousands of cases of this type of cancer in the United States each year, but the actual risk for a particular individual may differ. It is not possible to tell a person how long he or she will live with AdCC. Because the survival statistics are measured in five-year (or sometimes one-year) intervals, they may not represent advances made in the treatment or diagnosis of this cancer.
High-grade tumors include adenoid cystic carcinoma. Low-grade tumors have 10-year survival rates of 80-95%, while 10-year survival rates for high-grade tumors range from 25-50%.For adenoid cystic carcinoma, the distant metastasis rate is nearly 50%. The most common sites are lung and bone. Although patients with metastases from adenoid cystic carcinoma may survive longer than 10 years because of the slow growth of these tumors, their survival with metastatic disease is short. The Dutch group observed the survival rate for patients with adenoid cystic carcinoma with distant metastases is 68% ± 7% in the first year and 32% ± 7% by 5 years. For patients with acinic cell carcinoma, the survival rate with distant metastases is 80% ± 13% at 1 year and 30% ± 14% at 5 years.

DIFFERENTIAL DIAGNOSIS: ACINIC CELL CARCINOMA
Acinic cell carcinoma is a neoplastic growth of epithelial cells with acinar differentiation. It is a rarely occurring malignancy of the salivary gland. It dated back to 1892 by Nasse, who first described the tumor. It belongs to the family of Adenocarcinomas and has some similarities with adenoid cystic, muco-epidermoid carcinoma, low-grade adenocarcinomas, and possibly some Breast Cancers.
Acinic Cell Carcinomas are a slow growing, low grade tumor. It was earlier classified as an “acinic cell tumor” or benign adenoma but later literatures noted of the tumor’s high potential for recurrence, metastases and even death, which resulted in WHO’s re-classification as a "malignant carcinoma", though with more common low-grade behavior.
95% of the tumors arise in the parotid gland however, some may also occur in the submandibular gland and other major and minor salivary glands. About 3% of acinic cell carcinoma showed bilateral occurrence.
A. Etiology and EpidemiologyAcinic cell carcinoma can appear in all age groups. Compared with other salivary gland tumors, it presents at a younger median age, which is 52 years old. Occurrence in children is quite common which is about less than 12%. This type of cancer has a 2:3 male to female ratio of occurrence. About 58.8% of the cancer happens to females than males. There were no studies that show acinic cell tumor has a racial predilection.
Acinic cell carcinoma comprises approximately 6%-10% of all salivary gland cancers and accounts for approximately 3-13% of all malignancies of the parotid gland. They make up approximately 4% of all minor, and 2-4% of all major salivary gland tumors.
B. PathogenesisThe risk factors that lead to acinic cell carcinoma include radiation exposure, industrial exposure, tobacco use, diet—mainly decrease in vegetable and increase in fat intake, and family history of a salivary gland tumor.
The RB pathway is responsible in gene and cell replication regulation. Studies show that acinic cell carcinoma exhibited substantial numbers of positive cells against Rb antibody that recognizes both unphosphorylated and phosphorylated Rb proteins. The numbers of positive cells for pRb-S795 and cyclin D1 significantly increased in ACCs as compared with normal salivary glands. A study concluded that the phosphorylation of serine 795 is critical for inactivation of Rb-mediated growth suppression and may play an important role in the pathogenesis of ACC.
C. Clinical ManifestationsPatients with acinar cell tumor may present with a swelling or mass in the face, neck, mouth that slowly enlarges over a long period of time usually years. It may or may not cause pain, thus usually asymptomatic. Less than one third of patients with acinic cell carcinoma reported the presence of pain with the mass or swelling. ACC does not normally invade the facial nerve; but when it does, numbness or weakness in the affected part of the face may be present.

D. Gross MorphologyOn gross examination, acinic carcinoma presents as a single, well circumscribed, nodular to multinodular, encapsulated tumor. It may be firm to cystic, usually 0.5- 13cm, lobular with a red to tan color in cut surface.
E. HistologyTumor cell in acinic cell carcinoma are usually dispersed in patterns, which could be in sheets, microcystic, acini, gland, duct, papillary cystic and follicles. The follicular type resemble that of a thyroid where in multiple cystic lumens are filled with eosinophilic proteinaceous material.
Papillary Follicular
As the name implies, acinic cell carcinoma is similar to the acinar serous cells in the secretory unit of the parotid gland. The acinar epithelium is largely polygonal, lightly basophilic cytoplasm (blue dot tumors) with protuberance of the luminal membrane producing a tombstone appearance. The nuclei is uniform to eccentric and cytoplasmic granules (PAS positive-diastase resistant, micicarmine positive)

Vacuolated cells is characterized by cells with clear vacuoles, eosinophilic to ampophilic cytoplasm, and PAS and mucicarmine negative.
The stroma is characterized by a delicate fibrovascular tissue, lymphoid infiltration (in some cases)and hemorrhage (especially in the papillocystic type). In addition to the mentioned characterstics anaplasia and few mitoses can be observed.
F. Ultrastructural FeaturesBased on ultrastructural imaging thur the electron microscope, the following features can be observed in acinar cell carcinoma.
Multiple round, membrane bound, electron dense cytoplasmic granules Lumina Apical junctional complexes Few microvilli Clear cells Dilated ER Lipid inclusions Intracytoplasmic pseudolumina Myoepithelial cells Microfilaments Dense bodies
G. Immunohistochemical Features Cytokeratin(present) CEA (present) alpha 1 antitrypsin (present) alpha 1 antichymotrypsin (present) Leu-M1 (present) Amylase (present)

Transferrin (present) Lactoferrin (present) Vasocactive intestinal polypeptide (present) S-100 (some) GFAP (some)
H. PrognosisFor parotid tumors, acinic cell carcinomas had the best prognosis with a 10-year relative survival of 88%. Poor prognosis is associated with the following factors:
Short duration of symptoms Incomplete excision Frequent mitoses Focal necrosis Neural invasion Pleomorphism Infiltration Stromal hyalinization Large size Involvement of the deep lobe of the parotid gland
Acinic cell carcinoma is quite persistent in their potential for local recurrences and distant metastases, often occurring many years later. Local and multiple recurrences may occur in 50% of the patients. Recurrence rate of the carcinoma is 35%. Tumour size (> 2.75 cm) was a significant predictor of recurrent deep parotid lobe involvement, the presence of cervical nodal disease and lymphocytic infiltration, although not significant, factors showed a tendency towards recurrence. For acinic cell carcinoma, the predominant solid architecture appears to be a strong predictor of recurrence. Recurrences and metastases after 3-10 years are common, especially after inadequate primary tumor removal. Death from disease has been reported in 16% to 26% of patients, depending on study location and period. Patients with lung metastases have a poorer prognosis. Overall however, acinic cell carcinoma has been identified as the least aggressive of the salivary gland cancers.
Survival rates vary for 5 years, 10 years, and 20-years are approximately 90%, 83%, and 67% respectively. Worse survival has been associated with high grade, metastatic disease and age over 30 years.
Though uncommon, high grade variants of acinic cell carcinoma are definitely aggressive, and are usually associated with much poorer survival.

DIFFERENTIAL DIAGNOSIS: MUCOEPIDERMOID CARCINOMA
Mucoepidermoid carcinoma is the most commonly occurring malignant neoplasm of the parotid gland and is the second-most common malignant neoplasm of the submandibular gland after adenoid cystic carcinoma. Mucoepidermoid tumor represent about 5 to 10% of all salivary gland tumors and occurs predominantly in the parotids. It represents about 8% of all parotid tumors. These neoplasms are composed of variable mixtures of squamous cells, mucus-secreting cells and intermediate hybrids. (1) Mucoepidermoid carcinomas were first described by Masson and Berger in 1924. Since then, they have become well recognized as a common salivary gland neoplasm, accounting for approximately 35% of all malignancies of the major and minor salivary glands in general. Mucoepidermoid carcinomas have been reported at distant and atypical sites, including the breast, Eustachian tube of the ear, bronchi of the lungs, and thyroid. Women are more commonly affected than men (3:2), and the mean age at onset is in the 5th decade of life. MEC is also the most common salivary gland malignancy in children.
A. Etiology and Epidemiology The etiology of mucoepidermoid carcinoma is not fully understood.
The bicellular stem cell theory theory holds that tumors arise from 1 of 2 undifferentiated stem cells, the excretory duct reserve cell or the intercalated duct reserve cell. Excretory stem cells give rise to squamous cell and mucoepidermoid carcinomas, while intercalated stem cells give rise to pleomorphic adenomas, oncocytomas, adenoid cystic carcinomas, adenocarcinomas, and acinic cell carcinomas.
B. Clinical ManifestationsThe tumor usually forms as a painless, fixed, slowly growing swelling of widely varying duration that sometimes goes through a phase of accelerated growth immediately before clinical presentation. Symptoms include tenderness, otorrhea, dysphagia, and trismus.
C. HistologyMECs may be circumscribed and variably capsulated or infiltrative and fixed; the latter characteristics generally apply to higher-grade tumors. Areas of scarfing are relatively common. Most tumors are smaller than 4 cm in diameter. Cysts of variable sizes are often present, and they usually contain brownish fluid. MEC cells form sheets, islands, duct-like structures, and cysts of various sizes. The cysts may be lined with intermediate, mucous, or epidermoid cells, and they are filled with mucus. Papillary processes may extend into the cyst lumina, and this is occasionally a conspicuous feature.
The tumor is primarily made up of three cell types in widely varying proportions: intermediate, mucous, and epidermoid. These cell types help in the grading of the tumors.
a. Intermediate cells or hybrid cell type often have squamous features in which small to large mucus-filled vacuoles are present. This cells usually predominates. Their appearance ranges from small basal cells with scanty basophilic cytoplasm to larger and more oval cells with more abundant pale eosinophilic cytoplasm that appears to merge into epidermoid or mucous cells.
b. Mucous cells (mucocytes) can occur singly or in clusters, and they have pale and sometimes foamy cytoplasm, a distinct cell boundary, and small, peripherally placed, compressed nuclei. Mucocytes often form the lining of cysts or duct-like structures. Occasionally mucocytes are so scanty that they can be identified with confidence only by using stains such as mucicarmine.
c. Epidermoid cells may be uncommon and focally distributed. They have abundant eosinophilic cytoplasm, but they rarely show keratin pearl formation or dyskeratosis. Oncocytic metaplasia is seen occasionally.

E. Classification and GradingMECs exhibit remarkable variability in their clinical behavior. Several microscopic grading systems based on anumerical score have been advocated as a means of predicting outcome. These systems rely on subjective evaluations of the relative proportions of the various cell types, the degree of cellular atypia, mitotic frequency, presence of necrosis, and invasive characteristics. It has been proposed that mucoepidermoid tumors arise from subepithelial mucus glands that line the upper respiratory and digestive tracts. If so, this might explain why this tumor type is more common at the supraglottis, which is the subsite of the larynx that has the greatest concentration of subepithelial mucous glands.
Mucoepidermoid carcinoma cell types are classified histologically as low, intermediate, and high-grade types. High-grade tumors are poorly differentiated, and they are made up primarily of squamous epithelial and intermediate cells. Low-grade tumors are well differentiated and are made up primarily of mucus-secreting and squamous epithelial cells. The histologic features of intermediate-grade tumors fall in between. On microscopic examination, low-grade tumors contain sheets of mucoid cells separated by bands of epidermoid cells. Mucous cells are clear and plump with small nuclei. Epidermoid components resemble squamous cell carcinoma. High-grade mucoepidermoid carcinomas are composed nearly entirely of nests of malignant epidermoid cells. Few mucous cells or none at all are present, although when specially stained, cells containing mucous are apparent. This differentiates high-grade mucoepidermoid carcinoma from squamous cell carcinoma. In simple terms, it means that the ratio of epidermoid cells rises in higher grades and in low grade tumor, there is higher preponderance of mucus cells.
Figure 21. The tumor within the parotid gland is mostly solid, mostly squamous, and it has infiltrating characteristics. This places it in a higher grade than one might classify the subcutaneous component. Mitotic activity is very minimal; there is no necrosis, and neurotropism was not demonstrated. Therefore it could be designated as an intermediate grade tumor.
Histologic tumor grade is a useful prognostic indicator for mucoepidermoid carcinomas of the major and minor salivary glands. The prognosis is dependent on the clinical stage, site, grading, and adequacy of surgery. The biologic behavior of mucoepidermoid carcinoma is dependent on the grade of tumor. Low-grade lesions are fairly nonaggressive, and appropriate treatment imparts a good prognosis. High-grade neoplasms are much more aggressive, with high rates of regional lymph node metastases. Pires et. al. reviewed the literature and reported that overall 5-year survival rates ranged from 0 to 43% for patients with high-grade mucoepidermoid cancers of the salivary glands, 62 to 92% for patients with intermediate-grade tumors, and 92 to 100% for patients with low-grade tumors.

DIFFERENTIAL DIAGNOSIS: MALIGNANT MIXED CARCINOMA
Malignant mixed tumor of the salivary glands is a rare neoplasm, and the majority of these tumors arise from the parotid gland. Malignant mixed tumors represent approximately 11.6% of all malignant neoplasms of the salivary gland and mostly originate from major salivary glands. Histopathologically, there are three (3) distinct variants of malignant mixed tumors recognized.
The first type is the carcinoma ex-pleomorphic adenoma (CXPA), which is the most common of the three subtypes. It occurs when a carcinoma develops from the epithelial component of a pre-existing pleomorphic adenoma. This complication takes place in about 5% to 10% of these neoplasms. Carcinoma ex-pleomorphic adenoma presents in the 6th to 8th decases of life with patients averaging 10 years older than those with pleomorphic adenomas. It occurs most often in the parotid, followed by the submandibular gland and palate. Clinical features that suggest this event is usually long-standing painless masses that rapidly enlarge over a 3 to 6 month period. They often become painful and fixed to the skin. Facial paralysis is also variably present. A history of previous surgery and/or radiation therapy is often obtained. Documentation that a malignant salivary gland tumor arose from a pre-existent benign mixed tumor may be difficult to obtain. The above history although suggestive of the process, is not by itself diagnostic. It is necessary to have microscopic evidence of a previously existing benign tumor or to have benign and malignant tumor in the same neoplasm. This may require a thorough sampling of the tumor. Sometimes the preexisting benign lesion is represented only by a totally hyalinized round nodule surrounded by carcinoma. The malignancy is limited to the epithelial component. The risk of malignant degeneration in a pleomorphic adenoma increases from about 1.5% in the first five years to 9.5% for adenomas present longer than 15 years.
Figure 22. Carcinoma ex-pleomorphic adenoma. (a)Gross finding (b) Histologic finding. xii
Gross pathology of carcinoma ex-pleomorphic adenoma often shows a poorly circumscribed, infiltrative, hard mass. Gross tumors appear firm, unencapsulated, and nodular with areas of central necrosis and hemorrhage (Figure 22a). Microscopically, the diagnosis is based on a malignant process that infiltrates a neoplasm, which has the histologic features of a pleomorphic adenoma (Figure 22b). The malignant portion of the tumor can take the form of any epithelial malignancy except acinic cell. Most commonly this will be in the form of an undifferentiated carcinoma (30%) or adenocarcinoma (25%). This tumor tends to be more aggressive than other salivary
a b

malignancies and about 25% of patients will have lymph node metastasis on presentation. Regrettably, these cancers when they appear, are among the most aggressive of all salivary gland malignant neoplasms, accounting for 30% to 50% mortality in 5 years.
The treatment of choice for carcinoma in pleomorphic adenoma has consisted of en-bloc excision with wide margin, often in conjunction with neck dissection, and postoperative radiation therapy but recurrence is common. Prognosis appears to be related to local extent of disease and the histologic type of the carcinoma component.
The second type is the true malignant mixed tumor or carcinosarcoma, an extremely rare tumor, which has a biphasic composition similar to that of benign mixed tumor, but both the epithelial and the mesenchyme-like elements have a malignant appearance, the former often in the form of ductal carcinoma, and the latter in the form of chondrosarcoma. Carcinosarcoma accounts for only .05% of salivary gland neoplasms. Average age at presentation is about 60 years and men and women appear to be equally affected. The parotid is the most frequent site of occurrence. Swelling, pain, nerve palsy, and ulceration have been frequent clinical findings.
Figure 23. Carcinosarcoma. (a)Gross finding (b) Histologic finding xiii
Gross pathology of carcinosarcoma often shows a poorly circumscribed, infiltrative, cystic areas (Figure 23a). Microscopically, carcinosarcoma have both sarcomatous and carcinomatous elements (Figure 23b). In the majority, the sarcoma is the dominating component and chondrosarcoma is the most common cell type. The carcinoma element is usually an undifferentiated or high-grade ductal adenocarcinoma. This is also an aggressive tumor and it is not uncommon for patients to have distant metastasis on presentation.
Analogous to benign mixed tumor, carcinosarcomas are composed of both epithelial and mesenchymal appearing neoplastic tissues. Cytologic atypia, including cellular and nuclear pleomorphism, hyperchromatism, mitotic figures and invasive growth distinguish carcinosarcomas from benign mixed tumor.
Currently recommended treatment includes radical surgery, neck dissection for palpable nodes and postoperative XRT. Although efficacy has yet to be proven, chemotherapy is likely to have a role in the treatment of this disease given the high rate of distant metastasis.
a b

And, the third subtype is the metastasizing benign mixed tumor, which has benign-appearing epithelial and stromal components that develops metastatic deposits of tumor. If the cytologically malignant foci are found entirely within a benign mixed tumor (i.e., in the form of carcinoma in situ), they are not associated with clinical malignancy. Only when invasion occurs beyond the capsule of the original neoplasm will the lesion behave clinically in a malignant fashion. For invasive tumors, the extent of invasion beyond the capsule is of importance. The most common sites of metastases are regional lymph nodes, lungs, bone (especially the vertebral column), and abdominal organs.
Invasive carcinomas and carcinomas of high grade malignancy carried worse prognoses. Invasive growth, facial nerve involvement, lymph node metastasis or high-grade malignant tumors are grounds for postoperative radiation therapy. The role of chemotherapy has not yet been well established.

DIFFERENTIAL DIAGNOSIS: LYMPHADENOPATHY
Lymphadenopathy is a disease of the lymph nodes presenting as swelling and enlargement. When the infection is of the lymph nodes themselves, it is called lymphadenitis, but when the infection is of the lymph channels, it is called lymphangitis.
Enlarged lymph nodes are a common symptom in a number of infectious and cancerous diseases. It is a recognized symptom of many diseases, which include:
• Reactive: acute infection (bacterial or viral) or chronic infections (tuberculous lymphadenitis) o Infectious mononucleosis is an acute viral infection, the hallmark of which is marked enlargement of the
cervical lymph nodes. o It is also a symptom of cutaneous anthrax, measles and Human African trypanosomiasis, the latter two
giving lymphadenopathy in lymph nodes in the neck
• Tumoral: o Primary: Hodgkin lymphoma, non-Hodgkin lymphoma, hairy cell leukemia, give lymphadenopathy in all
or a few lymph nodeso Secondary: metastasis, Virchow's Node, Neuroblastoma
• Autoimmune etiology: sarcoidosis, systemic lupus erythematosus, rheumatoid arthritis all giving a generalized lymphadenopathy
• Immunocompromised etiology: AIDS. Generalized lymphadenopathy is an early sign of infection with human immunodeficiency virus (HIV), the virus that causes acquired immunodeficiency syndrome (AIDS). "Lymphadenopathy syndrome" has been used to describe the first symptomatic stage of HIV progression, preceding AIDS-related complex and full-blown AIDS.

DIFFERENTIAL DIAGNOSIS: LYMPHOMA
Lymphoma is a type of cancer involving lymphocytes, the cells of the immune system. It is a group of cancers that affect the cells that play a role in the immune system, and primarily represents cells involved in the lymphatic system of the body. It is a malignant transformation of either lymphocytes B or T cells or their subtypes.
Lymphomas fall into 1 of 2 major categories. Hodgkin lymphoma (HL, previously called Hodgkin's disease) and all other lymphomas (non-Hodgkin lymphomas or NHLs). Hodgkin lymphoma develops from a specific abnormal B lymphocyte lineage. NHL may derive from either abnormal B or T cells and are distinguished by unique genetic markers.
A. Risk FactorsAge: Generally the risk of NHL increases with advancing age. HL in the elderly is associated with a poorer prognosis than that observed in younger patients.
Infections: HIV, human T-lymphocytic virus type 1 (HTLV-1), Epstein-Barr virus (EBV), one of the etiologic factors in mononucleosis, Helicobacter pylori, a bacterium that lives in the digestive tract, hepatitis B or hepatitis C virus
Medical conditions that compromise the immune system: HIV, Autoimmune disease, Diseases requiring immune suppressive therapy, often used following organ transplant, Inherited immunodeficiency diseases (severe combined immunodeficiency, ataxia telangiectasia)
Genetics: Family history of lymphoma
B. EpidemiologyLymphoma is the most common type of blood cancer in the United States. It is the sixth most common cancer in adults and the third most common in children. Non-Hodgkin lymphoma is far more common than Hodgkin disease. It can occur at any age, including childhood. Hodgkin disease is most common in 2 age groups: young adults aged 16-34 years and in older people aged 55 years and older. Non-Hodgkin lymphoma is more likely to occur in older people. There is no sex predilection (M:F ratio of 1:1)
C. Clinical ManifestationsOften, the first sign of lymphoma is a painless swelling in the neck, under an arm, or in the groin. Lymph nodes or tissues elsewhere in the body may also swell. The enlarged lymph node sometimes causes other symptoms by pressing against a vein or lymphatic vessel (swelling of an arm or leg), a nerve (pain, numbness, or tingling), or the stomach (early feeling of fullness). The following are non-specific signs and symptoms: fevers, chills, unexplained weight loss, night sweats, lack of energy, and itching
D. Gross PathologyAffected lymph nodes (most often, laterocervical lymph nodes) are enlarged, but their shape is preserved because the capsule is not invaded. Usually, the cut surface is white-grey and uniform; in some histological subtypes (e.g. nodular sclerosis) a nodular aspect may appear.

E. HistologyHodgkin’s Lymphoma
Figure 24. Histology of Hodgkin Lymphoma
Microscopic examination of the lymph node biopsy reveals complete or partial effacement of the lymph node architecture by scattered large malignant cells known as Reed-Sternberg cells (typical and variants) admixed within a reactive cell infiltrate composed of variable proportions of lymphocytes, histiocytes, eosinophils, and plasma cells. The Reed-Sternberg cells are identified as large often bi-nucleated cells with prominent nucleoli and an unusual CD45-, CD30+, CD15+/- immunophenotype. In approximately 50% of cases, the Reed-Sternberg cells are infected by the Epstein-Barr virus.
Characteristics of classic Reed-Sternberg cells include large size (20–50 micrometres), abundant, amphophilic, finely granular/homogeneous cytoplasm; two mirror-image nuclei (owl eyes) each with an eosinophilic nucleolus and a thick nuclear membrane (chromatin is distributed at the cell periphery).
Non-Hodgkin Lymphoma
Figure 25. Histology of Non-hodgkin’s Lymphoma
Microscopic examination reveals effacement of the lymph node and replacement by uniform sheets of neoplastic lymphocytes. Reed-Sternberg cells are not present.
F. TreatmentStandard first-line therapy (primary therapy) for lymphoma includes radiation therapy for most early-stage lymphomas, or a combination of chemotherapy and radiation. For later-stage lymphomas, chemotherapy is primarily used, with radiation therapy added for control of bulky disease. Biological therapy, or immunotherapy, is increasingly being used in addition to or as an alternative to these standard therapies.
G. PrognosisThe outlook for HL is very good. It is one of the most curable cancers. The 5-year survival rate after treatment is greater than 80% for adults and greater than 90% for children. As a result of refinements in and more aggressive approaches to therapy, the outlook for NHL has improved significantly in the last few decades. The 5-year survival rate after treatment is 55% for adults and about 80% for children. The addition of immunotherapy to standard treatment for NHLs may further improve survival rates.

SUMMARY
Table 1. Benign neoplasms.
Case Pleomorphic Adenoma Warthin’s TumorMonomorphic
AdenomaOncocytoma
Peak Age of Incidence
48 y/o 4th decade 6th-7th decade 6th - 7th decade > 50 y/o
Sex Predilection Female Females Men Female Equal
Size 3x3 cm 2-5 cmSmaller than pleomorphic
adenoma< 4 cm
Tenderness/Pain Non-tender Painless PainlessConsistency Soft Soft Cystic Firm Firm
Mobility Mobile Mobile Fixed
Margin Well circumscribed SmoothWell-
circumscribed
Shape Round to ovalFirm; well-
encapsulated; smooth
Capsule Yes Yes Yes
Cut Ssurface
rubbery, resilient mass, with a bosselated surface and may grow to a large
size
Pale gray surface punctuated by
narrow cystic or cleft-like spaces
filled with mucinous secretion
Tan color
Histology
With Hyaline or myxoid matrix
and benign epithelial nests;
admixture of polygonal epithelial and spindle-shaped myoepithelial elements in a variable
background stroma that may be mucoid, myxoid, cartilaginous or hyaline;
cartilaginous differentiation are usually
found
epithelial cells forming papillary projections into
cystic spaces in a background of a lymphoid stroma
palisadesOncocytes;
Absent Mitotic figures
Radiographic findings
poorly enhancing mass involving
the left submandibular
gland
CT:rounded tumor
at the right parotid gland
MRI:hyperintense mass lesion
surrounded by a hypointense
capsule
Rate of growth Slow Slow Slow Slow
Other S/SxTinnitus, hearing
loss, earache

SUMMARY
Table 2. Malignant Neoplasms.
Case Adenocarcinoma Adenoid Cystic Adenoma
Acinic Cell Carcinoma Mucoepidermoid Carcinoma
CXPA Carcinosarcoma Lymphoma
Peak Age of Incidence (Mean)
48 y/o 58 y/o 40-60s 44-52 y/o 5th decade 6th -8th decade 6th decade 16-34 y/o; ≥55 y/o
Sex Predilection Female Equal Females Females Female Equal Equal Equal Size 3x3 cm 0.5 – 13 cm < 4 cm
Tenderness/Pain Non-tender Painful Painless painful May or may not cause pain
Painless Painless painful
Painless
Consistency Soft Firm Solid Firm to cystic Cystic Firm to hard CysticMobility Mobile Fixed Fixed
Margin Irregular Well-circumscribed can be circumscribed or infiltrative
Poorly circumscribed
Poorly circumscribed
ShapeCapsule No No No Variably capsulated No
Cut SsurfaceGray-pink and infiltrate the surrounding tissue
lobular with a red to tan color in cut
surfaceWhite-gray
Histology
With Hyaline or myxoid matrix and
benign epithelial nests; with
cartilaginous differentiation
Neoplastic cells form cords, sheets, nests and islands. Clear
cells and oncocytic cells may be present
Cribriform (sieve-like) appearance;
Tumors cells are arranged in clumps &
cords separated by fibrous stroma w/c may exhibit a marked degree
of hyalinization
similar to the acinar serous cells; blue dot tumors; tombstone
appearance; nuclei is uniform to eccentric
and cytoplasmic granules; with clear
vacuoles
cells form sheets, islands, duct-like
structures, and cysts of various sizes; made up
of intermediate, mucous, and
epidermoid cell types
Malignant cellular change adjacent
to typical pleomorphic
adenomaCarcinomatous
component
biphasic appearancesarcomatous component
carinomatous component
Reed-Sternberg cells for
Hodgkin’s
Radiographic findings
poorly enhancing mass involving the left submandibular
gland
MRI: hyoerintense lesion in the subglottis and distal hypopharynx.
Rate of growth Slow Slow Slow Slow Fast (3-6 months)
Other S/SxTinnitus, hearing
loss, earache Facial weakness
difficulties in swallowing, hoarseness, dull pain, a bump or nodule in front of the ear or underneath
the jaw, paralysis of a facial nerve, numbness of the face or tongue, a lump under the tongue
or on the palate
Weakness and numbness
invasion of the facial nerve
Otorrhea; dysphagia
facial paralysis is also variably
present
Swelling, pain, nerve palsy, and ulceration have been frequent
clinical findings.
fevers, chills, unexplained weight loss,
night sweats, lack of energy,
and itching

SUMMARY
Tumors of the salivary glands are not seen often. The most frequently encountered condition is pleomorphic adenoma. The initial presenting signs are also similar for the tumors, which is most of the time a mass at around the angle of the jaw or anywhere in the area between the ear and the jaw, so diagnosing these tumors based on clinical grounds alone is not sufficient. The use of histological and imaging techniques such as MRI and CT scans has to done in order to come up with a definitive diagnosis.
In the case, the patient is 48-year-old female who presented with a mass at the angle of the jaw. The mass was nontender, mobile and does not seem to be fixed to the underlying tissue. No other signs and symptoms were found. From these features alone, we made the assumption that the mass is a benign lesion since the mass has all the characteristics attributed to a benign lesion. Also, facial nerve paralysis, which is a sign of malignancy for salivary gland tumors, was not evident which aided in ruling out a malignant etiology. However, just because facial nerve paralysis and tenderness are absent does not immediately rule out malignancy. Malignant lesions are characterized by painless lesions. The non-tender mass that the patient exhibited is one of the reason for including malignant lesions in the differentials. Facial nerve paralysis is a late manifestation of malignant salivary gland tumors so it could be that the patient has a benign lesion now, but it can still progress to a more malignant one. Also, a malignant tumor can start as a painless lesion and later on becomes painful as the tumor becomes more advanced. However, because the mass of the patient is mobile, malignancy can be ruled out as most of the malignant neoplasms of the salivary glands ifnfiltrates and fix to tissues.
All of the malignant tumors considered as differential diagnoses are slow growing entities, taking years to be fully recognized. Their slow growth and predilection for the female sex are two things that were considered for ruling them in as possible causes of the patient’s condition. Acinic cell carcinoma is also ruled out because the cells in the case do not have distinct borders, unlike the polygonal shaped of the cells of acinic cell carcinoma. Adenoid cystic adenoma is also ruled out because the clinical symptoms of difficulties in swallowing, hoarseness, dull pain, a bump or nodule in front of the ear or underneath the jaw, paralysis of a facial nerve, numbness of the face or tongue, a lump under the tongue or on the palate are not seen in the patient. Basal cell carcinoma, which is a variant of monomorphic adenoma, does not contain the mesenchyme-like component of a benign mixed tumor.
Histologically speaking, the tumor had thyroid and cartilage elements present. Warthin’s has a low probability of being the cause of the patient’s signs and symptoms because it is characterized by the predominance of lymphoid elements which may have germinal centers. Also, Warthin’s tumor has a greater predilection for men than women. Oncocytoma is ruled out because of its later age of onset and because of its firm consistency because the patient’s lesion is soft.
Although lymphoma also causes painless masses on the neck, the associated signs and symptoms that accompany it such as weight loss, fever, chills, and night sweats is not seen. Also, the histological findings of the patient did not exhibit the characteristic Reed-Sternberg cells which are pathognomonic of lymphomas, particularly, Hodgkin’s lymphoma.
Among the tumors considered as a differential diagnosis, pleomorphic adenoma has the greatest possibility of being the cause of the patient’s condition. The histological findings of the patient’s tumor showed a hyaline or myxoid matrix with epithelial cells. Pleomorphic adenomas have a stroma which may have non-specific fibromyxoid appearance, sometimes containing abundant elastic tissue, however, areas of clearcut cartilaginous differentiation are usually found The patient also satisfied the manifestations of a pleomorphic adenoma.
The tinnitus, earache, and hearing problem could be a side effect of the antibiotics the patient took, particularly of streptomycin. Streptomycin is an aminoglycoside, an antibiotic whose adverse reactions are nephrotoxicity and ototoxicity. The three symptoms can also be caused by Warthin’s but as previously mentioned, the histologic features of Warthin’s tumor is not encountered in the case.

MANAGEMENT: DIAGNOSTICS
Pleomorphic adenomas most commonly occur in the parotid gland (about 85%). This tumor may also be encountered in the submandibular, lingual, and minor salivary glands.
The parotid gland is divided into a larger superficial lobe and smaller deep lobe by the facial nerve, which enters the posterior parotid, branches and then exits the gland anteriorly. Adjacent to but slightly deeper to the facial nerve is the retromandibular vein, followed by the external carotid artery, both of which have a number of branches within the gland. The retromandibular vein, which drains into the external jugular vein, roughly parallels the course of the facial nerve. Therefore, this vein can be used as guide to determine the location of the nerve on imaging studies.
Histologically, the gland is composed primarily of acinar cells, and upon stimulation, they produce a watery, serous solution, which is excreted by the parotid (Stensen) duct. This duct exits the anteromedial portion of the gland, crosses the masseter superficially, pierces the buccinator, and enters the oral cavity opposite the second maxillary molar. In addition to parotid tissue, parotid glands typically have lymph nodes that may or may not be visible on imaging (Figure 3). False positive or negative results may occur as many parotid tumors and lymph nodes can have a similar appearance.
CT or MRI depicts the mass, and the findings may be essentially diagnostic in routine cases with typical features. Some authors have reported excellent sensitivity with ultrasonography, though this study typically does not help the surgeon to understand the 3-dimensional (3D) relationship of the tumor to the parotid gland and the facial nerve.
A. Computed Tomography (CT) ScanOn CT Scan, pleiomorphic adenomas appear as typically smooth (Figure 1), well-marginated tumors, though nodularity along the outer surface is sometimes present (Figure 2). Fine needle aspiration confirms the diagnosis. The attenuation values (loss of energy of a beam of radiant energy due to absorption, scattering, beam divergence, and other causes as the beam propagates through a medium) of the mass are usually homogeneous and higher than that of the surrounding gland, though lower attenuation masses that resemble cysts are occasionally seen. Tumor enhancement is variable and can result in a missed diagnosis if delayed images are not acquired. Pleomorphic adenomas are poorly enhancing in the early phase of contrast enhancement, though the amount of enhancement increases over time. Delayed images obtained at 5-10 minutes are often useful.
When pleomorphic adenomas become large, they may develop a heterogeneous appearance with areas of necrosis, hemorrhage, cysts, and calcification. Large tumors commonly have a lobulated contour, which strongly suggests the diagnosis.
Figure 26. Axial contrast-enhanced CT scan that demonstrates a poorly enhancing, smoothly marginated mass involving the left submandibular gland.

Figure 27. Enhanced CT image that shows a lobular mass in the left parotid gland. The circumscribed borders, poor enhancement, and location are all highly suggestive of pleomorphic adenoma
Limitations of CT ScanCT is often the first study ordered in patients with neck masses, and scans can show the mass and the retromandibular vein. Newer multisection CT scanners offer multiplanar capabilities rivaling that of MRI. Although certain CT features (eg, lobulation, homogeneity, delayed contrast enhancement) can suggest the diagnosis of pleomorphic adenoma, these findings are not specific to the tumor. In addition, CT results may falsely suggest invasion of the surrounding tissue; in these cases, MRI should be performed to ensure that a diagnosis of malignancy is not incorrectly made. MRIs can demonstrate a well-defined capsule, even when the border appears irregular on CT scans.
Disadvantages of CT include radiation exposure, the use of iodinated contrast material, and tissue distinction poorer than that of other studies. CT may also be problematic in cases of benign pleomorphic adenomas when the outer margin of the tumor appears indistinct and suggests malignant invasion of the surrounding tissue. MRIs show the well-defined outer borders in these instances. In many cases, however, CT may be the only study needed to guide the surgeon.
B. Magnetic Resonance Imaging (MRI)Pleomorphic adenomas are usually well-circumscribed, homogeneous masses with low intensity on T1-weighted images and high intensity on T2-weighted images. They commonly have a rim of decreased signal intensity on T2-weighted images; this rim also appears hypointense on fat-suppressed T1-weighted images. This finding represents the surrounding fibrous capsule.
Figure 28. Coronal fat-saturated T2-weighted MRI demonstrates a hyperintense mass involving the deep lobe of the left parotid gland (arrow). The tumor has higher signal intensity than that of the visualized lymph nodes (arrowheads). This finding can help in distinguishing pleomorphic adenomas from intraparotid lymph nodes.
A well-defined parotid mass with increased signal intensity on proton density- and T2-weighted images is highly suggestive of the diagnosis. In fact, the increased signal intensity on T2-weighted images is so prevalent that any parotid mass with this finding should be viewed with suspicion, as this often indicates a carcinoma esp. pleomorphic adenoma.

When it becomes large, the tumor may lose its homogeneous appearance on MRI, as with CT. It may have areas of fibrosis, necrosis, and hemorrhage. Inhomogeneous signal intensity should be apparent in these cases. Lobulation is commonly visualized and is, in itself, also suggestive of the diagnosis.After gadolinium enhancement, the tumors are homogeneously enhancing unless they are large. Unlike CT, MRI has no role in delayed imaging.
Gadolinium-based contrast agents (gadopentetate dimeglumine [Magnevist], gadobenate dimeglumine [MultiHance], gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol [ProHance]) have recently been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans.
Limitations of MRIMRI has the advantages of multiplanar imaging, and MRI results may suggest the tissue type on the basis of signal intensity characteristics. The diagnosis of pleomorphic adenoma can be at least strongly suggested in most cases. Special attention should be paid to the signal intensity of the tumor and to any possible invasion into adjacent soft tissues.
C. UltrasoundOn sonograms, pleomorphic adenomas typically appear as smooth, round, hypoechoic masses with distal acoustical enhancement. Lobulations are commonly visualized. Large tumors appear more heterogeneous than small ones and are better imaged with CT or MRI than with sonography.
Figure 29. Longitudinal section through the left parotid gland demonstrates a typical pleomorphic adenoma (callipers) which is homogeneous, hypoechoic and well circumscribed with distal acoustic enhancement. This can be seen to lie superficial to the retro-mandibular vein (arrow) and hence in the superficial lobe.

Figure 29. Longitudinal section through the left parotid gland demonstrates a lobulated mass in the superficial lobe of the gland distorting the capsule. There is associated distal acoustic enhancement. Note marked heterogeneity of internal architecture. Biopsy confirmed this lesion to represent a pleomorphic adenoma. The mandible is indicated by arrowheads.
Limitation of UltrasoundAlthough sonographic findings can suggest the diagnosis of pleomorphic adenoma in many small tumors, CT or MRI is needed to fully evaluate large tumors. Even in patients in whom the diagnosis is made by means of sonography and biopsy, CT or MRI is needed for preoperative planning.
D. Nuclear MedicineEvidence suggests that dual-isotope imaging with technetium Tc 99m and thallium Tl 201 single-photon emission CT (SPECT) is accurate in distinguishing various tumors of the salivary glands, including pleomorphic adenomas.
E. SialographySialography (radiographic demonstration of the salivary ducts by means of the injection of substances opaque to x-rays) has been used in the past to diagnose parotid tumors, but it has been abandoned with the advent of CT and MRI. Pleomorphic adenomas appear as smoothly marginated masses that displace the parotid tissue and ducts.

MANAGEMENT: TREATMENT
Induction chemotherapy is normally done before patient undergoes surgery. Cisplatin and 5-flourouracil is taken by the patient for 3 cycles before the operation. This is to lessen the size of the tumor and make surgery less complicated. In the presence of recurrent malignancies however, concomitant chemoradiotherapy is indicated. Radiation along with chemotherapeutic agents are used to prevent recurrences post operatively.
Primary treatment of salivary malignancies is surgical excision. In this setting, basic surgical principles include en bloc removal of the involved gland with preservation of all nerves unless invaded directly by the tumor. For parotid tumors that arise in the lateral lobe, superficial parotidectomy with preservation of CN VII is indicated. If the tumor extends into the deep lobe of the parotid, a total parotidectomy with nerve preservation is performed. Although malignant tumors may abut the facial nerve, if a plane of dissection can be developed without leaving gross tumor, it is preferable to preserve the nerve. If the nerve is encased by tumor and preservation would mean leaving gross residual disease, the nerve is sacrificed. Sacrifice of the facial nerve and temporal bone resection is a component of the surgical removal of advanced tumors with direct extension into the facial nerve and temporal bone. Radiation therapy is used as adjuvant treatment in the post operative setting for specific indications.
The removal of submandibular malignancies include en bloc resection of the gland and submental and submandibular lymph nodes. Radical resection is indicated with tumors that invade the mandible, tongue and floor of the mouth. Therapeutic removal of the regional lymphatics is indicated for clinical adenopathy or when the risk of regional metastasis exceeds 20% based on tumor characteristics. High grade mucoepidermoid carcinomas have high risk of regional disease and require neck dissection. When gross nerve invasion is found, sacrifice of the nerve and retrograde frozen section biopsy are indicated to determine the extent of invasion.
Post operative radiation treatment plays an important role in the treatment of salivary malignancies. The presence of extraglandular disease, perineural invasion, direct invasion of regional structures, regional metastasis and high grade histology are all indications for radiation treatment.

REFERENCES
vi Okamura T, Kawabe J, Koyama K, et al. Fluorine-18 fluorodeoxyglucose positron emission tomography imaging of parotid mass lesions. Acta Otolaryngol Suppl 1998; 538:209–213.
vii Keyes JW Jr, Harkness BA, Greven KM, Williams DW 3rd, Watson NE Jr, McGuirt WF. Salivary gland tumors: pretherapy evaluation with PET. Radiology 1994; 192:99–102.
viii Eisele, DW, Johns, ME. Salivary Gland Neoplasms. In, Head & Neck Surgery-Otolaryngology, Ed, BJ Bailey. Philadelphia, Lippincott Williams & Wilkins; 2001: 1279-1297.
ix http://en.wikipedia.org/wiki/Adenoid_cystic_carcinoma
x http://en.wikipedia.org/wiki/Adenoid_cystic_carcinoma
xi MRI images from http://www.medcyclopaedia.com/library/topics/volume_vi_2/a/adenoid_cystic_carcinoma/
xii Source: http://www.utmb.edu/otoref/grnds/Salivary-020626/Salivary-020626-slides.pdf
xiii Source: http://www.utmb.edu/otoref/grnds/Salivary-020626/Salivary-020626-slides.pdf
Wagner, M.D., AL. “Parotid, Pleiomorphic Adenoma”. eMedicine Specialties. Last Updated: 18 April 2007. Date Accessed: 25 July 2008. (http://www.emedicine.com/radio/topic531.htm)
Howlett, M.R.C.P., F.R.C.R., DC. “High resolution ultrasound assessment of the parotid gland”. British Journal of Radiology (2003) 76, 271-277. http://bjr.birjournals.org/cgi/content/full/76/904/271
Ackerman’s Surgical Pathology
Feng Xu, Jin Wang, Zhong-guo Pang: Pleomorphic Adenoma of the Middle Ear. The Internet Journal of Otorhinolaryngology. 2005. Volume 4 Number 1. Accessed: http://www.ispub.com/ostia/index.php?xmlFilePath=journals/ijorl/vol4n1/ear.xml
http://en.wikipedia.org/wiki/Oncocytoma
http://www.thedoctorsdoctor.com/diseases/salivary_gland_oncocytoma.htm
http://www.thedoctorsdoctor.com/diseases/myoepithelioma.htm
http://www.ispub.com/ostia/index.php?xmlPrinter=true&xmlFilePath=journals/ijorl/vol3n1/spindle.xml
http://www.bioscience.org/lecture/tabibza.htm

http://www.medcyclopaedia.com/library/topics/volume_vi_2/a/adenoid_cystic_carcinoma/
http://www.emedicine.com/ent/TOPIC679.HTM
www.oralcancerfoundation.org/facts/rare/ac/index.htm
http://www.ghorayeb.com/ParotidAcinicCellCarcinoma.html
http://icarus.med.utoronto.ca/carr/manual/acinic.html
www.aciniccell.org
http://www.bioscience.org/lecture/tabibza/list.htm
http://www.thedoctorsdoctor.com/diseases/aciniccell_ca.htm#epidemiology
http://www.emedicine.com (Date Accessed: 27 Jul 2008)
http://www.utmb.edu/otoref/grnds/Salivary-020626/Salivary-020626.htm (Date Accessed: 27 Jul 2008)
http://www.thedoctorsdoctor.com/diseases/salivary_gland_adenocarcinoma.htm (Date Accessed: 27 Jul 2008)
http://www.oncologychannel.com/headneck/salivaryglands.shtml (Date Accessed: 27 Jul 2008)
http://en.wikipedia.org/wiki/Pleomorphic_adenoma
http://www.emedicine.com/radio/topic531.htm
http://www.emedicine.com (Date Accessed: 27 Jul 2008)
http://en.wikipedia.org (Date Accessed: 27 Jul 2008)