Resources - WKC Anatomy and Physiology - Home A&P...
Transcript of Resources - WKC Anatomy and Physiology - Home A&P...

Human Anatomy and Physiology I
Module 6: The Skeletal System: Muscle TissueLecture Outline
Resources1. Tortora, Principals of Anatomy and Physiology
Chapter 10. Muscular Tissue2. Allen, Laboratory Manual for Anatomy and Physiology
Exercise 12. Skeletal Muscle Structure
Overview of Muscular Tissue
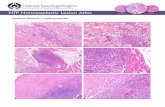
Types of Muscular TissueMuscle tissue is made up of many muscle cells and is well-vascularized. Muscles cells (also called muscle fibers) contain myofilaments that bring about movement or contraction in all cell types.
There are three kinds of muscle tissue: skeletal, cardiac, and smooth. Fill in the tables below using your lab manual – think about the similarities and differences between the three muscle tissues.
Skeletal Muscle Tissue – skeletal, striated, and voluntaryDescription
Function
Location
Red River College Jason J. Taylor MSc. 1

Human Anatomy and Physiology I
Cardiac Muscle Tissue – cardiac, striated, and involuntaryDescription
Function
Location:
Smooth Muscle Tissue – visceral, nonstriated, and involuntaryDescription
Function
Location:
Functions of Muscular TissueMuscle performs at least four important functions for the body
1. Producing movement – relies on the integrated functioning of muscle, bones, and joints
2. Maintaining posture and body position –
3. Stabilizing joints –
4. Generating heat –
Red River College Jason J. Taylor MSc. 2

Human Anatomy and Physiology I
Properties of Muscular TissueFour characteristics enable muscle tissue to perform its duties. 1. Excitability – the ability to respond to certain stimuli by producing
electrical signals (action potentials)
2. Contractility –
3. Extensibility –
4. Elasticity –
Skeletal Muscle AnatomyEach skeletal muscle is a discrete organ, made up of several kinds of tissues. Skeletal muscle fibers predominate, but blood vessels, nerve fibers, and substantial amounts of connective tissue are also present.
Nerve and Blood Supply In general, each muscle is served by one nerve, an artery, and by one or more veins. These structures all enter or exit near the central part of the muscle and branch profusely through its connective tissue sheaths (described below).
Muscle has a rich nerve supply. In fact each muscle fiber is innervated by its own nerve ending that controls its activity. This arrangement allows for precise neural control of the entire muscle during contraction.
Muscle has a rich blood supply because contracting muscle fibers use huge amounts of energy and require more or less continuous delivery of oxygen and nutrients via the arteries. Muscle capillaries are long and winding, features that accommodate changes in muscle length. They straighten when the muscle is stretched and contort when the muscle contracts.
Connective Tissue SheathsIn a muscle, individual muscle fibers are wrapped and held together by several different connective tissue sheaths. Together, they support each cell
Red River College Jason J. Taylor MSc. 3

Human Anatomy and Physiology I
and reinforce the muscle as a whole. From external to internal, the connective tissue sheaths are epimysium, perimysium, and endomysium.
Label this diagram:
AttachmentsMost skeletal muscles span joints and are attached to bones (or other structures) in at least two places. When a muscle contracts, the moveable bone, the insertion, moves towards the immoveable or less moveable bone, the origin. In the limb muscles, the origin typically lies proximal to the insertion.
Muscle attachments (origin or insertion) may be direct or indirect. In direct attachments, the muscle’s epimysium is fused to the bone’s periosteum. In indirect attachments, the muscle’s connective tissue sheaths are attached to the bone either as a ropelike tendon or as a sheetlike aponeurosis.
Skeletal Muscle Tissue AnatomyEach skeletal muscle fiber is a long cylindrical cell with multiple oval nuclei just beneath its sarcolemma (plasma membrane). The fiber’s sarcoplasm
Red River College Jason J. Taylor MSc. 4

Human Anatomy and Physiology I
(cytoplasm) is similar to other cells, but it contains unusually large amounts of glycosomes and myoglobin.
Glycosomes –
Myoglobin – Muscle fibers contain the usual organelles, along with some that are highly modified and play important roles in muscle contraction: myofibrils, the sarcoplasmic reticulum, and T tubules.
MyofibrilsEach muscle fiber contains thousands of rodlike myofibrils that run the length of the cell. The myofibrils are so densely packed in the fiber that mitochondria and other organelles appear to be squeezed between them. They account for about 80% of the cell’s volume. The myofibrils are composed of even smaller rodlike structures called myofilaments organized into sarcomeres. Understanding how myofilaments are organized into sarcomeres is key to understanding how muscle cells contract.
Striations, Sarcomeres, and MyofilamentsRepeating light and dark bands are evident along the length of each myofibril. The dark A bands and the light I bands are nearly perfectly aligned with each one another, giving the cell as a whole its striated appearance.
Each dark A band has a lighter region in its midsection called the H zone. Each H zone is bisected vertically by a dark line called the M line. The light I bands are also bisected by a dark line called the Z disk.
A sarcomere is the smallest contractile unit of a muscle fiber – the functional unit of skeletal muscle. A sarcomere is the region between two successive Z disks. In other words, a sarcomere contains an A band flanked by half an I band at each end. Within each myofibril, the sarcomeres are aligned end-to-end like boxcars in a train.
If you look closely at the sarcomere, you can see that its banding pattern is due to even smaller structures called myofilaments. The central thick filaments extend the entire length of the A band and are responsible for its dark appearance. The more lateral thin filaments extend across the I band and partway into the A band. They create the light appearance of the I band. Note that the ends of the A bands are even darker than the H zone
Red River College Jason J. Taylor MSc. 5

Human Anatomy and Physiology I
between them. This is due to the overlap of thick and thin filaments in these end regions.
Molecular Composition of MyofilamentsMuscle contraction is possible because of the contractile proteins that make up the thick and thin filaments. These two contractile molecules are myosin and actin.
The A band’s thick filaments are composed primarily of myosin protein. Each myosin molecule has a rodlike tail attached by a flexible hinge to two globular heads. Each head contains actin and ATP binding sites, as well as ATPase enzymes. The heads are the “business-end” of this molecule – during contraction they form cross-bridges with the thin filaments that overlap with the thick filaments at the ends of the A band. Each thick filament is composed of about 300 myosin molecules bundled together with their tails pointing towards the A band’s M line and the heads facing the I band’s Z disk.
The I band’s thin filaments are composed primarily of actin. Each actin molecule is kidney-shaped with a myosin binding site. It’s this site that myosin forms cross-bridges with to produce contraction. Each thin filament is composed of two strands of actin molecules twisted together. One end of the strand is firmly attached to the Z disk. The other end overlaps with the thick filaments on either side of the A band.
Two important regulatory proteins are also present in thin filaments – tropomyosin and troponin. Both help control the myosin-actin interactions involved in contraction.
Tropomyosin is a rod shaped protein that spirals around each thin filament and helps stiffen and stabilize it. In a relaxed muscle fiber, tropomyosin
Red River College Jason J. Taylor MSc. 6

Human Anatomy and Physiology I
blocks the myosin binding sites on actin so that the myosin heads on the thick filaments cannot bind to the thin filaments.
Troponin is a globular three-polypeptide complex. One part binds to actin. Another binds to tropomyosin. The third part binds calcium ions. During muscle contraction, troponin is signaled by calcium ion to lift tropomyosin off of the thin filament, exposing its myosin binding sites to the thick filaments.
In addition to the contractile and regulatory proteins discussed above, other proteins are associated with the myofilaments. Structural proteins such as titin and dystrophin help support the thick and thin filaments.
Red River College Jason J. Taylor MSc. 7

Human Anatomy and Physiology I
Sarcoplasmic Reticulum and T TubulesSkeletal muscle fibers contain two sets of intracellular tubules that participate in regulation of muscle contraction: the sarcoplasmic reticulum and T tubules.
The sarcoplasmic reticulum (SR) is an elaborate network of smooth endoplasmic reticulum wrapped each myofibril. The major role of the SR is to regulate intracellular levels of ionic calcium. It stores calcium and releases it on demand when the muscle fiber is stimulated to contract. As you will see, calcium provides the final “go” signal for contraction.
At each A band-I band junction, the muscle cell’s sarcolemma protrudes deep into the cell interior, forming an elongated tube called the T tubule, which comes into close contact with the sarcoplasmic reticulum.
Contraction and relaxation of Skeletal Muscle FibersThe sliding filament theory of contraction states that during contraction the thin filaments slide past the thick filaments. When muscle fibers are stimulated by the nervous system, the myosin heads of the thick filaments latch onto the myosin-binding sites of the actin molecules making up the thin filaments, and the sliding begins. These cross bridges are formed and broken several times during a contraction, acting like tiny ratchets to pull the thin filaments towards the middle of the sarcomere, shortening it. The sliding of filaments and shortening of sarcomeres causes the shortening of the whole muscle fiber and ultimately the entire muscle.
Draw pictures of a relaxed sarcomere and a contracted sarcomere:
Fully Relaxed Sarcomere Fully Contracted Sarcomere
Notice that as a muscle shortens, the distance between adjacent Z disks decreases, the I bands shorten, the H zones disappear and the area of
Red River College Jason J. Taylor MSc. 8

Human Anatomy and Physiology I
overlap within the A band increases. Also, notice that the length of the A band does not change.
The sliding filament model tells us how a muscle fiber contracts, but it doesn’t it tell us what induces it to contract in the first place. That story is next!
Skeletal Muscle Fiber ContractionFor a skeletal muscle fiber to contract, 3 events have to occur:
1. The fiber must be activated by a nerve ending, causing a change in the fiber’s membrane potential
A. Action potential (AP) arrives at axon terminal at neuromuscular junction
B. Ach released; binds to receptors on sarcolemmaC. Ion permeability of sarcolemma changesD. Local change in membrane potential (depolarization) occursE. Local depolarization ignites AP in sarcolemma
2. The fiber must generate and propagate an electrical current (action potential) along its sarcolemma and down its along T tubules.
3. Ionic calcium (Ca2+) must be released from the SR to trigger contractionA. SR releases Ca2+; Ca2+ binds to troponin; myosin binding sites on
actin exposedB. Myosin heads bind to actin; contraction begins
Now that we have a general idea of the steps, let’s look at the details:
The Neuromuscular JunctionMuscle action potentials arise at the neuromuscular junction (NMJ), the synapse between a somatic motor neuron and a skeletal muscle fiber. A synapse is a region of communication between two neurons or a neuron and a target cell (e.g., skeletal muscle cell). Synapses separate cells from direct physical contact. Neurotransmitters bridge that gap. The neurotransmitter at a NMJ is acetylcholine (ACh).
When a nerve impulse reaches the NMJ, Ach is released. Upon binding to sarcolemma receptors, Ach causes a change in sarcolemma permeability leading to a change in membrane potential. The events at the NMJ are:
1. Action potential arrives at motor neuron’s axon terminal2. Voltage-gated Ca2+ channels open and Ca2+ enters the axon
terminal
Red River College Jason J. Taylor MSc. 9

Human Anatomy and Physiology I
3. Ca2+ entry causes some synaptic vesicles to release acetylcholine by exocytosis
4. Ach diffuses across the synaptic cleft and binds to receptors in sarcolemma
5. Ach binding opens ion channels that allow Na+ to diffuse into the cell and K+ to diffuse out of the cell; More Na+ enters than K+ leaves, producing a local change in the membrane potential (depolarization)
6. Ach effects are terminated by its enzymatic breakdown in the synaptic cleft by acetylcholinesterase
Red River College Jason J. Taylor MSc. 10

Human Anatomy and Physiology I
The neuromuscular junction:
Generation and Propagation of the Action PotentialLike all plasma membranes, the sarcolemma is polarized – there is a potential difference (voltage) across the membrane with the inside negative relative to the outer membrane face. In other words, the sarcolemma is like a battery in that it can store and release electrical energy. The act of releasing this energy is called an action potential and involves 2 steps: depolarization and repolarization. The action potential is the result of a sequence of electrical events that once initiated occurs along the sarcolemma’s entire surface. Essentially, the steps required to generate and propagate an action potential are:
1. Binding of Ach to Ach receptors in the sarcolemma side of the NMJ opens ion channels that allow Na+ to diffuse into the cell and K+ to diffuse out of the cell; More Na+ enters than K+ leaves, producing a local change in the membrane potential called depolarization. In other words, the interior surface of the sarcolemma becomes more positive than the outside face.
2. Depolarization of the sarcolemma in the NMJ causes depolarization of adjacent segments of the sarcolemma. In this way, the action potential is propagated along the entire length of the membrane, much like a row of dominoes are knocked over, or as ripples from a pebble dropped in a pool of water.
3. The areas of depolarization in the sarcolemma quickly return to their resting state – negative on the interior relative to the exterior face. This is called repolarization and is a result of the opening of
Red River College Jason J. Taylor MSc. 11

Human Anatomy and Physiology I
membrane K+ channels, allowing K+ to diffuse rapidly out of the cell and repolarize it.
Red River College Jason J. Taylor MSc. 12

Human Anatomy and Physiology I
The action potential:
Excitation-Contraction CouplingAn increase in cytosolic Ca2+ concentration starts muscle contraction; a decrease stops it.
The term excitation-contraction coupling describes the events that connect nervous excitation of a skeletal muscle fiber to its contraction:
1. When a nerve stimulates a muscle fiber, an action potential propagates along the sarcolemma, into the T tubules, and towards the sarcoplasmic reticulum
2. When the action potential reaches the sarcoplasmic reticulum’s terminal cisterns, voltage-gated Ca2+ release channels in the sarcoplasmic reticulum open.
3. Ca2+ pours into the cytosol where it binds with troponin, causing it to change shape.
4. Troponin moves tropomyosin away from the myosin-binding sites on actin. Myosin is now free to bind with actin - the contraction cycle begins.
5. The contraction cycle continues until Ca2+ active transport pumps return Ca2+ to the sarcoplasmic reticulum. When Ca2+ levels drop in the cytosol, tropomyosin falls back onto actin’s myosin binding sites and the contraction cycle stops.
Red River College Jason J. Taylor MSc. 13

Human Anatomy and Physiology I
Steps of the Cross Bridge CycleThe cross bridge cycle is the series of events during which myosin heads pull thin filaments toward the center of the sarcomere (aka the sliding filament theory). The steps of cross bridge cycling are:
Red River College Jason J. Taylor MSc. 14

Human Anatomy and Physiology I
Summary of Skeletal Muscle Fiber Contraction
Red River College Jason J. Taylor MSc. 15

Human Anatomy and Physiology I
Red River College Jason J. Taylor MSc. 16

Human Anatomy and Physiology I
Contraction of Skeletal MuscleBefore we consider muscle contraction at the organ level, let’s take a look at a few principles of muscle mechanics:
1. The principles governing contraction of a single skeletal muscle fiber are pretty much the same as those governing an entire skeletal muscle.
2. The force exerted by a contracting muscle on an object is called muscle tension. The opposing force exerted on the muscle by the weight of the object to be moved is called the load.
3. A contracting muscle doesn’t always shorten and move the load. This is called an isometric contraction. If the muscle can generate enough muscle tension to overcome the object’s load, then the muscle will shorten and the load will move. This is called an isotonic contraction.
4. A skeletal muscle contracts with varying force and for different periods of time in response to stimuli of varying frequencies and intensities.
The Motor UnitA motor neuron and the muscle fibers it stimulates form a motor unit. A single motor unit may innervate as few as 10 or as many as 2,000 muscle fibers, with an average of 150 fibers being innervated by each motor neuron.
The motor unit is the functional unit of skeletal muscle. When a motor neuron fires, all of the muscle fibers it innervates respond by contracting in unison. The muscle fibers in a single motor unit are not clustered together, but are spread throughout the muscle. Therefore, stimulation of a single motor unit produces weak contraction of the entire muscle. Muscles that control precise movements (like the muscles of the hand) consist of many small motor units, each consisting of a motor neuron and 10-20 muscle fibers. Muscles that control large-scale and powerful movements (like the quadriceps) consist of fewer motor units that control 2000-3000 muscle fibers each.
Twitch ContractionA twitch contraction is a brief contraction of all the muscle fibers in a motor unit in response to a single action potential. A twitch contraction has three distinct phases:
1. Latent period: the brief time delay between excitation and contraction of the muscle; corresponds to the time required for Ca2+
Red River College Jason J. Taylor MSc. 17

Human Anatomy and Physiology I
to leave the sarcoplasmic reticulum and bind to the troponin-tropomyosin complexes of the thin filaments.
2. Contraction period: the time between the onset and peak of muscle tension; corresponds to the period of time when the thick filaments are pulling the thin filaments towards the M line. If muscle tension is great enough to overcome the load, the muscle shortens.
3. Relaxation period: the time between peak tension development and no tension; corresponds to the period of time where Ca2+ is transported back into the sarcoplasmic reticulum, which results in relaxation.
The actual duration of these three periods in a twitch contraction depends on the type of muscle fiber. Some fibers are fast-twitch (e.g. eye muscles), with a contraction period of 10 msec. Some fibers are slow-twitch (e.g. quadriceps), with a contraction period of 100 msec.
Graded Muscle ResponsesOur muscles do not normally operate using muscle twitches – single, jerky contractions. Instead, muscle contractions are relatively smooth and vary in strength as different demands are placed on them. These variations are called graded muscle responses. In general, muscle contraction can be graded in 2 ways:
1. By changing the frequency of stimulation to produce smooth muscle contractions
2. By changing the strength of stimulation to produce more or less muscle tension
Nervous Control Produces Smooth, Continuous Muscle Contractions
Red River College Jason J. Taylor MSc. 18

Human Anatomy and Physiology I
The nervous system produces smooth muscle contractions by regulating the frequency of stimulation to a motor unit. Let’s see what happens when you change the firing rate of motor neurons. Take a look at the graph below and note that the Y axis represents tension. When two identical electrical stimuli are delivered to a muscle in rapid succession, the second stitch is stronger than the first. Note in the graph that the second twitch rides on the shoulders of the first. This is called wave summation. It occurs because the second contraction happens before the muscle has completely relaxed from the first contraction. Looking at it from a molecular perspective, before the muscle fiber’s SR has been able to reabsorb the Ca2+ released from the first contraction, a second action potential stimulates it to release more Ca2+. The result is a greater sarcoplasmic concentration of Ca2+ following the second stimulus and, consequently, a stronger muscle contraction.
While wave summation does increases muscle tension, its physiological role is to produce smooth, continuous muscle contractions by rapidly stimulating all of the muscle fibers of a motor unit.
As the muscle is stimulated at an increasingly faster rate, relaxation time between twitches becomes shorter and shorter, sarcoplasmic Ca2+ concentration becomes higher, and the degree of wave summation becomes greater and greater. This sustained muscle contraction with partial relaxation between stimuli is called unfused tetanus. If we were to keep increasing the frequency of stimulation, muscle tension would increase until
Red River College Jason J. Taylor MSc. 19

Human Anatomy and Physiology I
maximum tension is reached. At this point all evidence of muscle relaxation disappears and the contractions fuse into a smooth sustained contraction plateau called fused tetanus.
Vigorous muscle activity cannot continue indefinitely. Prolonged tetanus inevitably leads to muscle fatigue – the muscle is unable to contract and its tension drops to zero.
Nervous Control Regulates the Force of ContractionAs we saw earlier, wave summation and incomplete tetanus is used to produce smooth, continuous muscle contractions. But, how can the hand muscles used to pat your cheek also deliver a stinging slap? The nervous system regulates muscle tension by regulating motor unit activation – the more motor units activated at the same time, the stronger the muscle contraction. This process is called recruitment.
Other Factors that Regulate Force of ContractionTwo other factors not related to nervous control help to regulate the force of a skeletal muscle contraction:
1. Size of the muscle fibers. Regular resistance exercise increases muscle force by causing muscle cells to hypertrophy, or increase in size.
2. Degree of muscle stretch. The forcefulness of muscle contraction depends on the amount of overlap of thick and filaments in a sarcomere before contraction begins. Maximum force is generated when a muscle’s sarcomeres are between 80 and 120% their optimal length. Increases and decreases beyond this optimal range result in decreased force and inability to generate muscle tension. This is called the length-tension relationship.
Muscle Tone Even relaxed skeletal muscle is almost always slightly contracted - at any given moment a few motor units within a muscle are contracted while most are relaxed. This is called muscle tone and is due to spinal reflexes that activate first one group of motor units and then another. Muscle tone keeps muscles firm, healthy, and ready to respond to stimulation. It also helps stabilize joints and maintain posture.
Isotonic and Isometric ContractionsAs noted earlier, there are two main kinds of skeletal muscle contraction – isotonic and isometric. In an isotonic contraction, muscle length changes and moves the load. This is due to the muscle developing enough tension to
Red River College Jason J. Taylor MSc. 20

Human Anatomy and Physiology I
overcome and move the load. Once enough muscle tension is developed, the tension remains relatively constant through the remainder of the contraction. Isotonic contractions are used to move objects.
There are two types of isotonic contraction:
1. Concentric: the muscle shortens and moves the load. Example: contraction of forearm flexors while picking up a book.
2. Eccentric: the muscle lengthens and resists the load. Example: contraction of forearm flexors while slowly lowering a book.
In an isometric contraction, muscle tension develops but the muscle’s length does not change – it neither shortens nor lengthens. This is due to the muscle not being able to generate enough tension to overcome an object’s load. Isometric contractions are used primarily to maintain posture and to stabilize joints.
Muscle MetabolismAs noted earlier, all muscle contraction requires energy in the form of ATP. Most of this energy is produced by the oxidation of nutrients within the cell’s mitochondria, especially the oxidation of glucose and fatty acids. Metabolism that requires oxygen is described as aerobic.
Storage CompoundsThe circulating blood constantly brings nutrients and oxygen to the cells, but muscle cells also store a small supply of each for rapid ATP generation, such as during vigorous exercise. For example:
Myoglobin stores additional oxygen. This compound is similar to the hemoglobin in blood, but is located specifically in muscle cells.
Glycogen is the storage form of glucose. It is a polysaccharide made of multiple glucose molecules and it can be broken down into glucose when needed by the muscle cells.
Fatty acids are stored as triglycerides formed into fat droplets. These droplets can be broken down into fatty acids when needed by the muscle cells.
Anaerobic metabolismAerobic metabolism is very efficient and yields a large amount of ATP, but it is relatively slow, so it cannot supply enough energy for the first few seconds of muscle contraction. Also, it requires an abundant oxygen supply. During strenuous activity, oxygen delivery to the tissues cannot keep up with the demands of hard-working muscles. Under these conditions, the
Red River College Jason J. Taylor MSc. 21

Human Anatomy and Physiology I
cells use faster mechanisms of ATP production that do not require oxygen. These processes are described as anaerobic:
Breakdown of creatine phosphate, a compound similar to ATP, in that it has a high energy bond that releases its energy when it is broken. This energy is used to make ATP for muscle contraction. It generates ATP very rapidly, but its supply is limited.
Anaerobic glycolysis, a process that breaks glucose down incompletely without using oxygen. A few ATPs are generated in these reactions, as is a by-product called lactic acid, which is later oxidized for energy when oxygen is available.
Excess Post-Exercise Oxygen ConsumptionChanging conditions limit the continuation of anaerobic metabolism. When a person stops exercising, enough ATP must be generated to reestablish a resting state by oxidizing any accumulated lactic acid and replenishing stored materials. The person must take in extra oxygen by continued rapid breathing, known as excess post-exercise oxygen consumption (EPOC).
Muscle FatigueIt is commonly thought that muscles tire because they are out of ATP or because lactic acid accumulates. In fact, fatigue in non-athletes frequently originates in the nervous system, not the muscles. People unaccustomed to strenuous exercise find the sensations it generates unpleasant and, consciously or unconsciously, reduce the nervous impulses to skeletal muscles. It is difficult to overcome the brain’s inhibition and truly fatigue a muscle, that is, take it to the point that it no longer responds to stimuli. True muscle fatigue has many causes, and may depend on individual factors, fitness and genetic make-up for example, and the type of exercise involved. These causes include depletion of glycogen reserves, inadequate oxygen supply, or the accumulation of phosphates from ATP breakdown.
Heat Production during Muscle ActivityOnly about 40% of ATP’s energy is harnessed to produce skeletal muscle contraction. The remainder is given off as heat. In order to maintain homeostasis, this heat is dissipated by several mechanisms including sweating and radiation of heat from the skin’s surface. On the opposite side of the coin, shivering is when muscle contractions are used to produce more heat.
Red River College Jason J. Taylor MSc. 22