Periodontal diseases
-
Upload
unpredictable-disha -
Category
Health & Medicine
-
view
146 -
download
0
Transcript of Periodontal diseases
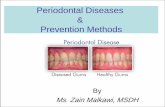
INTRODUCTION
CLASSIFICATION
GINGIVAL DISEASES
PERIODONTAL DISEASES
NECROTIZING PERIODONTAL DISEASES
ABSCESSES OF PERIODONTIUM
PERIODONTITIS ASSOCIATED WITH ENDODONTIC LESION
DEVELOPMENTAL OR ACQUIRED DEFORMATIES AND CONDITIONS
Components of periodontium:-
1. Gingiva
2. Periodontal ligament
3. Cementum
4. Alveolar bone
In 1999 a classification is given by AAP (American
Academy of Periodontology )
1. Gingival Diseases:-
A) Dental plaque induced gingival diseases:-
Most common form of gingival disease
associated with dental plaque is
GINGIVITIS.
i. Gingivitis associated with dental plaque only:-
It is the result of an interaction between the
microorganisms found in the dental plaque
biofilm and the tissues of the host .
ii. Gingival diseases modified by systemic factors:-
Systemic factors contributing to gingivitis , such as
endocrine changes associated with puberty ,
the menstrual cycle , pregnancy and diabetes
Blood Dyscrasias such as , leukemia
iii. Gingival diseases modified by
medications:-
anticonvulsant drugs such as
phenytoin ,
immunosuppressive
drugs such as cyclosporine
iv. Gingival diseases modified by malnutrition:-
such as in ascorbic acid deficiency
( bright red swollen bleeding gingiva)
scurvy
B) Non plaque induced gingival diseases:-
Mostly occurs in immunocompromised patients
and individuals belonging to lower
socioeconomic groups
i. Gingival diseases of specific bacterial origin:-
As a result of sexually transmitted diseases
like syphilis, gonorrhea , secondary to some
systemic infection like streptococcal gingivitis
ii. Gingival diseases of viral origin:- caused by the DNA and RNA virus like
herpes virus
iii. Gingival diseases of fungal origin:- occurs most commonly in immunocompromised patients and those on long term use of broad spectrum antibiotics. Most common fungal infection is candidiasis.
iv. Gingival Diseases of Genetic Origin:-
such as hereditary gingival fibromatosis in this the gingival enlargement
completely cover the teeth and delay eruption
v. Gingival manifestations of systemic conditions:-
such as allergic reactions due to toothpastes , mouthwashes , chewing gum
and food
vi. Traumatic lesions:-
Produced by intentional or unintentional artificial means examples of
traumatic lesion include tooth brush trauma , iatrogenic trauma etc.
vii. Foreign body reactions:-
Foreign body reactions lead to localized inflammatory condition of the
gingiva and are caused by the introduction of foreign materials into the
gingival connective tissues through breaks in epithelium. For example
introduction of amalgam into the gingiva during the placement of
restoration , extraction of tooth
2) Periodontitis
It is defined as an inflammatory
disease of the supporting tissues
of teeth caused by specific microorganisms,
resulting in destruction of the
periodontal ligament and alveolar bone with
increased probing depth formation, recession or both.
Difference between gingivitis and periodontitis is the loss of attachment of teeth.
Three general clinical manifestations of periodontitis are
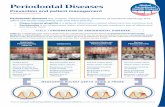
A) Chronic Periodontitis
B) Aggressive Periodontitis
C) Periodontitis as a manifestation of systemic diseases
CHRONIC PERIODONTITIS
Characteristics of chronic periodontitis:-
a) Prevalent in adults but can be observed in children also.
b) Associated with the accumulation of plaque and calculus.
c) Slow to moderate rate of progression
Chronic periodontitis may be further classified into :-
i. Localized form:- in this less than 30% of the evaluated site demonstrate attachment and bone loss
ii. Generalized form:- in this more than 30% of sites are affected
iii. Slight:- 1-2 mm clinical attachment loss (CAL)
iv. Moderate:- 3-4 mm (CAL)
v. Severe:- ≥5 mm (CAL)
AGGRESSIVE PERIODONTITIS
Aggressive periodontitis differs from the chronic periodontitis by
i. It has rapid rate of disease progression in healthy individuals
ii. Absence of large accumulations of plaque and calculus
iii. A family history of aggressive disease suggestive of a genetic trait
It usually affects young individuals at or shortly after puberty and is observed during second and third decades of life
Further classified as :-
I. Localized form:- Localized first molar or incisor disease with proximal attachment loss on at least two permanent teeth one of which is first molar.
II. Generalized form:- Generalized proximal attachment loss affecting at least three teeth other than first molars and incisors.
Periodontitis as a manifestation of systemic diseases
Periodontitis may be observed as a manifestation of
following systemic diseases:-
A) Hematological disorders
a) acquired Neutropenia
b) Leukemias
B) Genetic Disorders
a) down syndrome
b) Cohen syndrome
c) Chediak higashi syndrome
3) Necrotizing Periodontal diseases
These diseases have tissue necrosis as primary clinical feature.
There are two forms of necrotizing periodontal diseases
A) Necrotizing Ulcerative Gingivitis (NUG)
Its an acute lesion disease characterized by attachment loss.
Precipitating factors are psychologic stress, smoking and immunosuppression.
B) Necrotizing Ulcerative Periodontitis (NUP)
In this loss of clinical attachment and alveolar bone is a characteristic feature .
4) Abscess of Periodontium
A periodontal abscess is a purulent infection of periodontal
tissues and is classified by its tissue of origin
5) Periodontitis associated with endodontic lesions
Classification of lesions affecting the periodontium and pulp is based on the sequence of the disease process.
A) Endodontic-Periodontal lesions:- In this pulpal necrosis precedes periodontal changes. Clinically it presents as Localized , deep , periodontal pockets extending to apex of teeth
B) Periodontal-Endodontic lesion:- in this bacterial infection from periodontal pocket associated with loss of attachment and root exposure may spread through accessory canals to the pulp resulting in pulp necrosis
C) Combined lesions:- combined lesions occur when pulpal necrosis and a periapical lesion occur on a tooth that is also periodontally involved.
6) Developmental or Acquired Deformities and conditions
A. Tooth-Related factors:- these localized tooth related factors contribute to the initiation and progression of periodontal disease. These factors fall into four subgroups:-
a) Tooth anatomic factor.
b) Dental restoration and appliance
c) Root fractures
d) Cervical root resorption and cemental tears.B. Mucogingival deformities and conditions around teeth
C. Mucogingival deformities and conditions of edentulous ridges
D. Occlusal Trauma