Implantable Hemodynamic Monitoring for Heart Failure Patients › content › accj › 70 › 3 ›...
Transcript of Implantable Hemodynamic Monitoring for Heart Failure Patients › content › accj › 70 › 3 ›...

Listen to this manuscript’s
audio summary by
JACC Editor-in-Chief
Dr. Valentin Fuster.
J O U R N A L O F T H E AM E R I C A N C O L L E G E O F C A R D I O L O G Y V O L . 7 0 , N O . 3 , 2 0 1 7
ª 2 0 1 7 B Y T H E AM E R I C A N C O L L E G E O F C A R D I O L O G Y F O U N D A T I O N
P U B L I S H E D B Y E L S E V I E R
I S S N 0 7 3 5 - 1 0 9 7 / $ 3 6 . 0 0
h t t p : / / d x . d o i . o r g / 1 0 . 1 0 1 6 / j . j a c c . 2 0 1 7 . 0 5 . 0 5 2
REVIEW TOPIC OF THE WEEK
Implantable Hemodynamic Monitoringfor Heart Failure Patients
William T. Abraham, MD,a Leor Perl, MDb,c,dABSTRACT
Fro
Lu
Isr
Un
Ve
Ma
Rates of heart failure hospitalization remain unacceptably high. Such hospitalizations are associated with substantial
patient, caregiver, and economic costs. Randomized controlled trials of noninvasive telemedical systems have failed to
demonstrate reduced rates of hospitalization. The failure of these technologies may be due to the limitations of the
signals measured. Intracardiac and pulmonary artery pressure–guided management has become a focus of hospitalization
reduction in heart failure. Early studies using implantable hemodynamic monitors demonstrated the potential of
pressure-based heart failure management, whereas subsequent studies confirmed the clinical utility of this approach. One
large pivotal trial proved the safety and efficacy of pulmonary artery pressure–guided heart failure management, showing
a marked reduction in heart failure hospitalizations in patients randomized to active pressure-guided management.
“Next-generation” implantable hemodynamic monitors are in development, and novel approaches for the use of this data
promise to expand the use of pressure-guided heart failure management. (J Am Coll Cardiol 2017;70:389–98)
© 2017 by the American College of Cardiology Foundation.
H eart failure is a leading cause of morbidityand mortality, and it results in a substantialeconomic burden to the health care system.
It is particularly characterized by a very high rate ofhospital admission and readmission. Heart failure isthe primary diagnosis in more than 1 million hospital-izations annually in the United States alone (1), and itis associated with the highest rate of hospital read-missions when compared with all other medical orsurgical causes of hospitalization (2). Importantly,the number of decompensation events predictsincreased rates of morbidity and mortality in patientswith heart failure, independent of age and renalfunction (3,4). Despite advancements in diagnosticand therapeutic modalities, these rates have notchanged in recent years (5). In terms of financialburden, the costs of heart failure in the United Statesare currently estimated at just over $30 billion a year,and they are expected to exceed $70 billion annually
m the aDepartments of Medicine, Physiology, and Cell Biology, Division
ng Research Institute, The Ohio State University, Columbus, Ohio; bCardio
ael; cSackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel; and
iversity Medical Center, Stanford, California. Dr. Abraham has received co
ctorious Medical Technologies. Dr. Perl has received consulting fees from
nuscript received May 23, 2017; accepted May 24, 2017.
by 2030 (6). Two-thirds of the cost of heart failurecare is attributable to managing episodes of acutedecompensation in the hospital. A reduction of heartfailure hospitalizations is thus a major focus of theCenters for Medicare and Medicaid Services, and iscurrently considered a major unmet clinical need.
LIMITATIONS OF CURRENT HEART FAILURE
MONITORING SYSTEMS
Current attempts to estimate changes in volume sta-tus and, in turn, the risk for impending heart failureexacerbation are mostly dependent upon identifyingworsening heart failure signs and symptoms andchanges in body weight. However, these signalsappear late and are relatively unreliable (i.e., insen-sitive) markers of clinical status in patients with heartfailure. Daily measurement of body weight, forexample, has a sensitivity of only 9% for the
of Cardiovascular Medicine, and the Davis Heart &
logy Department, Rabin Medical Center, Petah Tikva,
the dDivision of Cardiovascular Medicine, Stanford
nsulting fees from Medtronic, St. Jude Medical, and
Vectorious Medical Technologies.

ABBR EV I A T I ON S
AND ACRONYMS
CIED = cardiac implantable
electronic devices
LAP = left atrial pressure
LVEDP = left ventricular
end-diastolic pressure
NYHA = New York Heart
Association
PAP = pulmonary artery
pressure
PCWP = pulmonary capillary
wedge pressure
RV = right ventricle/ventricular
Abraham and Perl J A C C V O L . 7 0 , N O . 3 , 2 0 1 7
Implantable Hemodynamic Monitoring J U L Y 1 8 , 2 0 1 7 : 3 8 9 – 9 8
390
development of a new heart failure exacer-bation (7,8). Although blood tests, such asB-type natriuretic peptide, are useful indistinguishing heart failure from other cau-ses of shortness of breath in patients who arealready presenting to the emergency depart-ment (9), they have yet to be proven helpfulin the ongoing management of patients withchronic heart failure (10). Moreover, heartfailure therapy guided by monitoring ofsigns, symptoms, weight, and biomarkers hasnot been shown to improve clinical out-comes, even when incorporated into remotetelemedicine systems.
These systems generally integrate regularcommunication between patients and their medicalproviders with or without electronic data transfer ofphysiological measurements, such as signs, symp-toms, body weight, and other information generallycollected by noninvasive devices. Although asystematic review published in 2010 (11) showedreductions in the rates of death from any cause and inheart failure–related hospitalizations using suchnoninvasive telemonitoring systems, subsequentrandomized controlled telemonitoring trials usingsimilar systems have failed to confirm these obser-vations (12–15). For example, the multicenter ran-domized controlled Tele-HF (Telemonitoring toImprove Heart Failure Outcomes) trial examinedwhether telemonitoring would reduce the combinedendpoint of readmission or death from any causeamong 1,653 patients recently hospitalized for heartfailure (12). In the treatment group, data wascollected on a daily basis by telephone, and includedan interactive voice response system that collectedinformation about symptoms and an electronic scalethat provided measurement of daily weight that wasreviewed by the patients’ clinicians so that treatmentcould be adjusted to keep the patient out of thehospital. After 180 days, there were no differences inoutcomes between the treatment group and the con-trol (usual care) group, nor were there any differencesin secondary endpoints, such as in the number ofhospitalizations or number of days in the hospital.
More recently, the BEAT-HF (Better EffectivenessAfter Transition–Heart Failure) randomized clinicaltrial evaluated a particularly robust approach tononinvasive telemonitoring of patients with heartfailure (14). The trial was performed at 6 academicmedical centers in California, all with great interest inheart failure management. Patients with acutedecompensated heart failure who were 50 years ofage or older were enrolled and followed for 180 daysafter discharge from the hospital. The intervention
combined health coaching telephone calls andtelemonitoring, including daily electronic collectionof blood pressure, heart rate, symptoms, and weight.Centralized nurses conducted telemonitoringreviews, protocolized actions, and telephone calls topatients. A total of 1,437 patients were randomized tothe intervention group or to usual care. The primaryoutcome was readmission for any cause within180 days after discharge. Secondary outcomes wereall-cause readmission within 30 days, all-cause mor-tality at 30 and 180 days, and quality of life at 30 and180 days. With the exception of the change in qualityof life over 180 days, none of these endpoints wereimproved by the intervention. That is, there were noimprovements in any of the pre-specified clinicaloutcomes measures in the intervention versus usualcare group. Regarding the modest, but statisticallysignificant improvement in quality of life observed,another randomized controlled trial evaluating apatient-centered disease management interventionfailed to confirm any improvement in quality of lifewith a similarly intense noninvasive disease man-agement program (15). Thus, noninvasive remotetelemedicine systems do not seem to make patientsfeel better or keep them out of the hospital.
Once seen as promising, remote monitoring ofheart failure patients with cardiac implantable elec-tronic devices (CIEDs) has not been proven to reducemorbidity or mortality. The use of these devices isbased on the reported high predictive value of device-based assessment of physiological parameters, suchas patient activity level, heart rate variability, andintrathoracic impedance. These parameters haveproven to be more sensitive than daily weight moni-toring in predicting fluid accumulation (16) and usefulin risk-stratification of patients with heart failure (17);however, randomized controlled trials using CIED-based heart failure diagnostics have demonstratedeither no effect or a detrimental effect on clinicaloutcomes (18,19). The potential role of CIED-baseddiagnostics in heart failure is reviewed in moredetail elsewhere (20).
The failure of these remote monitoring methodsmay have to do with the type of data collected, ratherthan with the specific idea of remote management. Asmentioned in the previous text, worsening signs andsymptoms of heart failure occur late in the naturalhistory of worsening heart failure, leading todecompensation and hospitalization. In fact, studiesof implanted hemodynamic monitoring systems inpatients with ambulatory heart failure have shownthat signs, symptoms, and weight change are poorsurrogates for ventricular filling pressures, and are notreliable predictors of impending hospitalization (21).

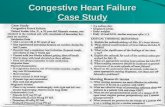
CENTRAL ILLUSTRATION The Concept of Pressure-Guided Heart Failure Therapy
Abraham, W.T. et al. J Am Coll Cardiol. 2017;70(3):389–98.
(Top) The usual-care approach to heart failure management is depicted, wherein the clinician relies on worsening symptoms and other noninvasive signals, such as
weight change, to treat clinical congestion, in the absence of knowledge about pre-symptomatic worsening of hemodynamics (called hemodynamic congestion).
Unfortunately, because the manifestations of clinical congestion present late in the course of heart failure decompensation, hospitalization is often inevitable, so the
usual-care approach can only be considered as reactive or too late to avert a heart failure hospitalization. (Bottom) By treating hemodynamic congestion during the
pre-symptomatic phase of worsening heart failure, a proactive approach to heart failure management is enabled, averting the risk of a future heart failure
hospitalization.
J A C C V O L . 7 0 , N O . 3 , 2 0 1 7 Abraham and PerlJ U L Y 1 8 , 2 0 1 7 : 3 8 9 – 9 8 Implantable Hemodynamic Monitoring
391
To the contrary, increases in ventricular fillingpressures, in both diastolic and systolic heart failurepatients, occur weeks before hospitalization for heartfailure (21). Thus, by targeting day-to-day mainte-nance of normal ventricular filling pressures, a heartfailure management system using ambulatory intra-cardiac or pulmonary artery pressure monitoringmight succeed in keeping patients out of the hospitalwhere other (noninvasive and CIED-based)approaches have failed (Central Illustration). Severalapproaches to chronic implantable hemodynamicmonitoring have been evaluated, and newer sensorsand systems are on the horizon.
THE CHRONICLE RIGHT VENTRICULAR
PRESSURE MONITORING SYSTEM
The first major breakthrough in the implantablemonitoring device arena was a right ventricular (RV)sensor, which, by measuring pressure during
pulmonic valve opening, could estimate the pulmo-nary artery diastolic pressure. A first study of thismethod, based on micromanometers implanted in theRVs and pulmonary arteries of 10 patients, was doneas a comparison with conventional pulmonary arterycatheter pressure measurement, and showed goodcorrelation (22). Next, 32 patients with heart failurewere tested with the implanted device, eventuallycalled the Chronicle IHM (Medtronic, Inc., Minneap-olis, Minnesota), which collected RV systolic anddiastolic pressures, heart rate, and pressurederivatives. During 36 volume-overload events inthese patients, RV systolic pressures increased by25% (p ¼ 0.05). There was an increase in pressure in 9of 12 hospitalization events approximately 4 daysbefore the exacerbation. There was also a 57%reduction (p < 0.01) in admission rate after hemody-namic data was used as an aid in patient management(23). This study was followed by the COMPASS-HF(Chronicle Offers Management to Patients with

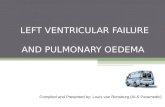
FIGURE 1 The Major Components of the CardioMEMS HF System
A B
03-07-2017 03-10-2017 03-13-2017 03-16-2017 03-19-2017 03-22-2017 03-25-2017 03-28-2017 03-31-2017 04-03-2017 04-06-2017 04-09-2017
05-2016 06-2016 07-2016 08-2016 09-2016 10-2016 11-2016 12-2016 01-2017 02-2017 03-2017 04-2017
0
20
40
60
80
C
100
From: To:03-06-2017 04-09-2017 Date Range: 30 days 90 days 180 days All
Fixed Auto
mm
Hg
PA Metrics and Events
0
20
40
60
80
140
120
100
bpm
PA Systolic PA Systolic Trend PA Mean PA Mean Trend
Medications
PA Diastolic PA Diastolic Trend Heart Rate from PA Sensor
Hospitalizations Notes Suspect Readings
NN N
(A) The MEMS-based pulmonary artery pressure sensor (Abbott, Sylmar, California). (B) The home electronics system that simultaneously powers and interrogates the
sensor, relaying pressure data to (C) a secure website for clinician review.
Abraham and Perl J A C C V O L . 7 0 , N O . 3 , 2 0 1 7
Implantable Hemodynamic Monitoring J U L Y 1 8 , 2 0 1 7 : 3 8 9 – 9 8
392
Advanced Signs and Symptoms of Heart Failure)study, which was the first randomized controlled trialfor the assessment of implantable hemodynamicmonitoring in patients with heart failure (24). A totalof 274 New York Heart Association (NYHA) functionalclass III and ambulatory class IV patients were ran-domized to the Chronicle IHM device managementalgorithm versus usual care. There was a nonsignifi-cant 21% reduction in the combined sum of heartfailure hospitalizations and emergency department orurgent clinic visits requiring intravenous therapy.However, a retrospective analysis of the time to firstHF hospitalization showed a 36% reduction (p ¼ 0.03)in the relative risk of heart failure hospitalizations inthe treatment group, and the potential efficacy ofpressure-guided therapy in this study appeared to begreatest in the NYHA functional class III patients. Infact, NYHA functional class IV patients randomized to
the treatment group actually had more decompensa-tion events compared with NYHA functional class IVcontrol subjects. These results, and the observation inthis study that high filling pressures precede theappearance of heart failure symptoms and predicthospitalizations for heart failure, were a motivationfor the next generations of implantable devices.
Several important lessons were learned from theCOMPASS-HF trial: 1) the main hemodynamic variablethat correlated with events was diastolic pulmonaryartery pressure (PAP), which usually rose gradually,rather than abruptly (21); 2) pressure-guided therapywas effective only if physicians actually modifiedtherapy in response to PAP, even in the absence ofsigns and symptoms of worsening heart failure (24);3) the absence of pre-specified pressure targetsallowed clinicians to leave PAPs in a range high abovenormal in many patients; and 4) NYHA functional

J A C C V O L . 7 0 , N O . 3 , 2 0 1 7 Abraham and PerlJ U L Y 1 8 , 2 0 1 7 : 3 8 9 – 9 8 Implantable Hemodynamic Monitoring
393
class IV patients did not benefit from PAP-guidedheart failure management. In the latter instance,low glomerular filtration rates and/or diuretic agentresistance may have prevented effective outpatienttreatment of elevated PAPs, necessitating hospitali-zation for intravenous therapies.
THE CardioMEMS PAP MONITORING SYSTEM
To date, the most significant advancement in thearena of implantable hemodynamic monitoringcapabilities was taken with a novel, wireless, battery-free, PAP monitoring system called the CardioMEMSHF System (Abbott, Sylmar, California) (Figure 1). Inthe CHAMPION (CardioMEMS Heart Sensor AllowsMonitoring of Pressure to Improve Outcomes inNYHA Class III Heart Failure Patients) trial (25,26),550 patients, regardless of left ventricular ejectionfraction, were randomized to 2 groups, one in whichthe clinicians used daily measurement of PAP inaddition to standard of care (treatment group;n ¼ 270) versus standard of care alone (control group;n ¼ 280) to manage patients. The CardioMEMS PAPsensor, previously shown to be safe (27), requires noleads or batteries, and is concurrently powered andinterrogated via an external antenna. It is implantedinto a branch of the pulmonary artery during rightheart catheterization, using a specialized deliverysystem. Pressure applied to the sensor causesdeflections of the pressure-sensitive surface, result-ing in a characteristic shift in the resonant frequency.Electromagnetic coupling is achieved by an externalantenna, which is held against the patient’s body orembedded in a pillow.
In the CHAMPION trial and in contrast toCOMPASS-HF, there were specific pressure targetsand suitable treatment algorithms that weremandated by protocol to ensure adequate testing ofthe hypothesis. Patients were considered hyper-volemic and at risk for heart failure hospitalization iftheir pressures were above the range of 15 to35 mm Hg for systolic PAP, 8 to 20 mm Hg for diastolicPAP, and 10 to 25 mm Hg for mean PAP, and weretreated by initiation or intensification of diureticagents, initiation or intensification of long-actingnitrates, and/or initiation or intensification of edu-cation regarding dietary salt and fluid restrictions.The primary endpoint was the rate of heart failurehospitalization over 6 months. There was a significantreduction of the primary endpoint, from a rate of 0.44in the control group to 0.32 in the treatment group(relative risk reduction: 28%; p ¼ 0.0002) (26). For theentire single-blinded follow-up period, which aver-aged more than 17 months, there was a reduction of
37% in the relative risk of heart failure hospitaliza-tions compared with the control group. There wasalso a significant reduction in PAP, a significantincrease in the number of days alive and out of thehospital for heart failure, a significant reduction inthe proportion of patients hospitalized for heartfailure, and a significant improvement in quality oflife in treatment versus control patients. Freedomfrom device- or system-related complications was98.6%, and overall freedom from pressure-sensorfailures was 100% (26).
An important pre-specified subgroup analysis ofthe CHAMPION trial demonstrated significant efficacyin patients with heart failure and a preserved ejectionfraction (28). Of the 550 patients enrolled in theCHAMPION study, 119 had left ventricular ejectionfraction $40% (average: 50.6%). The primary efficacyendpoint of heart failure hospitalization rate at6 months for patients with preserved ejection fractionwas 46% lower in the treatment group compared withthe control group (p < 0.0001). After an average of17.6 months of blinded follow-up, the hospitalizationrate was 50% lower (p < 0.0001). Other importantsubgroups of CHAMPION patients have been analyzedretrospectively. Taken together, these analysesdemonstrate the safety and effectiveness ofPAP-guided heart failure therapy in patients withsecondary pulmonary hypertension (29) and chronicobstructive pulmonary disease (30), and in those witha history of myocardial infarction, chronic kidneydisease, and atrial fibrillation. In addition, a recentreport from CHAMPION, which examined theextended efficacy of PAP-guided heart failure therapyover 18 months of randomized follow-up and theclinical effect of open access to pressure informationfor an additional 13 months in patients formerly in thecontrol group, demonstrated sustained efficacy andconfirmed the original CHAMPION trial findings (31).After PAP information became available to guidetherapy in the control group during open access(mean 13 months), rates of admissions to hospital forheart failure in the former control group werereduced by 48% (p < 0.0001), compared with rates ofadmissions in the control group during randomizedaccess. Another recent CHAMPION analysis examinedthe effect of PAP-guided heart failure therapy on30-day readmissions in Medicare-eligible patients,demonstrating a 49% reduction in total heart failurehospitalizations and a 58% reduction in all-cause30-day readmissions (32).
A detailed accounting of the pressure-guidedmedication interventions that led to improvedoutcomes in the CHAMPION trial has recently beenpublished (33), and may serve as a guide to the

Abraham and Perl J A C C V O L . 7 0 , N O . 3 , 2 0 1 7
Implantable Hemodynamic Monitoring J U L Y 1 8 , 2 0 1 7 : 3 8 9 – 9 8
394
“real-world” (post-approval) use of PAP-guided heartfailure management. (In May 2014, the U.S. Food andDrug Administration approved the CardioMEMS HFSystem for use in patients with NYHA functional classIII heart failure who had at least 1 heart failurehospitalization in the 12 months before implantationof the device.) Since approval, data on the generaluse of PAP-guided heart failure management hasbeen accrued. Although results from the ongoingCardioMEMS post-approval study (NCT02279888) arenot available, a recent publication reports the generaluse experience in 2,000 patients (34). Deidentifieddata from the remote monitoring database were usedto examine PAP trends from the first consecutive2,000 patients with at least 6 months of follow-up.The findings showed that these patients had higherPAPs at baseline and experienced a greater reductionin PAP over time compared with the pivotal CHAM-PION clinical trial. In addition, this study showedexcellent patient and clinician adherence to theCardioMEMS system, in that patients routinelyadhered to the taking of prescribed daily measure-ments and clinicians responded by adjustingmedications to lower PAPs. Another recent evaluationof the post-approval CardioMEMS experience retro-spectively studied a cohort of patients undergoingPAP sensor implantation between June 1, 2014, andDecember 31, 2015, using U.S. Medicare claims data(35). This analysis demonstrated that the use ofambulatory hemodynamic monitoring in clinicalpractice was associated with reductions in heartfailure hospitalizations and in comprehensive heartfailure costs.
OTHER PAP MONITORING SYSTEMS
Other PAP measurement systems are in development.One such pressure monitoring system is in develop-ment at Medtronic, Inc. (Minneapolis, Minnesota).This small, implanted sensor has a battery in thecapsule and talks through intrabody communicationto a Reveal LINQ Insertable Cardiac Monitor devicecoimplanted in the patient. Together, the 2 devicescan monitor not only PAP, but also cardiac arrhyth-mias, patient activity, and heart rate, among otherphysiological trends. The sensor is part of a largermanagement system that uses Bluetooth technologyand a patient’s cellular phone to provide data topatients and clinicians, and to improve clinicaloutcomes. Another system appears to be similar tothe CardioMEMS HF System, except for a differentexternal user interface (Endotronix, Inc., Woodridge,Illinois). Although PAP-guided heart failure therapywas proven to be effective in reducing the risk of
heart failure hospitalization in the CHAMPION trial,other implantable hemodynamic monitoring systemsare focused on direct measurement of left atrialpressure (LAP).
RATIONALE FOR THE DEVELOPMENT OF
LAP MONITORING SYSTEMS
Presuming that management of LAP or, perhaps moreproperly stated, LAP as a direct reflection of leftventricular filling pressure is the primary pressuretarget for the management of heart failure, directmeasurement of LAP may potentially provide moreclinical information in the management of heartfailure than measurement of right-sided pressures orPAPs. Evidence from animals regarding manipulationof pressure and the resultant pulmonary conse-quences has demonstrated strong correlationbetween increases in LAP and pulmonary congestion.In dogs, a rise in LAP over 11 mm Hg has been directlycorrelated with interstitial fluid leak (36). In rats, anincrease in LAP over 15 cm water inhibits the lungs’ability to reabsorb fluid by 50% (37). This process isreversible: a decrease in LAP from 15 to 0 cm waterresults in normalization of lung permeability tosolutes and alveolar fluid reabsorption. In assessingleft ventricular function in human subjects, LAP wasshown to correlate well with left ventricular end-diastolic pressure (LVEDP) when measured at thecorrect timing (at the “z point,” the foot of the leftatrial c-wave) (38). Although all pressures shouldtheoretically be equal during diastole, studies haveshown conflicting results. In 1970, an invasive studythat measured the relationship between mean LAPand end-diastolic PAP showed a significant correla-tion between the 2; however, the correlation provedto be inaccurate when the pulmonary vascular resis-tance was elevated (39). Although both systolic anddiastolic PAP were shown to correlate relatively wellwith pulmonary capillary wedge pressure (PCWP)(38,40,41), in patients with advanced heart failure,left- and right-sided filling pressures were found to bemismatched (42,43). Moreover, this discordance wasrelated to an increased risk of poor outcomes (44).Finally, PAP fails to correlate with LVEDP in a varietyof acute conditions, including in some patients withacute heart failure (45,46).
Importantly, pulmonary hypertension, a commoncondition affecting 25% to 83% of patients with heartfailure, depending on the population examined, is asignificant factor that affects the reliability of PAPmeasurement for estimating left-sided filling pres-sure. It is critical to know what the pulmonary resis-tance is, or more accurately, the gradient between

FIGURE 2 First- and Second-Generation LAP Sensors
(A) The HeartPOD left atrial pressure monitoring system (Abbott, Sylmar, California), which consists of a lead and a subcutaneous antenna coil. (B) The V-
LAP left atrial pressure sensor, which includes advanced onboard application-specific integrated circuit–based technologies that incorporate a novel drift
compensation mechanism. LAP ¼ left atrial pressure.
J A C C V O L . 7 0 , N O . 3 , 2 0 1 7 Abraham and PerlJ U L Y 1 8 , 2 0 1 7 : 3 8 9 – 9 8 Implantable Hemodynamic Monitoring
395
diastolic PAP and mean PCWP, because that value isless dependent upon blood flow, stroke volume, andchange in PCWP itself, but will reflect changes incompliance and distensibility of the pulmonaryarteries. In fact, tests have shown that there is a highgradient between PAP and mean PCWP (over5 mm Hg) in approximately one-half of all patientswith heart failure (47–50). This implies, on a physio-logical level, that PAP measurement alone may be aninaccurate indicator of LVEDP for many patients withheart failure, especially for those who also experiencecontributing factors, such as lung disease andthromboembolism. At the very least, any differencebetween PAP and LAP must be taken into account intreatment decisions.
It is possible that the frequency and timing ofpressure monitoring have an influence on the effi-ciency of heart failure management according to PAP.Although algorithms based on infrequent or 1-timePAP or PCWP measurement using right heart cathe-terization seem to be inefficient in improvingoutcomes (43), daily measurements conducted on anoutpatient basis can improve outcomes (26), mainlybecause they enable identification of a slow rise inpressure over longer periods of time, the indicatorthat best correlates with HF hospitalization risk.
Finally, there are specific cases in which LAPmonitoring might contribute valuable informationregarding conditions frequently associated withheart failure. An important example is functional(or secondary) mitral regurgitation, which is
associated with left ventricular enlargement anddysfunction. Earlier studies that directly measuredthe degree of mitral regurgitation and LAP showedgood correlation between the 2 during both angi-ography and surgery (51,52). Moreover, althoughthe enhanced LAP V-wave is generally not appre-ciated from the PAP waveform, it is readily seenwhen pressure is measured directly in the leftatrium. Another instance is the dynamic rise inLAP seen during cardiac ischemia. In 1 example,the detection of acute ischemia and subsequentrevascularization of a coronary artery was on thebasis of findings from an implanted LAP monitoringsystem (53).
THE HeartPOD LAP MONITORING SYSTEM
The HeartPOD (Abbott, formerly St. Jude Medical/Savacor, Inc.), a system that allowed for direct mea-surement of LAP in patients with ambulatory heartfailure, was studied over the past decade (54–56).This system was on the basis of an implantable sensorlead coupled to a subcutaneous antenna coil, a pa-tient advisory module, and remote clinician accessvia secure computer-based data management(Figure 2). The tip of the sensor system lead wasimplanted transvenously into the left atrium via theatrial septum. The implant was powered and interro-gated through the skin by wireless transmissions fromthe patient advisory module. A prospective, observa-tional, first-in-human study of this monitoring

Abraham and Perl J A C C V O L . 7 0 , N O . 3 , 2 0 1 7
Implantable Hemodynamic Monitoring J U L Y 1 8 , 2 0 1 7 : 3 8 9 – 9 8
396
system, using a physician-directed patient self-management paradigm, demonstrated improved he-modynamics, symptoms, and outcomes in patientswith advanced heart failure (56). A prospective ran-domized controlled outcomes study, the LAPTOP-HF(Left Atrial Pressure Monitoring to Optimize HeartFailure Therapy) trial, examined the safety and effi-cacy of the system in ambulatory NYHA functionalclass III patients who either were hospitalized for heartfailure during the previous 12 months or had anelevated B-type natriuretic peptide level, regardless ofejection fraction (57). LAP was measured twice daily,and LAP-guided therapy was compared with a controlgroup receiving optimal medical therapy alone.Randomization to the treatment or control group wasaccomplished using a 1:1 ratio in 3 strata based on theejection fraction (left ventricular ejection fraction>35% or #35%) and the presence of a de novo cardiacresynchronization therapy device indication. Enroll-ment in the LAPTOP-HF trial was stopped early, due toa perceived excess of implant-related complications.Preliminary results were presented during a LateBreaking Clinical Trials Session at the 2016 HeartFailure Society of America meeting (58). The overalltrial result was negative, demonstrating no reductionin a combined endpoint of recurrent heart failurehospitalizations and complications of heart failuretherapy. However, when the results were analyzedusing the CHAMPION trial endpoint of recurrent heartfailure hospitalizations, the results of the LAPTOP-HFtrial were similar to those of CHAMPION. Thus,although not a definitive evaluation of the efficacy ofLAP-guided heart failure therapy, LAPTOP-HFdemonstrated its potential and stimulated ongoingtechnology development in this arena.
OTHER LAP MONITORING SYSTEMS
The V-LAP system (Vectorious Medical Technologies,Tel Aviv, Israel) is an example of the next generationof implantable LAP monitoring systems, and usesadvanced application-specific integrated circuit–based technologies. It is a miniature percutaneousleft atrial pressure sensor that is robust, wireless,and leadless, and includes a novel drift compensa-tion mechanism. The device is implanted perma-nently in the septum using a transseptal approach. Ithas the advantage of a very low-profile design(14 mm in length and 2.5 mm in diameter). Theapplication-specific integrated circuit technologyallows for onboard drift compensation. The systemalso includes an external wearable belt that remotelypowers the implant, displays pressure readingsto the patient, and transmits LAP waveform
information to a web-based database. This data canbe analyzed with next-generation decision-supportsoftware systems to extract patient-specific physio-logical data, such as heart rate variability, thepresence of valvular pathologies, early warning forarrhythmias, and diastolic and exercise hemody-namics. In animal studies, the device was implantedin a transseptal approach; it was safe, and wasshown to communicate well with the externalbelt at depths of up to 30 cm. Another micro-electromechanical systems–based LAP monitoringsystem is implanted surgically, rather than trans-septally (Integrated Sensing Systems, Inc., Ypsilanti,Michigan). The surgical implantation approach limitsthe use of this sensor to patients undergoing cardiacsurgery; thus, it has been evaluated in first-in-manstudies in patients undergoing implantation of aleft ventricular assist device or other cardiacsurgery. These studies have demonstrated thefeasibility of the approach.
SUMMARY
The proximate cause of worsening heart failureleading to hospitalization is an increase in intracar-diac pressure and PAP. Noninvasive telemedicinesystems and CIED-based diagnostics provide onlypoor surrogates for these pressure changes, andmanagement based on such systems has failed toreduce the risk of heart failure hospitalization.Newer technologies, such as the CardioMEMS HFsystem, enable day-to-day remote management ofintracardiac pressure and PAP using implantablehemodynamic monitoring systems. In the CHAM-PION trial, this approach was shown to significantlyreduce the rate of heart failure hospitalizations inpatients with heart failure, regardless of their ejec-tion fractions. That is, the efficacy of pressure-guided therapy was demonstrated in heart failurepatients with either a reduced or a preserved ejec-tion fraction. In this regard, the CardioMEMS HFSystem has revolutionized the management of heartfailure by directing attention away from treatingsigns and symptoms alone to managing the under-lying cause of symptomatic and worsening heartfailure. To date, the reported real-world experiencewith this system has been encouraging. Additional,more technologically-advanced, implantable hemo-dynamic monitoring systems are in development,and newer approaches to the use of this data (suchas a physician-directed, patient self-managementapproach) may yet again revolutionize themanagement of patients with heart failure. Suchtechnologies provide a future platform for chronic

J A C C V O L . 7 0 , N O . 3 , 2 0 1 7 Abraham and PerlJ U L Y 1 8 , 2 0 1 7 : 3 8 9 – 9 8 Implantable Hemodynamic Monitoring
397
disease management that will allow us to look forother clinical applications of objective data collec-tion from within the cardiovascular system as wemove into the age of connected health, and thus,hopefully additionally reduce patient morbidityand mortality.
ADDRESS FOR CORRESPONDENCE: Dr. William T.Abraham, Division of Cardiovascular Medicine, TheOhio State University, 473 West 12th Avenue, Suite110P, Columbus, Ohio 43210. E-mail: [email protected].
RE F E RENCE S
1. Go AS, Mozaffarian D, Roger VL, et al., for theAmerican Heart Association Statistics Committeeand Stroke Statistics Subcommittee. Heart diseaseand stroke statistics: 2014 update: a report fromthe American Heart Association. Circulation 2014;129:e28–292.
2. Jencks SF, Williams MV, Coleman EA. Rehospi-talizations among patients in the Medicare fee-for-service program. N Engl J Med 2009;360:1418–28.
3. Lee DS, Austin PC, Stukel TA, et al. “Dose-dependent” impact of recurrent cardiac events onmortality in patients with heart failure. Am J Med2009;122:162–9.e1.
4. Setoguchi S, Stevenson LW, Schneeweiss S.Repeated hospitalizations predict mortality in thecommunity population with heart failure. AmHeart J 2007;154:260–6.
5. Ross JS, Chen J, Lin Z, et al. Recent nationaltrends in readmission rates after heart failurehospitalization. Circ Heart Fail 2010;3:97–103.
6. Heidenreich PA, Albert NM, Allen LA, et al., forthe American Heart Association Advocacy Coordi-nating Committee, Council on Arteriosclerosis,Thrombosis and Vascular Biology, Council onCardiovascular Radiology and Intervention, Coun-cil on Clinical Cardiology, Council on Epidemiologyand Prevention; and Stroke Council. Forecastingthe impact of heart failure in the United States: apolicy statement from the American Heart Asso-ciation. Circ Heart Fail 2013;6:606–19.
7. Lewin J, Ledwidge M, O’Loughlin C, McNally C,McDonald K. Clinical deterioration in establishedheart failure: what is the value of BNP and weightgain in aiding diagnosis? Eur J Heart Fail 2005;7:953–7.
8. Adamson PB. Pathophysiology of the transitionfrom chronic compensated to acute decom-pensated heart failure: new insights from contin-uous monitoring devices. Curr Heart Fail Rep2009;6:287–92.
9. Roberts E, Ludman AJ, Dworzynski K, et al., forthe NICE Guideline Development Group for AcuteHeart Failure. The diagnostic accuracy of thenatriuretic peptides in heart failure: systematicreview and diagnostic meta-analysis in the acutecare setting. BMJ 2015;350:h910.
10. Davenport C, Cheng EY, Kwok YT, et al.Assessing the diagnostic test accuracy of natri-uretic peptides and ECG in the diagnosis of leftventricular systolic dysfunction: a systematicreview and meta-analysis. Br J Gen Pract 2006;56:48–56.
11. Inglis SC, Clark RA, McAlister FA, et al. Struc-tured telephone support or telemonitoring
programmes for patients with chronic heart fail-ure. Cochrane Database Syst Rev 2010;8:CD007228.
12. Chaudhry SI, Mattera JA, Curtis JP, et al.Telemonitoring in patients with heart failure[Published corrections appear in N Engl J Med2011;364:490 and N Engl J Med 2013;369:1869].N Engl J Med 2010;363:2301–9.
13. Koehler F, Winkler S, Schieber M, et al., for theTelemedical Interventional Monitoring in HeartFailure Investigators. Impact of remote tele-medical management on mortality and hospitali-zations in ambulatory patients with chronic heartfailure: Telemedical Interventional Monitoring inHeart Failure study. Circulation 2011;123:1873–80.
14. Ong MK, Romano PS, Edgington S, et al., forthe Better Effectiveness After Transition—HeartFailure (BEAT-HF) Research Group. Effectivenessof remote patient monitoring after discharge ofhospitalized patients with heart failure: the BetterEffectiveness After Transition—Heart Failure(BEAT-HF) randomized clinical trial. JAMA InternMed 2016;176:310–8.
15. Bekelman DB, Plomondon ME, Carey EP, et al.Primary results of the Patient-Centered DiseaseManagement (PCDM) for Heart Failure study: arandomized clinical trial. JAMA Intern Med 2015;175:725–32.
16. Abraham WT, Compton S, Haas G, et al., forthe FAST Study Investigators. Intrathoracicimpedance vs daily weight monitoring for pre-dicting worsening heart failure events: results ofthe Fluid Accumulation Status Trial (FAST).Congest Heart Fail 2011;17:51–5.
17. Sharma V, Rathman LD, Small RS, et al. Strat-ifying patients at risk of heart failure hospitaliza-tion using existing device diagnostic thresholds.Heart Lung 2015;44:129–36.
18. van Veldhuisen DJ, Braunschweig F,Conraads V, et al., for the DOT-HF Investigators.Intrathoracic impedance monitoring, audible pa-tient alerts, and outcome in patients with heartfailure. Circulation 2011;124:1719–26.
19. Morgan JM, Dimitrov BD, Gill J, et al. Rationaleand study design of the REM-HF study: remotemanagement of heart failure using implanteddevices and formalized follow-up procedures. EurJ Heart Fail 2014;16:1039–45.
20. Abraham WT. Disease management: remotemonitoring in heart failure patients with implant-able defibrillators, resynchronization devices, andhaemodynamic monitors. Europace 2013;15 Suppl1:i40–6.
21. Zile MR, Bennett TD, St John Sutton M, et al.Transition from chronic compensated to acute
decompensated heart failure: pathophysiologicalinsights obtained from continuous monitoring ofintracardiac pressures. Circulation 2008;118:1433–41.
22. Reynolds DW, Bartelt N, Taepke R,Bennett TD. Measurement of pulmonary arterydiastolic pressure from the right ventricle. J AmColl Cardiol 1995;25:1176–82.
23. Adamson PB, Magalski A, Braunschweig F,et al. Ongoing right ventricular hemodynamics inheart failure: clinical value of measurementsderived from an implantable monitoring system.J Am Coll Cardiol 2003;41:565–71.
24. Bourge RC, Abraham WT, Adamson PB, et al.,for the COMPASS-HF Study Group. Randomizedcontrolled trial of an implantable continuoushemodynamic monitor in patients with advancedheart failure: the COMPASS-HF study. J Am CollCardiol 2008;51:1073–9.
25. Adamson PB, Abraham WT, Aaron M, et al.CHAMPION trial rationale and design: the long-term safety and clinical efficacy of a wirelesspulmonary artery pressure monitoring system.J Card Fail 2011;17:3–10.
26. Abraham WT, Adamson PB, Bourge RC, et al.,for the CHAMPION Trial Study Group. Wirelesspulmonary artery haemodynamic monitoring inchronic heart failure: a randomised controlledtrial. Lancet 2011;377:658–66.
27. Abraham WT, Adamson PB, Hasan A, et al.Safety and accuracy of a wireless pulmonary arterypressure monitoring system in patients with heartfailure. Am Heart J 2011;161:558–66.
28. Adamson PB, Abraham WT, Bourge RC, et al.Wireless pulmonary artery pressure monitoringguides management to reduce decompensation inheart failure with preserved ejection fraction. CircHeart Fail 2014;7:935–44.
29. Benza RL, Raina A, Abraham WT, et al. Pul-monary hypertension related to left heart disease:insight from a wireless implantable hemodynamicmonitor. J Heart Lung Transplant 2015;34:329–37.
30. Krahnke JS, Abraham WT, Adamson PB, et al.,Champion Trial Study Group. Heart failure andrespiratory hospitalizations are reduced inpatients with heart failure and chronic obstructivepulmonary disease with the use of an implantablepulmonary artery pressure monitoring device.J Card Fail 2015;21:240–9.
31. Abraham WT, Stevenson LW, Bourge RC,Lindenfeld JA, Bauman JG, Adamson PB, for theCHAMPION Trial Study Group. Sustained efficacyof pulmonary artery pressure to guide adjustmentof chronic heart failure therapy: complete

Abraham and Perl J A C C V O L . 7 0 , N O . 3 , 2 0 1 7
Implantable Hemodynamic Monitoring J U L Y 1 8 , 2 0 1 7 : 3 8 9 – 9 8
398
follow-up results from the CHAMPION randomisedtrial. Lancet 2016;387:453–61.
32. Adamson PB, Abraham WT, Stevenson LW,et al. Pulmonary artery pressure-guided heartfailure management reduces 30-day readmissions.Circ Heart Fail 2016;9:e002600.
33. Costanzo MR, Stevenson LW, Adamson PB,et al. Interventions linked to decreased heartfailure hospitalizations during ambulatory pulmo-nary artery pressure monitoring. J Am Coll CardiolHF 2016;4:333–44.
34. Heywood JT, Jermyn R, Shavelle D, et al.Impact of practice-based management of pulmo-nary artery pressures in 2000 patients implantedwith the CardioMEMS sensor. Circulation 2017;135:1509–17.
35. Desai AS, Bhimaraj A, Bharmi R, et al. Ambu-latory hemodynamic monitoring reduces heartfailure hospitalizations in “real-world” clinicalpractice. J Am Coll Cardiol 2017;69:2357–65.
36. Guyton AC, Lindsey AW. Effect of elevated leftatrial pressure and decreased plasma proteinconcentration on the development of pulmonaryedema. Circ Res 1959;7:649–57.
37. Saldías FJ, Azzam ZS, Ridge KM, et al. Alveolarfluid reabsorption is impaired by increased leftatrial pressures in rats. Am J Physiol Lung Cell MolPhysiol 2001;281:L591–7.
38. Forsberg SA. Relations between pressure inpulmonary artery, left atrium, and left ventriclewith special reference to events at end diastole. BrHeart J 1971;33:494–9.
39. Jenkins BS, Bradley RD, Branthwaite MA.Evaluation of pulmonary arterial end-diastolicpressure as an indirect estimate of left atrialmean pressure. Circulation 1970;42:75–8.
40. Drazner MH, Hamilton MA, Fonarow G,Creaser J, Flavell C, Stevenson LW. Relationshipbetween right and left-sided filling pressures in1000 patients with advanced heart failure. J HeartLung Transplant 1999;18:1126–32.
41. Lappas D, Lell WA, Gabel JC, Civetta JM,Lowenstein E. Indirect measurement of left-atrial
pressure in surgical patients–pulmonary-capillarywedge and pulmonary-artery diastolic pressurescompared with left-atrial pressure. Anesthesi-ology 1973;38:394–7.
42. Campbell P, Drazner MH, Kato M, et al.Mismatch of right- and left-sided filling pressuresin chronic heart failure. J Card Fail 2011;17:561–8.
43. Drazner MH, Velez-Martinez M, Ayers CR,et al. Relationship of right- to left-sided ventric-ular filling pressures in advanced heart failure:insights from the ESCAPE trial. Circ Heart Fail2013;6:264–70.
44. Grodin JL, Drazner MH, Dupont M, et al.A disproportionate elevation in right ventricularfilling pressure, in relation to left ventricularfilling pressure, is associated with renal impair-ment and increased mortality in advanceddecompensated heart failure. Am Heart J 2015;169:806–12.
45. Rahimtoola SH, Loeb HS, Ehsani A, et al.Relationship of pulmonary artery to left ventricu-lar diastolic pressures in acute myocardial infarc-tion. Circulation 1972;46:283–90.
46. Falicov RE, Resnekov L. Relationship of thepulmonary artery end-diastolic pressure to the leftventricular end-diastolic and mean filling pres-sures in patients with and without left ventriculardysfunction. Circulation 1970;42:65–73.
47. Vachiéry JL, Adir Y, Barberà JA, et al. Pulmo-nary hypertension due to left heart diseases. J AmColl Cardiol 2013;62:D100–8.
48. Naeije R, Vachiery JL, Yerly P, Vanderpool R.The transpulmonary pressure gradient for thediagnosis of pulmonary vascular disease. EurRespir J 2013;41:217–23.
49. Rapp AH, Lange RA, Cigarroa JE, Keeley CK,Hillis DL. Relation of pulmonary arterial diastolicand mean pulmonary arterial wedge pressures inpatients with and without pulmonary hyperten-sion. Am J Cardiol 2001;88:823–4.
50. Guazzi M, Borlaug BA. Pulmonary hyperten-sion due to left heart disease. Circulation 2012;126:975–90.
51. Grose R, Strain J, Cohen MV. Pulmonary arterialV waves in mitral regurgitation: clinical and exper-imental observations. Circulation 1984;69:214–22.
52. Klein AL, Stewart WJ, Bartlett J, et al. Effectsof mitral regurgitation on pulmonary venous flowand left atrial pressure: an intraoperative trans-esophageal echocardiographic study. J Am CollCardiol 1992;20:1345–52.
53. Ritzema-Carter JL, Smyth D, Troughton RW,et al. Images in cardiovascular medicine. Dynamicmyocardial ischemia caused by circumflex arterystenosis detected by a new implantable left atrialpressure monitoring device. Circulation 2006;113:e705–6.
54. Ritzema J, Melton IC, Richards AM, et al.Direct left atrial pressure monitoring in ambula-tory heart failure patients: initial experience with anew permanent implantable device. Circulation2007;116:2952–9.
55. Troughton RW, Ritzema J, Eigler NL, et al., forthe HOMEOSTATIS Investigators. Direct left atrialpressure monitoring in severe heart failure: long-term sensor performance. J Cardiovasc TranslRes 2011;4:3–13.
56. Ritzema J, Troughton R, Melton I, et al., for theHemodynamically Guided Home Self-Therapy inSevereHeart Failure Patients (HOMEOSTASIS) StudyGroup. Physician-directed patient self-managementof left atrial pressure in advanced chronic heartfailure. Circulation 2010;121:1086–95.
57. Maurer MS, Adamson PB, Costanzo MR,et al. Rationale and design of the Left AtrialPressure Monitoring to Optimize Heart FailureTherapy Study (LAPTOP-HF). J Card Fail 2015;21:479–88.
58. Abraham WT, Adamson PB, Costanzo MR,et al. Hemodynamic monitoring in advanced heartfailure: results from the LAPTOP-HF trial [abstr].J Card Fail 2016;22:940.
KEY WORDS disease management,hospitalization, patient readmission,pulmonary artery pressure, telemedicine