A systematic review and meta-analysis of oncologic outcomes in localized resectable soft-tissue...
-
Upload
isabel-lee -
Category
Documents
-
view
217 -
download
0
Transcript of A systematic review and meta-analysis of oncologic outcomes in localized resectable soft-tissue...
A systematic review and meta-analysis of oncologic outcomes in localized
resectable soft-tissue sarcoma
Emad Al-Absi MDForough Farrokhyar PhD
Rajrish Sharma MDKaitlyn Whelan
Tom Corbett MD, FRCPCMalti Patel MD, FRCPC
Michelle Ghert MD, FRCSC
Radiotherapy decreases local recurrence
(1) Leibel SA, Tranbaugh RF, Wara WM, Beckstead JH, Bovill EG, Phillips TL. Soft tissue sarcomas of the extremities: survival and patterns of failure with conservative surgery and postoperative irradiation compared to surgery alone. Cancer 1982; 50(6):1076-1083.
• (2) Lindberg RD, Martin RG, Romsdahl MM, Barkley HT, Jr. Conservative surgery and postoperative radiotherapy in 300 adults with soft-tissue sarcomas. Cancer 1981; 47(10):2391-2397.
• (3) Yang JC, Chang AE, Baker AR, Sindelar WF, Danforth DN, Topalian SL et al. Randomized prospective study of the benefit of adjuvant radiation therapy in the treatment of soft tissue sarcomas of the extremity. J Clin Oncol 1998; 16(1):197-203.
• (4) Strander H, Turesson I, Cavallin-Stahl E. A systematic overview of radiation therapy effects in soft tissue sarcomas. Acta Oncol 2003; 42(5-6):516-531.
• (5) DeLaney TF. Optimizing radiation therapy and post-treatment function in the management of extremity soft tissue sarcoma. Curr Treat Options Oncol 2004; 5(6):463-476.
• (6) Scoggins CR, Pollock RE. Extremity soft tissue sarcoma: evidence-based multidisciplinary management. J Surg Oncol 2005; 90(1):10-13.
• (7) Barker JL, Jr., Paulino AC, Feeney S, McCulloch T, Hoffman H. Locoregional treatment for adult soft tissue sarcomas of the head and neck: an institutional review. Cancer J 2003; 9(1):49-57.
• (8) Callister MD, Ballo MT, Pisters PW, Patel SR, Feig BW, Pollock RE et al. Epithelioid sarcoma: results of conservative surgery and radiotherapy. Int J Radiat Oncol Biol Phys 2001; 51(2):384-391.
• (9) Suit H, Spiro IJ. Soft tissue sarcomas: radiation as a therapeutic option. Ann Acad Med Singapore 1996; 25(6):855-861.
• (10) Tepper JE, Suit HD. The role of radiation therapy in the treatment of sarcoma of soft tissue. Cancer Invest 1985; 3(6):587-592.
• (11) Zlotecki RA, Katz TS, Morris CG, Lind DS, Hochwald SN. Adjuvant radiation therapy for resectable retroperitoneal soft tissue sarcoma: the University of Florida experience. Am J Clin Oncol 2005; 28(3):310-316.
Timing of peri-operative radiotherapy
• Single randomized controlled trial (RCT) of pre- vs. post-operative radiation
• O’Sullivan et al, Lancet 2002
• Primary endpoint: wound complications increased with pre-operative radiation
• Update 2005: late radiation morbidity increased with post-operative radiation
Survival
• Not defined as a primary a priori endpoint
• Trend towards improved survival in pre-operative radiotherapy
• ASCO Proceedings 2004: no difference in survival or local recurrence
Available data
• One landmark RCT, but oncologic outcomes were not a priori primary outcomes and power analysis not applied
• Can we use retrospective/observational data?
‘We found little evidence that estimatesof treatment effects in observational studies reported after 1984 are either consistently larger than or qualitatively different from those obtained in randomized, controlled trials.’ (N Engl J Med 2000;342:1878-86.)
‘The results of well-designed observationalstudies (with either a cohort or a case–controldesign) do not systematically overestimate the magnitude of the effects of treatment as compared with those in randomized, controlled trials on the same topic.’ (N Engl J Med 2000;342:1887-92.)
Conclusion
• Well-designed observational studies are appropriate for systematically performed meta-analyses
Purpose
To determine oncologic outcomes in pre- vs. postoperative radiation in localized
resectable soft-tissue sarcoma
Literature search
• MEDLINE, EMBASE, CancerLit and the Cochrane Database
• Text words and Medical Search Headings (MeSH terms): ‘soft-tissue’, ‘sarcoma’, ‘radiation’, ‘preoperative’ and ‘postoperative’.
• Varying combinations of the Boolean operators “AND,” “NOT,” and “OR”
• English
Inclusion and exclusion criteria
• Inclusion:– Compare outcomes pre- vs post-operative radiation– Oncologic outcomes reported in both groups
• Exclusion– Advanced or metastatic disease– Only outcomes related to wound complications
and/or radiation dosages– Review articles– Only one publication per cohort (duplicates
excluded)
Assessment of methodological quality
• Two independent reviewers
• Detsky Quality Scale for Randomized Trials
• Ottawa-Newcastle Quality Assessment Scale for case-control and cohort studies
• Level of agreement: intra class correlation coefficient
Statistical Analysis
• Cochran’s Q statistic for variability across studies
• Pooled odds ratio with 95% CI for local recurrence
• Fixed and random effects methods
Potentially relevant papers screened (n=1794)
Trial did not meet inclusion criteria n=10
1 review article1 no pre-operative arm
6 no oncologic outcomes2 cohorts included in
subsequent publications
Abstracts retrieved (n=92)
Full article reviewed for further evaluation
(n=15)
Papers used in meta-analysis (n=5)
Excluded solely based on abstract (n=77)
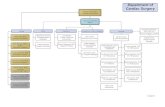
Literature review flow diagram
Study characteristics
• One RCT and 4 observational studies
• Total 1098 patients– 526 pre-operative radiation– 572 post-operative radiation
• Publication dates 1985-2005
• high level of agreement between reviewers (intra-class correlation coefficient 0.973; P=0.001) for study quality [all high])
Oncologic variables
Kuklo et al
Zagars et al Suit et al Cheng et al O-Sullivan et al
Tumor size >10 cm (%)
Pre-opPost-op
35.526
4221
4318
NANA
3533
Radiation dosage (mean Gy)
Pre-opPost-op
5163
5060
50-5264-66
4862
5066
Resection margin% positivePre-opPost-op
NANA
2412
NANA
4042
1715
Local recurrence
• 4 studies with available data
• 916 patients
• 134 local recurrences
• Risk for local recurrence lower in pre-operative radiation with fixed effects method
• Hazard ratio of 0.61 (95% CI, 0.42-0.89)
• Random effects: HR 0.67 (95% CI, 0.39-1.15)
Forest Plot: Fixed effects method
Citation EffectName Pre-op Post-op PValue Effect Lower Upper
Cheng Local Recurrence 7 / 48 6 / 64 .394 1.650 .517 5.272
Kuklo Local Recurrence 3 / 59 7 / 58 .177 .390 .096 1.590
SUIT Local Recurrence 6 / 60 13 / 110 .719 .829 .298 2.306
Zagars Local Recurrence 36 / 271 56 / 246 .005 .520 .328 .824
Fixed Combined (4) 52 / 438 82 / 478 .012 .614 .420 .898
0.1 0.2 0.5 1 2 5 10
Pre-op Post-op
Forest plot: Random effects method
Citation EffectName Pre-op Post-op PValue Effect Lower Upper
Cheng Local Recurrence 7 / 48 6 / 64 .394 1.650 .517 5.272
Kuklo Local Recurrence 3 / 59 7 / 58 .177 .390 .096 1.590
SUIT Local Recurrence 6 / 60 13 / 110 .719 .829 .298 2.306
Zagars Local Recurrence 36 / 271 56 / 246 .005 .520 .328 .824
Random Combined (4) 52 / 438 82 / 478 .146 .671 .392 1.149
0.1 0.2 0.5 1 2 5 10
Pre-op Post-op
Overall survival
• Lack of raw data for calculation of odds ratio
• Pre-operative 5-year survival: 76% (range, 62-88%)
• Post-operative 5-year survival: 67% (range 41-83%)
• Unable to determine statistical significance
Study heterogeneity
• P-value for heterogeneity 0.259
• I2 for differences across studies due to treatment effect 25%
• Moderate but acceptable heterogeneity
Funnel Plot
-3 -2 -1 0 1 2 3
0
1
2
Sta
nd
ard
Err
or
of
Lo
g O
R
Log Odds Ratio
Funnel Plot of Standard Error by Effect Size
O’Sullivan et el, ASCO 2004
• Actuarial data
• Local control: – Pre-operative radiation: 93%– Post-operative radiation: 92%
• Local control not a primary endpoint of RCT
• Pre-hoc power analysis for wound complications
Local recurrence
• Pooled data from 4 high quality observational studies
• Data suggests improved local control with pre-operative radiation
• However, random effects methods (preferred for heterogenous data) OR crossed 1.0 (0.39-1.15)
Oncologic variables
Kuklo et al
Zagars et al Suit et al Cheng et al O-Sullivan et al
Tumor size >10 cm (%)
Pre-opPost-op
35.526
4221
4318
NANA
3533
Radiation dosage (mean Gy)
Pre-opPost-op
5163
5060
50-5264-66
4862
5066
Resection margin% positivePre-opPost-op
NANA
2412
NANA
4042
1715
Local Recurrence
• Oncologic variables suggest pre-operative group at higher risk for local recurrence
• Therefore lower risk suggested in the current analysis might have some validity
Local recurrence
• Less ambiguity with respect to radiation field
• Dissection of tumor away from fixed structures (bone, vessel, nerve) facilitated by pre-operative radiation
• Higher oxygen tension in pre-operative tissue
Survival
• Pre-operative 76% (range, 62-88%)
• Post-operative 67% (range 41-83%)
• Is this statistically significant?
• All time-dependent data therefore pooling and analysis not possible
O’Sullivan et el, ASCO 2004
• Actuarial data
• Overall survival:– Pre-operative radiation : 73%– Post-operative radiation: 67%– Results very similar to observational data
• (76% vs 67%)
• Data does not suggest that waiting for surgery will result in death from metastases
Conclusions
* Large amount of published observational data
* One RCT
* Strict adherence to Evidence Based Medicine principles allows pooling of data
* Suggestion of improved local control with pre-operative radiation
* Patients not at risk of death from metastases if given pre-operative radiation
References1. O'Sullivan,B. et al. Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. Lancet. 359, 2235-2241 (2002).2. Suit,H.D., Mankin,H.J., Wood,W.C. & Proppe,K.H. Preoperative, intraoperative, and postoperative radiation in the treatment of primary soft tissue sarcoma. Cancer. 55, 2659-2667 (1985).3. Cheng,E.Y., Dusenbery,K.E., Winters,M.R. & Thompson,R.C. Soft tissue sarcomas: preoperative versus postoperative radiotherapy. J. Surg. Oncol. 61, 90-99 (1996).4. Kuklo,T.R. et al. Preoperative versus postoperative radiation therapy for soft-tissue sarcomas. Am. J. Orthop. 34, 75-80 (2005).5. Zagars,G.K. et al. Preoperative vs. postoperative radiation therapy for soft tissue sarcoma: a retrospective comparative evaluation of disease outcome. Int. J. Radiat. Oncol. Biol. Phys. 56, 482-488 (2003).