68 Current Respiratory Medicine Reviews , 2012, 68-78 ... › 94ca › 60e11a1bb...68 Current...
Transcript of 68 Current Respiratory Medicine Reviews , 2012, 68-78 ... › 94ca › 60e11a1bb...68 Current...

68 Current Respiratory Medicine Reviews, 2012, 8, 68-78
Weaning and Extubation in Pediatrics
Cíntia Johnston*,1
and Paulo Sérgio Lucas da Silva2
1Pediatric Intensive Care Unit, Department of Pediatrics, Universidade Federal de São Paulo, São Paulo, Brazil
2Pediatric Intensive Care Unit, Hospital do Servidor Publico Municipal, São Paulo, Brazil
Abstract: Mechanical ventilation is a life-supporting intervention that is used for a significant number of patients in
ICUs. The current pediatric literature shows that the science of ventilator weaning and extubation remains undetermined.
No optimal weaning method has been described for a more rapid and successful extubation. Protocol-based approaches to
weaning may have potential benefits in advancing readiness to extubation, but no significant outcome differences have
been found to date. The analysis of clinical markers of extubation success has not revealed any specific physiologic
predictor of extubation success in children. However, a daily trial of readiness to extubate is the most effective technique
to determine likelihood of success. Extubation failure rates range from 16% to 20% and bear little relation to the duration
of mechanical ventilation. Upper airway obstruction is the primary cause of extubation failure in most pediatric studies.
Therefore, efforts to decrease airway edema before extubation should be considered. Corticosteroids seem to be beneficial
for infants and children, but definitive evidence of their efficacy is lacking.
Keywords: Extubation, mechanical ventilation, respiratory support, weaning, pediatrics.
INTRODUCTION
Mechanical ventilation (MV) is often used to treat severely ill children in pediatric (PICU) and neonatal (NICU) intensive care units. The ideal time for MV discontinuation is usually defined by clinical and laboratory parameters available at the time when a decision is made about weaning or extubation [1]. These measurements usually indicate the capacity of the infant or child to keep spontaneous ventilation and adequate gas exchanges.
MV weaning or discontinuation is the total cessation of ventilatory support, whereas extubation is the removal of the endotracheal tube (artificial airway) [2]. The ideal time to interrupt MV and for extubation should not be determined by clinical impression alone. The decision to submit the patient to these two procedures depends on multiple factors, such as [3, 4]: neuromuscular conduction, which may be affected by sedation; ventilatory muscle strength, which may be affected by prolonged MV; endurance of ventilatory muscles; ventilatory changes, such as hyperthermia, excessive offer of carbon hydrate, and increase of the physiological dead space; and changes in ventilatory mechanics, which depends on the pulmonary elastic recoil and airway resistance.
Failure in MV weaning may be assigned to the unbalance between the load to ventilatory muscles and their competence to support this load, or to an inadequate energy supply to respond to the demands of these muscles.
The complexity of the decision about extubation provides solid reasons for the development of accurate predictors to evaluate success and failure. Extubation failure rates are based on clinical criteria and range from 17% to 19% in adults [5], from 22% to 28% in premature infants [6], and
*Address correspondence to this author at the Pediatric Intensive Care Unit,
Universidade Federal de São Paulo, Rua Napoleão de Barros, nº 748. São
Paulo – SP. Brazil; Tel: +55-11-55764288; Fax: +55-11-55764288;
E-mail: [email protected]
from 16% to 20% in pediatric patients [7, 8]. Early extubation exposes the patient to the risks of reintubation as an emergency procedure. However, the unnecessary prolonged use of MV increases the risk of airway trauma, nosocomial infection and discomfort, as well as hospital costs [3].
Several indices to measure oxygenation, such as maximal expiratory pressure (PEmax), lung function, minute ventilation (VE) and breathing reserve, have been suggested as useful predictors of weaning outcomes and of extubation success or failure in infants and children [4, 9]. Some of the indices commonly used in PICUs are the ratio of respiratory rate (RR) to tidal volume (VT) adjusted to weight (rapid shallow breathing index (RSBI), lung compliance, rate, oxygenation, pressure index (CROP index) and the spontaneous breathing trial (SBT) [3, 10]. However, objective criteria to predict extubation success or failure in pediatrics have not been established. These predictors do not seem to be sensitive or specific enough to predict extubation success or failure in pediatrics and neonatology [4]. Studies with adults [11, 12] and infants [13] used integrated indices, such as ventilatory drive, respiratory muscle load, respiratory muscle strength, and the quality of gas exchange.
1. Definitions
Weaning – transition from mechanical to assisted or spontaneous ventilation in patients on invasive MV for longer than 24 hours [14].
MV discontinuation – discontinuation of ventilatory support in patients that tolerate the SBT and that may be eligible for extubation [3].
Spontaneous breathing trial- SBT (a method to discontinue MV) – the patients is allowed to breath spontaneously through an endotracheal tube connected to a T-piece and an oxygen source. The patient receives continuous positive airway pressure (CPAP) of 5 cmH2O, or
1875-6387/12 $58.00+.00 © 2012 Bentham Science Publishers

Weaning and Extubation in Pediatrics Current Respiratory Medicine Reviews, 2012, Vol. 8, No. 1 69
pressure support ventilation (PSV) of 7 cmH2O [15, 16]. In pediatrics, PSV will depend on the diameter of the endotracheal tube.
Extubation and decannulation – Extubation is the removal of the artificial airway. In the case of patients that underwent tracheotomy, the word decannulation is used [17]. The need to reestablish an artificial airway is called reintubation or extubation failure. Early reintubation is the procedure that occurs less than 48 hours after extubation or decannulation [18].
Weaning success or failure – Successful ventilation weaning is defined as the maintenance of spontaneous ventilation for at least 48 hours after the interruption of MV. Weaning fails or is unsuccessful when mechanical ventilation is required within 48 hours of extubation [18].
MV discontinuation success or failure – MV discontinuation is defined as successful when the patient tolerates the SBT. These patients should be evaluated for the indication to remove the artificial airway (extubation) [19]. When the patient fails to SBT, MV discontinuation is unsuccessful.
Prolonged MV – It is defined when the patient depends on invasive or noninvasive ventilatory (NIV) support for longer than six hours per day for longer than one week, despite respiratory therapy programs, correction of functional disorders and use of new techniques for ventilatory support [17].
2. Weaning
To consider the beginning of the MV weaning process, the disease that caused or contributed to the ventilation decompensation should be resolved or on the way to resolution. The patient should be hemodynamically stable, which is indicated by good tissue perfusion, regardless of the use of vasopressor agents (low and stable doses are accepted), and no decompensated cardiac insufficiency or arrhythmias with hemodynamic instability. Moreover, gas exchanges should be within acceptable parameters (partial pressure of oxygen [PaO2]
60 mmHg, fraction of inspired
oxygen [FiO2]
0.40%, and positive end-expiratory pressure [PEEP] 5 to 8 cmH2O), and the patient should be able to initiate the inspiratory effort [2].
If the SBT is successful, other factors should be taken into consideration before extubation, such as mental state [17, 20] and sedation [21], degree of patient collaboration and the capacity to eliminate secretions from the airways.
To keep spontaneous breathing, inspiratory muscles should generate a force greater than lung and chest wall elastance (elastance load of lungs and chest wall), as well as airway and tissue resistance (resistive load). This demands adequate functioning of major ventilatory muscles, anatomical and functional integrity of the central and peripheral nervous system, preserved neuromuscular transmission, intact chest wall, and adequate muscle strength. This balance is usually polarized towards neuromuscular competence; in other words, there is a reserve that allows a considerable increase of the load offered to ventilatory muscles [22]. However, if competence is reduced to below a critical point, for example, myasthenia gravis or
drug intoxication, the balance may lean towards the load, so that the ventilatory pump cannot insufflate the lung and expand the chest wall [5]. The capacity of the ventilatory muscles to bear this load without apparent fatigue is called endurance and is determined by the balance between energy supply and demand. Under normal conditions, energy supply is adequate to meet these needs, and there is a large reserve. However, other factors, such as those associated with the increase of the resistive (bronchospasms, airway edema, airway secretion) and elastic (infection, atelectasis, hyperinflation), pulmonary and thoracic loads (pneumothorax, obesity, abdominal distension), as well as factors that decrease neuromuscular competence (decrease in respiratory drive, muscle weakness, changes in neuromus-cular transmission), may also determine MV weaning and extubation failures both in adult and pediatric or neonatal patients [7, 18, 23].
3. Spontaneous Breathing Trial
Several studies [3, 10, 14, 15, 18, 19, 24] showed that a 30-min to 2-hour SBT is useful to select patients ready for extubation. MV may be disconnected while supplemental oxygen is offered to keep the rate of arterial blood oxygen saturation (SaO2) above 90%. Oxygen supplementation should be offered when FiO2
is up to 40%, and should not be
increased during MV discontinuation. Other methods can also be used during SBT: biphasic positive airway pressure (BIPAP), automatic tube compensation (ATC) or proportional assist ventilation (PAV). The results of these methods are similar to those obtained when using the T-piece and PSV for the SBT [16, 25, 26].
Continuous bedside monitoring during the SBT is fundamental to detect early signs of intolerance and mechanisms of ventilatory failure (Table 1). When any sign of intolerance is detected, the SBT should be interrupted and ventilation with the previously adopted parameters should be resumed. Those patients that do not have any signs of intolerance to the test should be examined to assess the possibility of extubation, and should be observed (monitored) for 48 hours in the ICU. If ventilatory autonomy to maintained for 48 hours means that the extubation was successful [18, 27].
Table 1. Objective Parameters and Subjective Clinical
Assessment to be Considered During Spontaneous
Breathing Trial
Objective Parameters Subjective Clinical Evaluation
• Adequate gas exchange
• Hemodynamic stability
• Stable ventilatory status
• Changes in mental state
• Progression or deterioration of
ventilatory distress
• Signs of increased work of breathing
4. Management of the Patient that Does Not Tolerate the SBT
4.1. Ventilatory Muscle Rest
Patients that fail the first SBT should receive MV again and remain at least 24 hours using a ventilation mode that makes them comfortable according to the clinical evaluation.

70 Current Respiratory Medicine Reviews, 2012, Vol. 8, No. 1 Johnston and da Silva
During this time, the possible causes of intolerance to the SBT should be reassessed and treated. The main physiological disorder in ventilatory insufficiency seems to be the imbalance between the ventilatory system load and the capacity to respond to this demand. Evidence suggests that the patient should be kept on ventilatory support with the same parameters used before the SBT for 24 hours after extubation failure and before a new weaning attempt. The purpose of this rest is the functional recovery of the ventilatory system and the resolution of other causes that might have led to ventilatory muscle fatigue (use of sedation, electrolytic changes, infection). In patients that develop muscle fatigue, recovery does not occur in less than 24 hours. For adult patients [10] the use of the SBT using a T-piece twice a day did not benefit patients when compared with its performance only once a day.
4.2. New Attempt After 24 Hours
If the patient remains eligible for extubation, and if the causes of intolerance were reviewed, a new SBT should be performed after 24 hours. Evidence shows that the daily performance of SBT shortens the duration of MV when compared with protocols in which the SBT is not performed daily for adult patients [10].
4.3. Management of the Patient that Tolerates the SBT
When the patient is successful in the SBT may be are eligible or not to extubation. The following factors should be confirmed: reversal or resolution of acute event that led to MV; PaO
2 60 mmHg, FiO
2 0.40% and PEEP 5 to 8
cmH2O; hemodynamic evaluation that shows signs of good
tissue perfusion, weaning of vasopressor drugs (low and stable doses are acceptable) and no coronary insufficiency or arrhythmias with hemodynamic effects; capacity to initiate respiratory effort; good mental status; presence of cough reflex; acid-base balance; a restritive fluid balance; normal
serum electrolyte concentrations (K, Ca, Mg, P); no upcoming surgery.
5. Mechanical Ventilation Weaning Protocols
Few studies [28-30] analyzed weaning protocols in pediatrics, and none of them reported satisfactory results when compared with standard weaning procedures (Table 2). However, some studies [29-32] reported on improved PICU care when extubation protocols were adopted. These studies used similar criteria to assess the possibility of extubation in pediatrics (Table 3).
The most common approach to weaning infants and children is gradual reduction of ventilatory support [33]. Weaning with intermittent mandatory ventilation (IMV) or synchronized IMV (SIMV) occurs by reducing the ventilatory rate. With pressure support ventilation (PSV), the inspiratory pressure is initially set to provide the required support and then reduced gradually. PSV provides a progressive unloading of inspiratory muscles compared with SIMV. PSV is often combined with IMV/SIMV during weaning. Volume support and volume-assured pressure support are special forms of PSV available in certain ventilators that guarantee a minimal VT per assisted breath. Weaning with volume support is semiautomatic, and the PSV level required to maintain a certain VT is reduced automatically as respiratory mechanics improves. Extubation occurs at a low level of ventilatory support or after an extubation readiness test. Other authors recommend moderate amounts of ventilatory support to provide some rest to the patient’s respiratory muscles and the performance of a daily SBT. MV is discontinued if the SBT is well tolerated [14, 34]. This approach has been more commonly used to wean adult patients than children [33].
Duration of MV is known to be an independent risk factor for morbidity in patients requiring respiratory support [35]. In an attempt to shorten the duration of MV and
Table 2. Studies that Evaluated Weaning Protocols in Pediatrics
Randomized
Controlled
Trials
Intervention Number of
Patients
Type of
PICU
Inclusion
Criteria
Mechanical Ventilation
Duration
(Intervention vs Standard
Care)
p
Extubation
Success/Failure
Rate
(Intervention vs
Standard Care)
[%(n)]
p
Schultz et al., 2001
Protocol vs medical decision
223 One PICU
Mechanical ventilation
Total MV duration
-Mean 23.8 x 27.5 (days)
-Median 47.1 x 117.9 (hours)
Weaning duration
-Mean 0.8 x 10 (days)
-Median 5.9 x 25.2 (hours)
0.26
< 0.001
Extubation failure
4 x 2
Not significant
Randolph et al., 2002
Standard care vs Protocols
182
10 PICUs
Multiple
centers
Mechanical ventilation
duration 24 h
Result mean and median values
Not statistically significant
0.75
PSV extubation failure 15%
Volume support
24%
Standard care17%
0.44
Keogh et al., 2003
Standard care vs Protocols
220 One PICU
Age < 18 years
Total MV duration (hours)
-Median 47 x 31.2
Weaning duration
-Mean 6.1 x 6.3 (days)
-Median 20 x 18.5 (hours)
0.07
0.43
Reintubation rate
3.5 (4) x 4.6 (5) 0.37

Weaning and Extubation in Pediatrics Current Respiratory Medicine Reviews, 2012, Vol. 8, No. 1 71
decrease morbidity, weaning protocols have been implemented in adult ICU. A number of studies with adults demonstrated that implementation of a standardized ventilator weaning protocol shortens duration of MV without adversely affecting patient care [35-38].
Results from pediatric trials implementing ventilator weaning protocols are less promising. In a large multicenter study conducted by the PALISI investigators, no difference was found between groups randomized to either physician directed PSV weaning, automated ventilator-adjusted volume support protocol, or no protocol [29]. In addition to evaluating the impact of weaning protocols on the duration of MV, their study also examined the performance of a set of extubation readiness criteria and the relationship between sedative use and respiratory outcomes. The study was stopped because of lack of apparent differences between the three groups after 182 children were recruited (extubation failure rate was 19% with extubation readiness criteria vs 17% using physician judgment). Increased sedative use during the first 24 hours of weaning was an important predictor of weaning duration (P < .001) and weaning failure (P = .04) in that study. The limited adherence to protocol (66% compliance) reported in that study may have reduced the likelihood of detecting a possible beneficial effect. Shultz et al. [30] demonstrated shorter weaning times when they randomized pediatric patients to protocol-directed MV weaning versus physician-directed weaning, but, surprisingly, changes in total ventilator time and time to extubation were not statistically significant (10 versus 0.8 h). Restrepo et al. [38] also retrospectively reported shorter weaning times and shorter time to spontaneous modes of ventilation in the protocol group as compared to traditional
physician-directed weaning, but there was again no difference in overall ventilatory duration.
Recently, a weaning protocol integrated into a ventilator in closed loop was adapted for the weaning process [39, 40]. A multicenter randomized trial that included 144 adults and comparing a closed-loop protocol to a local weaning protocol found a significant reduction of 4.5 days in total mechanical ventilation duration [41]. However, a subsequent single-center study using the same computerized system was unable to confirm the superiority of this approach [42]. A pilot study conducted in pediatric patients showed that the computerized decision making seems reliable in a small population [43]. The authors showed that ventilation duration decreased from 5.1 ± 4.2 days in the closed-loop group to 6.7 ± 11.5 days in the clinician decision group (p = 0.33). The closed-loop protocol is designed to accelerate discontinuation of mechanical ventilation by modifying the pressure support level more frequently than a physician does [43]. It closely adjusts the level of pressure support by assessing its effects on the child’s breathing pattern. The closed-loop protocol uses three variables to automatically control the level of assistance: respiratory rate, VT, and partial end-tidal CO2 pressure (PetCO2). Respiratory rate, which seems to reflect how well the respiratory muscles adapt to the workload, is the main variable used. VT and PetCO2 are additional variables used to improve safety [43]. Further studies are required to assess the impact of this novel therapeutic strategy on the length of mechanical ventilation.
In an attempt to circumvent barriers to the effective use of protocols, some have implemented physician-independent treatment algorithms run by nurses and respiratory therapists. Current evidence suggests that respiratory therapist-driven
Table 3. Criteria for Decision to Extubate in Pediatrics
Authors Ventilatory Criteria General Criteria
Schultz et al., 2001
• FiO2 = 60% ( for SaO2 90-92%)
• PEEP = 5 cmH2O
• RR= 1.5 of predicted
• Expiratory VT < 2x predicted VT
• pH = 7.25
• No general criteria
Durand et al., 2001
• FiO2 = 40% or PaO2/ FiO2 > 150
• PEEP = 5 cmH2O
• PIP = 30 cmH2O
• No vasoactive agent
• Adequate mental state
• No sedation, no fever
• Correction of metabolic changes
• Baseline disease under control
Farias et al., 2002 • FiO2 = 40% and PaO2 > 60 mmHg
• PEEP = 5 cmH2O
• No vasoactive agent
• Adequate mental state
• No sedation, temperature < 38.5oC
• Hemoglobin >10g/dL
• Baseline disease under control
Randolph et al., 2002
• FiO2 = 40% and SaO2 = 95%
• PEEP = 7cmH2O
• pH = 7.32-7.47
• Spontaneous breathing
• Efficient cough
• No changes in mechanical ventilation parameter in 24 h
• No vasoactive agent
• Adequate mental state
• No sedation, temperature < 38.5oC
• Hemoglobin >10g/dL
• Baseline disease under control
• No surgery in the next 24 h

72 Current Respiratory Medicine Reviews, 2012, Vol. 8, No. 1 Johnston and da Silva
protocols for ventilator management and weaning results in shorter duration of mechanical ventilation compared with traditional physician-directed weaning, reduced costs, and improved resource allocation. In one study, respiratory therapist-driven protocols in patients requiring prolonged mechanical ventilation reduced median weaning time by almost 12 days [44]. Ely et al. [35] randomized 300 mechanically ventilated medical patients to either standard care or an intervention strategy that combined readiness testing with a daily screen. The intervention strategy resulted in significant decrease in weaning time, duration of mechanical ventilation, complication rate, and ICU costs; no differences were noted in ICU or hospital length of stay, hospital costs, or mortality. Two randomized clinical trials in medical and surgical ICUs found that a protocol directed by a respiratory care practitioner–ICU nurse also shortened mechanical ventilation duration [36, 37]. The superior outcomes obtained with nonphysician run protocols for mechanical ventilation has led a collective task force of pulmonary and critical care experts, facilitated by the American College of Chest Physicians (ACCP), the American Association for Respiratory Care, and the American College of Critical Care Medicine, to recommend that ICUs develop and implement respiratory-care protocols designed for nonphysician health care professionals [2, 35]. In a neonatal population study, Hermeto et al. [45] showed the implementation of a registered respiratory therapist-driven protocol had a positive impact on ventilatory outcomes of premature infants, without adverse effects. The major findings were shortening of time for the first extubation attempt, decreased rate of failure extubation (from 40% to 20%), and decreased duration under MV (from 5.0 to 1.2 days).
The success of non-invasive ventilation (NIV) for acute respiratory failure and its recent successful application in facilitating weaning has led to renewed interest in application to prevent extubation failure. Post-extubation NIV can be used in three ways: (1) as an adjunct to weaning patients from CMV by early extubation directly to NIV, (2) as a preventive application of NIV to higher-risk patients who were extubated at the time they fulfilled standard extubation criteria; or (3) as a curative or rescue application of NIV to patients who develop acute respiratory failure after having been extubated according to standard criteria. Two recently published randomized clinical trials indicate that immediate postextubation application of NIV in adults at highest risk for extubation failure is effective in preventing reintubation and may reduce mortality [46, 47]. Pediatric studies about NIV use after extubation in post-cardiac surgery patients [48, 49] showed that NIV was effective and safe in this population. Recently, Mayordomo-Colunga et al. [50] found that post-extubation NIV seems to be useful in avoiding reintubation in high-risk children when applied immediately after extubation. NIV was more likely to fail when acute respiratory failure has already developed, when respiratory rate at 6 hours did not decrease and if oxygen requirements increased.
Observational and randomized trials demonstrate that protocols directed at minimizing the use of sedative infusions shorten the weaning process. Specifically, approaches intended to avoid oversedation by limiting the use of continuous infusions either through sedation
assessment scoring [51, 52] or by daily cessation of sedative infusions [53] decrease duration of mechanical ventilation and duration of ICU stay. Daily sedation interruption (DSI) has been proposed as an adjunct to titrating continuous sedative infusions to a defined sedation score or level [53]. When using DSI continuous sedative infusions are interrupted each day and patients are allowed to wake up. Patients can then be assessed for neurological recovery and readiness for extubation, or re-sedated if required. Girard et al. [54] recently published the results of a trial that employed a ‘wake up and breathe’ strategy in adults. Patients randomized to a daily awakening trial followed by an SBT (versus SBT alone) experienced increased free-time ventilator, decreased time in coma, decreased ICU and hospital length of stay, and improved survival at 1 year.
Although DSI appears to be a simple and cost-efficient technique, there are risks to the patient. These risks include rebound agitation, pain, self-extubation or removal of invasive lines and possible adverse psychological sequelae (such as depression and post-traumatic stress disorder) related to the patient’s increased awareness of the ICU environment and their own life-threatening situation [55]. Despite the acknowledged risks, DSI has been incorporated into the Society of Critical Care Medicine sedation practice guidelines [56] and, more recently, into the ‘ICU Care Bundles’ to prevent ventilator-associated pneumonia [57]. There is little evidence on use of sedation protocols in the pediatric intensive care (PICU). One study evaluated a sedation and analgesic protocol in 10 PICU patients [58]. Patients received more sedation while on the protocol and the nurses found the protocol easy to use. A recent COMFORT scale study in PICU patients showed significant decreases of duration of mechanical ventilation and doses of sedatives in 21 patients managed with the use of a sedation protocol as compared with controls [59]. There is at present no validated instrument to diagnose and monitor pediatric delirium in the ICU setting by nonpsychiatrically trained clinicians. The lack of age-appropriate diagnostic tools in children results in a knowledge deficit regarding the incidence, clinical presentation, response to treatment, and consequence of pediatric delirium in the ICU.
Potential extubation failure should also be considered when evaluating MV weaning. Many studies have described extubation practices in pediatrics, most of them conducted in a single PICU [7-9, 32, 45, 60-66]. Only two were conducted in multiple centers [29, 67]. Most studies reporting clinical outcomes suggest that a failed extubation rate < 10% is the norm, as supported by the study conducted by Kurachek [7, 67]. Higher rates of failed extubation are reported in studies that used a readiness trial - about 14%–20% according to Randolph [29]. These differences may be, in part, caused by the inclusion of patients extubated in less than 24–48 h. Fontela et al. [68] found that younger age, mean oxygenation index (OI > 5), use of inotropic agents and duration of MV (> 15 days) were variables associated with an increased risk of extubation failure. The authors also suggested that prolonged treatment with sedative and analgesic drugs during MV might contribute significantly to the extubation failure rate [68]. Baisch et al. [64] reported a 4.1% extubation failure rate within 48h in 3.193 infants and children. Extubation failures occurred in younger patients (median age of 6.5 months vs 21.3 months), with longer

Weaning and Extubation in Pediatrics Current Respiratory Medicine Reviews, 2012, Vol. 8, No. 1 73
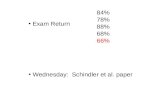
durations of intubation, PICU and hospital stays, but no difference in mortality. One algorithm utilized for us in the unit (Fig. 1) is demonstrated.
6. Extubation Predictive Factors
The ideal moment for extubation of children receiving MV remains subjective, and may be based on weaning protocols, ventilatory indices, or both. Extensive efforts have been made to identify predictors of extubation success in pediatrics [65]. Several criteria, such as minute ventilation (VE < 10 L/min), maximal inspiratory pressure (MIP) ! 50 cmH2O, RSBI, and load/force balance (LFB), have been used to make decisions about the ideal time to extubate adult and pediatric patients [4, 13, 69]. However, studies about the use of some of these extubation predictors in pediatrics and neonatology, particularly RSBI, showed inconclusive results [7-9, 65, 70]. Parameters such as VT, VE, RSBI, vital capacity and MIP, are often used in ICUs to support the decision to extubate. The following parameters may be used
to support the decision to extubate: respiratory rate (RR in incursion per minute- ipm) according to age (20-60 ipm < 6 months; 15-45 < 2 years; 15-40 < 5 years; 10-35 " 5 years); VT of 6-8ml/kg; RSBI (RR/ VT adjusted to weight) < 6.5 ipm/ml/Kg; vital capacity > 10-15 ml/kg; MIP " 30 cmH2O. Other parameters may also be used as aids in MV weaning and in making the decision about extubation, such as: occlusion pressure (P 0.1 or P 100), work of breathing (WOB = ! pressure x volume), esophageal (Pe) and transdiaphragmatic pressure, electromyographic activity of diaphragm, physiological dead space, gastric tonometry (PgCO2 –PaCO2 gradient), and others. However, these parameters demand the use of special measurement techniques, which are not often found routinely for bedside examinations, and are indicated for specific cases (when MV weaning is complicated or in cases of many weaning failures). The parameters that evaluated the capacity of airway protection [71] are easily observed and provide practical and
Fig. (1). Weaning and extubation algorithm.
Intubation and Beginning of Mechanical Ventilation
Beginning of the weaning process• Reduction of the mechanical ventilation parameters• Application of assisted ventilation modes (e.g.: SIMV, PAV)
Spontaneous breathing trial (SBT)• Time: 20-30 minutes • Ventilatory mode: PSV or CPAP of 7-10
cmH2O, depending on the tube diameter
Evaluation of the extubation predictive indexes• Choose one index to evaluate load/force and another to assess respiratory muscle resistance. E.g.: PIM e IRS
Are the indexes among the normal range for age and underlying disease?
Yes No
• Re-evaluate the patient• Perform mechanical ventilation weaning gradually
(return to the ventilation parameters of the assisted ventilation mode used before SBT)• Take care not to induce diaphragm exacerbated
contractions and let the patient fatigue.
Did the patient manage to sustain VE and TV with a SpO2 ≥ 92% and respiratory rate among acceptable
values for the age during SBT?
Yes No
Extubation feasibility• Controlled underlying disease• No vasoactive drug• Adequate conscience level• Approved in SBT• FiO2 < 40% with SpO2 ≥ 92% or PaO2/FiO2 > 150• PEEP = 5 cmH2O and PIP ≤ 30 cmH2O• pH – 7,32-7,47• Hemoglobin > 10g/dL• Force and respiratory muscle resistance appropriated for age and underlying
disease (Pimax ≥ 50 cmH2O and RSBI ≤ 6,5 cpm/ml/Kg• Effective cough
No
Yes Extubate

74 Current Respiratory Medicine Reviews, 2012, Vol. 8, No. 1 Johnston and da Silva
rapid support measured at bedside weaning and extubation decisions: maximum expiratory pressure (MEP), peak expiratory flow rate, cough reflex (response to stimulation with an aspiration catheter); cough efficacy; secretion volume; frequency of tracheal aspiration, and Glasgow coma score.
Some indices may be used to evaluate the progression of MV weaning and as predictors of extubation success. The indices listed below are easily measured by the bedside and have been used frequently in adult, pediatric and neonatal ICUs in several hospitals around the world: SBT [3, 15]; MIP, P0.1/P100 [2]; IP/MIP [11]; association of IP/MIP and RSBI [11]; RSBI = RR/ VT [71, 72]; RSBI = (RR/ VT /weight [4]; RSBI times P0.1 (4, 22); CROP = (Cdyn x MIP x (PaO2/PAO2))/RR) (2); Pressure-time product: PTP= (PTP/respiratory cycle time)/MIP (4, 12); Tension-time index 1 (TT1) and tension-time index 2 (TT2) [4, 12, 73, 74]; Simplified weaning index (SWI) [75].
6.1. Peak Maximum Inspiratory Pressure (MIP), P0.1/P100
Ratio, Combined PI/MIP and RSBI
The clinical progression of pulmonary disease is affected by acute or chronic inflammation of the airways and by nosocomial infections, to which children and infants receiving MV are exposed. These infections predispose to gas trapping and changes in compliance of the ventilatory system, with an increase of WOB and a decrease in the strength of inspiratory muscles [76]. The strength of ventilatory muscles may be measured using a compound gauge, a simple and practical noninvasive method. This test may be performed with intubated or tracheotomized patients ventilating spontaneously. To perform it in pediatric patients receiving ventilatory support, the gauge should be connected to the endotracheal tube or the tracheotomy, and the head of the bed should be raised to 30 degrees. The operator should wait until the child makes three inspiratory and three expiratory efforts. The highest of the three values should be recorded for each ventilatory phase (inspiratory and expiratory). The test should be performed in 15 to 45 seconds. The values recorded should be compared with normal parameters using equations for predicted values [77].
The first number seen in the gauge, in one second is called occlusion pressure (P1.0) and can be used to calculate P1.0 /P100. The combination of mean airway pressure [MAP={IP–PEEP)x[IT/(ET+IT]}+PEEP], MIP and RSBI is called load/strength ratio [LSR=15x(3xMAP)/(MIP+ 0.03)xRSBI-5]. It was created and first used for adult patients by Vassilakopoulos T et al. (2006) [11] and for pediatric patients by Johnston C et al. [13].
6.2. Rapid Shallow Breathing Index (RSBI) in Pediatrics and the RSBI-P1.0 Product
MV weaning failure is the result of the imbalance between the capacity of the muscles involved in ventilatory mechanics and the ventilatory demand. RR/VT adjusted to weight in kilograms, that is, the pediatric RSBI [4] during spontaneous ventilation increases when there is such imbalance. The RSBI is one of the indices that can be used to identify which patients will have a successful extubation [4, 5, 9, 13, 32].
Previous clinical studies [5, 72, 78-80] with adult patients showed that the RSBI has excellent sensitivity and moderate specificity. Specificity for postoperative patients is similar to that found for clinical patients.
The capacity of the RSBI and the RSBI-P0.1 product to predict extubation success or failure has been analyzed for adult, pediatric and neonatal patients [4, 23, 32, 79-81]. Studies conducted with pediatric and neonatal populations revealed moderate sensitivity and low specificity to predict failure or success using the RSBI [4, 13, 23, 32, 81]. Some hypotheses have been raised to explain this fact, such as the heterogeneity of samples (age, weight, variable vital signs, baseline disease), the type of study design, the characteristics that are inherent to tracheal intubation (endotracheal intubation duration, diameter of endotracheal tube, number of intubation attempts, use of endotracheal tube cuf) and MV features (MV duration, ventilatory mode, patient-ventilator asynchrony).
Most studies with pediatric patients, which showed that the RSBI is not a good extubation predictor, were conducted with patients of different age groups, with different diagnosis and different endotracheal intubation durations. However, when demonstrating that factors such as greater gestational age, postnatal age, intubation time, and birth weight were associated with extubation success or failure [4, 9, 32, 61, 82-85], Baumeister BL et al. [7] adjusted RSBI and dynamic compliance to infant weight. In their study, a 19% extubation failure rate was found at 24 hours. Khan N et al. (1996) [8] studied 208 children and used the same method to find a 10% extubation failure rate after 48 hours. Since then, a cut-off point for the RSBI lower than or equal to 6.5 ipm/ml/kg has been accepted to predict extubation success in pediatric patients, but its specificity is low (70%) [32].
6.3. CROP Index
This index uses data about dynamic compliance (Cdyn), RR, alveolar-arterial oxygen gradient (PaO2/PAO2) and MIP [68]. Values greater than 13 ml/cmH2O/ipm are predictive of extubation success for adult patients (81% sensitivity and 57% specificity) [71]. In pediatrics, the calculated CROP value should be adjusted to weight in kilograms, and the cut-off point for extubation success is 0.15 ml/kg/cmH2O/ipm [8].
6.4. Pressure-Time Product (PTP)
After VT and inspiratory time are defined, the intrinsic (elastic and frictional) properties of the ventilatory system define the pressure generated by the ventilatory effort, such as the WOB [85]. A cross-sectional study [86] measured the PTP for 31 adult patients with chronic obstructive pulmonary disease; 14 patients that tolerated the SBT and were extubated had PTP lower than 50 cmH2O/Kg/s. The PTP predicted extubation failure in that sample (P=0.001). Another cross-sectional study with 90 pediatric patients [13] with a diagnosis of acute viral bronchiolitis detected a cut-off point of 0.50 cmH2O/kg/s for PTP as a predictor of extubation success, with 94% sensitivity and 100% specificity according to ROC analysis. In the study conducted by Noizet et al. (2005) [4], extubation success was found for patients with PTP 0.08 cmH2O/kg/s. This index has not been studied in neonatology so far.

Weaning and Extubation in Pediatrics Current Respiratory Medicine Reviews, 2012, Vol. 8, No. 1 75
6.5. Tension-Time Index (TTI)
Two formulas can be used to calculate TTI (TTI1 and TTI2). MIP, inspiratory time and respiratory cycle time (RCT) are used to calculate TTI1 [73, 74]. In pediatrics, the cut-off point to predict extubation success is 0.02cmH2O/ml/min [4]. MAP, MIP, inspiratory time and RCT should be used to calculate TTI2 [12]. Noizet et al. [4] found that values below the cut-off point of 0.05 cmH2O/ml/min were predictive of extubation success in a general sample of pediatric patients.
6.6. Simplified Weaning Index (SWI)
The SWI takes into consideration the resistance of ventilatory muscles and the capacity to maintain adequate gas exchanges. This index is a combination of the modified PTP [MPTP=[(IT/RCT)x(IPxVT)]/(spontaneous VT/MIP)] and parameters that evaluate the efficacy of gas exchanges [GEE = (VE x PACO2)/ (spontaneous VT x 40)]. The SWI has been studied in only 38 adult patients with chronic obstructive pulmonary disease. Results showed a trend towards extubation failure for patients with greater SWI values, but sensitivity and specificity to predict extubation failure were low [75].
7. Air Leak Test
Upper airway obstruction has been reported to be the cause of up to 37% of failed extubations in children [33]. The air leak test (ALT) is the minimum air pressure (usually < 20–25 cm H2O) required to produce an audible rush of air around the endotracheal tube when auscultated by a stethoscope placed directly over the larynx. It is commonly used to predict upper airway obstruction after extubation [33]. This test is commonly performed to detect upper airway swelling that may lead to postextubation stridor or upper airway obstruction. In a survey of pediatric critical care fellowship directors, 76% of the physicians routinely used this test prior to extubation, 95% reported that they would delay extubation if the ALT was 30 cmH2O or greater, and 60% would delay extubation to administer steroids [87].
The ALT has proven to be a sensitive predictor of postextubation complications in patients with identified upper airway pathologies, such as croup, airway trauma, or postsurgical airway reconstruction [88]. However, the predictive ability of the ALT is limited when applied to the general population. Mhanna et al. [89] demonstrated that a leak test of < 20 mmHg (27.2 cmH2O) was better at predicting stridor in children older than 7 years of age than in younger patients, but neither case had very good sensitivity. In a prospective, blinded study of 50 pediatric patients, Wratney et al. [88] analyzed the change in airway leak as measured at the time of intubation and extubation as a predictor of extubation outcome. They found that measuring the leak serially over time was a better predictor of extubation success than of extubation failure (sensitivity 76%; specificity 44%; PPV 83%; NPV 33%) [88]. Recently, Wratney et al. [90] demonstrated that an ALT pressure 30 cmH2O before extubation or for the duration of MV was common and did not predict an increased risk of extubation failure (NPV 18%). The authors concluded that pediatric patients that are clinically identified as candidates for an
extubation trial but do not have an endotracheal tube air leak may successfully tolerate removal of the endotracheal tube.
Based on available data, it would appear that the presence of an audible leak (to the ear, not the stethoscope) can be heard at < 25 cmH2O in a patient with the head in neutral position; this is probably good news. However, extubation should not be delayed if the test is negative and all other conditions for extubation are favorable [33].
Prophylactic systemic corticosteroids are frequently administered in an attempt to minimize postextubation stridor. In a published meta-analysis, Markovitz and Randolph [91] demonstrated a reduced incidence of postextubation stridor in both neonatal and pediatric patients treated with systemic corticosteroids in the peri-extubation period. There was also a trend towards decreased rates of reintubation in the corticosteroid groups, which was not statistically significant. The two pediatric trials included in this meta-analysis used dexamethasone 0.5 mg/kg (up to 10 mg) 6 to 12 h before extubation and then every 6 h for six total doses; their findings showed discrepancies.
The Cochrane database system review found that use of corticosteroids to prevent or treat stridor after extubation has not proven effective for neonates or children. However, given the consistent trend towards beneficial effects, this intervention does merit further study, particularly for high risk children or neonates. In adults, multiple doses of corticosteroids begun 12-24 hours prior to extubation appear to be beneficial for patients with a high likelihood of postextubation stridor [92].
8. Net Fluid Balance
Volume overload frequently occurs during treatment of the systemic inflammatory response syndrome precipitated by severe infection, pancreatitis, major surgery, or other events. This extra volume will lead to decreased functional residual capacity of the lungs and alveolar collapse. This is associated with a ventilation/perfusion mismatch, which requires an increase in the PEEP to keep the alveoli opened and maintain good oxygenation. The mobilization of such fluid usually happens upon resolving the systemic inflation, and may be increased by diuretics. For the adult patient with acute respiratory distress syndrome, acute pulmonary edema or congestive heart failure, fluid restrictive management strategies have proven successful, leading to improved survival and a higher number of ventilator-free days [88]. The appropriate fluid management strategy for pediatric patient is still controversial.
Randolph et al. [93] assessed the effect of cumulative fluid intake minus output as a predictor of weaning duration and extubation outcome. The authors found that cumulative intake-output did not predict the duration of weaning or the extubation outcome. However, other studies showed that a decreased fluid balance was associated with higher survival rates among pediatric patients that had multiple-organ dysfunction [88].
9. Other Predictors
The following problems found in MV patients will affect either the capacity of or the demand on the respiratory

76 Current Respiratory Medicine Reviews, 2012, Vol. 8, No. 1 Johnston and da Silva
system. These include: hemodynamic instability, acid–base disorders, electrolyte disturbances, altered mental status, and decreased respiratory muscle function. Electrolyte disturbances during weaning have been studied extensively. It has been shown that hypophosphatemia, hypocalcemia, hypomagnesemia, and hypokalemia reduce muscle contractility and affect weaning. These disturbances must be corrected before weaning attempts [94].
Neurological deficit secondary to brain injury may impose quite a challenge as to the optimal time for weaning and/or extubation. Namem et al. [95] found that patients with successful extubation had a GCS score 8. A GCS 10 has been recently found to be a prerequisite to successful extubation [96].
Recent studies with adult patients have found that secretion burden and cough strength are important predictors of extubation outcome [97, 98]. Khamiees et al. [97] evaluated the cough strength on command (0 to 5) and amount of endotracheal secretions (none to abundant) in patients passing SBT. Patients were then asked to cough onto a white card test. Patients with weak (grade 0 to 2) coughs and abundant secretions were more likely to fail extubation. Negative white card test also predicted failed extubation.
Fatigue of patients undergoing weaning from MV is a major factor in failure to wean. Several studies using electromyogram (EMG) diagnosis showed that diaphragmatic fatigue occurs in the first day in all patients on MV, and those that recovered were extubated successfully [94]. The patients that continued to feel fatigued needed reintubation. It is not known how much diaphragmatic strength is needed to sustain spontaneous breathing, or how long the resting period should be to recover from diaphragmatic fatigue. It is possible that one day of rest, fully supported by MV, may be enough for diaphragmatic recovery [94].
Malnutrition causes reduction of muscle mass, endurance, and muscle strength. It also causes decreased immunity, predisposing the patient to further infections. Nutrition repletion in critically ill patients resulted in improved respiratory forces and easier weaning [94].
CONCLUSION
The current pediatric literature shows that the science of ventilator weaning and extubation remains undetermined. Indeed, no optimal weaning method has resulted in more rapid and successful extubation. Protocol-based approaches to weaning could have potential benefits in advancing readiness to extubate, but have not shown significant outcome differences so far. After the analysis of clinical markers of extubation success, we found that no specific physiological indicator has predicted extubation success in children. However, a daily trial of readiness to extubate is the most effective technique to determine likelihood of success. Upper airway obstruction is the primary cause of extubation failure in most pediatric studies. Therefore, efforts focused on decreasing airway edema before extubation should be considered. Corticosteroids seem to be beneficial for infants and children, but definitive evidence of efficacy is lacking.
REFERENCES
[1] Meade M, Guyatt G, Sinuff T, et al. Trials comparing alternative
weaning modes and discontinuation assessments. Chest 2001; 120(6 Suppl): 425S-37S.
[2] MacIntyre NR, Cook DJ, Ely EW, et al. Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task
force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American
College of Critical Care Medicine. Chest 2001; 120(6 Suppl): 375S-95S.
[3] Ely EW, Baker AM, Dunagan DP, et al. Effect on the duration of mechanical ventilation of identifying patients capable of breathing
spontaneously. N Engl J Med 1996; 335(25): 1864-9. [4] Noizet O, Leclerc F, Sadik A, et al. Does taking endurance into
account improve the prediction of weaning outcome in mechanically ventilated children? Crit Care 2005; 9(6): R798-807.
[5] Tobin MJ, Perez W, Guenther SM, et al. The pattern of breathing during successful and unsuccessful trials of weaning from
mechanical ventilation. Am Rev Respir Dis 1986; 134(6): 1111-8. [6] Balsan MJ, Jones JG, Watchko JF, Guthrie RD. Measurements of
pulmonary mechanics prior to the elective extubation of neonates. Pediatr Pulmonol 1990; 9(4): 238-43.
[7] Baumeister BL, el-Khatib M, Smith PG, Blumer JL. Evaluation of predictors of weaning from mechanical ventilation in pediatric
patients. Pediatr Pulmonol 1997; 24(5): 344-52. [8] Khan N, Brown A, Venkataraman ST. Predictors of extubation
success and failure in mechanically ventilated infants and children. Crit Care Med 1996; 24(9): 1568-79.
[9] Farias JA, Alia I, Esteban A, Golubicki AN, Olazarri FA. Weaning from mechanical ventilation in pediatric intensive care patients.
Intensive Care Med 1998; 24(10): 1070-5. [10] Esteban A, Frutos F, Tobin MJ, et al. A comparison of four
methods of weaning patients from mechanical ventilation. Spanish Lung Failure Collaborative Group. N Engl J Med 1995; 332(6):
345-50. [11] Vassilakopoulos T, Routsi C, Sotiropoulou C, et al. The
combination of the load/force balance and the frequency/tidal volume can predict weaning outcome. Intensive Care Med 2006;
32(5): 684-91. [12] Vassilakopoulos T, Zakynthinos S, Roussos C. The tension-time
index and the frequency/tidal volume ratio are the major pathophysiologic determinants of weaning failure and success. Am
J Respir Crit Care Med 1998; 158(2): 378-85. [13] Johnston C, de Carvalho WB, Piva J, Garcia PC, Fonseca MC. Risk
factors for extubation failure in infants with severe acute bronchiolitis. Respir Care 2010; 55(3): 328-333.
[14] Brochard L, Rauss A, Benito S, et al. Comparison of three methods of gradual withdrawal from ventilatory support during weaning
from mechanical ventilation. Am J Respir Crit Care Med 1994; 150(4): 896-903.
[15] Esteban A, Alia I, Gordo F, et al. Extubation outcome after spontaneous breathing trials with T-tube or pressure support
ventilation. The Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med 1997; 156(2 Pt 1): 459-65.
[16] Haberthur C, Mols G, Elsasser S, Bingisser R, Stocker R, Guttmann J. Extubation after breathing trials with automatic tube
compensation, T-tube, or pressure support ventilation. Acta Anaesthesiol Scand 2002; 46(8): 973-9.
[17] Carvalho W, Hirschheimer M, Matsumoto T. Terapia Intensiva Pediátrica 3a ed. Rio de Janeiro: Editora Atheneu; 2006.
[18] Esteban A, Alia I. Clinical management of weaning from mechanical ventilation. Intensive Care Med 1998; 24(10): 999-
1008. [19] Perren A, Domenighetti G, Mauri S, Genini F, Vizzardi N.
Protocol-directed weaning from mechanical ventilation: clinical outcome in patients randomized for a 30-min or 120-min trial with
pressure support ventilation. Intensive Care Med 2002; 28(8): 1058-63.
[20] Foronda FK, Troster EJ, Farias JA, et al. The impact of daily evaluation and spontaneous breathing test on the duration of
pediatric mechanical ventilation: A randomized controlled trial. Crit Care Med 2011; 39(11): 2526-33.
[21] Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J 1974; 2(5920):
656-9.

Weaning and Extubation in Pediatrics Current Respiratory Medicine Reviews, 2012, Vol. 8, No. 1 77
[22] Sasson C, Mahutte C. Airway occlusion pressure and breathing
pattern as predictors of weaning outcome. Am Rev Respir Dis 1993; 148: 860-6.
[23] Szymankiewicz M, Vidyasagar D, Gadzinowski J. Predictors of successful extubation of preterm low-birth-weight infants with
respiratory distress syndrome. Pediatr Crit Care Med 2005; 6(1): 44-9.
[24] Matic I, Majeric-Kogler V. Comparison of pressure support and T-tube weaning from mechanical ventilation: randomized prospective
study. Croat Med J 2004; 45(2): 162-6. [25] Elrazek EA. Randomized prospective crossover study of biphasic
intermittent positive airway pressure ventilation (BIPAP) versus pressure support ventilation (PSV) in surgical intensive care
patients. Middle East J Anesthesiol. 2004; 17(6): 1009-21. [26] Grasso S, Puntillo F, Mascia L, et al. Compensation for increase in
respiratory workload during mechanical ventilation. Pressure-support versus proportional-assist ventilation. Am J Respir Crit
Care Med 2000; 161(3 Pt 1): 819-26. [27] Brown BR. Understanding mechanical ventilation: indications for
and initiation of therapy. J Okla State Med Assoc 1994; 87(8): 353-7.
[28] Keogh S, Courtney M, Coyer F. Weaning from ventilation in paediatric intensive care: an intervention study. Intensive Crit Care
Nurs 2003; 19(4): 186-97. [29] Randolph AG, Wypij D, Venkataraman ST, et al. Effect of
mechanical ventilator weaning protocols on respiratory outcomes in infants and children: a randomized controlled trial. Jama 2002;
288(20): 2561-8. [30] Schultz TR, Lin RJ, Watzman HM, et al. Weaning children from
mechanical ventilation: a prospective randomized trial of protocol-directed versus physician-directed weaning. Respir Care 2001;
46(8): 772-82. [31] Durand DJ, Asselin JM, Hudak ML, et al. Early high-frequency
oscillatory ventilation versus synchronized intermittent mandatory ventilation in very low birth weight infants: a pilot study of two
ventilation protocols. J Perinatol 2001; 21(4): 221-9. [32] Farias JA, Alia I, Retta A, et al. An evaluation of extubation failure
predictors in mechanically ventilated infants and children. Intensive Care Med 2002; 28(6): 752-7.
[33] Newth CJ, Venkataraman S, Willson DF, et al. Weaning and extubation readiness in pediatric patients. Pediatr Crit Care Med
2009; 10(1): 1-11. [34] Ventilation with lower tidal volumes as compared with traditional
tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome
Network. N Engl J Med 2000; 342(18): 1301-8. [35] Ely EW, Meade MO, Haponik EF, et al. Mechanical ventilator
weaning protocols driven by nonphysician health-care professionals: evidence-based clinical practice guidelines. Chest
2001; 120(6 Suppl): 454S-63S. [36] Kollef MH, Shapiro SD, Silver P, et al. A randomized, controlled
trial of protocol-directed versus physician-directed weaning from mechanical ventilation. Crit Care Med 1997; 25(4): 567-74.
[37] Marelich GP, Murin S, Battistella F, Inciardi J, Vierra T, Roby M. Protocol weaning of mechanical ventilation in medical and surgical
patients by respiratory care practitioners and nurses: effect on weaning time and incidence of ventilator-associated pneumonia.
Chest 2000; 118(2): 459-67. [38] Restrepo RD, Fortenberry JD, Spainhour C, Stockwell J,
Goodfellow LT. Protocol-driven ventilator management in children: comparison to nonprotocol care. J Intensive Care Med
2004; 19(5): 274-84. [39] Dojat M, Harf A, Touchard D, Lemaire F, Brochard L. Clinical
evaluation of a computer-controlled pressure support mode. Am J Respir Crit Care Med 2000 ; 161(4 Pt 1): 1161-6
[40] Dojat M, Brochard L. Knowledge-based systems for automatic ventilatory management. Respir Care Clin N Am 2001; 7(3): 379-
96, viii. [41] 41 Lellouche F, Mancebo J, Jolliet P, Roeseler J, Schortgen F,
Dojat M, Cabello B, Bouadma L, Rodriguez P, Maggiore S, Reynaert M, Mersmann S, Brochard L. A multicenter randomized
trial of computer-driven protocolized weaning from mechanical ventilation. Am J Respir Crit Care Med 2006; 174(8): 894-900
[42] Rose L, Presneill JJ, Johnston L, Cade JF. A randomised, controlled trial of conventional versus automated weaning from
mechanical ventilation using SmartCare/PS. Intensive Care Med
2008; 34(10): 1788-95 [43] Jouvet P, Farges C, Hatzakis G, et al. Weaning children from
mechanical ventilation with a computer-driven system (closed-loop protocol): A pilot study. Pediatr Crit Care Med 2007; 8(5): 425-32
[44] DJ. Scheinhorn, D.C. Chao and M. Stearn-Hassenpflug, Wallace WA. Outcomes in post-ICU mechanical ventilation: a therapist-
implemented weaning protocol. Chest 2001; 119(1): 236-42 [45] Hermeto F, Bottino MN, Vaillancourt K, Sant'Anna GM.
Implementation of a Respiratory Therapist-Driven Protocol for Neonatal Ventilation: Impact on the Premature Population
Pediatrics 2009; 123(5): e907-16 [46] Ferrer M, Valencia M, Nicolas JM, Bernadich O, Badia JR, Torres
A. Early non-invasive ventilation averts extubation failure in patients at risk. a randomized trial. Am J Respir Crit Care Med
2006; 173(2): 164-70. [47] Nava SG, Gregoretti C, Fanfulla F, et al. Noninvasive ventilation to
prevent respiratory failure after extubation in high-risk patients. Crit Care Med 2005; 33(11): 2465-70.
[48] Stucki P, Perez MH, Scalfaro P, de HQ, Vermeulen F, Cotting J. Feasibility of non-invasive pressure support ventilation in infants
with respiratory failure after extubation: a pilot study. Intensive Care Med 2009; 35(9): 1623-7
[49] Pons OM, Piqueras MI, Segura MS, Balaguer AM, Palomeque R. Noninvasive ventilation after cardiac surgery. A prospective study.
An Pediatr (Barc) 2009; 71(1): 13-9. [50] Mayordomo-Colunga J, Medina A, Rey C, Concha A, Menéndez S,
Los Arcos M, García I. Non invasive ventilation after extubation in paediatric patients: a preliminary study. BMC Pediatr 2010; 10: 29
[51] Brook AD, Ahrens TS, Schaiff R, Prentice D, Sherman G, Shannon W, Kollef MH. Effect of a nursing-implemented sedation protocol
on the duration of mechanical ventilation. Crit Care Med 1999; 27(12): 2609-1552.
[52] Arias-Rivera S, Sanchez-Sanchez Mdel M, Santos-Diaz R, et al. Effect of a nursing-implemented sedation protocol on weaning
outcome. Crit Care Med 2008; 36(7): 2054-60 [53] Kress JP, Pohlman AS, O’Connor MF, Hall JB. Daily interruption
of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 2000; 342(20): 1471-7.
[54] Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically
ventilated patients in intensive care (awakening and breathing controlled trial): a randomized controlled trial. Lancet 2008;
371(9607): 126-34. [55] Heffner JE. A wake-up call in the intensive care unit. N Engl J Med
2000; 342(20): 1520-2 [56] Jacobi J, Fraser GL, Coursin DB, et al. Clinical practice guidelines
for the sustained use of sedatives and analgesics in the critically ill adult. Critical Care Medicine 2002; 30(1): 119-41.
[57] Fulbrook P, Mooney S. Review care bundles in critical care: a practical approach to evidence-based practice. Nurs Crit Care 2003;
8(6): 249-55. [58] Alexander E, Carnevale FA, Razack S. Evaluation of a sedation
protocol for intubated critically ill children Intensive Crit Care Nurs 2002; 18(5): 292-301
[59] Jin HS, Yum MS, Kim SL, et al. The efficacy of the COMFORT scale in assessing optimal sedation in critically ill children
requiring mechanical ventilation. J Korean Med Sci 2007; 22(4): 693-7.
[60] Harrison AM, Cox AC, Davis S, Piedmonte M, Drummond-Webb JJ, Mee RB. Failed extubation after cardiac surgery in young
children: Prevalence, pathogenesis, and risk factors. Pediatr Crit Care Med 2002; 3(2): 148-52.
[61] Thiagarajan RR, Bratton SL, Martin LD, Brogan TV, Taylor D. Predictors of successful extubation in children. Am J Respir Crit
Care Med 1999; 160(5 Pt 1): 1562-6. [62] Venkataraman ST, Khan N, Brown A. Validation of predictors of
extubation success and failure in mechanically ventilated infants and children. Crit Care Med 2000; 28(8): 2991-6.
[63] Hubble CL, Gentile MA, Tripp DS, Craig DM, Meliones JN, Cheifetz IM. Deadspace to tidal volume ratio predicts successful
extubation in infants and children. Crit Care Med 2000; 28(6): 2034-40.
[64] Baisch SD, Wheeler WB, Kurachek SC, Cornfield DN. Extubation failure in pediatric intensive care incidence and outcomes. Pediatr
Crit Care Med 2005; 6(3): 312-8.

78 Current Respiratory Medicine Reviews, 2012, Vol. 8, No. 1 Johnston and da Silva
[65] Edmunds S, Weiss I, Harrison R. Extubation failure in a large
pediatric ICU population. Chest 2001; 119(3): 897-900. [66] Chavez A, dela Cruz R, Zaritsky A. Spontaneous breathing trial
predicts successful extubation in infants and children. Pediatr Crit Care Med 2006; 7(4): 324-8.
[67] Kurachek SC, Newth CJ, Quasney MW, et al. Extubation failure in pediatric intensive care: a multiple-center study of risk factors and
outcomes. Crit Care Med 2003; 31(11): 2657-64. [68] Fontela PS, Piva JP, Garcia PC, Bered PL, Zilles K. Risk factors
for extubation failure in mechanically ventilated pediatric patients. Pediatr Crit Care Med 2005; 6(2): 166-70.
[69] Esteban A, Anzueto A, Alia I, et al. How is mechanical ventilation employed in the intensive care unit? An international utilization
review. Am J Respir Crit Care Med 2000; 161(5): 1450-8. [70] Martinez A, Seymour C, Nam M. Minute ventilation recovery time:
a predictor of extubation outcome. Chest 2003; 123(4): 1214-21. [71] Yang KL. Reproducibility of weaning parameters. A need for
standardization. Chest 1992; 102(6): 1829-32. [72] Yang KL, Tobin MJ. A prospective study of indexes predicting the
outcome of trials of weaning from mechanical ventilation. N Engl J Med 1991; 324(21): 1445-50.
[73] Gaultier C, Perret L, Boule M, Buvry A, Girard F. Occlusion pressure and breathing pattern in healthy children. Respir Physiol
1981; 46(1): 71-80. [74] Gaultier C. Tension-time index of inspiratory muscles in children.
Pediatr Pulmonol 1997; 23(5): 327-9. [75] Jabour ER, Rabil DM, Truwit JD, Rochester DF. Evaluation of a
new weaning index based on ventilatory endurance and the efficiency of gas exchange. Am Rev Respir Dis 1991; 144(3 Pt 1):
531-7. [76] Black LF, Hyatt RE. Maximal respiratory pressures: normal values
and relationship to age and sex. Am Rev Respir Dis 1969; 99(5): 696-702.
[77] Wilson SH, Cooke NT, Edwards RH, Spiro SG. Predicted normal values for maximal respiratory pressures in caucasian adults and
children. Thorax 1984; 39(7): 535-8. [78] Chatila W, Jacob B, Guaglionone D, Manthous CA. The unassisted
respiratory rate-tidal volume ratio accurately predicts weaning outcome. Am J Med 1996; 101(1): 61-7.
[79] Epstein S. Evaluation of the rapid shallow breathing index in the clinical setting. Am J Respir Crit Care Med 1995; 152: 545-9.
[80] Lee KH, Hui KP, Chan TB, Tan WC, Lim TK. Rapid shallow breathing (frequency-tidal volume ratio) did not predict extubation
outcome. Chest 1994; 105(2): 540-3. [81] Wilson BJ, Jr., Becker MA, Linton ME, Donn SM. Spontaneous
minute ventilation predicts readiness for extubation in mechanically ventilated preterm infants. J Perinatol 1998; 18(6 Pt
1): 436-9. [82] Dimitriou G, Greenough A, Endo A, Cherian S, Rafferty GF.
Prediction of extubation failure in preterm infants. Arch Dis Child Fetal Neonatal Ed 2002; 86(1): F32-5.
[83] Dimitriou G, Greenough A, Laubscher B. Lung volume
measurements immediately after extubation by prediction of "extubation failure" in premature infants. Pediatr Pulmonol 1996;
21(4): 250-4. [84] Dimitriou G, Greenough A. Computer assisted analysis of the chest
radiograph lung area and prediction of failure of extubation from mechanical ventilation in preterm neonates. Br J Radiol 2000;
73(866): 156-9. [85] Kavvadia V, Greenough A, Dimitriou G. Prediction of extubation
failure in preterm neonates. Eur J Pediatr 2000; 159(4): 227-31. [86] Jubran A. Monitoring patient mechanics during mechanical
ventilation. Crit Care Clin 1998; 14(4): 629-53, vi. [87] Foland JA, Super DM, Dahdah NS, Mhanna MJ. The use of the air
leak test and corticosteroids in intubated children: a survey of pediatric critical care fellowship directors. Respir Care 2002; 47(6):
662-6. [88] Wratney AT, Cheifetz IM. Extubation criteria in infants and
children. Respir Care Clin N Am 2006 Sep; 12(3): 469-81. [89] Martin RJ, Mhanna MJ, Haxhiu MA. The role of endogenous and
exogenous nitric oxide on airway function. Semin Perinatol 2002; 26(6): 432-8.
[90] Wratney AT, Benjamin DK, Jr., Slonim AD, He J, Hamel DS, Cheifetz IM. The endotracheal tube air leak test does not predict
extubation outcome in critically ill pediatric patients. Pediatr Crit Care Med 2008; 9(5): 490-6.
[91] Markovitz BP, Randolph AG. Corticosteroids for the prevention of reintubation and postextubation stridor in pediatric patients: A
meta-analysis. Pediatr Crit Care Med 2002; 3(3): 223-6. [92] Khemani RG, Randolph A, Markovitz B. Corticosteroids for the
prevention and treatment of post-extubation stridor in neonates, children and adults. Cochrane Database Syst Rev 2009(3):
CD001000. [93] Randolph AG, Forbes PW, Gedeit RG, et al. Cumulative fluid
intake minus output is not associated with ventilator weaning duration or extubation outcomes in children. Pediatr Crit Care Med
2005; 6(6): 642-7. [94] Eskandar N, Apostolakos MJ. Weaning from mechanical
ventilation. Crit Care Clin 2007; 23(2): 263-74. [95] Namen AM, Ely EW, Tatter SB, et al. Predictors of successful
extubation in neurosurgical patients. Am J Respir Crit Care Med 2001; 163(3 Pt 1): 658-64.
[96] Mokhlesi B, Tulaimat A, Gluckman TJ, Wang Y, Evans AT, Corbridge TC. Predicting extubation failure after successful
completion of a spontaneous breathing trial. Respir Care 2007; 52(12): 1710-7.
[97] Khamiees M, Raju P, DeGirolamo A, Amoateng-Adjepong Y, Manthous CA. Predictors of extubation outcome in patients who
have successfully completed a spontaneous breathing trial. Chest 2001; 120(4): 1262-70.
[98] Salam A, Tilluckdharry L, Amoateng-Adjepong Y, Manthous CA. Neurologic status, cough, secretions and extubation outcomes.
Intensive Care Med 2004; 30(7): 1334-9.
Received: November 22, 2010 Revised: December 28, 2010 Accepted: January 2, 2011











![Untitled-2 [] · FS 78 FS 68 , FOCUS ÉkJ ËFOCUS FS 78 FS 68 FS 68 , , , FS 68 Foundation FS 68 , FS 68 68 fi , FOCUS F-s 688 , , 68 , 688 FOCUS FS , FS 68 , , , 688 ,](https://static.fdocuments.us/doc/165x107/5b75f9b67f8b9a3b7e8b5e04/untitled-2-fs-78-fs-68-focus-ekj-efocus-fs-78-fs-68-fs-68-fs-68.jpg)