storage.googleapis.com · Web viewExtensive first-pass clearance; bioavailability is only about 20%...
Transcript of storage.googleapis.com · Web viewExtensive first-pass clearance; bioavailability is only about 20%...

1
Explain mechanisms and physiological consequences of alpha 1, alpha 2, beta 1 and beta 2 receptor blockade
Alpha receptor Beta receptor
Rank order of potency of agonists
Adr ≥ NA > Iso Iso > Adr > Na
Antagonist Phenoxybenzamine Propanolol
Effector pathway IP3/DAG↑, cAMP ↓, K+ channel ↑
cAMP ↑, Ca 2+ channel ↑
Beta 1 Beta 2 Beta 3
Location Heart, Jg cells in kidney
Bronchi, blood vessels, uterus, GIT, urinary tract, eye
Adipose tissue
Alpha 1 Alpha2
Location Postjunctional on effector organs
Prejunctional on nerve endings (α2A), also post junctional in brain, pancreatic β cells, platelets and extrajunctional in certain blood vessels
Function subserved Smooth muscle – contraction
Vasoconstriction
Gland-secretion
Gut relaxation
Heart arrythmia
Inhibition of transmitter release
Vasoconstriction
Decreased central sympathetic flow
Decreased insulin release
Platelet aggregation
Effector pathway IP3 /DAG ↑, phospholipase cAMP ↓

2
A2 ↑
K channel ↑
Ca2+ channel ↑ or ↓
IP3/DAG ↑
1 Receptor Antagonism 2 Adrenergic Receptor Antagonism
Inhibit vasoconstriction induced by endogenous catecholamines
Vasodilation may occur Fall in blood pressure due to decreased peripheral
resistance The magnitude of such effects is less in supine than in
upright subjects and is particularly marked if there is hypovolemia.
The fall in blood pressure is opposed by baroreceptor reflexes that cause increases in HR & CO, as well as fluid retention. These reflexes are exaggerated if the antagonist also blocks 2 receptors on peripheral sympathetic nerve endings, leading to enhanced release of norepinephrine and increased stimulation of postsynaptic 1 receptors in the heart and on juxtaglomerular cells.
Blockade of 1 receptors also inhibits vasoconstriction and the increase in blood pressure produced by the administration of a sympathomimetic amine. They block pressor action of Adr which then produces only fall in BP due to beta 2 mediated vasodilatation - vasomotor reversal of dale.
Tone of smooth muscle in the bladder trigone, sphincter and prostate is reduced by the blockade of alpha 1 receptors (mostly of the alpha 1A subtype) - urine flow in pts with BHP increases
Alpha blockers can inhibit ejaculation; this may manifest as impotence
Nasal stuffiness and miosis result from blockade of alpha receptors in the nasal blood vessels and radial muscles of iris respectively
intestinal motility is increased due to partial inhibition of relaxant sympathetic influences diarrhea may occur
Activation of presynaptic 2 receptors inhibits the release of norepinephrine and other cotransmitters from peripheral sympathetic nerve endings and leads to a fall in blood pressure;
Blockade of 2 receptors can increase sympathetic outflow and potentiate the release of norepinephrine from nerve endings, leading to activation of 1 and 1 receptors in the heart and peripheral vasculature with a consequent rise in blood pressure.
The physiological role of vascular 2 receptors in the regulation of blood flow within various vascular beds is uncertain.
the effect of blockade of platelet 2 receptors in vivo is not clear.
Blockade of pancreatic 2 receptors may facilitate insulin release. Alpha receptor antagonists reduce smooth muscle tone in the prostate and neck of the bladder, thereby decreasing resistance to urine outflow in benign prostatic hypertrophy (see below).

3
Beta 1 antagonism Beta 2 antagonism
receptor antagonists slow the heart rate and decrease myocardial contractility, especially during exercise or stress. However stroke volume is often preserved.
long-term administration of these drugs to hypertensive patients ultimately leads to a fall in peripheral vascular resistance
With long-term use of receptor antagonists, total peripheral resistance returns to initial values or decreases in patients with hypertension
Receptor antagonists reduce Sinus rate, slow conduction in atria and AV node and decrease automaticity.
improved relationship between cardiac oxygen supply and demand; exercise tolerance generally is improved in patients with angina, whose capacity to exercise is limited by the development of chest pain
The release of renin from the juxtaglomerular apparatus is stimulated by the sympathetic nervous system via 1 receptors, and this effect is blocked by receptor antagonists
During sympathetic activity peripheral resistance increases as a result of blockade of vascular 2 receptors and activation of vascular receptors.
Blockade of 2 receptors tends to blunt the increase in blood flow to active skeletal muscle during submaximal exercise
Increased incidence of bronchospasm in obstructive airway disease
glycogenolysis in the human liver is at least partially inhibited after β2-receptor blockade
Effects of non-selective betablockade: Metabolic Effects.

4
Nonselective blockers may delay recovery from hypoglycemia in IDDM but infrequently in NIDDM. Block glycogenolysis.
During hypoglycemia by blunt the perception of symptoms such as tremor, tachycardia, and nervousness.
Attenuate the release of free fatty acids from adipose tissue (important source of energy for exercising muscle)
Nonselective receptor antagonists consistently reduce HDL cholesterol, increase LDL cholesterol, and increase triglycerides. In contrast, 1-selective antagonists, including celiprolol, carteolol, nebivolol, carvedilol, and bevantolol, reportedly improve the serum lipid profile of dyslipidemic patients.
In contrast to classical blockers, which decrease insulin sensitivity, the vasodilating receptor antagonists (e.g., celiprolol, nipradilol, carteolol, carvedilol, and dilevalol) increase insulin sensitivity in patients with insulin resistance.
Eye: Decreased aqueous secretion from the ciliary epithelium
Classify alpha and beta receptor blocking agents according to their pharmacokinetic and pharmacodynamic properties
Classification of alpha blockers:
NON-COMPETITIVE ANTAGONISTS
β-Haloalkylamines: Phenoxybenzamine
COMPETITIVE ANTAGONISTS
Nonselective antagonists
α1 selectiveantagonists
α2 selectiveantagonists
Ergot alkaloids –Ergotamine, ergotoxin
Hydrogenated ergot alkaloids – dihydroergotamine,
Prazocin Terazocin Doxazosin Tamsulosin
Yohimbine

5
dihydroergotoxin
Imidazolines – Tolazoline, Phentolamine
Miscellaneous – chlorpromazine, ketanserine
Comparative Information About α Adrenergic Receptor Antagonists HALOALKYLAMINES IMIDAZOLINES QUINAZOLINESPrototype Phenoxybenzamine Phentolamine Prazosin Antagonism Irreversible Competitive CompetitiveSelectivity α1 with some α2 Nonselective
between α1 and α2
Selective for α1; does not distinguish among α1 subtypes
Hemodynamic effects
Decreased PVR and blood pressure
Similar to PBZ Decreased PVR and blood pressure
Venodilation is prominent Veins less susceptible than arteries; thus, postural hypotension less of a problem
Cardiac stimulation (cardiovascular reflexes and enhanced NE release due to α2 antagonism)
Cardiac stimulation is less (NE release is not enhanced due to α1 selectivity)
Actions other than α blockade
Some antagonism of ACh, 5-HT, and histamine
Cholinomimetic; adrenomimetic; histamine-like actions
At high doses some direct vasodilator action, probably due to PDE inhibition
Blockade of neuronal and extraneuronal uptake
Antagonism of 5-HT
Routes of Intravenous and oral; oral Similar to PZB Oral

6
administration absorption incomplete and erratic
Adverse reactions
Postural hypotension, tachycardia, miosis, nasal stuffiness, failure of ejaculation
Same as PBZ, plus GI disturbances due to cholinomimetic and histamine-like actions
Some postural hypotension, especially with the first dose; less of a problem overall than with PBZ or phentolamine
Therapeutic uses
Conditions of catecholamine excess (e.g., pheochromocytoma)
Same as PBZ Primary hypertension
Peripheral vascular disease Benign prostatic hypertrophy
Classification of beta blockers:
Pharmacological/Pharmacokinetic classification/properties of β Receptor Blocking AgentsDRUG MEMBRANE
STABILIZING ACTIVITY
INTRINSIC AGONIST ACTIVITY
LIPID SOLUBILITY
EXTENT OF ABSORPTION (%)
ORAL BIOAVAILABILITY (%)
t 1/2 (hours)
PROTEIN BINDING (%)
Classical non-selective β blockers: First generationNadolol 0 0 Low 30 30-50 20-24 30Propranolol ++ 0 High <90 30 3-5 90Timolol 0 0 Low to Moderate 90 75 4 <10Penbutolol 0 + High ≈100 ~100 ~5 80-98Pindolol + +++ Low >95 ~100 3-4 40
β1-Selective β blockers: Second generationAcebutolol + + Low 90 20-60 3-4 26Atenolol 0 0 Low 90 50-60 6-7 6-16Bisoprolol 0 0 Low ≤90 80 9-12 ~30Esmolol 0 0 Low NA NA 0.15 55Metoprolol +* 0 Moderate ~100 40-50 3-7 12
Non-selective β blockers with additional actions (α blocker): Third generationCarteolol 0 ++ Low 85 85 6 23-30Carvedilol ++ 0 Moderate >90 ~30 7-10 98Labetalol + + Low >90 ~33 3-4 ~50

7
β1-selective β blockers with additional actions (β 2 agonistic): Third generationBetaxolol + 0 Moderate >90 ~80 15 50Celiprolol 0 + Low ~74 30-70 5 4-5
Beta 2 selective blockerButoxamine
describe the pharmacology of alpha receptor blocking agents and apply this to their clinical use
PhenoxybenzaminePhysicochemical
Structure HaloalkylaminePresentation 10mg cap. And 50mg/ml inj.
Pharmacodynamics MOA blocks 1 and 2 receptors irreversibly
Inhibits reuptake of released norepinephrine by presynaptic adrenergic nerve terminals.Blocks histamine (H1), acetylcholine, and serotonin receptors at high doses
Use Treatment of pheochromocytoma almost always used to treat the patient in preparation for surgery.
Was used for BPH; not used any more due to side effects. Has been used to control the manifestations of autonomic
hyperreflexia in patients with spinal cord transection.Dose A conservative approach is to initiate treatment with
phenoxybenzamine (at a dosage of 10 mg twice daily) 1 to 3 weeks before the operation. The usual daily dose of phenoxybenzamine in patients with pheochromocytoma is 40 to 120 mg given in two or three divided portions.
CVS progressive decrease in peripheral resistance and reflex increase in COMarked postural hypotension
CNS fatigue, sedation, and nauseaRespiratory Nasal stuffiness due to vasodilatationOther Smooth muscle relaxation in bladder and vas deference Side effects/adverse effects
Postural hypotension with reflex tachycardia and other arrhythmias
Exaggerated hypotension in volume depleted subjects Reversible inhibition of ejaculation Nasal stuffiness Mutagenic in ames test
Interactions
Pharmacokinetics

8
Absorption absorbed after oral administration, although bioavailability is low. Administered orally.
Distribution Chronic administration leads to accumulation in adipose tissueMetabolism Cyclizes spontaneously into highly active intermediate. half-life of
phenoxybenzamine probably is less than 24 hours. However, the duration of its effect is dependent not only on the presence of the drug, but also on the rate of synthesis of receptors. irreversible blockade of long duration (14–48 hours or longer).
Excretion Most of the administered dose is excreted in urine in 24 hrs.
Prazocin
Physicochemical Structure contain a piperazinyl quinazoline nucleus. Structurally similar to
terazocinPresentation 0.5, 1 and 2 mg tabs
Pharmacodynamics MOA The major effects result from its potent and selective blockade of 1
receptors in arterioles and veins. 1:2 1000:1. Also inhibits phosphodiesterase.
Use HypertensionBHPLVF refractory to diuretics and digitalisRaynauds disease
Dose HT: The initial dose should be 1 mg at bed time to reduce the risk of syncopal reactions (The first dose effect). the dose is titrated upward depending on the blood pressure. A maximal effect generally is observed with a total daily dose of 20 mg in patients with hypertension in 2 to 3 divided doses. BPH: 1 to 5 mg twice daily typically are used.
CVS ↓ TPR & venous return ↓CO. usually does not increase heart rate as it has little or no 2 receptor-blocking effect and does not promote the release of norepinephrine from sympathetic nerve endings. depresses baroreflex function in hypertensive patients.
CNS suppress sympathetic outflowRespiratory Other favorable effects on serum lipids, ↓ LDL and triglycerides and ↑ HDLSide effects/adverse effects
1st dose effect: postural syncopeNasal stuffiness Relaxes bladder smooth muscle
Interactions
Pharmacokinetics Absorption Good oral absorption. bioavailability ~ 60%.

9
Distribution Peak conc. reached in ~ 2 hrs after oral dose. Tightly bound to plasma proteins (primarily 1-acid glycoprotein) and only 5% of the drug is free
Metabolism Extensively metabolized in the liver.T1/2 ~ 2.5 hrs ( 6 to 8 hours in congestive heart failure). The duration of action: 7 to 10 hours in the treatment of hypertension.
Excretion Excreted mainly in bile & little unchanged drug is excreted by the kidneys
Phentolamine (Regitine)
Physicochemical Structure ImidazolinePresentation 10mg/ml Inj.
Pharmacodynamics MOA competitive receptor antagonist that has similar affinities for 1 and
2 receptorsInhibits reuptake of released norepinephrine by presynaptic adrenergic nerve terminals.Phentolamine also can block receptors for 5-HT, and it causes release of histamine from mast cells; phentolamine also blocks K+ channels
Use short-term control of hypertension in patients with pheochromocytoma
relieve pseudo-obstruction of the bowel in patients with pheochromocytoma
used locally to prevent dermal necrosis after the inadvertent extravasation of an receptor agonist
Treatment of hypertensive crises that follow the abrupt withdrawal of clonidine or that may result from the ingestion of tyramine-containing foods during the use of nonselective MAO inhibitors.
Direct intracavernous injection of phentolamine (in combination with papaverine) has been proposed as a treatment for male sexual dysfunction.
Buccally or orally administered phentolamine may have efficacy in some men with sexual dysfunction
Dose 5mg IV repeated as required
CVS progressive decrease in peripheral resistance and reflex increase in COMarked postural hypotension
CNS fatigue, sedation, and nauseaRespiratory Nasal stuffiness due to vasodilatationOther Side effects/adverse
severe tachycardia, arrhythmias, and myocardial ischemia, especially after intravenous administration. With oral administration, adverse effects

10
effects include tachycardia, nasal congestion, and headache.Interactions
Pharmacokinetics Absorption limited absorption after oral administration. Distribution Its pharmacokinetic properties are not well known; Metabolism it may reach peak concentrations within an hour after oral administration
and has a half-life of 5–7 hoursExcretion
Tamsulosin
Physicochemical Structure BenzenesulfonamidePresentation 0.4 mg capsules
Pharmacodynamics MOA a1 receptor antagonist with some selectivity for a1A (and a1D) subtypes
compared to a1B subtype. This selectivity may favor blockade of a1A receptors in prostate
Use Treatment of BPH with little effect on BPDose Tamsulosin may be administered at a 0.4-mg starting dose; a dose of 0.8
mg ultimately will be more efficacious in some patientsCVS Little effect on BP as compared to other alpha antagonistsCNSRespiratory Other Side effects/adverse effects
Dizziness & retrogade ejaculation
Interactions
Pharmacokinetics Absorption well absorbed orally DistributionMetabolism It is extensively metabolized by CYPs in liver. T1/2 ~ 5 to 10 hours.
Excretion Biliary excretion

11
describe the pharmacology of beta blockers with particular reference to propanolol, atenolol, metoprolol, esmolol, carvedilol, sotalol and labetalol
Propanolol
Physicochemical Structure Presentation 10, 40, 80 mg tab, 1mg/ml Inj
Pharmacodynamics MOA Propranolol interacts with 1 and 2 receptors with equal affinity, lacks
intrinsic sympathomimetic activity, and does not block receptors.Use HT
Angina Arrythmias: supraventricular arrhythmias/tachycardias,
ventricular arrhythmias/tachycardias, premature ventricular contractions, digitalis-induced tachyarrhythmias
myocardial infarction pheochromocytoma prophylaxis of migraine variceal bleeding in portal hypertension generalized anxiety disorder
Dose For HT and angina initially 40 – 80 mg/day titrated upwards.
CVS Heart-decreases HR, force of contraction and CO. Cardiac work and O2 consumption reduced. Decreases automaticity. AV conduction is delayed.Blood vessels: Initially TPR increases and CO decreases, little change in BP. With prolonged administration BP decreases due to decrease in TPR. This is due to (i) reduced NA release from sympathetic terminus (ii) Decreased rennin release from kidney (beta 1) (iii) decreased central sympathetic outflow
CNS Forgetfulness, increased dreaming and nightmares, suppresses anxiety
Respiratory Inreases bronchial resisatnce by blocking beta 2 receptorsOther Metabolic: blocks adrenergically induced lipolysis reduced free fatty
acids. Plasma TGL and LDL/HDL ratio is increased. Inhibits glycogenolysis. Carbohydrate intolerance during prolonged administration. Potent local anaestheticInhibits adrenergically induced tremorsReduce exercise capacityReduced secretion of aqueous Relaxation of uterus is blocked
Side effects/adverse effects
Accentuates myocardial insufficiency- can ppt CHF and edemaBradycardiaRisk of life threatening attack of asthmaExacerbates variant anginaCarbohydrate intolerance

12
Altered lipid profileReduced exercise capacity- inability to increase blood flow Worsening of PVD-cold hands and feet
Interactions The bioavailability of propranolol may be increased by the concomitant ingestion of food and during long-term administration of the drug. Additive depression of Sinus node and AV conduction with digitalis and verapamilDelays recovery from hypoglycaemiaIndomethacin and other NSAIDs attenuate anti-hypertensive actionPropanolol decreases lignocaine metabolism by decreasing HBF
Pharmacokinetics Absorption highly lipophilic and is almost completely absorbed after oral
administration. Distribution large volume of distribution (4 liters/kg), 90% protein bound. Metabolism Extensive hepatic metabolism – systemic bioavailability ~ 25%. great
interindividual variation in the clearance of propranolol by the liver; this contributes to enormous variability in plasma concentrations (approximately twentyfold). Metabolism depends upon hepatic blood flow. Prolonged administration decreases HBF and decreases metabolism
Excretion Metabolites excreted in urine
The features of cardioselective beta blockers (metoprolol, atenolol, acebutolol)
lower propensity to cause bronchoconstriction
less interference with carbohydrate metabolism
less chance of ppt raynaud’s phenomenon
less deleterious effect on lipid profile
ineffective in blocking essential tremor
less liable to impair exercise tolerance
Atenolol
Physicochemical Structure Presentation 25, 50 mg tab
Pharmacodynamics

13
MOA 1-selective antagonist that is devoid of intrinsic sympathomimetic and membrane stabilizing activity
Use HTAngina
Dose The initial dose of atenolol for the treatment of hypertension usually is 50 mg per day, given once daily may be increased to 100 mg; higher doses are unlikely to provide any greater antihypertensive effect. The drug accumulates in patients with renal failure, and dosage should be adjusted for patients whose creatinine clearance is less than 35 ml/minute.
CVSCNSRespiratory Other Side effects/adverse effectsInteractions
Pharmacokinetics Absorption Atenolol is incompletely absorbed (about 50%), but most of the
absorbed dose reaches the systemic circulation. DistributionMetabolism There is relatively little interindividual variation in the plasma
concentrations of atenolol; peak concentrations in different patients vary over only a fourfold range., and the elimination half-life is about 5 to 8 hours.
Excretion The drug is excreted largely unchanged in the urine
Metoprolol
Physicochemical Structure Presentation 25, 50, 100mg tab/ 5mg/ml Inj
Pharmacodynamics MOA 1-selective receptor antagonist that is devoid of intrinsic
sympathomimetic activity and membrane-stabilizing activity.
Use chronic heart failure.HTMI

14
TachyarrythmiasDose Usual initial dose is 100 mg per day. Metoprolol generally is used in
two divided doses for the treatment of stable anginaCVSCNSRespiratory Other Side effects/adverse effectsInteractions
Pharmacokinetics Absorption Completely absorbed after oral administration, but bioavailability is
relatively low (about 40%) because of first-pass metabolism. DistributionMetabolism Metoprolol is extensively metabolized in the liver, with CYP2D6 the
major enzyme involved. Plasma concentrations of the drug vary widely (up to seventeenfold), perhaps because of genetically determined differences in the rate of metabolism. The half-life of metoprolol is 3 to 4 hours, but can increase to 7 to 8 hours in CYP2D6 poor metabolizers.
Excretion 90 % biliary excretion and 10% unchanged urinary excretion
Esmolol
Physicochemical Structure Presentation 100mg/ml Inj
Pharmacodynamics MOA 1-selective antagonist with a very short duration of action. It has little
if any intrinsic sympathomimetic activity, and it lacks membrane-stabilizing actions
Use SVTAFMIHypertension
Dose Loading dose 0.5mg/kg followed by 0.05 – 0.2mg/kg/min
CVSCNSRespiratory

15
Other Side effects/adverse effectsInteractions
Pharmacokinetics Absorption Administered IVDistribution apparent volume of distribution of approximately 2 liters/kg.Metabolism Inactivated by blood esterases. T1/2 < 10min. Action last 15-20min after
terminating infusion. Excretion Metabolite excreted in urine
Carvedilol
Physicochemical Structure Presentation 6.25, 12.5, 25mg tab
Pharmacodynamics MOA β1+ β2+α1 blocker + membrane-stabilizing activity
Use HTAnginaCHF
Dose 6.25mg BD initially, titrate to max 25mg BD
CVS Produces vasoldilatation and has anti-oxidant propertiesCNSRespiratory Other Side effects/adverse effectsInteractions
Pharmacokinetics Absorption Oral bioavailability 30%. peak plasma concentrations occurring in 1 to
2 hours. Distribution It is highly lipophilic and thus is extensively distributed into
extravascular tissues. It is 95% protein bound Metabolism T1/2 2-8hrs. Extensively metabolized in the liver, predominantly by
CYP2D6 and CYP2C9. The half life is 7 to 10 hours.

16
Excretion Biliary excretion
Sotalol
Physicochemical Structure Formulated as a racemic mixture of d- and l-sotalol.Presentation
40, 80mg Tab
Pharmacodynamics MOA Both b-adrenergic receptor-blocking (class 2) and action
potential prolonging (class 3) actions.
All the b-adrenergic blocking activity resides in the l-isomer; the d- and l-isomers share action potential prolonging actions.
Beta-adrenergic blocking action is not cardioselective and is maximal at doses below those required for action potential prolongation.
Use Approved for the treatment of life-threatening ventricular arrhythmias (superior to lidocaine to terminate VT) and the maintenance of sinus rhythm in patients with atrial fibrillation. It is also approved for treatment of supraventricular and ventricular arrhythmias in the pediatric age group. Sotalol decreases the threshold for cardiac defibrillation.
Dose IV dose : 0.5 -1.5 mg/kg over 5 – 20 min. oral therapy initiated at 80mg 12 hrly & increased to 160mg 12 hrly
CVS Prolongs APD & ERP in atria, AV node, ventricles, and accessory pathways.
CNSRespiratory Other

17
Side effects/adverse effects
dose-related incidence of torsade de pointesPatients with overt heart failure may experience further depression of left ventricular function
Interactions rare direct drug interactions because of simple pharmacokinetics
Pharmacokinetics Absorption Orally bioavailability of approx. 100%.
DistributionMetabolism half-life of approximately 12 hours.
Excretion Excretion is predominantly by the kidneys in the unchanged form
Labetalol
Physicochemical Structure Presentation 50, 100mg tab
Pharmacodynamics MOA competitive antagonists at both 1 and receptors. The potency of
the mixture for receptor blockade is fivefold to tenfold that for 1 receptor blockade. The R,R isomer has some intrinsic sympathomimetic activity at 2 adrenergic receptors; this may contribute to vasodilation
Use HTPheochromocytomaClonidine withdrawal
Dose Oral: 50mg BDIV: 20-40mg every 10min till desired response is achieved
CVS 1 Receptor blockade leads to relaxation of arterial smooth muscle and vasodilation, particularly in the upright position. The 1 blockade also contributes to a fall in blood pressure, in part by blocking reflex sympathetic stimulation of the heart. In addition, the intrinsic sympathomimetic activity of labetalol at 2 receptors may contribute to vasodilation. Relatively high doses decrease CO & TPR
CNSRespiratory

18
Other Limb blood flow increases in contrast to propanololSide effects/adverse effects
Labetalol has been associated with hepatic injury in a limited number of patients
Interactions
Pharmacokinetics Absorption Complete absorption from the gutDistributionMetabolism Extensive first-pass clearance; bioavailability is only about 20% to
40% and is highly variable. Bioavailability may be increased by food intake. The drug is rapidly and extensively metabolized in the liver by oxidative biotransformation and glucuronidation; very little unchanged drug is found in the urine. The rate of metabolism of labetalol is sensitive to changes in hepatic blood flow. The elimination half-life of the drug is about 8 hours. The half-life of the R,R isomer of labetalol (dilevalol) is about 15 hours.
Excretion Mainly biliary excretion
Classify the mechanisms of action of the anti-hypertensive agents
1. ACE inhibitors: Captopril, Enalapril, Lisinopril, Perindopril, Ramipril2. Angiotensin (AT1) antagonists: Losartan, Candesartan, Irbesartan3. Calcium channel blockers: Verapamil, Diltiazem, Nifedipine, Felodipine, Amlodipine,
Nitrendipine, Lacidipine4. Diuretic:
a. Thiazides: Hydrochlorthiazide, chlorthalidone, indapamideb. High ceiling: Furosemidec. K sparing: Spironolactone, triamterene, Amiloride
5. β adrenergic blockers: Metoprolol, propanolol, atenolol etc6. β + α adrenergic blockers: labetalol, Carvedilol 7. α adrenergic blockers: prazocin, terazocin, phentolamine, phenoxybenzamine8. Central sympatholytic: clonidine, methyldopa9. Vasodilator:
a. Arterial: hydralazine, minoxidil, diazoxide b. Arterial + Venous: sodium nitroprusside
Describe the pharmacology of centrally acting agents such as clonidine and alpha-methyl dopa
Clonidine
Physicochemical Structure Imidazoline

19
Presentation 150µg tab, transdermal patchPharmacodynamics
MOA Partial agonist with high affinity and high intrinsic activity at α2 receptors specially α2A receptor present post junctionally in medulla fall in BP and bradycardia. Plasma NA decreases.
Use HTOpioid withdrawalAnalgesiaAttenuates vasomotor symptoms of menopauseControl loose motions due to diabetic neuropathyClonidine suppression test for pheochromocytoma
Dose Started with 100 µg OD or BD maximum 300 µg TDS
CVS When the sympathetic tone to the vasculature is low, the major effect is to reduce both HR and SVWhen sympathetic outflow to the vasculature is normally increased eg when upright, these drugs reduce vascular resistance postural hypotension. The decrease in cardiac sympathetic tone leads to a reduction in myocardial contractility and heart rate; this could promote congestive heart failure in susceptible patients.Rapid IV injection raises BP transiently due to activation of peripheral post synaptic vasoconstrictor α2BTherapeutic window phenomenon: optimum lowering of BP occurs between blood levels of 0.2-2.0 ng/mlDecreased sympathetic flow to kidney results in reduced rennin release
CNS (see side effects)Respiratory -Other Side effects/adverse effects
Sedation
Xerostomia, dry nasal mucosa, dry eyes, and parotid gland swelling and pain. Postural hypotension and erectile dysfunction
vivid dreams or nightmares, restlessness, and depression.
Impotence
symptomatic bradycardia and sinus arrest in patients with dysfunction of the sinoatrial node and AV block in patients with AV nodal disease or in patients taking other drugs that depress AV conduction.
Sudden discontinuation increased sympathetic discharge withdrawal syndrome consisting of headache, apprehension, tremors, abdominal pain, sweating, tachycardia & HT.
Interactions RareDiuretics potentiate the hypotensive effect. Tricyclic antidepressants may inhibit the antihypertensive effect

20
Pharmacokinetics Absorption Well absorbed orally, peak occurs in 2-4hrsDistributionMetabolism T1/2 ~ 8-12 hrs. Effect of single dose lasts 6-24 hrs.
Excretion ½-2/3rd of oral dose is excreted unchanged in urine rest as metabolite. Dose modification required in renal insufficiency
Methyl Dopa
Physicochemical Structure analog of 3,4-dihydroxyphenylalanine (DOPA),Presentation 250mg tab
Pharmacodynamics MOA Centrally acting antihypertensive agent. It is a prodrug. metabolized
by the L-aromatic amino acid decarboxylase in adrenergic neurons to -methyldopamine, which then is converted to -methylnorepinephrine. -Methylnorepinephrine is stored in the secretory vesicles of adrenergic neurons, substituting for norepinephrine (NE) itself. Thus, when the adrenergic neuron discharges its neurotransmitter, -methylnorepinephrine is released instead of norepinephrine. Because -methylnorepinephrine is as potent as norepinephrine as a vasoconstrictor, its substitution for norepinephrine in peripheral adrenergic neurosecretory vesicles does not alter the vasoconstrictor response to peripheral adrenergic neurotransmission. Methylnorepinephrine acts as an agonist at presynaptic 2 adrenergic receptors in the brainstem, attenuating NE release and thereby reducing the output of vasoconstrictor adrenergic signals to the peripheral sympathetic nervous system.
Use Preferred drug for treatment of hypertension during pregnancy based on its effectiveness and safety for both mother and fetus.
Dose The usual initial dose of methyldopa is 250 mg twice daily, and there is little additional effect with doses above 2 g per day.
CVS It lowers blood pressure chiefly by reducing peripheral vascular resistance, with a variable reduction in heart rate and cardiac output.
Most cardiovascular reflexes remain intact after administration of methyldopa
Postural (orthostatic) hypotension may occur in volume-depleted patients.
The fall in arterial pressure is maximal 6 to 8 hours after an oral or intravenous dose.
CNS Methyldopa enters the brain via an aromatic amino acid transporter
Respiratory

21
Other Side effects/adverse effects
overt sedation ( most frequent )
mental lassitude and impaired mental concentration
Nightmares, mental depression, vertigo, and extrapyramidal signs
Lactation, associated with increased prolactin secretion
positive Coombs test, which sometimes makes cross-matching blood for transfusion difficult and rarely is associated with hemolytic anemia, as well as hepatitis and drug fever. The Coombs test may remain positive for as long as a year after discontinuation of methyldopa, but the hemolytic anemia usually resolves within a matter of weeks.
Interactions
Pharmacokinetics Absorption Absorbed by an active amino acid transporter. Peak concentrations in
plasma occur after 2 to 3 hours.Distribution small apparent volume (0.4 liter/kg)Metabolism Eliminated with a half-life of about 2 hours. The usual oral dose of
methyldopa produces its maximal antihypertensive effect in 4–6 hours, and the effect can persist for up to 24 hours. Because the effect depends on accumulation and storage of a metabolite (α-methylnorepinephrine) in the vesicles of nerve endings, the action persists after the parent drug has disappeared from the circulation.
Excretion Methyldopa is excreted in the urine primarily as the sulfate conjugate (50% to 70%) and as the parent drug (25%). The remaining fraction is excreted as other metabolites
Describe the physiology and pharmacology of the vascular endothelium and smooth muscle with particular reference to nitric oxide
Endothelial Cells and Vascular Smooth MuscleLarge number of substances can induce the contraction or relaxation of vascular smooth muscle. Many of these substances do so by acting directly on the arteriolar smooth muscle, but others act indirectly via the endothelialcells adjacent to the smooth muscle. Endothelial cells secrete several paracrine agents that diffuse to the adjacent vascular smooth muscle and induce either vasodilation or vasoconstriction. One very important paracrine vasodilator is nitric oxide which was called endothelium derived relaxing factor (EDRF). Nitricoxide is released continuously in significant amounts by endothelial cells in the arterioles and contributes toarteriolar vasodilation in the basal state. Another vasodilator released by endothelial cells is the eicosanoid prostacyclin (PGI2). There is little basal secretion of PGI2, but secretion can increase markedly in response to various inputs. One of the important vasoconstrictor paracrine agents released by endothelial cells in response to certain mechanical and

22
chemical stimuli is endothelin-1 (ET-1). ET-1 is a member of the endothelin family of peptide paracrine agents secreted by a variety of cells in diverse tissues, including the brain, kidneys, and lungs. Not only does ET-1 serve as a paracrine agent but under certain circumstances it can also achieve high enough concentrations in the blood to serve as a hormone, causing widespread arteriolar vasoconstriction.
In response to increased shear stress, arterial endothelium releases PGI2, increased amounts of nitric oxide, and less ET-1. All these changes cause the arterial vascular smooth muscle to relax and the artery to dilate. This flow-induced arterial vasodilation may be important in remodeling of arteries and in optimizing the blood supply to tissues under certain conditions.
There are several signal transduction mechanisms that modulate intracellular calcium concentration and therefore the state of vascular tone. Three different mechanisms are: 1) Gs-protein-coupled pathway, 2) phosphatidylinositol pathway, and 3) nitric oxide-cGMP pathway.Gs-Protein Coupled Signal Transduction
Gs-protein coupled pathway stimulates adenylyl cyclase (AC), which catalyzes the formation of cAMP. An increase in cAMP in vascular smooth muscle causes relaxation. cAMP inhibits Myosin light chain kinase (MLCK) which phosphorylates myosin and causes contraction
The Gs-protein is coupled to several important receptors that bind vasodilator substances:
β2-adrenoceptors A2 purinergic receptors IP receptors (bind prostacyclin, PGI2).

23
IP3- Coupled Signal Transduction
The phosphatidylinositol pathway: activated phospholipase C converts phosphatidylinositol (PIP2) to inositol triphosphate (IP3) which then stimulates the sarcoplasmic reticulum (SR) to release calcium. The formation of diacylglycerol (DAG) activates protein kinase C (PK-C), which can also contribute to vascular smooth muscle contraction via protein phosphorylation. This pathway is coupled to following receptors:
α1-adrenoceptors (Noradrenaline) AT1 receptors (Angiotensin) ETA receptors (Endothelin) V1 receptors (vasopressin) M3receptors (acetylcholine)
cGMP-Coupled Signal Transduction
Very important in regulating vascular smooth muscle tone.
Vascular endothelial cells normally produce NO, which diffuses from the endothelial cell to adjacent smooth muscle cells where it activates guanylyl cyclase leading to increased formation of cGMP and vasodilation. Nitric oxide (NO) is produced by many cells in the

24
body; however, its production by vascular endothelium is particularly important in the regulation of blood flow.
NO Biosynthesis
NO is produced from the amino acid L-arginine by the enzymatic action of nitric oxide synthase (NOS).
Two endothelial forms of NOS: o constitutive NOS (cNOS; type III)o inducible NOS (iNOS; type II)
Co-factors for NOS:o flavin adenine nucleotideso Oxygeno NADPHo Tetrahydrobiopterin
In addition to endothelial NOS, there is a neural NOS (nNOS; type I) that serves as a transmitter in the brain and in different nerves of the peripheral nervous system, such as non-adrenergic, non-cholinergic (NANC) autonomic nerves that innervate penile erectile tissues and other specialized tissues in the body to produce vasodilation.
Under basal conditions in blood vessels, NO is continually being produced by cNOS. The activity of cNOS is calcium and calmodulin dependent.
There are two basic pathways for the stimulation of cNOS, both of which involve release of calcium ions from subsarcolemmal storage sites:
o Flow-dependent NO formation: shearing forces generated by blood flow acting on the vascular endothelium causes a release of calcium and subsequent cNOS activation.
o Receptor-stimulated NO formation: endothelial receptors for a variety of ligands stimulate calcium release and subsequent NO production. Eg. Receptors for acetylcholine, bradykinin, substance-P, adenosine, and many others vasoactive substances.
iNOS differs from cNOS in that its activation is calcium independent. The activity of iNOS is stimulated during inflammation by bacterial endotoxins (e.g.,

25
lipopolysaccharide) and cytokines such as tumor necrosis factor (TNF) and interleukins.
Intracellular Mechanisms NO has a half-life of only a few seconds, because:
o Superoxide anion has a high affinity for NO & reduces NO bioavailability.o Diffuses into blood where it binds to heme moiety of hemoglobin and
subsequently broken downo Diffuses into the vascular smooth muscle cells adjacent to the endothelium
where it binds to and activates guanylyl cyclase
Activated guanylyl cyclase catalyzes the dephosphorylation of GTP to cGMP, which serves as a second messenger and induces smooth muscle relaxation by:
o increased intracellular cGMP, which inhibits calcium entry into the cell, and decreases intracellular calcium concentrations
o activates K+ channels, which leads to hyperpolarization and relaxation o stimulates a cGMP-dependent protein kinase that activates myosin light
chain phosphatase, the enzyme that dephosphorylates myosin light chains, which leads to smooth muscle relaxation.
Increased cGMP also has an important anti-platelet, anti-aggregatory effect.Vascular Effects of NO
Vascular actions of NO include the following:
Direct vasodilation (flow dependent and receptor mediated) Indirect vasodilation by inhibiting vasoconstrictor influences (e.g.,
inhibits angiotensin II and sympathetic vasoconstriction) Anti-thrombotic effect - inhibits platelet adhesion to the vascular endothelium Anti-inflammatory effect - inhibits leukocyte adhesion to vascular endothelium;
scavenges superoxide anion Anti-proliferative effect - inhibits smooth muscle hyperplasia
Because of the above actions of NO, when its production is impaired or its bioavailability is reduced, the following can result:
Vasoconstriction (e.g., coronary vasospasm, elevated systemic vascular resistance, hypertension)
Thrombosis due to platelet aggregation and adhesion to vascular endothelium

26
Inflammation due to upregulation of leukocyte and endothelial adhesion molecules
Vascular hypertrophy and stenosis
Diseases or Conditions Associated with Abnormal NO Production and Bioavailability Hypertension Obesity Dyslipidemias (particularly hypercholesterolemia and hypertriglyceridemia) Diabetes (both type I and II) Heart failure Atherosclerosis Aging Cigarette smoking
NO releasing drugs:
o Nitroglycerineo Amylnitriteo Isosorbide dinitrateo Nitroprusside
describe the pharmacology of calcium antagonists with reference to the management of hypertension
Mechanisms of Action. An increased concentration of cytosolic Ca2+ causes increased contraction in cardiac and vascular smooth muscle cells. The entry of extracellular Ca2+ is more important in initiating the contraction of cardiac myocytes (Ca2+-induced Ca2+ release). The release of Ca2+ from intracellular storage sites also contributes to contraction of vascular smooth muscle, particularly in some vascular beds. Cytosolic Ca2+ concentrations may be increased by various contractile stimuli. The Ca2+ channel antagonists produce their effects by binding to the 1 subunit of the L-type Ca2+ channels and reducing Ca2+ flux through the channel.

27
Pharmacological Properties
Cardiovascular Effects.
Actions in Vascular Tissue.
An increase in cytosolic Ca2+ results in enhanced binding of Ca2+ to calmodulin. The Ca2+-calmodulin complex in turn activates myosin light-chain kinase, with resulting phosphorylation of the myosin light chain. Such phosphorylation promotes interaction between actin and myosin and contraction of smooth muscle. Ca2+ channel antagonists inhibit the voltage-dependent Ca2+ channels in vascular smooth muscle. All Ca2+ channel blockers relax arterial smooth muscle, but they have little effect on most venous beds and hence do not affect cardiac preload significantly.
Actions in Cardiac Cells. Within the cardiac myocyte, Ca2+ binds to troponin, relieving the inhibitory effect of troponin on the contractile apparatus and permitting a productive interaction of actin and myosin leading to contraction. Thus Ca2+ channel blockers can produce a negative inotropic effect. Although this is true of all classes of Ca2+ channel blockers, the greater degree of peripheral vasodilation seen with the dihydropyridines is accompanied by a sufficient baroreflex-mediated increase in sympathetic tone to overcome the negative inotropic effect. In the SA and AV nodes, depolarization largely depends on the movement of Ca2+ through the slow channel. The effect of a Ca2+ channel blocker on AV conduction and on the rate of the sinus node pacemaker depends on whether or not the agent delays the recovery of the slow channel. Although nifedipine reduces the slow inward current in a dose-dependent manner, it does not affect the rate of recovery of the slow Ca2+ channel. Nifedipine does not affect conduction through the node. In contrast, verapamil not only reduces the magnitude of the Ca2+ current through the slow channel but also decreases the rate of recovery of the channel. Verapamil and diltiazem depress the rate of the sinus node pacemaker and slow AV conduction; the latter effect is the basis for their use in the treatment of supraventricular tachyarrhythmias. Its electrophysiological properties lead to slowing of the heart rate, prolongation of the AV nodal effective refractory period, and importantly, prolongation of the QTc interval. Particularly in the setting of hypokalemia, the last effect can be associated with torsades de pointes, a potentially lethal ventricular arrhythmia
Hemodynamic Effects. All the Ca2+ channel blockers increase coronary blood flow. The dihydropyridines are more potent vasodilators in vivo and in vitro than verapamil, which is more potent than diltiazem. Nifedipine causes selective dilation of arterial resistance vessels. The decrease in arterial blood pressure elicits sympathetic reflexes, with resulting tachycardia and positive inotropy. Nifedipine also has direct negative inotropic effects in vitro. venous tone does not change.
The other dihydropyridinesamlodipine, felodipine, isradipine, nicardipine, nisoldipine, and nimodipineshare many of the cardiovascular effects of nifedipine. Nimodipine has high lipid solubility and was developed as an agent to relax the cerebral vasculature. It is effective in inhibiting cerebral vasospasm and has been used primarily to treat patients with neurological defects

28
associated with cerebral vasospasm after subarachnoid hemorrhage.
Absorption, Fate, and Excretion. Although the absorption of these agents is nearly complete after oral administration, their bioavailability is reduced, in some cases markedly, by first-pass hepatic metabolism. The effects of these drugs are evident within 30 to 60 minutes of an oral dose, with the exception of the more slowly absorbed and longer-acting agents amlodipine, isradipine, and felodipine. For comparison, peak effects of verapamil occur within 15 minutes of its intravenous administration. These agents all are bound extensively to plasma proteins (70% to 98%); their elimination half-lives vary widely and range from 1.3 to 64 hours. During repeated oral administration, bioavailability and half-life may increase because of saturation of hepatic metabolism. A major metabolite of diltiazem is desacetyldiltiazem, which has about one-half of diltiazem's potency as a vasodilator. N-Demethylation of verapamil results in production of norverapamil, which is biologically active but much less potent than the parent compound. The half-life of norverapamil is about 10 hours. The metabolites of the dihydropyridines are inactive or weakly active. In patients with hepatic cirrhosis, the bioavailabilities and half-lives of the Ca2+ channel blockers may be increased, and dosage should be decreased accordingly. The half-lives of these agents also may be longer in older patients.
Toxicity and Untoward Responses. dizziness, hypotension, headache, flushing, ankle edema, digital dysesthesia, and nausea. constipation, peripheral edema, coughing, wheezing, and pulmonary edema. muscle cramps. Less common side effects include rash, somnolence, and occasional minor elevations of liver function tests. Worsened myocardial ischemia has been observed in two studies with the dihydropyridine nifedipine - coronary steal. Although bradycardia, transient asystole, and exacerbation of heart failure have been reported with verapamil, these responses usually have occurred after intravenous administration of verapamil in patients with disease of the SA node or AV nodal conduction disturbances or in the presence of adrenergic receptor blockade. In the setting of hypokalemia and/or bradycardia, polymorphic ventricular tachycardia (torsades de pointes), a potentially lethal arrhythmia, can be seen. Agranulocytosis also has been reported.
Interactions:β blockers – additive depression of conduction Digitalis – increased levelsCardiac depressants like quinidine and disopyramide
Therapeutic Uses
Variant & Exertional Anginaantiarrhythmic agents hypertension heart failure Nimodipine has been approved for use in patients with neurological deficits secondary to cerebral vasospasm after the rupture of a congenital intracranial aneurysm.

29
Nifedipine, diltiazem, amlodipine, and felodipine appear to provide symptomatic relief in Raynaud's disease.
describe in detail the pharmacodynamics and pharmacokinetics of sodium nitroprusside and glyceryl trinitrate including their adverse effects
Sodium nitroprusside
Physicochemical

30
Structure
Presentation 50mg vialPharmacodynamics
MOA Nitroprusside undergoes reduction in red cells & endothelial cells to form MetHb and release NO and 5 cyanide molecules. NO activates the guanylyl cyclase – cGMP – PKG pathway, leading to vasodilation
Tolerance does not develop to SNP unlike nitroglycerin
Use Hypertensive emergencies Short-term reduction of cardiac preload and/or afterload - improve cardiac
output in congestive heart failure, especially in hypertensive patients with pulmonary edema that does not respond to other treatment. Decrease myocardial oxygen demand after acute myocardial infarction.
Controlled hypotension to reduce bleeding In the treatment of acute aortic dissection along with blocker
Dose Because the compound decomposes in light, only fresh solutions should be used, and the bottle should be covered with an opaque wrapping. Rapid photoreduction occurs to form HCN- which changes colour of solution from browny-red → blue. The drug must be administered as a controlled continuous infusion, and the patient must be closely observed. The majority of hypertensive patients respond to an infusion of 0.25 to 1.5 g/kg per minute
CVS Dilates both arterioles and venules: combination of venous pooling and reduced arterial impedance.
In subjects with normal left ventricular function, venous pooling predominates and CO decreases, whereas in poor LV function reduced afterload and increased cardiac output predominates. renal blood flow and glomerular filtration are maintained, and plasma renin activity increases.
Only a modest increase in HR and an overall reduction in myocardial demand for oxygen unlike minoxidil, hydralazine, diazoxide, and other arteriolar vasodilators
CNS Headache and nausea due to raised ICPRespiratory VQ mismatchOther Side effects/adverse effects
Cyanide toxicity:o Occurs when sodium nitroprusside is infused at a rate greater than
5 g/kg/min or about 2 g/kg per minute for a prolonged period. o Limiting factor in the metabolism of cyanide - availability of sulfur-
containing substrates in the body (mainly thiosulfate). The

31
concomitant administration of sodium thiosulfate can prevent accumulation of cyanide.
o CN- binds inactive cytochrome oxidase → inhibiting oxidative phosphorylation ↑anaerobic metabolism → lactic acidosis
o ↓O2 utilisation → ↑mixed venous O2 content o Suspect in Pts with HT resistant to therapy:
↑HR Diaphoretic ↑MV Can progress CNS Sx inc seizure, coma
o ↑risk in hypothermic patients-↓rate of rhodanase conversion CN- o Treatment:
Cease infusion ↑O2 available → supplemental O2 Correct acidosis → NaHCO3 ↑Sulfur donors → IV Na thiosulfate (150mg/kg over
15min) ↑CN- binders → hydroxycobalbumin (Vit B12a) →
cyanocobalbumin (Vit B12) ↑metHb → Na nitrite 5mg/kg slow IV **if severe**
Thiocyanate toxicity: o Risk increases with infusions > 24 to 48 hrs especially if renal
function is impairedo Symptoms - anorexia, nausea, fatigue, disorientation, and toxic
psychosiso Plasma conc. of thiocyanate should be monitored and should not
be allowed to exceed 0.1 mg/mlo Rarely, excessive concentrations of thiocyanate may cause
hypothyroidism by inhibiting iodine uptake by the thyroid gland. In patients with renal failure, thiocyanate can be removed readily by hemodialysis.
MetHb: o Unlikely to accumulate to levels which are toxic, even in Pts
with congenital MetHb reductase deficiency o To develop 10% metHb → need 10mg/kg SNP (really high dose) o Treatment: methylene blue (1-2mg/kg) BUT not advised as
metHb needed for CN- clearance
Worsening of arterial hypoxemia in patients with COPD because the drug interferes with hypoxic pulmonary vasoconstriction ventilation perfusion mismatch.
↑ICP and ↓CPP ↓ Platelet aggregation

32
Interactions
Pharmacokinetics Unstable molecule - decomposes under alkaline conditions or when exposed to light Onset of action is within 30 seconds; the peak hypotensive effect occurs within 2 minutes,
and when the infusion of the drug is stopped, the effect disappears within 3 minutes. Nitroprusside undergoes reduction in red cells to form MetHb and release NO and 5 cyanide
molecules. MetHb binds one cyanide molecule to form non-toxic compound. Cyanide is further metabolized by liver mitochondrial enzyme rhodanase to thiocyanate,
which is eliminated almost entirely in the urine. The mean elimination half-time for thiocyanate is 3 days in patients with normal renal function, and it can be much longer in patients with renal insufficiency.
GTNPhysicochemical
Structure
Presentation S/L spray 400mcg/dose S/L tablets 300-600mcg Buccal tabs 1-5mg Oral tablets 2.6-10mg Patch 5-15mg/24hrs Injection 1-5mg/ml → diluted to 100mcg/ml (0.01%)
Pharmacodynamics MOA Nitroglycerin is denitrated by glutathione S-transferase. Free nitrite ion is
released, which is then converted to nitric oxide. A different unknown enzymatic reaction releases nitric oxide directly from the parent drug molecule. NO activates guanylyl cylase → ↑cGMP → ↓Ca2+ influx into vascular smooth mm / ↑Ca2+ uptake into smooth ER Overall ↓Ca2+ in cytoplasm → relaxation smooth mm → vasodilatation
Use Angina CHF & acute LVF MI Biliary colic Esophageal spasm

33
Cyanide poisoning
Dose Drug Dose Duration of Action
"Short-acting"
Nitroglycerin, sublingual 0.15–1.2 mg 10–30 minutes
NTG infusion 5µg/min - 100µg/min
"Long-acting"
Nitroglycerin, oral sustained-action
6.5–13 mg per 6–8 hours 6–8 hours
Nitroglycerin, 2% ointment, transdermal
1–1.5 inches per 4 hours 3–6 hours
Nitroglycerin, slow-release, buccal
1–2 mg per 4 hours 3–6 hours
Nitroglycerin, slow-release patch, transdermal
10–25 mg per 24 hours (one patch per day)
8–10 hours
CVS Vessels:
- 1° venodilatation ↓tendency for VR ↓preload RV
- Vasodilation ↓end-diastolic pressure / ↓vent wall tension → ↓afterload
Heart:
- ↓metabolic O2 requirements 2° above factors → ↓myocardial work → ↓O2 demand
- ↑coronary BF 2° ↓vent wall tension (↓afterload), redirecting blood flow to
subendocardium 2° coronary vasodilatation → improve O2 supply

34
- Results in favourable ↑supply:demand ratio
- CO
o ↓VR → ↓CO in normal Pts
HF Pts → ↑CO 2° ↓SVR and improved myocardial performance
Periphery:
- Vasodilatation
o Orthostatic hypotension
o High doses → ↓systemic vascular resistance (SVR)
↓MAP more pronounced in volume depletedCNS ↑CBF/↑ICP 2° vasodilatation, headacheRespiratory ↓PVR → ↑capacitance of pulmonary vessels → favour absorption
transudate Release of hypoxic pulmonary vasoconstriction → ↑shunt
Other - Uterus ↓uterine tone ↑blood flow → ↑risk haemorrhage
Haematological Rarely precipitates metHb Platelets → ↑cGMP → ↓Ca2+ in cytoplasm → ↓platelet
aggregation
Side effects/adverse effects
Methemoglobinemia (rare): Nitrite ion reacts with hemoglobin (which contains ferrous iron) to produce methemoglobin (which contains ferric iron). Because methemoglobin has a very low affinity for oxygen, large doses of nitrites can result in pseudocyanosis, tissue hypoxia, and death.
orthostatic hypotension
tachycardia
Throbbing headache.
TOLERANCE: may be caused in part by a decrease in tissue sulfhydryl groups. Increased generation of oxygen free radicals during nitrate therapy may be another important mechanism of tolerance

35
Interactions Sildenafil – dangerous hypotension
Pharmacokinetics Absorption High first pass metabolism – oral bioavailability < 10%
Distribution The volume of distribution following intravenous administration is 3.3 L/kgMetabolism Unchanged nitrate compounds have half-lives of only 2–8 minutes.
Partially denitrated metabolites have much longer half-lives (up to 3 hours).
Nitroglycerin metabolites - two dinitroglycerins and two mononitro forms. the dinitro derivatives have significant vasodilator efficacy
Excretion Excretion, primarily in the form of glucuronide derivatives of the denitrated metabolites, is largely by way of the kidney
Describe the pharmacology of the ACE inhibitors and angiotensin receptor antagonists with reference to the management of hypertension

36
Differences amongst ACE inhibitors are primarily pharmacokinetic, no single drug is superior to others
CaptoprilPhysicochemical
Structure Sulphydryl containing dipeptide surrogate of proline
Presentation 12.5, 25mg tabPharmacodynamics
MOA Inhibits ACE and abolishes pressor action of angiotensin I. Also increases plasma levels of kinins. (see diagram above)
Use HT: advantages no postural hypotension, no CNS effects, safe in asthmatics, prevention of secondary hyperaldosteronism, renal blood flow mentained, reverse left ventricular hypertrophy, no effect on lipid profile, no rebound HT, reduce cardiovascular morbidity and increase life expectancy.
CHF: reduce afterload and preload. ↑CO. Accumulated salt and water is lost because of increased renal perfusion and abolition of

37
mineralocorticoid mediated Na+ retension. Cardiac work (HR*SBP) ↓ and exercise capacitance ↑
MI Prophylaxis in high risk cardiovascular risk subjects Diabetic nephropathy – prevents or delays ESRD Hypertensive nephropathy Scleroderma crisis-↑BP and ↓renal function is caused by AII. ACE
inhibitors Dramatic improvement and life savingDose Started with 25mg BD gradually increased to 50mg TDS. In CHF start with
6.25mg BD to avoid sudden fall in BP. Should be taken 1 hr before or 2 hr after a meal.
CVS relax smooth muscle and thereby promote vasodilationarterioles dilate and compliance of large arteries ↑ ↓TPR
increase renal salt and water excretion,
reduce plasma volume
Both systolic and diastolic BP falls. Magnitude of drop in BP depends on Na+ and renin status.
decrease cellular hypertrophy.
CV reflexes intact and no effect on capacitance vessels.Reflex increase in aldosterone is abolished
CNS Poor penetrationRespiratory Cough in 15% due to inhibition of bradykinin/substance POther Renal: renal blood flow is mentained. Anti-proliferative effects. in the treatment of
patients with diabetes, slowing the development and progression of diabetic glomerulopathy. slowing the progression of other forms of chronic renal disease, such as glomerulosclerosis
Side effects/adverse effects
Well tolerated if daily dose is < 150mg
Hypotension: especially in those with high pre-treatment renin/angiotensin II eg vol depleted, CHF, cirrhosis, renovascular HT
Hyperkalemia - when ACE inhibitors are used with other drugs that can cause K+ retention
reduced renal function, including that associated with bilateral renal artery stenosis and stenosis in the artery of a solitary kidney
Cough, an adverse effect of ACE inhibitors, is less frequent with angiotensin II receptor antagonists.
Angioedema occurs very rarely.

38
Teratogenicity
Cough – with ace inhibitors
Headache, dizziness, nausea and GI upset
Rare – granulocytopenia and protienuria especially in renal disease
Interactions Indomethacin (and other NSAID) attenuate the hypotensive action. Hyperkalemia with K supplements/K sparing diureticsAntaacids reduce bioavailability of captoprilLi+ clearance is reduced predisposition to toxicity
Pharmacokinetics Absorption 70% oral bioavailability. Food reduces absorption. Distribution Penetration in brain is poor. Metabolism T1/2 ~ 2 hrs. Action lasts 6-12 hrs.
Excretion Partly metabolized and partly excreted unchanged in urine. 40% to 50% as captopril and the rest as captopril disulfide dimers and captopril-cysteine disulfide
Pharmacology of AT1 antagonists differ from ACE inhibitors in following ways:1. No interference with degradation of bradykinin and substance p2. More complete inhibition of AT1 receptor activation. With ACE inhibitors the alternative
pathways lead to formation of some Angiotensin II and hence some ATI receptor activation does occur
3. The AT2 receptor: adrenal medulla, kidney, and in the CNS, and may play a role in vascular development. renin and angiotensin II conc. increased during AT1-receptor antagonism act on uninhibited AT2 receptors elicit antigrowth and antiproliferative responses.
4. The AT1 receptor: vascular and myocardial tissue and also in brain, kidney, and adrenal glomerulosa cells, which secrete aldosterone
Losartan Physicochemical
Structure
Presentation 25, 50mg tabPharmacodynamics
MOA Competitive antagonist for AII. 10000 times more selective blocker of ATI receptors than ATII receptors. Partially carboxylated in liver to an active

39
metabolite which is 10-30 times more potent non-competitive AT1 antagonist. (see diagram above). Blocks all overt actions of AII viz- vasoconstriction, central and peripheral sympathetic stimulation, release of aldosterone from adrenals, renal actions promoting salt and water retention, central actions like thirst, vasopressin release and growth promoting actions on heart and blood vessels.
Use Systemic HT: Max effect in 3-4weeks. advantages no postural hypotension, no CNS effects, safe in asthmatics, prevention of secondary hyperaldosteronism, renal blood flow mentained, reverse left ventricular hypertrophy, no effect on lipid profile, no rebound HT, reduce cardiovascular morbidity and increase life expectancy.
Portal HT CHF: reduce afterload and preload. ↑CO. Accumulated salt and
water is lost because of increased renal perfusion and abolition of mineralocorticoid mediated Na+ retension. Cardiac work (HR*SBP) ↓ and exercise capacitance ↑
MI Prophylaxis in high risk cardiovascular risk subjects Diabetic nephropathy – prevents or delays ESRD Hypertensive nephropathy Scleroderma crisis-↑BP and ↓renal function is caused by AII. ACE
inhibitors Dramatic improvement and life savingDose 50mg OD, in liver disease 25mg OD
CVS relax smooth muscle and thereby promote vasodilationarterioles dilate and compliance of large arteries ↑ ↓TPR
increase renal salt and water excretion,
reduce plasma volume
Both systolic and diastolic BP falls. Magnitude of drop in BP depends on Na+ and renin status.
decrease cellular hypertrophy.
CV reflexes intact and no effect on capacitance vessels.Reflex increase in aldosterone is abolished
CNS No penetrationRespiratory Other Renal: renal blood flow is mentained. Anti-proliferative effects. in the treatment of
patients with diabetes, slowing the development and progression of diabetic glomerulopathy. slowing the progression of other forms of chronic renal disease, such as glomerulosclerosis
losartan is a competitive antagonist of the thromboxane A2 receptor and attenuates platelet aggregatio.

40
EXP3179, an active metabolite of losartan, reduces COX-2 mRNA up-regulation and COX-dependent prostaglandin generation
Side effects/adverse effects
Well tolerated
Hypotension: especially in those with high pre-treatment renin/angiotensin II eg vol depleted, CHF, cirrhosis, renovascular HT
Hyperkalemia - when ACE inhibitors are used with other drugs that can cause K+ retention
reduced renal function, including that associated with bilateral renal artery stenosis and stenosis in the artery of a solitary kidney
Cough, an adverse effect of ACE inhibitors, is less frequent with angiotensin II receptor antagonists.
Angioedema occurs very rarely.
Teratogenicity
Occasional Headache, dizziness, nausea and GI upset
Interactions Hyperkalemia with K supplements/K sparing diuretics
Pharmacokinetics Absorption Oral bioavailability 33% due to high first pass metabolism. Not affected by
food. Distribution 98% plasma protein boundMetabolism Partially carboxylated in liver to an active metabolite (EXP3179) which is
10-30 times more potent non-competitive AT1 antagonist. The metabolism of losartan to EXP 3174 and to inactive metabolites is mediated by CYP2C9 and CYP3A4. Peak plasma levels occur in 1 hr. T1/2 of losartan 2hr, T1/2 of metabolite 6-9hrs. No dose adjustment required in renal insufficiency but required in hepatic dysfunction
Excretion Excreted in urine
Outline the pharmacology of hydrallazine and the potassium channel activators (nicorandil and minoxidil)
HydrallazinePhysicochemical

41
Structure
Presentation 25-50 mg tabParenteral: 20 mg/mL for injection
Pharmacodynamics MOA Direct relaxation of arteriolar smooth muscle - mechanisms unclear - may
involve a fall in intracellular calcium conc.
Use Not a first-line drug in the treatment of hypertension. used in combination in the treatment of severe hypertension, CHF and in the treatment of hypertensive emergencies in pregnant women (especially preeclampsia)
Dose Usual dosage ranges from 40 mg/d to 200 mg/d. Dosing two or three times daily provides smooth control of blood pressure.
CVS Dilates arterioles but not veins/coronaries - powerful stimulation of the sympathetic nervous system, IIº to baroreceptor-mediated reflexes ↑ HR and contractility, ↑ plasma renin activity, and fluid retention counteract the antihypertensive effect of hydralazine. tachyphylaxis to its antihypertensive effects developed rapidly.
CNSRespiratory Other
Side effects/adverse effects
Most common adverse effects: headache, nausea, anorexia, palpitations, sweating, and flushing
The higher dosage (>400mg/day) lupus erythematosus-like syndrome - arthralgia, myalgia, pleuritis, pericarditis, skin rashes, and fever
Uncommon - pyridoxine-responsive polyneuropathy and drug fever
Coronary steal
Interactions
Pharmacokinetics Absorption Well absorbed but high first pass – oral bioavailability ~25%DistributionMetabolism Metabolized in part by acetylation in bowel/liver. rapid acetylators have
greater first-pass metabolism, lower bioavailability, and less antihypertensive benefit. T1/2~ 1.5 to 3 hours, but vascular effects persist

42
longer. peak hypotensive effect of the drug occur within 30 to 120 minutes of ingestion.
Excretion Biliary excretion
NicorandilPhysicochemical
Structure nicotinamide ester esterPresentation 5, 10mg tab, 2mg/vial inj
Pharmacodynamics MOA Activates ATP sensitive K channels- hyperpolarizing vascular smooth muscle
vasodilatationAlso donates NO which increase cGMP and cause vasodilatation – both arterial and venous
Use AnginaHTMICHF
Dose 5-20mg BD
CVS vasodilating properties in normal coronary arteries but more complex effects in patients with angina. Reduces both preload and afterload. No significant effects on contractility or conductionProvides some myocardial protection via preconditioning by activation of cardiac KATP channels.Mitochondrial K+ channel opening exerts myocardial protection by process of ischaemic preconditioning which reduces myocardial stunning, arrhythmias and infarct size when coronary artery is suddenly blocked
CNSRespiratory Other
Side effects/adverse effects
FlushingPalpitationWeaknessHeadache DizzinessMouth ulcers, nausea and vomiting
Interactions

43
Pharmacokinetics Absorption Absolute bioavailability is 75 ± 23%. peak plasma levels occur within 0.30 to
1.0 hours after dosingDistribution weakly bound to human plasma proteins (free fraction greater than 75%)Metabolism Main biotransformation pathways are de-nitration and then introduction
into the nicotinamide metabolism.Excretion
MinoxidilPhysicochemical
Structure
Presentation Oral: 2.5, 10 mg tablets
Topical: 2% lotionPharmacodynamics
MOA Metabolized by hepatic sulfotransferase to the active molecule, minoxidil sulfate. Minoxidil sulfate opens the ATP-modulated K+ channel K+ efflux hyperpolarization relaxation of smooth muscle
Use Reserved for poorly responding severe hypertension, especially in male patients with renal insufficiency. Used concurrently with a diuretic to avoid fluid retention and with a sympatholytic drug (usually a receptor antagonist) to control reflex cardiovascular effects.
AlopeciaDose The initial daily dose of minoxidil may be as little as 1.25 mg, which
can be increased gradually to 40 mg in one or two daily doses.CVS Produces arteriolar vasodilation. no effect on the capacitance vessels.
Increases blood flow to skin, skeletal muscle, the gastrointestinal tract, and the heart more than to the CNS. Strong reflex increase in heart rate, myocardial contractility and in cardiac output.
CNSRespiratory Other renal artery vasodilator, but systemic hypotension can ↓ RBF. Renal
function usually improves in patients who take minoxidil for the treatment

44
of hypertension. Very potent stimulator of renin secretion.
Side effects/adverse effects
Tachycardia, palpitations, angina, and edema
Headache, sweating, and hirsutism
fluid and salt retention
Interactions
Pharmacokinetics Absorption Well absorbed. peak conc. occur 1 hour after oral administration, the
maximal hypotensive effect of the drug occurs later
DistributionMetabolism Metabolized by hepatic sulfotransferase to the active molecule,
minoxidil sulfate. Minoxidil has a half-life in plasma of 3 to 4 hours, but its duration of action is 24 hours or occasionally even longer.
Excretion 20% of the absorbed drug is excreted unchanged in the urine, and the main route of elimination is by hepatic metabolism
physiological and pharmacological basis of antiarrhythmic therapy

45
A schematic representation of Na+ channels cycling through different conformational states during the cardiac action potential. Transitions between resting, activated, and inactivated states are dependent on membrane potential and time. The activation gate is shown as m and the inactivation gate as h. Potentials typical for each state are shown under each channel schematic as a function of time. The dashed line indicates that part of the action potential during which most Na+ channels are completely or partially inactivated and unavailable for reactivation
Inactivation gate (h) have voltage dependent function. They begin to close between -70 to - 55 mv and begin to recover from -55 to -70 mv
Refractory period
• The time between phase 0 and sufficient recovery of sodium channels in phase 3 to permit a new propagated response to an external stimulus is the refractory period.
• Less negative resting membrane potential results in prolongation of refractory time. Since inactivation gates of sodium channels close between -70 to - 55 mv, hence, fewer sodium channels are available for diffusion of sodium ions when an AP is evoked from a resting potential of -60mv than when it is evoked from resting potential of – 80 mv

46
• SA node and AV node have resting membrane potential in the range of – 50 to -70 mv hence all na channels are inactivated.
• Such depolarized cells exhibit “slow responses” – slow upstroke velocity and slow conduction – which depends on calcium inward current.
• Other relatively depolarized cells exhibiting slow depolarization & conduction include cells exposed to hyperkalemia, sodium pump blockade, or ischemic cells.
Mechanisms of arrhythmias
Abnormal automaticity• Non-pacemaker cells begin to spontaneously and abnormally initiate an impulse, believed
to be the result of reduced (more positive) RMP bringing it closer to the threshold potential. Eg. Ischemia and electrolyte imbalances

47
• Acceleration of pacemaker discharge, brought about by increased phase 4 depolarization slope. Eg. hypokalemia, β stimulation, positive chronotropic drugs, fibre stretch, acidosis and partial depolarization by currents of injury.
After depolarization (or triggered activity)• Spontaneous depolarizations requiring a preceding impulse (a triggering beat) • Early after depolarizations (EAD): After depolarizations originating during phase 2 or 3 of
the AP • Delayed afterdepolarization (DAD): After depolarizations originating during phase 4 of AP
Early after depolarization
• Prolonged action potential eg. Prolongation of QT interval (repolarization) by inhibition of delayed rectifier potassium current (sotalol, quinidine, dofetilide and procainamide)
• Torsade de pointe (TdP), a potentially lethal polymorphic ventricular arrhythmia, is an example of EAD, precipitated by K+channel blockers
Delayed after depolarization
• Ventricular arrhythmias secondary to digoxin toxicity is an example of delayed afterdepolarization.
• Digoxin mediated increased intracellular Ca++ is believed to be the mechanism of this type of arrhythmia

48
Disorders of impulse conduction• Most common mechanism of arrhythmias• Can result in conduction block and reentry
Re-entry• Impulse recirculates in the heart and cause repititive activation• Pre-requisites:
– Propagating impulse encounters electrophysiologically inhomogeneous tissue with unidirectional block allowing retrograde conduction
– retrograde conducting impulse encounters excitable tissue
• Lengthening of the refractory period and / or slowing of the velocity of conduction may help terminate reentry.
• Examples of reentrant arrhythmias:– AV nodal reentrant tachycardia (AVNRT)– Atrioventricular reentrant tachycardia (AVRT)– Atrial flutter– Atrial fibrillation– Ventricular tachycardia.
Mechanism of action of anti-arrhythmics• Aim of therapy:
– Reduce ectopic pacemaker activity– Modify conduction or refractoriness in reentry circuits to disable circus movement
• Major mechanisms to accomplish these goals: – 1. Sodium channel blockade– 2. Blockade of sympathetic autonomic effects in heart– 3. Prolongation of effective refractory period– 4. Calcium channel blockade
Abnormal automaticity• State dependent action of Na+ blockers: binding preference to the activated & inactivated
channels than the resting channels • Hence arrhythmic cells with rapid activity and depolarization of resting potential will have
more channels in A and I stage and hence will be favorably blocked by the drug. • In cells with abnormal automaticity most of the drugs reduce phase 4 slope by blocking
either sodium and calcium channel thereby reducing the ratio of sodium to potassium permeability.
Reentry arrhythmias• Slow conduction by:

49
– Steady state reduction in the number of the unblocked channels which reduces the excitatory current to a level below that required for propagation
– Prolongation of refractory time. (conversion to bi-direction block)• Excessive slowing promotes reentry by allowing time for unidirectional block to recover.
Hence powerful Na+ channel blockers e.g. Flecainide, Propafenone may actually promote ventricular tachyarrhythmias
Classify antiarrhythmic agents by their electro-physiological activity and mechanisms of action
• The widest employed Vaughan-Williams classification. • Major drawbacks:
– Over simplification of the effect– The classification relies on the effect these agents have on normal tissue– Major effects of an agent from one group overlaps with the effects of agents from
other groups• A more comprehensive classification of anti arrhythmic agents is available and has been
called the “Sicilian Gambit”.Vaughan-Williams classification (1969) involves 4 classes. In 1979 harrison divided class I into subclass A B & C.

50
describe the pharmacology, with particular reference to the antiarrhythmic properties, of the sodium channel blocking agents (eg. lignocaine and flecainide)
Subclass IA Intermediate kinetics of binding & dissociation.Combined Na+ & K+ blockade

51
Supress AV conduction, prolong PR, QRS, QT and APD

52
Subclass IB Rapid kinetics of binding and dissociation
Do not delay channel recovery or depress AV conduction or prolong APD, ERP & QT

53
Subclass IC Slow kinetics of binding and dissociation
Most potent Na+ channel blockers with more prominent action on open state and longest recovery times. Markedly delays conduction, prolong PR, broaden QRS but have variable effect on APD.
Lignocaine

54
Physicochemical Structure
Presentation 20mg/ml injPharmacodynamics
MOA • Blocks preferentially inactivated Na+ channels. Hence selective for partially depolarized cells & those with long AP (eg. PF & ventricular). Automaticity and after depolarizations in these cells supressed
• PF and Ventricular muscle: decreases APD duration (no class III action), and ERP to a lesser extent
• No action on APD or ERP of Atrial fibres. • SA and AV node not affected
Use • Only in ventricular tachyarrythmias especially in digitalis toxicity setting where it does not effect AV node
• Used to be given prophylactially by infusion in acute MI – reduces incidence of VF
• Current status: not used as prophylactic as failed to show survival and also increase short term mortality, possibly by increasing the incidence of asystole
Dose • loading dose of 150–200 mg over 15 minutes followed by a maintenance infusion of 2–4 mg/min. Therapeutic plasma conc. 2-5 microgram/ml. steady-state concentrations may be achieved in 8–10 hours in normal patients .
• In liver disease, the maintenance dose should be decreased, but usual loading doses can be given.
• In patients with heart failure, lidocaine's volume of distribution and total body clearance may both be decreased. Thus, both loading and maintenance doses should be decreased.
• No change in renal disease
CVSCNS High dose can cause seizuresRespiratory Other
Side effects/adverse
Cardiac

55
effects • least cardiotoxic of the currently used sodium channel blockers
• Only in toxic doses:
• Proarrhythmic effects (uncommon) - sinoatrial node arrest, worsening of impaired conduction, and ventricular arrhythmias
• May cause hypotension—partly by depressing myocardial contractility.
Extra-cardiac
• Seizures
• Nystagmus
• Paresthesia
• Blurred vision
• Disorientation
• Drowsiness
• Nausea
• Hypotension at high doses
Interactions • Drugs that decrease liver blood flow (eg, propranolol, cimetidine) reduce lidocaine clearance and so increase the risk of toxicity unless infusion rates are decreased.
Pharmacokinetics Absorption • High hepatic 1st pass metabolism: 3% oral bioavailability
DistributionMetabolism • Duration of action 10 to 20 min because of rapid redistribution
• Hydrolyzed, deethylated and conjugated. Metabolites excreted in urine
• T1/2 of early distribution phase is 8 min while late elimination is 2 hours
Excretion
Flecainide Physicochemical

56
Structure
Presentation Oral: 50, 100, 150 mg tablets
Pharmacodynamics MOA Flecainide blocks Na+ current and delayed rectifier K+ current (IKr).
very long recovery from Na+ channel blockalso blocks Ca2+ currentsAPD ↓ in Purkinje cells ↑ in ventricular cells, probably owing to block of delayed rectifier currentFlecainide does not cause EADs in vitro or torsades de pointes. In atrial tissue, flecainide disproportionately prolongs action potentials at fast ratesFlecainide prolongs the duration of PR, QRS, and QT intervals even at normal heart rates.
Use maintenance of sinus rhythm in patients with supraventricular arrhythmias, including atrial fibrillation, in whom structural heart disease is absent, WPW
Dose 100–200 mg twice a day
CVSCNSRespiratory Other
Side effects/adverse effects
Dose-related blurred vision
can exacerbate CHF in pts with LV dysfunction
Pro-arrythmogenic: acceleration of ventricular rate in patients with atrial flutter, increased frequency of episodes of re-entrant ventricular tachycardia, and increased mortality in patients convalescing from MI
Interactions
Pharmacokinetics Absorption Well absorbed. DistributionMetabolism T1/2~20hrs. Elimination occurs by both renal excretion of
unchanged drug and hepatic metabolism by CYP2D6 to inactive metabolites.
Excretion Both biliary and urinary excretion

57
The beta blockers
These drugs diminish phase 4 depolarization thus depressing automaticity, prolonging AV conduction, and decreasing HR and contractilityUseful in treating tachyarrhythmias caused by increased sympathetic activity. They are also used for atrial flutter and fibrillation and for AV nodal reentrant tachycardia

58
All betablockers covered above
Class III agents
Class III: Potassium channel blockers• Action is manifest by prolongation of the APD• Most drugs with this action block the rapid component of the delayed rectifier
potassium current, IKr.• Undesirable property of "reverse use-dependence": action potential prolongation is
least marked at fast rates (where it is desirable) and most marked at slow rates, where it can contribute to the risk of torsade de pointes.

59

60
Amiodarone
Flecainide Physicochemical
Structure
Presentation 400mg, 200mg tab
150mg/3ml Inj
Pharmacodynamics MOA • Markedly prolongs the APD (and the QT interval on the ECG) by
blockade of IKr. • IKs is blocked during chronic administration. • Does not have reverse use-dependent action. • Also significantly blocks inactivated sodium channels & decreases
conduction velocity. • Weak adrenergic and calcium channel blocking actions. • Effects: slowing of the HR & AV node conduction. • The broad spectrum of actions may account for its relatively high
efficacy and low incidence of torsade de pointes despite significant QT interval prolongation.
• Extracardiac Effects: peripheral vasodilation, following intravenous administration. May be related to the action of the vehicle. (Polysorbate 80 and benzyl alcohol)
Use • Low doses (100–200 mg/d) of amiodarone are effective in maintaining normal sinus rhythm in patients with atrial fibrillation.
• Effective in the prevention of recurrent ventricular tachycardia. • Its use is not associated with an increase in mortality in patients with
coronary artery disease or heart failure. • In many centers, the implanted cardioverter-defibrillator (ICD) has
succeeded drug therapy as the primary treatment modality for ventricular tachycardia, but amiodarone may be used for ventricular tachycardia as adjuvant therapy to decrease the frequency of uncomfortable ICD discharges.
• The drug increases the pacing and defibrillation threshold and these devices require retesting after a maintenance dose has been

61
achieved.
Dose • A total loading dose of 10 g is usually achieved with 0.8–1.2 g daily doses. The maintenance dose is 200–400 mg daily. Intravenous: 300 mg intravenously, over 10—60 min depending on the circumstances and haemodynamic stability of the patient, followed by an infusion of 900 mg over 24 h. Additional infusions of 150 mg can be repeated. Maximum total daily dose of 2 g. Can cause thrombophlebitis if given by peripheral vien. Can be given by large bore peripheral line in emergency.
• Shock resistant VF: 300 mg followed by 150 mg if required. • Therapeutic plasma range - 0.5 to 2.5 μg/mL. Measured levels do
not correlate well with efficacy or adverse effects• Pharmacologic effects achieved rapidly by intravenous loading. With
this route QT-prolonging effect is modest whereas bradycardia and atrioventricular block may be significant.
CVSCNSRespiratory Other
Side effects/adverse effects
• Cardiac: may produce symptomatic bradycardia & heart block in patients with preexisting sinus or AV node disease.
• Extracardiac: Accumulates in many tissues, including the heart (10–50 times greater than plasma), lung, liver, and skin, and is concentrated in tears.
Neuropsychiatric
• The most common are tremor and ataxia (3%-35%, depending on dose and duration of therapy).
• Peripheral neuropathy is uncommon (0.3% annually) but may be severe, requiring dose reduction or discontinuation of therapy.
• Insomnia, memory disturbances, and delirium also have been reported.
Eye
• Asymptomatic corneal microdeposits (>90%), drug discontinuation is usually not required.
• Optic neuropathy/ neuritis (<1%-2%)
Thyroid
• Contains 37.3% iodine by weight
• Inhibits peripheral conversion of T4 to T3

62
• Hypothyroidism (Wolff-Chaikoff effect)(6%)
• Hyperthyroidism ( Jodbasedow effect)(0.9%-2%)
Lungs
• Dose-related pulmonary toxicity is the most important adverse effect. Even on a low dose of 200 mg/d, fatal pulmonary fibrosis may be observed in 1% of patients.
• Risk factors for pulmonary fibrosis include:
– Underlying lung disease
– Dosages greater than 400 mg/d
– recent pulmonary insults
Skin
• Skin deposits result in a photodermatitis and a gray-blue skin discoloration (4%-9%), in sun-exposed areas, eg, the malar regions.
Interactions Drugs that increase amiodarone levels
• Cimetidine • Protease inhibitors
Drugs that decrease amiodarone levels
• Cholestyramine • Rifampin
Amiodarone increases the following drug levels
• Cyclosporine• Digoxin (reduce digoxin
dose by 50% and monitor levels)
• Theophylline • Flecainide • Lidocaine • Procainamide • Quinidine
others Azole antifungals (prolong QTc)B-blockers (sinus bradycardia or AV block)Calcium channel blockers (sinus bradycardia or AV block)Fentanyl (bradycardia, sinus arrest, and hypotension)Fluoroquinolones (prolong QTc—use of sparfloxacin contraindicated)Statins (lovastatin, simvastatin) (increase the risk of rhabdomyolysis or myopathy)Macrolide antibiotics (prolong QTc)Warfarin (potentiates effect—reduce warfarin dose by 25%-33% & monitor INR)
Pharmacokinetics

63
Absorption • Variable absorbtion - bioavailability of 35–65%.
Distribution • Highly lipophilic, with a large volume of distribution (66 L/kg)Metabolism • Hepatic metabolism (CYP3A4)- major active metabolite:
desethylamiodarone. • Elimination t1/2 is complex: rapid component of 3–10 days (50% of
the drug) and a slower component of several weeks. • Following discontinuation, effects are maintained for 1–3 months &
measurable tissue levels up to 1 year.
Excretion Metabolites excreted in feces
Sotalol discussed above
IbutilidePhysicochemical
Structure
Presentation 0.1 g/mL solution for IV infusionPharmacodynamics
MOA IKr blocker + activates an inward Na+ current. The action potential-prolonging effect of the drug may arise from either mechanism.
Use The drug's efficacy rate is higher in patients with atrial flutter (50% to 70%) than in those with atrial fibrillation (30% to 50%). In atrial fibrillation, the conversion rate is lower in those in whom the arrhythmia has been present for weeks or months compared with those in whom it has been present for days.
Dose Ibutilide is administered as a rapid infusion (1 mg over 10 minutes) for the immediate conversion of atrial fibrillation or flutter to sinus rhythm.
CVSCNSRespiratory Other
Side effects/ The major toxicity with ibutilide is excessive QT prolongation and torsades

64
adverse effects
de pointes, which occurs in up to 6% of patients and requires immediate cardioversion in up to one-third of these.
Interactions
Pharmacokinetics Absorption The drug undergoes extensive first-pass metabolism and so is not
used orally.DistributionMetabolism It is eliminated by hepatic metabolism and has a half-life of 2 to 12
hours (average of 6 hours).Excretion metabolites are excreted by the kidney
Calcium channel antagonists

65
Electrophysiological actions of CCB
Verapamil: pharmacodynamics
• Cardiac Effects • Blocks both activated and inactivated L-type calcium channels. • Decreased slope of phase 4 depolarization & phase 0 in cal. Dependent slow fibres (AV, SA,
depolarized tissues). • AV nodal conduction time and effective refractory period are invariably prolonged • Usually slows the SA node by its direct action, but its hypotensive action may occasionally
result in a small reflex increase of sinoatrial nodal rate.• Suppress both early & delayed afterdepolarizations.• May antagonize slow responses arising in severely depolarized tissue.• Extracardiac Effects: peripheral vasodilation, and smooth muscle relaxation
Pharmacokinetics & Dosage
• T1/2 = 7 hours. • Metabolized by the liver. Oral bioavailability =20%. Caution in patients with hepatic
dysfunction.

66
• Verapamil dosage is an initial bolus of 5 mg administered over 2–5 minutes, followed a few minutes later by a second 5 mg bolus if needed. Thereafter, doses of 5–10 mg can be administered every 4–6 hours, or a constant infusion of 0.4 mcg/kg/min may be used.
• Effective oral dosages range from 120 to 640 mg daily, divided into three or four doses
Adverse effects• Cardiac • dose-related and usually avoidable. • A common error: intravenous verapamil to a patient with ventricular tachycardia
misdiagnosed as supraventricular tachycardia. In this setting, hypotension and ventricular fibrillation can occur. Should be avoided in wide complex tachy.
• Negative inotropic effects- may limit its clinical usefulness in diseased hearts • AV block in large doses or in AV nodal disease. • In sinus node disease, verapamil can precipitate sinus arrest.• Extracardiac • Adverse effects include constipation, lassitude, nervousness, and peripheral edema.
Uses• SVT is the major arrhythmia indication for verapamil. • Verapamil can also reduce the ventricular rate in atrial fibrillation and flutter. • MAT
Diltiazem• Hepatic metabolism• T1/2 = 3.5 hrs• Oral bioavailabiltiy 40 % (extensive 1st pass)• Dose: loading 0.25mg/kg, followed by 0.35mg/kg. IV maintenance: 5-15 mg/hr. Oral
maintenance: 60 -120 mg 6-8 hourly
Digoxin
Physicochemical Structure
Molecule consist of aglycone to which are attached one or more sugars. Pharmacological properties reside in aglycone and attached sugars modify

67
solubility and and cell permeability.
Presentation 0.25mg tab
0.5mg/2ml Inj
Pharmacodynamics MOA positive inotropic effects results from increased intracellular Ca2+ . Binding of
cardiac glycosides to the sarcolemmal Na+,K+-ATPase and inhibition of cellular Na+ pump activity results in a reduction in the rate of active Na+ extrusion and a rise in cytosolic Na+. This increase in intracellular Na+ reduces the transmembrane Na+ gradient that drives the extrusion of intracellular Ca2+ during myocyte repolarization. With reduced Ca2+ efflux and repeated entry of Ca2+ with each action potential, Ca2+ accumulates in the myocyte: Ca2+ uptake into the SR is increased; this increased Ca2+ becomes available for release from the SR onto troponin C and other Ca2+-sensitive proteins of the contractile apparatus during the next cycle of excitation-contraction coupling, thereby augmenting myocyte contractility.
Cardiac glycosides increase phase 4 slope (i.e., increase the rate of automaticity), especially if [K]o is low.
Prominent vagotonic actions, resulting in inhibition of Ca2+ currents in the AV node and activation of acetylcholine-mediated K+ currents in the atrium. Thus the major "indirect" electrophysiological effects of cardiac glycosides are hyperpolarization, shortening of atrial action potentials, and increases in AV nodal refractoriness.
In heart transplant patients--ineffective for rate control.
Use • CHF• Rate control in AF and AFL and PSVT

68
Dose The antiarrhythmic effects of digoxin can be achieved with intravenous or oral therapy. However, digoxin undergoes relatively slow distribution to effector site(s); therefore, even with intravenous therapy, there is a lag of several hours between drug administration and the development of measurable antiarrhythmic effects
To avoid intoxication, a loading dose of approximately 1 to 1.5 mg digoxin is administered over 24 hours. Measurement of postdistribution serum digoxin concentration and adjustment of the daily dose (0.125 to 0.375 mg) to maintain concentrations of 0.5 to 2 ng/ml are useful during chronic digoxin therapy.
CVS
Force of contraction: dose dependant increase in force of contraction, increased velocity of tension development, increased CO. systole is shortened and diastole is prolonged.Tone: defined as maximum length of fibre at a given filling pressure. Tone is not changed, end diastolic volume is reduced due to increased ejection fractionRate: decreased by digitalis. In CHF sympathetic overactivity is also abolished due to improved CO. In addition digitalis slows HR by vagal and extra vagal effectsVagal tone is increased:
• Refelexly through nodose ganglion and sensitization of baroreceptors: amplify parasympathetic discharge to the heart
• Direct stimulation of vagal centre• Sensitization of SA node to Ach.
Extravagal: direct action on SA and AV nodes, probably an antiadrenergic action exerted beyond receptor level.
Electrophysiological action: Action potential:
• RMP is shifted towards isoelectric level – increased excitability • Rate of phase 0 depolarization reduced• Phase 4 slope is increased in PF- ectopic automaticity increased• At high doses coupled beats occur due to oscillations in phase 4
resulting in DAD• APD and amplitude is reduced

69
ERP• Atrium – decreased by vagal action, increased by direct action• AV node and bundle of his – increased by direct, vagomimetic and
antiadrenergic actions. Conduction hence reduced. • Ventricle – abbreviated by direct action
ECG: • Decreased amplitude or inversion of t wave• Increased PR interval• Shortening of QT interval• Depression of ST segment
Blood vessels: mild vasoconstrictor
CNS Higher doses cause CTZ activation nausea vomiting. Very high doses produce hyperapnoea, central sympathetic stimulation, confusion and visual disturbances
Respiratory Other Kidney – increased dieresis due to improved renal perfusion
Side effects/adverse effects
Increased sympathetic activity, electrolyte abnormalities (e.g., hypokalemia, hypomagnesemia, and hypercalcemia) and hypoxia increase the risk of digitalis toxicity.
Digitalis exerts direct arterial vasoconstrictor effects, which can be especially deleterious in patients with advanced atherosclerosis who receive intravenous drug; mesenteric and coronary ischemia have been reported.
low therapeutic index – 1.5 - 3
Toxicity:
• Extracardiac manifestations: fatique, nausea, vomiting, abdominal pain, disturbances of cognitive function, and blurred or yellow vision
• Cardiac: characteristic digitalis arrhythmias: DAD-related tachycardias along with impairment of sinus node or AV nodal function. Atrial tachycardia with AV block is classic, but ventricular bigeminy (sinus beats alternating with beats of ventricular origin), "bidirectional" ventricular tachycardia (a very rare entity), AV junctional tachycardias, and various

70
degrees of AV block also can occur. With severe intoxication (e.g., with suicidal ingestion), severe hyperkalemia owing to poisoning of Na+,K+-ATPase and profound bradyarrhythmias, which may be unresponsive to pacing therapy, are seen.
Treatment of toxicity:
• For tachyarrythmias: infuse KCL 20mmol/hr to max 100mmol. K antagonizes digitalis induced automaticity and decreases binding of digoxin to Na-K ATPase. K contraindicated in presence of AV blocks. Avoided in presence of very high plasma K.
• Ventricular arrhythmias: Lignocaine is drug of choice, repeated as required.
• Supraventricular arrhythmias: propanolol may be given.
• AV blocks and bradycardia: atropine may work temporarily. Temporary pacing may be required.
• Cardioversion should be avoided because severe conduction defects may be unmasked.
• Hemodylasis is not very effective owing to large molecule
• Digoxin antibody (DIGIBIND): the Fab fragment – ultimate antidose
• Sinus bradycardia and AV block often respond to intravenous atropine, but the effect is transient. Mg2+ has been used successfully in some cases of digitalis-induced tachycardia. Any serious arrhythmia should be treated with antidigoxin Fab fragments (DIGIBIND)
Caution • Hypokalemia – enhances toxicity
• Elderly, renal dysfunction/ severe hepatic dysfunction – more sensitive
• MI-arrythmogenic dose is reduced. Should be used after MI only when heart failure is accompanied by AF and rapid ventricular rate
• Thyrotoxicosis – reduces responsiveness + increased incidence of arrhythmias
• Myxoedema – reduced digitalis clearance
• Acute myocarditis – poor response + more arrythmogenic

71
• WPW – digitalis contraindicated
Interactions • Amiodarone, quinidine, verapamil, diltiazem, cyclosporine, itraconazole, propafenone, and flecainide decrease digoxin clearance, likely by inhibiting P-glycoprotein, the major route of digoxin elimination. New steady-state digoxin concentrations are approached after 4 to 5 half-lives, i.e., in about a week.
• Hypokalemia, which can be caused by many drugs (e.g., diuretics, amphotericin B, and corticosteroids), will potentiate digitalis-induced arrhythmias.
• Succinylcholine causes arrhythmias in digitalized pts
• Metoclopramide, sucralfate neomycin, erythromycin reduce absorption
Pharmacokinetics Absorption Oral bioavailability 60-80%
Distribution Plasma protein binding ~ 25%
Volume of distribution 4 to 7 liters/kg. The principal tissue reservoir is skeletal muscle
Metabolism intestinal microflora may metabolize digoxin, markedly reducing bioavailability. Destruction of flora by antibiotics increases bioavailability. Toxicity can occur with drugs like tetracycline/erythromycin
The elimination half-life of digoxin ordinarily is approximately 36 hours
Onset of action – 15-30min
Peak – 2-5hrs
Duration 2-6 days
Excretion Renal elimination of unchanged drug accounts for less than 80% of digoxin elimination.
Digoxin doses should be reduced (or dosing interval increased) and serum concentrations monitored closely in patients with impaired excretion owing to renal failure or in patients who are hypothyroid

72
adenosine
mechanism of action• Nucleoside composed of a molecule of adenine attached to
a ribose sugar molecule (ribofuranose)• Activates acetylcholine-sensitive K+ current in the atrium and sinus and
AV nodes, resulting in shortening of action potential duration, hyperpolarization, and slowing of normal automaticity.
• Inhibits the electrophysiological effects of increased intracellular cyclic AMP that occur with sympathetic stimulation. Because adenosine thereby reduces Ca2+ currents, it can be antiarrhythmic by increasing AV nodal refractoriness and by inhibiting DADs elicited by sympathetic stimulation.
• Intravenous bolus transiently slows sinus rate and AV nodal conduction velocity and increases AV nodal refractoriness.
Pharmacokinetics• Half-life of seconds by carrier-mediated uptake, in most cell types, and
subsequent metabolism by adenosine deaminase. • Dose: 61212 mg, bolus by large bore IV access preferably central. • potentiated by dipyridamole, an adenosine-uptake inhibitor, and in
patients with cardiac transplants owing to denervation hypersensitivity.• Methylxanthines block adenosine receptors; therefore, larger than usual
doses are required Adverse Effects.
• Transient asystole (lack of any cardiac rhythm whatsoever) is common but usually lasts less than 5 seconds and is in fact the therapeutic goal.
• sense of chest fullness and dyspnea • Rarely can precipitate bronchospasm or atrial fibrillation presumably by
heterogeneously shortening atrial action potentials. Magnesium
• Blocks voltage dependent L type Ca2+ channels• Necessary co-factor for membrane enzyme Na+/K+ ATPase. By
reducing the availability of intracellular Na+, reduces the ca inward current and triggered activity. Hence best classified as Na/K pump agonist
• Decreases RMP -> reduced automaticity. APD is increased thereby increasing absolute refractory period and reducing relative refractory period.

73
• Electrophysiological properties enhanced in the setting of increased extracellular K, hence, utility appears greatest in setting of ischemia (loss of intracellular K)
Uses• Acute rate control of AF• Preventive post op SVT• Acute control of MAT• Ventricular arrythmias associated with triggered activity eg. Torsades
& digoxin toxicity• Polymorphic VT induced by class I agents• Very effective at controlling transient ventricular arrythmia in setting
of ischemia eg post infarct and cardiac surgeryDose
• AF rate and MAT control: 0.15 mmol/kg slow IV push. Subsequent dose recommendation has varied from 60 mmol to 0.1 mmol/kg/hr for 24 hrs
• SVT prophylaxis following cardiac surgery: 20-25 mmol / day for 4 days• Transient ventricular arrythmia: 10 mmol slow iv push• LIMIT-2 post MI dose: 8 mmol bolus over 5 min, followed by 65 mmol
over 24 hrs• Plasma levels for potent anti-arrythmic action are atleast 1.8mmol/l
Adverse effects• Rapid bolus hypotension by vasodilatation• Skeletal muscle weakness• Excessive action in the setting of hyperkalemia bradycardia and
heart block
Proarrythmic effects of anti-arrythmic drugs• ‘quinidine syncope’ due to VF and polymorphic VT at therapeutic
concentration (also seen with disopyramide)• CAST trial which involved flecainide, encainide and morizicine was
terminated early because of adverse outcome in flecainide and encainide groups (RR of arrythmic death or non-fatal cardiac arrest of 3.6)
• Most pro-arrythmic events occur soon after starting the drug• Proarrythmia appears to be correlated with the degree of drug induced
QT prolongation or characteristics of sodium channel blockade• Agents with short time constant of sodium channel blockade where
sodium channel blockade is more pronounced at fast hr are less pro-

74
arrythmic than drugs with long time constants (eg flecanide and propafenone)
• Class III drugs and quinindine pr-arrythmia correlate with the degree of QT prolongation
• Reentry is more likely to occur with shorter refractory period and reduced conduction velocity. Class Ib shorten RP. While class 1A and III prolong and hence would be beneficial in re-entry
• The scale of potency of pro-arrythmia has been found to be: flecainide > propafenone > quinidine > disopyramide > procainamide > mexiletine > lidocaine > sotalol
• Anti-arrythmic drugs are effective at suppressing abnormal automaticity with the exception of triggered automaticity due to EAD. Class IA and III can produce proarrythmia due to EAD
• Digoxin can be pro-arrythmic via production of triggered activity due to DAD
INOTROPES & VASOPRESSORS

75
Adrenaline Physicochemical
Structure
Presentation First, epinephrine is unstable in alkaline solution; when exposed to air or light, it turns pink from oxidation to adrenochrome and then brown from formation of polymers. Epinephrine injection is available in 1 mg/ml (1:1000), 0.1 mg/ml (1:10,000), and 0.5 mg/ml (1:2,000) solutions.
Pharmacodynamics MOA potent stimulant of 1, 1 and 2 receptors
Use respiratory distress due to bronchospasmrapid relief of hypersensitivity reactions, including anaphylaxisProlong the action of local anesthetics, presumably by decreasing local blood flow cardiac arresttopical hemostatic agent on bleeding surfaces such as in the mouth or in bleeding peptic ulcers during endoscopyinhalation of epinephrine may be useful in the treatment of postintubation and infectious croup. Refractory shock especially where both inotropic & vasoconstrictive effects are desired
Dose Usual S/C dose 0.3 to 0.5 mg.
Dose in cardiac arrest 1mg IV boluses
Anaphylaxis, 1ml boluses of 1:10000 soln
1% (10 mg/ml; 1:100) formulation is available for inhalation.
IV infusions 2-5µg/min for shock.
CVS Blood Pressure.
IV blous of normal dose ↑systolic > ↑diastolic, ↑ pulse pressure. As the response wanes, the mean pressure may fall below normal before returning to control levels.
mechanism: (1) positive inotropic action (2) positive chronotropic action and (3) vasoconstriction in many vascular bedsespecially in the precapillary resistance vessels of skin, mucosa, and kidneyalong with marked constriction of the veins. ↑HR ↑BPvagal discharge ↓HR

76
IV bolus of low dose (0.1 g/kg) ↓BP. Reason greater sensitivity to 2 receptors than receptors
Slow IV infusion or S/C adrenaline ↓peripheral resistance owing to dominant action on 2 receptors of vessels in skeletal muscle ↓ diastolic BP & ↑blood flow. ↑ systolic pressure due to ↑HR, SV, and CO ↑blood flow ↑ venous return, ↑ RAP. At higher doses of infusion α actions predominate and ↑ TPR.
Vascular Effects.
Marked ↓ cutaneous blood flow. constricting precapillary vessels and small venules
↓ renal blood flow by as much as 40%
Blood flow to skeletal muscles ↑ by therapeutic doses. 2 effect > α effect. At higher doses α effect predominates.
Arterial and venous pulmonary pressures ↑due to direct pulmonary vasoconstriction + redistribution of blood from the systemic to the pulmonary circulation pulmonary edema can occur
Coronary blood flow ↑ under physiological conditions. Cause: ↑ diastolic time, ↑blood pressure, ↑myocardial O2 demand metabolic vasodilatation mediated by adenosine.
Cerebral circulation does not constrict in response to arenaline. Autoregulation limits ↑ in CBF
Cardiac Effects.
predominant 1 stimulation. ↑HR, ↑SV, ↑CO, ↑work & O2 consumption. Cardiac systole is shorter.
↓ Cardiac efficiency (work done relative to oxygen consumption)
Pro-arrythmic :
Activates latent pacemakers, ↑ automaticity. ↑ slope of phase 4 depolarization, ↑ amplitude and rate of phase 0 depolarization seen in conducting fibres. Not in atrial and ventricular muscle fibres.
↓ refractory period of AV node by direct effects. However reflex vagal discharge may indirectly tend to prolong it.

77
CNS Poor penetration. At therapeutic doses restlessness, apprehension, headache, and tremor due to effects on cardiovascular system
Respiratory Relaxes bronchial muscle (β2 effect).
Inhibition of antigen-induced release of inflammatory mediators from mast cells (β effect), diminution of bronchial secretions and congestion within the mucosa (effect.
Other Smooth Muscles.
Gastrointestinal smooth muscle – relaxed. Pyloric and ileocecal sphincters are contracted, but these effects depend on the preexisting tone of the muscle. If tone already is high, epinephrine causes relaxation; if low, contraction.
During the last month of pregnancy and at parturition, epinephrine inhibits uterine tone and contractions (2 effect)
Urinary bladder: relaxes detrusor muscle ( effect) and contracts the trigone and sphincter muscles ( effect).
Metabolic Effects.
20% to 30% ↑ in oxygen consumption
Hyperglycemia
↑ lactate
↑insulin secretion due to 2 receptors , ↓ insulin secretion due to α receptors. Predominant effect is inhibition.
↑Glucagon secretion ( receptors on cells of pancreatic islets).
↓ uptake of glucose by peripheral tissues
↑ glycogenolysis ( receptors)
↑ free fatty acid conc. ( receptors in adipocytes)
Renal: ↓RBF. Since the glomerular filtration rate is only slightly and variably altered, the filtration fraction is consistently increased. Excretion of Na+, K+, and Cl- is decreased. The secretion of renin is increased as a consequence of a direct action of epinephrine on 1 receptors in the juxtaglomerular apparatus.

78
Miscellaneous
↑ number of circulating polymorphonuclear leukocytes
accelerates blood coagulation and promotes fibrinolysis.
Stimulates lacrimation and a scanty mucus secretion from salivary glands.
Mydriasis
lowers intraocular pressure
increase physiological tremor, at least in part due to receptor-mediated enhancement of discharge of muscle spindles.
Epinephrine promotes a fall in plasma K+, largely due to stimulation of K+ uptake into cells.
Side effects/adverse effects
restlessness, throbbing headache, tremor, and palpitations.
cerebral hemorrhage and cardiac arrhythmias.
Angina may be induced by epinephrine in patients with coronary artery disease.
Contraindicated in patients who are receiving nonselective receptor blocking drugs, since its unopposed actions on vascular 1 receptors may lead to severe hypertension and cerebral hemorrhage.
Interactions
Pharmacokinetics Absorption Not effective orally. Rapidly conjugated and oxidized in the GI mucosa and liver.
Absorption from subcutaneous tissues occurs relatively slowly, more rapid after intramuscular injection. In emergencies, it may be necessary to administer epinephrine intravenously.
DistributionMetabolism
Rapidly inactivated. The liver is rich in both of the enzymes responsible for destroying circulating epinephrine (COMT and MAO).
Excretion only small amounts appear in the urine

79
Noradrenaline Physicochemical
Structure
Presentation 1 mg/mL for injection
Pharmacodynamics MOA Major chemical mediator liberated by mammalian postganglionic sympathetic
nerves
Sympathomimetic
• Acts on both & 1- receptors but has relatively little effect on 2-receptors
• Like adrenaline: low dose predominantly beta effect; higher dose alpha
• Causes i) vasoconstriction [-receptor]
ii) Inotrope [1-receptors]
iii) Chronotrope [1-receptors]
• Consequently increases systemic BP and coronary artery blood flow
Use In the treatment of low blood pressure, the dose is titrated to the desired pressor response.
Dose 0.06-0.15µg/kg/min
CVS ↑Systolic, diastolic and pulse pressureCO - unchanged or decreased↑ TPRvagal reflex activity ↓ HR↓ renal blood flowConstricts mesenteric vessels and ↓ splanchnic and hepatic blood flow. Coronary flow ↑
CNSRespiratory Other hyperglycemia and other metabolic effects similar to those produced by
epinephrine but these are observed only when large doses are given because
Clinical effects offset by increased afterload

80
norepinephrine is not as effective a "hormone" as epinephrine.
Side effects/adverse effects
severe hypertension
necrosis and sloughing can occur at the site of intravenous injection owing to extravasation of the drug. The infusion should be made high in the limb, preferably through a long plastic cannula extending centrally. Impaired circulation at injection sites, with or without extravasation of norepinephrine, may be relieved by infiltrating the area with phentolamine, an receptor antagonist.
Caution:
• Should not be mixed in saline alone [water O.K.]• Risk of arrhythmias with volatile anaesthetics• Give with caution to patients on MAO or tricyclics as will prolong action
Interactions • Should not be mixed in saline alone [water O.K.]• Risk of arrhythmias with volatile anaesthetics• Give with caution to patients on MAO or tricyclics as will prolong action
Pharmacokinetics Absorption ineffective when given orally and is absorbed poorly from sites of
subcutaneous injection DistributionMetabolism Rapidly inactivated. The liver is rich in both of the enzymes responsible for
destroying circulating epinephrine (COMT and MAO).
Excretion Small amounts normally are found in the urine
Evidence
some survival benefit in septic shock, compared with high-dosage dopamine and epinephrine
epinephrine norepinephrine
Heart rate + -
Stroke volume ++ ++
Cardiac output +++ 0/-
Arrhythmias ++++ ++++
Coronary blood flow ++ ++

81
Systolic BP +++ +++
MAP + ++
Diastolic BP +/0/- ++
Mean PAP ++ ++
TPR -/+ ++
Cerebral blood flow ++ 0/-
Muscle blood flow +++ 0/-
Skin blood flow -- --
Renal blood flow - -
Splanchnic blood flow - 0/-
Oxygen demand ++ 0/+
Blood glucose +++ 0/+
Blood lactate +++ 0/+
Vasopressin Physicochemical
Structure nonapeptide with a 6-amino-acid ring and a 3-amino-acid side chain.
Presentation Inj 20 U/ml
Pharmacodynamics MOA Vasopressin is a peptide hormone released by the posterior pituitary in response
to rising plasma tonicity or falling blood pressure. Vasopressin possesses antidiuretic and vasopressor properties. Acts via G protein coupled V1 and V2 receptors. It exerts its circulatory effects through V1 (V1a invascular smooth muscle, V1b in the pituitary gland) and V2receptors (renal collecting duct system; Table). V1a stimulationmediates constriction of vascular smooth muscle,whereas V2 receptors mediate water reabsorption by enhancingrenal collecting duct permeability.
Use Cardiac arrestVasopressor sparing/catecholamine hyposensitivity in shock statesBleeding esophageal varices
Dose 0.01 to 0.05 units/min40 U boluses in cardiac arrest
CVS Vasopressin causes less direct coronary and cerebral vasoconstrictionthan catecholamines and has a neutral or inhibitory

82
impact on CO, depending on its dose-dependent increasein SVR and the reflexive increase in vagal tone. Avasopressin-modulated increase in vascular sensitivity tonorepinephrine further augments its pressor effects. The agentmay also directly influence mechanisms involved in thepathogenesis of vasodilation, through inhibition of ATP-activatedpotassium channels, attenuation of nitric oxideproduction, and reversal of adrenergic receptor downregulation. The pressor effects of vasopressin are relativelypreserved during hypoxic and acidotic conditions, whichcommonly develop during shock of any origin.
CNS does not penetrate BBBRespiratory Other
Side effects/adverse effects
Allergic reactions & anaphylaxis
Cardiac arrest, circumoral pallor, arrhythmias, decreased cardiac output, angina, myocardial ischemia, peripheral vasoconstruction and gangrene.
Gastrointestinal: abdominal cramps, nausea, vomiting.
Nervous System: tremor, vertigo, palpitations
Respiratory: bronchial constriction.
Skin and Appendages: sweating, urticaris, cutaneous gangrene
Interactions Drugs which potentiate antidiuretic effect: carbamazepine; chlorpropamide; clofibrate; urea; fludrocortisone; tricyclic antidepressants.
Drugs which decrease the antidiuretic effect of vasopressin: demeclocyline; norepinephrine; lithium; heparin, alcohol.
Ganglionic blocking agents may produce a marked increase in sensitivity to the pressor effects of vasopressin.
Pharmacokinetics Absorption Orally destroyed by trypsinDistributionMetabolism T1/2 10 to 20 minutes. Metabolized by enzymatic cleavage in many
organs especially liver and kidney Excretion
Dobutamine Physicochemical

83
Structure
Presentation 12.5mg/ml Injection
Pharmacodynamics MOA strong +ve inotropy due to beta1 agonist effects and
alpha1 agonism- mild +ve chronotropy due (+) isomer effect on beta receptors- weaker alpha receptor blockade and beta2 stimulation, produced by (+) isomer and alpha1 agonism produced by(-) isomer- overall peripheral effect should be an increase in blood flow to skeletal muscle (beta2 agonism) and some reduction in skin blood flow (alpha1 agonism balanced by some alpha blockade). These effects are weak compared to the myocardial effects- net effects are an increase in SV and CO. SVR may be unchanged or moderately decreased and arterial pressure may thus rise, fall slightly or remain unchanged- at doses > 15 mcg/kg/min tachycardia and arrhythmias are more likely- tolerance may be seen after 48-72 hrs, presumably due to down-regulation of beta receptors. May necessitate an increase in dose. Dose required to produce toxic effects seems to be increased equivalently
Use Dose
CVSCNSRespiratory Other
Side effects/adverse effects
tachycardia and tachyarrhythmias less frequent than with dopamine- enhances AV conduction and may precipitate AF in predisposed patients
Interactions
Pharmacokinetics

84
Absorption DistributionMetabolism Onset of action within 2 min and maximal effect associated
with a given infusion rate occurs approximately 10 min after starting the infusion. metabolized by COMT to. t1/2 2.3 min
Excretion inactive metabolites which are excreted in the urine
DopaminePhysicochemical
Structure
Presentation 200mg ampule
Pharmacodynamics MOA Acts on D1, D2, α and β1 receptors
D1 receptors in renal and mesenteric blood vessels are most sensitive-at low doses-increased blood flow->↑GFR↑Na excretion Higher doses stimulate β1 receptors inotropic actionsLarge doses have predominant αactions vasoconstriction
Use CHF, particularly in patients with oliguria and low or normal peripheral vascular resistance. Cardiogenic and septic shock.
Dose Dopamine hydrochloride is used only intravenously. The drug initially is administered at a rate of 2 to 5 g/kg per minute; this rate may be increased gradually up to 20 to 50 g/kg per minute or more as the clinical situation dictates
CVS At low doses (1 to 3 µg/kg per min) Vascular D1 receptors in in the renal, mesenteric, and coronary beds activates adenylyl cyclase, ↑cAMP vasodilation ↑ GFR, renal blood flow, and Na+ excretion. Total peripheral resistance usually is unchanged
At higher conc. (3 to 10 µg/kg per min) 1 receptors +ve inotropic actions, release of norepinephrine from nerve terminals ↑SBP & pulse pressure, minimal effect on DBP.
At ever higher conc. (10 to 20 µg/kg per min) predominant

85
activation of vascular 1 receptors generalized vasoconstrictionCNS Poor penetration – no effectRespiratory Other
Side effects/adverse effects
Nausea, vomiting, tachycardia, anginal pain, arrhythmias, headache, hypertension, and peripheral vasoconstriction
Extravasation ischemic necrosis and sloughing.
Rarely, gangrene of the fingers or toes
Interactions MAO inhibitor, TCA
Pharmacokinetics Absorption ineffective when administered orallyDistributionMetabolism Dopamine is a substrate for both MAO and COMT
Excretion
evidence
Published data in sepsis suggest that dopamine may impair hepatosplanchnicNo benefit of renal dose dopamine
IsoprenalinePhysicochemical
Structure
Presentation 1000 microgram/5mL
Pharmacodynamics MOA activating β1 and β2 receptors equally
Use To treat shock, cardiac arrest, bradyarrythmias, bronchospasmDose 0.05 - 0.5 microgram/kg/minute
CVS positive chronotropic, dromotropic, and inotropic effect ↑SBP. In skeletal muscle arterioles it produces vasodilatation ↓DBP
CNSRespiratory relaxation of bronchial smooth muscle

86
Other
Side effects/adverse effects
Tachycardia – continuously monitor heart rate.
Cardiac dysrhythmia, hypertension, hypotension, vomiting, tremor.
Interactions
Pharmacokinetics Absorption DistributionMetabolism T1/2 ~2hrs
Excretion
milrinonePhysicochemical
Structure
Class Phosphodiesterase inhibitorPresentation Injection, solution: 1 mg/mL (10 mL, 20 mL, 50 mL)
Pharmacodynamics MOA phosphodiesterase III inhibitors potentiates the effect of cyclic adenosine
monophosphate (cAMP).Milrinone also enhances relaxation of the left ventricle by increasing Ca2+-ATPase activity on the cardiac sarcoplasmic reticulum. This increases calcium ion uptake.
Use Cardiogenic shockPulmonary hypertension eg with PE
Dose Adults: I.V.: Loading dose (optional): 50 mcg/kg administered over 10 minutes followed by a maintenance dose titrated according to the hemodynamic and clinical response; Maintenance dose: I.V. infusion: 0.375-0.75 mcg/kg/minute.If hypotension is a problem, loading doses may be omitted and maintenance infusions initiated. There is some delay in hemodynamic effects, but it is minimal (1-3 hours).

87
Monitoring ParametersPlatelet count, CBC, electrolytes (especially potassium and magnesium), liver function and
renal function tests; ECG, CVP, SBP, DBP, heart rate; infusion site
CVS +ve inotropic and vasodilatation CNSRespiratory Other
Side effects/adverse effects
>10%: Cardiovascular: Ventricular arrhythmia (ectopy 9%, NSVT 3%, sustained ventricular
tachycardia 1%, ventricular fibrillation <1%)
1% to 10%:
Cardiovascular: Supraventricular arrhythmia (4%), hypotension (3%), angina/chest pain (1%)
Central nervous system: Headache (3%)
<1% (Limited to important or life-threatening): Atrial fibrillation, hypokalemia, MI,
thrombocytopenia, tremor, ventricular fibrillation
Postmarketing and/or case reports: Anaphylaxis, bronchospasm, injection site reaction, liver
function abnormalities, rash, torsade de pointes
Interactions no known significant interactions
Pharmacokinetics Absorption Good Oral absorption Distribution Onset of action: I.V.: 5-15 minutes
Distribution: Vdss: 0.32-0.45 L/kg
Protein binding, plasma: ~70%
Metabolism Metabolism: Hepatic (12%)
Half-life elimination: Normal renal function: ~2.5 hours; CVVH: 20.1 hours (Taniguchi, 2000)

88
Excretion Excretion: Urine (85% as unchanged drug) within 24 hours; active tubular secretion is a
major elimination pathway for milrinone
levosimendanPhysicochemical
Structure
Class Calcium sensitizerPresentation 2.5 mg
per 5 mL per ampoule and 10mL per ampoule
Pharmacodynamics MOA does not increase intracellular
concentrations of free calcium. It binds to cardiactroponin C in a calcium-dependent manner andstabilises troponin C. This causes actin-myosincross-bridges, without increasing myocardialconsumption of adenosine triphosphate (ATP). Also opening of ATP-dependent potassium (K_) channels causes vasodilatation
Use indicated for inotropic support in acutely-decompensated severe congestive heart failure
Dose 6 to12 μg/kg loading dose over 10 minutes followed by0.05 to 0.2 μg/kg/min as a continuous infusion
CVS enhance cardiac contractility. No arrythmogenic potential. venous, arterial andcoronary vasodilation, probably by opening ATPsensitivepotassium channels in smooth muscle.
CNSRespiratory Other
Side effects/adverse effects
Tachycardia, enhanced AV conductionHypotension

89
Interactions No significant interactions
Pharmacokinetics Absorption well
absorbed orallyDistribution 98% bound to plasma proteins
Metabolism 5% dose is converted in intestines to highly active metabolite with t1/2 75-80h. Effects after infusion hence may persist 7-9 days after stopping infusion. T1/2 of levosimendan otherwise is 1hr.
Excretion
Evidence
Some of the Phase-III studies in the extensive clinical program were the trials LIDO (200 patients), RUSSLAN (500), CASINO (250), REVIVE-I (100), REVIVE-II (600) and finally SURVIVE (1350),[1] a head-to-head trial between levosimendan and dobutamine in acute decompensated heart failure. levosimendan did not significantly reduce all-cause mortality at 180 daysIn the randomised Levosimendan Infusion versus Dobutamine (LIDO) trial in 203 patients with severe, low-output decompensated CHF,[10] significantly more patients in the levosimendan group achieved the primary efficacy end-point of an increase from baseline in cardiac index ≥ 30% and a decrease in PCWP ≥ 25% than in the dobutamine group (5 to 10 µg/kg/min for 24 hours) [28 and 15%, respectively].



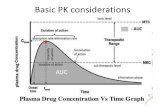












![NANOSUSPENSION: BIOAVAILABILITY ENHANCING NOVEL … · or previous GI surgery (e.g. bariatric surgery) can also affect drug bioavailability [23]. Improvement of bioavailability: The](https://static.fdocuments.us/doc/165x107/5eb46ef2a9b685351d4067b1/nanosuspension-bioavailability-enhancing-novel-or-previous-gi-surgery-eg-bariatric.jpg)


