Validation of Terminal Sterilization.pdf
Transcript of Validation of Terminal Sterilization.pdf

13
Validation of Terminal SterilizationThomas J. Berger and Kevin D. TruppDepartment of Microbiology and Global Process Sterilization Engineering, Hospira, Inc.,
Lake Forest, Illinois, U.S.A.
INTRODUCTION TO PARENTERAL PRODUCTSTERILIZATION
The previous chapter discussed the steam sterilizationapproach for the processing of hard goods or porousloads. This chapter will discuss the sterilization vali-dation approach that can be used in the processing ofparenteral products by terminal sterilization using moistheat. The underlying principles of steam sterilization areapplicable to both hard goods and terminal sterilizationof parenteral products, but both have their uniquecharacteristics.
An organized sequential flow of activities mustoccur as new parenteral formulations are developed,and subsequently processed in the manufacturing facility.The moist heat sterilization of pharmaceutical solutions isestablished and verified through a series of activities thatconfirm the product has received a defined thermalexposure that renders the product sterile. R&D activitiescan include sterilization developmental engineeringstudies consisting of sterilization cycle development;container thermal mapping; microbial closure validation,D- and z-value analysis; container–closure integrity vali-dations as well as final formulation stability studies.
The subsequent production phase activities mustinclude initial sterilization vessel qualification whichdemonstrates that the vessel will deliver the definedsterilization process in a consistent and reproduciblemanner. Also, solution and container–closure microbialvalidation studies must be conducted at subprocessproduction sterilization conditions employing heat-resistant microorganisms. Equipment validation,filtration studies and assessment of the bioburden on
component parts, as well as the environment, must alsobe ascertained.
The developmental and production phases of ster-ilization technology activities are then drafted intodocuments that are submitted as part of a new drugapplication for the particular parenteral formulation.These reports must follow applicable regulatory require-ments for products that are terminally sterilized. Suchstudies allow one to establish, with a high levelof sterilization assurance, the correct sterilization cycle(F0, temperature, product time above 1008C, etc.) to beused for the steam sterilization of a specific parenteralformulation in a particular container–closure system.
STERILIZER DESIGN
The validation of a steam sterilization cycle is dependenton the equipment chosen. The sterilizer and its supportsystems must be designed and constructed to deliver theeffective cycles repeatedly and consistently. Qualificationof the sterilizer consists of proper design, installationaccording to design, operational testing to ensure thatdesign criteria and operational requirements are met andperformance qualification to confirm that the product issterilized per specification.
Sterilizer design is geared to the type of product ormaterials/equipment to be sterilized. All steam steriliza-tion cycles are based on contact with saturated steam,steam–air mixtures or superheated water. Saturatedsteam is water vapor in equilibrium with liquid water.The values of temperature and pressure at which puresaturated steam can exist are shown by the phasediagram in Chapter 12, Figure 3. Saturated steam canexist only along the phase boundary for liquid andgaseous water; that is, the relation between its tempera-ture and pressure is fixed. An increase or reduction in thetemperature of saturated steam must result in a corre-sponding increase or decrease in its pressure and viceversa. Steam–air mixtures can be usedwhen overpressureis required to maintain product shape or containerintegrity. Superheated water cycles require air overpres-sure and the water is either heated by direct injection ofsteam or indirectly via a heat exchanger.
Parts and hard goods are typically steam sterilizedusing a saturated steam process whereas the trend forproduct sterilization is towards the use of superheatedwater or steam–air mixture processes. These processes areneeded as a majority of the new products require airoverpressure during the sterilization process to maintaindesired container characteristics and integrity.
Abbreviations used in this chapter: AAMI, Association for theAdvancement of Medical Instrumentation; APE, antimicrobialpreservative efficacy; API, active pharmaceutical ingredient;ASME, American Society of Mechanical Engineers; BET, bacterialendotoxin testing; BI, biological indicator; BIER, biologicalindicator evaluator resistometer; DP, direct plate; EMA, EuropeanMedicinal Agency; F/N, fraction/negative; GAMP, good auto-mated manufacturing practice; HMI, human–machine interface;I/O, input/output; ICH, International Conference on Harmoniza-tion; ISPE, International Society for Pharmaceutical Engineering;LAL, limulus amebocyte lysate; LVP, large volume parenterals;MES, manufacturing execution system; MOS, maintenance ofsterility; P&D, penetration and distribution; PLC, programmablelogic controller; PSLR, predicted spore logarithmic reduction; R&D,research and development; RTD, resistance temperature detector;SCADA, supervisory control and data acquisition; SLR, sporelogarithmic reduction; SVP, small volume parenterals; TC,thermocouple.

Products in glass containers can utilize the satu-rated steam processes as described in Chapter 12, butmany products and containers require the use of airoverpressure during the sterilization process. Thissection will discuss some of the key design considerationsfor terminal steam sterilizers and provide some specificsfor the various type steam sterilization processes utilizingair overpressure.
Typical Design Considerations for Steam Sterilizers
1. A pressure vessel constructed according to theASME or equivalent international code. This mustwithstand at least 50% in excess of the requiredinternal pressures.
2. A safety door mechanism to prevent opening whilethe unit is under pressure: the locking device may beactuated directly by internal pressure or indirectlythrough an automatic switch. The door itself may beof the swing-out or sliding type. Separate entry andexit doors are preferable.
3. Process control system (typically a PLC for control-ling and monitoring the process).
4. Process data recorder or data collection system.5. Product racks designed to hold/support the sealed
product containers and to provide adequateheating/cooling media flow throughout theproduct zone.
6. Pressure safety relief valves for both the chamber andjacket (if equipped with jacket).Note. A microbial retentive vent/air filter would not
typically be required for processes used for terminalsterilization as there is no direct contact between theheating/cooling media and the contents of the containers.
Steam Air Mixture SterilizationThe primary benefit to the steam–air mixture process overa superheated water process is the product is notsubjected to direct contact with water (except as conden-sate), which in some cases can cause cosmetic issues withthe container. Steam–air mixture processes typicallyutilize large recirculating fans to prevent the formationof cold/hot spots in the sterilizer. The steam–air mixtureprocess typically uses an indirect cooling method such ascooling of the jacket or with cooling coils within thesterilizer. Because of this indirect cooling method, thecooling rate of the product is typically much slower andless efficient than direct exposure of the productcontainers to cooling water.
Some of the specific sterilizer design considerationsfor a steam–air mixture process include the following:1. A jacket and insulation: the jacket would utilize steam
during heating and exposure phases of the cycles andcooling water can be introduced to the jacket duringthe cooling phase of the process.
2. A thermostatic steam trap to efficiently remove thecondensate from the chamber: this is open when cool(in contact with air or condensate) and closed when incontact with steam. As condensate collects, the trapopens owing to the slight temperature reduction andthe condensate is discharged. There is also a similarsteam trap to remove steam condensate fromthe jacket.
3. Fan(s) to continuously recirculate the steam–airmixture during heat-up and exposure and to recircu-late the air during cooling.
4. Cooling provisions (e.g., cooling coils) to cool theair/product.
Recirculated Superheated Water SterilizationSterilization with recirculating superheated water (some-times referred to as a water cascade or raining process) ismore efficient than a steam–air mixture and is thereforemore common. There are many types of recirculatingsuperheated water processes, the most common is aprocess where the bottom portion of the sterilizer(below the product zone) is filled with water and arecirculation pump is used to continuously recirculatewater from the bottom of the sterilizer to spray nozzlesabove the product zone. A slight modification to thatprocess is the use of a water distribution pan in lieu ofspray nozzles. Another version of the recirculatingsuperheated water process is to completely submergethe product in water but this process is inefficient froma utilities consumption standpoint. All of these recircu-lating superheated water processes utilize airoverpressure and the overpressure can be controlledduring the sterilization process to minimize most typesof container deformation. There is no limit to themaximum overpressure used but it would typically belimited by the chamber pressure rating. The minimumoverpressure will be driven by the temperature beingused, the pressure needed to maintain the desiredproduct characteristics and the required overpressureneeded to prevent the recirculation pump from loosingprime. These recirculating processes are typically heatedand cooled indirectly with external heat exchangerslocated in the recirculating water loop but direct injectionof steam and cooling water can also be used.
In addition to the typical sterilizer design consider-ations mentioned earlier, a superheated water sterilizerwould also include a large recirculating water system(e.g., pump, pipes, heat exchangers, headers, spraynozzles) including specific water level control valvesand monitoring devices.
Rotary and Shaker SterilizationIn some cases, certain products (i.e., suspensions andemulsions) require agitation during the sterilizationprocess. For those types of products, it is typical to use arotating rack within the sterilizer but other agitationmethods such as an internal shaking device are available.Refer to Figure 1 for the typical design of a rotary sterilizerand Figure 2 for the typical design of a sterilizer usinga shaking mechanism. It is possible to use any of thesterilization processes listed abovewith product agitation.
Continuous SterilizationFor this version of the superheated water process,containers are terminally heat sterilized in a continuoussterilizer by a processwhere the containersmove through aconstantly controlled environment in carriers with individ-ual compartments. The time, temperature, and pressurerequirements are set to predetermined values and areautomatically and continuously controlled, monitored,and recorded. Refer to Figure 3 which depicts the pattern
188 III: STERILIZATION, SANITIZATION AND STERILITY ASSURANCE

that containers (e.g., parenteral flexible product containers)follow as theymove automatically through the continuoussterilizer. The water lock of the pressure vessel is used toprovide product entrance into and out of the overpressureenvironment. The overpressure environment is constantlymaintained within predetermined limits.
The sterilizing phase begins as the product entersthe hot water environment within the pressure vessel.The hot water environment may be a superheated water
spray, which is circulated over the top of the continuouslymoving carriers. The residence time of the product withinthis sterilizing environment and the water temperatureare controlled within predetermined limits to assure therequired heat input.
Cooling begins as the product transfers from thesterilizing environment and enters the cooling environ-ment, which is also within the pressure vessel. Thecooling water environment is a cool water spray that iscirculated over the top of the continuously movingcarriers. The temperature of this water is controlledwithin predetermined limits to assure that the requireddegree of cooling is achieved before the product leavesthe cooling environment.
A system offixed temperature sensors located in theentering and exiting recirculating water for both heatingand cooling continuously monitors, records, and controlsthe temperature of the process water.
Air overpressure is required to protect the con-tainer from stress while exposed to the high sterilizingtemperatures.
STERILIZER CONTROL SYSTEMS
A key to effective sterilizer operation lies in the auto-mated process control system. By eliminating thedependence on operator intervention and data recording,automatic temperature and sequential control providesassurance that the “validated” sterilization cycle isconsistently and repeatedly delivered. A typical controlsystem for a new sterilizer includes the following hard-ware components:& PLC& Operator interface panel(s)& Data recorder/data collection system& Process Variable Sensors& I/O devices
The PLC is most commonly used as the primarycomponent of the automated process control system as itprovides sequential control of the process, providescontrol of all proportional valves, controls all devices,receives operator input via the operator interface panelsand provides process information (such as process vari-able information and alarms) to the operator via displaysand/or operator interface panels. The PLC typicallycontains specific recipe information for the variouscycles to be utilized. In some cases the PLC can be usedfor data collection, but it is much more common to use aseparate data recorder/data collection system.
The operator interface panel can be as simple asswitches and displays or as complex as a stand-alone PCrunning a SCADA with a HMI software package. Thesedevices are typically used to select the recipe, start thecycle and display process information during the cycle.The higher level PC based SCADA type operator inter-face panels can provide detailed cycle reports andtrending information.
The data recorder/data collection system can rangefrom a simple strip chart recorder to a full-blown MEStype data collection system. In many cases the PLC canalso provides batch data logging functionality. Theminimum variables to record for steam sterilizationprocesses are typically time, temperature, and pressure.
Figure 1 Photo of sterilizer with a rotary mechanism. Source:
Photo Provided by Fedegari Autoclavi SpA, Albuzzano, Italy.
Suspension Rods
Platform Frame
Platform Lock Arm
Bridge PlatePlatform Rails
Lock Screw
Figure 2 Photo of sterilizer with a shaking mechanism.
13: VALIDATION OF TERMINAL STERILIZATION 189

Typical sensors include temperature measurementdevices (RTDs or TCs), pressure measurement devices,and where applicable level measurement devices andflow measurement devices. It is customary that thetemperature sensor used to control the process tempera-ture not be used to provide the batch record process data.An independent/secondary temperature sensor for batchreporting provides a high degree of insurance that thecycle actually ran within its defined limits. Heavy wallthermowells should not be used, as this will affect thetime response of the measurement. Thin-walled thermo-wells or temperature elements with stainless steel sheathsshould be used for temperature measurement.
The pressure sensor should be equipped with asanitary-type diaphragm and connected to the sterilizerusing a sanitary fitting. A sanitary diaphragm can intro-duce errors to the pressure measurement due to thestiffness of the diaphragm. This stiffness is related to thesize of the diaphragm. The impact is negligible fordiaphragms above 3 inches diameter. This should beconsidered when sizing the connection to the sterilizer.
Sterilizers that maintain a specific water level (i.e.,recirculatedwater process) should be equippedwith liquidlevel sensors. These sensors may be in the form of single-point-level-typeprobeora continuous level sensor.Regard-less ofwhat type sensor is used a separate high-level sensormust also be provided. The separate high-level sensorprovides greater assurance that the collected water at thebottom of the vessel remains below the product level.
Sterilizers that rely on recirculated water as part ofthe sterilization process can include a flow sensor. Theflow sensor may be a direct measurement such as a flowmeter (i.e., coriolis, ultrasonic, magnetic, etc.) or anindirect measurement such as differential pressuresensor across the recirculation pump. Direct measure-ments are always preferred.
For I/O devices, there are analog types and discretetypes. The analog inputs are typically from processsensors and the analog outputs are typically for controlof proportional valves. The discrete inputs are typicallyfrom switch type (operator and process) devices and thediscrete outputs are typically for activating hardwaresuch as valves, pumps, lights, etc.
The design and development of the sterilizercontrol system software should follow the principles ofISPE GAMP 4 Guide for Validation of AutomatedSystems (1). This guideline details a software life cyclefrom conception thru decommissioning.
STERILIZATION CYCLES
The type of steam sterilization cycle to be utilized isdependent on product needs and equipment availability.As discussed in Chapter 12, the sterilization of hard goodsor porous loads typically require the use of a pulsed pre-vacuum cycle as it is preferable to remove the air from theporous materials being sterilized whereas in the terminalsterilization of aqueous solutions in sealed containers,
Steam FlowrateSensor
Pump
Surge Tank
EntryLock
Take-Up
Indexer
Shuffle
Unloading
Surge Tank
Heaters
Sterilizing Tank
PumpPumpOzone
Tower WaterPump
Surge Tank
Cooling Tank
Temperature
Sensor
TemperatureSensor
MixingTank
ExitLock
Tower WaterHeat Exchangers
Figure 3 Schematic of a sterilizer for “continuous” processing of flexible containers.
190 III: STERILIZATION, SANITIZATION AND STERILITY ASSURANCE

the major concern is to provide rapid heat transfer to thewall of the filled product containers and air removal is notrequired (nor even desirable as the hydrating moisture iscontainedwithin each container). Parenteral products maybe filled into rigid or flexible containers. In either there istypically air or nitrogen present in the headspace above theliquid. As the solution is heated, this gas expands and addsto the internal pressure increase resulting from theevolution of water vapor from the aqueous vehicle withinthe heated container. Thus, the pressure within thecontainer will exceed the chamber pressure during steamprocess for sealed containers.
Glass vials can be sealed with special closures towithstand this pressure. As long as the pressure differ-ential between the chamber and the containers does notbecome too great during the steam exhaust portion of thecycle, the vials will not burst. If rapid cooling of the loadis desired, the pressure differential might become signi-ficant enough to cause closure integrity to be lost.
Plastic bags, semi-rigid containers and syringespresent a greater problem because they do not have theinherent strength of glass and may burst or deform as thepressure differential increases. To prevent this, air must beinjected into the chamber to raise the pressure above thesaturation pressure of the steam. This is particularlyimportant during the cooling cycle, when the chamberpressure is reduced at a much faster rate than that withinthe container.
The following section provides a description of thevarious steam sterilization cycles used for parenteralproducts in sealed containers.
Saturated Steam Pre-Vacuum CycleFor a saturated steam process, the most common (andperhaps most effective) method to remove the entrappedair from the sterilizer is to remove it mechanically beforethe actual sterilization begins. This is done by means of amechanical vacuum pump or steam eductor. This cyclecan be used for products in glass containers. A sketch of atypical pre-vacuum cycle is shown in Chapter 12,Figure 7.
Saturated Steam Gravity Displacementor Steam Purge CycleOther means for eliminating air without a vacuumsource include the use of a gravity displacement cycleor a steam purge cycle. For the gravity displacementcycle, steam is introduced on the side or top of thevessel and the cold air is forced out via the drain. Thesteam purge cycle uses large quantities of steam distrib-uted via headers under the entire product zone withnumerous large vents located at the top of the vessel.For these types of cycles, the appropriate vents or drainsshould be fully open and the large steam supply valvefully open for an extended time and temperature toensure that the air is adequately removed from thesterilizer. Once the vents and drains close, the processruns like a traditional saturated steam process. It isimportant to determine that the measured temperatureand pressure are consistent with the steam saturationcurve in Chapter 12, Figure 3. This process can be usedwith glass containers.
Steam Air Mixture CycleIt is important to understand the physical principleinvolved in a mixture of steam and air. The fixed rela-tionship between temperature and pressure seen inChapter 12, Figure 3 no longer applies. Dalton’s lawstates that the pressure of an ideal mixture of gases isequal to the sum of the partial pressure of the gases, or
PZPACPBCPC:
Raoult’s law further states that, for ideal mixtures,the partial pressure of the gas is equal to its vapor pressuremultiplied by the mole fraction in the liquid. For steam inequilibrium with pure condensate, this reduces to
PAZ pA
where PA is the partial pressure of steam and pA is thevapor pressure of the condensate. The difference betweenthe observed chamber pressure P and PA is the partialpressure of air.
The presence of air, although necessary for themaintenance of container integrity, can reduce the heattransfer efficiency. The objective of the design in the“air overpressure” cycle is to maintain a well-mixedchamber. This assures that the heat transfer to the loadwill be uniform regardless of the presence of air. Mixingmay be accomplished in several ways. The air may beinjected directly into the incoming steam. Usually,though, some mechanical means is selected.
Most steam–air sterilizers use a fan built into the topor end of the chamber, which circulates and mixes the airand the steam (Chapter 12, Fig. 9). Some steam–airsterilizers are capable of using water during the cool-down process to cool the containers more rapidly. Thisrapid cooling may also be necessary for product stability.Various methods (i.e., direct injection, recirculationthrough a heat exchanger, etc.) for introducing thecooling media can be utilized.
Recirculating Superheated Water CycleThe typical recirculating superheated water process(sometimes referred to as a water cascade or rainingprocess) begins by the addition of water to the sterilizerto a predefined level (below the product zone). Then awater recirculation pump is started to continuouslyrecirculate water from the bottom of the sterilizer tospray nozzles or a water distribution pan above theproduct zone. The recirculation pump is on throughoutthe heat-up exposure and cool-down phases. Duringheat-up, the water is heated at a pre-defined rate via aheat exchanger in the recirculation loop or with the directinjection of steam. Also during heat-up, compressed air isadded to the chamber to attain the desired overpressurelevels. Once the temperature set point is achieved, thecontroller steps into the hold portion of the cycle and thetemperature and pressures are maintained at the desiredlevels. For cooling, the steam supply is shut off and therecirculating water is cooled at a controlled rate byintroducing cooling media to a heat exchanger installedin the water recirculation loop or by the direct injection ofcooling water into the recirculating loop. This type ofprocess does not require the use of a jacket but doesrequire specific water level controls.
13: VALIDATION OF TERMINAL STERILIZATION 191

The recirculating superheated water process is veryefficient and the temperatures and pressures can betightly controlled during the entire process, thus mini-mizing container stresses.
STERILIZATION CYCLE DEVELOPMENT
This section will address sterilization and associatedmicrobiological activities that occur in R&D areas aswell as the production environment when using theBI/bioburden approach in support of a parenteralproduct. The list below depicts some of the sterilizationengineering and microbiological activities associatedwith a parenteral product as it moves through develop-ment. These studies or similar ones are ordinarilyconducted in developmental sterilizers or may occur asinvestigative engineering studies in a production steri-lizer as appropriate. The overkill method can be used forsome of the more stable parenteral formulations, and itsvalidation is accomplished as described in Chapter 12.
Sterilization development activity Activity statement
Cycle development Develop preliminary
container sterilization
specifications with
engineering parameters
such as temperature,
time and F0Container thermal mapping Determine cold spot and
assess heat penetration
within finished container
Formulation development Perform analytical
feasibility studies prior to
product finalization with
method’s validations
Parenteral solution microbiological
evaluations:
Moist heat D- and z-value analysis Perform triplicate D-value
analysis on each
parenteral formulation at
three temperatures,
e.g., 1128C, 1188C and
1218C and then
calculate the z-value
APE Perform on final product if
it contains a
preservative or if there is
a multidose claim for the
container
In-process bioburden analysis Perform studies with a
panel of microorganisms
to validate 70% recovery
for the filtration process
Spike hold time studies Inoculate parenteral
product with bioburden
and growth promotion
compendia organisms to
evaluate the product’s
ability to support
microbial growth
Container closure evaluations:
Microbial closure inactivation Perform kill curve kinetics
using bioburden and BI
(spores) inoculated onto
the worse case closure
site
Container integrity Perform dye ingress,
microbial challenge or
physical integrity tests
following exposure to
maximum sterilization
conditions that stress
the container
Stability runs Perform analytical
chemistry and
microbiological
evaluations at various
temperatures and times
per ICH and or
compendia
requirements
BET Perform test method
validation of API,
excipients and final
product per compendia
requirements
Sterilization engineering personnel primarily focustheir efforts in determining whether a parenteral formu-lation packaged in a particular container configuration canbe sterilized in a current cycle or whether a new cyclemustbe developed. The referenced EMEA (2) decision tree isfollowed when evaluating a new parenteral product in anLVP or SVP container. Sterilization feasibility studies areconducted in a sterilizer to ascertain the physical effects ofthe cycle on the product in question. Product attributesthat can be affected by a cycle are closure integrity, productpotency, pH, color, shelf-life stability, visible, and subvi-sible particulates as well as final product sterility. Once thebasic engineering parameters (e.g., temperature, time andF0) are established, then engineering thermal containermapping studies can be performed (3,4).
Container Thermal Mapping Validation StudiesAn R&D sterilizer is smaller than a production facilitysterilizer, but can simulate the sterilization cyclesconducted in the larger production vessels. Containerthermal mapping studies (when applicable) are typicallyperformed in a laboratory sterilizer:1. To locate the coldest zone or area inside a container.2. To determine the cold zone in the container and its
relationship to the location monitored duringvalidation studies.
3. To generate data thatmaybeusedduring the setting ofproduction sterilization control parameters.When conducting thermal mapping studies, there
are various factors to be considered, and these aredependent upon the:1. Type of container (flexible or rigid)2. Container orientation, size and fill volume3. Cycle type and temperature4. Viscosity5. Autoclave trays/design/surface contact6. Autoclave spray patterns/water flow.
Typical container mapping data obtained for lipidemulsions contained within a 1000 mL glass container areshown as an example in Tables 1 and 2. The followingsummarizes the process for obtaining heat map data fromthe glass intravenous container filled with approximately1000 mL of lipid emulsion.
192 III: STERILIZATION, SANITIZATION AND STERILITY ASSURANCE

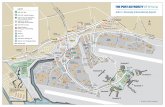
TC probes (Copper Constantan, type T,0.005 in. diameter) were used to monitor 11 locationswithin the 1000 mL container. The TC probes were posi-tioned at various distances (in inches) as depicted (Fig. 4).Each container was filled with approximately 1000 mLof the lipid emulsion, evacuated to 20 in. of mercury andsealed with an aluminum overseal.
A flat perforated rack on a reciprocating shaker cartwas used in the autoclave. The cycle’s target temperaturewas 1238C, recirculating water spray cycle with 70 rpm ofaxial agitation and 30 psig (pounds per square inch) of airoverpressure.
When the sterilization cycle was controlled to give aheat input of approximately 7.5 F0 minutes in the coldestemulsion area, the average coldest emulsion area wasfound to be measured by TC number (TC#) 3,14. Theaverage hottest emulsion area was measured by TC# 10,21. The difference between the hottest and coldest emul-sion areas ranged from 7.5 to 10.0 F0 minutes with anaverage of 8.6 F0 minutes. Therefore, when the coldest
emulsion area registered 7.5 F0 minutes, the hottestemulsion area would average 16.1 F0 minutes.
The emulsion area approximating the validation TClocation was measured by TC # 2,13 and averaged 7.7 F0minutes when the coldest emulsion was approximately7.5 F0 minutes (Fig. 5).
Solution/Product Moist Heat Resistance D- andz-Value AnalysisA BIER vessel meets specific performance requirementsfor the assessment of BIs per American National Stan-dards developed and published by AAMI (5). Oneimportant requirement for a BIER steam vessel is thecapability of monitoring a square wave heating profile.
Refer to Figure 6 for a schematic of the steam BIERvessel used to generate the D- and z-value data. D-valueis the time in minutes required for a one log or 90%reduction in microbial population (Refer to Chapter 12,Fig. 1). The z-value is the number of degrees of
Table 1 Heat Input (F0 Units)
1000 mL glass I.V. containers-heat mapping study (lipid emulsion)
Run CLHK00.049 Run CLHK01.050
TC number btl 1 btl 2 btl 1 btl 2 Average (SD)
1,12 7.91 C7.28 8.13 C7.36 7.67 (0.415)
2,13 (PC) 7.79 7.49 8.02 7.64 7.74 (0.226)
3,14 C7.46 7.40 C7.71 7.47 C7.51 (0.137)
4,15 7.64 7.80 7.87 7.96 7.82 (0.135)
5,16 12.66 12.90 12.95 12.91 12.86 (0.132)
6,17 12.73 12.46 12.77 12.68 12.66 (0.138)
7,18 12.78 12.69 12.95 12.91 12.83 (0.120)
8,19 13.32 13.33 13.42 13.78 13.46 (0.223)
9,20 14.21 14.33 14.03 14.56 14.28 (0.222)
10,21 H15.87 H17.24 H15.18 H16.09 H16.10 (0.856)
11,22 15.47 16.56 14.77 16.07 15.72 (0.773)
H–C 8.41 9.96 7.47 8.73 8.64 (1.028)
PC–C 0.33 0.21 0.31 0.28 0.28 (0.053)
Note: H denotes hottest TC location; C denotes coldest TC location; PC denotes approximate location of the production profile TC; Data from TC#9 used with apostcalibration variance ofC0.258C at 1008C; All heat input values are calibration corrected.
Table 2 Solution Heat Rates (Minutes)
1000 mL glass I.V. containers-heat mapping study (lipid emulsion)
Run CLHK00.49 Run CLHK01.050
btl 1 btl 2 btl 1 btl 2 Average (SD)
Coldest location
Thermocouple number 3 12 3 12 –
Time to 1008C 19.0 19.0 19.0 19.0 19.00 (0.000)
TimeR1008C 21.0 21.0 21.0 21.0 21.00 (0.577)
TimeR1208C 4.0 3.0 4.0 3.0 3.50 (0.577)
TimeR120K1008C 4.0 5.0 4.0 5.0 4.50 (0.577)
Maximum temperature (8C) 120.82 120.77 120.92 120.77 120.82 (0.071)
Heat input (F0) 7.46 7.28 7.71 7.36 7.45 (0.187)
Production profile TC location
Thermocouple number 2 13 2 13 –
Time to 1008C 19.0 19.0 19.0 19.0 19.00 (0.000)
TimeR1008C 22.0 21.0 22.0 21.0 21.50 (0.577)
TimeR1208C 4.0 3.0 4.0 3.0 3.50 (0.577)
TimeR120K1008C 5.0 5.0 5.0 5.0 5.00 (0.000)
Maximum temperature (8C) 120.91 120.82 120.91 120.92 120.89 (0.047)
Heat input (F0) 7.79 7.49 8.02 7.64 7.74 (0.226)
Note: H denotes hottest TC location; C denotes coldest TC location; PC denotes approximate location of the production profile TC; Data from TC#9 used with apostcalibration variance ofC0.258C at 1008C; All heat input values are calibration corrected.
13: VALIDATION OF TERMINAL STERILIZATION 193

temperature required for a 10-fold change in the D-value.(Refer to Chapter 11 for additional details on F-, D- andz-values.)
Master Solution/Product ConceptThe family categoryof lipid emulsions and their respectiveD1218C and z values as well as classification in terms ofmicrobial resistance is shown in Table 3. A categorizationof parenteral formulations with associated D1218C andz-values and their potential impact onmicrobial resistanceusing the BI, Clostridium sporogenes were previouslyreported (6). In addition, the methodologies used for D-and z-value analysis were likewise cited. The data inTable 3 indicate that the # 1 emulsion is at the top of thelist, since it affords the most microbial moist heat resist-ance. It is therefore the emulsion that should bemicrobiologically challenged (inoculated with spores) aspart of the emulsion validation scheme. D- and z-valuedata have been reported for other BIs such as Geobacillusstearothermophilus (6–8) and Bacillus subtilis 5230 (9). Thereare many factors that can affect moist heat resistanceincluding a BI’s age, sporulation media used, as well asthe particular spore strain employed (10).
PSLR ValuesLipid emulsion moist heat resistance values (D1218C andz-values) were generated in the steam BIER vessel usingthe BI C. sporogenes as shown in Table 3. The columns inthe Table list the representative code or list number of theproduct, the emulsion or product name, its averageD1218Cvalue and z-value and finally the PSLR value. Thoseparenteral formulations with the lowest PSLR value(s)are those that should be used for the microbial validationat subprocess conditions, since these provide the mostmicrobial resistance (6).
Accumulated Fbio for Lipid EmulsionsAccumulated Fbio and z-values (Table 4) were used toconstruct the PSLR ranking for lipid emulsions as pre-viously discussed for Table 3. The Fbio is the heat input forthe biological solution based on the emulsion’s moist heatD- and z-values. By inputting the sterilizer temperaturesfrom the coldest TC of an engineering run for a particularcontainer/sterilization cycle, the emulsion can be rankedaccording to PSLR values. The combined D1218C andz-value allows comparison of moist heat rankingsbetween emulsions.
The data in Table 4 demonstrate that the #1 Emul-sion has the lowest PSLR (7.105), thereby affording thehighest moist heat resistance upon inoculation. Gener-ation of this table allows prediction of which emulsion tomicrobiologically challenge as part of validation in theproduction sterilizer.
Microbial Closure Inactivation Validation in aDevelopmental SterilizerIn lieu of using the large type steam sterilizers in theproduction environment, microbial inactivation at theclosure/bottle interface of an emulsion container can beassessed in a developmental sterilizer. The closure micro-bial inactivation (kinetic) studies can determine how thesize of the container, type of closure compound used aswell as closure preparatory processes (e.g., leaching,washing, siliconizing, autoclaving) influence microbialinactivation. Microbial closure kinetic studies areconducted at various time intervals in a given steriliza-tion cycle. DP count or F/N methodologies are used to
1–1/12 1–1/2 1–1/2 1–1/2
Fill Level
3/4
1–1/12
9,208,19
4,15
7,18
3,142,131,12
5,16 6,17
10,21 11,22
1000 mL Glass I.V. Container
- Heat Mapping Study
Thermocouple Locations
Figure 4 Heat mapping study using a 1000 mL glass container.
12.9
7.7 7.7 7.5 7.8
12.7 12.8 13.5 14.3
Fill Level
15.716.1
1000 mL Glass I.V. Container- Heat Mapping Study
Average Heat Input (F0) at Various Locations
Figure 5 Heat mapping study with averageheat input (F0) at various locations in a1000 mL glass container.
194 III: STERILIZATION, SANITIZATION AND STERILITY ASSURANCE

TopChamberVent
SampleChamber
Drain/LowerChamberVent
SteamControlValve
PressureRecordingController
Steam Reservoir
MainSteamSupply
InstrumentWell Vent
Thermocouplesto Digital Displayand Datalogger
Schematic of the Steam B.I.E.R Vessel
Figure 6 Schematic of a steam biologicalindicator evaluator resistometer vessel usedfor generating moist heat resistance D- and z-values for inoculated parenteral solutions or forbiological indicators.
Table 3 IV Lipid Emulsions Ranking
List # Solution D121 z-valuePredicted spore log
reduction
1 20% Emulsion 0.7 10.6 7.1
2 10% Emulsion w/increased linolenate 0.7 11.4 7.5
3 10% Emulsion w/100% soybean oil 0.6 10.1 8.0
4 20% Emulsion w/100% soybean oil 0.7 12.8 8.2
5 20% Emulsion w/increased linolenate 0.6 10.6 8.3
6 10% Emulsion w/50% safflower & 50% soybean oil 0.6 10.7 8.4
7 20% Emulsion w/50% safflower & 50% soybean oil 0.6 12.7 9.5
8 10% Emulsion 0.4 11.1 12.9
Table 4 Accumulated Fbio by List Number and z Value
Solution
F (PHY)zZ10.0
1zZ10.6
2zZ11.4
3zZ10.1
4zZ12.8
5zZ10.6
6zZ10.7
7zZ12.7
8zZ11.1
Temperature(8C)
Time(min)
105.4 1 0.0269 0.0330 0.0419 0.0278 0.0592 0.0330 0.0340 0.0579 0.0384
110.1 1 0.0793 0.0915 0.1082 0.0813 0.1380 0.0915 0.0935 0.1359 0.1019
114.1 1 0.1991 0.2181 0.2427 0.2023 0.2834 0.2181 0.2212 0.2806 0.2336
116.2 1 0.3228 0.3442 0.3709 0.3265 0.4134 0.3442 0.3476 0.4106 0.3611
118.1 1 0.5000 0.5200 0.5445 0.5035 0.5819 0.5200 0.5232 0.5794 0.5356
119.1 1 0.6295 0.6462 0.6663 0.6324 0.6966 0.6462 0.6489 0.6946 0.6591
119.4 1 0.6745 0.6897 0.7079 0.6772 0.7352 0.6897 0.6921 0.7334 0.7014
119.2 1 0.6442 0.6604 0.6799 0.6470 0.7092 0.6604 0.6630 0.7073 0.6729
118.5 1 0.5483 0.5672 0.5903 0.5515 0.6253 0.5672 0.5703 0.6230 0.5819
117.8 1 0.4667 0.4872 0.5124 0.4702 0.5513 0.4872 0.4905 0.5487 0.5033
116.2 1 0.3228 0.3442 0.3709 0.3265 0.4134 0.3442 0.3476 0.4106 0.3611
114.1 1 0.1991 0.2181 0.2427 0.2023 0.2834 0.2181 0.2212 0.2806 0.2336
110.6 1 0.0889 0.1020 0.1197 0.0911 0.1510 0.1020 0.1042 0.1487 0.1130
105.9 1 0.0301 0.0367 0.0463 0.0312 0.0648 0.0367 0.0379 0.0634 0.0426
101.7 1 0.0115 0.0148 0.0198 0.0120 0.0305 0.0148 0.0153 0.0296 0.0178
Total F 4.7436 4.9734 5.2646 4.7826 5.7366 4.9734 5.0107 5.7044 5.1573
D value 0.70 0.70 0.60 0.70 0.60 0.60 0.60 0.40
PSLR 7.105 7.521 7.971 8.195 8.289 8.351 9.507 12.893
13: VALIDATION OF TERMINAL STERILIZATION 195

evaluate the surviving organisms. Test data has beengenerated demonstrating the value of using both amoist heat organism (C. sporogenes) and a dry heatorganism (B. subtilis now known as Bacillus atrophaeus)as BIs for the sterilization validation of closure systems(11,12). A typical graphic representation of the inacti-vation kinetics is illustrated in Figure 7. The abovestudies may also be performed in a production sterilizeras engineering or feasibility studies.
Container Closure Integrity ValidationContainer–closure integrity or MOS validations are runon all moist heat terminally sterilized products with
closure systems of a parenteral container. This validationis performed to demonstrate that the closure system of acontainer is capable of maintaining the emulsion andfluid path in a sterile condition throughout the shelf lifeof the product.
In a typical MOS study, the product container issterilized at a temperature which is higher than theupper temperature limit of the chosen sterilizationcycle and for a time that is greater than the maximumtime limit for the cycle or producing an F0 subzero levelgreater than the maximum F0 level for the cycle. Therationale for the selection of the maximum temperatureand heat input level for the prechallenge sterilization is
1.0E+06
1.0E+05
1.0E+04
1.0E+03
1.0E+02
1.0E+01
1.0E+00
1.0E−01
1.0E−02
1.0E−030.0 5.0 10.0 15.0 20.0 25.0 30.0 35.0 40.0 45.0
0.99
0.95
0.90
0.80
0.700.600.500.400.300.200.100.050.01
Fraction ofNegativeUnits
Sur
vivo
rs
Study 1
Study 2
Linear Regression
C. sporogenes
Fraction/Negative Zone
B. subtilis
Enhanced Bioburden
Time Above 100 CAverage Count of 0 for Direct Plate Testing is Given a Value of 1.00E−01
Average Count of 0 for Fraction/Negative Testing is Given a Value of 1.00E−02
Figure 7 Microbial kinetic inacti-vation of bioburden as comparedto biological indicators, Bacillusatrophaeus (formerly namedBacillus subtilis) and Clostridiumsporogenes.
196 III: STERILIZATION, SANITIZATION AND STERILITY ASSURANCE

that rubber and plastic closures are subjected to thermalstresses during sterilization and those stresses are maxi-mized at the highest temperature and the longest timeallowed.
In some cases, the closures, e.g., administration oradditive port are claimed to be sterile by a radiationprocess. In such cases, the closures are sterilized in bulkexceeding the maximum end of the radiation processe.g., 40 kGy, then fabricated to the flexible containerand exposed to steam sterilization cycle conditionsexceeding the maximum temperature end of the cycle.Thus, the closures are stressed by a joint process ofradiation as well as steam prior to performing theclosure integrity test.
Product Validation for EndotoxinEndotoxins are lipopolysaccharides from the outer cellmembrane of gram-negative bacteria. Endotoxins can bedetected by the manual gel-clot method known as theLAL test. There are also various quantitative methods(turbidimetric and chromogenic) which use more rapidautomated methodologies. All final product formulationshave regulatory requirements to be tested for endotoxinsand the method must be validated using three differentlots of final product. LAL testing should be performed onfinal product formulations per FDA Guidelines and otherregulatory compendia. Emulsion formulations, if coloredor opaque cannot be tested by the turbidimetric methodand therefore may use a comparable test e.g., LAL,chromogenic or kinetic.
The LAL test is for products other than oral and topicalproducts (e.g., parenteral solutions, some devices, etc). Endo-toxin testing is usually required at three different times inthe cycle of the product. First, endotoxin testing should beperformed on the lot of drug being used in clinical studies toensure that the product is safe for the patients with respect toendotoxin. Second, in the developmental stages, endotoxintesting is usually required at the beginning and end of thestability studies. Finally, once the product is ready to bemarketed, each lot of the product requires endotoxin testingprior to release.
To improve in-process control, a process shouldalso be in place to decide if endotoxin testing should beperformed on the APIs and/or excipients used in theproduct. In order to determine this, the ICH guidelinesfor quality should be used; i.e., Q7A “Good Manufac-turing Practice Guidance for APIs.”
PRODUCTION FACILITY STERILIZATIONDEVELOPMENT
The production list below depicts some of the sterilizationengineering and microbiological activities associatedwith a parenteral product as it moves into the productionenvironment. These studies occur in a productionenvironment as appropriate.
Production facility activity Activity statement
Heat P&Ds Perform triplicate studies for
minimum and maximum
loading conditions using
temperature probes within
the product containers and
outside the containers to
measure the sterilizer
heating medium
temperature
Solution (master)
microchallenge validation
Perform microbial validation
of a parenteral solution or
master solution at sub-
process conditions in the
production sterilizer
Container–closure microchallenge
validation as applicable
Perform microbial validation
of the container–closure
system at sub-process
conditions in the
production sterilizer
Hold time studies Microbial, chemical and
endotoxin studies are
performed to establish the
longest time that a product
can be held following
manufacture but prior to
filling and sterilization
Engineering P&D ValidationPerform triplicate studies with minimum and maximumloading configurations with temperature probes pene-trating the product containers as well as temperatureprobes distributed outside the product containers in aproduction sterilizer at nominal operating processparameters.
Microbial Solution Validation in a ProductionSterilizerTable 5 shows the microbial solution validation con-ducted at subprocess conditions in a fully loaded
Table 5 Lipid Emulsion Microbial Solution Validation
Fraction negative method
Organism CodeAverage no.spores/bottle
No. positivea/no. positivecontrols
No. positivea/no. negativecontrols
No. positivea/no. test samples
Sporeb
logarithmicreduction
C. sporogenes 5C6 4.8!105 2/2 0/4 0/20 O7.0C. sporogenes 15C6 6.4!105 2/2 0/4 0/20 O7.1G. stearothermophilus 5B2 7.6!101 2/2 0/4 0/20 O3.2G. stearothermophilus 15B2 7.7!101 2/2 0/4 0/20 O3.1
F0 Rangec: 5.8–7.6; Temperature Range: 120–1258C; Agitation: 67–73cpm
a Positive for the indicator microorganism.b Spore logarithmic reductionZlog aKlog b; where a, initial population of spores; b, 2.303 log (N/q)Zln (N/q); where N, total number of units tested; q, number ofsterile units.
c F, integrated lethality or equivalent minutes at 121.18C for hottest and coldest thermocoupled containers.
13: VALIDATION OF TERMINAL STERILIZATION 197

production sterilizer. The acceptance criteria of 6 SLR wassetup for the BI C. sporogenes and a 3 SLR for the highermoist heat-resistant BI, G. stearothermophilus. Each emul-sion (20 containers) is inoculated with the appropriate BIat a target level of 1.0!106 and 1.0!102 for C. sporogenesand G. stearothermophilus, respectively. The 20 inoculatedcontainers are distributed throughout the productionsterilizer for sterilization at subprocess conditions. Thetest containers are then returned to the lab for testing bythe F/N test method.
Microbial Closure Validation in a ProductionSterilizerTable 6 shows the microbial closure validation at sub-process conditions in a fully loaded production sterilizer.The BIs usedwereC. sporogenes and B. subtilis. Acceptancecriteria of three SLR must be achieved for moist heat(C. sporogenes) and dry heat (B. subtilis indicators). Thesurface of the stopper that comes into direct contact withthe sidewall of the bottle was inoculated with the appro-priate BI, dried and then a few drops of emulsion wereplaced over the inoculum to simulate manufacturingconditions. The inoculated closure was assembled to thefinished container, exposed to subprocess steam
conditions in the production sterilizer and subsequentlytested in the lab by the F/N test method. The datademonstrate that aO3 SLR was achieved at subminimalprocess conditions. Replicate test samples (e.g., 3 to 5)should be considered for use to verifymicrobial kill in coldzone locations.
ANCILLARY SUPPORT PROCESS TESTING
Bioburden Analysis for Closures and CommoditiesDetermine microbial load on closures and commoditiesas well as their moist heat resistance analysis.
As part of the microbiological quality controlprogram, products and commodities are routinelysampled during the production process in order toassess the microbial load. This assessment is performedvia the bioburden test for terminally sterilized product.The bioburden test method is developed during theproduct development stage prior to transfer to the pro-duction plant. This test assesses the microbial load of asolution prior to terminal sterilization (In-ProcessBioburden Test). Micro R&D is responsible for the vali-dation of the bioburden method prior to transfer to theproduction plant. The validation will demonstrate that
Table 6 Lipid Emulsion Microbial Closure validation
MicroorganismInitial
population/stopperNo. positivea/
no. positive controlsNo. positivea/
no. negative controlsNo. positivea/test samples
Sporeb
logarithmicreduction
C. sporogenes 8.4!103 2/2 0/4 0/20 O5.2B. subtillis 3.0!104 2/2 0/4 0/20 O5.8
F0 Rangec: 5.8–7.6; Temperature Range: 120–1258C; Agitation: 67–73 cpm
Sterilization validation of 200 mL bottle inoculated closure surface coated with I.V. fat emulsion in cycle with agitation.a Positive for the indicator microorganism.b Spore logarithmic reductionZlog aKlog b; where a, initial population of spores; b, 2.303 log (N/q)ZIn (N/q); whereN, total number of units tested; q, number of sterileunits.
c F, integrated lethality of equivalent minutes at 121.18C for hottest and coldest thermocoupled containers.
Heat Shock Positives
Gram Stain/Plate Morphology
Yeasts, MoldsGram Negative Rods
Cocci
Retesting with 30-minHeat Shock not
Routinely Required
Gram Positive Rods
Second Heat Shock
10 min (+)30 min (–)
10 min (+)30 min (+)
CalculateProbabilityof Non-Sterility
Moist HeatResistance Analysis
Required
Production Environment BioburdenScreening Program
Figure 8 Representative pro-duction environment bioburdenscreening program.
198 III: STERILIZATION, SANITIZATION AND STERILITY ASSURANCE

recovery of microbial load at a relatively low level canbe achieved.
The Microbial Limits Test is essentially a bioburdentest of raw materials used to make the final product.The test method and validation are conducted in muchthe same manner as the bioburden test. The limit for themicrobial limits test is calculated as follows: final ProductAction Level/maximum concentration of API in the finalproduct. This limit is then “normalized: by dividing bythe total amount of APIs in the final product.”
In addition, the production bulk solution is moni-tored for total bioburden load including spore formers.The screening allows the plant quality lab to ascertain ifthere are any moist heat-resistant microflora present inthe bulk solution prior to the terminal sterilization of theparenteral solution in its finished container (Fig. 8).
Antimicrobial Preservative EfficacyPerform on those formulations containing a preservativeand those container configurations that have a multidoseclaim. This validation is performed per compendialrequirements.
Sterility Testing (if Required)Once parametric release is approved by regulatoryauthorities, then sterility testing is no longer requirednor can it be used as an alternative in case parametricrelease parameters are not used.
Biological Testing Support of R&D and MarketedProduct Stability ProgramsThere are a number of analytical andmicrobiological testsperformed over the shelf life of a product. A number ofmicrobiological tests include BET, Container–ClosureIntegrity and APE if applicable.
CONCLUSION
As one reviews the final configuration that a terminallysterilized parenteral product is packaged in, it is notsurprising that a similar evaluation occurred when onewas contemplating how to present the new product asbeing sterile and non-pyrogenic. The product develop-ment team focused on the various designs of sterilizersand the various manufacturing site locations for thesupport of currently marketed products. Once the teamdecided the appropriate facility for manufacture, then thevarious sterilization cycles discussed in this chapter wereevaluated in order to select the appropriate one bestsuited for that parenteral product in its final containerconfiguration. If a product is destined for the inter-national market, then R&D personnel will follow the
EMEA decision tree to determine if the product can besterilized at 1218C for 15 minutes minimum. If it cannot,then a justification is documented explaining the reasonfor selection of an alternate sterilization cycle. Personnelperform the applicable studies in a developmental steri-lizer as detailed in this chapter, as well as feasibilitystudies in development or production sterilizers tomonitor and test the physical attributes of the finaldesigned container. Once the parenteral product’sdesigns as well as sterilization processes have beenfinalized, then the plant/site can perform their standardpenetration, distribution and microbiological studies inthe production sterilizer.
REFERENCES
1. ISPE, GAMP 4 Guide for Validation of Automated Systems.December 2001.
2. Committee for Proprietary Medicinal Products (CPMP)Decision Trees for the Selection of Sterilisation Methods(CPMP/QWP/054/98), Annex to Note for Guidance onDevelopment Pharmaceutics, EMEA 2000, 1–3.
3. Young JH. Sterilization with steam under pressure. In:Morrissey RF, Phillips GB, eds. Sterilization Technology.New York: Van Nostrand Reinhold, 1993:120–51.
4. Owens JE. Sterilization of LVP’s and SVP’s. In:Morrissey RF, Phillips GB, eds. Sterilization Technology.New York: Van Nostrand Reinhold, 1993:254–85.
5. AAMI. BIER/Steam Vessels (ST45). Arlington, VA:American National Standard for the Advancement ofMedical Instrumentation, 1992.
6. Berger TJ, Nelson PA. The effect of formulation of parenteralsolutions on microbial growth-measurement of D- andz-values. PDA J Pharm Sci Technol 1995; 49(1):32–41.
7. Feldsine PT, Schechtman AJ, Korczynski MS. Survivorkinetics of bacterial spores in various steam heated parent-eral solutions. Dev Ind Microbial 1977; 18:401–7.
8. Moldenhauer J. How does moist heat inactivate micro-organisms?. In: Moldenhauer J, ed. Steam Sterilization, APractitioner’s Guide. Bethesda, MD/Godalming, UK: PDA,2003:1–15.
9. Caputo RA, Odlaug TE, Wilkinson RL, et al. Biologicalvalidation of a sterilization process for a parenteralproduct-fractional exposure method. J Parent Drug Assoc1979; 33:214–21.
10. Pflug IJ, Holcomb RG. Principles of thermal destruction ofmicroorganisms. In: Block SS, ed. Disinfection, Sterilizationand Preservation. 3rd ed. Philadelphia, PA: Lea andFebiger, 1983:759–66.
11. Berger TJ, May TB, Nelson PA, et al. The effect of closureprocessing on the microbial inactivation of biologicalindicators at the closure–container interface. PDA J PharmSci Technol 1998; 52(2):70–4.
12. Berger TJ, Chavez C, Tew RD, et al. Biological comparativeanalysis in various product formulations and closure sites.PDA J Pharm Sci Technol 2000; 54(2):101–9.
13: VALIDATION OF TERMINAL STERILIZATION 199