Usability, feasibility, and safety test of a new ...
Transcript of Usability, feasibility, and safety test of a new ...

Original Article
Usability, feasibility, and safety test of a new thermosensitive liquid crystal film
for the early detection of extravasation in clinical practice: A pilot study
Mari Abe-Doi1)
; Ryoko Murayama1) 2)
; Hidenori Tanabe3)
; Emiko Kamiyama4)
;
Chieko Komiyama4)
; Yuko Matsui5)
and Hiromi Sanada2) 6)
1)Department of Advanced Nursing Technology, Graduate School of Medicine, the University of Tokyo
2)Global Nursing Research Center, Graduate School of Medicine, the University of Tokyo
3)Research and Development Center, Terumo Corporation
4)Department of Nursing, The University of Tokyo Hospital
5)Department of Nursing, Faculty of Health Sciences, Komatsu University
6)Department of Gerontological Nursing/Wound Care Management, Graduate School of Medicine, the University of Tokyo
Abstract
Early detection of extravasation is important due to possible drug leakage, which can cause severe tissue damage.
However, its signs and symptoms are difficult to be assessed, and objective assessment is necessary. Given that fluid
accumulation provides a low skin-surface temperature, a thermosensitive liquid crystal film was developed to be used as
a noninvasive, continuous, and safe extravasation assessment tool. This study aimed to confirm its usability, safety, and
feasibility for visualizing skin temperature in the clinical setting. This study included clinical nurses and outpatients who
received chemotherapy. No extravasation occurred. Forty patients and 8 nurses were included. All patients responded
that they did not mind using the film, and they did not experience any side effects due to using the film, such as itching,
tightened feeling, or other discomfort. Nurses placed the film on a catheter securement film and routinely administered
drugs. Nurses evaluated the usability of the film after every use. The frequency of observation remained unchanged,
according to 80% of the nurses:answers. It suggested that additional treatment time due to film use was acceptable.
During treatment, the skin-surface temperature distribution pattern was recorded using a camera. The temperature
distribution patterns were classified into six. The thermosensitive liquid crystal film can be a potential assessment tool to
early detect extravasation.
Key words: chemotherapy, extravasation, peripheral intravenous catheter, skin temperature
Introduction
Vesicant antineoplastic drugs can cause sub-
cutaneous tissue injury when they extravasate from
the vein1). Extravasation incidence is low
2), but some
anticancer drugs, even with few leakages, induce
ulceration or necrosis, which requires surgical treat-
ment and possibly results in a limited range of motion
in the joints at worst3)4)
. Thus, extravasation should be
early detected.
Conventionally, extravasation is detected by asses-
sing patients:symptoms (e. g., tingling, burning,
discomfort/pain, or swelling or redness at the
injection site) or problems in treatment (e.g., absence
of blood return, resistance on the plunger of the
syringe when administering a bolus drug, or interrup-
tion to the free flow of an infusion)5). This conventional
approach has some challenges. Nearly half of an
extravasation injury can be detected by patient:s
complaint of pain or discomfort6). However, subjective
― 89 ―
JNSE, 7 : 89〜98, 2020
Corresponding author: Hiromi Sanada Manuscript received: 30 September 2019
Department of Gerontological Nursing/Wound Care Management, Division of Health Sciences and Nursing, Graduate School of
Medicine, The University of Tokyo
7-3-1 Hongo, Bunkyo-ku, Tokyo 113-0033, Japan
E-mail: [email protected]

symptoms depend on the sensation of each patient,
and young children or people with impaired cognition
have communication difficulties of pain; thus, they are
considered risk factors7)8)
. Additionally, some treat-
ment strategies, such as using analgesics or anesthe-
sia, may negatively affect early detection due to
obtundation.
The change in skin-surface temperature has been
paid attention to because it does not influence
patients:subjective signs. Infiltration or extravasation
can be visualized macroscopically by thermography9)10)
.
One of our previous studies found a relationship
between a unique low-temperature distribution
pattern, that is,K fan at the puncture site, Lduring
anticancer drug administration and the onset of
induration at the next treatment day11)
. In the previous
study, temperature distribution images were shot
continuously by infrared thermography. An infrared
thermography is a noninvasive but expensive method
that requires enough space for taking images or skills
for focusing on the target area. If patients move their
catheterization sites, we have to rearrange the
position of the infrared thermographic camera. Hence,
taking images of multiple patients simultaneously is
difficult.
Thus, our research group had developed a thermo-
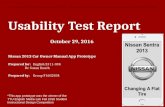
sensitive liquid crystal film (Figure 1) that can
visualize skin-surface temperature with a medical
device company. The film is placed directly on the
skin surface covered with a securement film. This
film-type thermography requires low cost, no space,
no skills for taking temperature distribution images,
and unconstrained patients:movement.
This pilot study aimed to confirm its usability for
clinical nurses, feasibility as a thermosensor, and
safety for the patients in the clinical setting, given that
some points are different from the ones in the
previous study. In the previous study, a noncontact
method was used, and skin-temperature data were
obtained. Additionally, nurses did not participate in
any skin-temperature data collection. We need to
confirm whether using the film can be added in the
nurses:daily routine, considering that chemotherapy
requires extremely tight schedule and complicated
therapy.
Method
The study design was cross-sectional.
1. Study setting and participants
This study was conducted in a chemotherapy room
with outpatients in a university hospital in Japan.
Patients participated only once in this study.
The inclusion criteria for patients were as follows:
aged over 19 years, undergoing chemotherapy
treatment using a peripheral intravenous catheter for
cancer, and received permission to participate in this
study from their physicians and clinical nurses.
Meanwhile, the exclusion criterion was the use of an
infusion warming device.
Clinical nurse participants were those who worked
in the chemotherapy room within the study period
and provided an informed consent. They were trained
by the researchers on how to use the film (i.e., how to
place it on the skin surface properly and how to peel it
safely). Data obtained between January 2018 and
March 2018 were collected.
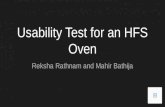
2. Thermosensitive liquid crystal film
This film was developed by our laboratory and
Terumo Corporation (Tokyo, Japan). The size was 55×
90 mm. The temperature range was 30. 0℃-34. 0℃.
The color of the film changes with the skin-surface
temperature (Figure 2). This film can be repetitively
used, but it was used once in this study to rule out
infection. As necessary, nurses can observe the site
under the thermosensitive liquid crystal film after
peeling it during administration, and they can place it
back again. The adhesive strength condition of the
thermosensitive liquid crystal film can be verified as
follows: the skin-surface temperature could be
captured enough, and when it was peeled off carefully,
the securement dressing attached below remained
Journal of Nursing Science and Engineering(2020)
― 90 ―
Figure 1 Thermosensitive liquid crystal film during
infusion therapy
Low-temperature area is shown along the blood vessel.

intact. The experiment was repeated when the
abovementioned conditions were achieved; then, the
adhesive strength was decided. Its international
patent application number is WO2015/045371.
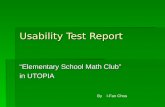
3. Analytical method for the qualitative analysis of
the low-temperature distribution patterns using the
thermosensitive liquid crystal film
One researcher who had an experience in thermo-
graphic analysis classified the low-temperature
distribution patterns. The researcher was blinded
about the details of the administered drugs as well as
the characteristics of participants and their symp-
toms. The researcher checked all pictures of the films
that changed colors with skin temperature and then
classified the pictures by using a previous study as a
reference8). In the previous study, low-temperature
distribution patterns obtained by infrared thermogra-
phy were classified into the following six patterns:
K no low-temperature area L(this pattern did not
feature a low-temperature area during the infusion),
K sharp line along the vein L(the shape of the
low-temperature area was similar to the sharp line
along the vein),Kbroad area from the veinL(a low-
temperature line was initially displayed that widened
from the vein during the infusion),Klarge area of the
external sideL(the entire external side of the arm was
cooled in patients catheterized at the wrist),Kcircle to
the line along the veinL(a circular low-temperature
area appeared at the catheter tip position; the circle
did not enlarge, and a low-temperature line some-
times appeared along the vein during infusion), and
Kfan at the puncture siteL(a fan-shaped low-temper-
ature area was observed at the puncture site). The
Kfan at puncture siteLpattern specifically predicted
the occurrence of induration compared with the other
patterns.
4. Procedure, survey items, and data source
1) Usability
In this study, usability was operationally defined as
the nurses:evaluation of the film in terms of placing
and peeling the film from the patients: skin and the
time and/or frequency of observation for the early
detection of extravasation during drug administra-
tion.
For the usability evaluation, the nurses were
questioned about the level of ease in placing and
peeling the film and the time and frequency of clinical
observations during drug administration.
During the procedure, a nurse or a physician
inserted a catheter into the patient to administer the
anticancer drugs; then, the nurse placed the thermo-
sensitive liquid crystal film on a securement film and
routinely started the chemotherapy. Using a question-
naire, a researcher interviewed the nurses regarding
the usability of the film application after finishing drug
administration. The nurses were also asked about
their years of clinical experience.
The questionnaire for nurses consisted of
closed-ended questions, the visual analog scale (VAS),
a three-grade evaluation, and open-ended questions.
We used the following open-ended question:K Did
you change your actions or feelings regarding the
patients because of changes in the temperature
distribution pattern? If you have changed your
actions or feelings regarding the patients, please
freely describe these changes.L
2)Feasibility
Feasibility was operationally defined as the film:s
ability to provide visualization of skin temperature
and to detect extravasation.
For the feasibility evaluation, we examined the
color change of the film, drug administration informa-
tion, catheterization site, drug type, and administra-
tion rates.
We collected data on the patients:characteristics
from their medical records, including information on
age, gender, body mass index (BMI), type of cancer,
and frequency of anticancer drug exposure. A
researcher photographed the film at repeatedly
observation during drug administration. We observed
the film at an interval time of roughly less than 30 min.
Journal of Nursing Science and Engineering(2020)
― 91 ―
Figure 2 Specification and usage of thermosensitive
liquid crystal film

3) Safety
We confirmed the safety of the film by assessing the
patients:symptoms or feedback just after using the
film. The patients were asked about their impression
and symptoms when using the film during drug
administration. Using a questionnaire, a researcher
interviewed the patients with regard to the safety of
film application after finishing drug administration.
The questionnaire for the patients consisted of
closed-ended questions, the VAS, and the following
open-ended question: Please let us know if you have
any impressions about the film.
Ethical consideration
An informed written consent was obtained from all
participants after receiving a written explanation of
the study. This study was conducted in accordance
with the Declaration of Helsinki, and the study
protocol was approved by the Research Ethics
Committee of the University of Tokyo (No: 11650).
Results
Eight of 10 nurses who worked in the chemother-
apy room participated in this study. All participating
nurses had over 2 years of clinical experience.
Meanwhile, 40 patients participated in the study
wherein 60% were female, the average age was 69.1
(SD 12.9) years, and the average BMI was 21.1 (SD 3.8)
(Table 1). All 40 patients with film application could
use the film continuously until completing their
anticancer drug administration without well-defined
extravasation. Median of the total drug administration
time was 111 min (IQR: 86-201).
1. Usability
Generally, 2 or 3 nurses were responsible for 1
patient. Nurses answered one questionnaire corres-
ponding to 1 patient. Thus, one questionnaire sheet
was filled out by multiple nurses.
During the clinical observations, 77.5% (31/40) and
80.0% (32/40) of the answers indicated that using the
Journal of Nursing Science and Engineering(2020)
― 92 ―
Table 1 Demographic characteristics and anticancer drugs (patient N=40)
Number, (%)/Mean±SD/Median (IQR1-IQR3)
Age (years) 69.4±12.9
Gender
Female 24 (60.0)
BMI N=39 21.2±3.8
Kind of cancer
Pancreatic cancer 14 (35.0)
Breast cancer 10 (25)
Stomach cancer 5 (12.5)
Lung cancer 2 (5.0)
Ovarian tumor 2 (5.0)
Skin cancer 2 (5.0)
Brain cancer 2 (5.0)
Others 3 (7.5)
Kinds of anticancer drug (viewpoints of tissue damage)
Vesicant 17 (42.5)
Irritant 5 (12.5)
Non-vesicant 18 (45.0)
Drug administration time (minutes) 111 (86-201)
Frequency of anticancer drug exposure 9.5 (5.25-14.0)
Catheterization site
Forearm 33 (82.5)
Cubital fossa 3 (7.5)
Hand 4 (10.0)
BMI: Body mass index

film did not affect the time and frequency of
observations, respectively. Other questions were
answered with the VAS. Median of the answers on
whether the location where the film should be placed
was easy to decide or not was 21 (Easiest=0). All
answers about the size, hardness, form, and color
obtained a median of around 50. Median of the
answers on whether the peeling of the film was easy
or not was 48 (Easy=0, Difficult=100), but the maximal
value was 90 (Table 2).
Some nurses described freely the usability of the
film. Nurses felt secured because they could visualize
the infusion flow along the vein in six cases. One of the
responses was,K I had a sense of security that the
drug solution is surely administered in the blood
vessel.LNurses also perceived that the film is
strongly adhesive in three cases. One response was,
KWhen I removed the thermosensitive liquid crystal
film, I had to pay attention not to remove the
securement film simultaneously, because I felt its
adhesion ability is quite strongL.
2. Feasibility
No evident extravasation features, such as occlu-
sion, redness, severe pain, absence of blood return, and
an interruption to the free flow of an infusion, were
noted. All patients completed their anticancer drug
administration without local adverse events.
Administration rates of anticancer drugs were 56-
500 ml/h. No cases without a low-temperature area
were found under anticancer drug administration of
more than 500 ml/h. In the current study, low-
temperature area distribution patterns were classified
into six types as follows:Kno low-temperature area,L
Ksharp line along the vein,LKbroad area from the vein,L
K circle to the line along the vein, LK fan at the
puncture site, LandK spot keeping. LOnlyK spot
keeping Lwas found as the new low-temperature
distribution pattern. Additionally,Klarge area of the
external side,Lwhich was observed in the previous
study, was not observed in the current study (Figure 3).
Journal of Nursing Science and Engineering(2020)
― 93 ―
Table 2 Nurses:usability evaluation of the thermo-sensitive liquid crystal film
QuestionsNumbers
respondedAnswers
Did you peel off the film for observation? 37 I did. 11/I did not. 26
How difficult was peeling the film off? 48 (0,90)*1
Did observation time change for catheterization sites or skin by using the film? 40 Increase 9/No change 31/Decrease 0
Did frequency of observation change for catheterization sites or skin by using the film? 40 Increase 8/No change 32/Decrease 0
When you observe the catheterization sites, have you experienced as follow?
I was about to remove a catheter, with the thermo-sensitive liquid crystal film. 37 I was. 3/I was not. 18/I did not peel it off. 16
I was about to peel off the securement film, with the thermo-sensitive liquid crystal film. 38 I was. 0/I was not. 20/I did not peel it off. 18
Did you change your action or feeling against for the patients with the change of the temperature
distribution pattern?38 I did. 9/I did not. 29
About putting the thermo-sensitive liquid crystal film
When you decide location for putting the film on, was it easy to put?*1 40 21 (0,68)
How did you think about the size?*2 40 41 (0,60)
How did you think about the hardness?*3 40 45 (0,59)
How did you think about the form?*4 40 49.5 (0,60)
How did you think about color that the film shows?*5 40 51 (0,60)
How did you feel about adhesive power of the film after putting it on?*6 38 48 (5,57)
Evaluation of VAS was showed as median (minimum, max)
* 1: Easy=0, Difficult=100, * 2: Large=0, Small=100, * 3: Hard=0, Soft=100, * 4: Good=0, Bad=100, * 5: Deep=0, Light=100, * 6: Strong=0, Weak=100

Journal of Nursing Science and Engineering(2020)
― 94 ―
Figure 3 Examples of low-temperature distribution pattern
The schema on the left, excluding theKspot keepingLpattern, are based from a previous
study using an infrared thermography.

3. Safety
Forty patients answered the questionnaire regard-
ing the thermosensitive liquid crystal film. All of them
responded that they did not mind using the film, and
they did not have any symptoms due to using the film,
such as itching, pain, cold or hot feeling, tightened
feeling, and other discomfort. The patients reported
their feelings of using the film during chemotherapy
and the visualization of their skin temperature. Two
patients experienced that a nurse peeled off the film,
observed the site under the film, and placed it back
during drug administration. These 2 patients
answered about their impression at that time using
the VAS (Feel secure=0, Feel anxious=100); one
patient answered 0, and another answered 50 (Table
3). In 11 cases, the nurses reported peeling the
thermosensitive liquid crystal film for observation
during drug administration; however, 9 of the 11
patients did not notice this.
One patient who had an extravasation experience
stated,K I had anxiety about extravasation recurr-
ence, but today, I had been relieved by this film
because the drug flow during anticancer administra-
tion can now be visualized.L
There was no epidermal peeling due to the use of
the thermo-sensitive liquid crystal film.
Discussion
In all 40 cases that were applied with the
thermosensitive liquid crystal film, the films were
continuously used until completing the anticancer
drug administration. Extravasation did not occur in
the participants. In addition, they did not complain
such as itching, pain, cold or hot feeling, tightened
feeling, and discomfort, when using such film.
Thermosensitive liquid crystal film can be used as a
new observation tool for extravasation detection in
clinical setting because additional time to treat the
film was considered acceptable according to data. In
such data, approximately 80% of nurses:answers
revealed that the time and frequency of observation
remained unchanged compared with those before
using the film, and most nurses could decide easily
where the film should be placed. The size, hardness,
shape, color and adhesive power of the film were
asked in bipolar. Medians for each of these ratings
were around 50, thus there was no clinical issue and it
was considered that there was no need to change the
specifications. Some nurses had an impression that the
film:s adhesion power was strong; however, we had
performed adhesive/remove test repeatedly, and we
confirmed that the adhesive strength that did not
affect the securement film and the skin at the
insertion site in the developing phase. Thus, we think
that the adhesive strength does not require modifica-
tion immediately. However, thorough education on
how to safely peel the film is essential because older
patients or other patients receiving some chemother-
apy have vulnerable skin.
The thermosensitive liquid crystal film may make
Journal of Nursing Science and Engineering(2020)
― 95 ―
Table 3 Patients:safety evaluation of the thermo-sensitive liquid crystal film
Questions Numbers responded Answers
Did you mind using the film? 40 I did. 0/I did not. 40
Did you feel any of the following symptoms?
Itching 40 Yes 0/No 40
Pain 40 Yes 0/No 40
Heat feeling 40 Yes 0/No 40
Cold feeling 40 Yes 0/No 40
Tightening sansation 40 Yes 0/No 40
Other discomfort 40 Yes 0/No 40
How did feel about being able to visualize skin temperature? 40 38 (0, 53)*
How did feel about using the film in the area around the secured catheter? 40 20 (0, 52)*
Did you have an experience with peeling off the film, and reapplying it? Yes 2/No 38
If you have the above experience, how did you feel? 2 25 (0, 50)*
Evaluations of VAS shows as median (range)*: Feel secure=0, Feel anxious=100

the nurses feel secured, considering that nurses had a
sense of security because they could visualize the
infusates flowing along the vein in six cases. Accord-
ing to one previous study, 83.4% of nurses reported
that they had experienced at least one undesirable
error while preparing or administering chemother-
apeutic drugs during their professional life, and
Kstress, tiredness, and burn-out syndromeLwas one
of the reasons of that error12)
. Current chemotherapy is
an extremely complex treatment due to using
multiple drugs, having various sequences of drug
administration, and requiring strict infusion time.
Furthermore, most anticancer drugs are highly
toxic13)
; thus, nurses must be sensitive to prevent
extravasation and occupational exposure14)
. Given the
abovementioned points, anticancer drug administra-
tion may lead to heavy stress to nurses, and reducing
nurses:stress is important. This pilot study suggested
that the thermosensitive liquid crystal film may help
reduce their stress.
In current study, the low-temperature distribution
patterns on the skin surface using the thermosensi-
tive liquid crystal film were classified into six patterns.
Most of the distribution patterns of skin-surface
temperature of the film were similar to those in our
previous study that used infrared thermography7)
(Table 4). When the administration rate was 500 ml/h
or more, all cases with low-temperature area were
confirmed. This condition is essential for the assess-
ment tool (film) to be used as an extravasation
detection device. Early detection of extravasation
during high-speed drug administration is the crucial
point to reduce tissue damage because large amounts
of leaked drugs may result in severe damage on the
subcutaneous tissue15)
.
Using this film may lead to patients:feeling of
security because according to their answers, the
maximum, median, and minimum values were 52, 20,
and 0, respectively, in the VAS (Feel security=0, Feel
anxiety=100). In other words, using this film could
provide a sense of security to patients during
anticancer administration and not only early detection
of extravasation. Especially, anticancer administration
may lead to stress for patients who had an extravasa-
tion experience. Visualization of anticancer flow can
make the patients feel secured.
This study has some limitations. We could not
confirm the feasibility of early extravasation detection
because sample size was small due to this is a pilot
study, possibly leading to such result. We could not
observe onset delayed extravasation symptoms such
as ulcer or induration, because this study was cross-
sectional study. Extrapolation of results requires
attention because this pilot study was conducted in a
chemotherapy room in outpatient service. Generally,
anticancer drug administration time in the outpatient
service is shorter than that in the inpatient ward, it
means that the using time of the thermosensitive
crystal liquid film in the outpatient service is shorter
than that in the inpatient ward. Thus, the usability
and safety of this film were unclear in the inpatient
ward.
In future studies, a sufficient number of patients,
longitudinal research and a different situation, such as
in the inpatient ward, are necessary.
Conclusion
The thermosensitive liquid crystal film was used in
40 patients undergoing anticancer treatment using a
peripheral intravenous catheter in a chemotherapy
room without adverse events. Most of the nurses:
answers indicated that the film did not influence the
Journal of Nursing Science and Engineering(2020)
― 96 ―
Table 4 Temperature distribution patterns
Results from preveous study using aninfrared thermography(n=74)
Results of this study using the thremo-sensitive liquid crystal film(n=40)
No low temperature area 14 (18.9%) 6 (15.0%)
Sharp line along vein 40 (54.1%) 16 (40.0%)
Broad area from vein 7 (9.5%) 5 (12.5%)
Circle to line along vein 2 (2.7%) 3 (7.5%)
Fan at puncture site 7 (9.5%) 2 (5.0%)
Large area of external side 4 (5.4%) 0 (0.0%)
Spot keeping − 8 (20.0%)

time and frequency of observing the catheterization
sites. Therefore, the usability and safety of the film
were confirmed acceptable in the clinical setting. Six
types of temperature distribution patterns were
observed using the thermosensitive liquid crystal film.
However, extravasation did not occur; thus, the film:s
feasibility still needs to be confirmed. A larger sample
size and longitudinal study is required in future
studies to verify the effectiveness of the thermosensi-
tive liquid crystal film in early detecting extravasa-
tion.
Conflict of interest
This study was a part of the joint research of a
peripheral intravenous catheter management with
Terumo Co. Mari Abe-Doi and Ryoko Murayama
belong to the laboratory supported by Terumo Co.
Hidenori Tanabe is an employee of Terumo Co. The
thermosensitive liquid crystal films were provided by
Terumo Co.
Funding
This work was supported by JSPS KAKENHI
Grant Number 17H06645 and The Yasuda Medical
Foundation.
Reference
1) Wengström Y, Margulies A.European Oncology
Nursing Society Task Force. European Oncology
Nursing Society extravasation guidelines. Eur J Oncol
Nurs 12: 357-361, 2008.
2) Jackson-Rose J, Del Monte J, Groman A, et al.
Chemotherapy Extravasation: Establishing a National
Benchmark for Incidence Among Cancer Centers.
Clin J Oncol Nurs 21: 438-445, 2017.
3) U. S. Department of Health and Human Services.
National Institutes of Health National Cancer Institute
Common Terminology Criteria for Adverse Events
(CTCAE) Version 5.0, Page 42 (2017/11). 2019/9/17,
[https://ctep.cancer.gov/protocolDevelopment/elec-
tronic_applications/docs/CTCAE_v5_Quick_Refer-
ence_8.5x11.pdf]
4) Wickham R, Engelking C, Sauerland C, et al. Vesicant
extravasation part II: Evidence-based management
and continuing controversies. Oncol Nurs Forum 33:
1143-1150, 2006.
5) J A Pérez Fidalgo, L García Fabregat, A Cervantes, et
al. Management of Chemotherapy Extravasation:
ESMO Clinical Practice Guidelines. Ann Oncol 23:
vii167-vii173, 2012.
6) Sakaida E, Sekine I, Iwasawa S, et al. Incidence, risk
factors and treatment outcomes of extravasation of
cytotoxic agents in an outpatient chemotherapy
clinic. Jpn J Clin Oncol 44: 168-171, 2014.
7) Onesti MG, Carella S, Fioramonti P, et al. Chemother-
apy Extravasation Management: 21-Year Experi-
ence. Ann Plast Surg 79: 450-457,2017.
8) Schulmeister L. Extravasation management: clinical
update. Semin Oncol Nurs 27: 82-90, 2011.
9) Matsui Y, Murayama R, Tanabe H, et al. Evaluation of
the Predictive validity of thermography in identifying
extravasation with intravenous chemotherapy infu-
sions. J Infus Nurs 40: 367-374, 2017.
10) Oya M, Takahashi T, Tanabe H, et al. Low-tempera-
ture infiltration identified using infrared thermogra-
phy in patients with subcutaneous edema revealed
ultrasonographically: A case report. Drug Discov
Ther 10: 117-122, 2016.
11) Oya M, Murayama R, Oe M, et al. Continuous
thermographic observation may predict extravasa-
tion in chemotherapy-treated patients. Eur J Oncol
Nurs 28: 56-61, 2017.
12) Ulas A, Silay K, Akinci S, et al. Medication errors in
chemotherapy preparation and administration: a
survey conducted among oncology nurses in Turkey.
Asian Pac J Cancer Prev 16: 1699-1705, 2015.
13) Pluschnig U, Haslik W, Bayer G, et al. Outcome of
chemotherapy extravasation in a large patient series
using a standardised management protocol. Support
Care Cancer 23: 1741-1748, 2015.
14) Graeve CU, McGovern PM, Alexander B, et al.
Occupational Exposure to Antineoplastic Agents: An
Analysis of Health Care Workers and Their Environ-
ments. Workplace Health Saf 65: 9-20, 2017.
15) Darcy Doellman, Lynn Hadaway, Leigh Bowe-Ged-
des, et al. Infiltration and extravasation: update on
prevention and management. J Infus Nurs 32:
203-211, 2009.
Journal of Nursing Science and Engineering(2020)
― 97 ―

原 著
抗がん剤の血管外漏出早期発見のための新しい液晶感温フィルム
の使用感,実現可能性,安全性における臨床評価:
パイロットスタディ
阿 部 麻 里.)
・村 山 陵 子.)/)
・田 邊 秀 憲0)
・上山恵三子1)
小見山智恵子1)
・松 井 優 子2)
・真 田 弘 美/)3)
.)東京大学大学院医学系研究科社会連携講座アドバンストナーシングテクノロジー/)東京大学医学部附属グローバルナーシングリサーチセンター
0)テルモ株式会社研究開発部門1)東京大学医学部附属病院看護部
2)公立小松大学保健医療学部看護学科3)東京大学大学院医学系研究科健康科学・看護学専攻老年看護学/創傷看護学分野
要 旨
抗がん剤の血管外漏出の早期発見は重要であるが,そのアセスメントはむずかしく,客観的手法が求められている.
そこで液体貯留が皮膚表面温度の低下をもたらすことから,非侵襲的かつ持続使用可能で安全な血管外漏出アセスメン
トツールとして,液晶感温フィルムを開発した.研究目的は,開発したフィルムの使用感,安全性,皮膚表面温度の可
視化における実現可能性を確認することである.患者 40名と看護師 8名を対象とした.明らかな血管外漏出はなかっ
た.使用後の調査において,患者は全員がフィルムを使用してもよいと答え,かゆみなどの不快感があったものはいな
かった.看護師は,感温フィルムをカテーテル固定用フィルムの上に貼付し,通常通り薬剤投与を行い,使用感を感温
フィルム 1枚ごとに評価した.看護師の回答の 80%において観察の頻度は変わらなかったことから,業務負担への影響
は少ないと考えられた.カメラで記録された温度分布は 6つのパターンに分類された.以上より,血管外漏出アセスメ
ントツールとしての実現可能性が示唆された.
キーワード:化学療法,血管外漏出,末梢静脈カテーテル,皮膚表面温度
キーメッセージ
�.今回の研究は看護・介護のどのような問題をテーマにしているのか?
研究を行うきっかけとなったことはどのようなことか?
抗がん剤静脈投与における血管外漏出の早期発見をテーマとしている.血管外漏出により重篤な障害を起こす可能
性のある抗がん剤治療を,患者も看護師も安心して治療を行う方法はないかと考えた.
�.この研究成果が看護・介護にどのように貢献できるのか?あるいは,将来的に貢献できることは何か?
視診・触診・問診で行われてきた血管外漏出のアセスメントにカテーテル留置部周囲の皮膚温度という新たな方法
が加わる可能性が示唆された.将来的には,抗がん剤投与中の異常の早期発見に貢献できる.
�.今後どのような技術が必要になるのか?
持続的にモニタリングしている温度変化により発見される異常をすみやかに医療従事者へ知らせるような技術開発
が必要である.
Journal of Nursing Science and Engineering(2020)
― 98 ―