The Digestive System Part 2. Bowel Infections 2 Clostridium difficile: An opportunistic infection...
-
Upload
donald-melton -
Category
Documents
-
view
214 -
download
0
Transcript of The Digestive System Part 2. Bowel Infections 2 Clostridium difficile: An opportunistic infection...
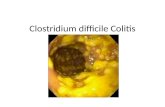
- Slide 1
- The Digestive System Part 2
- Slide 2
- Bowel Infections 2
- Slide 3
- Clostridium difficile: An opportunistic infection associated with broad-spectrum antibiotic use (a suprainfection). E. coli O157:H7: A strain of E. coli that produces a toxin that can make some humans very sick. This strain of E. coli is carried by cattle and is transmitted to humans through fecal contamination. 3
- Slide 4
- E. coli O157:H7 4
- Slide 5
- Not everyone infected with E. coli O157:H7 gets diarrhea or any other symptoms. Ex. people who work around cattle their entire lives may be immune to the strain Some people get very sick or even die. Some may develop hemolytic-uremic syndrome. Some may develop thrombotic thrombocytopenic purpura (TTP). 5
- Slide 6
- Bowel Infections Appendicitis 6
- Slide 7
- Appendicitis is a localized infection of the appendix, which is a blind outpouching from the cecum. 7
- Slide 8
- Appendicitis Signs and Symptoms 8
- Slide 9
- Manifests as ill-defined pain starting in the area of the umbilicus and later progressing to the lower right quadrant. Fever is an undependable sign. A feeling of abdominal fullness and wanting to defecate is common. The bowel is shut down because of inflammation. Bowel sounds will be absent and the patient may think he/she is constipated. Vomiting or loss of appetite is common. If the appendix ruptures, pain may abate to return later with signs of an acute abdomen. 9
- Slide 10
- Diverticulitis 10
- Slide 11
- Diverticulitis Diverticuli are outpouchings that have developed throughout the intestine, although they are most common in the large bowel. Most adults have them to some degree, some more than others They can get infected and rupture, similar to the appendix. Signs and symptoms are similar to appendicitis except they may not necessarily be on the right lower quadrant 11
- Slide 12
- Duodenal Diverticuli 12
- Slide 13
- Duodenal Diverticuli 13
- Slide 14
- Irritable Bowel Syndrome Diagram 14
- Slide 15
- An 80-year-old man with a history of irritable bowel syndrome presented with a 5-day history of abdominal pain in the left lower quadrant, without aggravating or relieving factors Fisher R and Doma S. N Engl J Med 2009;361:286 15
- Slide 16
- Stages of Diverticulitis 16
- Slide 17
- Jacobs D. N Engl J Med 2007;357:2057-2066 Stages of Diverticulitis Antibiotics are prescribed to treat the infection. Abscesses may be drained percutaneously. In about 10% of cases, surgery is necessary to remove a section of the colon or even to remove the entire colon (total colectomy) 17
- Slide 18
- Colorectal Cancer Polyps 18
- Slide 19
- Colorectal Cancer Polyps Third cause of death from cancer for both men and women Most colorectal cancer starts out as a benign polyp which progresses to carcinoma in situ and finally to invasive cancer. Not all polyps progress to cancer. Most polyps bleed sporadically. Bleeding can be detected by the fecal occult blood test (FOBT). 19
- Slide 20
- Colorectal Cancer Treatment 20
- Slide 21
- Colorectal Cancer Treatment We can prevent the development of most colorectal cancer by removing all polyps. Do not know which, if any, will become cancer but just to be safe all of them should be removed Polyps, and therefore colorectal cancer, develop in the lumen of the colon. In order to become metastatic, the cancer has to invade the smooth muscle of the intestine and gain access to blood vessels and/or the peritoneal cavity. If the cancer has not invaded very far, the prognosis is very good. If it has metastasized, colorectal cancer always metastasizes to the liver and sometimes elsewhere. 21
- Slide 22
- Colonoscopy Diagram 22
- Slide 23
- 23 Fu K and Sano Y. N Engl J Med 2006;355:1912 A 56-year-old man underwent a colonoscopy after a positive fecal occult-blood test 23
- Slide 24
- The Gallbladder Diagram 24
- Slide 25
- The Gallbladder Diagram Porth, 2007, Essential of Pathophysiology, 2 nd ed., Lippincott, p. 632 25
- Slide 26
- Components of Bile 26
- Slide 27
- Components of Bile 1.Bile salts are detergents which emulsify fat for digestion. 2.Bile pigments are mainly conjugated bilirubin. 3.Cholesterol. 27
- Slide 28
- Function of the Gallbladder 28
- Slide 29
- Function of the Gallbladder The gallbladder also concentrates the bile by removing water If it removes too much water, it can precipitate the bile (which is usually made of cholesterol) Many people have gallstones and do not even know it The problems come when the gallstones leave the gallbladder and get stuck somewhere 29
- Slide 30
- Causes of Gallstones 30
- Slide 31
- Guyton & Hall, Textbook of Medical Physiology, 9 th ed., Saunders, 1996, p.830. Causes of Gallstones 31
- Slide 32
- Gallstones Diagram 32
- Slide 33
- Yekeler & Akyol, NEJM 351:2318, 2004 33
- Slide 34
- 34 Porth, 2007, Essential of Pathophysiology, 2 nd ed., Lippincott, p. 653 34
- Slide 35
- Treatment of Gallstones 35
- Slide 36
- Treatment of Gallstones Since it is felt that new stones will probably re-form if we just remove the stones, the gall bladder is usually removed. When the gall bladder is no longer present, the bile will not be as concentrated and precipitation of the components probably will not occur. Gall bladder surgery is typically done endoscopically through the abdominal wall. In patients who are not candidates for surgery, stones can be fragmented with lithotripsy. If they are in the duct, they can be crushed endoscopically from the stomach. There are drugs that dissolve gallstones, but they are not used very much. 36
- Slide 37
- The Liver Diagram 37
- Slide 38
- Porth, 2007, Essential of Pathophysiology, 2 nd ed., Lippincott, p. 633 The Liver Diagram 38
- Slide 39
- Functions of the Liver 39
- Slide 40
- Functions of the Liver A. Carbohydrate metabolism B. Lipid metabolism. C. Protein and energy metabolism. 1.Enzymes important in energy metabolism: ALT, AST, GGT - Used as tests for liver necrosis 2. Synthesis of plasma proteins: albumin, coagulation factors, etc. 40
- Slide 41
- Blood Flow of the Liver 41
- Slide 42
- Blood Flow of the Liver 1.Hepatic artery: 350 ml/min 2.Portal vein: 1100 ml/min 3.Total blood flow: 1450 ml/min, 29% of resting cardiac output. 4.The liver is drained by the hepatic vein, which enters the inferior vena cava. 42
- Slide 43
- Detoxification 43
- Slide 44
- Detoxification The liver binds polar molecules to drugs and other molecules. This is called conjugation. Conjugating drugs and other molecules makes them easier to excrete, either by the kidney or in the bile. Bilirubin is detoxified by conjugation (addition) of a glucuronic acid molecule. 44
- Slide 45
- Bilirubin Formation, Circulation, and Elimination Diagram 45
- Slide 46
- Porth, 2007, Essential of Pathophysiology, 2 nd ed., Lippincott, p. 636 The process of bilirubin formation, circulation and elimination Urobilinogen is responsible for the brown color of the stool 46
- Slide 47
- Excretion by the Liver 47
- Slide 48
- Excretion by the Liver Bile is the vehicle for excretion What is excreted? 1. Some drugsmost are conjugated before excretion 2. Bilirubin 3. Cholesterol 48
- Slide 49
- Hepatitis 49
- Slide 50
- Hepatitis Means inflammation of the liver. Stating hepatitis does not indicate what the cause is, just that there is inflammation. There are several different etiologies: 1.Toxic Hepatitis is caused by drugs/chemicals like halothane or isoniazid. 2.Bacterial hepatitis is caused by such organisms as TB, Staph, or Pseudomonas 3.Parasitic hepatitis is caused by a variety of parasites 4.Viral hepatitis is caused by such viruses as Epstein Barr, and Hepatitis A, B, or C - This is usually what the person means 50
- Slide 51
- Hepatitis A: Viral 51
- Slide 52
- Hepatitis A: Viral Sort of a mild disease May feel sick, but most people do not die from hepatitis A Vaccine available No carrier state You have it and then you get over it and do not have it anymore Caused by oral ingestion of contaminated water or food (fecal- oral route). Lifetime protection against re-infection if you get either the vaccine or the infection 52
- Slide 53
- Hepatitis B: Viral 53
- Slide 54
- Hepatitis B: Viral Vaccine available Carrier (chronic active) state Spread by parenteral routes and exchange of body fluids For the majority of hepatitis B patients, it is unknown how they got it because there is a long incubation period and the person does not remember Long incubation period Acute disease can last weeks or months Afterward may get rid of the disease or may go into an active chronic hepatitis and have it forever 54
- Slide 55
- Hepatitis B: Viral Diagram 55
- Slide 56
- Hepatitis B: Viral Diagram Porth, 2007, Essential of Pathophysiology, 2 nd ed., Lippincott, p. 640 56
- Slide 57
- Progression/Outcomes of Hepatitis B Infection 57
- Slide 58
- Kumar et al, 2010, Robbins & Cotran, Pathologic Basis of Disease, 8 th ed. Elsevier, Progression/Outcomes of Hepatitis B Infection 58
- Slide 59
- Blood Markers of Acute Hepatitis B Infection and Recovery 59
- Slide 60
- Blood Markers of Acute Hepatitis B Infection and Recovery Kumar et al, 2010, Robbins & Cotran, Pathologic Basis of Disease, 8 th ed. Elsevier, 60
- Slide 61
- Blood Markers of Chronic Active Hepatitis B Infection 61
- Slide 62
- Blood Markers of Chronic Active Hepatitis B Infection Kumar et al, 2010, Robbins & Cotran, Pathologic Basis of Disease, 8 th ed. Elsevier, 62
- Slide 63
- Hepatitis C 63
- Slide 64
- Hepatitis C Parenteral routes of transmission. Carrier (chronic active) state is more frequent with hepatitis C than with hepatitis B. Blood tests are available for the virus itself or for antibodies. 64
- Slide 65
- Progression/Outcomes for Hepatitis C 65
- Slide 66
- Kumar et al, 2005, Robbins & Cotran, Pathologic Basis of Disease, Elsevier, p.894 Progression/Outcomes for Hepatitis C 66
- Slide 67
- A patient has the following lab tests: Hepatitis B viral DNA is negative; IgG- anti-HBc is positive. IgM-anti-HBc is negative. What can we say about this patient? 67
- Slide 68
- A patient has the following lab tests: Hepatitis B viral DNA is negative; IgG-anti-HBc is positive. IgM-anti-HBc is negative. What can we say about this patient? 1.He has active hepatitis B 2.He is contagious with hepatitis B 3.He was exposed to hepatitis B in the past but has recovered 4.We can't tell whether he has active hepatitis B from these tests 68
- Slide 69
- Characteristics of Hepatitis A, Hepatitis B, and Hepatitis C 69
- Slide 70
- Characteristics of Hepatitis A, Hepatitis B, and Hepatitis C Point of comparisonHepatitis AHepatitis BHepatitis C Causative agentHepatitis A virusHepatitis B virusHepatitis C virus Infections that become chronicNone3%-5%>70% Acute infections each year in the US 179,000185,00038,000 US residents with chronic infection None1.25 million2.7 million Annual deaths in the US from chronic infection None60008000-10,000 People worldwide with chronic infection None350 million170 million Method of preventionHepatitis A vaccine Hepatitis B vaccineHepatitis C vaccine (not yet available) Preferred treatmentNoneInterferon alfa or lamivudine Interferon alfa plus ribavirin Adapted from Lehne, 2009, Pharmacology for Nursing Care, 7 th ed., Elsevier, p. 1076 70
- Slide 71
- Complications of Chronic Active Hepatitis B or C 71
- Slide 72
- Complications of Chronic Active Hepatitis B or C Cirrhosis with portal hypertension may manifest as: 1. Varices in the GI tract 2. Ascites 3. Congestive splenomegaly Hepatocellular carcinoma Liver failure may manifest as: 1. Low coagulation factors/bleeding 2. Low serum albumin lowers the serum osmolic pressure/edema 3. Hepatic encephalopathy 72
- Slide 73
- Features of Cirrhosis 73
- Slide 74
- Features of Cirrhosis 1.Fatty liver: reversible, caused by alcohol consumption and many other things. 2.Fibrosis: not reversible; hepatic vasculature is rearranged, causing portal hypertension and varices. 74
- Slide 75
- The Liver and its Venous Vasculature 75
- Slide 76
- Porth, 2007, Essential of Pathophysiology, 2 nd ed., Lippincott, p. 633 The Liver and its Venous Vasculature 76
- Slide 77
- Consequences of Cirrhosis/Liver Failure 77
- Slide 78
- Consequences of Cirrhosis/Liver Failure 1.Portal hypertension with varices 2.Ascites - The pressure in the liver vasculature is so great that fluid is squeezed out of the vasculature and into the portal cavity 3.Portosystemic venous shunts 4.Congestive splenomegaly - Blood backs up out of the liver 5.Hepatic encephalopathy - Brain problems and confusion due to buildup of ammonia because it cannot be converted into urea and excreted from the body 78
- Slide 79
- Consequences of Liver Failure 79
- Slide 80
- Porth, 2007, Essential of Pathophysiology, 2 nd ed., Lippincott, p. 649 Consequences of Liver Failure 80
- Slide 81
- Consequences of Portal Hypertension 81
- Slide 82
- Porth, 2007, Essential of Pathophysiology, 2 nd ed., Lippincott, p. 646 Consequences of Portal Hypertension 82
- Slide 83
- Portal Hypertension and the Diversion of Blood Flow Diagram 83
- Slide 84
- Porth, 2007, Essential of Pathophysiology, 2 nd ed., Lippincott, p. 648 Portal Hypertension and the Diversion of Blood Flow Diagram 84
- Slide 85
- Portal Hypertension and the Diversion of Blood Flow 85
- Slide 86
- Portal Hypertension and the Diversion of Blood Flow The portal veins drain the lower part of the esophagus and the stomach Normally, blood is going through the blood vessels, down the veins, into the liver and the portal vein Other blood goes through the vessel into the vena cava If there is a backup, the blood cannot get through the liver and it results in portal hypertension The veins enlarge and you get varicosities in the lower esophagus and throughout the gastrointestinal tract People can actually bleed to death from lower esophageal varices 86
- Slide 87
- Porto-systemic Venous Shunts 87
- Slide 88
- Porto-systemic Venous Shunts 88 Caput medusa. Esophageal varices. Yang P and Chen D. N Engl J Med 2005;353:e19 88
- Slide 89
- Varices Caused by Portal Hypertension 89
- Slide 90
- Varices Caused by Portal Hypertension The varices in the esophagus are typically the most troublesome and bleed, sometimes profusely. Bleeding varices can also develop in the stomach or intestinal mesentery. Internal hemorrhoids are varices of veins that drain the rectum and are frequently caused by liver disease. (External hemorrhoids are not caused by liver disease and are almost a universal finding in people over about age 30). 90
- Slide 91
- Causes of Ascites Liver Disease 91
- Slide 92
- Causes of Ascites Liver Disease Causes: 1. Increased lymph formation by liver with transudation through hepatic capsule. Transudation involves the slow escape of liquids from blood vessels through pores or breaks in cell membranes. 2. Sodium and water retention by kidney. 3. Hypoalbuminemia 92
- Slide 93
- Ascites Diagram 93
- Slide 94
- Ascites Diagram 94
- Slide 95
- Cirrhosis Diagram 95
- Slide 96
- A 52-year-old man with cirrhosis associated with alcohol abuse presented to the emergency department with hematemesis and lightheadedness, which had developed 3 hours earlier, after binge drinking Torrazza-Perez E and Carreno N. N Engl J Med 2010;362:e13 Video: http://www.nej m.org/doi/full/1 0.1056/NEJMic m0807812 96
- Slide 97
- Other Consequences of Liver Failure 97
- Slide 98
- Other Consequences of Liver Failure Congestive splenomegaly caused by portal hypertension. Hepatic encephalopathy: not sure of cause, but probably ammonia is not the whole story. Difficulty in metabolizing particular drugs (acetaminophen). 98
- Slide 99
- Hepatocellular Carcinoma 99
- Slide 100
- Hepatocellular Carcinoma Associated with cirrhosis, hepatitis B, or hepatitis C Environmental toxins can cause it (aflatoxins). The liver is a favorite site of metastasis for many different kinds of cancer that arise elsewhere, such as colon, breast, and lung. These cancers are not liver cancers. 100