Survival, Prognostic Factors, and Therapeutic Efficacy in Low …€¦ · of treatment, and...
Transcript of Survival, Prognostic Factors, and Therapeutic Efficacy in Low …€¦ · of treatment, and...

Survival, Prognostic Factors, and Therapeutic Efficacyin Low-Grade Glioma: A Retrospective
Study in 379 Patients
By Knut Lote, Thore Egeland, Bjarne Hager, Beth Stenwig, Kari Skullerud, Jon Berg-Johnsen,Ingebjerg Storm-Mathisen, and Henry Hirschberg
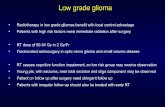
Purpose: We report survival, prognostic factors, andtreatment efficacy in low-grade glioma.
Patients and Methods: A total of 379 patients withhistologic intracranial low-grade glioma received post-operative radiotherapy (n = 361) and intraarterial car-mustine (BCNU) chemotherapy (n = 153). Overall sur-vival and prognostic factors were evaluated with theSPSS statistical program (SPSS Inc, Chicago, IL).
Results: Median survival (all patients) was 100months (95% confidence interval [CI], 87 to 113); in agegroup 0 to 19 years (n = 41), 226 months; in age group20 to 49 years (n = 263), 106 months; in age group 50to 59 years (n = 49), 76 months; and for older patients(n = 26), 39 months. Projected survival at 10 and 15years was 42% and 29%, respectively. Patient age,World Health Organization (WHO) performance status,tumor computed tomography (CT) contrast enhancement,mental changes, or initial corticosteroid dependencywere significant independent prognostic factors (P <.05), while histologic subgroup, focal deficits, presence
THE NATURAL COURSE of a low-grade glioma isthat of an indolent or slowly growing CNS tumor
that in some patients, may persist for decades, while otherpatients with similar histology for largely unknown rea-sons may die within a few years.' 6 Age is a salient prog-nostic factor. Pilocytic and cerebellar astrocytomas ofchildhood, 3'6 as well as hemispheric low-grade gliomasin children and teenagers, 3'7 have an excellent prognosis.Adult low-grade gliomas are usually more aggressive,with median reported survival times that range from 3 to5 years ' 28'9 to 7 to 9 years in a recent series of reports.' 0 '4
Reported negative prognostic factors in low-grade gliomainclude reduced performance,9-" mental changes,3 '9" 2 andfocal neurologic deficits. '"" Histologic grade 2'610 or con-trast enhancement on computed tomography (CT)'2 '3 areof prognostic value in some,2 61 2' 3 but not all ' ° studies.Seizures are a common presenting symptom of reportedpositive prognostic significance. 1
' 51'2 '13
Controversy exists with regard to optimal managementof adult low-grade gliomas. Macroscopic complete surgi-cal resection may5'9 12'15 '16 or may not13 '17 increase survivalcompared with partial resection. The infiltrative nature ofthese tumors, where tumor cells have been demonstratedbeyond the area of radiologic abnormalities,18-20 may ex-clude surgical cure.
Radiotherapy may be of benefit in low-grade gli-oma, 1.45 although conclusive data for such benefit are still
of seizures, prediagnostic symptom duration, tumor cat-egory, and tumor stage were not. Patients aged 20 to 49years with no independent negative prognostic factors (n= 132) had a median survival time of 139 months versus41 months in patients with two or more factors (n = 33).Patients who presented with symptoms of expansion (n= 97) survived longer when resected (P < .03); otherwiseno survival benefit was associated with initial tumor re-section compared with biopsy. Intraarterial chemother-apy and radiation doses more than 55 Gy were not asso-ciated with prolonged survival. Among 66 reoperatedpatients, 45% progressed to high-grade histology within25 months.
Conclusion: Prognosis in low-grade glioma followingpostoperative radiotherapy seems largely determinedby the inherent biology of the glioma and patient age atdiagnosis.
J Clin Oncol 15:3129-3140. © 1997 by American So-ciety of Clinical Oncology.
incomplete. 2' 5 '0 '12 Serious late radiation effects may occurafter radiation doses of 45 to 60 Gy to the brain,2 22
especially in small children.'6 '24 Chemotherapy has notbeen shown to prolong survival in low-grade gliomas,although tumor regression may be induced.6 '2 5
We report age distribution, prognostic factors, efficacyof treatment, and survival in 379 patients with low-gradeglioma seen at a single institution during the CT era.
PATIENTS AND METHODS
The records of all patients with primary CNS tumors seen at theNorwegian Radium Hospital during the years 1980 to 1995 wereretrospectively registered in a data base. The hospital is a regionalcancer center that serves a population of 1.6 million living m Easternand Southern Norway outside the town of Oslo. During the years1980 to 1987, the hospital also served as a radiotherapy center for
From the Departments of Oncology, Radiology, and Pathology,Norwegian Radium Hospital; Department of Neurosurgery, OsloCity Hospital; and Departments of Statistics, Pathology, Pediatrics,and Neurosurgery, National Hospital, Oslo, Norway.
Submitted February 3, 1997; accepted June 10, 1997.K.L. was a Research Fellow for the Norwegian Cancer Society.
Oslo, Norway.Address reprint requests to Knut Lote, MD, Department of Oncol-
ogy, Norwegian Radium Hospital, 0310 Oslo, Norway.© 1997 by American Society of Clinical Oncology.0732-183X/97/1509-001 7$3.00/0
Journal of Clinical Oncology, Vol 15, No 9 (September), 1997: pp 3129-3140 3129

LOTE ET AL
the population in the two northern regions of Norway. All regionalglioma patients had to register at the hospital if they were to receiveradiotherapy. Adult patients with performance status worse thanWorld Health Organization (WHO) 3 were usually not admitted.Megavoltage equipment was used in all patients who received radio-therapy.
Variables registered included month and year of first symptom,type of symptoms experienced before admittance, date of radiologicdiagnosis, CT and magnetic resonance image (MRI) findings, histo-logic diagnosis according to the WHO classification system,26 WHOfunctional status 27 at first stay in the hospital, as well as data withregard to tumor localization, tumor category and stage 28 treatment,and survival. Patients usually underwent surgery at either of the twoNeurosurgical Departments in our catchment area before admissionto the Norwegian Radium Hospital. Histologic diagnosis was ob-tained in 90.6% of all registry patients. All consecutive 379 patientswith primary intracranial histological low-grade gliomas (astrocy-toma, oligodendroglioma, or mixed glioma) are included in this re-port.
The prediagnostic period was defined as months that elapsed fromthe first tumor-related symptom to radiologic tumor diagnosis. Sur-vival was calculated from the date of radiologic diagnosis to deathor to date of last observation. All patients were monitored until deathor to December 31, 1995. Date of death for deceased patients wereobtained either from case records or from the Census Bureau.
Statistics
The SPSS statistical package29 was used for data evaluation andpresentation. Tables were tested for statistical significance by x2
tests. Two-sided P values are reported throughout. Differences be-tween means were tested using the two-sample t test. Survival curveswere produced according to the Kaplan-Meier method and differ-ences in survival tested for statistical significance by the log-ranktest. For the purpose of multivariate Cox regression, patients diag-nosed before 1980 (n = 18) were excluded from the analysis. Sepa-rate analysis with these patients included did not materially alterhazards ratios, 95% confidence intervals (CIs), or P values.
With regard to the multivariate model, there are several algorithmsand principles to follow searching for optimal prognostic factors.We used the manual procedure described in Collett.30 First, a numberof Cox regressions, each with one covariate, were performed. Prog-nostic variables with P values less than .10 were considered ascandidates for the multivariate model. In the final model, only covari-ates with P values less than .05 were accepted. The P values werecalculated in the usual way, being based on likelihood ratio tests.We mainly used plots to check the adequacy of the model. No strongclaims are made in cases in which we fail to reject a hypothesis.Therefore, power calculations are omitted.
RESULTS
A total of 379 patients (231 males and 148 females)with histologic low-grade gliomas were seen at the Nor-wegian Radium Hospital during the years 1980 to 1995.Sex did not significantly influence survival (P > .09,Kaplan-Meier log-rank test). Mean and median ages were37 and 38 years, respectively (range, 3 to 72 years). Agedistribution in 10-year age groups is shown in Fig 1.
Only patients with a definite histologic diagnosis of
low-grade glioma are included in the present report.Astrocytoma was by far the largest histologic subgroup(n = 268), followed by oligodendroglioma (n = 69) andmixed glioma (n = 42).
Radiologic diagnosis was based on CT with or withoutMRI in 369 patients (97.4%), on MRI alone in five pa-tients (1.3%) and on other methods, usually angiography,in five patients (1.3%).
All patients had a surgical procedure to obtain tissuefor histologic diagnosis. Operations were registered asbiopsy procedures or resections according to the surgicalreport. Retrospective evaluation of the degree of surgicalresection in resected patients was not attempted.
Radiotherapy was usually given within 1 to 2 monthsfollowing surgery in patients who did not receive intraar-terial chemotherapy. A total of 369 patients received ex-ternal fractionated radiotherapy. Patients were irradiatedto local fields (n = 320), or to whole brain fields (n =47). Field specifications were lacking for two patients.Ten patients were not irradiated and a further eight pa-tients received total doses less than 45 Gy. Fraction dosewas 1.8 Gy, and only eight irradiated patients receivedless than 25 fractions. A total of 361 patients receivedfractionated external radiotherapy to accumulated dosesin the 45- to 70.4-Gy range. The standard fractionationregimen was 1.8 Gy five times a week to a total dose of54 Gy, and 250 patients were so treated. As a matter ofpolicy, no patients in WHO performance group 4 and fewpatients in group three received radiotherapy.
A total of 179 patients received chemotherapy duringtheir illness, usually in the first 2 to 4 months followingsurgery, or at clinical relapse. Chemotherapy consistedof intraarterial carmustine (BCNU)31 in 153 patients, lo-mustine, procarbazine, and vincristine (PCV)32 in 22 pa-tients, and other regimens in four patients. Patients se-lected for intraarterial BCNU had to be younger than 55years, with WHO functional status 2 or better, and withtumor location in brain areas that receive blood supplyfrom the internal carotid artery. These selection criteriaalone probably ensured that patients who received in-traarterial chemotherapy had a better than average prog-nosis.
Survival by Pretreatment Prognostic Factors
Age. Forty-one patients were younger than 20 years.Tumor localization in these young patients was cerebel-lum (n = 10), n. opticus (n = 1), hemispheres (n = 23),and other intracranial loci in seven patients. Histologywas astrocytoma (n = 28), oligodendroglioma (n = 7),and mixed glioma (n = 6). Within the astrocytoma sub-group, histology was juvenile astrocytoma (n = 9), pilo-
3130

SURVIVAL FACTORS IN LOW-GRADE GLIOMA
Fig 1. Age distribution in 379patients with histologic intra-cranial low-grade gliomas seenat the Norwegian Radium Hospi-tal during the years 1980 to1995.
30-3940-49
50-5960-69
70-79
Age Group
cytic astrocytoma (n = 1), and astrocytoma in the re-maining 18 patients.
Patient age was a prominent prognostic factor as shownin Table 1 and Fig 2. Children and teenagers had a 10-year survival rate of 80%. Separate analysis showed thatsurvival in age groups 20 to 29 years, 30 to 39 years,and 40 to 49 years was not substantially different, whilepatients in age groups 50 to 59 and those older than 60years had successively worse prognoses. Accordingly, theKaplan-Meier plot shows survival in age groups 0 to 19years, 20 to 49 years, 50 to 59 years, and older than 60years. The differences in survival are highly significant(P < .001, log-rank; Fig 2). The overall median survivalduration in all patients (n = 379) was 100 months (95%CI, 87 to 113). The projected overall survival rate (allpatients) was 42% at 10 years and 29% at 15 years.
Histologic diagnosis. No difference in survival be-
Table 1. Median Survival With 95% Confidence Intervals by Age Group
Age Group No of Median Survival(years) Patients (months) 95% Cl
0-19 41 226 67-38520-49 263 106 93-11950-59 49 76 40-11260+ 26 39 28-50
tween patients with astrocytoma (n = 268), oligodendro-glioma (n = 69), or mixed glioma (n = 42) was discern-ible (Kaplan-Meier log-rank test). Our data indicate thatthere are no significant differences in prognoses amongthe three major histologic subgroups of low-grade glioma.Admittedly, the oligodendroglioma and mixed gliomagroups are small. However, when survival in astrocytomapatients (median, 105 months; 95% CI, 92 to 118) wascompared with survival in the combined group (n = 111)of oligodendroglioma and mixed glioma patients (median,86 months; 95% CI, 69 to 103), there was no significantdifference in survival by log-rank test.
WHO performance groups. WHO performance statuswas registered after surgery at admission to the NorwegianRadium Hospital. There was no significant difference in sur-vival between patients with performance scale 0 comparedwith patients with scale I (log-rank, P = .1). However, whenthe patients were separated in group 1, WHO 0 to 1 (n =344), versus group 2, WHO 2 to 3 (n = 35), patient perfor-mance status was a powerful predictor of survival (P <.001, log-rank; Fig 3). Patients with minimal or no functionaldeficits had the best prognosis.
Focal neurologic deficits. Patients with affected vi-sual fields (n = 51), cranial nerve palsies, or paresis ofany degree (n = 78) had impaired survival compared with
1
1
c
00
01-0910-19
3131
l

12 24 36 48 60 72 84
LOTE ET AL
Age Groups
a 60-72
+ n=26
= 50-59
_- n=49
= 20-49
+ n=263
= 0-19
Fig 2. Survival according toage in 379 patients with histo-logic intracranial low-grade gli-oma in the age groups 0 to 19,20 to 49, 50 to 59, and > 60years (Kaplan-Meier, P < .001,log-rank).
+ n=4120
Observation Time (months)
patients without these symptoms and signs (P < .0415and P < .0015, respectively, Kaplan-Meier log-rank test).There was no sex difference with regard to cranial nerve
palsies or pareses. However, males were at greater riskfor visual deficits as a symptom of their glioma (P <.0055, X2 test).
Nausea and emesis. Nausea or emesis at admissionwas seen in 58 patients and was not significantly associ-ated with shortened survival (P = .19, Kaplan-Meier log-rank test) compared with patients without these symptoms(n = 321).
Mental Changes. Patients with any degree of tumor-related cognitive or emotional mental changes registeredby themselves, their relatives, or doctor at admission (n
= 106) had a significantly worse prognosis (P < .0001,
I .U
Fig 3. Survival in 379 pa-tients with histological intra-cranial low-grade glioma ac-cording to WHO performancestatus. Patients in performancegroups 0 to 1 were comparedwith patients in performancegroups 2 to 3 (Kaplan-Meier, P< .001, log-rank).
"3
')
E
0
.8-
.6
.4
.2
0.0
Kaplan-Meier log-rank test; Fig 4) compared with pa-tients without mental changes at admission (n = 273).
Presence of seizures. A total of 85% of all patients with
histologic low-grade intracranial glioma developed seizuresduring their illness. Most patients (78%) had their first seizurebefore radiologic tumor diagnosis, and 7% afterwards. Therewas no sex difference in seizure prevaInce. Patients withseizures (n = 322) had a nonsignificant trend toward longermean duration of the prediagnostic period compared withpatients with no seizures (10 months v 6 months, P = .3,two-sample t test), but the presence of seizures was not associ-
ated with prolonged survival (P = .5, Kaplan-Meier log-ranktest). However, the high prevalence of seizures may tend todiminish the weight of seizures as a prognostic factor withinthe low-grade group.
WHO Groups
= 2-3
+ n=35
= 0-1
+ n=3440 12 24 36 48 60 72 84 96 108 120
Observation Time (months)
3132
c',
iD')
EC-)
--.
. .; -..IIA-,
..
.
I.,......;
1..
-
"I1.........
.........,111-I.... I
: ........ .....
1
--

SURVIVAL FACTORS IN LOW-GRADE GLIOMA
Fig 4. Survival in 379 pa-tients with histologic intracraniallow-grade glioma according topresence of any degree of men-tal changes at admission. Af-fected patients were comparedwith patients without thesesymptoms (Kaplan-Meier, P <.0001, log-rank).
C,)W
-5E
0
.8
.6
.4-
.2
0.0U 12 24 ib 4 iU0 /2 84 9 t 108 1ZU
Observation Time (months)
Tumor category and stage. It was possible to assign364 patients to their respective tumor category.28 Reliableinitial CT descriptions or images were missing in 15 pa-tients. There was no significant survival difference be-tween T1 and T2 patients. When survival in patients withT1 and T2 tumors (n = 128) was compared with survivalin the group of patients with T3 and T4 tumors (n =236), the differene was statistically significant (P = .014,Kaplan-Meier log-rank test; Fig 5). Although there wasa trend towards longer survival in stages I and II, thedifference was riot statistically significant (P = .2). Weconclude that the tumor-node-metastasis (TNM) stagingsystem in its present form is of marginal value as a prog-nostic factor in low-grade gliomas.
Tumor CT contrast enhancement. In 353 patients, itwas possible to assess tumor contrast enhancement onthe initial diagnostic CT scan. Reliable data were missing
.e
ia
EO
in 26 cases. The presence of tumor contrast enhancement(n = 84) was a prominent negative prognostic factor (P= .0001, Kaplan-Meier log-rank test; Fig 6) comparedwith patients (n = 269) with a hypodense, nonenhancingtumor, which was the typical finding in most patients. Nosignificant difference was seen between patients youngerthan 20 years or those older with regard to the frequencyof contrast enhancement. Most of the few patientsyounger than 20 years of age with juvenile astrocytoma(n = 9) had tumor contrast enhancement, and they stillhad an excellent prognosis. Contrast enhancement in chil-dren or teenagers with low-grade glioma does not neces-sarily indicate an adverse prognosis. Tumor calcificationswere seen in 70 patients, 50 of whom had oligodendrogli-oma or mixed glioma, which were more likely to showtumor calcifications than astrocytoma (P < .001, X2 test).The presence of detectable calcifications on CT was of
= T3-4
+ n=236
= T1-2
-- n=128
Fig 5. Survival in 364 pa-tients with histologic intracraniallow-grade glioma according toUICC tumor-category.? Patientsin categories 1 to 2 were com-pared with patients in categories3 to 4 (Kaplan-Meier, P < .014,log-rank).
Observation Time (months)
3133
......
= Present
+ n=106
= AbsentAlA
n=273
IA1.v
, · I k . .
-r,~~~~~~~~~%N
·:.~~~~~~~~~~
:·~~~~~~~~% .%..... .....
-A A -AA -- ---

LOTE ET AL
Fig 6. Survival in 353 pa-tients with histologic intracraniallow-grade glioma according tothe presence of tumor contrastenhancement on initial CT. Pa-tients showing enhancementwere compared with patientswith no contrast enhancement(Kaplan-Meier, P < .0001, log-rank).
Observation Time (months)
diagnostic value, but had no discernible prognostic impacton patient survival.
Length of prediagnostic period. The median durationof symptoms before radiologic tumor diagnosis in patientswith low-grade gliomas was 6 months (range, 0 to 300).Forty-two patients had a prediagnostic period greater than5 years, and the duration of the prediagnostic period wasgreater than 10 years for 14 patients. One might expectpatients who harbor such indolent tumors to have betterprospects for long-term survival following tumor diagno-sis. However, patients with a prediagnostic period greaterthan 12 months did not survive significantly longer fromthe time of radiologic diagnosis than patients with shorterprediagnostic periods (Kaplan-Meier log-rank test).
Synopsis of prognostic factors. Table 2 presents anoverview of prognostic factors tested in univariate analy-sis and not found significant in multivariate analysis. Ta-
Table 2. Prognostic Factors Evaluated by Univariate Analysis(Kaplan-Meier, log-rank) and Not Found Significant
in Multivariate Cox's Analysis
Variable P
Histologic subtype of low-grade glioma NS
Prediagnostic period > 12 months NSSurgical volume reduction all patients) NSPresence of seizures NSPresence of initial nausea/emesis NSRadiation dose level 45 to 70.4 Gy NSTreatment with intraarterial BCNU NS
Presence of focal neurologic deficits < .04 (-)Surgical volume reduction in a subset of patients presenting
with signs of expansion < .03 (+)Tumor category 1-2 v 3-4 < .014 (+)
Abbreviations: NS, not significant; (+), positive factor; (-) negative fac-
tor
ble 3 lists the five prognostic factors found to be signifi-cant in multivariate analysis.
Treatment-Related Prognostic Factors
Corticosteroid dependency. Patients who needed cor-ticosteroids in any dose for palliation of symptoms atadmission (n = 50) had significantly reduced survivalcompared with other patients (P < .001, Kaplan-Meierlog-rank test; Fig 7). However, the median survival timein corticosteroid-dependent patients was 43 months (95%CI, 20 to 66 months). Thus, corticosteroid dependencyduring the initial postoperative clinical course of a low-grade glioma does not necessarily indicate immediate de-mise.
Survival according to type of initial surgery. All pa-tients had a surgical procedure to obtain tissue for histo-logic diagnosis. Whenever possible, the neurosurgeonperformed a macroscopically radical resection. A total of272 patients were resected with partial or total macro-scopic tumor volume reduction. Retrospective assessmentof the degree of resection was not attempted. A biopsyprocedure, usually stereotactic, was performed in 103 pa-tients. In four patients, the surgical procedure could notretrospectively be classified with certainty. By univariateanalysis, there was no difference in survival between pa-tients who initially underwent tumor resection with tumorvolume reduction compared with patients who initiallyonly had a biopsy procedure (P = .7, Kaplan-Meier log-rank test; Fig 8). In the subset of patients (n = 97) whopresented with nausea and/or emesis or corticosteroid de-pendency (eg, serious symptoms of an expansive lesion),resected patients (n = 77) survived significantly longer(median, 64 months; 95% CI, 10 to 118) than patients (n= 20) who only had a biopsy procedure (median, 23
3134
caI
s)
Eo3
= Present
+ n=84
= Absent
-n=269

SURVIVAL FACTORS IN LOW-GRADE GLIOMA
Table 3. Prognostic Factors Found Significant in Multivariate Cox's Analysis
Variable Hazards Raho 95% CI P
WHO performance 2-3 v 0-1 2.258 1.422-3.586 .0006
Any mental changes present 2.067 1.510-2.830 .0001
Contrast enhancement present 1.918 1.354-2.718 .0002
Corticosteroid dependency initially present 1.570 1.028-2.397 .0370
Age +1 year vage 1 029 1.017-1.041 .0001
NOTE. Patients diagnosed before 1980 n = 18) were excluded from the analysis. Hazards ratios for mortality for the 5 statistically significant independent
negative prognostic variables are listed with their respective 95% CIs and P values.
months; 95% CI, 10 to 36; P < .0287, Kaplan-Meier log-rank test; Fig 9). However, even within this subgroup,the type of initial surgical treatment did not qualify as asignificant independent prognostic factor for survival inmultivariate analysis.
Fourteen patients who initially underwent biopsy and50 patients initially resected were reoperated with tumorresection at relapse. Thus, few patients with initial biopsywere resected at relapse. In two additional patients whodid not initially have surgery, the histologic diagnosiswas obtained at relapse. Thirty-six patients relapsed withlow-grade histology, 16 progressed to anaplastic gliomas,and 14 progressed to glioblastomas. Overall, 30 of 66patients (45%) with an initial low-grade glioma showedhistologic progression to high-grade gliomas at relapse.The median time to clinical relapse that necessitated reop-eration was 25 months. The median survival durationcalculated from the date of reoperation was 19.5 months(range, 0.6 to 136).
Survival according to radiotherapy. Since 361 of 379patients received conventionally fractionated postopera-tive radiation to doses of at least 45 Gy, we could notassess the effect, if any, of radiotherapy in treated com-pared with untreated low-grade glioma patients. Most pa-
1.
Fig 7. Survival in 379 pa-tients with histologic intracraniallow-grade glioma according tothe presence of corticosteroiddependency at admission. Sur-vival in corticosteroid-depen-dent patients was compared withsurvival in patients not needingcorticosteroids (Kaplan-Meier, P< .001, log-rank).
C.
a,
E0
U
.8
.6
.4
.2
nn
0
tients received 54 Gy in 30 fractions over 6 weeks, al-though total dose varied somewhat during the years 1980to 1995. Thus, it was possible to define three dose ranges:total dose 45 to 50 Gy (n = 45), total dose 51 to 55 Gy(n = 277), and total dose 56 Gy (n = 39). Patientswho for various reasons received doses less than 45 Gy(n = 8) or no radiotherapy at all (n = 10) were excludedfrom the analysis. Survival was not statistically differentfor the three dose levels (P = .2, Kaplan-Meier log-ranktest). Thus, we could not observe any dose-response withregard to survival in the dose range 45 to 70.4 Gy. Norwas there any difference in survival between patients whoreceived radiation to local fields (n = 320) compared withpatients who received whole-brain irradiation (n = 47).
Survival according to chemotherapy. PCV chemo-therapy,3 2 as well as intraarterial chemotherapy withBCNU in selected low-grade glioma patients, was usedduring the years 1983 to 1995.2531 Patients selected forchemotherapy usually received four courses during 4months before radiotherapy. Two hundred patients hadno chemotherapy, four received different regimens, 22received PCV chemotherapy, and 153 received fourcourses of intraarterial BCNU, intravenous vincristine,and oral procarbazine. 3
1 PCV chemotherapy did not seem
12 24 36 48 60 72 84 96 108 120
= Present
+ n=50
= Absent
n=329
Observation Time (months)
...�
.u 1 1 I
3135
n._
'' ~ ~ ~ - .
··~~~~~~~~~~.·- ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ . .. 1 .. I. ._ .··~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ...

LOTE ET AL
12 24 36 48 60 72 84
= Resection
- n=272
= Biopsy
-- n=103
Fig 8. Survival in 375 pa-tients with histologic intracraniallow-grade glioma according toinitial surgical treatment. Pa-tients who had a tumor resectionwith volume reduction were com-pared with patients who only un-derwent a biopsy procedure. Nodifference in survival was ob-served (Kaplan-Meier log-rank).
Observation Time (months)
to influence survival in the few patients treated. Intraarte-rial BCNU chemotherapy was of no statistically signifi-cant benefit for survival compared with the group thatreceived no chemotherapy (P = .35, Kaplan-Meier log-rank test; Fig 10). It is noteworthy that patients selectedfor intraarterial BCNU were younger, had a better perfor-mance status, less often had contrast enhancement on CT,and less often had mental changes. Although marginallyso, they were in a prognostically advantageous group.Chemotherapy did induce tumor regression in some pa-tients, but these responses did not statistically prolongsurvival in treated compared with untreated low-gradeglioma patients.
Multivariate Analysis of Prognostic Factors
Prognostic factors in the multivariate Cox model wereselected from candidate factors with P values less than
Fig 9. Survival in a subset ofpatients n = 97) with histologicintracranial low-grade gliomawho presented with symptoms ofnausea/emesis or initial cortico-steroid dependency according totype of initial surgical treatment.Resection with tumor volume re-duction was associated with pro-longed survival in this subgroup(Kaplan-Meier, P < .0287, log-rank).
:3
U,CD
-5
EO
.8.
.6'
.4'
.2-
nn
.10 as described earlier. Only the five factors presentedin Table 3 were significant independent prognostic factorsat P levels less than .05. Hazards ratios computed relativeto the reference case are given with 95% CIs and theirrespective P values. Statistically significant independentrisk factors for mortality in our low-grade glioma patientswere age, WHO performance status 2 to 3, presence ofany mental or cognitive changes, corticosteroid depen-dency, and tumor contrast enhancement on the initial CTscan (Table 3). Whether the 18 patients diagnosed before1980 were included or excluded from the multivariateanalysis did not materially affect the computed hazardsratios, 95% CIs, or P values. The median survival timeand the proportion who survived 10 years among 132patients aged 20 to 49 years without any of the previousindependent risk factors were 139 months (95% CI, 101to 177) and 60%, respectively; the median survival time
0 12 24 36 48 60 72 84 96 108 120
' Resection
= n=77
= Biopsy
-- n=20
Observation Time (months)
a(I)
-5
E0
ULV · · · · · · ·
3136
...
.. . . . . .. . . . . . .. . . . . .
,..,...... ~ ~ ~ ~ ~ ~ ~ .....
........... -

SURVIVAL FACTORS IN LOW-GRADE GLIOMA
Fig 10. Survival in 353 pa-tients with histologic intracraniallow-grade glioma according tointra-arterial chemotherapy. Pa-tients who received intraarterialBCNU chemotherapy were com-pared with patients who didnot receive any chemotherapy.There was no statistical differ-ence in survival (Kaplan-Meier,log-rank).
3U)ci)
E0
12 24 36 48
=Intraarterial BCNU
+ n=153
= No chemotherapy
+ n=200
Observat
and 10-year survival rate in 33 patients with two or morerisk factors were 41 months (95% CI, 22 to 60) and 16%.
DISCUSSION
Age at diagnosis in adult patients with low-grade glio-mas shows an incidence maximum in the fourth decadeof life in a population-based report from Norway33 andin larger series from single institutions." 2 The observedage distribution in our low-grade glioma patient popula-tion recruited from a defined geographic region indicatesthat the patients are representative for the disease. A nota-ble exception is that few children and young patients andfew children with juvenile or pilocytic astrocytomas areincluded. Our treatment policy usually did not includeradiotherapy in children operated for low-grade gliomas,who generally have an excellent prognosis after surgicaltreatment. 1-3' 6.7 A few adult patients in WHO performancegroups 3 to 4 may not have been referred for radiotherapy.All other low-grade patients in our region received radio-therapy at the hospital, so selection of patients by thereferral pattern was minimal.
We further confirm the good prognosis for patientsyounger than 20 years of age found by other investiga-tors, -3
,6,7 as well as the successively worse prognosis that
can be expected in older age groups. '9" The profoundeffect of age on prognosis renders any median survivalcalculated for low-grade glioma patients meaningless iftheir age at diagnosis is not clearly stated. The mediansurvival time for our patients in age group 20 to 49 yearswas 9 years, which is comparable to other recent re-ports.10,13,14
We did not observe any plateau in survival during thefirst 15 years following diagnosis. This finding contraststo previous reports on patient materials that included a
ion Time (months)
larger proportion of children,1 3' 5' 6 which tends to showa plateau in survival curves after 3 to 5 years of observa-tion,1.'3 L5 1'6 probably largely due to the excellent progno-sis -3 '67 of the many included children. Survival curves instudies that report adult patients show no plateau phase,9 '"although the median survival time was considerablyshorter9 than in our report. Although prognosis may ap-pear favorable compared with high-grade brain tumors,most patients will ultimately die of their low-grade gli-oma.
The present histologic subdivision of low-grade glio-mas into astrocytoma, oligodendroglioma, and mixed gli-oma has been generally accepted.26 Our retrospectivestudy indicates that if tumor morphology fits the histo-logic criteria of a low-grade glioma, further subdivisionmay not much increase the prognostic value of the histo-logic diagnosis.
Performance status,' 9" focal neurologic deficits,' "1.34mental changes,'"134 seizures,19' 1234 35 symptoms ofexpansion, '4 "1 and contrast enhancement on CT'0 " ' 3' 36
have all been reported as possible prognostic factors ingliomas. Most investigators agree that age, performancestatus, mental changes, and seizures are of prognosticvalue, while the implications of TNM category, con-trast enhancements,' 1 '13 36 macroscopic radical sur-gery,1,9,13,17 37 and radiotherapy, as well as radiotherapydose, '-35 '10 '12 '17 3 839 are still debated.
Performance status remained an important prognosticfactor in our study, although the difference between theprognostic impact of WHO performance grade 0 com-pared with grade 1 was marginal. However, a highly sig-nificant difference in survival and hazards ratio for mor-tality was observed between performance scales 0 to 1compared with scales 2 to 3.
3137

LOTE ET AL
Focal neurologic deficits may affect performance anddid have a significant univariate negative impact on sur-vival in affected patients. For unknown reasons, malesseemed to be at an increased risk for affection of vision.
Headache, nausea, and emesis are symptoms usuallyassociated with large expansive intracranial lesions, andtherefore these symptoms are readily understandable asa negative prognostic factor in low-grade gliomas. In ourstudy, initial symptoms of expansion did not qualify asa statistically significant negative prognostic factor in af-fected patients. However, in patients who needed initialcorticosteroid treatment to alleviate these symptoms, suchcorticosteroid dependency was a significant negativeprognostic factor in univariate and multivariate analysis.Considering the large number of hypotheses statisticallytested, we admit that the associated multivariate P valueof .037 is by no means as convincing as the remainingP values of Table 3, all less than .001. The latter smallP values would remain clearly significant following, eg,Bonferroni corrections that account for multiple tests.
Like other investigators,'" we found that the presenceof mental changes in low-grade glioma patients was astrong independent negative prognostic factor for sur-vival, with a hazards ratio of approximately 2.
In some contrast to the results reported by Karim eta139 in their large prospective study, tumor category ac-cording to the Intemation Union Against Cancer (UICC)TNM classification 28 was, in our experience, a prognosticfactor limited to univariate significance only. Karim eta139 discerned between Tla (tumor diameter < 3 cm) andTlb (diameter 3 to 5 cm), and prognosis in the two T1subgroups differed considerably. We adhered to the origi-nal T1 definition (tumor diameter < 5 cm). 28 A prospec-tive investigation, even a large multicenter study of 6years accrual duration, may allow for more precise collec-tion of radiologic data, possibly making tumor categoryassessment in the study by Karim et al39 more exact thanour own retrospective tumor category classification. Onthe other hand, the median survival time in their heavilyselected patients was only 6 years,39 compared with morethan 8 years in our largely unselected regional patients;so, subtle differences in our respective patient populationsmay have differently influenced tumor category assess-ments and the relative weight of tumor subtype as a prog-nostic factor in the two studies.
Tumor contrast enhancement on initial CT was a sig-nificant univariate, as well as multivariate, negative prog-nostic factor for survival, with approximately a doubledhazards ratio in affected patients. A report from 1981based on few patients concluded that tumor contrast en-hancement was of no prognostic value in low-grade gli-
oma,36 while two later reports based on much larger seriesfound enhancement to be of negative prognostic im-pact.11'1 3 A recent large study again found tumor enhance-ment of no significant prognostic value.' ° In the presentstudy, initial pretreatment tumor contrast enhancement onCT definitely was a strong negative prognostic factor inlow-grade glioma patients.
Our data confirm the textbook adage that calcificationin a brain tumor is a radiologic marker that favors adiagnosis of oligodendroglioma. Calcification was alsoseen in a third of patients with mixed low-grade gliomas,but was otherwise of no prognostic significance.
The presence of seizures has long been recognized asa possible positive prognostic factor in brain tu-mors.1,'9 1235 40 Eighty-five percent of our low-grade gliomapatients experienced seizures. A glance at the Kaplan-Meier survival graph might suggest that the death rate ofunaffected patients was slightly increased during the first2 to 3 years following diagnosis, although the differencedid not reach univariate statistical significance. Thus, wecould not confirm that the presence of seizures is a posi-tive prognostic factor in low-grade gliomas diagnosed andtreated in the CT era.
The well-recognized inherent tendency of low-gradegliomas to develop gradually anaplasia and increasinglyaggressive biology6 ' 9'41 was confirmed by our finding that45% of reoperated patients had progressed from an initiallow-grade glioma to a high-grade glioma at a mediantime of 25 months after the first operation. Since onlyselected patients were reoperated, the true extent of trans-formation in the total patient population may have beenconsiderably higher.
The median duration of the symptomatic period priorto radiologic diagnosis was 6 months in our patients. Theduration of of this prediagnostic period varied consider-ably, but its length did not significantly influence survivalfrom diagnosis. Possibly, low-grade gliomas at the timeof diagnosis have reached a potential for growth andanaplastic dedifferentiation that renders median durationof the symptomatic period before diagnosis immaterial tofurther prognosis. Also, the present sensitive neuroradio-logic methods may tend to considerably shorten the lengthof the prediagnostic period compared with patient materi-als accrued before the CT era.5"'3
The efficacy and indications for various treatment mo-dalities in patients with low-grade glioma are de-bated. " ' 2 '7 A number of reports indicate that completesurgical resection is curative in juvenile or pilocytic astro-cytomas in children, -3 '4 2 and may also render adult pa-tients with low-grade gliomas tumor-free, or at least se-cure longer survival than for nonresectable patients. 1'9"1617
3138

SURVIVAL FACTORS IN LOW-GRADE GLIOMA
In our patients, a macroscopically complete resection wasperformed whenever possible. However, compared withbiopsy followed by radiotherapy, tumor volume reductionby resection followed by radiotherapy was not associatedwith increased duration of survival in our low-grade gli-oma patients, except in the subgroup of patients whopresented with symptoms of increased intracranial pres-sure. Debulking surgery was associated with prolongedsurvival in this subset of patients. Few patients who un-derwent initially biopsy were resected at relapse, so ourdata indicate that initial tumor resection does not prolongsurvival in low-grade glioma patients who do not showclear symptoms of expansion, provided the patients havereceived postoperative radiotherapy. A possible explana-tion is that the effect of radiotherapy was so great that anyeffect of tumor resection was overshadowed. However, adistinct plateau phase following radiotherapy might thenbe expected to appear on survival curves, and that wasnot the case. An equally plausible interpretation is thateither treatment modality may be of marginal survivalbenefit for most patients with adult low-grade gliomas.
Believers and nonbelievers in the efficacy of radiotherapyin patients with low-grade gliomas are awaiting the resultsof ongoing prospective randomized trials.'7'39 Serious lateeffects of radiotherapy may include endocrine dysfunc-tion,2343 intellectual impairment,22 radionecrosis,2 122 or secondtumors.44 Late sequelae in children are especially trou-bling.' 162 224 Retrospective nonrandomized reports indicate asurvival benefit from higher radiation doses,3 '9'37 but no dose-response effect of radiotherapy on survival has been found
in a recent large prospective randomized study.39 Nor couldwe demonstrate a dose-response effect of radiotherapy onsurvival in our retrospective study, although any effect musthave been large to be detectable.
The risk of second tumors following radiation to thebrain probably is approximately 1% to 2% after 10 to 20years.44 Concerns that malignant anaplastic changes maybe induced by radiation in low-grade gliomas are notcorroborated in the present report, in which 45% of reop-erated patients had progressed to high-grade gliomas ata median interval of 25 months after radiotherapy, a shortinduction period for a putative radiation-induced cancer.44
Nor did we observe any increased death rate after 10 to15 years of observation, which might conceivably ariseif a substantial number of patients developed more ag-gressive tumors as a late effect of radiotherapy.
Chemotherapy may induce tumor responses in patientswith low-grade gliomas,6 '2 5'3 1 although no clear survivalbenefits from chemotherapy have been demonstrated. ThePCV regimen3 2 nor intraarterial BCNU chemotherapy 3 'did not have any discernible impact on survival in ouradult low-grade glioma patients after correction for selec-tion criterias.
We conclude that in low-grade glioma patients whohave received postoperative radiotherapy, prognosisseems largely predetermined by the inherent tumor biol-ogy and age at diagnosis. Age, tumor contrast enhance-ment, mental changes, reduced performance status, andinitial corticosteroid dependency are important indepen-dent negative prognostic factors in these patients.
REFERENCES
1. Laws ER, Taylor WF, Clifton MB, et al: Neurosurgical man-agement of low-grade astrocytoma of the cerebral hemispheres. JNeurosurg 61:665-673, 1984
2. Westergaard L, Gjerris F, Klinken L: Prognostic parameters inbenign astrocytomas. Acta Neurochir (Wien) 123:1-7, 1993
3. Shaw EG, Daumas-Duport C, Scheithauer BW, et al: Radiationtherapy in the management of low-grade supratentorial astrocytomas.J Neurosurg 70:853-861, 1989
4. Shaw EG, Scheithauer BW, O'Fallon JR, et al: Oligodendrogli-omas: The Mayo Clinic experience. J Neurosurg 76:428-434, 1992
5. Celli P, Nofrone I, Palma L, et al: Cerebral oligodendroglioma:Prognostic factors and life history. Neurosurgery 35:1018-1035, 1994
6. Macdonald DR: Low-grade gliomas, mixed gliomas, and oligo-dendrogliomas. Semin Oncol 21:236-248, 1994
7. Pollack IF, Claassen D, al-Shboul Q, et al: Low-grade gliomasof the cerebral hemispheres in children: An analysis of 71 cases. JNeurosurg 82:536-547, 1995
8. Lindegaard KF, M0rk SJ, Eide GE, et al: Statistical analysisof clinicopathological features, radiotherapy, and survival in 170cases of oligodendroglioma. J Neurosurg 67:224-230, 1987
9. Soffietti R, Chio A, Giordana MT, et al: Prognostic factors inwell-differentiated astrocytomas in the adult. Neurosurgery 24:686-692, 1989
10. Philippon JH, Clemenceau SH, Fauchon FH, et al: Supraten-torial low-grade astrocytomas in adults. Neurosurgery 32:554-559,1993
11. Hutton JL, Smith DF, Sandemann D, et al: Development ofprognostic index for primary supratentorial intracerebral tumours. JNeurol Neurosurg Psychiatry 55:271-274, 1992
12. Smith DF, Hutton JL, Sandemann D, et al: The prognosis ofprimary intracerebral tumours presenting with epilepsy: The out-come of medical and surgical management. J Neurol NeurosurgPsychiatry 54:915-920, 1991
13. Piepmeier JM: Observations on the current treatment of low-grade astrocytic tumors of the cerebral hemispheres. J Neurosurg67:177-181, 1987
14. Bahary JP, Villemure JG, Choi S, et al: Low-grade pure andmixed cerebral astrocytomas treated in the CT scan era. J Neurooncol27:173-177, 1996
15. Janny P, Cure H, Mohr M, et al: Low grade supratentorialastrocytomas. Cancer 73:1937-1945, 1994
16. North CA, North RB, Epstein JA, et al: Low-grade cerebralastrocytoma. Cancer 66:6-14, 1990
17. Vecht CJ: Effect of age on treatment decisions in low-gradeglioma. J Neurol Neurosurg Psychiatry 56:1259-1264, 1993
18. Daumas-Duport C, Scheithauer B, Kelly P: A histologic and
3139

3140
cytologic method for the spatial definition of gliomas. Mayo ClinProc 62:435-449, 1987
19. Kelly P, Daumas-Duport C, Scheithauer B, et al: Stereotactichistologic correlations of computed tomography- and magnetic reso-nance imaging-defined abnormalities in patients with glial neo-plasms. Mayo Clin Proc 62:450-459, 1987
20. Roselli R, lacoangeli M, Scerrati M, et al: Natural history ofneuroepithelial tumours: contribution of stereotactic biopsy. ActaNeurochir 46:79-81, 1989 (suppl)
21. Emami B, Lyman J, Brown A, et al: Tolerance of normaltissue to therapeutic radiation. Int J Radiat Oncol Biol Phys 21:109-122, 1991
22. Schultheiss TE, Kun LE, Ang KK, et al: Radiation responseof the central nervous system. Int J Radiat Oncol Biol Phys 31:1093-1112, 1995
23. Sklar CA, Constine LS: Chronic neuroendocrinological se-quelae of radiation therapy. Int J Radiat Oncol Biol Phys 31:1113-1121, 1995
24. Syndikus I, Tait D, Ashley S, et al: Long-term follow-up ofyoung children with brain tumors after irradiation. Int J Radiat OncolBiol Phys 30:781-787, 1994
25. Watne K, Hannisdal E, Nome O, et al: Combined intra-arterialand systemic chemotherapy for recurrent malignant brain tumors.Neurosurgery 30:223-227, 1992
26. WHO: International Classification of Tumours No. 21. Histo-logical Typing of Tumours of the Central Nervous System. Geneva,Switzerland, World Health Organization, 1979
27. WHO Handbook for Reporting Results of Cancer Treatment.WHO offset publication no. 48. Geneva, Switzerland, World HealthOrganization, 1979
28. Hermanek P, Sobin LH (eds): UICC: TNM Classification ofMalignant Tumours (ed 4). Berlin, Germany, Springer Verlag, 1987
29. SPSS Advanced Statistics 6.1. Chicago, IL, SPSS Inc, 199430. Collett: Modelling Survival in Medical Research. New York,
NY, Chapmann & Hall, 199431. Watne K, Hannisdal E, Nome O, et al: Combined mintra-arterial
chemotherapy followed by radiation in astrocytomas. J Neurooncol14:73-80, 1992
LOTE ET AL
32. Levin VA, Silver P, Hannigan J, et al: Superiority of post-radiotherapy adjuvant chemotherapy with CCNU, procarbazine, andvincristine (PCV) over BCNU for anaplastic gliomas: NCOG 6G61final report. Int J Radiat Oncol Biol Phys 18:321-324, 1990
33. Helseth A, M0rk S: Neoplasms of the central nervous systemin Norway. III. Epidemiological characteristics of intracranial glio-mas according to histology. APMIS 97:547-555, 1989
34. Walker MD, Green SB. Byar DP, et al: Randomized compari-sons of radiotherapy and nitrosureas for the treatment of malignantglioma after surgery. N Engl J Med 303:1323-1329, 1980
35. Scott GM, Gibberd FB: Epilepsy and other factors in theprognosis of glioma. Acta Neurol Scand 61:227-239, 1980
36. Silverman C, Marks JE: Prognostic significance of contrastenhancement in low grade astrocytomas of the adult cerebrum. Radi-ology 139:211-213, 1981
37. Medbery CA, Straus KL, Steinberg SM, et al: Low-gradeastrocytomas: Treatment results and prognostic variables. Int J Rad-iat Oncol Biol Phys 15:837-841, 1988
38. Recht LD, Bernstein M: Low-grade gliomas. Neurol Clin13:847-859, 1995
39. Karim ABMF, Maat B, Hatlevoll R, et al: A randomized trialon dose-response in radiation therapy of low-grade cerebral glioma:European Organization for Research and Treatment of Cancer(EORTC) study 22844. Int J Radiat Oncology Biol Phys 36:549-556, 1996
40. Lund M: Epilepsy in association with intracranial tumour.Acta Psych Neurol Scand 81:3-149, 1952 (suppl)
41. Morantz RA: Radiation therapy in the treatment of cerebralastrocytoma. Neurosurgery 20:975-982, 1987
42. Clark GB, Henry JM, McKeever PE: Cerebral pilocytic astro-cytoma. Cancer 56:1128-1133, 1985
43. Constine LS, Woolf PD, Cann D, et al: Hypothalamic-pitu-itary dysfunction after radiation for brain tumors. N Engl J Med328:87-94, 1993
44. Brada M, Ford D, Ashley S, et al: Risk of second brain tumourafter conservative surgery and radiotherapy for pituitary adenoma.Br Med J 304:1343-1346, 1992