Study Guide for the RN NCLEX-RN EXAM 12 Sensory System
-
Upload
delindaevans -
Category
Documents
-
view
53 -
download
1
description
Transcript of Study Guide for the RN NCLEX-RN EXAM 12 Sensory System
-
LSensorySystem
213
CHAPTER TWELVE
PHYSIOLOGY OF THE EYE
A. Eyeballs.1. External layer.
a. Sclera: tough, protective covering of the outside of the eye; the white of the eye.
b. Cornea: transparent tissue that covers the front of the eyeball over the pupil.
c. Conjunctiva: the thin, transparent mucous mem-brane that covers the outer surface of the eyeball and lines the inner surface of the eyelid.
2. Middle layer.a. Choroid: pigmented layer containing large number
of blood vessels that nourish the retina.b. Ciliary muscle: muscular body that allows the eye
to focus through contraction and relaxation.c. Ciliary body: produces aqueous humor.d. Iris: controls the size of the pupil in order to regu-
late the amount of light that enters the eye; gives the eye its characteristic color.
e. Pupil: the opening in the center of the iris; the size of the pupil determines the amount of light that enters the eye.
3. Inner layer.a. Retina: thin innermost lining (or the inside back
wall) of the eyeball; contains millions of light-sensitive nerve cells to coordinate and transmit signals via the optic nerve to the brain; similar to film in a camera.
b. Macula: the part of the retina responsible for pro-viding optimum visual focusing.
c. Aqueous humor: fluid that fills anterior and pos-terior chambers; circulates through the pupil and empties into canal of Schlemm.
d. Trabecula: mesh network through which the aqueous humor fluid drains into the canal of Schlemm.
e. Vitreous humor: fluid that fills the cavity posterior to the lens.
f. Crystalline lens: provides for the convergence and refraction of light rays and images onto the retina; enables vision to be focused.
g. Optic nerve: leaves the eyeball through the retina at the location of the optic disc.
h. Choroid: blood supply to the retina.B. Eyelids: protective coverings of the eye.
1. Conjunctiva: inner lining of the eyelid.2. Lacrimal gland: excretes lacrimal fluid (tears) to
lubricate, clean, and protect the outer surface of the eye.
SystemAssessmentA. External assessment.
1. Assess position and alignment of the eyes: both eyes should fixate on one visual field simultane-ously.
2. Evaluate for presence of ptosis.3. Inspect lids and conjunctiva for discharge or
inflammation.4. Assess color of sclera: normally, a thin white coating;
may yellow with age.5. Evaluate size and equality of pupils: should be equal
in size and shape.6. Evaluate pupillary reaction to light.
a. Direct light reflex: constriction of pupil when stimulated with light.
b. Consensual reflex: constriction of opposite pupil when stimulated with light.
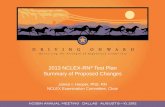
7. Extraocular muscle function: hold finger or object about 12 inches in front of the eye and ask the client to follow the object with only the movement of the eyes; assists to evaluate for paralysis or weakness in extraocular muscle and cranial nerve function (Figure 12-1).
B. Evaluate visual acuity and check for refractive errors (see Appendix 12-1).1. Myopia (nearsightedness): vision for near objects is
better than vision for distant objects.2. Hyperopia (farsightedness): vision for distant objects
is better than vision for near objects.3. Determine any problems with double vision.
C. Assess for presence of pain and any recent change in vision.
-
LHHHHH5HHHHH10HHHHH15HHHHH20HHHHH25HHHHH30HHHHH35HHHHH40HHHHH45HHHHH50HHHHH55H56H57H58
214 CHAPTER 12 Sensory System
DISORDERS OF THE EYE
GlaucomaGlaucoma is a group of disorders characterized by an increase in intraocular pressure and progressive loss of peripheral vision. It is a chronic condition and a leading cause of blindness.
TypesA. Primary open-angle glaucoma (POAG chronic glau-
coma): most common form. Flow of aqueous humor is slowed or stopped by obstruction, thus increasing intra-ocular pressure; characterized by a slow onset; chronic and progressive.
B. Primary angle-closure glaucoma (PACGacute glau-coma): caused by rapid increase in intraocular pressure. Iris is pushed against drainage system, blocking flow of aqueous humor. Immediate treatment is required.
C. Secondary glaucoma: caused by trauma or optic neoplasm.
AssessmentA. Risk factors.
1. Familial tendency.2. Agingoccurs most often in clients more than
40 years old.3. Chronic diseases and eye injury.
B. Diagnostics: intraocular pressure is above 22 mm Hg (see Appendix 12-1).
C. Clinical manifestations of chronic primary open-angle glaucoma (POAG)develops slowly and frequently without symptoms.1. Gradual loss of peripheral vision (i.e., tunnel vision).2. Vague headache around lights.3. Blindness may eventually occur if untreated.
4. Central vision is normal, even with loss of peripheral vision.
D. Clinical manifestations of acute primary angle-closure glaucoma (PACG).1. Medical emergency requiring immediate treatment.2. Decreased central vision.3. Severe eye and brow pain, blurred vision.4. Headache.
TreatmentA. Medications (see Appendix 12-2).
1. Topical (ophthalmic) beta blockers, carbonic anhy-drase inhibitors, cholinergics (miotics), and prosta-glandins may be used alone or in combination.
2. Oral glycerin preparations promote diuresis and lower intraocular pressure.
B. Surgical intervention: most often done on outpatient basis with topical anesthetic.1. Argon laser trabeculoplasty: microscopic laser burns
applied to the trabecula open the fluid channels facili-tating outflow of aqueous humor.
2. Trabeculectomy: creation of an artificial drain to bypass the trabecular meshwork, allowing aqueous humor to flow.
Nursing InterventionsGoal: To prevent progression of visual impairment.A. Teaching plan.
1. Explanation of the problem of increased intraocular pressure.
2. Visual damage cannot be corrected, but further damage can be prevented.
3. Correct use of prescribed medications; client must continue to take medication in order to control disease; otherwise, visual problem will progress.
4. Importance of continued follow-up medical care.5. Advise all health care providers of glaucoma condi-
tion; numerous medications affect intraocular pres-sure; wear medical alert identification.
Goal: To decrease intraocular pressure.
ALERT Assist client to cope with sensory impairment (e.g., hearing, sight, etc.).
FIGURE12-1 Extraocular eye movements. (From: Seidel HM, et al: Mosbys guide to physical examination, ed 6, St. Louis, 2006, Mosby.)
Medialrectus,CN III
Inferioroblique,CN III
Inferioroblique,CN III
Superiorrectus,CN III
Lateralrectus,CN VI
Lateralrectus,CN VI
Superiorrectus,CN III
Superioroblique, CN IV
Superioroblique, CN IV
Inferiorrectus, CN III
Inferiorrectus, CN III
-
LCHAPTER 12 Sensory System 215
A. Avoid straining at stool, lifting, or stooping.B. Administer medications to decrease intraocular
pressure.Goal: To provide appropriate preoperative nursing mea-
sures if surgery is indicated.A. Surgery and treatments are frequently done on an out-
patient basis and with a local anesthetic. Orient the client to the surroundings and sounds that will occur during the procedure.
B. For outpatient surgery, client should wear comfortable clothes and arrange for someone to provide transporta-tion home.
C. Postoperative instructions should be given to the client or family in writing.
Goal: To prevent client from experiencing postoperative complications (surgery frequently done under local anesthesia).
A. Administer medications: miotics, antibiotics, and steroids.
B. Be sure medication is administered in the eye for which it is ordered; the unaffected eye may be treated with a different medication.
C. Client may eat and ambulate as desired after the initial sedative effect is gone.
HomeCareA. Emphasize the importance of follow-up care.B. Teach the client not to rub the eyes.C. Demonstrate the correct administration of eye medica-
tion and have the client return the demonstration.D. Advise the client to avoid activities that increase intra-
ocular pressure.E. Teach the client to report pain that is not relieved by
prescribed analgesics.
CataractA cataract is a complete or partial opacity of the lens that occurs when clumps of protein compromise the sharpness of images on the retina. It may occur at birth (congenital cataract); however, it occurs most commonly in adults past middle age (senile cataracts).
AssessmentA. Risk factors.
1. Diabetes mellitus.2. Corticosteroids: long-term systemic or topical use.3. Age: 70% of adults over age 75 years have cataracts.
B. Clinical manifestations.1. Painless with gradual decrease in visual acuity, blurry
vision.2. Pupil appears gray or yellowish brown to
milky white.3. Red light reflex is distorted on direct ophthalmo-
scopic examination.4. Poor color perception.5. Glare due to light scatter on lens; worse at night.
C. Diagnostics (see Appendix 12-1).
TreatmentSurgical treatment is the only method of correcting cataract; surgery is usually performed when client begins to experi-ence problems in activities of daily living (Box 12-1). If both eyes require surgical correction, each is treated individually, about 4 to 8 weeks apart.A. Phacoemulsification (Phaco): a small incision on the side
of the cornea allowing a tiny probe to be inserted to emit ultrasound, which fragments the lens; cataract is then aspirated.
B. Intraocular lens (IOL) implant to restore visual correction.
Nursing InterventionsGoal: To provide appropriate teaching and nursing care.A. Orient the client to the surroundings and sounds that
will occur during the procedure.
Box 12-1 OLDER ADULT CARE FOCUS
Promoting Independent Activities of Daily Living for the Client With Diminished Vision
Medications When client is taking several medications, use containers
that have different shapes (square, round, triangular). Obtain medication boxes with raised letters or numbers on
them representing the days of the week. Obtain a talking clock that states the time.
Safety Remove throw rugs. Use unbreakable dishes, cups, and glasses. Keep appliance cords short and out of walkways. Avoid footstools in favor of a recliner with a built-in
footrest. Label all cleansers, cleaning fluids, and caustic chemicals
with large, raised lettering. Have hand grips installed in bathrooms. Put nonskid stripping on the surface of the tub floor. Encourage use of an electric razor.
Communication Teach caregivers to always introduce themselves when
entering the clients room and before touching client. Teach the client to use telephones that have programmable
automatic dialing features. Be sure to include emergency phone numbers.
Recognize that much communication is nonverbal; therefore frequent clarification of meaning may be required.
Daily Living Considerations Provide information on Meals on Wheels for delivery of
cooked, ready-to-eat meals. Encourage use of a microwave for cookingit is safer than
using a standard stove. Encourage the use of large-print books, newspapers, and
magazines for reading. Also, many publications are available as audiotapes and CDs at local libraries and vision aid services.
Avoid rearranging furniture and other belongings.
-
LHHHHH5HHHHH10HHHHH15HHHHH20HHHHH25HHHHH30HHHHH35HHHHH40HHHHH45HHHHH50HHHHH55H56H57H58
216 CHAPTER 12 Sensory System
B. For outpatient surgery, client should wear comfortable clothes and arrange for someone to provide transporta-tion home.
C. Before surgery, the nurse will instill mydriatic eye drops; frequently, cycloplegic drops are also used; client will be photosensitive.
D. Normal for visual acuity to be decreased immediately after surgery.
HomeCare(see Box 12-1)A. Maintain clients orientation to surroundings.B. Eye patch may be used for about 24 hours or until the
client returns to the physician for a follow-up visit.C. Client should avoid stooping, lifting, or straining in the
early postoperative period.D. Client should avoid sleeping on the affected side.E. Teach the client to avoid rubbing the eye; there should
be minimal discomfort, and this is generally relieved by acetaminophen; report any pain that is not easily relieved.
F. Teach client how to administer eye drops (antibiotic and steroid eye drops); have client demonstrate procedure.
G. Provide written instructions; make sure the type is large enough for client to read.
RetinalDetachmentA separation of the sensory retina and the underlying epithelium, which allows fluid to collect in the space. Untreated symptomatic retinal detachment almost always results in the loss of vision in the eye.
AssessmentA. Risk factors.
1. Severe myopia (nearsightedness).2. Diabetic retinopathy: sclerosed capillaries of the
retina.3. Trauma.4. Degenerative changes in the retina.5. Previous cataract surgery.
B. Diagnostics (see Appendix 12-1).C. Clinical manifestations.
1. Flashes of light in the visual field.2. Sensation of a curtain or shadow over a portion of the
visual field.3. Painless loss of peripheral or central vision.4. Area of lost vision correlates with location of retinal
detachment.
TreatmentThere is no medical treatment. The surgical repair may be done on an outpatient basis or may require hospitalization.A. Laser photocoagulation: laser light beam to create
inflammation and sealing of the tear or break.B. Cryotherapy: a supercooled probe directed over retinal
tear to produce inflammation to seal the tear.C. Scleral buckling: extraocular surgery in which the sclera
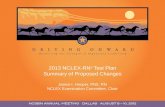
is depressed from the outside with the application of a silicone buckle to weld the retina in contact with the choroid (Figure 12-2).
Nursing InterventionGoal: To enable client and significant others to discuss
problems associated with detachment of the retina, the rationale for surgery, and anticipated preoperative and postoperative activities.
A. Discourage client from jerky head movements, stooping or straining; may have activity restrictions, depending on degree of detachment.
B. Local anesthesia may be used; client may be discharged within hours or may remain in hospitaldepends on the degree of detachment and the type of repair.
Goal: To prevent postoperative complications.A. Orient client to surroundings (see Box 12-1).B. Postoperative pain may require narcotic analgesic.C. Client may experience redness and swelling of the lids.D. Warm or cool compresses may be used to promote
comfort.E. Postoperative medications usually include antibiotic
eye drops, ophthalmic steroid drops, and dilating agents.
Goal: To help client understand and perform own eye care.A. Activities requiring visual acuity may be restricted for
several weeks (reading, driving, etc.).B. Discourage any straining, lifting, or stooping during the
postoperative recovery period.C. Make sure client understands symptoms of detachment
and importance of seeking immediate attention if it occurs again (increased incidence of reoccurrence).
Age-RelatedMacularDegeneration(AMD)Most common cause of central vision loss in clients over 40 years old; related to retinal aging.
FIGURE12-2 Scleral buckling. (From Black JM, Hawks JH: Medical-surgical nursing: clinical management for positive outcomes, ed 8, Phila-delphia, 2009, Saunders.)
Siliconesponge
Retinaltear
Encirclingband
Detached retinaVitreous seepsbehind retina
Anteriorchamber
LensVitreous body
-
LCHAPTER 12 Sensory System 217
AssessmentA. Risk factors.
1. Familial tendency: gene has been identified.2. Long-term exposure to UV lights and eye irritants.
B. Clinical manifestations.1. Blurred, darkened vision.2. Presence of scotomas (blind spots in visual field).3. Distortion of vision.4. Permanent loss of central vision.5. Wet exudativemore severe form.
a. Development of abnormal vessels in or near macula.
b. New vessels begin to leak and form scar tissue.c. Rapid onset.
6. Dry nonexudativeless severe form.a. More common form.b. Accumulation of yellow pigment in retinal
epithelium.c. Atrophy and degeneration of macular cells.
C. Diagnostics (see Appendix 12-1).
TreatmentDirected toward stopping progression; affected vision cannot be restored.A. Laser treatment of abnormal vessels, macular photoco-
agulation of abnormal vessels.B. Medications to inhibit growth of endothelial tissue and
vessels.
Nursing InterventionsGoal: To promote prevention and/or early identification
of problem and care of client with decreased visual acuity.
A. Encourage regular visual checkups.B. Encourage diet high in leafy green vegetables and vita-
mins A and E, beta carotene, and zinc.C. Promote independence in clients with decreased vision
(see Box 12-1).
VisualImpairmentinChildrenA. Refractory problems: same as those of an adult (see
Appendix 12-1).B. Amblyopia: reduced visual acuity in one eye; preventable
if primary problem is corrected before age of 6 years.C. Strabismus (misalignment of eyes) may result if amblyo-
pia is not corrected.D. Conjunctivitis: an inflammation of the conjunctiva.
1. Characterized by redness, tearing, and exudate.2. Warm, moist compresses to remove crust and
exudates.3. Always clean eye from inner canthus downward and
outward to prevent contamination of other eye.4. May be viral, bacterial, or allergic.5. Treatment with antibiotic eye drops; instill after eye
has been cleaned.6. Highly contagious; spreads easily from one eye
to other.7. Encourage good handwashing.
E. Retinopathy of prematurity: originally known as retro-lental fibroplasia; results in vasoconstriction of retina vessels causing retinal damage.
Nursing InterventionsA. Promote discovery of the problem as early as
possible.1. Identify children at increased risk because of history
(prematurity).2. Assess children for behaviors that indicate poor
vision.3. Encourage screening for visual acuity (schools,
clinics).B. Educate parents regarding importance of therapy and
continued medical follow-up.
EyeTraumaEye trauma may include surface injuries (e.g., burns or splash injuries), imbedded or impaled objects, or orbital trauma. History is usually congruent with eye injury.A. Assessment and treatment are often carried out at the
same time.B. As soon as the eye injury is detected, the client should
be seen by a physician (ophthalmologist).
AssessmentA. Identify eye in which trauma occurred.B. Determine whether client has a contact lens in the
affected eye.C. Pain, inability to open the eye.D. Decreased visual acuity: may be unable to distinguish
light and images.E. Ecchymosis, swelling.
TreatmentA. If there is visible trauma, but no penetrating object,
gently apply dressing soaked with normal saline solution to prevent drying during transport.
B. Any suspected or known corneal abrasion should be examined with fluorescein, followed by ocular irrigation with normal saline solution (see Appendix 12-2, and 12-3).
C. Nonpenetrating foreign objects may be removed by irri-gation with normal saline solution.
D. Penetrating foreign bodies must be removed by a physi-cian (ophthalmologist) as soon as possible. Do not attempt to remove foreign objects from eye, but protect from movement while seeking emergency care.
E. Do not attempt to stop bleeding from the eye or the eyelid with direct pressure, do not patch the eye until type of injury is determined.
F. For chemical eye burns, before going to emergency department, irrigate the eye with copious amounts warm tap water to remove chemical. Normal saline irri-gation in ED; may require short-acting ophthalmic anesthetic drops.
-
LHHHHH5HHHHH10HHHHH15HHHHH20HHHHH25HHHHH30HHHHH35HHHHH40HHHHH45HHHHH50HHHHH55H56H57H58
218 CHAPTER 12 Sensory System
Nursing InterventionsGoal: To prevent further eye damage.A. Have client rest the eyes: provide dimly lit room; use
eye patches if necessary.B. Irrigate eyes with normal saline solution from inner
canthus to outer canthus so solution does not flow into unaffected eye.
C. Eye may remain irritated after foreign body is removed; eye patch may be necessary.
D. If penetrating eye injury is present, decrease activities that cause increased ocular pressure.
E. Keep client immobilized until evaluated by an ophthalmologist.
Goal: To care for a client with an enucleation.A. Immediate: obtain vital signs; monitor for bleeding.B. Instillation of topical ointments until prosthesis is
fitted.C. A clear conformer may be placed in the eye socket to
allow the area to heal so a permanent prosthesis can be fitted.
D. Eye prosthesis.1. Insertion: notched end of prosthesis should be closest
to the clients nose; lift upper eyelid (using nondomi-nant hand) and insert saline solution-rinsed prosthe-sis into socket area with top edge slipping under upper lid; gently retract lower lid until bottom edge of prosthesis slips behind it.
2. Removal: retract the lower lid and apply slight pres-sure just below the eye, this should release the suction holding the eye in place; assess the socket for signs of infection.
3. The prosthesis is usually cleansed with normal saline.
PHYSIOLOGY OF THE EARA. External ear.
1. External auditory canal: function is to transmit the collected sound waves to the tympanic membrane; outer half of canal secretes cerumen, or wax, which has a protective function.
2. Tympanic membrane: a tough membrane separating the external and middle ear; transmits vibrations from external ear to the malleus of the middle ear; normally a pearly gray color.
B. Middle ear.1. Middle ear is filled with air at atmospheric pressure
by means of the eustachian tubes; the eustachian tubes of infants and young children are shorter and wider than those of adults.
2. The external and middle ear function is to transmit and magnify sound waves by air conduction.
3. Problems in the external and middle ear cause con-ductive hearing loss.
C. Inner ear.1. Bony labyrinth.
a. Vestibule: central area contains oval window and is bathed in fluid.
b. Semicircular canals: open into the vestibule; related to maintaining equilibrium.
c. Cochlea: contains organ of Corti, which is the receptive end organ for hearing.
2. Disease of the inner ear or nerve pathway can result in sensorineural hearing loss.
SystemAssessmentA. External assessment of the ear.
1. Assess placement of the ears: low-set ears may be indicative of congenital anomalies in the newborn.
2. Movement of the auricle should not elicit pain.3. Note presence of any discharge in the external
canal.4. With an otoscope, examine tympanic membrane for
landmarks, color, and intactness.5. Note color and consistency of cerumen.
B. Assessment of bone and air conduction (see Appendix 12-1).
C. Assess for vertigo: ask client to close eyes and stand on one foot; have client walk with eyes closed; client may fall to one side or complain of the room spinning.
DISORDERS OF THE EAR
OtitisMediaOtitis media is an infection of the middle ear caused by a viral or bacterial agent. Infants and young children are predisposed to the development of acute otitis media because of the physiologic characteristics of the earthe eustachian tube is shorter, wider, and straighter in chil-dren than in adults.
AssessmentA. Acute otitis media (AOM).
1. May be purulent (pus-filled) or suppurative (capable of producing pus).
2. Symptoms vary with the severity of the infection.3. Increased incidence in bottle-fed babies.
B. Repeated or persistent acute infections lead to perfora-tion of the tympanic membrane or more severe compli-cations such as mastoiditis.
C. Otitis media with effusion (OME): a collection of fluid in the middle ear without infection or acute symptoms that results from a blocked eustachian tube; may persist for weeks to months; most common cause of conductive hearing loss.
D. Risk factors.1. Age: increased incidence from 6 months to 20
months; decreases with age.2. Upper respiratory tract infection.3. Allergies, asthma.4. Increased incidence in infants who are exposed to
passive cigarette smoke.E. Clinical manifestations (Figure 12-3).
1. Otalgia (pain from pressure in the middle ear).a. Infants are irritable; may pull at their ears; sucking
exacerbates pain.
-
LCHAPTER 12 Sensory System 219
b. Young children verbally complain of severe ear pain.
2. Fever as high as 104 F is not uncommon with AOM.
3. Otoscopic examination.a. AOMtympanic membrane is immobile, bright
red, and bulging, with no light reflex and purulent effusion.
b. OMEimmobile and discolored tympanic membrane.
4. Postauricular and cervical lymph node enlargement.5. If tympanic membrane ruptures, purulent drainage or
blood may be present in the outer ear; pain will decrease temporarily (AOM and OME).
6. Conductive hearing loss may occur with recurrent rupture.
7. Speech and language development may be delayed.
TreatmentA. Medications.
Nursing Interventions
Goal: To enable parents of clients to describe problem, handle medication schedule, and cope with home care.
A. Recurrent infections cause an increased risk for perma-nent hearing loss or mastoiditis with potential intracra-nial spread of infection.
B. Antibiotics should be continued until all prescribed medication is taken, even after all symptoms are relieved.
C. Administer acetaminophen or ibuprofen for pain and fever. There should be relief of symptoms within 24 to 72 hours; if not, the health care provider should be contacted.
D. Pain-relieving ear drops (Auralgan, Pramotic) should be used only when there is no tympanostomy tube or rupture of the tympanic membrane.
NURSINGPRIORITY Teach the parents to administer the full course of the antibiotic.
1. Antibiotics, analgesics, antipyretics.2. Ear drops (antibiotic and steroid combination).3. Decongestants and antihistamines.4. Corticosteroids for eustachian tube edema as needed.5. OME does not require antibiotic therapy.
B. Surgicalmyringotomy: drainage of the middle ear with insertion of tubes or grommets (or tympanostomy myr-ingotomy) to relieve pressure and promote healing; used for recurrent cases that do not respond to medication; tubes also known as pressure equalizing tubes (PE tubes).
NURSINGPRIORITY Aspirin should not be used for fever or pain in children 18 years or younger.
E. Control allergies and upper respiratory congestion.F. The child should be discouraged from forcefully blowing
his or her nose or holding his or her nose closed when sneezing.
G. Decrease risk for recurrence by preventing fluids from pooling around eustachian tube.1. Hold or elevate infants head while feeding.2. Do not prop bottle or allow infant to fall asleep with
a bottle.3. Encourage intake of water before sleeping.
H. Encourage application of a drying agent (e.g., Swim-EAR) after swimming, showering, or bathing to dry external ear canal and/or use of earplugs when child goes swimming.
Goal: Care for child after placement of tympanostomy tubes (myringotomy tubes or grommets).
A. Do not allow soapy or dirty water to get into the childs ears; use of earplugs is currently controversial.
B. Assure parents that if the ear grommet or tube falls out, it is not a significant problem.
AcousticNeuromaA benign tumor of cranial nerve VIII, vestibulocochlear.
AssessmentA. Clinical manifestations.
1. Sensorineural hearing loss.2. Tinnitus.3. Intermittent vertigo.4. Impairment of facial movement (CN VII, V).
B. Diagnostics (see Appendix 12-1 and Appendix 20-1).C. Treatmentsurgical removal of tumor.
Nursing InterventionsGoal: Promote communication and prepare client for
surgery.A. Assist hearing-impaired client with communication
(Box 12-2).
FIGURE12-3 Otitis media. (From Zerwekh J, Claborn J: Memory note-book of nursing, vol 2, ed 3, Ingram, Texas, 2007, Nursing Education Consultants.)
-
LHHHHH5HHHHH10HHHHH15HHHHH20HHHHH25HHHHH30HHHHH35HHHHH40HHHHH45HHHHH50HHHHH55H56H57H58
220 CHAPTER 12 Sensory System
B. Determine presence of vertigo and plan for client safety.C. Preoperative preparation (see Chapter 3).
1. Assess level of hearing loss and communication skills.2. Encourage client to discuss fear regarding loss of
hearing on affected side.3. Establish communication system for postoperative
period.Goal: To provide postoperative craniotomy care (see
Chapter 20).A. Assess for surgical interference with other cranial nerves
(VII, facial; V, trigeminal; IX, glossopharyngeal).1. Assess for equal movement of face: smile, show teeth.2. Evaluate for problem swallowing.3. Evaluate speech.
B. Evaluate balance and hearing loss regarding ADLs and safety.
HearingLossHearing loss results from an impairment of the transmis-sion of sound waves.A. Conductive: results from mechanical dysfunction in
transmission of sound from the outer or middle ear or both. Client will be able to benefit from a hearing aid. Example of conductive hearing loss is impacted cerumen, which often occurs in older adults.
B. Sensorineural (perceptive): results from a problem in the inner ear (cochlea) or auditory nerve pathway.
Often results from injury to cilia that transmit sound. Incoming sound cannot be analyzed correctly. Client may benefit from cochlear implant. Example of sensori-neural hearing loss is presbycusis, which occurs in older adults.
C. Otosclerosis: an immobilization of the small bones in the inner ear; it occurs most often in women; an auto-somal-dominant disease that is usually bilateral.
D. Congenital: rubella or nutritional deficiencies.E. Toxicity from aminoglycosides.F. Occupational.
AssessmentA. Risk factors.
1. Prolonged exposure to high-intensity sound waves.
Box 12-2 OLDER ADULT CARE FOCUS
Improving Communication With Hearing-Impaired Clients
Stand in front of the client at eye level to speak. An adequate light source on your face will help with speech reading (i.e., reading lips).
Get the clients attention by raising your hand or arm. Do not walk back and forth in front of the client while
speaking. Speak clearly and in an even tone; do not shout. Do not chew gum, cover your mouth, or smile excessively
while talking. Because clients rely on visual cues, watch your facial
expressions. Encourage professional counseling in speech reading and
sign language. Assist the client in obtaining a hearing aid; if appropriate,
promote social interaction. Do not avoid conversation with the client; do not depend
on family to interpret information. Investigate use of TDD (telecommunication device for
the deaf ). Use light-activated devices: door bell, smoke alarms,
telephones. Client should avoid noisy environments where it is difficult
to interpret sound. Provide client instruction in a quiet room with minimal
distractions.
NURSINGPRIORITY Earplugs should be worn when the potential for exposure to loud noise exists.
2. Repeated, chronic ear infections.3. Prenatal problems of rubella and eclampsia.4. Ototoxic medications: aminoglycosides, diuretics.5. Female with family history of otosclerosis.
B. Diagnostics (see Appendix 12-1).C. Clinical manifestations.
1. Speech problems: deterioration of present speech or delayed speech development.
2. Fails to respond to oral communication or responds inappropriately.
3. Excessively loud speech.4. General indifference to sound.5. Tinnitus.6. Responds more to facial expressions than to verbal
ones.7. Inappropriate emotional response.
TreatmentA. Speech therapy.B. Sign language.C. Stapedectomy for otosclerotic lesions.D. Cochlear implants for profound sensorineural hearing
loss.
Nursing InterventionsGoal: To promote communication and socialization of the
hearing-impaired client (Box 12-2).A. Teach client how to care for hearing aid (Box 12-3).B. Teach client how to remove ear wax if impacted cerumen
is a problem; may need an ear irrigation (see Appendix 12-3).
Goal: To prevent complications after stapedectomy.A. Assess client for dizziness, nausea, and vomiting.B. Teach client to avoid sudden movement to prevent
dizziness.C. Maintain safety measures.D. Instruct client that hearing may not improve until edema
subsides in the operative area.
-
LCHAPTER 12 Sensory System 221
BalanceDisordersThe vestibular system of the inner ear maintains balance and coordination.A. Disorders.
1. Mnires disease: an inner ear disorder caused by excess endolymph in the vestibular and semicir-cular canals; also known as endolymphatic hydrops.
2. Labyrinthitis: an inflammation of the cochlear and/or vestibular portion of the inner ear.
AssessmentA. Diagnostics (see Appendix 12-1).
1. Results of Weber test and auditory testing may indi-cate hearing loss.
2. Romberg test (see Chapter 20 for Neurologic System Assessment).
Box 12-3 OLDER ADULT CARE FOCUS
Hearing Aid Care
Keep the hearing aid dry; do not wear it while bathing or swimming.
Avoid using hair spray, cosmetics, or oils around the ear. Clean hearing aid with soft cloth and recommended cleanser;
do not immerse in water. At night turn it off and open the battery compartment to
prevent draining the battery. Avoid exposing it to extreme temperatures (e.g., leaving it
on a window ledge in the sunlight). When cleaning the hearing aid, use a toothpick or pipe
cleaner to remove any debris or cerumen from the hole in the middle part of the device that goes in the ear.
If the hearing aid does not work, change the battery or check the on/off switch; check the connection between the ear mold and receiver; clean it using the steps described above, or take it to an authorized hearing aid service center.
B. Clinical manifestations.1. Vertigo: a sense of moving or spinning that is usually
stimulated by sudden movement of the head; may occur when lying down.
2. Sudden, severe paroxysmal episodes of vertigo (Mnires disease).a. Severe nausea, vomiting.b. Nystagmus.c. Loss of balance.d. No pain or loss of consciousness.
3. Fluctuating hearing loss and tinnitus (Mnires disease).
4. Client may have no symptoms between attacks.5. Manifestations become less severe with time.
TreatmentA. Medications (Mnires disease).
1. Atropine may stop an acute attack.2. Sedatives.3. Antihistamines, anticholinergics.4. Diuretics (to decrease endolymph fluid).5. Meclizine hydrochloride (Antivert) for prevention
and treatment of motion sickness symptoms.6. Antiemetics.
B. Diet: low-sodium.
Nursing InterventionsGoal: To provide emotional and physical support during an
acute attack.A. Maintain bed rest in a quiet, dimly lit room; avoid flick-
ering lights and television.B. Position of comfort.C. Avoid unnecessary nursing procedures.D. Minimize stimulation and sudden position changes.E. If client is severely nauseated, administer medications
parenterally.F. Maintain safety: instruct client to always call before
getting out of bed.
ALERT Hearing loss is very common in older adult clients. Watch for questions about hearing loss to be incorporated into test situations pertaining to other chronic health care problems.
NURSINGPRIORITY As a safety precaution, instruct the client to lie down immediately if an attack feels imminent.
-
LHHHHH5HHHHH10HHHHH15HHHHH20HHHHH25HHHHH30HHHHH35HHHHH40HHHHH45HHHHH50HHHHH55H56H57H58
222 CHAPTER 12 Sensory System
Appendix 12-1 OPHTHALMIC AND HEARING DIAGNOSTICS
Ophthalmic DiagnosticsSnellen chart is used in screening for visual acuity problems.
Client is placed 20 feet from the chart, and visual acuity is expressed as a ratio (what the client should see at 20 feet compared with what he or she can see at 20 feet). A ratio of 20/50 means that the client can see at 20 feet what he or she should see at 50 feet.
A noncontact tonometer is an instrument used to measure intraocular pressure noninvasively. Normal pressure is 12 to 22 mm Hg. A puff of air is directed toward the cornea, which causes indentation and allows measurement of intraocular pressure, a screen for diagnosis of glaucoma.
Direct ophthalmoscopy is examination of the fundus or back portion of the interior of the eyeball, which provides for visual evaluation of the retina, vascular patterns, and optic disk.
Biomicroscopy (slit-lamp examination) is used to assess the anterior eye for problems of the cornea, iris, and lens and to evalu-ate the depth of the anterior chamber.
Refractive error evaluation determines what refractive errors have occurred because light is not correctly focused on the retina. Conditions that occur in refractive errors are: Myopia (nearsightedness)sees near objects clearly; light ray
is focused in front of the retina Hyperopia (farsightedness)sees distant objects clearly; light
ray is focused behind the retina
Presbyopiaa decrease in the elasticity of the lens that causes poor accommodation for near vision (common in older adults)
Astigmatisman uneven curvature of the cornea; light rays do not focus on the retina at the same time
Hearing DiagnosticsAudiometry is used to measure a clients hearing by the use of
various tones and intensities of sound produced by an audiometer.The Rinne test is conducted by holding a tuning fork on the
mastoid bone (bone conduction). When the client indicates that he or she no longer hears sound, the vibrating tuning fork is moved to about 2 inches from the external ear (air conduction). The client who hears normally will continue to hear the vibrations. This demonstrates that air conduction will last longer than bone con-duction. When the tone is louder through air, the test result is positive and indicates normal hearing. If the bone conduction is louder than air conduction, it is indicative of a conductive loss.
The Weber test is conducted by placing a vibrating tuning fork on top of the clients head or in the middle of the forehead; the sound should be heard equally well in each ear. The tone is louder in an ear with unilateral conductive loss and quieter in an ear with sensorineural loss.
Otoscopy is the examination of the external ear and the tym-panic membrane by the use of an otoscope.
Appendix 12-2 OPHTHALMIC MEDICATIONS
General Nursing ImplicationsOnly use ophthalmic preparations of medications. To decrease systemic absorption of ophthalmic topical medications, teach client to apply gentle pressure
(punctal occlusion) to the lacrimal duct (tear duct) during and immediately after instillation of drops. Instruct client or family in proper administration of eye drops or ointment, (i.e., maintain sterile
technique and prevent dropper contamination; clearly mark each container to indicate what eye medication is for).
Expect some blurriness from ointments; apply at bedtime, if possible, to avoid safety problems from diminished vision.
Instruct client to report changes in vision, blurring, difficulty breathing, or flushing. Teach client to gently close eye and allow medication to distribute evenly over eyeball.
MEDICATIONS SIDE EFFECTS NURSING IMPLICATIONSGlaucoma Medications Used to reduce production of aqueous humor and increase outflow, thereby decreasing ocular pressure.
Alpha2 Adrenergic AgonistsBrimonidine (Alphagan) Dry mouth, ocular hyperemia, local burning
and stingingSystemic absorption: hypotension
1. Can be absorbed into contact lens, wait 15 minutes after instill drops to replace contacts.
Beta BlockersNonselective Beta1 and Beta2 BlockersTimolol maleate (Timoptic)Carteolol (Ocupress)
Eye irritation, dry eyesBradycardia, AV block, bronchospasm
1. Assess for cardiac and respiratory changes with systemic absorption.
Selective Beta1 BlockersBetaxolol (Betoptic) Bradycardia, AV block 1. Recommended for use in clients with history
of chronic pulmonary disease. Assess for systemic absorption.
-
LMEDICATIONS SIDE EFFECTS NURSING IMPLICATIONSProstaglandin AnalogsLatanoprost (Xalatan)Travoprost (Travatan)Bimatoprost (Lumigan)
Increases pigmentation of eyelid and growth of eyelashes; conjunctiva hyperemia
1. Minimal systemic effects.
AnticholinergicsPilocarpine hydrochloride
(IsoptoCarpine, Pilocar): 0.25% to 10% solutions
Conjunctive irritationProvocation of asthmaHeadache, ciliary spasm
1. Contraindicated in clients with inflammatory eye conditions.
2. Miotic; causes constriction of pupil.
NURSINGPRIORITY Only use ophthalmic preparations of any medication for eye drops.
Cycloplegic and Mydriatics Work by blocking response of sphincter muscle of iris; produce dilation of pupil; may cause paralysis of accommodation. Used in eye examination and diagnosis.
Atropine sulfate (Atropisol): 0.25% to 2% solution
Cyclopentolate HCl (Cyclogyl): 0.5% to 1% solution
Tropicamide (Mydriacyl)
Blurred vision, photophobia, headache, hyperemia; systemic effects: flushing, sweating, dry mouth, dizziness
1. Contraindicated in clients with glaucoma.2. Dark glasses may be worn to decrease
discomfort from photophobia.3. Use only ophthalmic preparations.
Diagnostics Surface of eye absorbs dye, thus demonstrating corneal abrasions in eye trauma.
Fluorescein sodium (Fluorocyte, Fluor-L-Strip)
Stinging, burning sensation 1. Cornea remains uncolored; abrasions and defects turn green.
Antiinfectives Used for treatment of eye infections.
Neomycin-Polymyxin (Neosporin)Erythromycin (Ilotycin)
ophthalmic ointment
Drops and ointment may cause burning or irritation.
1. Vision may be blurred.2. Teach correct application of medication.3. Use only eye preparations of medications.
CNS, Central nervous system; GI, gastrointestinal; IV, intravenously; PO, by mouth (orally).
Appendix 12-2 OPHTHALMIC MEDICATIONScontd
Appendix 12-3 NURSING PROCEDURE: EAR AND EYE IRRIGATION
Ear IrrigationsCommon SolutionsWarm tap water or normal saline solution.
Hydrogen peroxide.
KEYPOINTS: Irrigation Before irrigation, visually inspect the external ear canal with
otoscope to ensure that tympanic membrane is intact and that auditory canal is not obstructed by a foreign body. Do not irrigate an ear with otitis media present.
Temperature of irrigating solution should be near body temperature (37 C, approximately 98 F). If too cold or hot, dizziness and/or nausea may occur.
Cerumen may be softened by adding a few drops of warm mineral oil or OTC preparation.
A rubber bulb syringe or a water pressure device may be used. Straighten the ear canal by either pulling the outer ear up for
adults or down for children under 3 years. Direct water flow toward the top of the ear canal to create a
circular motion. Do not forcefully push fluid into the ear canal, because this
may rupture the eardrum. If severe pain, nausea, vomiting, or dizziness develop, stop the irrigation immediately.
Eye IrrigationsCommon SolutionsNormal saline.
KEYPOINTS: Eye Irrigation Place client in position in which solution does not run into
unaffected eye. Small amount of fluid: use a cotton ball moistened in solution. Moderate amount of fluid: use a plastic squeeze bottle to direct
fluid along conjunctiva and over the eyeball from inner to outer canthus.
Large amount of fluid: bags of intravenous solutions may be used to provide constant stream and adequate flushing of chemical from the eye.
Do not allow tip of irrigating equipment to touch the eye. Immersion technique: place entire face in basin of lukewarm
water and have client open and close eyes repeatedly. Avoid use of contact lenses for a period of time after eye
irritation.
-
LHHHHH5HHHHH10HHHHH15HHHHH20HHHHH25HHHHH30HHHHH35HHHHH40HHHHH45HHHHH50HHHHH55H56H57H58
224 CHAPTER 12 Sensory System
6. The nurse is admitting a postoperative client after removal of an acoustic neuroma. What would be most important to include in the postoperative nursing care for this client?1 Determining when the client will begin chemo-
therapy2 Evaluating hearing status3 Assessing the clients ability to swallow4 Encouraging the client to discuss problems with
hearing loss7. A clients eye has been anesthetized for an ophthalmol-
ogy examination. What instructions will be important for the nurse to give the client?1 Do not watch television for at least 1 day.2 Do not rub the eye for 15 to 20 minutes.3 Irrigate the eye every hour to prevent dryness.4 Wear sunglasses when in direct sunlight for the next
6 hours.8. A child is diagnosed with conjunctivitis. Which state-
ment indicates that the child understood the nurses teaching?1 Its okay for me to let my friends use my sunglasses
while we are playing together.2 Its okay for me to softly rub my eye, as long as I
use the back of my hand.3 I can pick the crusty stuff out of my eyelashes with
my fingers when I wake up in the morning.4 I will use my own washrag and towel while my eyes
are sick.9. An unknown chemical was splashed into a clients eyes.
What is most important for the nurse to tell the client to do immediately?1 Rinse the eye with a large amount of water or saline
solution.2 Put a pad soaked in sterile saline solution over the
eye.3 Go to the closest emergency department.4 Have a co-worker visually check the eye for a foreign
body.10. Which client is at highest risk for retinal detachment?
1 A 4-year-old with amblyopia2 A 17-year-old who plays physical contact sports3 A 33-year-old with severe ptosis and diplopia4 A 72-year-old with nystagmus and Bells palsy
StudyQuestions Sensory System
1. The nurse would question which medication order for a client with acute primary angle-closure glaucoma?1 Atropine (Atropisol) 1 to 2 drops in each eye now2 Hydrochlorothiazide (Diuril) 25 mg PO daily3 Propranolol (Inderal) 20 mg PO two times a day4 Carbamyl choline (Isopto carbachol) eye drops, 1
drop two times a day2. A client who has glaucoma is concerned about her adult
children inheriting the condition. What is the best nursing response?1 There is no need for concern; glaucoma is not a
hereditary disorder.2 Your children should have an ophthalmologic
examination with screening for glaucoma around age 40. After that, examinations should be done every 2 to 3 years.
3 There may be a genetic factor with glaucoma, and your children over 30 years old should be screened yearly.
4 Are your grandchildren complaining of any eye problems? Glaucoma generally skips a generation.
3. The nurse is evaluating a client recently diagnosed with chronic primary open-angle glaucoma (POAG). What will be an important nursing action?1 Review all medications the client is currently taking
to determine whether any of them cause an increase in intraocular pressure as a side effect.
2 Determine whether the client has experienced any sudden loss of vision accompanied by pain.
3 Discuss with the client the importance of controlling blood pressure to decrease the potential loss of peripheral vision.
4 Instruct the client to take analgesics as soon as any discomfort occurs in the eye and to notify clinic if pain is not relieved.
4. A child is scheduled for a myringotomy with placement of tympanostomy tubes. What is the goal of this proce-dure that the nurse will discuss with the parents?1 To decrease infection in the ear2 To irrigate the eustachian tube3 To correct a malformation in the inner ear4 To equalize pressure on the tympanic membrane
5. A client comes to the clinic with decreased hearing. Examination of the ear canal reveals a large amount of cerumen. What is the recommended method for removal of the cerumen?1 Curettage with suction and irrigation2 Normal saline solution irrigation3 D5W irrigation4 Cotton swab applicator
More questions on companion CD!
Answers and rationales to these questions are in the section at the end of the book titled Chapter Study Questions: Answers and Rationales.