SKA barudfd
-
Upload
firman-saputra -
Category
Documents
-
view
234 -
download
0
Transcript of SKA barudfd
-
7/28/2019 SKA barudfd
1/77
TATALAKSANA SINDROM
KORONER AKUTDENGAN ELEVASI SEGMEN ST
Saharman Leman, Rony Y Syarif
Sub-bagian Kardiologi Ilmu Penyakit Dalam
Fakultas Kedokteran Universitas Andalas Padang
-
7/28/2019 SKA barudfd
2/77
Acute CoronarySyndrome
What is Acute Coronary Syndrome ?
How can I look at an EKG and tell whatpart of the heart is affected ?
What do Emergency Room need to know ?
-
7/28/2019 SKA barudfd
3/77
Scope of Problem(2004 stats)
CHD single leading cause ofdeath in United States 452,327 deaths in the U.S. in 2004
1,200,000 new & recurrentcoronary attacks per year
38% of those who with
coronary attack die within a yearof having it
Annual cost > $300 billion
-
7/28/2019 SKA barudfd
4/77
Definitions
Acute coronary syndrome is defined asmyocardial ischemia due to myocardialinfarction (NSTEMI or STEMI) or unstable
angina
Unstable angina is defined as angina at rest, newonset exertional angina (
-
7/28/2019 SKA barudfd
5/77
Who is at risk for ACS?
Conditions that may mimic ACS include:
Musculoskeletal chest pain Pericarditis (can have acute ST changes)
Aortic dissection
Central Nervous System Disease (may mimicMI by causing diffuse ST-T wave changes)
Pancreatitis/Cholecystitis
-
7/28/2019 SKA barudfd
6/77
Expanding Risk Factors
Smoking
Hypertension
Diabetes Mellitus
Dyslipidemia
Low HDL < 40
Elevated LDL / TG
Family Historyevent infirst degree relative >55male/65 female
Age-- > 45 for male/55for female
Chronic Kidney Disease
Lack of regular physicalactivity
Obesity
Lack of Etoh intake
Lack of diet rich in fruit,veggies, fiber
-
7/28/2019 SKA barudfd
7/77
Acute Coronary Syndromes
Similar pathophysiology
Similar presentation andearly management rules
STEMI requires evaluationfor acute reperfusionintervention
Unstable Angina
Non-ST-SegmentElevation MI(NSTEMI)
ST-SegmentElevation MI(STEMI)
-
7/28/2019 SKA barudfd
8/77
Diagnosis of Angina
Typical anginaAll three of the following Substernal chest discomfort
Onset with exertion or emotional stress
Relief with rest or nitroglycerin
Atypical angina 2 of the above criteria
Noncardiac chest pain 1 of the above
-
7/28/2019 SKA barudfd
9/77
Diagnosis of Acute MI
STEMI / NSTEMI
At least 2 of the following
Ischemic symptoms
Diagnostic ECGchanges
Serum cardiac marker
elevations
-
7/28/2019 SKA barudfd
10/77
No ST Elevation ST Elevation
Acute Coronary Syndrome
Unstable Angina NQMI Qw MI
NSTEMI
Myocardial Infarction
Davies MJHeart 83:361, 2000
Ischemic DiscomfortPresentation
Working Dx
ECG
Biochem.
Marker
Final Dx
Hamm Lancet 358:1533,2001
STEMI
-
7/28/2019 SKA barudfd
11/77
The Three Is
Ischemia=ST depression or T-wave inversionRepresents lack of oxygen to myocardial tissue
-
7/28/2019 SKA barudfd
12/77
The Three Is
Injury = ST elevation -- represents prolongedischemia; significant when > 1 mm above the baselineof the segment in two or more leads
-
7/28/2019 SKA barudfd
13/77
The Three Is
Infarct = Q waverepresented by firstnegative deflection after P wave; must bepathological to indicate MI
-
7/28/2019 SKA barudfd
14/77
Unstable
Angina STEMINSTEMI
Non occlusive
thrombus
Non specific
ECG
Normal cardiac
enzymes
Occluding thrombus
sufficient to cause
tissue damage & mild
myocardial necrosis
ST depression +/-
T wave inversion on
ECG
Elevated cardiac
enzymes
Complete thrombus
occlusion
ST elevations on
ECG or new LBBB
Elevated cardiac
enzymes
More severe
symptoms
-
7/28/2019 SKA barudfd
15/77
Acute Management
Initial evaluation &stabilization
Efficient riskstratification
Focused cardiac care
-
7/28/2019 SKA barudfd
16/77
Evaluation
Efficient & direct history Initiate stabilization interventions
Plan for moving rapidly toindicated cardiac care
Directed Therapies
are
Time Sensitive!
Occurs
simultaneously
-
7/28/2019 SKA barudfd
17/77
Chest pain suggestive of ischemia
12 lead ECG Obtain initial
cardiac enzymes
electrolytes, cbclipids, bun/cr,glucose, coags
CXR
Immediate assessment within 10 Minutes
Establishdiagnosis
Read ECG
Identifycomplications
Assess forreperfusion
Initial labsand tests
Emergentcare
History &Physical
IV access Cardiac
monitoring
Oxygen
Aspirin
Nitrates
-
7/28/2019 SKA barudfd
18/77
Focused History
Aid in diagnosis and ruleout other causes
Palliative/Provocativefactors
Quality of discomfort
Radiation
Symptoms associatedwith discomfort
Cardiac risk factors
Past medical history -especially cardiac
Reperfusion questions
Timing of presentation
ECG c/w STEMI
Contraindication tofibrinolysis
Degree of STEMI risk
-
7/28/2019 SKA barudfd
19/77
TargetedPhysical
Recognize factors thatincrease risk
Hypotension
Tachycardia Pulmonary rales, JVD ,
pulmonary edema,
New murmurs/heart sounds
Diminished peripheralpulses
Signs of stroke
ExaminationVitals
Cardiovascular
system Respiratory system
Abdomen
Neurological status
-
7/28/2019 SKA barudfd
20/77
ECG assessment
ST Elevation or new LBBBSTEMI
Non-specific ECG
Unstable Angina
ST Depression or dynamicT wave inversions
NSTEMI
-
7/28/2019 SKA barudfd
21/77
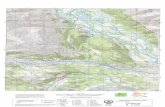
Lokasi infark berdasarkan letak
perubahan gambaran EKG
Anterior : V1-V6Anteroseptal : V1-V4Anterior ekstensif : V1-V6, I-AVLInferior : II, III, AVFLateral : I, AVL, V5-V6
Posterior : V7-V9Ventrikel Kanan : V3R-V4R
-
7/28/2019 SKA barudfd
22/77
Normal or non-diagnostic EKG
-
7/28/2019 SKA barudfd
23/77
ST Depression or Dynamic T wave
Inversions
-
7/28/2019 SKA barudfd
24/77
-
7/28/2019 SKA barudfd
25/77
ST-Segment Elevation MI
-
7/28/2019 SKA barudfd
26/77
New LBBB
QRS > 0.12 sec
L Axis deviation
Prominent R wave V1-V3
Prominent S wave 1, aVL, V5-V6
with t-wave inversion
-
7/28/2019 SKA barudfd
27/77
Cardiac markers
Troponin ( T, I) Very specific and more
sensitive than CK Rises 4-8 hours after
injury May remain elevated for
up to two weeks Can provide prognostic
information
Troponin T may beelevated with renal dz,poly/dermatomyositis
CK-MB isoenzyme
Rises 4-6 hours after injuryand peaks at 24 hours
Remains elevated 36-48
hours Positive if CK/MB > 5%
of total CK and 2 timesnormal
Elevation can be predictive
of mortality False positives with
exercise, trauma, muscle dz,DM, PE
-
7/28/2019 SKA barudfd
28/77
Risk Stratification
UA or NSTEMI- Evaluate for Invasive vs.
conservative treatment
- Directed medical therapy
Based on initial
Evaluation, ECG, and
Cardiac markers
- Assess for reperfusion
- Select & implementreperfusion therapy
- Directed medical therapy
STEMI
Patient?YES NO
-
7/28/2019 SKA barudfd
29/77
Cardiac Care Goals
Decrease amount of myocardial necrosis
Preserve LV function
Prevent major adverse cardiac events
Treat life threatening complications
-
7/28/2019 SKA barudfd
30/77
Tabel . Kelas Rekomendasi
Kelas I Terapi atau prosedur yang telah terbukti secara
klinis atau disepakati secara umum memberikan
manfaat dan efektif
Kelas II
Kelas IIa
Kelas IIb
Bukti klinis yang diperoleh mengenai suatu terapi
atau prosedur masih memiliki kontroversiStudi klinis cenderunglebih banyak menyatakan
suatu terapi atau prosedur memberikan manfaat dan
efektif
Studi klinis menunjukkan suatu terapi atau prosedur
masih diragukanapakah memberikan manfaat danefektif
Kelas III Studi klinis atau kesepakatan umum bahwa suatu
terapi atau prosedur tidak bermanfaat atau tidak
efektif dan bahkan pada beberapa kasus dapat
membahayakan
T l k P R h S ki
-
7/28/2019 SKA barudfd
31/77
1. Bagi orang awam
Mengenali gejala serangan jantung dan segera mengantarkan pasienmencari pertolongan ke rumah sakit atau menelpon rumah sakitterdekat meminta dikirimkan ambulan beserta petugas kesehatanterlatih.
2.Petugas kesehatan/dokter umum di klinik- Mengenali gejala sindrom koroner akut dan pemeriksaan EKG bila ada- Tirah baring dan pemberian oksigen 2-4 L/menit- Berikan aspirin 160-325 mg tabletkunyah bila tidak ada riwayat alergi aspirin
- Berikan preparat nitrat sublingualmisalnya isosorbid dinitrat 5 mg dapat diulangsetiap 5-15 menit sampai 3 kali
- Bila memungkinkan pasangjalur infus- Segera kirim ke rumah sakit terdekat dengan fasilitas ICCU (Intensive Coronary CareUnit) yang memadai denganpemasangan oksigen dan didampingi
dokter/paramedik yang terlatih
Tatalaksana Pra Rumah Sakit
-
7/28/2019 SKA barudfd
32/77
-
7/28/2019 SKA barudfd
33/77
-
7/28/2019 SKA barudfd
34/77
-
7/28/2019 SKA barudfd
35/77
-
7/28/2019 SKA barudfd
36/77
-
7/28/2019 SKA barudfd
37/77
-
7/28/2019 SKA barudfd
38/77
-
7/28/2019 SKA barudfd
39/77
-
7/28/2019 SKA barudfd
40/77
-
7/28/2019 SKA barudfd
41/77
-
7/28/2019 SKA barudfd
42/77
STEMI cardiac care
STEP 1: AssessmentTime since onset of symptoms
90 min for PCI / 12 hours for fibrinolysis
Is this high risk STEMI? KILLIP classification
If higher risk may manage with more invasive rx
Determine if fibrinolysis candidate
Meets criteria with no contraindications
Determine if PCI candidate Based on availability and time to balloon rx
-
7/28/2019 SKA barudfd
43/77
Fibrinolysis Indications
ST segment elevation >1mm in twocontiguous leads
New LBBB
Symptoms consistent with ischemia
Symptom onset less than 12 hrs prior topresentation
Absolute contraindications for fibrinolysis
-
7/28/2019 SKA barudfd
44/77
Absolute contraindications for fibrinolysis
therapy in patients with acute STEMI
Any prior ICH Known structural cerebral vascular lesion (e.g., AVM)
Known malignant intracranial neoplasm
(primary or metastatic) Ischemic stroke within 3 months EXCEPT acute
ischemic stroke within 3 hours
Suspected aortic dissection
Active bleeding or bleeding diathesis (excluding menses)
Significant closed-head or facial trauma within 3 months
Relati e contraindications for fibrinol sis
-
7/28/2019 SKA barudfd
45/77
Relative contraindications for fibrinolysis
therapy in patients with acute STEMI
History ofchronic, severe, poorly controlled hypertension Severe uncontrolled hypertension on presentation (SBP greater than 180 mmHg
or DBPgreater than 110 mmHg) History of prior ischemic stroke greater than 3 months, dementia, or known
intracranial pathology not covered in contraindications Traumatic or prolonged (greater than 10 minutes) CPR or major surgery (less
than 3 weeks) Recent (within 2-4 weeks) internal bleeding Noncompressible vascular punctures For streptokinase/anistreplase: prior exposure (more than 5 days ago) or prior
allergic reaction to these agents Pregnancy
Active peptic ulcer Current use of anticoagulants: the higher the INR, the higher the risk of
bleeding
-
7/28/2019 SKA barudfd
46/77
STEMI cardiac care
STEP 2: Determine preferred reperfusion strategy
Fibrinolysis preferred if: 90min
door to balloon minusdoor to needle > 1hr
Door to needle goal 3 hr High risk STEMI
Killup 3 or higher
STEMI dx in doubt
Medical Therapy
-
7/28/2019 SKA barudfd
47/77
Medical Therapy
MONA + BAH
Morphine (class I, level C)Analgesia
Reduce pain/anxietydecrease sympathetic tone, systemic
vascular resistance and oxygen demand Careful with hypotension, hypovolemia, respiratory
depression
Oxygen(2-4 liters/minute) (class I, level C) Up to 70% of ACS patient demonstrate hypoxemia
May limit ischemic myocardial damage by increasingoxygen delivery/reduce ST elevation
-
7/28/2019 SKA barudfd
48/77
Nitroglycerin(class I, level B)
Analgesiatitrate infusion to keep patient pain free Dilates coronary vesselsincrease blood flow
Reduces systemic vascular resistance and preload
Careful with recent ED meds, hypotension, bradycardia,tachycardia, RV infarction
Aspirin(160-325mg chewed & swallowed) (class I, level A) Irreversible inhibition of platelet aggregation
Stabilize plaque and arrest thrombus
Reduce mortality in patients with STEMI
Careful with active PUD, hypersensitivity, bleedingdisorders
-
7/28/2019 SKA barudfd
49/77
Beta-Blockers(class I, level A) 14% reduction in mortality risk at 7 days at 23% long term
mortality reduction in STEMIApproximate 13% reduction in risk of progression to MI
in patients with threatening or evolving MI symptoms
Be aware of contraindications (CHF, Heart block,Hypotension)
Reassess for therapy as contraindications resolve
ACE-Inhibitors / ARB (class I, level A) Start in patients with anterior MI, pulmonary congestion,
LVEF < 40% in absence of contraindication/hypotension Start in first 24 hours
ARB as substitute for patients unable to use ACE-I
-
7/28/2019 SKA barudfd
50/77
Heparin (class I, level C to class IIa, level C) LMWH or UFH(max 4000u bolus, 1000u/hr)
Indirect inhibitor of thrombin
less supporting evidence of benefit in era of reperfusion
Adjunct to surgical revascularization and thrombolytic /PCI reperfusion
24-48 hours of treatment
Coordinate with PCI team (UFH preferred)
Used in combo with aspirin and/or other platelet inhibitors
Changing from one to the other not recommended
-
7/28/2019 SKA barudfd
51/77
Additional medication therapy
Clopidodrel(class I, level B) Irreversible inhibition of platelet aggregation
Used in support of cath / PCI intervention or ifunable to take aspirin
3 to 12 month duration depending on scenario
Glycoprotein IIb/IIIa inhibitors(class IIa, level B)
Inhibition of platelet aggregation at final common
pathway In support of PCI intervention as early as possible
prior to PCI
-
7/28/2019 SKA barudfd
52/77
Additional medication therapy
Aldosterone blockers (class I, level A)
Post-STEMI patients
no significant renal failure (cr < 2.5 men or 2.0 for women)
No hyperkalemis > 5.0 LVEF < 40%
Symptomatic CHF or DM
-
7/28/2019 SKA barudfd
53/77
-
7/28/2019 SKA barudfd
54/77
-
7/28/2019 SKA barudfd
55/77
Rekomendasi pengobatan SKA
Rekomendasi terapi antitrombotik tampa terapireperfusi
Rekomendasi terapi antirombotik pada pemberianterapi fibrinolitik
Rekomendasi antitrombotik pada terapi angioplastikoroner perkutan (PCI) primer
Dosis ACE-Inhibitor pada tatalaksana SKA
Dosis ARB pada SKA Rekomendasi terapi untuk mengatasi nyeri, sesak dan
anxietas
-
7/28/2019 SKA barudfd
56/77
-
7/28/2019 SKA barudfd
57/77
-
7/28/2019 SKA barudfd
58/77
-
7/28/2019 SKA barudfd
59/77
-
7/28/2019 SKA barudfd
60/77
-
7/28/2019 SKA barudfd
61/77
-
7/28/2019 SKA barudfd
62/77
STEMI care CCU
Monitor for complications: recurrent ischemia, cardiogenic shock, ICH, arrhythmias
Review guidelines for specific management ofcomplications & other specific clinical scenarios PCI after fibrinolysis, emergent CABG, etc
Decision making for risk stratification at hospitaldischarge and/or need for CABG
Risk Stratification to Det
ermine the Likelihood of
-
7/28/2019 SKA barudfd
63/77
Assessment Findings indicatingHIGHl ikel ihood of ACS
Findings indicating
INTERMEDIATEl ikel ihood o f ACS in
absence of high-
l ikel ihood f ind ings
Findings indicating
LOWl ikel ihood of ACSin absence of high- or
intermediate-l ikel ihood
f ind ings
History Chest or left arm pain ordiscomfort as chief
symptom
Reproduction of previous
documented angina
Known history of coronary
artery disease, including
myocardial infarction
Chest or left arm pain or
discomfort as chief
symptom
Age > 50 years
Probable ischemic
symptoms
Recent cocaine use
Physical
examination
New transient mitral
regurgitation,
hypotension, diaphoresis,
pulmonary edema or rales
Extracardiac vascular
disease
Chest discomfort
reproduced by palpation
ECG New or presumably newtransient ST-segment
deviation (> 0.05 mV) or T-
wave inversion (> 0.2 mV)
with symptoms
Fixed Q waves
Abnormal ST segments or
T waves not documented
to be new
T-wave flattening or
inversion of T waves in
leads with dominant R
waves
Normal ECG
Serum cardiac
markers
Elevated cardiac troponin
T or I, or elevated CK-MB
Normal Normal
Acute Coronary Syndrome
ACS i k i i
-
7/28/2019 SKA barudfd
64/77
ACS risk criteria
Low Risk ACS
No intermediate or high
risk factors
10 minutes rest pain,
now resolved
T-wave inversion > 2mm
Slightly elevated cardiac
markers
-
7/28/2019 SKA barudfd
65/77
High Risk ACS
Elevated cardiac markersNew or presumed new ST depression
Recurrent ischemia despite therapy
Recurrent ischemia with heart failure
High risk findings on non-invasive stress testDepressed systolic left ventricular function
Hemodynamic instability
Sustained Ventricular tachycardia
PCI with 6 monthsPrior Bypass surgery
-
7/28/2019 SKA barudfd
66/77
Low
risk
High
risk
Conservative
therapy
Invasive
therapy
Chest Pain
center
Intermediate
risk
-
7/28/2019 SKA barudfd
67/77
Secondary Prevention
Disease
HTN, DM, HLP
Behavioral smoking, diet, physical activity, weight
Cognitive
Education, cardiac rehab program
Secondary Prevention
-
7/28/2019 SKA barudfd
68/77
Secondary Prevention
disease management
Blood Pressure Goals < 140/90 or 500; consider omega-3 fatty acids
DiabetesA1c < 7%
Secondary prevention
-
7/28/2019 SKA barudfd
69/77
Secondary prevention
behavioral intervention
Smoking cessation Cessation-class, meds, counseling
Physical Activity Goal 30 - 60 minutes daily
Risk assessment prior to initiation
Diet DASH diet, fiber, omega-3 fatty acids
-
7/28/2019 SKA barudfd
70/77
Thinking outside the box
Secondary prevention
-
7/28/2019 SKA barudfd
71/77
Secondary prevention
cognitive
Patient education
In-hospitaldischargeoutpatient clinic/rehab
Monitor psychosocial impact Depression/anxiety assessment & treatment
Social support system
Medication Checklist
-
7/28/2019 SKA barudfd
72/77
after ACS
Antiplatelet agentAspirin* and/or Clopidorgrel
Lipid lowering agent Statin* Fibrate / Niacin / Omega-3
Antihypertensive agent Beta blocker*ACE-I*/ARBAldactone (as appropriate)
Pr nti n n
-
7/28/2019 SKA barudfd
73/77
Prevention news
From 1994 to 2004 the death rate fromcoronary heart disease declined 33%...
But the actual number of deaths declinedonly18%
Getting better with treatment
But more patients developing diseaseneed forprimary prevention focus
-
7/28/2019 SKA barudfd
74/77
Summary
ACS includes UA, NSTEMI, and STEMI
Management guideline focus Immediate assessment/intervention (MONA+BAH)
Risk stratification (UA/NSTEMI vs. STEMI)
RAPID reperfusion for STEMI (PCI vs. Thrombolytics)
Conservative vs Invasive therapy for UA/NSTEMI
Aggressive attention to secondary preventioninitiatives for ACS patients
Beta blocker, ASA, ACE-I, Statin
Conclusions; Treatment of
-
7/28/2019 SKA barudfd
75/77
Conclusions; Treatment of
NSTEMI/USA ASA NTG (consider MSO4 if pain not relieved)
Beta Blocker
Heparin/LMWH ACE-I
+/- Statin
+/- Clopidogrel (dont give if CABG is a possibility)
+/- IIBIIIA inhibitors (based on TIMI risk score)
Conclusions; Treatment of
-
7/28/2019 SKA barudfd
76/77
Conclusions; Treatment of
STEMI ASA NTG (consider MSO4 if pain not relieved)
Beta Blocker
Heparin/LMWH ACE-I
+/-Clopidogrel (based on possibility of CABG)
IIBIIIA
+/- Statin
Activate the Cath Lab!!!
-
7/28/2019 SKA barudfd
77/77