Scleroderma: skin stiffness assessment using the stress–strain relationship under progressive...
Transcript of Scleroderma: skin stiffness assessment using the stress–strain relationship under progressive...

1. Introduction
2. Mechanotransduction in the
skin connective tissue
3. Materials and methods
4. Progressive stress-vs-strain
relationship
5. Discussion
Original Research
Scleroderma: skin stiffnessassessment using the stress--strainrelationship under progressivesuctionGerald E Pierard†, Trinh Hermanns-Le & Claudine Pierard-FranchimontUniversity Hospital of Liege, Department of Dermatopathology, Liege, Belgium
Introduction: A few non-invasive biometrological methods are available
for monitoring skin stiffening in systemic scleroderma. Among them, the
Cutometer� is used for years by several clinical teams.
Objectives: To revisit the microscopic structure of the dermal fibrous networks
in scleroderma and the relationship with changes in viscoelasticity.
Methods: The suction method delivered by the Cutometer� was applied
following the progressive stress-vs-strain modality.
Results: The test procedure was sensitive enough to document the initial pro-
gression steps of acroscleroderma. Four stages were thus identified including
i) the incipient, ii) the progressive, iii) the overt, and iv) the regressive
acroscleroderma.
Conclusion: The non-invasive determination of skin biomechanical functions
is relevant both in routine clinical practice and in antisclerotic drug develop-
ment. It is complementary although not a substitute for the determination
of selected serum biomarkers.
Keywords: biomechanics, scleroderma, skin stiffness, skin viscoelasticity, tensile strength
Expert Opin. Med. Diagn. (2013) 7(2):119-125
1. Introduction
In recent decades, various instrumentations were used for assessing the in vivoviscoelasticity of skin [1-3]. The methods relied on various approaches includingthe uniaxial and biaxial stretching, torsion, elevation, indentation, ballistometry,and suction procedures [1,4]. The time-honored suction method aims at measuringthe skin deformation caused by any loss of pressure exerted over a defined skinarea [5-10]. Skin deformation occurs as a function of the suction force, its time ofapplication, and the surface area of the stressed skin [11-13]. It is regarded as thein vivo expression of the overall skin viscoelasticity.
From a skin physiopathological standpoint, it is crucial to determine at least threeclinically-relevant physical characteristics, namely i) the skin stiffness correspondingto the resistance to shape changes, ii) the skin elasticity representing the ability toshape recovery after deformation, and iii) the skin viscous deformation over timeand the creep extension [14]. Over the large part of the body, the overall skin visco-elasticity mainly depends on the skin connective tissue (SCT) structures present inthe dermo-hypodermal tissues, with minimal contribution from the epidermis [12].
Skin is anisotropic both in its structure and mechanical functions [12,15]. In addi-tion, the value of the skin viscoelastic parameters is time-dependent and related tothe thickness of the involved tissues. On the overall, data vary with the body region,age, gender, duration of the test procedure and some specific environmentalconditions [12]. The variability in these features induces some uncertaintiesassociated with the collection, comparison, and interpretation of data.
10.1517/17530059.2013.753877 © 2013 Informa UK, Ltd. ISSN 1753-0059, e-ISSN 1753-0067 119All rights reserved: reproduction in whole or in part not permitted
Exp
ert O
pin.
Med
. Dia
gn. D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y D
alho
usie
Uni
vers
ity o
n 04
/29/
13Fo
r pe
rson
al u
se o
nly.

As a rule, the in vivo viscoelasticity of human SCT is quitedifficult to assess with confidence and repeatability. Clearly, aseries of physiological variables (age, hormonal status, bodymass index, etc.) modulate the SCT viscoelasticity [12]. Theselimitations are mainly due to: i) the complex relationshiplinking the various SCT components involved in any testprocedure, ii) the ill-defined intrinsic viscoelasticity of theSCT, and iii) the unknown influence of previous mechanicalpreconditioning at the test site [12]. Hence, there is a riskfor some misconceptions and scientific prejudices cloudingcritical issues for some data interpretations.The purpose of this work was to revisit a specific non-
invasive suction method routinely applicable to clinical andexperimental settings dealing with scleroderma. We focusedour attention on the relevant structures of the SCT. Theprinciples of mechanical testing and their controlled para-meters are critically reviewed and explored in acrosclerodermaassociated with Raynaud’s phenomenon.
2. Mechanotransduction in the skinconnective tissue
The bulk of the normal SCT controlling skin viscoelasticityconsists of a complex fibrous network forming the scaffoldof the extracellular matrix (ECM). The major set of compo-nents is composed of collagen fibers whose organizationdetermines both the mechanical stability of the tissue and itsresistance to deformation. A second set of components corre-sponds to elastic fibers present in smaller amounts. They serveto restore bended collagen bundles to their relaxed standingposition [15,16]. The loosely interconnected complex fiber scaf-fold is permeated by the amorphous hydrated ECM enrichedin proteoglycans, glycoproteins, and glycosaminoglycans.This composite material embeds cells globally responsiblefor maintaining or remodeling the structural steady state ofthe SCT. In different body regions, considerable differencesexist in the relative proportions and three-dimensional organi-zation of each SCT component. In addition, some expectedvariations occur during ageing and diseases [15,16]. In sclero-derma, collagen bundles are thickened and they merge eachother laterally. Such fusion between collagen bundles wrecks,at least in part, the function of the elastic fibers entrappedinside the massive bulk of collagen bundles [17-19].With respect to structural determinants involved in the
SCT viscoelasticity, the dermis is conveniently divided intotwo main layers, namely the adventitial and the reticulardermis [15]. The former is a superficial zone of loose connec-tive tissue abutted to the epidermis and its hair folliclescorresponding to the papillary and the perifollicular dermis,respectively. By contrast, the reticular dermis is formedby a netlike scaffold of fiber bundles. In the hypodermis,distinct SCT layers partition the lobules of adipocytes. Therelative density and organization of fibers, rather than anyabsolute molecular difference, distinguish these compart-ments. However, both the differences in the intimate
structure and the boundaries between these layers are notsharply defined, particularly in scleroderma [17].
The global response of skin to any mechanical stressdepends on tensile biomechanical and rheological functionsprovided by the composite nature of the skin and subcu-taneous tissues [15]. In a mechanical standpoint, the expectedproperties of the normal adventitial dermis resemble thoseof the hypodermal septae. Their flexibility is conditionedby a loose open meshwork of fine collagen fibers runninghaphazardly with regard to the skin surface [13]. The reticulardermis is somewhat stiffer because collagen bundles arethicker, closely packed parallel to the skin surface, but moder-ately interconnected. Environmental factors including ultra-violet and infrared wavelengths superimpose their effects onthose of chronological ageing [13]. In scleroderma, the dermalremodeling affects indiscriminately all levels of the SCT. In aglobal view, the function of the coarse collagen networkspredominates over other structures. This is particularly truein scleroderma.
3. Materials and methods
3.1 DesignThe study was approved by the Ethic Committee of ourUniversity Hospital, and it was performed in accordancewith the Declaration of Helsinki. A total of 93 Caucasian sub-jects of both genders, aged 24 -- 48 years, were enrolled. Thevolunteers signed an informed consent after the entire proce-dure of the study had been fully explained. The study wasperformed between Fall 2007 and Spring 2012.
A total of 70 healthy subjects (32.1 ± 9.9 years, M/F:27/43) established the normal reference group. Another groupcorresponded to 23 subjects with Raynaud’s phenomenonassociated with a discrete skin induration identified as incipi-ent acroscleroderma. They consisted of 17 women and 6 menaged 28.6 ± 7.3 years. Nailfold capillaroscopy had identifiedthe vascular changes since 3.2 ± 1.9 years. At the time ofassessments, the patients had never been treated for theirskin condition. This group of incipient acroscleroderma alsoencompassed 14 patients (10 women and 4 men aged34.7 ± 4.1 years) exhibiting typical changes at the nailfoldcapillaroscopy without evidence for Raynaud’s phenomenon.Three other groups of patients were constituted. They corre-sponded to progressive acroscleroderma (33 women and15 men aged 39.2 ± 5.5 years), overt acroscleroderma(7 women and 3 men aged 42.6 ± 4.4 years) and regressiveacroscleroderma (4 women and 1 men aged 40.8 ± 6.0 years).
3.2 ProcedureThe Cutometer� SM 474 and MPA 580 versions (C+Kelectronic, Cologne, Germany) were equipped with a hollowprobe centered by a 4-mm diameter suction aperture. Thehand-held probe was maintained onto the skin surface witha constant pressure guaranteed by a built-in spring. Anadditional outer concentric 55-mm diameter steel guard ring
G. E. Pierard et al.
120 Expert Opin. Med. Diagn. (2013) 7(2)
Exp
ert O
pin.
Med
. Dia
gn. D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y D
alho
usie
Uni
vers
ity o
n 04
/29/
13Fo
r pe
rson
al u
se o
nly.

was affixed to the skin by a double-side adhesive film [14].Adhesive tapes (acrylate paper type or silicone tape) wereplaced in a crosswise pattern between the outer guard ringand the probe. In each individual, duplicate measurementsat 1-h interval were performed on the volar aspect of bothforearms. The respective viscoelastic values were averaged.
The progressive suction modality with a stress-vs-strainrecording [14,20,21] was performed at different time intervalsaccording to the clinicians’ demands and to the clinical statusof the disease. In a theoretical basis, a purely elastic materialis typically characterized by a straight linear relationshipbetween stress and strain that is independent of time. Visco-sity refers to changes in deformation occurring in time undera sustained constant force [12]. Plasticity implies resistance toany deformation for small forces. Such combination of basicproperties is expressed by a non-linearity of the relationshipof force (stress) to deformation (strain).
At each session of evaluation, the maximum vertical skindeformation (MD) representing the skin stiffness was measuredafter applying a progressive suction force at a 25 mbar/s rate for20 s. This step procedure was followed by a similar lineardecrease in suction during a 20--s relaxation phase. Duringthe 20-s relaxation period, the strain values did not returnto the baseline value, and the intercept of the curve on thestrain axis defined the residual deformation (RD). This para-meter shows a short-term limitation in elastic recovery. Thebiological elasticity (BE) was expressed in % and defined as102(MD -- RD)MD-1. The stress-vs-strain curve on suctionwas not superposed to the relaxation curve. The area delimitedby the two curves corresponded to the hysteresis loop.
The present skin deformation test under progressivesuction corresponds to a cycle comprising a two-step proce-dure involving the application of increasing and decreasingforces at a constant pace. The skin deformation is alwaysmore manifest when the force is decreasing than in theincreasing phase at the same force.
According to the evolution in time of the viscoelastic para-meters relevant to the clinical presentation, four rheologicalstages of acroscleroderma were tentatively proposed. Theycorresponded to the incipient, progressive, overt and regressivestages, respectively. Individual values were compared to the10th and 90th percentiles of the normal reference popula-tion [11]. For each acroscleroderma stage, data were summarizedas means and standard deviations. Variance analysis wasused for comparing normal skin with each of the four definedrheological stages. A p-value less than 0.05 was consideredstatistically significant.
4. Progressive stress-vs-strain relationship
In normal subjects as well as in the acroscleroderma/Raynaud’s phenomenon group, an hysteresis loop wasdisclosed under the progressive suction modality. During thephase of suction increment on normal skin, the rate of skindeformation was discretely curved. By contrast, the relaxation
curve appeared more bulky. Its initial portion showed plasti-city with a near absence or discrete reduction in the straindeformation. By contrast, the rate of strain reduction wasaccelerated during the late phase of recovery.
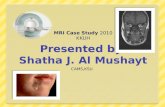
In the acroscleroderma/Raynaud’s phenomenon group, theshape of the curves appeared altered according to the severityof the skin condition. The disease severity rating yieldeddistinct rheological stages (Table 1). The incipient stage wasidentified by a significant RD increase (p < 0.05) and BEdecrease (p < 0.01). The progressive stage was characterizedby the combination of an ongoing RD increase and significant(p < 0.01) MD and BE reductions, while hysteresis increased(p < 0.05) (Figure 1). The overt stage was recognized by signi-ficant (p < 0.01) MD and BE decreases with hysteresis shrink-age (Figure 2). The regressive stage of acroscleroderma showeda trend in MD and RD recovery.
5. Discussion
It is inarguable that in vivo mechanical bioinstrumentationprovides insight into skin physiopathology [12]. The effectsof a number of physiological and environmental variablesimpacting the skin tensile functions have been documentedin the medical literature. However, it remains some confusionregarding the expression and interpretation of specific data onskin mechanical testing [1]. These limitations result from: theabsence or misuse of i) a standardized nomenclature of para-meters, ii) a uniform system of units, and iii) controlled orstandardized methods.
The quantitative non-invasive assessment of skin toughnessin acroscleroderma is of interest for monitoring the diseaseevolution and the therapeutic efficacy. Until now, only fewstudies on suction-mediated skin viscoelasticity have beencarried out in patients with scleroderma [16,22-24]. Differentdevices and modalities had been employed. Hence, resultsare difficult to compare, even though there is overall agree-ment about the basic changes in the altered skin viscoelasticityfound in acroscleroderma. During the past 15 years, the suc-tion method was used by the majority of researchers [25-30].Increased deep dermal tethering is a feature of both Raynaud’sphenomenon and acroscleroderma. One could speculatethat both conditions alter the SCT following microcircu-latory functional damage and deposition of various ECMmacromolecules [31-35].
The deflection of the suction curve during progressive skinsclerosis was interpreted as a sign of increased plasticity indi-cating a limitation in collagen bundle reorientation underlow stress. The reduction in MD probably results from theincreased cohesiveness between collagen bundles responsiblefor a limitation in tissue extension. During the relaxationphase, early plasticity reflects the limitation in flexibility ofthe collagen network that fails to return to its initial position.At that stage, the elastic fibers are unable to overcome thecompactness of the collagen scaffold [16]. The last portion ofthe relaxation curve shows an attempt at returning to the
Scleroderma: skin stiffness assessment using the stress--strain relationship under progressive suction
Expert Opin. Med. Diagn. (2013) 7(2) 121
Exp
ert O
pin.
Med
. Dia
gn. D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y D
alho
usie
Uni
vers
ity o
n 04
/29/
13Fo
r pe
rson
al u
se o
nly.

initial position. All these curve alterations are responsible foran overall change in hysteresis.When a force is applied to the dermis, fibers are first
directed parallel to the force and after completion, they arepossibly elongated [15]. Elongation is easily obtained for elasticfibers. By contrast, collagen fibers are almost inextensible.Some authors have postulated that cross-links were
responsible for the resistance of fibers to deformation. How-ever, cross-links probably play a limited role in the responseof normal skin in the physiological range of stress. In fact,they are mainly involved in resisting larger forces resultingin fiber breaking. Their role under casual stress is likelylimited because they correspond to covalent bonds linkingadjacent parallel collagen molecules. Hence their direction is
Table 1. Viscoelastic parameters (means ± SD) yielded by the progressive suction procedure according to the
functional stage of acroscleroderma (ASD) with Raynaud’s syndrome.
Stage n MD (mm) RD (mm) BE (%) Hysteresis (AU)
Normal 70 0.42 ± 0.08 0.10 ± 0.04 76.2 ± 3.5 47.8 ± 13.5Incipient ASD 37 0.39 ± 0.12 0.18* ± 0.07 53.8z ± 10.1 52.5 ± 15.1Progressive ASD 48 0.33z ± 0.09 0.22* ± 0.08 33.4z ± 12.8 62.7* ± 11.8Overt ASD 10 0.29z ± 0.06 0.17 ± 0.05 41.4z ± 8.5 36.8z ± 6.3Regressive ASD 5 0.37 ± 0.17 0.15 ± 0.11 59.5 ± 13.8 55.9 ± 15.6
In the comparison with normal skin.
*p < 0.05.zp < 0.01.
AU: Arbitrary unit; BE: Biological elasticity; MD: Maximum deformation; RD: Residual deformation.
Suction (mbar)A. B.
C.
Skin deformation (mm)
500
450
350
250
200
150
100
50
00.0 0.1 0.2 0.3 0.4 0.5
300
400
Suction (mbar)
Skin deformation (mm)
500
450
350
250
200
150
100
50
00.0 0.1 0.2 0.3 0.4 0.5
300
400
Suction (mbar)
Skin deformation (mm)
500
450
350
250
200
150
100
50
00.0 0.1 0.2 0.3 0.4 0.5
300
400
Suction (mbar)
Skin deformation (mm)
500
450
350
250
200
150
100
50
00.0 0.1 0.2 0.3 0.4 0.5
300
400
D.
Figure 1. Stress-vs-strain relationship representing the progressive skin deformation cycle by suction (Cutometer�) in a
patient with Raynaud’s phenomenon. A. Initial aspect. B. One year later, some plasticity occurs during low depression in the
loading curve, and the residual deformation increases. C. 15 months later, skin stiffening was clinically perceptible. MD has
decreased, RD has increased and hysteresis as well. D. 27 months later, MD appeared improved, RD remained stable but
plasticity at low suction increased.
G. E. Pierard et al.
122 Expert Opin. Med. Diagn. (2013) 7(2)
Exp
ert O
pin.
Med
. Dia
gn. D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y D
alho
usie
Uni
vers
ity o
n 04
/29/
13Fo
r pe
rson
al u
se o
nly.

perpendicular to the forces that first direct the collagen fibers.Being at right angles to the force, they supposedly supportlittle of it. In the physiological range of tension, the structuralorganization of collagen bundles, their orientations, theanchorage of bundles together, and their relationship to elasticfibers and proteoglycans are probably predominant [12].
The efficacy of various antisclerotic therapies is difficult toestablish by clinical inspection alone [36,37] unless objectivebioinstrumentation is used. In our experience, determiningskin viscoelasticity is an appropriate non-invasive procedureto shed some light on therapeutic efficacy.
In general, it is reasonable to interpret the in vivo skin tensilefunctions of whole skin as representing the global properties ofthe dermis and subcutaneous tissues. Hence, understanding thein vivo mechanical measurements requires a knowledge of theoverall microstructure of the SCT, including the arrangementof collagen and elastic fibers, and their relation to other macro-molecules. Such information is limited as far as microanato-mical differences exist between SCT in healthy subjects andpatients with acroscleroderma and Raynaud’s phenomenon.Advances in knowledge of the skin tensile functions are ham-pered by various difficulties, although they must not inhibitclinicians and researchers who are keen to get relevant dataon SCT disorders. An innovative yet pragmatic approach isneeded to force the topic forward.
The end result of the biological manifestations of acroscle-roderma is the deposition of collagen polymers. As a result ofthe accumulation of collagen and other biomolecules in acro-scleroderma, skin thickens. It becomes impossible to pinchskin into a regular skinfold. This phenomenon, known as“hidebinding” or “tethering,” is the most impressive change
in sclerotic skin. The Cutometer� lifting the skin into a mea-surement probe represents the closest possible mechanicalmimicry of pinching skin into a skinfold. This process isdependent from the activity and severity of the disease. Dueto the easy access to the skin by the clinician, it seems reason-able to use a simple non-invasive method allowing themeasurement of the SCT viscoelasticity. Although it may bean important step in the clinical evaluation of SCT altera-tions, the assessment of skin stiffening has not yet gainedgeneral acceptance. It remains that the Cutometer� is atime-honored device designed for measuring the in vivo skinmechanical functions. Both the suction force and its rate ofapplication are controlled. Data have been presented in theliterature about the changes observed in scleroderma usingthe Cutometer� under the stress-vs-time modality. By con-trast, in the present study, the stress-vs-strain modality wasused. This procedure is more subtle and probably disclosesmore subtle rheological changes occurring during theevolution of sclerosis.
The present biomechanical changes are relevant to clinicalsettings. In patients with systemic sclerosis, the sclerotic skinchanges correlate with the overall disease activity and progno-sis. The regular clinical evaluation is solely based on subjectiveexamination of the skin by a trained observer. In thesecircumstances, the interobserver and intraobserver reliabilityis typically low, but it remains surprisingly regarded as asuitable primary outcome variable in most clinical trials. Toreduce subjectivity and increase reliability, some investigatorsused devices measuring skin sclerosis objectively and quantita-tively. At present there is no biomarker directly related to theactual SCT stiffening. Hence, both direct estimates of skinsclerosis (biomechanical assessments) and its precursor stages(serum biomarkers) could be combined when assessing drugefficacy during trials and individual follow-up.
Acknowledgments
The authors appreciate the excellent secretarial assistance ofI Leclercq and M Pugliese.
Declaration of interest
This work was supported by a grant from the “Fonds d’Inves-tissement de la Recherche Scientifique” of the UniversityHospital of Liege. No other sources of funding were used toassist in the preparation of this manuscript. The authorshave no conflict of interest that are directly relevant to thecontent of this review.
Suction (mbar)
Skin deformation (mm)
500
450
350
250
200
150
100
50
00.0 0.1 0.2 0.3 0.4 0.5
300
400
Figure 2. Stress-vs-strain relationship inovert acroscleroderma.
Both MD and hysteresis are low.
Scleroderma: skin stiffness assessment using the stress--strain relationship under progressive suction
Expert Opin. Med. Diagn. (2013) 7(2) 123
Exp
ert O
pin.
Med
. Dia
gn. D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y D
alho
usie
Uni
vers
ity o
n 04
/29/
13Fo
r pe
rson
al u
se o
nly.

BibliographyPapers of special note have been highlighted as
either of interest (�) or of considerable interest(��) to readers.
1. Rodrigues L; EEMCO group. EEMCO
guidance to the in vivo assessment of
tensile functional properties of the skin.
Part 2: instrumentation and test modes.
Skin Pharmacol Appl Skin Physiol
2001;14:52-67.. A comprehensive review of
bioinstrumentations available for
measuring the skin
biomechanical functions.
2. Shang X, Yen MR, Gaber MW. Studies
of biaxial mechanical properties and
nonlinear finite element modeling of
skin. Mol Cell Biomech 2010;7:92-104
3. Sandford E, Chen Y, Hunter I, et al.
Capturing skin properties from
dynamic mechanical analyses.
Skin Res Technol Epub
2012;[Epub ahead of print]
4. Murry BC, Wickett RR. Correlations
between dermal torque meter�,
cutometer�, and dermal phase meter�measurements of human skin.
Skin Res Technol 1997;3:101-6
5. Cua AB, Wilhelm KP, Maibach HI.
Elastic properties of human skin :
relation to age, sex, and anatomical
region. Arch Dermatol Res
1990;282:283-8. A well-designed consideration of data
gained by the Cutometer�.
6. Pierard GE, Kort R, Letawe C, et al.
Biomechanical assessment of
photodamage. Derivation of a
cutaneous extrinsic ageing score.
Skin Res Technol 1995;1:17-20
7. Diridollou S, Patat F, Gens F, et al. In
vivo model of the mechanical properties
of the human skin under suction.
Skin Res Technol 2000;6:214-21
8. Gniadecka M, Serup J. Suction chamber
method for measuring skin mechanical
properties: The Dermaflex�; In: Serup J,
Jemec GBE, Grove GL, editors.
Handbook of non-invasive methods and
the skin. 2nd edition. CRC Press, Boca
Raton; 2006. p. 571-8
9. Barel AO, Courage W, Clarys P. Suction
chamber method for measurement
of skin mechanics: The new digital
version of the Cutometer�. In: Serup J,
Jemec GBE, Grove GL, editors.
Handbook of non-invasive methods and
the skin. 2nd edition. CRC Press; Boca
Raton; 2006. p. 583-91
10. Livarinen JT, Korhonen RK, Julkunen P,
et al. Experimental and computational
analysis of soft tissue mechanical response
under negative pressure in forearm.
Skin Res Technol 2012; Epub May 31
11. Pierard GE, Nikkels-Tassoudji N,
Pierard-Franchimont C. Influence of the
test area on the mechanical properties of
skin. Dermatology 1995;191:9-15. Original work alluding to the
influence of the size of skin
under suction.
12. Pierard GE. EEMCO guidance to the
in vivo assessment of tensile functional
properties of the skin. Part 1: relevance
to the structures and ageing of the
skin and subcutaneous tissues. Skin
Pharmacol Phys 1999;12:352-62.. A comprehensive analysis of the
relationship between the skin tensile
functions and the structure of
the dermis.
13. Schlangen LJM, Brooken D,
Van Kemenade PM. Correlations
between small aperture skin suction
parameters: statistical analysis and
mechanical model. Skin Res Technol
2003;9:122-30
14. Pierard GE, Pierard S, Delvenne P.
In vivo evaluation of the skin tensile
strength by the suction method. Coping
with hysteresis and creep extension.
J Biosc Med; In press. An important contribution about
controlled procedures in the
Cutometer handling.
15. Pierard GE, Lapiere CHM.
Microanatomy of the dermis in relation
to relaxed skin tension lines and Langer’s
lines. Am J Dermatopathol
1987;9:219-24
16. Langton AK, Sherratt MJ, Griffiths CE,
et al. Differential expression of elastic
fibre components in intrinsically aged
skin. Biogerontology 2012;13:37-48
17. Pierard GE, Pierard-Franchimont C.
Lapiere ChM. Connective tissue
compartments in scleroderma. Study
of the structure and biomechanical
properties. Dermatologica
1985;170:105-13
18. Pierard GE. Histological and rheological
grading of cutaneous sclerosis in
scleroderma. Dermatologica
1989;179:18-20
19. Walters R, Pulitzer M, Kamino H.
Elastic fiber pattern in scleroderma/
morphea. J Cutan Pathol 2009;36:952-7
20. Pierard GE, Vanderplaetsen S,
Pierard-Franchimont C. Comparative
effect of hormone replacement therapy
on bone mass density and skin tensile
properties. Maturitas 2001;40:221-7
21. Pierard GE, Pierard-Franchimont C,
Vanderplaetsen S, et al. Relationships
between bone mass density and tensile
strength of the skin in women. Eur J
Clin Invest 2001;31:731-5
22. Kalis B, de Rigal J, Leonard F, et al.
In vivo study of scleroderma
by non-invasive techniques.
Brit J Dermatol 1990;122:785-91
23. Enomoto D, Mekkes NH, Bossuyt JR,
et al. Quantification of cutaneous
sclerosis with a skin elasticity meter in
patients with generalized scleroderma.
J Am Acad Dermatol 1996;35:381-7
24. Zhang X, Osborn TG, Pittelkow MR,
et al. Quantitative assessment of
scleroderma by surface wave technique.
Med Eng Phys 2011;33:31-7
25. Ishikawa T, Tamura T. Measurement of
skin elastic properties with a new suction
device: systemic sclerosis. J Dermatol
1996;23:165-8
26. Nikkels-Tassoudji N, Henry F,
Pierard-Franchimont C, et al.
Computerized evaluation of skin
stiffening in scleroderma. Eur J
Clin Invest 1996;26:457-60
27. Pierard-Franchimont C,
Nikkels-Tassoudji N, Lefebvre P, et al.
Subclinical skin stiffening in adults
suffering from type 1 diabetes mellitus.
A comparison with Raynaud’s syndrome.
J Med Engin Technol 1998;22:206-10
28. Dobrev HP. In vivo study of skin
mechanical properties in patients with
systemic sclerosis. J Am Acad Dermatol
1999;40:436-42
29. Fraiture AL, Henry F, Goffin V, et al.
How I explore… A cutaneous
scleroderma using noninvasive methods.
Rev Med Liege 2002;57:179-82
30. Dobrev H. In vivo study of skin
mechanical properties in Raynaud’s
phenomenon. Skin Res Technol
2007;13:91-4
G. E. Pierard et al.
124 Expert Opin. Med. Diagn. (2013) 7(2)
Exp
ert O
pin.
Med
. Dia
gn. D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y D
alho
usie
Uni
vers
ity o
n 04
/29/
13Fo
r pe
rson
al u
se o
nly.

31. Stucker M, Quinna S, Memmel U, et al.
Macroangiopathy of the upper
extremities in progressive systemic
sclerosis. Eur J Med Res
2000;19:295-302
32. Fett N, Werth VP. Update on morphea:
part II. Outcome measures and
treatment. J Am Acad Dermatol
2011;64:231-42
33. Pauling JD, Shipley JA, Harris ND,
et al. Use of infrared thermography as
an endpoint in therapeutic trials of
Raynaud’s phenomenon and systemic
sclerosis. Clin Exp Rheumatol
2012;30:S103-15
34. Pistorius MA, Carpentier PH. Minimal
work-up for Raynaud syndrome:
a consensus report. J Mal Vasc
2012;37:207-12. A thorough review of the exploration
of Raynaud’s syndrome.
35. Martin P, Teodoro WR, Velosa AP,
et al. Abnormal collagen V deposition in
dermis correlates with skin thickening
and disease activity in systemic sclerosis.
Autoimmun Rev 2012;11:827-35
36. Andres C, Kollmar A, Mempel M, et al.
Successful ultraviolet A1 phototherapy in
the treatment of localized scleroderma:
a retrospective and prospective study.
Brit J Dermatol 2010;162:445-7
37. Beyer C, Distler O, Distler JH.
Innovative antifibrotic therapies
in systemic sclerosis. Curr Opin
Rheumatol 2012;24:274-80. An important contribution about the
current treatments of scleroderma.
AffiliationGerald E Pierard†, Trinh Hermanns-Le &
Claudine Pierard-Franchimont†Author for correspondence
University of Liege,
Laboratory of Skin Bioengineering
and Imaging (LABIC),
CHU Sart Tilman,
BE-4000 Liege, Belgium
Tel: +32 4 3662408;
Fax: +32 4 3662976;
E-mail: [email protected]
Scleroderma: skin stiffness assessment using the stress--strain relationship under progressive suction
Expert Opin. Med. Diagn. (2013) 7(2) 125
Exp
ert O
pin.
Med
. Dia
gn. D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y D
alho
usie
Uni
vers
ity o
n 04
/29/
13Fo
r pe
rson
al u
se o
nly.