Rheumatic Fever & Rheumatic Heart Disease. Rheumatic fever (RF) is an acute, immunologically...
-
Upload
alvin-mclaughlin -
Category
Documents
-
view
230 -
download
5
Transcript of Rheumatic Fever & Rheumatic Heart Disease. Rheumatic fever (RF) is an acute, immunologically...
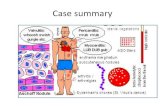
•Rheumatic fever (RF) is an acute, immunologically mediated, multisystem inflammatory disease that occurs a few weeks following an episode of group A streptococcal pharyngitis.•Major involvement of systemic connective tissue, it often violate connective tissue of heart, joint, skin, and subcutaneous and vascular connective tissue. Key pathologic features is Rheumatic Granuloma. •It occurs in children in age 5 to 15 years, 20% -adults•The clinical course of rheumatic fever involves a childhood infection with complications in adulthood (cardiac defect).
Rheumatic FeverRheumatic Fever
Etiology and pathogenesis
It is an immune response associated with streptococcal infection, but it is not caused by bacteria directly effects.
1. There is a streptococcus infection history before the onset of RF.
2. A variety of antibodies of the streptococcus and its products can be detected in the onset phase. serous "O" antibody in 95% patients is high, > 500 units.
3. Regional distribution consistent with area of streptococcal infection.
4. Antibiotic prophylaxis treatment is effective.
The evidence related with group A β-β-hemolytic streptococcus infection including:
The evidence which is not directly caused by streptococcus infection including:
1. The disease is not appeared in infected at the time, but in 2-3 weeks later, it is in line with emergence period of the general immune response.
• No evidence of direct invasion of organ by streptococcus.
• Streptococcus has never been found in the RF patient's blood .
• Not purulent inflammation, but the fibrinoid necrosis.
Antigen and antibody cross-reactivity:
The antigens of streptococcus may stimulate the immunological cross-reactivity in patients.
M antibody+Vascular smooth muscle
C antibody+Cardiovascular connective tissue
Pathogenesis
Antigen antibody complex
Local depositionalexin platelet
activation of
coagulation
system Embolism,
bleedingNeutrophil infiltration
Release of lysosomal enzymes(Neutral, acid hydrolases, elastase, collagenase and so on
Blood vessel, tissue injury
Basic pathological changes
1. Exudative and degenerative phase
2. The proliferative phase (Granulomatous period)
3. Scar phase (healed phase\Fibrosis phase\Hardening phase)
Exudative and degenerative phase It is characterized by serofibrinous exudate, with deposits of immune precipitate on collagen fibers that lead to fibrinoid
necrosis. About 1 months.
The proliferative phase (Granulomatous period)
Aschoff Body:
Structure:
center : fibrinoid necrosis
around the center : Anitschkow cells , lymphocytes, occasional plasma cells
Distribution:
Myocardial interstitial, subendocardial and subcutaneous connective tissue. Epicardial, joints and blood vessels is rare.
pathognomonic for RF
Anitschkow cells:These distinctive cells have abundant cytoplasm
and central round-to-ovoid nuclei in which the
chromatin is disposed in a central, slender, wavy
ribbon (hence the designation "caterpillar cells“--
cross section named Owl 's eye cells).
Some of the larger macrophages become multinucleated to form Aschoff cells(inflammatory
giant cells).
The myocardial interstitium has a circumscribed collection of mononuclear inflammatory cells, including some large histiocytes with prominent nucleoli and a prominent binuclear histiocyte, and central necrosis
Scar phase
Emergence of fibroblasts and collagen production, formation of small spindle scar, 2-3 months or so. The above three stages repeated attacks, the old and new lesions coexist.The whole course about 4-6 months.
RF involves various organs
Rheumatic heart diseaseRheumatic arthritisRheumatic arteritisRheumatic disease of skin Rheumatic disease of brain
Rheumatic heart disease
Divided into rheumatic endocarditis, rheumatic myocarditis and rheumatic pericarditis, often for rheumatic pancarditis.
60% to 80% children associated with pancarditis。
rheumatic endocarditis
Lesions were most often involved: mitral valve Secondly: both mitral and aortic valve
The most important lesions caused by rheumatism, valvular deformity and dysfunction
Pathological changes:
early stage: serous endocarditis , valve swelling,translucent Microscopically: valve become loose due to serous exudate , accompanied by macrophages entering and fibrinoid necrosis of collagen fiber.Concomitant involvement of the endocardium and the left-sided valves by inflammatory foci typically results the small (diameter 1- to 2-mm) vegetations .Vegetations: White thrombus consist of platelet
and cellulose.
Acute rheumatic endocarditis: small (diameter 1- to 2-mm) vegetations along the mitral valve margin, insufficient to cause valvular deformation.
Small vegetations (verruca) are visible along the line
of closure of the mitral valve leaflet (arrows).
Advanced: vegetations organization, recurrent organization cause chronic heart valve disease ( valvular stenosis and / or valvular insufficiency )
Mitral stenosis with diffuse fibrous thickening and distortion of
the valve leaflets, commissural fusion (arrows), and thickening
and shortening of the chordae tendineae.
rheumatic myocarditislocation:Myocardial interstitial connective tissue pathological changes: Rheumatic Granuloma
Perivascular Rheumatic Granuloma formation. Children often occurred to diffuse myocardial interstitial edema, inflammatory cell infiltration, congestive heart failure. Late effects myocardial contractile force.
A serous or serous fibrinous inflammation. Can
form a pericardial effusion, trichocardia
and constrictive pericarditis.
rheumatic pericarditis
pericardial effusion
Can lead to heart sound far, around the heart boundary expanding, serious cardiac X-ray showed a flask
Adhesive pericardit is in cardiac surface of patients. From the epicardial surface to the pericardial sac visible fibrinous exudate, which is typical for a fibrinous pericarditis.
trichocardia
Can lead to precordial pain, pericardial friction sound, serious cause constrictive pericarditis, influence on cardiac function.
Rheumatoid arthritis predilection age: Adults predilection site: involving the large joints, most
commonly in the knee and ankle joint, followed by the shoulder, wrist, elbow and other joints
Lesion characteristics: migratory polyarthritis. Local serous exudate, appear red, swelling, heat, pain and dysfunction. As the heals , serous exudate is absorbed, generally no sequela.
Microscopic lesions mainly for serous inflammation.
lick the knee but bite the heart.
Involving the coronary arteries, renal artery, brain artery etc, small arteries see more.
Vascular wall connective tissue myxoid degeneration and fibrinoid necrosis. There can see Rheumatic
Granuloma, and later wall narrow even block, with thrombosis.
Rheumatoid coronary artery inflammation.
rheumatic arteritis
Mainly in acute period1 subcutaneous nodules ( hyperplasia ):
2 The annular erythema (exudative lesions) :
Appear on the extremities and the trunk skin. 1-2 days. Hyperemia, edema changes of the superficial layer of dermis. (pathognomonic )
Rheumatic disease of skin
Mainly involving the cerebral cortex, basal ganglia, thalamus and cerebellum cortex.Lesions to rheumatic arteritis and subcortical encephalitis. In 5-12 years old children, girls see more.
Rheumatic disease of brain
Infective endocarditis, one of the most serious of all infections, is characterized by colonization or invasion of the heart valves or the mural endocardium by a microbe, leading to the formation of bulky, friable vegetations composed of thrombotic debris and organisms, often associated with destruction of the underlying cardiac tissues.
Infective endocarditis
(IE)
Traditionally, IE has been classified on
clinical grounds into acute and subacute forms.
1. Acute IE
2. Subacute IE
1Acute IE :The strong pathogenic pyogenic bacteria( carbuncle, puerperal fever, osteomyelitis ) ---resistance down---bacteria into the blood---sepsis---normal endocardium ---invasion of mitral valve, aortic valve---acute septic endocarditis---bacterial vegetations
2Subacute IE: Streptococcus viridans (localized infection focus in vivo or iatrogenic infection)---- bacteria into the blood---the mitral valve or/and aortic valve with original lesions ( 80%, congenital heart disease, RHD or valve repair)-- Subacute IE--bacterial vegetations
Pathological change
In both the subacute and acute forms of the disease, friable, bulky, and potentially destructive vegetations containing fibrin, inflammatory cells, and bacteria or other organisms are present on the heart valves.
In the aortic opening a larger, irregular red vegetations, this mostly by Staphylococcus aureus infection.
Acute IE :Caused the distant organ septic infarction and abscess. Valve rupture, perforation, rupture of chordae tendineae, leading to chronic valvular heart disease. 50% died in days or weeks.
End and complications:1.Fever: it is the most consistent sign of IE. However, with
subacute disease, particularly in the elderly, fever may be slight or absent, and the only manifestations are sometimes nonspecific fatigue, loss of weight, and a flulike syndrome. In contrast, acute endocarditis has a stormy onset with rapidly developing fever, chills, weakness, and lassitude.
2.Arterial embolization ( 20%-40% ): embolism of 2.Arterial embolization ( 20%-40% ): embolism of brain ,heart, kidney, spleen, mesenteric, limbs and brain ,heart, kidney, spleen, mesenteric, limbs and pulmonary.pulmonary.
3.Chronic valvular disease
4.non-specific symptoms: Splenomegaly (15%-50% )AnemiaClubbing finger / toe
5. Peripheral symptoms
splinter or subungual splinter or subungual hemorrhageshemorrhages
Osler nodesOsler nodes
Janeway lesionsJaneway lesions
Roth spotsRoth spots
Peripheral symptoms
Peripheral symptoms: Micro vasculitis or micro thrombus
splinter or subungual Hemorrhages:petechiae, red, linear, or flame-shaped streaks in the nail bed of the digits
Janeway lesions: are small erythematous or hemorrhagic, macular, nontender lesions on the palms and soles and are the consequence of septic embolic events.
Osler nodesOsler nodes: are small, tender subcutaneous nodules that develop in the pulp of the digits or occasionally more proximally in the fingers and persist for hours to several days.
Subacute IE Acute IE
bacterial virulence
weak strong
valve Have lesions normal
Dry, crisp A larger, soft
vegetation Bacteria are less, little or no necrosis
Many bacteria, much necrosis
final result the vast majority of people heal
50% died in days or weeks.
Bacteria into the blood
ichorrhemia Sepsis
embolism Non-infectious infarction
Multiple embolic microabscesses
rheumatic endocarditis
Subacute IE
Etiology immunologically mediated
bacterial infection
grossly White, small, compact vegetations
gray red, large, loose vegetations, fall off
easily
microscopically white thrombus White thrombus with necrosis, colony etc.
clinical feature Valvular Disease Valvular heart disease, thromboembolism,
infarction, Septicemia
connection SIE often occurs on the basis of RE