Retinoblastoma
-
Upload
puneet-sharma -
Category
Health & Medicine
-
view
2.253 -
download
5
description
Transcript of Retinoblastoma

RETINOBLASTOMA Presented by-Dr.Puneet SharmaPost graduate student ( 2nd yr )Department of Ophthalmology
MMIMSR,MullanaAmbala

History Pawius described retinoblastoma in 1597. In 1809, wardop referred to tumor as fungus
haematodes as suggested enucleation as primary mode of management.
Discovery of ophthalmoscope in 1851 facilitated reconginition of clinical features of retinoblastoma.
Thought to be derived from glial cells, was called glioma of retina by virchow (1864).
Flexner (1891) and wintersteiner (1897) believed it to be a neuroepithelioma because of presence of rosettes.
Later, consensus was that tumor originated from retinoblasts and officially american ophthalmological society (1926) accepted the term retinoblastoma.

Introduction Most common intraocular malignancy in
children ( 1 in 15,000 to 1 in 18,000 live births).
No racial or gender predisposition.
Bilateral in 25 to 35% cases.
Age of diagnosis is 18 months.
Unilateral cases around 24 months & bilateral before 12 months.

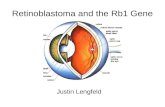
Genetics RB gene is located on long arm of
chromosome 13 (13q14) containing 27 exons & 26 introns.
2 normal copies of RB gene present in most human cells. RB gene product is 928 AA phosphoprotein whose normal func. is to suppress cell growth.
RB represents phenotypic expression of abnormal or absent tumour suppressor gene aka RB1.
Most RB1 mutations are minute deletions, duplications & point mutations.


Out of newly diagnosed cases
6% familial
94% sporadic
Bilateral RB involve germinal mutations
Approx. 15% unilateral sporadic RB caused by germinal mutation, affecting one eye , 85% sporadic

Genetic counselling
Imp. Aspect in management of RB
Pts, positive family history, 40% siblings would be at risk & 40% offspring of affected patient may develop RB
Pts, no family history, if affected child has unilateral RB, 1% of sibilings are at risk & 8% of offspring may develop RB
Bilateral RB, no family history 6% siblings & 40% offspring have chance of developing RB

Histopathology On low magnification, basophilic
areas of tumor are seen along with eosinophilic areas of necrosis & more basophilic areas of calcification within the tumor.
Poorly differentiated tumors consist of small to medium sized round cells with large hyperchromatic nuclei & scanty cytoplasm with mitotic figures.
Well defined tumor show Rosettes & Fleurettes,
.

Histopath. cut section

Rosettes Flexner-wintersteiner rosettes
consist of columnar cells arranged around a central lumen,highly characteristic of retinoblastoma, also seen in medulloepithelioma.

Homer wright rosettes, cells arranged around central neuromuscular
tangle (neuroblastomas, medulloblastomas & medulloepitheliomas)

Pseudo-rossettes
Arrangement of tumor cells around blood vessels.

Fleurettes Fleurettes -eosinophilic structures,
composed of tumor cells with pear shaped eosinophilic processes, projecting through fenestrated membrane.
Basophilic deposits,precipitated DNA (released from tumor necrosis) can be found in walls of lumen of blood vessels.

Classification of retinoblastoma
Reese-Ellsworth classification (1960)
Was designed for treatment with EBRT. Was in use till 1980
Now not used as EBRT has been replaced by chemotherapy as preferred mode of treatment

International classification of R.B.(shields)
Group A Small tumor
R.B < 3 mm in basal dimension/thickness
Group B Larger tumor
R.B > 3 mm in basal dimension/thickness
Macula location ( < 3 mm to foveola)
Juxtapapillary location ( < 1.5 mm to disc)
Clear subretinal fluid < 3 mm from margin

Group C Focal seeds
C1 Subretinal seeds < 3 mm from R.B
C2 Vitreous seeds < 3 mm from R.B
C3 Subretinal & vitreous seeds < 3 mm from R.B

Group D Diffuse seeds
D1 Subretinal seeds > 3 mm
D2 Vitreous seeds > 3mm
D3 Subretinal & vitreous seeds > 3 mm

Group E Extensive R.B
Occupying > 50% globe
Neovascular glaucoma
Opague media from haemorrhage in A.C & vitreous or subretinal space.
Invasion of postlaminar optic nerve, choroid (> 2 mm), sclera, orbit, A.C

Common presenting features ofR.B
Leucocoria 56% Strabismus 20% Red painful eye 7% Poor vision 5% Asymptomatic 3% Orbital cellulitis 3% Unilateral mydriasis 2% Heterochromia iridis 1% Hyphema 1%

Types of RB
Endophytic
Exophytic
Diffuse infiltrating tumor

Endophytic Tumor grows into vitreous cavity
yellow white mass
Progressively fills vitreous cavity &
vitreous seeds occur
Retinal vessels not seen on tumor surface

Vitreous seeding

Vitreous seeding

Exophytic
Tumor grows towards sclera Solid R.D usually occurs Retinal vessels seen on tumor surface

Diffuse infiltrating tumor Tumor diffusely involves retina
causing placoid thickness of retina (not mass)
Seen in older children

Grades of optic nerve involvement
Grade 1superficial involvement of optic nerve
head only
Grade 2 Involvement upto or involving lamina
cribrosa

Grade 3Involvement beyond lamina cribrosa
Grade 4Involvement upto surgical margin

Diagnosis
History
Prenatal/natal/postnatal Maternal rubella ( cong. Cat.) Gestation period or delivery ( ROP ) Oxygen therapy ( ROP )
Family history 6% of RB pts have positive family history

Physical examination
Rule out tuberous sclerosis, cong. defects asso. with trisomy 13-15, rubella syndrome
Ocular examination
Squint, leukocoria, heterochromia, proptosis, lymphadenopathy ( adv. cases )
pseudohypopyon, rubeosis iridis

Detailed Anterior segment examination
I O P
Indirect Ophthalmoscopy with Scleral indentation
Fundus drawing denoting site & extent
Gross systemic examination

Fundus drawing

Fully Dilated fundus examination
Bilateral with 360 degree scleral depression
Indirect ophthalmoscopy (diagnostic in 90%
cases)
Wide angle fundus camera ( Retcam)

RB on scleral indentation

U S G B-SCAN
rounded or irregular intraocular mass
representing typical intralesional calcification

3 D U S G

C T SCAN
delineates extraocular extension, can detect asso. Pinealoblastoma Cases with atypical manisfestations
Diagnostic dilemma Extraocular &intracranial tumor extension is suspected


M R I
optic nerve invasion or intracranial extension

M R I

F F A
Not required in routine work up.
Can be used to differentiate viable tumour from an avascular residue following radiotherapy or spontaneously regressed retinoblastoma.
Active lesion shows hypervascularity,dilated feeders and late staining

BIO-CHEMICAL TESTS
helpful in endophthalmitis like presentation
AQUEOUS HUMOUR ENZYME ASSAY
normal aqueous to plasma LDH >1.0
increased phosphoglucoisomerase levels
increased neuron specific enolase levels

Fine needle aspiration biopsy
Rarely done, invasive procedure
Approach through peripheral cornea, A/C, zonules, vitreous is recommended
Complication potential of needle track
dissemination of tumor cells

BONE MARROW BIOPSY & LUMBAR PUNCTURE
Useful in ruling out intracranial or distant spread as primary mode of spread of RB is hematogenous.
EXAMINATION OF SIBLINGS/PARENTS
To detect small lesions which may otherwise go undetected in siblings.
Parents may harbour regressed RB lesions. Blood specimens of patient/parents/siblings
should be taken for DNA analysis which could aid in genetic counselling.

To be continued.

D/D of leukocoria
Congenital cataract
10% of all vision loss in children world wide
prevalence of 1 to 6 cases per 10,000 live
births
cataract resulting from congenital rubella syndrome

PHPV
rare congenital developmental anomaly
purely anterior (
persistent tunica vasculosa lentis and persistent posterior fetal fibrovascular sheath of the lens)
purely posterior (falciform retinal septum) and a combination of both

Norrie disease
Genetic disorder (inherited X link recessive)
Features – shrinkage of globewasting of the iris30-50%have developmental
delay/mental retardationPsychotic like featuresBehavioral abnormalities

Coat’s diseaseVery rare, congenital non hereditary
eye disorder
Unilateral 6-8 years of age range ( 5 mnths to 71 yrs )Blood leaks from abnormal vessels in
back of the eye, leaving cholesterol deposits & damaging retina
RD, Glaucoma, Atrophy, Cataracts secondary to Coat’s.

ROP
Oxygen toxicity, relative hypoxia
Disorganized growth of retinal blood vessels ( scarring & RD )

Stage 1 is a faint demarcation line
Stage 2 is an elevated ridge
Stage 3 is extraretinal fibrovascular tissue
Stage 4 is sub-total retinal detachment
Stage 5 is total retinal detachment.

Toxocariasis
Uveitis
Endophthalmitis
Retinal dysplasia
Retinoma

Enucleation
Special considerations for enucleation in R.B Minimal manipulation Avoid perforation of eye Harvest long ( >15 mm) optic nerve
stump Inspect the enucleated eye for
macroscopic extraocular extension & optic nerve involvement
Harvest fresh tissue for genetic studies Place a primary implant Avoid biointegrated implant if
postoperative radiotherapy is necessary



Cryotherapy Equatorial & Peripheral retinal tumors
upto 4 mm in diameter & 2 mm in thickness.
Triple freeze thaw cryotherapy at 4-6 week interval until complete tumor regression.

Complications of Cryotherapy
Transient serous R.D
Retinal tear
Rhegmatogenous R.D

Laser photocoagulation Small post. tumors 4 mm basal
diameter & 2 mm in thickness.
Idea is too
Delimit tumor
Restrict blood supply to tumor by surrounding it with 2 rows of overlapping laser burns


Complications of L.P
Transient serous R.D
Retinal vascular occlusion
Retinal hole
Retinal traction
Preretinal fibrosis
Large visual field defect ( tumor in juxtapapillary area)

Contraindication in L.P
Pt on active chemoreduction protocol, restricts blood supply to tumor & reduces intraocular concentration of chemotherapeutic agent

Systemic chemotherapy
Day 1: vincristine + Etoposide + Carboplatin
Day 2: Etoposide
Standard dose: (3 weekly, 6 cycles): Vincristine 1.5 mg/m2 (0.05 mg/kg for children < 36 mnths of age & maximum dose < 2 mg), Etoposide 150 mg/m2 (5 mg/kg for children < 36 mnths of age ), Carboplatin 560 mg/m2 (18.6 mg/kg for children < 36 mnths of age)
High – dose (3 weekly, 6-12 cycles) : Vincristine 0.025 mg/kg, Etoposide 12 mg/kg, Carboplatin 28 mg/kg




Thermotherapy Focused heat generated by infrared
radiation, applied to tissues at subphotocoagulation levels to induce tumor cell apoptosis.
Achieve slow & sustained ( 40 to 60 degree C) within tumor, sparing retinal vessels.
Transpupillary thermotherapy using infrared radiation from semiconductor diode laser delivered (1300 micron large spot indirect ophthalmoscope, operating microscope, transscleral route with diopexy probe).

Tumor heated till it turns gray Satisfactory control for small
tumors(4 mm basal diam. & 2 mm thickness).
Complete tumor regression 85% (3-4 sessions)

Complication of Thermotherapy
Focal iris atrophy
Focal paraxial lens opacity (minimised using 1300 micron indirect ophthalmoscope, duration 5 mins in single session)
Retinal traction
Serous R.D

Plaque Brachytherapy
Placement of radioactive implant on sclera corresponding to base of tumor,transsclerally irradiate tumor.
Radioactive materials – Ruthenium 106 & Iodine 125
Tumors < 16mm basal diameter & < 8 mm thickness
Primary or Secondary Primary- chemotherapy is
contraindicated, secondary treatment in eyes that fail to respond to chemoreduction & external beam radiotherapy or tumor recurrences.


Tumor thickness measured by ultrasonography
Plaque design depending on basal tumor dimensions, its location & configuration e.g notched plaque used to protect optic nerve ( tumors peripapillary in location)
Dose – 4000 – 5000 cGy
Plaque sutured to sclera after tumor centration & left for duration of exposure (ranging 36 to 72 hrs)
90% tumor control


Regressed RB after exposure to iodine 125

Advantages of P.B
Focal delivering of radiation, minimal damage to surrounding normal structures
Minimal periorbital tissue damage
Cosmetic abnormality absent, retarded bone growth in field of irradiation ( as in external beam radiotherapy )
Reduced risk of second malignant neoplasm
Shorter duration of treatment

Complications of P.B
Radiation papillopathy
Radiation retinopathy

External beam radiotherapy
Used less often, newer chemotherapy protocols
Indicated- primary chemotherapy & local therapy has failed or rarely chemotherapy is contraindicated.
Delivered using Cobalt 60 (gamma rays) or linear accelerator ( X-rays)
Linear accelerator with multi-beam technique, image guided radiotherapy & stereotactic radiotherapy, better treatment accuracy.


EBRT

RB AFTER EBRT

Complication of EBRT
Stunting of orbital growth Dry eye Cataract Radiation retinopathy Optic neuropathy Second malignant neoplasms (hereditary
form of retinoblastoma) 30% chance of another malignancy by
30 yrs Risk of second malignant neoplasm
greater in children under 12 mnths

Orbital implants
Buried
Non-buried

Buried implants
Better cosmosis & safety
Materials used- plastic, silicone & hydroxyappatite ( currently recommended )

Non- buried implants
have problems of -
migration
extention
infection

Orbital Retinoblastoma
Rare in developed countries Common in developing countries In Mexico, 18% of 500 pts presented
with orbital RB Taiwanese group, 36% (42 of 116)
pts manifested orbital RB In Nepal, incidence is higher 40% (19
of 43) with proptosis being most common manifestation of RB

Clinical manifestations of orbital RB
Primary orbital RB- clinical or radiologically
detected orbital extension of intraocular RB at
initial clinical presentation with or without
proptosis or fungating mass.
Silent proptosis without orbital & periocular inflammation in pt will manifest intraocular tumour,with inflammation indicates reactive sterile orbital cellulitis sec. to intraocular tumor necrosis.

Secondary orbital RB-
recurrence following uncomplicated
enucleation for intraocular RB.
Unexplained displacement, bulge or extrusion of previously well fitting conformer or prosthesis is an ominous finding sugg. of orbital recurrence


Accidental orbital RB-
Inadvertent perforation
Fine-needle aspiration biopsy
Intraocular surgery with unsuspected intraocular RB


Overt orbital RB
Unrecognized extrascleral or optic n. extension discovered during enucleation.
Pale pink to cherry red episcleral nodule (juxtapapillary location or at site of vortex v.)
Enlarged and inelastic optic n. with or without nodular optic n. sheath is an indicator of optic n. extension.

Microscopic orbital RB
Detection of full thickness scleral infiltration, extra scleral extension & invasion of optic n. on histopathologic evaluation on enucleated eye
Tumor cells in choroidal & scleral emissaria & optic n. sheath indicates orbital extension.

Diagnosis
General physical examination- includes regional lymph nodes palpation
MRI or CT Scan of orbit & brain (axial & coronal orientation)
FNAC Chest X-RAY USG abdomen Bone marrow biopsy CSF cytology

Treatment of orbital RB
Combination therapy more effective
Vincristine, Etoposide, Carboplatin high dose chemotherapy (3-6 cycles or even 12 cycles) followed by enucleation, extended enucleation or orbital exenteration