Research Report - Chris O'Brien Lifehouse · 2020-02-20 · At any one time, there are more than...
Transcript of Research Report - Chris O'Brien Lifehouse · 2020-02-20 · At any one time, there are more than...
At any one time, there are more than 100
clinical trials being undertaken by or in
collaboration with our researchers and
clinicians.
Research courses through every department
of Chris O'Brien Lifehouse, from medical
oncology and radiation oncology, to surgery,
nursing, and complementary therapies.
Not only does Chris O'Brien Lifehouse
emphasise continual interaction between
clinicians and researchers to drive standards
of care forward, in many cases the treating
clinician and researcher are one and the
same, eliminating the gap between lab and
clinic altogether.
This report summarises research highlights
from our programs and departments for years
2017 and 2018.
Never to be forgotten are the people behind
this data: real patients and families. The
ultimate benchmarks by which we measure
ourselves are how their lives are improved.
Clinical excellence underpinned by research.
This has always been at the heart of the vision
for Chris O'Brien Lifehouse.
The comprehensive cancer centre model is
internationally accepted as the organisational
setting most likely to generate clinical and
research advantage. It is defined by integrated
co-location of services, contribution to
education and research output.
In 2007, Professor Chris O'Brien AO said, "With
a modern comprehensive cancer centre where
clinical care and research are integrated, and
where treatment is underpinned and, indeed,
driven by research, we are entering a new
era."
We now live in that era.
Today, Chris O'Brien Lifehouse is the largest cancer clinical trials unit in NSW.
Foreword
4
6 20Introduction Research Highlights
22 Medical Oncology
24 Head and Neck
28 Radiation Oncology
31 Gynaecological Oncology
33 Breast
35 Neurosurgery
37 Uro-Oncology
38 Supportive Care and Integrative Medicine
40 Affiliates
8 Message from the CEO
10 Message from the Director of Research
12 Research Snapshots
13 Collaborative Network
14 Research Committee
15 In Focus
CHRIS O'BRIEN LIFEHOUSE
5
44 70
Contents
Publications Grants
72 Medical Oncology
74 Head and Neck
75 Radiation Oncology
75 Gynaecological Oncology
76 Breast
76 Supportive Care and Integrative Medicine
46 Medical Oncology
59 Head and Neck
63 Radiation Oncology
66 Gynaecological Oncology
67 Breast
67 Uro-Oncology
68 Supportive Care and Integrative Medicine
RESEARCH REPORT 2017 & 2018
The third point is impact. Chris O'Brien
Lifehouse has participated in — and led
— research that has changed practice and
changed lives.
Our medical oncologists have presented globally and had stakes in some of the most exciting developments in cancer treatment in recent years.
In a hugely significant development, Professor
Michael Boyer AM, our Chief Clinical Officer,
was a co-author in a global study that has
made immunotherapy part of standard
care in lung cancer treatment.
Associate Professor Peter Grimison, one of
our senior medical oncologists, is leading
the world's largest and most definitive
trial of medicinal cannabis' feasibility,
effectiveness and consequences in alleviating
the debilitating side-effects of chemotherapy.
So, what lies ahead for Chris O'Brien
Lifehouse research? In order to achieve
significant impact, we must continue to
reach beyond our own circles and work
actively and collaboratively with partners.
Looking back at the clinical trials that came
across my desk for approval throughout 2017
and 2018, research at Chris O'Brien Lifehouse
has evolved in three critical ways.
The first is sheer quantity. Our clinical trials
program has rapidly expanded. The most
recent data from Cancer Institute NSW's
Cancer Clinical Trials Portal shows Chris
O'Brien Lifehouse has the most cancer clinical
trials in NSW.
This is a testament to the energy and
dedication of our clinicians, researchers and
leaders. It also shows that while we may be a
young organisation (2018 marked five years
of operation), we have become a valuable
contributor to the Australian cancer network.
An evidence-based approach is essential as
we continue to build in both substance and
reputation.
The second way our research has evolved is
in breadth and scope, as various departments
have grown their research programs and
output. There are more strong studies
coming out of our Radiation Oncology and
surgical departments such as Head and
Neck. This can partly be attributed to the
investments in technology that we have made
in the last few years. Our departments of Uro-
Oncology and Neurosurgery have started
their own programs and we look forward to
their results in future years.
Message from the CEOEileen Hannagan
CHRIS O'BRIEN LIFEHOUSE
8
'A core part of our mission is finding the answers that will make it easier to treat, and cure, people with cancer tomorrow. It is just part of what we do.'- Professor Michael Boyer AM, Chief Clinical Officer
We are committed to strengthening our
relationships and networks throughout the
precinct, the country and internationally.
Research is pivotal to the Chris O'Brien
Lifehouse vision. From the design of the
building, to the way departments are
organised, to the professional development
and mentoring of staff, we are determined to
break partitions wherever possible, in order to
encourage relationships, propagate ideas, and
give science the opportunity to flourish.
9
RESEARCH REPORT 2017 & 2018
Chris O'Brien Lifehouse celebrated a major
milestone in November 2018: five years of
operation. As the clinical service grows and
diversifies, so too does the research program.
Two new departments — Uro-Oncology and
Neuro-Oncology — have launched research
programs in the last year.
This Research Report, covering 2017 and
2018, demonstrates the depth of research
within the cancer centre and its collaborative
network with over 250 publications, more
than 200 national and international
Message from the Director of ResearchProfessor Lisa Horvath
presentations, more than 70 grants and 62
research students (undergraduate, Masters
and PhD).
This should be read as a collaborative
report. Chris O'Brien Lifehouse researchers
have many roles, often numerous affiliations
and do their research as part of networks.
The annual Chris O'Brien Lifehouse Research
Symposia are attracting a range of speakers
and poster presenters from within Lifehouse
and our collaborative network across the
CHRIS O'BRIEN LIFEHOUSE
10
spectrum of cancer treatment including
surgery, medical oncology, radiation oncology
and molecular pathology.
In 2018, the symposium celebrated the 40-
year career of Professor Martin Tattersall,
who has influenced many areas of cancer
therapy across sarcoma, breast cancer, ovari-
an cancer and cancer survivorship.
We also held our first Lifehouse Concept De-
velopment workshop in conjunction with the
NHMRC Clinical Trials Centre with more than
20 concept participants including doctors,
nurses and allied health researchers.
A key aspect of the Chris O'Brien Lifehouse
research agenda is patient-focused research,
especially that which changes clinical practice.
Our researchers have been part of a wide range of practice-changing studies.
These include immunotherapy in metastatic
lung cancer, extracorporeal radiotherapy
for sarcomas, improved patient decision-
making in cancer therapy, pre-operative
dietary improvements for surgery and
techniques to address fear of cancer
recurrence.
The research has spanned clinical trials
(phase 1-3), biomarkers, supportive cancer,
surgical techniques, quality of life and can-
cer outcomes.
Collaboration remains the cornerstone of Chris O'Brien Lifehouse research. Our Head and Neck Cancer Research Group
continues to expand their network nationally
and internationally to address this uncommon
cancer. Chris O'Brien Lifehouse is now part of
brain cancer research alliances and sarcoma
research networks.
The national cancer co-operative clinical trials
groups remain important research partners
across genito-urinary cancers (ANZUP), breast
cancer (BCT), gynae cancers (ANZGOG), sar-
coma (ASSG), brain cancer (COGNO), gastro-
intestinal cancers (AGITG), lung cancer (ALTG)
and radiation therapy (TROG).
The NSW Early Phase Clinical Trials Alliance
(NECTA) was established three years ago with
Chris O'Brien Lifehouse, The Kinghorn Can-
cer Centre and Scientia Clinical Research and
aimed to grow the early phase clinical trial
portfolio in NSW. NECTA now has 6 active sites
across metropolitan and regional NSW with
more than 50 active Phase 1 trials across the
network.
11
RESEARCH REPORT 2017 & 2018
12
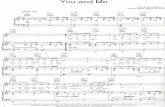
Research Snapshots
2017 2018
200
400
600
Number of Phase 1-3 studies across cancer tumour streams
(2017-18)
Number of participants on clinical trials across cancer
tumour streams (2018)
Number of participants by Phase
Phase 1
Phase 2
Phase 3
Phase 1
Phase 2
Phase 3
Other
CHRIS O'BRIEN LIFEHOUSE
13
* Collaborative networks include:
University of Sydney: NHMRC Clinical Trial Centre, Cancer Nursing Research Unit, The Psycho-oncology Co-operative Research Group (PoCoG), The Centre for Medical Psychology & Evidence-Based Decision-Making (CeMPED), Surgical Outcomes Research Centre (SOuRCe).
Research Institutes: Garvan Institute of Medical Research, The Centenary Institute, Asbestos Diseases Research Institute (ADRI), Charles Perkins Centre, The ANZAC Research Institute, Melanoma Institute of Australia, The Institute for Glycomics, The South Australian Health and Medical Research Institute (SAHMRI).
Other Cancer Centres and Hospitals: Concord Repatriation General Hospital - Concord Cancer Centre, St Vincent's Hospital Sydney - The Kinghorn Cancer Centre, Westmead Hospital - The Crown Princess Mary Cancer Centre Westmead, Royal North Shore Hospital - Northern
University ofSydney*
RPA Institute ofAcademicSurgery
Royal PrinceAlfred Hospital
RPA Institute of Academic
Surgery
Pharma / Biotec
ResearchInstitutes*
National CancerConsortia*
Sydney HealthPartners
SydneyCatalyst
Other CancerCentres*
Collaborative Network
Sydney Cancer Centre, Prince of Wales Hospital - Nelune Comprehensive Cancer Centre, Coffs Harbour Health Campus, Mid North Coast Cancer Institute (MNCCI), John Hunter Hospital, Calvary Mater Newcastle, Peter MacCallum Cancer Centre, The Royal Melbourne Hospital, Monash Health, Princess Alexandra Hospital Brisbane. Internationally, Dana-Farber Cancer Institute Boston, University of Southern California (USC).
National Cancer Consortia: Australasian Gastro-Intestinal Trials Group (AGITG), Australia and New Zealand Breast Cancer Trials Group (ANZBCTG), Australian and New Zealand Urogenital and Prostate Cancer Trials Group (ANZUP), Australia New Zealand Gynaecological Oncology Group (ANZGOG), Australasian Sarcoma Study Group (ASSG), Trans-Tasman Radiation Oncology Group (TROG).
RESEARCH REPORT 2017 & 2018
Rebecca Davies, Board Director, Chris O'Brien Lifehouse
Lisa Horvath, Director of Research, Chris O'Brien Lifehouse (Chair)
Michael Boyer, Clinical Director, Chris O'Brien Lifehouse
Christopher Milross, Director of Radiation Oncology, Chris O'Brien Lifehouse
Jonathan Carter, Director of Gynae Oncology, Chris O'Brien Lifehouse
Sam Saidi, Gynae Oncology, Chris O'Brien Lifehouse
Jonathan Clark, Head and Neck Surgery, Chris O'Brien Lifehouse
Michael Elliott, Head and Neck Surgery, Chris O'Brien Lifehouse
Sanjay Warrier, Breast Surgery, Chris O'Brien Lifehouse
Christopher Young, Head of Colorectal Surgery, Royal Prince Alfred Hospital
Paul Stalley, Program Director Surgery/ Head of Sarcoma, Sydney Local Health District
Charbel Sandroussi, Director of Clinical Research, RPA Institute of Academic Surgery
Paul Bannon, Head of Cardiothoracic Research, Royal Prince Alfred Hospital
Stephen Larsen, Institute of Haematology Research Unit, Royal Prince Alfred Hospital
John Boulas, Head of Urology Department, Royal Prince Alfred Hospital
James Kench, Head of Department, Tissue Pathology and Diagnostic Oncology,
Royal Prince Alfred Hospital
John Simes, Director, NHMRC Clinical Trials Centre
Martin Stockler, Co-Director, Cancer NHMRC CTC
Kate White, Chair, Cancer Nursing Research Unit
Phyllis Butow, Co-Director, CeMPED The University of Sydney
Michael Solomon, Co-Chair, RPA Institute of Academic Surgery
Julie Charlton, Research Governance Manager, Chris O'Brien Lifehouse
Jacquie Harvey, Business Manager, Clinical Trials, Chris O'Brien Lifehouse
Brindha Shivalingham, Director of Neurosurgery, The Chris O'Brien Lifehouse
Natalka Suchowerska, Head of Physics Research and Education, Chris O'Brien Lifehouse
Toni Lindsay, Allied Health Manager, Chris O'Brien Lifehouse
Steven Kao, Thoracic Oncology Research lead, Chris O'Brien Lifehouse
Jane Young, Research Director, RPA Institute of Academic Surgery
David Gattas, Research Lead ICU, Chris O'Brien Lifehouse
Lyndal Trevena, The University of Sydney Professor of Primary Health Care
Bev Noble, Partnership Advisory Council, Chris O'Brien Lifehouse
Sarah Charlton Li, Research Program Manager, Chris O'Brien Lifehouse
Trevor Tejada-Berges, Gynae Oncology, Chris O'Brien Lifehouse
MacDonald Christie, Associate Dean (Research), Sydney Medical School and
NHMRC Senior Principal Research Fellow
Martin Butson, Principal Medical Physics Specialist, Chris O'Brien Lifehouse
Leanne Hodgkiss, Trusts and Foundations, Chris O'Brien Lifehouse
Henry Woo, Director of Urology and Head of Robotics, Chris O'Brien Lifehouse
Carsten Palme, Director of Head and Neck Surgery, Chris O'Brien Lifehouse
Research Committee
CHRIS O'BRIEN LIFEHOUSE
14
15
In FocusMeet Our Researchers
Associate Professor Peter GrimisonAssociate Professor Peter Grimison is a senior
medical oncologist. His clinical work focuses on
testicular cancer, sarcoma and upper gastro-
intestinal cancers. He is a leader in producing
high-quality research through clinical trials,
especially in matters of patient quality of life
and cost-effectiveness of treatment.
MEDICINAL CANNABIS TRIAL
Nausea and vomiting are notorious side-
effects of chemotherapy. For many, these
symptoms are alleviated with advanced anti-
nausea drugs but for a small group of patients,
they persist.
The medicinal cannabis trial is aimed at
testing whether it is feasible and effective
to administer medicinal cannabis for these
patients, and what side effects, if any, it
may cause. Professor Grimison says this trial is
an opportunity to create reliable evidence
in an area of acute community demand. Up
until now, this area has had limited scientific
understanding.
"Presently, doctors in Australia can prescribe
medicinal cannabis, but without sufficient ev-
idence and understanding of its side effects,
Associate Professor Peter Grimison (right).
RESEARCH REPORT 2017 & 2018
there is still a reluctance to do so," Professor
Grimison said.
"My hope is that this study will provide the
kind of evidence which will allow doctors to
make that decision, and also to know whether
the treatment will be cost-effective."
"The way we are administering the cannabis
treatment is quite novel. Traditionally, pa-
tients who buy cannabis for medicinal needs
will smoke it, or more recently use a vaporiz-
er or an oil. These methods are not practical
in a chemotherapy suite, so we are trialling a
unique oral capsule. If we can show that the
capsule is safe and effective, then it will hope-
fully be easier for patients and doctors to use."
This will be the largest and most definitive trial of its kind in the world.
The first part of the trial is currently recruiting
across 11 cancer centres in NSW, including
Chris O'Brien Lifehouse.
GERM CELL TUMOURS
Professor Grimison's areas of interest extend to
testicular cancer and related cancers known
as germ cell tumours.
Testicular cancer is a disease that dispropor-
tionately affects young men aged between 15
and 40 years old. Most people with testicular
cancer are cured, but a small number are not.
"We are interested in improving treatment for
this group," Professor Grimison said.
Working with the Australian and New Zealand
Urogenital and Prostate Cancer Trials Group
(ANZUP), based at the NHMRC Clinical Trials
Centre at University of Sydney, co-located at
Chris O'Brien Lifehouse, Professor Grimison is
testing the delivery of standard chemotherapy
treatment in a different way.
"It's an important trial in a number of ways,"
he said. "It is recruiting from four different
countries; it's recruiting in both adults and
children; and it's recruiting in men and wom-
en."
"Most trials will focus on only one of these
groups, but germ cell tumours cross over.
They are present in males, females, young and
old. Not only will the phase 3 accelerated BEP
study allow us to test the drug schedule in all
of these groups, but it allows us to form the
kind of cross-national collaborations which will
enable us to do better research in the future."
Nurse Practitioner Justine OatesNurse Practitioner Justine Oates works
alongside Nurse Practitioner Sarah Davies in
the Head and Neck service of Chris O'Brien
Lifehouse. They are leaders in promoting an
evidence-based approach to nursing, using
a research framework to evolve practice and
improve patient quality of life.
In an example of research underpinning
nursing and patient care, Nurse Practitioner
Oates led a retrospective review of head and
neck microvascular free flap surgical out-
comes.
The study was initiated after the clinical
governance board noted head and neck
surgical patients represented a large
proportion of patients who returned to theatre
postoperatively.
16
CHRIS O'BRIEN LIFEHOUSE
17
'We wanted to find out if there was something we could improve here.'"Or are there systems in place that aren't
working to the best of their ability?" Ms Oates
said.
"A retrospective review over a two-year period
from 2017 to 2018 was conducted involving
a comprehensive assessment of each case,
responsiveness to the deteriorating patient
and evaluation of outcomes to further identify
causal factors, current clinical practice and
opportunities for improvement."
The study showed positive outcomes in all
areas. The volume of complex surgeries was
extremely large; incidence of microvascular
free flap failure was below international
benchmarks; the response time to re-
exploration was impressive at less than 3.5
hours, 24/7.
"They're really positive outcomes for high
volume, high complexity patients with high
co-morbidities," Ms Oates said.
"Through this study, we recognised the need
for a formal guideline for critical information
and escalation of free flap management.
So while there were clear communication
pathways for the escalation of a deteriorating
patient, we're now formalising a pathway for
escalation management."
Nurse Practitioner Justine Oates.
RESEARCH REPORT 2017 & 2018
Tony PorterTony Porter's perspective on clinical trials and
the opportunity to take part in them is deeply
personal, saying "it means the world" to him.
Mr Porter was active and healthy — a keen
cyclist, boxing class instructor, even a triathlon
and Iron Man competitor — when he was
diagnosed with melanoma.
He underwent treatment and it was believed
to be successful until a routine scan in 2017
showed what had first presented as melanoma
was in fact a rare form of soft tissue sarcoma.
Mr Porter had five tumours throughout his
body — in his neck, lungs and hamstring.
"I had trouble walking upstairs, I was coughing
up blood… I was in a fair bit of trouble," he
said. Despite chemotherapy treatment, the
cancer continued to grow.
"They gave me three options. Two of them
were more chemo, and the third was a clinical
trial. I took that option."
Mr Porter enrolled in a trial for INCMGA00012
— a type of immunotherapy. The drug is a
PD-1 inhibitor, which increases the body's im-
mune reaction to the cancer.
"I had read a fair bit about immunotherapy.
The very first day I met Professor Tattersall, I
asked him about it, and he helped to find the
trial," Mr Porter said. "The tumour on my neck
was gone after about three treatments. I now
have scans every three months, and every scan
has shown that the tumours have shrunk."
Mr Porter continues fortnightly treatment,
overseen by oncologist Dr Vivek Bhadri, who is
the study's principal investigator since Profes-
sor Tattersall's retirement.
"I'm appreciative of the opportunity to be on
a trial," Mr Porter said.
'It means the world, because I probably wouldn't be here without it.'
Flavio RoncolatoIn December 2018, Flavio Roncolato was to
undergo a parotidectomy to remove a pea-
sized lump under the corner of his jaw.
Surgery of the parotid gland is particularly
complicated because the facial nerve courses
through the gland. Nearly half of all patients
who undergo a parotidectomy experience
Patient ImpactIn Focus
18
CHRIS O'BRIEN LIFEHOUSE
19
moderate to severe nerve dysfunction
afterwards.
Mr Roncolato's surgeon, Professor Jonathan
Clark AM, suggested that Mr Roncolato take
part in a trial aimed at reducing the risk
of infection and problems with swelling,
numbness, and loss of movement.
"It was Professor Clark who suggested the
clinical trial, and I said yeah, no problem. It
can't hurt, just do it," Mr Roncolato said.
During surgery, Professor Clark coated Mr
Roncolato's exposed facial nerve with a
solution of corticosteroid dexamethasone in a
slow release hyaluronic acid gel.
"Considering what they did in surgery, my
recovery [was] great," Mr Roncolato said. "I
[could] eat, I had very little pain – in fact, it was
more a slight discomfort," Mr Roncolato said.
"I think that having clinical trials of any sort
in a hospital just shows that the facility that
you're at is probably pushing boundaries, and
the doctors who want to push those bounda-
ries are generally the better doctors."
'In my mind, that's what you would expect of a good researcher – they're out there looking for the next best thing.'"They're not just sitting there saying 'well this
is the way we've always done it'."
Above, Tony Porter. Right, Flavio Roncolato.
RESEARCH REPORT 2017 & 2018
22
* Includes co-publications with other Chris O'Brien Lifehouse departments
novel TargomiR, a miRNA drug developed in
Australia to target malignant mesothelioma
(Lancet Oncology).
The study of TargomiR represents a highly
successful collaboration between the Asbestos
Diseases Research Institute (University of
Sydney), industry (Engeneic) and clinicians
(Chris O'Brien Lifehouse, Concord Hospital
and Royal North Shore Hospital).
Among the Phase 3 studies, our team have been
involved in studies that have contributed to
the registration of immunotherapy agents
HighlightsThe Medical Oncology department has
excelled in research over the last two years
with more than 160 publications across a
wide range of research areas including clinical
trials, biomarkers, cancer biology, health
economics and quality of life.
The members of our department have
recruited patients to more than 100 clinical
trials (Phase 1-3 trials) and contributed to 41
clinical trial publications in the same period.
These include first-in-human studies of a
novel EGFR inhibitor to treat CNS metastases
from lung cancer, a MET inhibitor and the
Department List Prof Lisa Horvath MBBS FRACP PhD (Director of Medical Oncology)
A/Prof Philip Beale MBBS FRACP PhD
A/Prof Jane Beith MBBS FRACP PhD
Dr Vivek Bhadri MBBS FRACP PhD
Prof Michael Boyer AM MBBS FRACP PhD
A/Prof Peter Grimison MBBS FRACP PhD
Dr Michelle Harrison BSc (Med) MBBS FRACP
Dr Mun Hui MBBS FRACP PhD
Dr Steven Kao MBBS FRACP PhD
Dr Jenny Lee MBBS FRACP
Dr Yeh Chen Lee MBBS BMedSci FRACP
Dr Kate Mahon MBBS FRACP PhD
A/Prof Catriona McNeil MBBS FRACP PhD
Dr Hao-Wen Sim MBBS(Hons) BMedSci FRACP
Prof John Simes BSc (Med) MBBS FRACP SM MD
DepartmentsMedical Oncology
Summary By Numbers
165* publications
59 presentations
7 students
39 grants
Prof Martin Stockler MBBS FRACP MSc (Clin Epi)
Prof Martin Tattersall AO MBBS FRACP PhD
Prof David Thomas MBBS FRACP PhD
Dr Alison Zhang MBBS FRACP
CHRIS O'BRIEN LIFEHOUSE
23
in which it was confirmed that a blood marker,
mGTSP1, predicts outcomes after Docetaxel
chemotherapy in men with metastatic
castrate resistant prostate cancer. This marker
may accelerate future clinical trials of new
therapies and be useful in the clinic to guide
treatment decisions. This paper was the
subject of an editorial in the journal European
Urology.
Postgraduate students are essential to the
progress of research. They produce high-
quality research and become part of the next
generation of clinician scientists who bridge
the gap between the lab and the clinic.
Two of our new consultants (Dr Mun Hui and
Dr Alison Zhang) have completed their PhD
studies over the last two years and produced
outstanding papers as part of this. Dr Mun
Hui has been studying aggressive triple
negative breast cancer and published a
study identifying Hedgehog signaling as a key
driver of cross-talk between cancer cells and
stromal cells driving chemoresistance (Nature
Communications).
This raises exciting possibilities for therapeutic strategies in advanced breast cancer.
Dr Alison Zhang published a prospective
multicentre phase 3 validation study of
AZGP1, a tissue biomarker which can
predict outcomes after surgery for localised
prostate cancer (Annals of Oncology).
This study provides robust evidence for the
incorporation of this biomarker into clinical
practice.
as standard of care in melanoma and non-
small cell lung cancer. Professor Michael
Boyer AM was a co-author in a global
study that identified the immunotherapy,
Pembrolizumab, added to chemotherapy
improves survival in patients with newly
diagnosed non-small cell lung cancer (New
England Journal of Medicine).
This study has resulted in immunotherapy with chemotherapy as a new standard of care for lung cancer.
In addition, we have contributed to
randomised trials of exercise in advanced
lung cancer and psychosocial interventions
to address patients' fear of cancer
recurrence. Associate Professor Jane Beith was
part of a collaborative team that completed a
randomised controlled trial of ConquerFear,
a psychological intervention to treat the fear
of cancer recurrence. The anxiety and distress
associated with fear of cancer recurrence is
a substantial problem for patients and this is
one of the first psycho-oncology treatments
to improve patients' quality of life (Psycho-
oncology).
Several of the members of the Medical
Oncology department are clinician scientists
with research interests crossing biomarkers
and cancer biology. More than 20 papers
have been published on new biomarkers
to potentially direct cancer therapy in the
future.
These included two Phase 3 studies of
new biomarkers to guide treatment of
prostate cancer. Dr Kate Mahon led a study
RESEARCH REPORT 2017 & 2018
24
* Includes co-publications with other Chris O'Brien Lifehouse departments
Dr Ilias Kotranakis MBBS (Hons) FRACS
Dr Arjuna Ananda MBBS FRACS
Dr Raewyn Campbell FRACS BMed (Hons) BAppSc(Physio) Grad Dip (Ex Sport Sc)
Dr Glen Croxson MBBS FRACS
A/Prof Alexander Saxby MB BChir MA (Hons) (Cantab.) FRACS
Dr Phaethon Karagiannis MBBS MPH
A/Prof Jonathan Kong FRACS FRCS MBBS AMusA
A/Prof Payal Mukherjee MBBS FRACS MS
Dr Eileen Tan-Gore MBBS MDSc FRACDS
Our current research priorities are advanced
and metastatic cutaneous squamous cell
carcinoma, investigating the rising incidence
of oral cancer (particularly in young patients
who have never smoked), aggressive salivary
Department List A/Prof Carsten Palme MBBS FRACS (Director)
Prof Jonathan Clark MBBS (Hons 1) BSc (Med) MBiostat FRACS (Head of Research)
Dr James Wykes Sci (Med) MBBS (Hons) FRACS (Head of Fellowship program)
Dr David Leinkram MBBS, FRACDS (OMS) BDSc
Dr Hubert Low MBBS BSc (Med) (Hons) FRACS
A/Prof Sydney Ch'ng MBBS FRACS PhD
Dr Anthony Clifford MBBS FRACS
Dr Kerwin Shannon MBBS FRACS
A/Prof Michael Elliott MBBS MPhil FRACS
Dr Bruce Ashford MBBS FRACS BDSc (Hons)
Nurse Practitioner Sarah Davies NP, RN, BN (UTS) MN (NP) (Sydney)
Nurse Practitioner Justine Oates NP, RN
Dr Lydia Lim BDS (Hons) FRACDS MDSc FRACDS (OMS)
Dr John McGuinness BDS(Hons) FDS RCS MBChB FRCS(ORL-HNS) FRACS
Dr Daniel Novakovic MBBS FRACS MPH
A/Prof Mark Schrifter BDS MDSc M SND RCSEd M Oral M RCSEd FFD RCSI FRACDS
Dr Jasvir Singh BDS MBBS D ClinDen (OMS) FRACDS (OMS)
Dr Sue-Ching Yeoh BDS (Hons) MDSc FRACDS FRACDS FOMAA FICD
Head and Neck
Summary By Numbers
59* publications
28 presentations
20 students
27 grants
HighlightsThe last two years have been highly productive
for the Sydney Head and Neck Cancer Institute
(SHNCI), which is the research organisation of
the Head and Neck service at Chris O'Brien
Lifehouse.
CHRIS O'BRIEN LIFEHOUSE
25
cancer cells. They observed an enrichment
of SOX9 at drug-induced H3K27ac sites,
suggesting tumour evolution could be driven
by stem cell-switch-mediated epigenetic
plasticity. Importantly, JQ1 mediated
inhibition of BRD4 could reverse drug-induced
adaptation. These results provide insights
into the modes of therapy-induced cellular
plasticity and underscore the use of epigenetic
inhibitors in targeting tumour progression.
Cutaneous squamous cell carcinoma is a
common cancer that most often occurs in
the head and neck. Its underlying genetic
mechanisms are poorly understood. Through
targeted sequencing of 48 clinically relevant
genes, researchers gained insights into
somatic mutations in non-metastatic high-
risk head and neck cutaneous squamous cell
carcinoma.
This has led to the identification of potential therapeutic targets. In particular, alterations in FGFR2 and
NOTCH1, which may have roles in local and
distant disease progression.
Working with the Department of Radiation
Oncology on a multi-institutional survey,
researchers aimed to characterise the
experiences and unmet needs of patients
with head and neck cancer with regard
to information and support provision.
While patients were largely satisfied with the
information received about disease process,
prognosis and treatment, they reported
receiving only minimal information related
to stress and anxiety, including such topics
as psychological well-being, patient support
groups, and psychosexual health. Verbal
gland cancers, reconstructive approaches to
assist patients with advanced facial cancers
and facial paralysis, and patient education for
head and neck cancer.
The Head and Neck service at Chris O'Brien
Lifehouse performs the largest number of
head and neck cancer surgeries in NSW,
with more resections than the next two
busiest hospitals combined. (See Graph A).
This high volume of patients generates invaluable data. We hold the largest head and neck patient research database and biobank in Australia, with more than 14,000 registered patients.
This data has contributed to important
developments in research.
In a study of somatic mutations in salivary
duct carcinoma (a rare, highly aggressive
cancer with limited therapeutic options for
disseminated disease), multiple mutations
were identified, some of which are responsive
to drugs while others are resistant to
treatments currently under investigation.
These findings emphasise the need to develop
complementary biomarker and treatment
strategies for salivary duct carcinomas.
Chemo-resistance is one of the major causes
of cancer-related deaths. Using single-cell
transcriptomics, researchers investigated
divergent modes of chemo-resistance in
RESEARCH REPORT 2017 & 2018
26
communication needs to be reinforced by
accessible, well-constructed, written and
multimedia resources appropriate to the
patient's educational level.
Researchers have completed the design,
development, data collection and analysis in
an important study of patient and health
system barriers to early diagnosis of head
and neck cancer in Australia. The study
examines geographical variation in pathways
to treatment for head and neck patients
in NSW and investigates patient and carer
perceptions of facilitators and barriers.
This research has the potential to shape health policy to ensure more equitable outcomes for patients with head and neck cancers.Publication is due in 2019.
Graph A: Annual average resections, by NSW public and private hospitals, head and neck cancer, 2016-2017
Chris O'Brien Lifehouse
CHRIS O'BRIEN LIFEHOUSE
28
* Includes co-publications with other Chris O'Brien Lifehouse departments
Highlights
Researchers in the Radiation Oncology
department at Chris O'Brien Lifehouse have
had a productive two years, participating in
several practice-changing studies as both lead
researchers and collaborators.
In a study initiated by our researchers and
Department List A/Prof Christopher Milross MBBS MD FRANZCR FRACMA FAICD (Director of Radiation Oncology)
Dr Leily Gholemrezai MBBS FRANZCR
A/Prof Angela Hong MBBS MMed PhD FRANZCR
Dr Nitya Patanjali MBBS FRANZCR
Dr Mo Mo Tin MBBS FRANZCR
Dr Regina Tse MBBS MClinEpi FRANZCR
Dr Georgia Harris BSc MBBS MPH FRANZCR
Dr Ee Siang Choong MBBS FRANZCR
Dr Kavita Morarji MBBS FRANZCR
Dr Sandy Sampaio MBBS FRANZCR
Dr Eric Khoo MB ChB FRANZCR
Dr Carol Haddad MBBS FRANZCR
VectorLabA/Prof Natalka Suchowerska PhD MAppSc BSc FACPSEM
Linda Rogers B Med Sc
Dr Ana Esteves BSc PhD
Prof David R McKenzie PhD BSc FAIP (collaborator from University of Sydney)
Radiation Oncology
Summary By Numbers
44* publications
11 presentations
13 students
4 grants
carried out across four institutions, patients
who had received treatment for head and neck
cancer were surveyed to find a relationship
between decision-making preferences and
psychological distress.
Researchers found that while patients do
Medical PhysicsElizabeth Claridge Mackonis BSc (Hons) MMedPhys
Dr Samara Alzaidi BEng (Hons) GradDip (Medical Physics) PhD
Johnny Morales BSc (Hons) MSc (Medical Physics)
Dr Martin Butson BSc (Hons) PhD DScBSc (Hons) PhD DSc
Dr Robin Hill BSc (Hons) MSc (Medical Physics) PhD
CHRIS O'BRIEN LIFEHOUSE
29
experience paternalistic decision-making,
most patients would prefer an active or shared
approach to making decisions, especially if
they are tertiary educated or female. However,
psychological distress is more likely in patients
who are actively involved, younger, and
female. The upshot is that clinicians should
be aware of this potential and refer active-
decision makers for psychosocial support.
In a significant collaboration with Royal
Prince Alfred Hospital, researchers undertook
a retrospective review of patients treated
with extracorporeally irradiated allografts
for primary and secondary bone cancers,
studying mid- and long-term survivorship and
functional and radiographic outcomes.
The study looked at patients treated with
extracorporeally irradiated allografts for bone
tumours between 1996 and 2014, examining
the clinical, functional and radiological
outcomes for patients. It demonstrated
that extracorporeal irradiation is a versatile
reconstructive technique for dealing with
large defects after resection of bone tumours
with good functional and radiographic
outcomes. Functional outcomes as measured
by Musculoskeletal Tumor Society (MSTS)
scoring system, the Toronto Extremity Salvage
Score (TESS) and Quality of Life-C30 (QLQ-
30) were strongly correlated to radiographic
outcomes.
Our researchers also contributed to the
national Trans Tasman Radiation Oncology
Group randomised phase 3 trial that looked
at whether postoperative concurrent
chemoradiotherapy, where there is high-
risk cutaneous squamous cell carcinoma
(SCC) of the head and neck, improves patient
outcomes as opposed to postoperative
radiotherapy.
While the combination of surgery and
postoperative radiotherapy was shown to
give excellent results, researchers found that
additional weekly carboplatin (chemotherapy)
brought no added benefit.
These findings eliminate an unnecessary treatment burden for patients.
VectorLAB at Chris O'Brien Lifehouse
combines medicine, physics, biology and
chemistry in order to solve some of the
most urgent problems in cancer. Comprised
of a diverse team of specialist scientists
and clinicians, VectorLAB aims to translate
advances in science and technology to help
people with cancer.
In 2018, VectorLAB acquired a customised
3D printer from the startup company AON3D
in Montreal. Georgio Katsifis, a postgraduate
student from the School of Physics at
University of Sydney, took up the challenge to
use the printer to build bone scaffolds using
the strong polymer Poly-ethyl-ethyl ketone
(PEEK). The scaffolds were then treated using
a plasma gas method to attract bone growth.
(Mr Katsifis was awarded the Robinson Prize by
ACPSEM for the best biomedical engineering
project in 2018.)
The team comprises Head and Neck Surgeon
Jonathan Clark AM, cell biologist Linda Rogers,
and medical physicist Natalka Suchowerska
from Chris O'Brien Lifehouse working in
collaboration with materials physicist Professor
David McKenzie and Georgio Katsifis.
RESEARCH REPORT 2017 & 2018
30
This study will ultimately enable patients who have lost bone to receive a customised scaffold implanted to support regrowth of the patient's own cells.
In working to reduce the risk of infection
during cancer surgery and treatment,
VectorLAB has developed an innovation with
the potential to benefit all surgical patients,
not just those being treated for cancer.
The antimicrobial treatments, developed
using a powerful combination of peptides,
in collaboration with the University of NSW,
were tested on urinary catheters and found to
prevent infection in the form of biofilms from
developing. This finding means that patients'
risk of infection, associated with medical
devices, is significantly reduced and the need
for catheter replacement is reduced.
Funds from Tour de Cure were used to create a
magnetic nanoparticle treatment that can
carry therapeutic molecules into cancer
cells. Many types of treatments can now be
considered for targeted delivery to cancer
cells by nanoparticles, one of them being
a gene silencing therapy for hard to treat
cancers such as mesothelioma.
CHRIS O'BRIEN LIFEHOUSE
31
Department List Prof Jonathan Carter MBBS Dip RACOG FACS FRANZCOG CGO MS MD
(Director)
A/Prof Selvan Pather MBChB FCOG FRANZCOG CGO
A/Prof Samir Saidi MBChB MRCOG FRANZCOG PhD
A/Prof Trevor Tejada-Berges MD MSc FRCPSC FACOG FRANZCOG
Dr Rhonda Farrell BAppSc MBBS (Hons) Dip ObGyn FRANZCOG CGO MS (Incoming Deputy Director)
Dr Robyn Sayer MD FACOG FRANZCOG CGO
Nurse Practitioner Shannon Philp NP RN BN MN (NP) GradCertCancNurs GradCertWomen'sHealthNurs
Nurse Specialist Katie Dicks RN BN
Dr Gemma Blain MBBS (Hons) MRMed BSc FRANZCOG
A/Prof Michael Cooper OAM MBBS MRCOG FRANZCOG MHKCOG FRCOG
Gynaecological Oncology
Summary By Numbers
15 publications
69 presentations
17 students
1 grant
Dr Paulette Maroun MBBS FRANZCOG
Dr Karuna Raja MBBS MS MOHS FRANZCOG
Dr Anthony Richards MBBS FRANZCOG MBA MRMed CGO
Dr Sofia Smirnova MBBS Mmed (RHHG) FRANZCOG
A/Prof Nesrin Varol PhD MIPH FRANZCOG MBBS
Dr Joyce Wu BSc MBBS FRANZCOG
Highlights
For years, the question of optimal adjuvant
therapy for lymph node-negative cervical
cancer patients with intermediate risk factors
has been debated.
Extra treatment modalities come with
substantial risks to patients, increasing the
chances and severity of complications and
side effects. Yet adjuvant radiotherapy after
radical surgery has been advocated for these
cervical cancer patients since the GOG 92
trial (a Gynecologic Oncology Group study
initiated in 1989) found that it reduced the
rate of recurrence and improved survival.
Through a review of the literature and
retrospective cohort study using data from
multiple institutions, researchers found
adjuvant therapy is not a significant prognostic
factor for these patients. This different and
RESEARCH REPORT 2017 & 2018
32
substantially better outcome can be attributed
to improved surgical techniques and more
accurate preoperative and pathological
staging.
The result will lead to fewer patients enduring unnecessary radiotherapy treatment, reducing complications and risks, and improving quality of life.
The role of lymphadenectomy (surgical
removal of one or more groups of lymph nodes)
in patients with early-stage endometrial
cancer is controversial. Previous studies
have grouped patients with varying risks
and histologies together, giving an unclear
picture of the benefits of lymphadenectomies
in different patients. Furthermore, Long-
term morbidity after lymphadenectomy has
remained uncertain.
By analysing data from a large prospective Aus-
tralian National Endometrial Cancer Study, re-
searchers examined the association between
lymphadenectomy and clinicopathological
characteristics, adjuvant treatment, sur-
vival, patterns of disease recurrence, and
morbidity. In a large cohort of patients with
early-stage intermediate- and high-risk endo-
metrioid endometrial cancer, lymphadenecto-
my was found not to improve survival, yet was
associated with significantly higher rates of
critical events and lymphoedema. The result
from these findings will be that fewer patients
in this group will undergo lymphadenectomy
and avoid higher related morbidity.
To date, our understanding of the relationship
between diet and ovarian cancer
survival has been limited. By examining the
relationship between pre-diagnostic diet and
overall survival in a population-based cohort
of Australian women diagnosed with invasive
epithelial ovarian cancer, researchers have
discovered links between ovarian cancer
survival a patient's pre-diagnosis diet.
Researchers observed improved survival linked to fibre intake.
There was suggested further improvement
linked to eating green leafy vegetables, fish
and poly- to mono-unsaturated fat ratio. Also
observed was a worse survival rate associated
with a higher glycaemic index.
This new knowledge about the impact of a
pre-diagnosis diet on survival raises possibili-
ties for dietary choices after diagnosis.
CHRIS O'BRIEN LIFEHOUSE
33
Department List Dr Cindy Mak MBBS (Hons) FRACS (Head of Department)
A/Prof Sanjay Warrier BSc (Med) MBBS FRACS MS
Dr Farhad Azimi-Rashti MBBS MS FRACS
Dr Ping-En Chen BHB MBCHB MS FRACS
Dr Deborah Cheung MBBS FRAC
Dr Senarath Edirimanne BMBS (Hons) FRACS
Dr George Fleischer BMBS FRACS
Dr Irandi Jayatilleke BMedSc BMBS(Hons) FRACS
Dr David LittleJohn MBBS FRACS
Dr Belinda Chan MBBS FRACS MS
Breast
Summary By Numbers
5 publications
6 presentations
1 student
1 grant
Dr Joel Symonds BMedSc (Hons) MBBS FRACS GradCertSurg
Dr April Wong MBChB MS FRACS
Dr Michael Yunaev MBBS MPH BMedSc (Hons) MS FRACS
Highlights
In a significant development in reducing the
risk of necrosis (cell death) following complex
breast reconstruction procedures for women
who have had mastectomy, researchers
have demonstrated how intraoperative
assessment of skin flaps using SPY Elite
influences decision-making in direct to implant
and expander-based reconstruction.
SPY Elite technology gives surgeons the ability
to monitor intraoperatively blood flow to
different areas of the breast during surgery.
Surgeons who use this technology have
reported being better informed to consider
delayed techniques or avoid reconstruction
altogether.
Anecdotally, rates of necrosis have decreased and a prospective trial is underway to determine the full impact of this technology.
The role of antibiotics in reconstructive
implant work has been a matter of scrutiny,
with the question of clinical benefits derived
from using antibiotics and antiseptics to
washout the breast pocket or soak the breast
implant during surgery remaining inconclusive.
RESEARCH REPORT 2017 & 2018
34
The Centers for Disease Control and Prevention
give a muted recommendation for washing
tissues in iodophor, but until now, the efficacy
and impact of this practice in reducing
infection rates had not been adequately
examined.
Through a systematic review of cohort stud-
ies involving an implant or tissue expander in
augmentative surgery, researchers found that
using antibiotics in pocket washout or implant
immersion does indeed reduce infection rates,
however the evidence is deficient. While data
trends towards better outcomes with beta-
dine and antibiotics, it remains unproven and
a randomised control trial is needed.
As part of an ongoing series, researchers from
multiple hospitals examined approaches to
managing complications relating to breast
implant infections. In one instance, they dis-
cussed treatment using Veraflo™ device and
irrigation, which couples Negative Pressure
Wound Therapy with automated, controlled
delivery of topical wound treatment solutions
to and from the wound bed.
The findings showed rapid cleaning of the
wound and formation of granulations, and
was followed by successful reinsertion of
breast implants.
In what is a relatively simple solution, this treatment was demonstrably capable of salvaging reconstruction in the event of infection.
CHRIS O'BRIEN LIFEHOUSE
35
Highlights
The Neurosurgery research program launched
with the aim of improving the clinical manage-
ment and outcomes for patients diagnosed
with primary brain cancer.
While primary malignant brain cancers have
a relatively low incidence, they carry a high
disease burden. The most frequent subtype,
glioblastoma, is incurable and often rapidly
fatal. Despite paradigm-shifting advances in
science, technology and healthcare over the
last 30 years, survival rates for patients with
glioblastoma have remained dismally low.
This is a direct result of a lack of fundamental scientific research.
While community awareness of brain cancer
and its associated burden is growing, critical
research is hampered by the absence of ma-
terials to study.
In 2019, through our partnerships with
Brainstorm Brain Cancer Research at the
Brain and Mind Centre, Sydney University
and RPA Neuropathology Department, we
aim to launch Chris O'Brien Lifehouse as
a new collection site of the Sydney Brain
Tumour Bank. Tumour tissues, cells and blood
specimens will be collected, preserved and
made freely available to researchers world-
wide to support a variety of research into
brain cancer.
With this framework in place, we are working
towards the launch of GlioNET, a multi-centre,
observational trial for newly diagnosed glioma
patients within the next 12 months.
This ambitious project will track Australian
patients diagnosed with glioma over the
entire course of their cancer journey.
This will be the first concerted effort to
record complete longitudinal clinical and
pathological information, bio-specimens
(blood, tumour tissues and cells), imaging
and patient- and caregiver-centred data (self-
reported quality of life questionnaires, sleep
and exercise data). Materials and information
Neurosurgery
Department List Dr Brindha Shivalingam MBBS FRACS (Director)
Dr Benjamin Jonker MBBS MMed FRACS
Dr Rodney Allan MBBS (Hons) FRACS
Dr Johnny Wong MBBS (Hons) MMed PhD FRACS
Dr Kim Kaufman, BMedSc (Hons) PhD
RESEARCH REPORT 2017 & 2018
36
captured during GlioNET will create a unique,
open-access platform to:
1. Understand the molecular events driving
tumour evolution and adaptation, and
failure of current standard therapies.
2. Discover and confirm novel biomarkers
that can accurately diagnose and predict
tumour progression and treatment
responses.
3. Identify opportunities for improving
services and patient and carer morbidity.
4. Drive the implementation of adaptive
clinical trials and ultimately, precision
medicine.
GlioNET longitudinal data and specimens will
support a number of specific sub-studies,
including the translation of a non-invasive
blood test for monitoring glioma tumour
progression, published by our group in 2018.1
Here we showed that robust molecular
signatures are detectable in blood exosomes
and are specific to glioblastoma and lower
grade gliomas.
This approach has enormous potential to revolutionise how brain tumours are monitored. It could allow us to detect the very early stages
of treatment failure, tumour recurrence and
progression via simple blood tests.
1 Ebrahimkhani S., Vafaee F., Hallal S., Wei H., Lee M. Y. T., Young P. E., Satgunaseelan L., Beadnall H., Barnett M. H., Shivalingam B., Suter C. M., Buckland M. E., Kaufman K. L. 2018. Deep sequencing of circulating exosomal microRNA allows non-invasive glioblastoma diagnosis. npj Precision Oncology, 2, 28 (2018). URL: https://www.nature.com/articles/s41698-018-0071-0.
CHRIS O'BRIEN LIFEHOUSE
37
HighlightsThe Uro-Oncology research program launched
in 2018 and has contributed to several salient
projects in its first months.
Inguinal hernia is a known consequence
of radical prostatectomy that contributes
to patient morbidity and leads to higher
health care costs. Lesser known is that it
is also common after minimally invasive
radical prostatectomy. In a systematic
review of incidence, predictive factors and
preventive measures, researchers found
high-level evidence that clarifies risk factors
and preventive strategies are lacking for
inguinal hernia following robotic and
laparoscopic radical prostatectomy. The study
demonstrated a justification for randomised
control trials to further evaluate this under-
recognised clinical problem, which causes
patients distress and may require a second
operation to fix.
In a multicentre phase 3 trial, researchers
studied whether androgen-deprivation ther-
apy for patients with prostate cancer (who
have relapsed with rising prostate-specific
antigen concentration only or with non-cur-
able but asymptomatic disease at diagnosis),
could adversely affect quality of life at a time
when the disease itself does not. Involving
29 public and private cancer centres across
Australia, New Zealand and Canada, the aim
was to compare the effect of immediate ver-
sus delayed androgen-deprivation therapy on
health-related quality of life over five years.
Researchers found that immediate use of
androgen-deprivation therapy was associated
with early detriments in specific hormone-
treatment-related symptoms, but no other
demonstrable effect on overall functioning
of health-related quality of life. This evidence
can be used to help decision-making about
treatment initiation for men at this disease
stage.
Researchers from multiple institutions sought
to evaluate the impact of publications on
urological participation in social media
by virtue of citations in the urological and
non-urological literature. They found that uro-
logical social media journal articles are highly
cited, particularly in the non-urological litera-
ture. It's likely the magnitude of citations has
positively contributed to the impact factors of
publishing journals.
Department List Professor Henry Woo MBBS FRACS (Director)
Dr Nariman Ahmadi BSc (Med) MBBS FRACS
Dr Norbert Doeuk MBBS MS FRACS
Dr Scott Leslie BSc (Med) MBBS (Hons) FRACS
Uro-Oncology
Dr Paul Sved BSc (Med) (Hons) MBBS (Hons) MMed FRACS
Dr Ruban Thanigasalam MBBS MS FRACS
Dr Arthur Vasilaras MBBS (Hons) FRACS
Dr Tania Hossack MBBS (Hons) FRACS MSPro
RESEARCH REPORT 2017 & 2018
38
* Includes co-publications with other Chris O'Brien Lifehouse departments
HighlightsIntegrative oncology is a fast-evolving field as
more patients seek a holistic approach to their
disease and symptoms. The research strategy
of the Supportive Care and Integrative Med-
icine service at Chris O'Brien Lifehouse is fo-
cused on developing a strong evidence base
to support the integration of holistic medical
care, complementary therapies, exercise and
nutrition into standard cancer care.
Furthermore, as people with cancer live
longer, there is a growing need to develop
programs that support them to live well. The
research program in the Supportive Care ser-
vice aims to identify the best ways to support
patients with a focus on symptoms.
Chris O'Brien Lifehouse is committed to
developing integrative oncology research
in Australia, working in collaboration with
the University of Sydney, Western Sydney
University, University of Technology, Sydney,
NSW Health and other institutions nationally
and internationally. The last two years have
been particularly productive as this service has
developed.
Our researchers initiated a practice-chang-
ing study into living well with melanoma
and immunotherapy. Despite an increasing
number of metastatic melanoma patients
receiving immunotherapy treatment, includ-
ing Pembrolizumab, the long term impacts
on their well-being remain underexplored. A
Department List A/Prof Judith Lacey MBBS FRACGP FAChPM (FRACP) (Director)
Dr Suzanne Grant BAppSc (TCM) MPS PhD (Acupuncturist)
Dr Toni Lindsay PhD (Clinical Psychologist)
Mr Michael Marthick BSc GradDipSc (Ex Rehab) MPH (Exercise
Physiologist)
Dr Diana Naehrig (Research Fellow, Supportive Care)
Dr Victoria Choi (Acupuncturist, Researcher)
Supportive Care and Integrative Medicine
Summary By Numbers
14* publications
37 presentations
4 students
9 grants
CHRIS O'BRIEN LIFEHOUSE
39
pilot study assessed the feasibility, perceived
benefit, and acceptability of a supportive care
intervention for people with metastatic mela-
noma being treated with immunotherapy.
This pilot has paved the way for a feasible model of care in supportive cancer care and immunotherapy.
It will contribute data to develop guidelines to
support these patients, and will inform a model
of care for programs beyond melanoma.
This research informed a secondary objective,
which was to explore the lived experience of
these patients. The publication highlighted
the patient experience of coping with
uncertainty.
Exercise physiologist and researcher, Michael
Marthick, investigated the feasibility, usability
and acceptability of an interactive web
portal developed to support patients with
cancer to increase daily physical activity
levels. He found that the portal was feasible,
but further research is needed to determine
optimal coaching methods.
In a paper that explored the establishment
of an integrative oncology service in the
Australian healthcare setting, researchers
reflected on the Chris O'Brien Lifehouse
hospital experience.
They found the strategic integration of medical specialist and integrative oncology services, as part of the hospital's supportive care services, led to improved acceptance by specialists and nursing staff.
Researchers have undertaken a retrospective
evaluation over one year, interviewing
oncologists, radiation oncologists, surgeons
and clinical staff, to investigate how they
approach meeting the supportive care
needs of their patients. This qualitative data
is being analysed and written. By evaluating
the unmet supportive care needs of cancer
patients at Chris O'Brien Lifehouse, this
research will inform interventions and service
development and enable benchmarking with
services within Australia and internationally,
promoting collaboration in the integrative
oncology and supportive care space.
RESEARCH REPORT 2017 & 2018
The Psycho-oncology Co-operative Research
Group (PoCoG) and Centre For Medical Psy-
chology & Evidence-Based Decision-Making
(CeMPED), are research centres of the Univer-
sity of Sydney collaborating with Chris O'Brien
Lifehouse on a large project that is evaluat-
ing the resources and support required to
implement a clinical pathway to manage
anxiety and depression in cancer patients
(ADAPT).
The ultimate goal of this project is to ensure all patients receive the best care possible, including for the emotional impact of cancer.
In this study, twelve oncology units in NSW are
randomised to receive basic versus extended
support to implement ADAPT.
After training staff members in the clinical
pathway and how to use the online portal
through which ADAPT operates, the project
has these key features:
• All patients are invited to complete reg-
ular screening for anxiety and depression
by completing a short online question-
naire.
• Staff are alerted by the online system if
patients' scores indicate they are experi-
encing anxiety and depression.
• The system recommends appropriate care
for that individual's level of anxiety and
depression.
• Staff are prompted to discuss treatment
options with the patient, and they record
actions taken on the portal, including re-
ferrals to psychosocial health profession-
als.
• The portal triggers treatment comple-
tion reports, and re-screening every three
months.
• An online intervention using cognitive-be-
haviour therapy is available to patients
with mild to moderate anxiety/depres-
sion.
ADAPT has recently 'gone live' at Chris O'Brien
Lifehouse, with two patients registered in
the system in the first week. Chris O'Brien
Lifehouse will use ADAPT for one year. Staff are
surveyed and a small group are interviewed
three times during the year, to gain feedback
on how ADAPT is functioning.
AffiliatesPoCoG & CeMPED
40
CHRIS O'BRIEN LIFEHOUSE
41
Chris O'Brien Lifehouse is one of the original
member groups of Sydney Catalyst and the re-
lationship between the two organisations has
gone from strength to strength.
The Sydney Catalyst central office is housed
within the Lifehouse building. This has provided
an important opportunity for the groups
to work closely together across a range of
translational research projects and activities,
challenging institutional and work culture
boundaries. Co-location also provides Sydney
Catalyst staff with a unique opportunity to
experience the inner workings of Chris O'Brien
Lifehouse, enriching their understanding of
clinical practice and breaking down some of
the walls between researchers and clinicians.
The appointment of Professor Michael
Boyer AM as the Director of Sydney Catalyst
further harnesses the relationship, as does
the involvement of Professor Lisa Horvath,
Director of Research, on the Sydney Catalyst
Scientific Advisory Committee.
EnRICH is an important example of translational
research collaboration between Chris O'Brien
Lifehouse and Sydney Catalyst.
The Embedding Research (and Evidence)
in Cancer Healthcare (EnRICH) program
is the major flagship translational cancer
research program for Sydney Catalyst. Chris
O'Brien Lifehouse is a significant partner in this
program.
EnRICH is assembling a clinical cohort of
1,000 patients with lung cancer to:
• Describe the natural history of and
patterns of care for lung cancer;
• Better define, treat and care for patients
across Sydney Catalyst member hospitals,
including Chris O'Brien Lifehouse;
• Create a platform for researchers across
the T1-T3 translational research spectrum
to develop and initiate clinical research
and intervention studies to address gaps.
Professor Boyer is a clinical lead for EnRICH
and more than one-third of patients currently
involved in EnRICH have been recruited from
and/or treated at Chris O'Brien Lifehouse.
Some of the key research questions being
addressed by EnRICH include:
• What are the molecular, disease and pa-
tient characteristics of patients with lung
cancer?
• What is the natural history of patients with
lung cancer in terms of recurrence-free
survival, overall survival and patient re-
ported outcomes?
• What are the main prognostic factors for
these outcomes related to molecular, dis-
ease and patient characteristics?
• What are current patterns of care for pa-
tients with lung cancer? How and why do
patterns of care vary?
Significant new research opportunities have
been made possible by EnRICH enabling Syd-
ney Catalyst members and others locally and
internationally to use the resource to improve
outcomes for people affected by cancer. A
number of sub-studies using biospecimens
and data from the EnRICH cohort are currently
being undertaken.
Sydney Catalyst
RESEARCH REPORT 2017 & 2018
The Cancer Nursing Research Unit is a member
group of Sydney Catalyst and advances clinical
nursing practice by supporting cancer nurses
in research, higher degree studies and hosting
postgraduate students.
The CNRU conducts its research activities
under four themes:
• Supportive care;
• Psychosocial and quality of life;
• Models of healthcare delivery; and
• Improving research capacity and skills for
cancer and palliative care nurses.
Recruitment has been completed and data
analysis is well underway in a project that
evaluates shared care pathway interven-
tion to reduce chemotherapy outpatients'
unplanned presentations to hospital (a part-
nership with Lifehouse and Concord Repatria-
tion General Hospital).
A project to assess adolescent and young
adult cancer patients' transition to palli-
ative care and the effect on health care
professionals has been completed to recruit-
ment, with a paper in draft.
Outside of these formal research activities, the
CNRU continues to demonstrate the benefits
of co-location through its informal support
and mentorship of specialist nurses at Chris
O'Brien Lifehouse.
Collaboration and one-on-one mentoring
has led to more nurses working more fre-
quently within a research framework. The
CNRU supports nurses to develop projects,
prepare papers and presentations, and submit
abstracts for presentations.
By encouraging nurses to work within a research framework, the CNRU empowers nurses to proactively respond to patient needs that they observe through their work.
An example is a scalp cooling initiative
which helps reduce the volume of hair that
is lost during chemotherapy. A methodology
has been developed on another site and
CNRU is working with Chris O'Brien Lifehouse
to evaluate factors that will facilitate
implementation.
Cancer Nursing Research
42
CHRIS O'BRIEN LIFEHOUSE
43
Established in 2014, the RPA Institute of
Academic Surgery (IAS) supports surgical
departments across the broader Royal Prince
Alfred Hospital (RPAH), Chris O'Brien Lifehouse
and University of Sydney campus to enhance
their research and education. The IAS worked
in close collaboration with a number of
Chris O'Brien Lifehouse surgical and medical
departments on a range of research projects
during 2017 and 2018.
Within the Head and Neck surgery
department this included commencing
pilot studies examining the effectiveness of
designing and printing 3D models to assist
with the surgical planning for complex
reconstruction cases and the utilisation of
the IAS surgical skills facilities to undertake
pre-clinical investigations as part of the
BLINC research project aiming to assist
patients with severe nerve damage to their
eyelids.
The delivery of the Advanced GI Surgical
Program incorporating pelvic exenteration,
peritonectomy and advanced upper GI
malignancy continues to be a strong point of
collaboration between the IAS and a range of
leading clinicians from Chris O'Brien Lifehouse,
from Medical Oncology, Gynae Oncology
and Radiation Oncology. This includes
contributing to the program-wide research
databases (PESQI, PREMIER and HUGO).
This crucially underpins more than 35 studies across the entire Advanced GI Surgical Program.
A new and exciting multi-site study that has
been developed and commenced in 2017/18
is the ReLaPSeD trial. This is a prospective
randomised controlled trial comparing re-
look laparoscopy versus standard follow-up
for early detection and treatment of patients
at high risk of peritoneal metastases after
resection of colorectal cancer.
Within breast surgery, projects were
undertaken looking at the use of 3D printed
models to assist in surgical planning and
patient education, as well as the ongoing
investigation of the use and potential
benefits of SPY imaging technology for
breast reconstruction patients.
In addition to their specific areas of research,
surgical staff from Chris O'Brien Lifehouse also
provide regular teaching and mentoring to
a range of junior medical, nursing and allied
health staff doing research at the IAS, as well
as the supervision of research projects being
undertaken by MD students at the University
of Sydney.
RPA Institute of Academic Surgery
RESEARCH REPORT 2017 & 2018
AHMADZADA, T., KAO, S., REID, G., BOYER, M., MAHAR, A. &
COOPER, W. A. 2018. An Update on Predictive Biomarkers
for Treatment Selection in Non-Small Cell Lung Cancer. J
Clin Med, 7.
AHMADZADA, T., REID, G. & KAO, S. 2018. Biomarkers in
malignant pleural mesothelioma: current status and fu-
ture directions. J Thorac Dis, 10, S1003-s1007.
AHN, M. J., KIM, D. W., CHO, B. C., KIM, S. W., LEE, J. S.,
AHN, J. S., KIM, T. M., LIN, C. C., KIM, H. R., JOHN, T., KAO,
S., GOLDMAN, J. W., SU, W. C., NATALE, R., RABBIE, S., HAR-
ROP, B., OVEREND, P., YANG, Z. & YANG, J. C. 2017. Ac-
tivity and safety of AZD3759 in EGFR-mutant non-small-
cell lung cancer with CNS metastases (BLOOM): a phase
1, open-label, dose-escalation and dose-expansion study.
Lancet Respir Med, 5, 891-902.
AMUNDSEN, A., BERGVIK, S., BUTOW, P., TATTERSALL, M. H.
N., SORLIE, T. & NORDOY, T. 2018. Supporting doctor-pa-
tient communication: Providing a question prompt list
and audio recording of the consultation as communica-
tion aids to outpatients in a cancer clinic. Patient Educ
Couns, 101, 1594-1600.
AMUNDSEN, A., ERVIK, B., BUTOW, P., TATTERSALL, M. H.,
BERGVIK, S., SORLIE, T. & NORDOY, T. 2017. Adapting an
Australian question prompt list in oncology to a Norwe-
gian setting-a combined method approach. Support Care
Cancer, 25, 51-58.
ARMSTRONG-GORDON, E., GNJIDIC, D., MCLACHLAN, A.,
HOSSEINI, B., GRANT, A., BEALE, P. & WHEATE, N. J. 2018.
Patterns of platinum drug use in an acute care setting: a
retrospective study. Journal of Cancer Research and Clini-
cal Oncology, 144, 1561-1568.
ASCIERTO, P. A., DEL VECCHIO, M., ROBERT, C., MACKIEW-
ICZ, A., CHIARION-SILENI, V., ARANCE, A., LEBBE, C., BAST-
HOLT, L., HAMID, O., RUTKOWSKI, P., MCNEIL, C., GARBE,
C., LOQUAI, C., DRENO, B., THOMAS, L., GROB, J. J., LISZ-
KAY, G., NYAKAS, M., GUTZMER, R., PIKIEL, J., GRANGE, F.,
HOELLER, C., FERRARESI, V., SMYLIE, M., SCHADENDORF,
D., MORTIER, L., SVANE, I. M., HENNICKEN, D., QURESHI, A.
& MAIO, M. 2017. Ipilimumab 10 mg/kg versus ipilimum-
ab 3 mg/kg in patients with unresectable or metastat-
ic melanoma: a randomised, double-blind, multicentre,
phase 3 trial. Lancet Oncol, 18, 611-622.
ASCIERTO, P. A., LONG, G. V., ROBERT, C., BRADY, B., DUTR-
IAUX, C., DI GIACOMO, A. M., MORTIER, L., HASSEL, J. C.,
RUTKOWSKI, P., MCNEIL, C., KALINKA-WARZOCHA, E., SAV-
AGE, K. J., HERNBERG, M. M., LEBBE, C., CHARLES, J., MI-
HALCIOIU, C., CHIARION-SILENI, V., MAUCH, C., COGNET-
TI, F., NY, L., ARANCE, A., SVANE, I. M., SCHADENDORF,
D., GOGAS, H., SACI, A., JIANG, J., RIZZO, J. & ATKINSON,
V. 2018. Survival Outcomes in Patients With Previously
Untreated BRAF Wild-Type Advanced Melanoma Treated
With Nivolumab Therapy: Three-Year Follow-up of a Rand-
omized Phase 3 Trial. JAMA Oncol.
BALACHANDRAN, V. P., LUKSZA, M., ZHAO, J. N., MAKAROV,
V., MORAL, J. A., REMARK, R., HERBST, B., ASKAN, G.,
BHANOT, U., SENBABAOGLU, Y., WELLS, D. K., CARY, C.
I. O., GRBOVIC-HUEZO, O., ATTIYEH, M., MEDINA, B.,
ZHANG, J., LOO, J., SAGLIMBENI, J., ABU-AKEEL, M., ZAPPA-
SODI, R., RIAZ, N., SMORAGIEWICZ, M., KELLEY, Z. L., BAS-
TURK, O., GONEN, M., LEVINE, A. J., ALLEN, P. J., FEARON,
D. T., MERAD, M., GNJATIC, S., IACOBUZIO-DONAHUE, C.
A., WOLCHOK, J. D., DEMATTEO, R. P., CHAN, T. A., GREEN-
BAUM, B. D., MERGHOUB, T. & LEACH, S. D. 2017. Identi-
fication of unique neoantigen qualities in long-term survi-
vors of pancreatic cancer. Nature, 551, 512-516.
BARNET, M. B., BLINMAN, P., COOPER, W., BOYER, M. J.,
KAO, S. & GOODNOW, C. C. 2018. Understanding Im-
mune Tolerance of Cancer: Re-Purposing Insights from
Fetal Allografts and Microbes. Bioessays, 40, e1800050.
Medical Oncology
46
CHRIS O'BRIEN LIFEHOUSE
47
BARNET, M. B., COOPER, W. A., BOYER, M. J. & KAO, S.
2018. Immunotherapy in Non-Small Cell Lung Cancer:
Shifting Prognostic Paradigms. J Clin Med, 7.
BARNET, M. B., O'TOOLE, S., HORVATH, L. G., SELINGER, C.,
YU, B., NG, C. C., BOYER, M., COOPER, W. A. & KAO, S.
2017. EGFR-Co-Mutated Advanced NSCLC and Response
to EGFR Tyrosine Kinase Inhibitors. J Thorac Oncol, 12,
585-590.
BARNET, M. B., ZIELINSKI, R. R., WARBY, A., LEWIS, C. R. &
KAO, S. 2018. Pseudoprogression Associated with Clinical
Deterioration and Worsening Quality of Life in Malignant
Pleural Mesothelioma. J Thorac Oncol, 13, e1-e2.
BLINMAN, P. L., DAVIS, I. D., MARTIN, A., TROON, S., SEN-
GUPTA, S., HOVEY, E., COSKINAS, X., KAPLAN, R., RITCHIE,
A., MEADE, A., EISEN, T. & STOCKLER, M. R. 2018. Patients'
preferences for adjuvant sorafenib after resection of renal
cell carcinoma in the SORCE trial: what makes it worth-
while? Ann Oncol, 29, 370-376.
BLOCK, M. S., VIERKANT, R. A., RAMBAU, P. F., WINHAM, S. J.,
WAGNER, P., TRAFICANTE, N., TOLOCZKO, A., TIEZZI, D. G.,
TARAN, F. A., SINN, P., SIEH, W., SHARMA, R., ROTHSTEIN, J.
H., RAMON, Y. C. T., PAZ-ARES, L., OSZUREK, O., ORSULIC,
S., NESS, R. B., NELSON, G., MODUGNO, F., MENKISZAK, J.,
MCGUIRE, V., MCCAULEY, B. M., MACK, M., LUBINSKI, J.,
LONGACRE, T. A., LI, Z., LESTER, J., KENNEDY, C. J., KALLI,
K. R., JUNG, A. Y., JOHNATTY, S. E., JIMENEZ-LINAN, M.,
JENSEN, A., INTERMAGGIO, M. P., HUNG, J., HERPEL, E.,
HERNANDEZ, B. Y., HARTKOPF, A. D., HARNETT, P. R., GHAT-
AGE, P., GARCIA-BUENO, J. M., GAO, B., FEREDAY, S., EILBER,
U., EDWARDS, R. P., DE SOUSA, C. B., DE ANDRADE, J. M.,
CHUDECKA-GLAZ, A., CHENEVIX-TRENCH, G., CAZORLA, A.,
BRUCKER, S. Y., ALSOP, J., WHITTEMORE, A. S., STEED, H.,
STAEBLER, A., MOYSICH, K. B., MENON, U., KOZIAK, J. M.,
KOMMOSS, S., KJAER, S. K., KELEMEN, L. E., KARLAN, B. Y.,
HUNTSMAN, D. G., HOGDALL, E., GRONWALD, J., GOOD-
MAN, M. T., GILKS, B., GARCIA, M. J., FASCHING, P. A., DE
FAZIO, A., DEEN, S., CHANG-CLAUDE, J., CANDIDO DOS
REIS, F. J., CAMPBELL, I. G., BRENTON, J. D., BOWTELL, D.
D., BENITEZ, J., PHAROAH, P. D. P., KOBEL, M., RAMUS, S.
J. & GOODE, E. L. 2018. MyD88 and TLR4 Expression in
Epithelial Ovarian Cancer. Mayo Clin Proc, 93, 307-320.
BONAVENTURA, A., O'CONNELL, R. L., MAPAGU, C., BEALE,
P. J., MCNALLY, O. M., MILESHKIN, L. R., GRANT, P. T., HAD-
LEY, A. M., GOH, J. C. H., SJOQUIST, K. M., MARTYN, J., DE-
FAZIO, A., SCURRY, J. & FRIEDLANDER, M. L. 2017. Paragon
(ANZGOG-0903): Phase 2 Study of Anastrozole in Wom-
en With Estrogen or Progesterone Receptor-Positive Plat-
inum-Resistant or -Refractory Recurrent Ovarian Cancer.
Int J Gynecol Cancer, 27, 900-906.
BOYLE, F., BEITH, J., BURSLEM, K., DE BOER, R., HUI, R., LIM,
E., MCCARTHY, N., REDFERN, A. & WOODWARD, N. 2018.
Hormone receptor positive, HER2 negative metastatic
breast cancer: Impact of CDK4/6 inhibitors on the cur-
rent treatment paradigm. Asia Pac J Clin Oncol, 14 Suppl
4, 3-11.
BUI, K. T., COOPER, W. A., KAO, S. & BOYER, M. 2018. Tar-
geted Molecular Treatments in Non-Small Cell Lung Can-
cer: A Clinical Guide for Oncologists. J Clin Med, 7.
BUTOW, P., SHARPE, L., THEWES, B., TURNER, J., GILCHRIST,
J. & BEITH, J. 2018. Fear of Cancer Recurrence: A Practical
Guide for Clinicians. Oncology (Williston Park), 32, 32-8.
BUTOW, P., SHAW, J., SHEPHERD, H., PRICE, M., MASYA, L.,
KELLY, B., RANKIN, N., GIRGIS, A., HACK, T., BEALE, P., DHILL-
ON, H., COLL, J. R., KELLY, P. J., LOVELL, M. R., GRIMISON, P.,
SHAW, T., CUDDY, J., WHITE, F. & ET AL. 2018. Comparison
of implementation strategies to influence adherence to
the clinical pathway for screening, assessment and man-
agement of anxiety and depression in adult cancer pa-
tients (ADAPT CP): study protocol of a cluster randomised
controlled trial. BMC Cancer, 18, 1077.
BUTOW, P., SHAW, J., SHEPHERD, H. L., PRICE, M., MASYA,
L., KELLY, B., RANKIN, N. M., GIRGIS, A., HACK, T. F., BEALE,
P., VINEY, R., DHILLON, H. M., COLL, J., KELLY, P., LOVELL, M.,
GRIMISON, P., SHAW, T., LUCKETT, T., CUDDY, J. & WHITE,
F. 2018. Comparison of implementation strategies to in-
fluence adherence to the clinical pathway for screening,
assessment and management of anxiety and depression in
adult cancer patients (ADAPT CP): study protocol of a clus-
ter randomised controlled trial. BMC Cancer, 18, 1077.
BUTOW, P. N., TURNER, J., GILCHRIST, J., SHARPE, L., SMITH,
A. B., FARDELL, J. E., TESSON, S., O'CONNELL, R., GIRGIS,
A., GEBSKI, V. J., ASHER, R., MIHALOPOULOS, C., BELL, M.
L., ZOLA, K. G., BEITH, J. & THEWES, B. 2017. Randomized
Trial of ConquerFear: A Novel, Theoretically Based Psycho-
social Intervention for Fear of Cancer Recurrence. J Clin
Oncol, 35, 4066-4077.
CAZET, A. S., HUI, M. N., ELSWORTH, B. L., WU, S. Z., RO-
DEN, D., CHAN, C. L., SKHINAS, J. N., COLLOT, R., YANG,
RESEARCH REPORT 2017 & 2018
J., HARVEY, K., JOHAN, M. Z., COOPER, C., NAIR, R., HERR-
MANN, D., MCFARLAND, A., DENG, N., RUIZ-BORREGO, M.,
ROJO, F., TRIGO, J. M., BEZARES, S., CABALLERO, R., LIM, E.,
TIMPSON, P., O'TOOLE, S., WATKINS, D. N., COX, T. R., SAM-
UEL, M. S., MARTIN, M. & SWARBRICK, A. 2018. Targeting
stromal remodeling and cancer stem cell plasticity over-
comes chemoresistance in triple negative breast cancer.
Nat Commun, 9, 2897.
CHIM, L., SALKELD, G., KELLY, P., LIPWORTH, W., HUGHES, D.
A. & STOCKLER, M. R. 2017. Societal perspective on access
to publicly subsidised medicines: A cross sectional survey
of 3080 adults in Australia. PLoS One, 12, e0172971.
CHO D, RONCOLATO FT, MAN J, SIMES J, LORD SJ, LINKS MJ
& CK, L. 2017. Clinical equipoise for trials of novel biolog-
ic therapies, therapeutic success rates, and predictors of
success: a meta-analysis. JCO Precision Oncology 1.
COHEN, P. A., BRAND, A., SYKES, P., WREDE, D. C. H., MC-
NALLY, O., EVA, L., RAO, A., CAMPION, M., STOCKLER,
M., POWELL, A., CODDE, J., BULSARA, M. K., ANDERSON,
L., LEUNG, Y., FARRELL, L. & STOYLES, P. 2017. Excisional
treatment in women with cervical adenocarcinoma in situ
(AIS): a prospective randomised controlled non-inferiori-
ty trial to compare AIS persistence/recurrence after loop
electrosurgical excision procedure with cold knife cone
biopsy: protocol for a pilot study. BMJ Open, 7, e017576.
COLLEONI, M., LUO, W., KARLSSON, P., CHIRGWIN, J., AEBI,
S., JERUSALEM, G., NEVEN, P., HITRE, E., GRAAS, M. P., SI-
MONCINI, E., KAMBY, C., THOMPSON, A., LOIBL, S., GAVILA,
J., KUROI, K., MARTH, C., MULLER, B., O'REILLY, S., DI LAU-
RO, V., GOMBOS, A., RUHSTALLER, T., BURSTEIN, H., RIBI, K.,
BERNHARD, J., VIALE, G., MAIBACH, R., RABAGLIO-PORETTI,
M., GELBER, R. D., COATES, A. S., DI LEO, A., REGAN, M.
M. & GOLDHIRSCH, A. 2018. Extended adjuvant intermit-
tent letrozole versus continuous letrozole in postmeno-
pausal women with breast cancer (SOLE): a multicentre,
open-label, randomised, phase 3 trial. Lancet Oncol, 19,
127-138.
COOPER WA, B. M., KAO SC, SCOLIER RA. 2018. Biomark-
ers that predict response to immunotherapy – no magic
bullet. Cancer Forum, 42.
DADAEV, T., SAUNDERS, E. J., NEWCOMBE, P. J., ANOKIAN,
E., LEONGAMORNLERT, D. A., BROOK, M. N., CIEZA-BOR-
RELLA, C., MIJUSKOVIC, M., WAKERELL, S., OLAMA, A. A. A.,
SCHUMACHER, F. R., BERNDT, S. I., BENLLOCH, S., AHMED,
M., GOH, C., SHENG, X., ZHANG, Z., MUIR, K., GOVIN-
DASAMI, K., LOPHATANANON, A., STEVENS, V. L., GAP-
STUR, S. M., CARTER, B. D., TANGEN, C. M., GOODMAN,
P., THOMPSON, I. M., JR., BATRA, J., CHAMBERS, S., MOYA,
L., CLEMENTS, J., HORVATH, L., TILLEY, W., RISBRIDGER, G.,
GRONBERG, H., ALY, M., NORDSTROM, T., PHAROAH, P.,
PASHAYAN, N., SCHLEUTKER, J., TAMMELA, T. L. J., SIPEKY,
C., AUVINEN, A., ALBANES, D., WEINSTEIN, S., WOLK, A.,
HAKANSSON, N., WEST, C., DUNNING, A. M., BURNET, N.,
MUCCI, L., GIOVANNUCCI, E., ANDRIOLE, G., CUSSENOT,
O., CANCEL-TASSIN, G., KOUTROS, S., FREEMAN, L. E. B.,
SORENSEN, K. D., ORNTOFT, T. F., BORRE, M., MAEHLE, L.,
GRINDEDAL, E. M., NEAL, D. E., DONOVAN, J. L., HAMDY,
F. C., MARTIN, R. M., TRAVIS, R. C., KEY, T. J., HAMILTON, R.
J., FLESHNER, N. E., FINELLI, A., INGLES, S. A., STERN, M. C.,
ROSENSTEIN, B., KERNS, S., OSTRER, H., LU, Y. J., ZHANG, H.
W., FENG, N., MAO, X., GUO, X., WANG, G., SUN, Z., GILES,
G. G., SOUTHEY, M. C., MACINNIS, R. J., FITZGERALD, L. M.,
KIBEL, A. S., DRAKE, B. F., VEGA, A., GOMEZ-CAAMANO,
A., FACHAL, L., SZULKIN, R., EKLUND, M., KOGEVINAS, M.,
LLORCA, J., CASTANO-VINYALS, G., PENNEY, K. L., STAMPFER,
M., PARK, J. Y., SELLERS, T. A., et al. 2018. Fine-mapping of
prostate cancer susceptibility loci in a large meta-analy-
sis identifies candidate causal variants. Nat Commun, 9,
2256.
DEAR, R. F., MCGEECHAN, K., BARNET, M. B., BARRATT, A.
L. & TATTERSALL, M. H. N. 2017. "Standard Care" in Can-
cer Clinical Trials: An Analysis of Care Provided to Women
in the Control Arms of Breast Cancer Clinical Trials. J Natl
Compr Canc Netw, 15, 1131-1139.
DHILLON, H. M., BELL, M. L., VAN DER PLOEG, H. P., TURN-
ER, J. D., KABOURAKIS, M., SPENCER, L., LEWIS, C., HUI,
R., BLINMAN, P., CLARKE, S. J., BOYER, M. J. & VARDY, J. L.
2017. Impact of physical activity on fatigue and quality of
life in people with advanced lung cancer: a randomized
controlled trial. Ann Oncol, 28, 1889-1897.
DUCHESNE, G. M., WOO, H. H., KING, M., BOWE, S. J.,
STOCKLER, M. R., AMES, A., D'ESTE, C., FRYDENBERG, M.,
LOBLAW, A., MALONE, S., MILLAR, J., TAI, K. H. & TURNER, S.
2017. Health-related quality of life for immediate versus
delayed androgen-deprivation therapy in patients with
asymptomatic, non-curable prostate cancer (TROG 03.06
and VCOG PR 01-03 [TOAD]): a randomised, multicentre,
non-blinded, phase 3 trial. Lancet Oncol, 18, 1192-1201.
*
EPSTEIN, R. M., DUBERSTEIN, P. R., FENTON, J. J., FISCELLA,
48
CHRIS O'BRIEN LIFEHOUSE
49
K., HOERGER, M., TANCREDI, D. J., XING, G., GRAMLING, R.,
MOHILE, S., FRANKS, P., KAESBERG, P., PLUMB, S., CIPRI, C.
S., STREET, R. L., JR., SHIELDS, C. G., BACK, A. L., BUTOW,
P., WALCZAK, A., TATTERSALL, M., VENUTI, A., SULLIVAN, P.,
ROBINSON, M., HOH, B., LEWIS, L. & KRAVITZ, R. L. 2017.
Effect of a Patient-Centered Communication Interven-
tion on Oncologist-Patient Communication, Quality of
Life, and Health Care Utilization in Advanced Cancer: The
VOICE Randomized Clinical Trial. JAMA Oncol, 3, 92-100.
EVANS, V. A., VAN DER SLUIS, R. M., SOLOMON, A., DAN-
TANARAYANA, A., MCNEIL, C., GARSIA, R., PALMER, S., FRO-
MENTIN, R., CHOMONT, N., SEKALY, R. P., CAMERON, P. U. &
LEWIN, S. R. 2018. Programmed cell death-1 contributes
to the establishment and maintenance of HIV-1 latency.
Aids, 32, 1491-1497.
FIELD, K. M., FITT, G., ROSENTHAL, M. A., SIMES, J., NOWAK,
A. K., BARNES, E. H., SAWKINS, K., GOH, C., MOFFAT, B. A.,
SALINAS, S., CHER, L., WHEELER, H., HOVEY, E. J. & PHAL, P.
M. 2017. Comparison between site and central radiolog-
ical assessments for patients with recurrent glioblastoma
on a clinical trial. Asia Pac J Clin Oncol.
FIELD, K. M., KING, M. T., SIMES, J., ESPINOZA, D., BARNES,
E. H., SAWKINS, K., ROSENTHAL, M. A., CHER, L., HOVEY, E.,
WHEELER, H. & NOWAK, A. K. 2017. Health-related qual-
ity of life outcomes from CABARET: a randomized phase
2 trial of carboplatin and bevacizumab in recurrent glio-
blastoma. J Neurooncol, 133, 623-631.
FIELD, K. M., PHAL, P. M., FITT, G., GOH, C., NOWAK, A. K.,
ROSENTHAL, M. A., SIMES, J., BARNES, E. H., SAWKINS, K.,
CHER, L. M., HOVEY, E. J. & WHEELER, H. 2017. The role of
early magnetic resonance imaging in predicting survival
on bevacizumab for recurrent glioblastoma: Results from
a prospective clinical trial (CABARET). Cancer, 123, 3576-
3582.
FRANCIS, P. A., PAGANI, O., FLEMING, G. F., WALLEY, B.
A., COLLEONI, M., LANG, I., GOMEZ, H. L., TONDINI, C.,
CIRUELOS, E., BURSTEIN, H. J., BONNEFOI, H. R., BELLET,
M., MARTINO, S., GEYER, C. E., JR., GOETZ, M. P., STEARNS,
V., PINOTTI, G., PUGLISI, F., SPAZZAPAN, S., CLIMENT, M. A.,
PAVESI, L., RUHSTALLER, T., DAVIDSON, N. E., COLEMAN,
R., DEBLED, M., BUCHHOLZ, S., INGLE, J. N., WINER, E. P.,
MAIBACH, R., RABAGLIO-PORETTI, M., RUEPP, B., DI LEO, A.,
COATES, A. S., GELBER, R. D., GOLDHIRSCH, A. & REGAN,
M. M. 2018. Tailoring Adjuvant Endocrine Therapy for Pre-
menopausal Breast Cancer. N Engl J Med, 379, 122-137.
GANDHI, L., RODRIGUEZ-ABREU, D., GADGEEL, S., ESTE-
BAN, E., FELIP, E., DE ANGELIS, F., DOMINE, M., CLINGAN, P.,
HOCHMAIR, M. J., POWELL, S. F., CHENG, S. Y., BISCHOFF,
H. G., PELED, N., GROSSI, F., JENNENS, R. R., RECK, M., HUI,
R., GARON, E. B., BOYER, M., RUBIO-VIQUEIRA, B., NOVEL-
LO, S., KURATA, T., GRAY, J. E., VIDA, J., WEI, Z., YANG, J.,
RAFTOPOULOS, H., PIETANZA, M. C. & GARASSINO, M. C.
2018. Pembrolizumab plus Chemotherapy in Metastatic
Non-Small-Cell Lung Cancer. N Engl J Med, 378, 2078-
2092.
GAO, B., LU, Y., NIEUWEBOER, A. J. M., XU, H., BEESLEY, J.,
BOERE, I., DE GRAAN, A. M., DE BRUIJN, P., GURNEY, H., C,
J. K., CHIEW, Y. E., JOHNATTY, S. E., BEALE, P., HARRISON,
M., LUCCARINI, C., CONROY, D., MATHIJSSEN, R. H. J., P, R.
H., BALLEINE, R. L., CHENEVIX-TRENCH, G., MACGREGOR,
S. & DE FAZIO, A. 2018. Genome-wide association study
of paclitaxel and carboplatin disposition in women with
epithelial ovarian cancer. Sci Rep, 8, 1508.
GARSED, D. W., ALSOP, K., FEREDAY, S., EMMANUEL, C.,
KENNEDY, C. J., ETEMADMOGHADAM, D., GAO, B., GEBSKI,
V., GARES, V., CHRISTIE, E. L., WOUTERS, M. C. A., MILNE,
K., GEORGE, J., PATCH, A. M., LI, J., ARNAU, G. M., SEMPLE,
T., GADIPALLY, S. R., CHIEW, Y. E., HENDLEY, J., MIKESKA,
T., ZAPPAROLI, G. V., AMARASINGHE, K., GRIMMOND, S.
M., PEARSON, J. V., WADDELL, N., HUNG, J., STEWART, C.
J. R., SHARMA, R., ALLAN, P. E., RAMBAU, P. F., MCNALLY,
O., MILESHKIN, L., HAMILTON, A., ANANDA, S., GROSSI, M.,
COHEN, P. A., LEUNG, Y. C., ROME, R. M., BEALE, P., BLOM-
FIELD, P., FRIEDLANDER, M., BRAND, A., DOBROVIC, A., KO-
BEL, M., HARNETT, P., NELSON, B. H., BOWTELL, D. D. L. &
DEFAZIO, A. 2018. Homologous Recombination DNA Re-
pair Pathway Disruption and Retinoblastoma Protein Loss
Are Associated with Exceptional Survival in High-Grade Se-
rous Ovarian Cancer. Clin Cancer Res, 24, 569-580.
GERBER, D. E., HORN, L., BOYER, M., SANBORN, R., NATALE,
R., PALMERO, R., BIDOLI, P., BONDARENKO, I., GERMONPRE,
P., GHIZDAVESCU, D., KOTSAKIS, A., LENA, H., LOSONCZY,
G., PARK, K., SU, W. C., TANG, M., LAI, J., KALLINTERIS, N. L.,
SHAN, J. S., RECK, M. & SPIGEL, D. R. 2018. Randomized
phase III study of docetaxel plus bavituximab in previously
treated advanced non-squamous non-small-cell lung can-
cer. Ann Oncol, 29, 1548-1553.
GLIGOROV, J., ATASEVEN, B., VERRILL, M., DE LAURENTI-
IS, M., JUNG, K. H., AZIM, H. A., AL-SAKAFF, N., LAUER, S.,
SHING, M. & PIVOT, X. 2017. Safety and tolerability of
subcutaneous trastuzumab for the adjuvant treatment of
RESEARCH REPORT 2017 & 2018
human epidermal growth factor receptor 2-positive early
breast cancer: SafeHer phase III study's primary analysis of
2573 patients. Eur J Cancer, 82, 237-246.
GROGAN, J., GUPTA, R., MAHON, K. L., STRICKER, P. D.,
HAYNES, A. M., DELPRADO, W., TURNER, J., HORVATH, L. G.
& KENCH, J. G. 2017. Predictive value of the 2014 Inter-
national Society of Urological Pathology grading system
for prostate cancer in patients undergoing radical prosta-
tectomy with long-term follow-up. BJU Int, 120, 651-658.
HALVORSEN, A. R., KRISTENSEN, G., EMBLETON, A., ADU-
SEI, C., BARRETINA-GINESTA, M. P., BEALE, P. & HELLAND,
A. 2017. Evaluation of Prognostic and Predictive Signif-
icance of Circulating MicroRNAs in Ovarian Cancer Pa-
tients. Dis Markers, 2017, 3098542.
HAYNE, D., STOCKLER, M., MCCOMBIE, S. P., LAWRENCE,
N., MARTIN, A., SENGUPTA, S. & DAVIS, I. D. 2017. BCG +
Mitomycin trial for high-risk non-muscle-invasive bladder
cancer: progress report and lessons learned. BJU Int, 119
Suppl 5, 55-57.
HEINIGER, L. E., SMITH, A. B., OLVER, I., GRIMISON, P., KLEIN,
B., WOOTTEN, A., ABBOTT, J. M., PRICE, M. A., MCJANNETT,
M., TRAN, B., STOCKLER, M. R., GURNEY, H. & BUTOW, P.
N. 2017. e-TC: Development and pilot testing of a web-
based intervention to reduce anxiety and depression in
survivors of testicular cancer. Eur J Cancer Care (Engl), 26.
HERZOG, S., SHANAHAN, M., GRIMISON, P., TRAN, A.,
WONG, N., LINTZERIS, N., SIMES, J., STOCKLER, M. & MOR-
TON, R. L. 2018. Systematic Review of the Costs and
Benefits of Prescribed Cannabis-Based Medicines for the
Management of Chronic Illness: Lessons from Multiple
Sclerosis. Pharmacoeconomics, 36, 67-78.
HORN, L., MANSFIELD, A. S., SZCZESNA, A., HAVEL, L.,
KRZAKOWSKI, M., HOCHMAIR, M. J., HUEMER, F., LOSON-
CZY, G., JOHNSON, M. L., NISHIO, M., RECK, M., MOK, T.,
LAM, S., SHAMES, D. S., LIU, J., DING, B., LOPEZ-CHAVEZ, A.,
KABBINAVAR, F., LIN, W., SANDLER, A. & LIU, S. V. 2018. First-
Line Atezolizumab plus Chemotherapy in Extensive-Stage
Small-Cell Lung Cancer. N Engl J Med, 379, 2220-2229.
INVESTIGATORS, O. B. O. C. C., LIVINGSTONE, A., NOWAK,
A. K., GOH, C., BARNES, E. H., WHEELER, H., SIMES, J.,
SAWKINS, K., FIELD, K. M., CHER, L., ROSENTHAL, M. A.,
PHAL, P. & HOVEY, E. J. 2017. Continuing or ceasing bev-
acizumab beyond progression in recurrent glioblastoma:
an exploratory randomized phase II trial. Neuro-Oncology
Practice, 4, 171-181.
IP, E., POKORNY, A. M. J., DELLA-FIORENTINA, S., BEALE, P.,
BRAY, V., KIELY, B. E. & BLINMAN, P. 2017. Use of palliative
chemotherapy in patients aged 80 years and over with
incurable cancer: experience at three Sydney cancer cen-
tres. Internal Medicine Journal, 47, 75-81.
JOHNSON, S., BUTOW, P., BELL, M., DETERING, K., CLAY-
TON, J., SILVESTER, W., KIELY, B. E., CLARKE, S., VACCARO,
L., STOCKLER, M., BEALE, P., TATTERSALL, M. & ET AL. 2018.
A randomised controlled trial of an advance care planning
intervention for patients with incurable cancer. British
Journal of Cancer, 119, 1182-1190.
JOHNSON, S., KERRIDGE, I., BUTOW, P. N. & TATTERSALL, M.
H. 2017. Advance Care Planning: is quality end of life care
really that simple? Intern Med J, 47, 390-394.
JOHNSON, S., KERRIDGE, I., BUTOW, P. N. & TATTERSALL, M.
H. N. 2017. Author reply. Intern Med J, 47, 1092.
JOHNSON, S. B., BUTOW, P. N., KERRIDGE, I., BELL, M. L. &
TATTERSALL, M. H. N. 2018. How Well Do Current Meas-
ures Assess the Impact of Advance Care Planning on Con-
cordance Between Patient Preferences for End-of-Life
Care and the Care Received: A Methodological Review. J
Pain Symptom Manage, 55, 480-495.
JOHNSON, S. B., BUTOW, P. N., KERRIDGE, I. & TATTERSALL,
M. H. 2017. What do patients with cancer and their fam-
ilies value most at the end of life? A critical analysis of
advance care planning. Int J Palliat Nurs, 23, 596-604.
JOHNSON, S. B., BUTOW, P. N., KERRIDGE, I. & TATTERSALL,
M. H. N. 2018. Patient autonomy and advance care plan-
ning: a qualitative study of oncologist and palliative care
physicians' perspectives. Support Care Cancer, 26, 565-
574.
JOHNSON, T. G., SCHELCH, K., CHENG, Y. Y., WILLIAMS, M.,
SARUN, K. H., KIRSCHNER, M. B., KAO, S., LINTON, A., KLEBE,
S., MCCAUGHAN, B. C., LIN, R. C. Y., PIRKER, C., BERGER, W.,
LASHAM, A., VAN ZANDWIJK, N. & REID, G. 2018. Dysreg-
ulated Expression of the MicroRNA miR-137 and Its Target
YBX1 Contribute to the Invasive Characteristics of Malig-
nant Pleural Mesothelioma. J Thorac Oncol, 13, 258-272.
JONKER, D. J., NOTT, L., YOSHINO, T., GILL, S., SHAPIRO, J.,
50
CHRIS O'BRIEN LIFEHOUSE
51
OHTSU, A., ZALCBERG, J., VICKERS, M. M., WEI, A. C., GAO,
Y., TEBBUTT, N. C., MARKMAN, B., PRICE, T., ESAKI, T., KO-
SKI, S., HITRON, M., LI, W., LI, Y., MAGOSKI, N. M., LI, C. J.,
SIMES, J., TU, D. & O'CALLAGHAN, C. J. 2018. Napabucasin
versus placebo in refractory advanced colorectal cancer:
a randomised phase 3 trial. Lancet Gastroenterol Hepatol,
3, 263-270.
KALSBEEK, A. M. F., CHAN, E. K. F., GROGAN, J., PETERSEN, D.
C., JARATLERDSIRI, W., GUPTA, R., LYONS, R. J., HAYNES, A.
M., HORVATH, L. G., KENCH, J. G., STRICKER, P. D. & HAYES,
V. M. 2018. Altered mitochondrial genome content sig-
nals worse pathology and prognosis in prostate cancer.
Prostate, 78, 25-31.
KANDULA, T., FARRAR, M. A., KIERNAN, M. C., KRISHNAN, A.
V., GOLDSTEIN, D., HORVATH, L., GRIMISON, P., BOYLE, F.,
BARON-HAY, S. & PARK, S. B. 2017. Neurophysiological and
clinical outcomes in chemotherapy-induced neuropathy
in cancer. Clin Neurophysiol, 128, 1166-1175.
KAO, S. C., CHENG, Y. Y., WILLIAMS, M., KIRSCHNER, M.
B., MADORE, J., LUM, T., SARUN, K. H., LINTON, A., MC-
CAUGHAN, B., KLEBE, S., VAN ZANDWIJK, N., SCOLYER, R.
A., BOYER, M. J., COOPER, W. A. & REID, G. 2017. Tumor
Suppressor microRNAs Contribute to the Regulation of PD-
L1 Expression in Malignant Pleural Mesothelioma. J Thorac
Oncol, 12, 1421-1433.
KARAPETIS, C. S., GUCCIONE, L., TATTERSALL, M. H., GOOD-
EN, H., VAJDIC, C. M., LAMBERT, S., ROBOTIN, M., MILESH-
KIN, L. & SCHOFIELD, P. 2017. Perceptions of cancer of
unknown primary site: a national survey of Australian
medical oncologists. Intern Med J, 47, 408-414.
KARIKIOS, D. J., CHIM, L., MARTIN, A., NAGRIAL, A., HOW-
ARD, K., SALKELD, G. & STOCKLER, M. R. 2017. Is it all
about price? Why requests for government subsidy of an-
ticancer drugs were rejected in Australia. Intern Med J,
47, 400-407.
KARIKIOS, D. J., MILESHKIN, L., MARTIN, A., FERRARO, D. &
STOCKLER, M. R. 2017. Discussing and prescribing expen-
sive unfunded anticancer drugs in Australia. ESMO Open,
2, e000170.
KING, M. T., STOCKLER, M. R., O'CONNELL, R. L., BUIZEN, L.,
JOLY, F., LANCELEY, A., HILPERT, F., OKAMOTO, A., AOTANI,
E., BRYCE, J., DONNELLAN, P., OZA, A., AVALL-LUNDQVIST,
E., BEREK, J. S., SEHOULI, J., FEENEY, A., BERTON-RIGAUD,
D., COSTA, D. S. J. & FRIEDLANDER, M. L. 2018. Measuring
what matters MOST: validation of the Measure of Ovarian
Symptoms and Treatment, a patient-reported outcome
measure of symptom burden and impact of chemother-
apy in recurrent ovarian cancer. Qual Life Res, 27, 59-74.
KING, M. T., VINEY, R., SIMON PICKARD, A., ROWEN, D.,
AARONSON, N. K., BRAZIER, J. E., CELLA, D., COSTA, D. S.
J., FAYERS, P. M., KEMMLER, G., MCTAGGART-COWEN, H.,
MERCIECA-BEBBER, R., PEACOCK, S., STREET, D. J., YOUNG,
T. A. & NORMAN, R. 2018. Australian Utility Weights for
the EORTC QLU-C10D, a Multi-Attribute Utility Instrument
Derived from the Cancer-Specific Quality of Life Question-
naire, EORTC QLQ-C30. Pharmacoeconomics, 36, 225-
238.
KONDRASHOVA, O., TOPP, M., NESIC, K., LIESCHKE, E., HO,
G. Y., HARRELL, M. I., ZAPPAROLI, G. V., HADLEY, A., HOLIAN,
R., BOEHM, E., HEONG, V., SANIJ, E., PEARSON, R. B., KRAIS,
J. J., JOHNSON, N., MCNALLY, O., ANANDA, S., ALSOP, K.,
HUTT, K. J., KAUFMANN, S. H., LIN, K. K., HARDING, T. C.,
TRAFICANTE, N., DEFAZIO, A., MCNEISH, I. A., BOWTELL,
D. D., SWISHER, E. M., DOBROVIC, A., WAKEFIELD, M. J. &
SCOTT, C. L. 2018. Methylation of all BRCA1 copies pre-
dicts response to the PARP inhibitor rucaparib in ovarian
carcinoma. Nat Commun, 9, 3970.
KRESOJA-RAKIC, J., SULEMANI, M., KIRSCHNER, M. B., RON-
NER, M., REID, G., KAO, S., SCHWALLER, B., WEDER, W.,
STAHEL, R. A. & FELLEY-BOSCO, E. 2017. Posttranscription-
al Regulation Controls Calretinin Expression in Malignant
Pleural Mesothelioma. Front Genet, 8, 70.
LAU, B., KUMAR, S., YAN, T., BURN, J., KENNEDY, C., MCLEAN,
J., BOYER, M., MCCAUGHAN, B. & KAO, S. 2017. Pathologi-
cal complete response in malignant pleural mesothelioma
patients following induction chemotherapy: Predictive
factors and outcomes. Lung Cancer, 111, 75-78.
LAWRENCE, N. J., CHAN, H., TONER, G., STOCKLER, M. R.,
MARTIN, A., YIP, S., WONG, N., YEUNG, A., MAZHAR, D.,
PASHANKAR, F., FRAZIER, L., MCDERMOTT, R., WALKER, R.,
TAN, H., DAVIS, I. D. & GRIMISON, P. 2018. Protocol for the
P3BEP trial (ANZUP 1302): an international randomised
phase 3 trial of accelerated versus standard BEP chemo-
therapy for adult and paediatric male and female patients
with intermediate and poor-risk metastatic germ cell tu-
mours. BMC Cancer, 18, 854.
LAWRENCE, N. J., MARTIN, A., DAVIS, I. D., TROON, S., SEN-
RESEARCH REPORT 2017 & 2018
GUPTA, S., HOVEY, E., COSKINAS, X., KAPLAN, R., SMITH, B.,
RITCHIE, A., MEADE, A., EISEN, T., BLINMAN, P. & STOCKLER,
M. R. 2018. What Survival Benefits are Needed to Make
Adjuvant Sorafenib Worthwhile After Resection of Inter-
mediate- or High-Risk Renal Cell Carcinoma? Clinical In-
vestigators' Preferences in the SORCE Trial. Kidney Cancer,
2, 123-131.
LEONG, T., SMITHERS, B. M., HAUSTERMANS, K., MICHAEL,
M., GEBSKI, V., MILLER, D., ZALCBERG, J., BOUSSIOUTAS,
A., FINDLAY, M., O'CONNELL, R. L., VERGHIS, J., WILLIS, D.,
KRON, T., CRAIN, M., MURRAY, W. K., LORDICK, F., SWAL-
LOW, C., DARLING, G., SIMES, J. & WONG, R. 2017. TOP-
GEAR: A Randomized, Phase III Trial of Perioperative ECF
Chemotherapy with or Without Preoperative Chemoradia-
tion for Resectable Gastric Cancer: Interim Results from an
International, Intergroup Trial of the AGITG, TROG, EORTC
and CCTG. Ann Surg Oncol, 24, 2252-2258.
LEVY, D., DHILLON, H. M., LOMAX, A., MARTHICK, M., MC-
NEIL, C., KAO, S. & LACEY, J. 2018. Certainty within uncer-
tainty: a qualitative study of the experience of metastatic
melanoma patients undergoing pembrolizumab immuno-
therapy. Support Care Cancer. *
LIM, E., BEITH, J., BOYLE, F., DE BOER, R., HUI, R., MCCAR-
THY, N., REDFERN, A., WADE, T. & WOODWARD, N. 2018.
Emerging data and future directions for CDK4/6 inhibi-
tor treatment of patients with hormone receptor positive
HER2-non-amplified metastatic breast cancer. Asia Pac J
Clin Oncol, 14 Suppl 4, 12-21.
LIM, K., VAN DYK, S., KHAW, P., VEERA, J., MILESHKIN, L.,
OHANESSIAN, L., HARRISON, M. & VINOD, S. K. 2017. Pat-
terns of practice survey for brachytherapy for cervix can-
cer in Australia and New Zealand. J Med Imaging Radiat
Oncol, 61, 674-681.
LIN, H. M., LEE, B. Y., CASTILLO, L., SPIELMAN, C., GROGAN,
J., YEUNG, N. K., KENCH, J. G., STRICKER, P. D., HAYNES,
A. M., CENTENERA, M. M., BUTLER, L. M., SHREEVE, S. M.,
HORVATH, L. G. & DALY, R. J. 2018. Effect of FAK inhibi-
tor VS-6063 (defactinib) on docetaxel efficacy in prostate
cancer. Prostate, 78, 308-317.
LIN, H. M., MAHON, K. L., SPIELMAN, C., GURNEY, H.,
MALLESARA, G., STOCKLER, M. R., BASTICK, P., BRISCOE, K.,
MARX, G., SWARBRICK, A. & HORVATH, L. G. 2017. Phase 2
study of circulating microRNA biomarkers in castration-re-
sistant prostate cancer. Br J Cancer, 116, 1002-1011.
LIN, H. M., MAHON, K. L., WEIR, J. M., MUNDRA, P. A., SPIEL-
MAN, C., BRISCOE, K., GURNEY, H., MALLESARA, G., MARX,
G., STOCKLER, M. R., CONSORTIUM, P. R., PARTON, R. G.,
HOY, A. J., DALY, R. J., MEIKLE, P. J. & HORVATH, L. G. 2017.
A distinct plasma lipid signature associated with poor
prognosis in castration-resistant prostate cancer. Int J Can-
cer, 141, 2112-2120.
LIN, H. M., NIKOLIC, I., YANG, J., CASTILLO, L., DENG, N.,
CHAN, C. L., YEUNG, N. K., DODSON, E., ELSWORTH, B.,
SPIELMAN, C., LEE, B. Y., BOYER, Z., SIMPSON, K. J., DALY,
R. J., HORVATH, L. G. & SWARBRICK, A. 2018. MicroRNAs
as potential therapeutics to enhance chemosensitivity in
advanced prostate cancer. Sci Rep, 8, 7820.
LINDEMANN, K., KOK, P. S., STOCKLER, M., JAABACK, K. &
BRAND, A. 2017. Enhanced Recovery After Surgery for Ad-
vanced Ovarian Cancer: A Systematic Review of Interven-
tions Trialed. Int J Gynecol Cancer, 27, 1274-1282.
LINDEMANN, K., KOK, P. S., STOCKLER, M., SYKES, P. &
BRAND, A. 2017. Enhanced Recovery After Surgery for
Suspected Ovarian Malignancy: A Survey of Perioperative
Practice Among Gynecologic Oncologists in Australia and
New Zealand to Inform a Clinical Trial. Int J Gynecol Can-
cer, 27, 1046-1050.
LINTON, A., SOEBERG, M., BROOME, R., KAO, S. & VAN
ZANDWIJK, N. 2017. Geographic and socioeconomic
factors in patients with malignant pleural mesothelioma
in New South Wales and their impact upon clinical out-
comes. Respirology, 22, 978-985.
LIU, R. C., SEBARATNAM, D. F., JACKETT, L., KAO, S. &
LOWE, P. M. 2018. Subacute cutaneous lupus erythema-
tosus induced by nivolumab. Australas J Dermatol, 59,
e152-e154.
LOMAX, A. J., LIM, J., CHENG, R., SWEETING, A., LOWE, P.,
MCGILL, N., SHACKEL, N., CHUA, E. L. & MCNEIL, C. 2018.
Immune Toxicity with Checkpoint Inhibition for Metastatic
Melanoma: Case Series and Clinical Management. J Skin
Cancer, 2018, 9602540.
LOMAX, A. J., MCGUIRE, H. M., MCNEIL, C., CHOI, C. J.,
HERSEY, P., KARIKIOS, D., SHANNON, K., VAN HAL, S., CARR,
U., CROTTY, A., GUPTA, S. K., HOLLINGSWORTH, J., KIM, H.,
FAZEKAS DE ST GROTH, B. & MCGILL, N. 2017. Immuno-
therapy-induced sarcoidosis in patients with melanoma
treated with PD-1 checkpoint inhibitors: Case series and
52
CHRIS O'BRIEN LIFEHOUSE
53
immunophenotypic analysis. Int J Rheum Dis, 20, 1277-
1285. *
LOMAX, A. J. & MCNEIL, C. 2017. Acute management of
autoimmune toxicity in cancer patients on immunother-
apy: Common toxicities and the approach for the emer-
gency physician. Emerg Med Australas, 29, 245-251.
LOMAX, A. J., NIELSEN, T., VISINTIN, L., O'CARRIGAN, B.,
HONEYBALL, F., SHUM, B., SAW, R. P. M. & MCNEIL, C.
2017. Clinical Nurse Consultant Support: Management of
Patients With Melanoma Receiving Immunotherapy and
Targeted Therapy. Clin J Oncol Nurs, 21, E93-e98.
LONG, G. V., ATKINSON, V., CEBON, J. S., JAMESON, M. B.,
FITZHARRIS, B. M., MCNEIL, C. M., HILL, A. G., RIBAS, A.,
ATKINS, M. B., THOMPSON, J. A., HWU, W. J., HODI, F. S.,
MENZIES, A. M., GUMINSKI, A. D., KEFFORD, R., KONG, B.
Y., TAMJID, B., SRIVASTAVA, A., LOMAX, A. J., ISLAM, M.,
SHU, X., EBBINGHAUS, S., IBRAHIM, N. & CARLINO, M. S.
2017. Standard-dose pembrolizumab in combination
with reduced-dose ipilimumab for patients with advanced
melanoma (KEYNOTE-029): an open-label, phase 1b trial.
Lancet Oncol, 18, 1202-1210.
LONG, G. V., WEBER, J. S., LARKIN, J., ATKINSON, V.,
GROB, J. J., SCHADENDORF, D., DUMMER, R., ROBERT, C.,
MARQUEZ-RODAS, I., MCNEIL, C., SCHMIDT, H., BRISCOE,
K., BAURAIN, J. F., HODI, F. S. & WOLCHOK, J. D. 2017.
Nivolumab for Patients With Advanced Melanoma Treat-
ed Beyond Progression: Analysis of 2 Phase 3 Clinical Tri-
als. JAMA Oncol, 3, 1511-1519.
MAHON, K. L., QU, W., LIN, H. M., SPIELMAN, C., CAIN, D.,
JACOBS, C., STOCKLER, M. R., HIGANO, C. S., DE BONO, J.
S., CHI, K. N., CLARK, S. J. & HORVATH, L. G. 2018. Serum
Free Methylated Glutathione S-transferase 1 DNA Levels,
Survival, and Response to Docetaxel in Metastatic, Castra-
tion-resistant Prostate Cancer: Post Hoc Analyses of Data
from a Phase 3 Trial. Eur Urol.
MALALASEKERA, A., BLINMAN, P. L., DHILLON, H. M., STE-
FANIC, N. A., GRIMISON, P., JAIN, A., D'SOUZA, M., KAO, S.
C. & VARDY, J. L. 2018. Times to Diagnosis and Treatment
of Lung Cancer in New South Wales, Australia: A Multi-
center, Medicare Data Linkage Study. J Oncol Pract, 14,
e621-e630.
MALALASEKERA, A., DHILLON, H. M., BLINMAN, P. L., KAO,
S. C. & VARDY, J. L. 2018. Delays to diagnosis and treat-
ment of lung cancer in Australia: healthcare professional
perceptions of actual versus acceptable timeframes. In-
tern Med J, 48, 1063-1071.
MALALASEKERA, A., NAHM, S., BLINMAN, P. L., KAO, S. C.,
DHILLON, H. M. & VARDY, J. L. 2018. How long is too long?
A scoping review of health system delays in lung cancer.
Eur Respir Rev, 27.
MARTIN, A. J., GIBBS, E., SJOQUIST, K., PAVLAKIS, N., SIMES,
J., PRICE, T., SHANNON, J., GILL, S., JAIN, V., LIU, G., KAN-
NOURAKIS, G., KIM, Y. H., KIM, J. W. & GOLDSTEIN, D. 2017.
Health-related quality of life associated with regorafenib
treatment in refractory advanced gastric adenocarcino-
ma. Gastric Cancer.
MARTIN, A. J., GIBBS, E., SJOQUIST, K., PAVLAKIS, N., SIMES,
J., PRICE, T., SHANNON, J., GILL, S., JAIN, V., LIU, G., KAN-
NOURAKIS, G., KIM, Y. H., KIM, J. W. & GOLDSTEIN, D. 2018.
Health-related quality of life associated with regorafenib
treatment in refractory advanced gastric adenocarcino-
ma. Gastric Cancer, 21, 473-480.
MCBRIDE, K. A., BALLINGER, M. L., SCHLUB, T. E., YOUNG,
M. A., TATTERSALL, M. H. N., KIRK, J., EELES, R., KILLICK, E.,
WALKER, L. G., SHANLEY, S., THOMAS, D. M. & MITCHELL, G.
2017. Psychosocial morbidity in TP53 mutation carriers:
is whole-body cancer screening beneficial? Fam Cancer,
16, 423-432.
MCCRARY, J. M., GOLDSTEIN, D., BOYLE, F., COX, K., GRIM-
ISON, P., KIERNAN, M. C., KRISHNAN, A. V., LEWIS, C. R.,
WEBBER, K., BARON-HAY, S., HORVATH, L. & PARK, S. B.
2017. Optimal clinical assessment strategies for chemo-
therapy-induced peripheral neuropathy (CIPN): a system-
atic review and Delphi survey. Support Care Cancer, 25,
3485-3493.
MCNEIL, C. 2017. The aftermath of loss. Med J Aust, 207,
476-477.
MCNEIL, C. M. 2017. Banter. J Clin Oncol, 35, 3262-3263.
MCNEIL, C. M. 2018. A Cup of Coffee. N Engl J Med, 379,
312-313.
MCNEIL, C. M. 2018. The Gift. J Am Geriatr Soc, 66, 1437-
1438.
MCNEIL, C. M. 2018. Grace and Forgiveness. J Clin Oncol,
RESEARCH REPORT 2017 & 2018
36, 1045-1046.
MCNEIL, C. M. & HARNETT, P. R. 2017. Our Faustian pact
with the digital world. Lancet Oncol, 18, 171-172.
MCNEIL, C. M. & TATTERSALL, M. H. N. 2017. Bereaved
and aggrieved in the age of social media. Lancet Oncol,
18, 1008.
MCNEIL, C. M. & TATTERSALL, M. H. N. 2017. Misunder-
standings, mandatory biopsies, and conflicts of interests
in clinical trials: a coercive cocktail? Lancet Oncol, 18,
851-852.
MERCIECA-BEBBER, R., CALVERT, M., KYTE, D., STOCKLER,
M. & KING, M. T. 2018. The administration of patient-re-
ported outcome questionnaires in cancer trials: Interviews
with trial coordinators regarding their roles, experiences,
challenges and training. Contemp Clin Trials Commun, 9,
23-32.
MERCIECA-BEBBER, R., FRIEDLANDER, M., CALVERT, M.,
STOCKLER, M., KYTE, D., KOK, P. S. & KING, M. T. 2017. A
systematic evaluation of compliance and reporting of pa-
tient-reported outcome endpoints in ovarian cancer ran-
domised controlled trials: implications for generalisability
and clinical practice. J Patient Rep Outcomes, 1, 5.
MERCIECA-BEBBER, R., FRIEDLANDER, M., KOK, P. S., CAL-
VERT, M., KYTE, D., STOCKLER, M. & KING, M. T. 2017.
Erratum to: The patient-reported outcome content of
international ovarian cancer randomised controlled trial
protocols. Qual Life Res, 26, 2249-2250.
MERSIADES, A. J., STOCKLER, M. R., OLVER, I. N. & GRIMI-
SON, P. 2018. Medicinal cannabis for chemotherapy-in-
duced nausea and vomiting: prescribing with limited evi-
dence. Med J Aust.
MERSIADES, A. J., TOGNELA, A., HABER, P. S., STOCKLER,
M., LINTZERIS, N., SIMES, J., MCGREGOR, I., OLVER, I., ALL-
SOP, D. J., GEDYE, C., KIRBY, A. C., MORTON, R. L., FOX,
P., CLARKE, S., BRISCOE, K., AGHMESHEH, M., WONG, N.,
WALSH, A., HAHN, C. & GRIMISON, P. 2018. Oral cannab-
inoid-rich THC/CBD cannabis extract for secondary pre-
vention of chemotherapy-induced nausea and vomiting:
a study protocol for a pilot and definitive randomised
double-blind placebo-controlled trial (CannabisCINV). BMJ
Open, 8, e020745.
METAXAS, Y., RIVALLAND, G., MAUTI, L. A., KLINGBIEL, D.,
KAO, S., SCHMID, S., NOWAK, A. K., GAUTSCHI, O., BART-
NICK, T., HUGHES, B. G., BOUCHAAB, H., ROTHSCHILD, S.
I., PAVLAKIS, N., WOLLEB, S., PETRAUSCH, U., O'BYRNE, K.,
FROESCH, P., LOFFLER-BAUMANN, M., PRATSCH-PETER, S.,
RUSSELL, P., MINGRONE, W., SAVIC, S., THAPA, B., FRUH, M.,
PLESS, M., VON MOOS, R. & JOHN, T. 2018. Pembrolizum-
ab as Palliative Immunotherapy in Malignant Pleural Meso-
thelioma. J Thorac Oncol, 13, 1784-1791.
MOTH, E. B., KIELY, B. E., STEFANIC, N., NAGANATHAN, V.,
MARTIN, A., GRIMISON, P., STOCKLER, M. R., BEALE, P. &
BLINMAN, P. 2018. Oncologists' perceptions on the use-
fulness of geriatric assessment measures and the CARG
toxicity score when prescribing chemotherapy for older
patients with cancer. J Geriatr Oncol.
MOTH, E. B., KIELY, B. E., STEFANIC, N., NAGANATHAN, V.,
MARTIN, A., GRIMISON, P., STOCKLER, M. R., BEALE, P. &
BLINMAN, P. 2018. Predicting chemotherapy toxicity in
older adults: Comparing the predictive value of the CARG
Toxicity Score with oncologists' estimates of toxicity based
on clinical judgement. J Geriatr Oncol.
NAIR, S. S., LUU, P. L., QU, W., MADDUGODA, M., HUSCHTS-
CHA, L., REDDEL, R., CHENEVIX-TRENCH, G., TOSO, M.,
KENCH, J. G., HORVATH, L. G., HAYES, V. M., STRICKER, P. D.,
HUGHES, T. P., WHITE, D. L., RASKO, J. E. J., WONG, J. J. &
CLARK, S. J. 2018. Guidelines for whole genome bisulphite
sequencing of intact and FFPET DNA on the Illumina HiSeq
X Ten. Epigenetics Chromatin, 11, 24.
NGUYEN, E. V., CENTENERA, M. M., MOLDOVAN, M., DAS,
R., IRANI, S., VINCENT, A. D., CHAN, H., HORVATH, L. G.,
LYNN, D. J., DALY, R. J. & BUTLER, L. M. 2018. Identification
of Novel Response and Predictive Biomarkers to Hsp90
Inhibitors Through Proteomic Profiling of Patient-derived
Prostate Tumor Explants. Mol Cell Proteomics, 17, 1470-
1486.
NIKOLIC, I., ELSWORTH, B., DODSON, E., WU, S. Z., GOULD,
C. M., MESTDAGH, P., MARSHALL, G. M., HORVATH, L. G.,
SIMPSON, K. J. & SWARBRICK, A. 2017. Discovering cancer
vulnerabilities using high-throughput micro-RNA screen-
ing. Nucleic Acids Res, 45, 12657-12670.
O'CARRIGAN, B., WONG, M. H., WILLSON, M. L., STOCKLER,
M. R., PAVLAKIS, N. & GOODWIN, A. 2017. Bisphospho-
nates and other bone agents for breast cancer. Cochrane
Database Syst Rev, 10, Cd003474.
54
CHRIS O'BRIEN LIFEHOUSE
55
PARK, S., KWOK, J., ASHER, R., LEE, C. K., BEALE, P., SELLE,
F. & FRIEDLANDER, M. 2017. Clinical and genetic predic-
tors of paclitaxel neurotoxicity based on patient- versus
clinician reported incidence and severity of neurotoxicity
in the ICON7 trial. Annals of Oncology, 28, 2733-2740.
PARK, S. B., KWOK, J. B., ASHER, R., LEE, C. K., BEALE, P.,
SELLE, F. & FRIEDLANDER, M. 2017. Clinical and genetic
predictors of paclitaxel neurotoxicity based on patient-
versus clinician-reported incidence and severity of neu-
rotoxicity in the ICON7 trial. Ann Oncol, 28, 2733-2740.
PAZ-ARES, L., TAN, E. H., O'BYRNE, K., ZHANG, L., HIRSH, V.,
BOYER, M., YANG, J. C., MOK, T., LEE, K. H., LU, S., SHI, Y.,
LEE, D. H., LASKIN, J., KIM, D. W., LAURIE, S. A., KOLBECK,
K., FAN, J., DODD, N., MARTEN, A. & PARK, K. 2017. Afatin-
ib versus gefitinib in patients with EGFR mutation-positive
advanced non-small-cell lung cancer: overall survival data
from the phase IIb LUX-Lung 7 trial. Ann Oncol, 28, 270-
277.
PIDSLEY, R., LAWRENCE, M. G., ZOTENKO, E., NIRANJAN, B.,
STATHAM, A., SONG, J., CHABANON, R. M., QU, W., WANG,
H., RICHARDS, M., NAIR, S. S., ARMSTRONG, N. J., NIM, H.
T., PAPARGIRIS, M., BALANATHAN, P., FRENCH, H., PETERS,
T., NORDEN, S., RYAN, A., PEDERSEN, J., KENCH, J., DALY,
R. J., HORVATH, L. G., STRICKER, P., FRYDENBERG, M., TAY-
LOR, R. A., STIRZAKER, C., RISBRIDGER, G. P. & CLARK, S. J.
2018. Enduring epigenetic landmarks define the cancer
microenvironment. Genome Res, 28, 625-638.
PO, J. W., ROOHULLAH, A., LYNCH, D., DEFAZIO, A., HAR-
RISON, M., HARNETT, P. R., KENNEDY, C., DE SOUZA, P. &
BECKER, T. M. 2018. Improved ovarian cancer EMT-CTC
isolation by immunomagnetic targeting of epithelial Ep-
CAM and mesenchymal N-cadherin. J Circ Biomark, 7,
1849454418782617.
PRASANNA, T., BEITH, J., KAO, S., BOYER, M. & MCNEIL, C.
M. 2018. Dose modifications in adjuvant chemotherapy
for solid organ malignancies: A systematic review of clini-
cal trials. Asia Pac J Clin Oncol, 14, 125-133.
PRASANNA, T., MCNEIL, C. M., NIELSEN, T. & PARKIN, D.
2018. Isolated immune-related pancreatic exocrine in-
sufficiency associated with pembrolizumab therapy. Im-
munotherapy, 10, 171-175.
QUINN, D. I., SANDLER, H. M., HORVATH, L. G., GOLDKO-
RN, A. & EASTHAM, J. A. 2017. The evolution of chemo-
therapy for the treatment of prostate cancer. Ann Oncol,
28, 2658-2669.
RANKIN, N., LAI, M., MILLER, D., BEALE, P., SPIGELMAN, A.,
PREST, G., TURLEY, K. & SIMES, R. J. 2018. Cancer multi-
disciplinary team meetings in practice: Results from a
multi-institutional quantitative survey and implications for
policy change. Asia-Pacific Journal of Clinical Oncology,
14, 74-83.
RANKIN, N. M., COLLETT, G. K., BROWN, C. M., SHAW, T.
J., WHITE, K. M., BEALE, P. J., TREVENA, L. J., ANDERIESZ, C.
& BARNES, D. J. 2017. Implementation of a lung cancer
multidisciplinary team standardised template for report-
ing to general practitioners: a mixed-method study. BMJ
Open, 7, e018629.
RANKIN, N. M., LAI, M., MILLER, D., BEALE, P., SPIGELMAN,
A., PREST, G., TURLEY, K. & SIMES, J. 2018. Cancer multi-
disciplinary team meetings in practice: Results from a
multi-institutional quantitative survey and implications for
policy change. Asia Pac J Clin Oncol, 14, 74-83.
RICCIARDELLI, C., BIANCO-MIOTTO, T., JINDAL, S., BUTLER,
L. M., LEUNG, S., MCNEIL, C. M., O'TOOLE, S. A., EBRA-
HIMIE, E., MILLAR, E. K. A., SAKKO, A. J., RUIZ, A. I., VOWLER,
S. L., HUNTSMAN, D. G., BIRRELL, S. N., SUTHERLAND, R. L.,
PALMIERI, C., HICKEY, T. E. & TILLEY, W. D. 2018. The Mag-
nitude of Androgen Receptor Positivity in Breast Cancer Is
Critical for Reliable Prediction of Disease Outcome. Clin
Cancer Res, 24, 2328-2341.
RONCOLATO, F. T., BERTON-RIGAUD, D., O'CONNELL,
R., LANCELEY, A., SEHOULI, J., BUIZEN, L., OKAMOTO, A.,
AOTANI, E., LORUSSO, D., DONNELLAN, P., OZA, A., AV-
ALL-LUNDQVIST, E., BEREK, J., HILPERT, F., LEDERMANN,
J. A., KAMINSKY, M. C., STOCKLER, M. R., KING, M. T. &
FRIEDLANDER, M. 2018. Validation of the modified Glas-
gow Prognostic Score (mGPS) in recurrent ovarian cancer
(ROC) - Analysis of patients enrolled in the GCIG Symptom
Benefit Study (SBS). Gynecol Oncol, 148, 36-41.
RONCOLATO, F. T., GIBBS, E., LEE, C. K., ASHER, R., DAVIES,
L. C., GEBSKI, V. J., FRIEDLANDER, M., HILPERT, F., WEN-
ZEL, L., STOCKLER, M. R., KING, M. & PUJADE-LAURAINE, E.
2017. Quality of life predicts overall survival in women
with platinum-resistant ovarian cancer: an AURELIA sub-
study. Ann Oncol, 28, 1849-1855.
RONCOLATO, F. T., JOLY, F., O'CONNELL, R., LANCELEY, A.,
RESEARCH REPORT 2017 & 2018
HILPERT, F., BUIZEN, L., OKAMOTO, A., AOTANI, E., PIGNATA,
S., DONNELLAN, P., OZA, A., AVALL-LUNDQVIST, E., BEREK,
J. S., HEITZ, F., FEENEY, A., BERTON-RIGAUD, D., STOCKLER,
M. R., KING, M. & FRIEDLANDER, M. 2017. Reducing Un-
certainty: Predictors of Stopping Chemotherapy Early and
Shortened Survival Time in Platinum Resistant/Refractory
Ovarian Cancer-The GCIG Symptom Benefit Study. Oncol-
ogist, 22, 1117-1124.
ROOHULLAH, A., COOPER, A., LOMAX, A. J., AUNG, J.,
BARGE, A., CHOW, L., MCHALE, M., DESAI, J., WHITTLE,
J. R., TRAN, B., DE SOUZA, P. & HORVATH, L. G. 2018. A
phase I trial to determine safety and pharmacokinetics of
ASLAN002, an oral MET superfamily kinase inhibitor, in pa-
tients with advanced or metastatic solid cancers. Invest
New Drugs.
ROPER, E., LUM, T., PALME, C. E., ASHFORD, B., CH'NG, S.,
RANSON, M., BOYER, M., CLARK, J. & GUPTA, R. 2017. PD-
L1 expression predicts longer disease free survival in high
risk head and neck cutaneous squamous cell carcinoma.
Pathology, 49, 499-505. *
SCHACHTER, J., RIBAS, A., LONG, G. V., ARANCE, A., GROB,
J. J., MORTIER, L., DAUD, A., CARLINO, M. S., MCNEIL, C.,
LOTEM, M., LARKIN, J., LORIGAN, P., NEYNS, B., BLANK, C.,
PETRELLA, T. M., HAMID, O., ZHOU, H., EBBINGHAUS, S.,
IBRAHIM, N. & ROBERT, C. 2017. Pembrolizumab versus
ipilimumab for advanced melanoma: final overall survival
results of a multicentre, randomised, open-label phase 3
study (KEYNOTE-006). Lancet, 390, 1853-1862.
SCHUMACHER, F. R., AL OLAMA, A. A., BERNDT, S. I., BEN-
LLOCH, S., AHMED, M., SAUNDERS, E. J., DADAEV, T., LE-
ONGAMORNLERT, D., ANOKIAN, E., CIEZA-BORRELLA, C.,
GOH, C., BROOK, M. N., SHENG, X., FACHAL, L., DENNIS,
J., TYRER, J., MUIR, K., LOPHATANANON, A., STEVENS, V. L.,
GAPSTUR, S. M., CARTER, B. D., TANGEN, C. M., GOODMAN,
P. J., THOMPSON, I. M., JR., BATRA, J., CHAMBERS, S., MOYA,
L., CLEMENTS, J., HORVATH, L., TILLEY, W., RISBRIDGER, G.
P., GRONBERG, H., ALY, M., NORDSTROM, T., PHAROAH, P.,
PASHAYAN, N., SCHLEUTKER, J., TAMMELA, T. L. J., SIPEKY,
C., AUVINEN, A., ALBANES, D., WEINSTEIN, S., WOLK, A.,
HAKANSSON, N., WEST, C. M. L., DUNNING, A. M., BURNET,
N., MUCCI, L. A., GIOVANNUCCI, E., ANDRIOLE, G. L., CUS-
SENOT, O., CANCEL-TASSIN, G., KOUTROS, S., BEANE FREE-
MAN, L. E., SORENSEN, K. D., ORNTOFT, T. F., BORRE, M.,
MAEHLE, L., GRINDEDAL, E. M., NEAL, D. E., DONOVAN, J.
L., HAMDY, F. C., MARTIN, R. M., TRAVIS, R. C., KEY, T. J.,
HAMILTON, R. J., FLESHNER, N. E., FINELLI, A., INGLES, S. A.,
STERN, M. C., ROSENSTEIN, B. S., KERNS, S. L., OSTRER, H.,
LU, Y. J., ZHANG, H. W., FENG, N., MAO, X., GUO, X., WANG,
G., SUN, Z., GILES, G. G., SOUTHEY, M. C., MACINNIS, R.
J., FITZGERALD, L. M., KIBEL, A. S., DRAKE, B. F., VEGA, A.,
GOMEZ-CAAMANO, A., SZULKIN, R., EKLUND, M., KOGEVI-
NAS, M., LLORCA, J., CASTANO-VINYALS, G., PENNEY, K. L.,
STAMPFER, M., PARK, J. Y., SELLERS, T. A., LIN, H. Y., STAN-
FORD, J. L., CYBULSKI, C., et al. 2018. Association analyses
of more than 140,000 men identify 63 new prostate can-
cer susceptibility loci. Nat Genet, 50, 928-936.
SELINGER, C. I., LI, B. T., PAVLAKIS, N., LINKS, M., GILL, A.
J., LEE, A., CLARKE, S., TRAN, T. N., LUM, T., YIP, P. Y., HOR-
VATH, L., YU, B., KOHONEN-CORISH, M. R., O'TOOLE, S. A. &
COOPER, W. A. 2017. Screening for ROS1 gene rearrange-
ments in non-small-cell lung cancers using immunohisto-
chemistry with FISH confirmation is an effective method
to identify this rare target. Histopathology, 70, 402-411.
SHAPIRO, J. D., THAVANESWARAN, S., UNDERHILL, C. R.,
ROBLEDO, K. P., KARAPETIS, C. S., DAY, F. L., NOTT, L. M.,
JEFFORD, M., CHANTRILL, L. A., PAVLAKIS, N., TEBBUTT, N.
C., PRICE, T. J., KHASRAW, M., VAN HAZEL, G. A., WARING, P.
M., TEJPAR, S., SIMES, J., GEBSKI, V. J., DESAI, J. & SEGELOV,
E. 2018. Cetuximab Alone or With Irinotecan for Resist-
ant KRAS-, NRAS-, BRAF- and PIK3CA-wild-type Metastatic
Colorectal Cancer: The AGITG Randomized Phase II ICE-
CREAM Study. Clin Colorectal Cancer, 17, 313-319.
SIMES, J., ROBLEDO, K. P., WHITE, H. D., ESPINOZA, D.,
STEWART, R. A., SULLIVAN, D. R., ZELLER, T., HAGUE, W.,
NESTEL, P. J., GLASZIOU, P. P., KEECH, A. C., ELLIOTT, J.,
BLANKENBERG, S., TONKIN, A. M. & INVESTIGATORS, L. S.
2018. D-Dimer Predicts Long-Term Cause-Specific Mortal-
ity, Cardiovascular Events, and Cancer in Patients With Sta-
ble Coronary Heart Disease. Circulation, 138, 712-723.
SJOQUIST, K. M., RENFRO, L. A., SIMES, R. J., TEBBUTT, N.
C., CLARKE, S., SEYMOUR, M. T., ADAMS, R., MAUGHAN,
T. S., SALTZ, L., GOLDBERG, R. M., SCHMOLL, H. J., VAN
CUTSEM, E., DOUILLARD, J. Y., HOFF, P. M., HECHT, J. R.,
TOURNIGAND, C., PUNT, C. J. A., KOOPMAN, M., HURWITZ,
H., HEINEMANN, V., FALCONE, A., PORSCHEN, R., FUCHS,
C., DIAZ-RUBIO, E., ARANDA, E., BOKEMEYER, C., SOUG-
LAKOS, I., KABBINAVAR, F. F., CHIBAUDEL, B., MEYERS, J. P.,
SARGENT, D. J., DE GRAMONT, A. & ZALCBERG, J. R. 2018.
Personalizing Survival Predictions in Advanced Colorectal
Cancer: The ARCAD Nomogram Project. J Natl Cancer Inst,
110, 638-648.
56
CHRIS O'BRIEN LIFEHOUSE
57
SMITH, A., SHARPE, L., THEWES, B., TURNER, J., GILCHRIST, J.,
FARDELL, J. E., GIRGIS, A., TESSON, S., DESCALLAR, J., BELL,
M. L., BEITH, J. & BUTOW, P. 2018. Medical, demographic
and psychological correlates of fear of cancer recurrence
(FCR) morbidity in breast, colorectal and melanoma can-
cer survivors with probable clinically significant FCR seek-
ing psychological treatment through the ConquerFear
study. Support Care Cancer, 26, 4207-4216.
SMITH, A. B., RUTHERFORD, C., BUTOW, P., OLVER, I., LUCK-
ETT, T., GRIMISON, P., TONER, G., STOCKLER, M. & KING, M.
2018. A systematic review of quantitative observational
studies investigating psychological distress in testicular
cancer survivors. Psychooncology, 27, 1129-1137.
STEVENSON, A. R. L., SOLOMON, M. J., BROWN, C. S. B.,
LUMLEY, J. W., HEWETT, P., CLOUSTON, A. D., GEBSKI, V.
J., WILSON, K., HAGUE, W. & SIMES, J. 2018. Disease-free
Survival and Local Recurrence After Laparoscopic-assisted
Resection or Open Resection for Rectal Cancer: The Aus-
tralasian Laparoscopic Cancer of the Rectum Randomized
Clinical Trial. Ann Surg.
STOCKLER, M. R. 2018. Pooled RCTs: Reanalysis account-
ing for screening intensity suggests that screening reduc-
es prostate cancer mortality. Ann Intern Med, 168, Jc5.
TANDSTAD, T., KOLLMANNSBERGER, C. K., ROTH, B. J.,
JELDRES, C., GILLESSEN, S., FIZAZI, K., DANESHMAND, S.,
LOWRANCE, W. T., HANNA, N. H., ALBANY, C., FOSTER, R.,
CEDERMARK, G. C., FELDMAN, D. R., POWLES, T., LEWIS,
M. A., GRIMISON, P. S., BANK, D., PORTER, C., ALBERS, P.,
DE SANTIS, M., SRINIVAS, S., BOSL, G. J. & NICHOLS, C. R.
2017. Practice Makes Perfect: The Rest of the Story in Tes-
ticular Cancer as a Model Curable Neoplasm. J Clin Oncol,
35, 3525-3528.
TATTERSALL, M. H., JEFFORD, M., MARTIN, A., OLVER, I.,
THOMPSON, J. F., BROWN, R. F. & BUTOW, P. N. 2017. Par-
allel multicentre randomised trial of a clinical trial ques-
tion prompt list in patients considering participation in
phase 3 cancer treatment trials. BMJ Open, 7, e012666.
TATTERSALL, M. H. N. 2017. Gaps in patients' understand-
ing of palliative chemotherapy. Can we better commu-
nicate that treatment is not curative? Expert Review of
Quality of Life in Cancer Care, 2, 245-249.
TATTERSALL, M. H. N. 2018. Patient-Oncologist Commu-
nication: Sharing Decisions in Cancer Care. J Oncol Pract,
14, 9-10.
TO, S. Q., KWAN, E. M., FETTKE, H. C., MANT, A., DOCANTO,
M. M., MARTELOTTO, L., BUKCZYNSKA, P., NG, N., GRAHAM,
L. K., PARENTE, P., PEZARO, C., MAHON, K., HORVATH, L.,
TODENHOFER, T. & AZAD, A. A. 2018. Expression of Andro-
gen Receptor Splice Variant 7 or 9 in Whole Blood Does
Not Predict Response to Androgen-Axis-targeting Agents
in Metastatic Castration-resistant Prostate Cancer. Eur
Urol, 73, 818-821.
TRAN, A. D., FOGARTY, G., NOWAK, A. K., ESPINOZA, D.,
ROWBOTHAM, N., STOCKLER, M. R. & MORTON, R. L. 2018.
A systematic review and meta-analysis of utility estimates
in melanoma. Br J Dermatol, 178, 384-393.
VAFAEE, F., DIAKOS, C., KIRSCHNER, M. B., REID, G., MI-
CHAEL, M. Z., HORVATH, L. G., ALINEJAD-ROKNY, H.,
CHENG, Z. J., KUNCIC, Z. & CLARKE, S. 2018. A data-driv-
en, knowledge-based approach to biomarker discovery:
application to circulating microRNA markers of colorectal
cancer prognosis. NPJ Syst Biol Appl, 4, 20.
VALDES-MORA, F., GOULD, C. M., COLINO-SANGUINO, Y.,
QU, W., SONG, J. Z., TAYLOR, K. M., BUSKE, F. A., STATHAM,
A. L., NAIR, S. S., ARMSTRONG, N. J., KENCH, J. G., LEE, K.
M. L., HORVATH, L. G., QIU, M., ILINYKH, A., YEO-TEH, N. S.,
GALLEGO-ORTEGA, D., STIRZAKER, C. & CLARK, S. J. 2017.
Acetylated histone variant H2A.Z is involved in the activa-
tion of neo-enhancers in prostate cancer. Nat Commun,
8, 1346.
VAN DEN BENT, M., GAN, H. K., LASSMAN, A. B., KUMTHEK-
AR, P., MERRELL, R., BUTOWSKI, N., LWIN, Z., MIKKELSEN, T.,
NABORS, L. B., PAPADOPOULOS, K. P., PENAS-PRADO, M.,
SIMES, J., WHEELER, H., WALBERT, T., SCOTT, A. M., GOMEZ,
E., LEE, H. J., ROBERTS-RAPP, L., XIONG, H., BAIN, E., ANSELL,
P. J., HOLEN, K. D., MAAG, D. & REARDON, D. A. 2017.
Efficacy of depatuxizumab mafodotin (ABT-414) mono-
therapy in patients with EGFR-amplified, recurrent glio-
blastoma: results from a multi-center, international study.
Cancer Chemother Pharmacol, 80, 1209-1217.
VAN ZANDWIJK, N., PAVLAKIS, N., KAO, S. C., LINTON, A.,
BOYER, M. J., CLARKE, S., HUYNH, Y., CHRZANOWSKA, A.,
FULHAM, M. J., BAILEY, D. L., COOPER, W. A., KRITHARIDES,
L., RIDLEY, L., PATTISON, S. T., MACDIARMID, J., BRAHMB-
HATT, H. & REID, G. 2017. Safety and activity of microR-
NA-loaded minicells in patients with recurrent malignant
pleural mesothelioma: a first-in-man, phase 1, open-label,
RESEARCH REPORT 2017 & 2018
dose-escalation study. Lancet Oncol, 18, 1386-1396.
WALCZAK, A., BUTOW, P. N., TATTERSALL, M. H., DAVIDSON,
P. M., YOUNG, J., EPSTEIN, R. M., COSTA, D. S. & CLAYTON,
J. M. 2017. Encouraging early discussion of life expectan-
cy and end-of-life care: A randomised controlled trial of
a nurse-led communication support program for patients
and caregivers. Int J Nurs Stud, 67, 31-40.
WALLER, A., DODD, N., TATTERSALL, M. H. N., NAIR, B. &
SANSON-FISHER, R. 2017. Improving hospital-based end
of life care processes and outcomes: a systematic review
of research output, quality and effectiveness. BMC Palliat
Care, 16, 34.
WEBER, J., MANDALA, M., DEL VECCHIO, M., GOGAS, H. J.,
ARANCE, A. M., COWEY, C. L., DALLE, S., SCHENKER, M.,
CHIARION-SILENI, V., MARQUEZ-RODAS, I., GROB, J. J., BUT-
LER, M. O., MIDDLETON, M. R., MAIO, M., ATKINSON, V.,
QUEIROLO, P., GONZALEZ, R., KUDCHADKAR, R. R., SMYLIE,
M., MEYER, N., MORTIER, L., ATKINS, M. B., LONG, G. V.,
BHATIA, S., LEBBE, C., RUTKOWSKI, P., YOKOTA, K., YAMAZA-
KI, N., KIM, T. M., DE PRIL, V., SABATER, J., QURESHI, A., LAR-
KIN, J. & ASCIERTO, P. A. 2017. Adjuvant Nivolumab versus
Ipilimumab in Resected Stage III or IV Melanoma. N Engl J
Med, 377, 1824-1835.
WETZIG, N., GILL, P. G., ESPINOZA, D., MISTER, R., STOCK-
LER, M. R., GEBSKI, V. J., UNG, O. A., CAMPBELL, I. & SIMES, J.
2017. Sentinel-Lymph-Node-Based Management or Rou-
tine Axillary Clearance? Five-Year Outcomes of the RACS
Sentinel Node Biopsy Versus Axillary Clearance (SNAC) 1
Trial: Assessment and Incidence of True Lymphedema. Ann
Surg Oncol, 24, 1064-1070.
WONG, S. E., NORTH, S. A., SWEENEY, C. J., STOCKLER, M. R.
& SRIDHAR, S. S. 2017. Screen Failure Rates in Contempo-
rary Randomized Clinical Phase II/III Therapeutic Trials in
Genitourinary Malignancies. Clin Genitourin Cancer.
WU, Y. L., SEQUIST, L. V., TAN, E. H., GEATER, S. L., ORLOV,
S., ZHANG, L., LEE, K. H., TSAI, C. M., KATO, T., BARRIOS,
C. H., SCHULER, M., HIRSH, V., YAMAMOTO, N., O'BYRNE,
K., BOYER, M., MOK, T., PEIL, B., MARTEN, A., CHIH-HSIN
YANG, J., PAZ-ARES, L. & PARK, K. 2018. Afatinib as First-line
Treatment of Older Patients With EGFR Mutation-Positive
Non-Small-Cell Lung Cancer: Subgroup Analyses of the
LUX-Lung 3, LUX-Lung 6, and LUX-Lung 7 Trials. Clin Lung
Cancer, 19, e465-e479.
YOUNG, R., MAINWARING, P., CLINGAN, P., PARNIS, F. X., AS-
GHARI, G., BEALE, P., ALY, A., BOTTEMAN, M., ROMANO, A.,
FERRARA, S., MARGUNATO-DEBAY, S. & HARRIS, M. 2018.
nab-Paclitaxel plus gemcitabine in metastatic pancreatic
adenocarcinoma: Australian subset analyses of the phase
III MPACT trial. Asia Pac J Clin Oncol.
ZAHEED, M., BRAY, V. J., ITCHINS, M., STORER, P. & KAO, S.
2018. Development of Complex Hepatic Cysts Is a Poten-
tial Side Effect of Crizotinib. J Thorac Oncol, 13, e62-e64.
ZHANG, A. Y., GROGAN, J. S., MAHON, K. L., RASIAH, K.,
SVED, P., EISINGER, D. R., BOULAS, J., VASILARIS, A., HEN-
SHALL, S. M., STRICKER, P. D., KENCH, J. G. & HORVATH,
L. G. 2017. A prospective multicentre phase III validation
study of AZGP1 as a biomarker in localized prostate can-
cer. Ann Oncol, 28, 1903-1909.
ZHANG, A. Y., JUDSON, I., BENSON, C., WUNDER, J. S.,
RAY-COQUARD, I., GRIMER, R. J., QUEK, R., WONG, E.,
MIAH, A. B., FERGUSON, P. C., DUFRESNE, A., TEH, J. Y. H.,
STOCKLER, M. & TATTERSALL, M. H. N. 2017. Chemother-
apy with radiotherapy influences time-to-development of
radiation-induced sarcomas: a multicenter study. Br J Can-
cer, 117, 326-331.
* Publication shared with other Chris O'Brien Lifehouse depart-
ment
58
CHRIS O'BRIEN LIFEHOUSE
59
Head and Neck
ALLANSON, B. M., LOW, T. H., CLARK, J. R. & GUPTA, R.
2018. Squamous Cell Carcinoma of the External Auditory
Canal and Temporal Bone: An Update. Head Neck Pathol,
12, 407-418.
ASHFORD, B. G., CLARK, J., GUPTA, R., IYER, N. G., YU, B. &
RANSON, M. 2017. Reviewing the genetic alterations in
high-risk cutaneous squamous cell carcinoma: A search
for prognostic markers and therapeutic targets. Head
Neck, 39, 1462-1469.
BADLANI, J., GUPTA, R., BALASUBRAMANIAN, D., SMITH, J.,
LUK, P. & CLARK, J. 2018. Primary salivary gland malignan-
cies: a review of clinicopathological evolution, molecular
mechanisms and management. ANZ J Surg, 88, 152-157.
BADLANI, J., GUPTA, R., SMITH, J., ASHFORD, B., CH'NG, S.,
VENESS, M. & CLARK, J. 2018. Metastases to the parotid
gland - A review of the clinicopathological evolution, mo-
lecular mechanisms and management. Surg Oncol, 27,
44-53.
BARRY, C. P., WONG, D., CLARK, J. R., SHAW, R. J., GUPTA,
R., MAGENNIS, P., TRIANTAFYLLOU, A., GAO, K. & BROWN,
J. S. 2017. Postoperative radiotherapy for patients with
oral squamous cell carcinoma with intermediate risk of
recurrence: A case match study. Head Neck, 39, 1399-
1404.
BRUNNER, M., CH'NG, S., SHANNON, K., CLIFFORD, A.,
ASHFORD, B., ELLIOTT, M. & CLARK, J. R. 2017. Bone re-
section for facial cutaneous malignancies. J Surg Oncol,
116, 545-549.
BUCKLEY, L., JACKETT, L., CLARK, J. & GUPTA, R. 2018.
HPV-related Oropharyngeal Carcinoma: A Review of Clin-
ical and Pathologic Features With Emphasis on Updates
in Clinical and Pathologic Staging. Adv Anat Pathol, 25,
180-188.
CHIA, N., WEN, L., LYONS, J. G., ELLIOTT, M., LEE, M.,
PALME, C. E., CLARK, J. R. & GUPTA, R. 2018. Challenges
and recommendations for minimally resourced biobanks
in tertiary Australian hospitals. ANZ J Surg, 88, 115-116.
CH'NG, S. 2018. Commentary on: Supratrochlear Artery
Based Periosteal Flaps: A New Alternative Technique for
Nasal Lining Reconstruction. Plast Reconstr Surg.
CH'NG, S. 2018. Reply: The Inside-Out Septal Mucoperi-
chondrial Flap: Reconstruction of Nasal Lining Simplified.
Plast Reconstr Surg, 142, 101e-102e.
CHONG, L. S. H., EVISTON, T. J., LOW, T. H., HASMAT, S.,
COULSON, S. E. & CLARK, J. R. 2017. Validation of the
Clinician-Graded Electronic Facial Paralysis Assessment.
Plast Reconstr Surg, 140, 159-167.
CHONG, L. S. H., TJAHJONO, R., EVISTON, T. J. & CLARK, J.
R. 2017. Dual chimeric innervated vastus lateralis free
flap for single stage blink and midface reanimation. Head
Neck, 39, 1894-1896.
DIRVEN, R., EBRAHIMI, A., MOECKELMANN, N., PALME, C.
E., GUPTA, R. & CLARK, J. 2017. Tumor thickness versus
depth of invasion - Analysis of the 8th edition American
Joint Committee on Cancer Staging for oral cancer. Oral
Oncol, 74, 30-33.
DORT, J. C., FARWELL, D. G., FINDLAY, M., HUBER, G. F.,
KERR, P., SHEA-BUDGELL, M. A., SIMON, C., UPPINGTON, J.,
ZYGUN, D., LJUNGQVIST, O. & HARRIS, J. 2017. Optimal
Perioperative Care in Major Head and Neck Cancer Sur-
gery With Free Flap Reconstruction: A Consensus Review
and Recommendations From the Enhanced Recovery Af-
ter Surgery Society. JAMA Otolaryngol Head Neck Surg,
143, 292-303.
EVISTON, T. J., CHONG, L. S. H. & CLARK, J. R. 2018. Reply:
RESEARCH REPORT 2017 & 2018
Validation of the Clinician-Graded Electronic Facial Paraly-
sis Assessment. Plast Reconstr Surg, 141, 615e-616e.
EVISTON, T. J., CHONG, L. S. H., KWAI, N. C. G., CLARK, J. R.
& KRISHNAN, A. V. 2018. Altered axonal excitability prop-
erties in facial palsy. Muscle Nerve, 57, 268-272.
FINDLAY, M., RANKIN, N., SHAW, T., WHITE, K., BOYER, M.,
MILROSS, C., DE ABREU LOURENCO, R., BROWN, C., COLL,
J., BEALE, P. & ET AL. Innovation in implementation: A new
model of nutrition care for patients with head and neck
cancer improves outcomes. Dietitians Association of Aus-
tralia 35th National Conference, 2018 Sydney.
FRIDMAN, E., NA'ARA, S., AGARWAL, J., AMIT, M., BACHAR,
G., VILLARET, A. B., BRANDAO, J., CERNEA, C. R., CHATURVE-
DI, P., CLARK, J., EBRAHIMI, A., FLISS, D. M., JONNALAGA-
DDA, S., KOHLER, H. F., KOWALSKI, L. P., KREPPEL, M., LIAO,
C. T., PATEL, S. G., PATEL, R. S., ROBBINS, K. T., SHAH, J. P.,
SHPITZER, T., YEN, T. C., ZOLLER, J. E. & GIL, Z. 2018. The
role of adjuvant treatment in early-stage oral cavity squa-
mous cell carcinoma: An international collaborative study.
Cancer, 124, 2948-2955.
GNANASEKARAN, T., LOW, H., GUPTA, R., GAO, K. & CLARK,
J. 2018. Prognosis of metastatic head and neck squamous
cell carcinoma over the last 30 years. ANZ J Surg, 88,
1158-1162.
GUPTA, S., PARIKH, S. & GOEL, S. 2018. Parosteal osteosar-
coma of mandible: A rare case report. J Cancer Res Ther,
14, 471-474.
HASAN, Z., DWIVEDI, R. C., GUNARATNE, D. A., VIRK, S. A.,
PALME, C. E. & RIFFAT, F. 2017. Systematic review and me-
ta-analysis of the complications of salvage total laryngec-
tomy. Eur J Surg Oncol, 43, 42-51.
HAYDU, L. E., SCOLYER, R. A., LO, S., QUINN, M. J., SAW, R. P.
M., SHANNON, K. F., SPILLANE, A. J., STRETCH, J. R., MCCAR-
THY, W. H. & THOMPSON, J. F. 2017. Conditional Survival:
An Assessment of the Prognosis of Patients at Time Points
After Initial Diagnosis and Treatment of Locoregional Mel-
anoma Metastasis. J Clin Oncol, 35, 1721-1729.
INFANTINO, S., LIGHT, A., O'DONNELL, K., BRYANT, V.,
AVERY, D. T., ELLIOTT, M., TANGYE, S. G., BELZ, G., MACKAY,
F., RICHARD, S. & TARLINTON, D. 2017. Arginine methyla-
tion catalyzed by PRMT1 is required for B cell activation
and differentiation. Nat Commun, 8, 891.
JABBOUR, J., DHILLON, H. M., SHEPHERD, H. L., SUNDARE-
SAN, P., MILROSS, C. & CLARK, J. R. 2017. Challenges in
Producing Tailored Internet Patient Education Materials.
Int J Radiat Oncol Biol Phys, 97, 866-867. *
JABBOUR, J., DHILLON, H. M., SHEPHERD, H. L., SUNDARE-
SAN, P., MILROSS, C. & CLARK, J. R. 2018. The relationship
between role preferences in decision-making and level of
psychological distress in patients with head and neck can-
cer. Patient Educ Couns, 101, 1736-1740. *
JABBOUR, J., MILROSS, C., SUNDARESAN, P., EBRAHIMI, A.,
SHEPHERD, H. L., DHILLON, H. M., MORGAN, G., ASHFORD,
B., ABDUL-RAZAK, M., WONG, E., VENESS, M., PALME, C. E.,
FROGGATT, C., COHEN, R., EKMEJIAN, R., TAY, J., ROSHAN,
D. & CLARK, J. R. 2017. Education and support needs in
patients with head and neck cancer: A multi-institutional
survey. Cancer, 123, 1949-1957. *
JABBOUR, J., WYKES, J., MILROSS, C., SUNDARESAN, P.,
EBRAHIMI, A., SHEPHERD, H. L., DHILLON, H. M. & CLARK,
J. R. 2018. Examining clinicians' perceptions of head and
neck cancer (HNC) information. Asia Pac J Clin Oncol. *
KARAGIANNIS, P., CLARK, J. R. & CH'NG, S. 2017. The In-
side-Out Septal Mucoperichondrial Flap: Reconstruc-
tion of Nasal Lining Simplified. Plast Reconstr Surg, 140,
644e-645e.
KHOO, T. K., YU, B., SMITH, J. A., CLARKE, A. J., LUK, P. P.,
SELINGER, C. I., MAHON, K. L., KRAITSEK, S., PALME, C.,
BOYER, M. J., DINGER, M. E., COWLEY, M. J., O'TOOLE, S.
A., CLARK, J. R. & GUPTA, R. 2017. Somatic mutations in
salivary duct carcinoma and potential therapeutic targets.
Oncotarget, 8, 75893-75903.
LIU, J., EBRAHIMI, A., LOW, T. H., GAO, K., PALME, C. E.,
SYDNEY, C., ASHFORD, B. G., IYER, N. G., CLARK, J. R. & GUP-
TA, R. 2018. Predictive value of the 8th edition American
Joint Commission Cancer (AJCC) nodal staging system for
patients with cutaneous squamous cell carcinoma of the
head and neck. J Surg Oncol, 117, 765-772.
LOMAX, A. J., MCGUIRE, H. M., MCNEIL, C., CHOI, C. J.,
HERSEY, P., KARIKIOS, D., SHANNON, K., VAN HAL, S., CARR,
U., CROTTY, A., GUPTA, S. K., HOLLINGSWORTH, J., KIM, H.,
FAZEKAS DE ST GROTH, B. & MCGILL, N. 2017. Immuno-
therapy-induced sarcoidosis in patients with melanoma
treated with PD-1 checkpoint inhibitors: Case series and
immunophenotypic analysis. Int J Rheum Dis, 20, 1277-
60
CHRIS O'BRIEN LIFEHOUSE
61
1285. *
LOW, T. H., LINDSAY, A., CLARK, J., CHAI, F. & LEWIS, R. 2017.
Reconstruction of maxillary defect with musculo-adipose
rectus free flap. Microsurgery, 37, 137-141.
LOW, T. H., YEH, D., ZHANG, T., ARASLANOVA, R., HAM-
MOND, J. A., PALMA, D., READ, N., VENKATESAN, V., MAC-
NEIL, S. D., YOO, J., NICHOLS, A. & FUNG, K. 2017. Evalu-
ating organ preservation outcome as treatment endpoint
for T1aN0 glottic cancer. Laryngoscope, 127, 1322-
1327.
LOW, T. H. & YOO, J. 2017. Subtotal Parathyroidectomy
and Relocation of the Parathyroid Remnant for Renal Hy-
perparathyroidism: modification of a traditional opera-
tion. J Otolaryngol Head Neck Surg, 46, 60.
LUK, P. P., SELINGER, C. I., COOPER, W. A., MAHAR, A., PALME,
C. E., O'TOOLE, S. A., CLARK, J. R. & GUPTA, R. 2018. Clini-
cal Utility of In Situ Hybridization Assays in Head and Neck
Neoplasms. Head Neck Pathol.
MOECKELMANN, N., EBRAHIMI, A., DIRVEN, R., LIU, J., LOW,
T. H., GUPTA, R., ASHFORD, B., CH'NG, S., PALME, C. E. &
CLARK, J. R. 2018. Analysis and Comparison of the 8th
Edition American Joint Committee on Cancer (AJCC) Nod-
al Staging System in Cutaneous and Oral Squamous Cell
Cancer of the Head and Neck. Ann Surg Oncol, 25, 1730-
1736.
MOECKELMANN, N., EBRAHIMI, A., TOU, Y. K., GUPTA, R.,
LOW, T. H., ASHFORD, B., CH'NG, S., PALME, C. E. & CLARK,
J. R. 2018. Prognostic implications of the 8th edition
American Joint Committee on Cancer (AJCC) staging sys-
tem in oral cavity squamous cell carcinoma. Oral Oncol,
85, 82-86.
MORTON, R. L., TRAN, A., VESSEY, J. Y., ROWBOTHAM, N.,
WINSTANLEY, J., SHANNON, K., SPILLANE, A. J., STRETCH, J.,
THOMPSON, J. F. & SAW, R. P. 2017. Quality of Life Follow-
ing Sentinel Node Biopsy for Primary Cutaneous Melano-
ma: Health Economic Implications. Ann Surg Oncol, 24,
2071-2079.
MUELLER, S. A., GAUTHIER, M.-E. A., ASHFORD, B., GUPTA,
R., GAYEVSKIY, V., CH'NG, S., PALME, C. E., SHANNON, K.,
CLARK, J. R., RANSON, M. & COWLEY, M. J. Mutational Pat-
terns in Metastatic Cutaneous Squamous Cell Carcinoma.
Journal of Investigative Dermatology.
NARAYANAPPA, H., LOW, T. H., VARGAS CALDERON, A. C.,
SELINGER, C. & GUPTA, R. 2018. Inflammatory myofibro-
blastic tumours of the head and neck. Pathology, 50, 356-
358.
NELIGAN PC, C. N. S. 2018. The evolution of head and
neck reconstruction. Aust J Plast Surg., 1(2), 24-30.
ROPER, E., LUM, T., PALME, C. E., ASHFORD, B., CH'NG, S.,
RANSON, M., BOYER, M., CLARK, J. & GUPTA, R. 2017. PD-
L1 expression predicts longer disease free survival in high
risk head and neck cutaneous squamous cell carcinoma.
Pathology, 49, 499-505. *
SATGUNASEELAN, L., CHIA, N., SUH, H., VIRK, S., ASHFORD,
B., LUM, T., RANSON, M., CLARK, J. & GUPTA, R. 2017. p16
expression in cutaneous squamous cell carcinoma of the
head and neck is not associated with integration of high
risk HPV DNA or prognosis. Pathology, 49, 494-498.
SELINGER C, E. B., GUPTA, ET AL. 2018. Examples of the di-
agnostic utility of USP6 Fish in soft tissue and bone pahtol-
ogy. Pathology, 50, S141-S142.
SHARMA, A., CAO, E. Y., KUMAR, V., ZHANG, X., LEONG, H.
S., WONG, A. M. L., RAMAKRISHNAN, N., HAKIMULLAH, M.,
TEO, H. M. V., CHONG, F. T., CHIA, S., THANGAVELU, M.
T., KWANG, X. L., GUPTA, R., CLARK, J. R., PERIYASAMY, G.,
IYER, N. G. & DASGUPTA, R. 2018. Longitudinal single-cell
RNA sequencing of patient-derived primary cells reveals
drug-induced infidelity in stem cell hierarchy. Nat Com-
mun, 9, 4931.
SMITH, J. A., VIRK, S., PALME, C. E., LOW, T. H., CH'NG, S.,
GUPTA, R., GAO, K. & CLARK, J. 2018. Age is not a predictor
of prognosis in metastatic cutaneous squamous cell carci-
noma of the head and neck. ANZ J Surg, 88, E273-e277.
SMITHERS, F. A. E., CHENG, K., JAYARAM, R., MUKHERJEE, P.
& CLARK, J. R. 2018. Maxillofacial reconstruction using in-
house virtual surgical planning. ANZ J Surg, 88, 907-912.
SUAN, D., KRAUTLER, N. J., MAAG, J. L. V., BUTT, D., BOURNE,
K., HERMES, J. R., AVERY, D. T., YOUNG, C., STATHAM, A.,
ELLIOTT, M., DINGER, M. E., BASTEN, A., TANGYE, S. G. &
BRINK, R. 2017. CCR6 Defines Memory B Cell Precursors
in Mouse and Human Germinal Centers, Revealing Light-
Zone Location and Predominant Low Antigen Affinity. Im-
munity, 47, 1142-1153.e4.
RESEARCH REPORT 2017 & 2018
SUBRAMANIAM, N., BALASUBRAMANIAN, D., LOW, T. H.,
MURTHY, S., CLARK, J. R., THANKAPPAN, K. & IYER, S. 2018.
Factors Affecting Survival in Surgically Salvaged Locore-
gional Recurrences of Squamous Cell Carcinoma of the
Tongue. J Oral Maxillofac Surg, 76, 1133.e1-1133.e6.
SUBRAMANIAM, N., MURTHY, S., BALASUBRAMANIAN, D.,
LOW, T. H., VIDHYADHARAN, S., CLARK, J. R., THANKAPPAN,
K. & IYER, S. 2018. Adverse pathologic features in T1/2
oral squamous cell carcinoma classified by the American
Joint Committee on Cancer eighth edition and implica-
tions for treatment. Head Neck, 40, 2123-2128.
TAM, S., ARASLANOVA, R., LOW, T. H., WARNER, A., YOO,
J., FUNG, K., MACNEIL, S. D., PALMA, D. A. & NICHOLS, A.
C. 2017. Estimating Survival After Salvage Surgery for Re-
current Oral Cavity Cancer. JAMA Otolaryngol Head Neck
Surg, 143, 685-690.
TRAUTMAN, J., GORE, S., POTTER, M., CLARK, J., HYAM, D.,
TAN, N. C., NGO, Q. & ASHFORD, B. 2018. Supraclavicular
flap repair in the free flap era. ANZ J Surg, 88, 540-546.
TSEROS, E., RIFFAT, F., PALME, C. E., COLEMAN, H. G. & SIN-
GH, N. P. 2017. Neville Wran's voice: how the Premier's
Teflon-coated vocal cords came unstuck. Med J Aust, 207,
468-470.
VAREY, A. H. R., GOUMAS, C., HONG, A. M., MANN, G. J.,
FOGARTY, G. B., STRETCH, J. R., SAW, R. P. M., SPILLANE, A.
J., SHANNON, K. F., LEE, K. J., QUINN, M. J., THOMPSON,
J. F. & SCOLYER, R. A. 2017. Neurotropic melanoma: an
analysis of the clinicopathological features, management
strategies and survival outcomes for 671 patients treated
at a tertiary referral center. Mod Pathol, 30, 1538-1550. *
VASAN, K., LOW, T. H., GUPTA, R., ASHFORD, B., ASHER,
R., GAO, K., CH'NG, S., PALME, C. E. & CLARK, J. R. 2018.
Lymph node ratio as a prognostic factor in metastatic cu-
taneous head and neck squamous cell carcinoma. Head
Neck, 40, 993-999.
YIP, S., FLEMING, J., SHEPHERD, H. L., WALCZAK, A., CLARK,
J. & BUTOW, P. 2018. "As Long as You Ask": A Qualita-
tive Study of Biobanking Consent-Oncology Patients' and
Health Care Professionals' Attitudes, Motivations, and Ex-
periences-the B-PPAE Study. Oncologist.
ZHOU, K., LUONG, J. K., CLARK, J. R. & CH'NG, S. 2018.
Coned Radial Forearm Free Flap for Improved Retention
of Orbital Prosthesis following Orbital Exenteration. Plast
Reconstr Surg, 142, 818e-819e.
ZILBERG, C., LEE, M. W., YU, B., ASHFORD, B., KRAITSEK,
S., RANSON, M., SHANNON, K., COWLEY, M., IYER, N. G.,
PALME, C. E., CH'NG, S., LOW, T. H., O'TOOLE, S., CLARK, J.
R. & GUPTA, R. 2018. Analysis of clinically relevant somat-
ic mutations in high-risk head and neck cutaneous squa-
mous cell carcinoma. Mod Pathol, 31, 275-287.
* Publication shared with other Chris O'Brien Lifehouse
department
62
CHRIS O'BRIEN LIFEHOUSE
63
Radiation Oncology
ALI, M. A., HIRSHMAN, B. R., WILSON, B., CARROLL, K. T.,
PROUDFOOT, J. A., GOETSCH, S. J., ALKSNE, J. F., OTT, K.,
AIYAMA, H., NAGANO, O., CARTER, B. S., FOGARTY, G.,
HONG, A., SERIZAWA, T., YAMAMOTO, M. & CHEN, C. C.
2017. Survival Patterns of 5750 Stereotactic Radiosur-
gery-Treated Patients with Brain Metastasis as a Function
of the Number of Lesions. World Neurosurg, 107, 944-
951.e1.
ARASARATNAM, M., HONG, A., SHIVALINGAM, B., WHEEL-
ER, H., GUMINKSI, A. D., LONG, G. V. & MENZIES, A. M.
2018. Leptomeningeal melanoma-A case series in the era
of modern systemic therapy. Pigment Cell Melanoma Res,
31, 120-124.
BENNETT, M. H., FELDMEIER, J., SMEE, R. & MILROSS, C.
2018. Hyperbaric oxygenation for tumour sensitisation to
radiotherapy. Cochrane Database Syst Rev, 4, Cd005007.
BEZAK, E., SUCHOWERSKA, R., CLARIDGE MACKONIS, E.,
PILLEN, H., RALSTON, A., HAWORTH, A. & SUCHOWERSKA,
N. 2018. Women and men in the Australasian College of
Physical Scientists and Engineers in Medicine: workforce
survey. Australas Phys Eng Sci Med.
BUSTON M., GORJIARA T., ALZAIDI S, HAQUE M 2017. Ul-
traviolet dosimetry. In: DAS, I. (ed.) Radiochromic Film:
Role and Applications in Radiation Dosimetry 2017. 1 ed.
BUTSON, M., CARROLL, S., BUTSON, M. & HILL, R. 2017.
Characterization of a novel scale maille contralateral
breast shield: SMART Armor. J Appl Clin Med Phys, 18,
220-224.
BUTSON, M., HAQUE, M., SMITH, L., BUTSON, E., ODGERS,
D., POPE, D., GORJIANA, T., WHITAKER, M., MORALES, J.,
HONG, A. & HILL, R. 2017. Practical time considerations
for optically stimulated luminescent dosimetry (OSLD) in
total body irradiation. Australas Phys Eng Sci Med, 40,
167-171.
BUTSON M, C. G., ODGERS D, PODER J 2017. In vivo do-
simetry. In: DAS, I. (ed.) Radiochromic Film: Role and Appli-
cations in Radiation Dosimetry 2017. 1 ed.
BUTSON M, C. G., GILL S, POPE D 2017. Physics and char-
acteristics of radiochromic films. In: DAS, I. (ed.) Radi-
ochromic Film: Role and Applications in Radiation Dosim-
etry 2017. 1 ed.
BUTSON M, N.-R. A. 2017. Historical background, devel-
opment, and construction of radiochromic films. In: DAS,
I. (ed.) Radiochromic Film: Role and Applications in Radia-
tion Dosimetry 2017. 1 ed.
CHOONG, E. S., LO, S., DRUMMOND, M., FOGARTY, G. B.,
MENZIES, A. M., GUMINSKI, A., SHIVALINGAM, B., CLARKE,
K., LONG, G. V. & HONG, A. M. 2017. Survival of patients
with melanoma brain metastasis treated with stereotac-
tic radiosurgery and active systemic drug therapies. Eur J
Cancer, 75, 169-178.
CLARIDGE MACKONIS, E., HAMMOND, L., ESTEVES, A. I. S.
& SUCHOWERSKA, N. 2018. Radiation dosimetry in cell bi-
ology: comparison of calculated and measured absorbed
dose for a range of culture vessels and clinical beam qual-
ities. Int J Radiat Biol, 94, 150-156.
CLARIDGE MACKONIS, E. R., ESTOESTA, R. P. & CARROLL,
S. 2018. In-vivo dosimetry comparison of supraclavicular
junction dose for breast and chest-wall patients with and
without deep inspiration breath hold (DIBH). Phys Med,
54, 15-20.
CLARKE, K., B FOGARTY, G., LO, S., IZARD, M. & HONG, A.
2017. Optic Nerve Movement May Need to be Consid-
ered When Treating with Stereotactic Radiosurgery.
RESEARCH REPORT 2017 & 2018
DAS I.J., MORALES J. 2017. Small-field dosimetry in meg-
avoltage x-ray beams. In: DAS, I. (ed.) Radiochromic Film:
Role and Applications in Radiation Dosimetry 2017. 1 ed.
ESTOESTA, R. P., ATTWOOD, L., NAEHRIG, D., CLAR-
IDGE-MACKONIS, E., ODGERS, D., MARTIN, D., PHAM, M.,
TOOHEY, J. & CARROLL, S. 2017. Assessment of voluntary
deep inspiration breath-hold with CINE imaging for breast
radiotherapy. J Med Imaging Radiat Oncol, 61, 689-694. *
FOGARTY, G. B., HONG, A., ECONOMIDES, A. & GUIT-
ERA, P. 2018. Experience with Treating Lentigo Maligna
with Definitive Radiotherapy. Dermatol Res Pract, 2018,
7439807.
HEWSON, E. A., BUTSON, M. J. & HILL, R. 2018. Evaluating
TOPAS for the calculation of backscatter factors for low
energy x-ray beams. Phys Med Biol, 63, 195014.
HILL R., PODER J. 2017. Kilovoltage X-ray beam dosimetry
and imaging In: DAS, I. (ed.) Radiochromic Film: Role and
Applications in Radiation Dosimetry 2017. 1 ed.
HIRSHMAN, B. R., WILSON, B. R., ALI, M. A., SCHUPPER, A.
J., PROUDFOOT, J. A., GOETSCH, S. J., CARTER, B. S., SIN-
CLAIR, G., BARTEK, J., JR., CHIANG, V., FOGARTY, G., HONG,
A. & CHEN, C. C. 2018. Cumulative Intracranial Tumor Vol-
ume Augments the Prognostic Value of Diagnosis-Specific
Graded Prognostic Assessment Model for Survival in Pa-
tients with Melanoma Cerebral Metastases. Neurosurgery,
83, 237-244.
HONG, A. M., JONES, D., BOYLE, R. & STALLEY, P. 2018. Ra-
diation Therapy as an Alternative Treatment for Desmoid
Fibromatosis. Clin Oncol (R Coll Radiol), 30, 589-592.
JABBOUR, J., DHILLON, H. M., SHEPHERD, H. L., SUNDARE-
SAN, P., MILROSS, C. & CLARK, J. R. 2017. Challenges in
Producing Tailored Internet Patient Education Materials.
Int J Radiat Oncol Biol Phys, 97, 866-867. *
JABBOUR, J., DHILLON, H. M., SHEPHERD, H. L., SUNDARE-
SAN, P., MILROSS, C. & CLARK, J. R. 2018. The relationship
between role preferences in decision-making and level of
psychological distress in patients with head and neck can-
cer. Patient Educ Couns, 101, 1736-1740. *
JABBOUR, J., MILROSS, C., SUNDARESAN, P., EBRAHIMI, A.,
SHEPHERD, H. L., DHILLON, H. M., MORGAN, G., ASHFORD,
B., ABDUL-RAZAK, M., WONG, E., VENESS, M., PALME, C. E.,
FROGGATT, C., COHEN, R., EKMEJIAN, R., TAY, J., ROSHAN,
D. & CLARK, J. R. 2017. Education and support needs in
patients with head and neck cancer: A multi-institutional
survey. Cancer, 123, 1949-1957. *
JABBOUR, J., WYKES, J., MILROSS, C., SUNDARESAN, P.,
EBRAHIMI, A., SHEPHERD, H. L., DHILLON, H. M. & CLARK,
J. R. 2018. Examining clinicians' perceptions of head and
neck cancer (HNC) information. Asia Pac J Clin Oncol. *
JONES, C. W., SHATROV, J., JAGIELLO, J. M., MILLINGTON,
S., HONG, A., BOYLE, R. & STALLEY, P. D. 2017. Clinical,
functional and radiological outcomes of extracorporeal
irradiation in limb salvage surgery for bone tumours. Bone
Joint J, 99-b, 1681-1688.
KROON, H. M., VAN DER BOL, W. D., TONKS, K. T., HONG,
A. M., HRUBY, G. & THOMPSON, J. F. 2018. Treatment of
Clinically Positive Cervical Lymph Nodes by Limited Local
Node Excision and Adjuvant Radiotherapy in Melanoma
Patients with Major Comorbidities. Ann Surg Oncol, 25,
3476-3482.
LAI, K., KILLINGSWORTH, M., YONG, J., MATTHEWS, S.,
EBRAHIMI, A., MCGUINNESS, J., NGO, Q., CAIXEIRO, N.,
HONG, A. & LEE, C. S. 2017. Specific localization of LC3B
in autophagosome: A correlative labelling study with nan-
oparticle in oral squamous cell carcinoma. Exp Mol Pathol,
102, 422-427.
LAI, K., MATTHEWS, S., WILMOTT, J. S., KILLINGSWORTH, M.
C., YONG, J. L., CAIXEIRO, N. J., WYKES, J., SAMAKEH, A.,
FORSTNER, D., LEE, M., MCGUINNESS, J., NILES, N., HONG,
A., EBRAHIMI, A. & LEE, C. S. 2018. Differences in LC3B
expression and prognostic implications in oropharyngeal
and oral cavity squamous cell carcinoma patients. BMC
Cancer, 18, 624.
LONG, G. V., ATKINSON, V., HONG, A., MCARTHUR, G. A. &
MENZIES, A. M. 2018. Omitting radiosurgery in melanoma
brain metastases: a drastic and dangerous de-escalation -
Authors' reply. Lancet Oncol, 19, e367.
MARTINAGE, G., HONG, A. M., FAY, M., THACHIL, T., ROOS,
D., WILLIAMS, N., LO, S. & FOGARTY, G. 2018. Quality
assurance analysis of hippocampal avoidance in a mela-
noma whole brain radiotherapy randomized trial shows
good compliance. Radiat Oncol, 13, 132.
OLEJNIK, J., SUCHOWERSKA, N., HERRID, M., JACKSON, A.,
64
CHRIS O'BRIEN LIFEHOUSE
65
JACKSON, M., ANDRONICOS, N. M., HINCH, G. N. & HILL, J.
R. 2018. Sensitivity of spermatogonia to irradiation var-
ies with age in pre-pubertal ram lambs. Anim Reprod Sci,
193, 58-67.
OLEJNIK, J., SUCHOWERSKA, N., HERRID, M., JACKSON,
M., HINCH, G. & HILL, J. 2018. Spermatogonia survival in
young ram lambs following irradiation, Busulfan or ther-
mal treatment. Small Ruminant Research, 166, 22-27.
PENG, V., SUCHOWERSKA, N., ESTEVES, A. D. S., ROGERS,
L., CLARIDGE MACKONIS, E., TOOHEY, J. & MCKENZIE, D.
R. 2018. Models for the bystander effect in gradient radi-
ation fields: Range and signalling type. J Theor Biol, 455,
16-25.
PENG, V., SUCHOWERSKA, N., ROGERS, L., CLARIDGE MACK-
ONIS, E., OAKES, S. & MCKENZIE, D. R. 2017. Grid therapy
using high definition multileaf collimators: realizing bene-
fits of the bystander effect. Acta Oncol, 56, 1048-1059.
POLLOCK, S., TSE, R., MARTIN, D., MCLEAN, L., PHAM, M.,
TAIT, D., ESTOESTA, R., WHITTINGTON, G., TURLEY, J., KEAR-
NEY, C., CHO, G., HILL, R., PICKARD, S., ASTON, P., MAKHIJA,
K., O'BRIEN, R. & KEALL, P. 2018. Impact of audiovisual bi-
ofeedback on interfraction respiratory motion reproduci-
bility in liver cancer stereotactic body radiotherapy. J Med
Imaging Radiat Oncol, 62, 133-139.
PORCEDDU, S. V., BRESSEL, M., POULSEN, M. G., STONELEY,
A., VENESS, M. J., KENNY, L. M., WRATTEN, C., CORRY, J.,
COOPER, S., FOGARTY, G. B., COLLINS, M., COLLINS, M. K.,
MACANN, A. M. J., MILROSS, C. G., PENNIMENT, M. G., LIU,
H. Y., KING, M. T., PANIZZA, B. J. & RISCHIN, D. 2018. Post-
operative Concurrent Chemoradiotherapy Versus Postop-
erative Radiotherapy in High-Risk Cutaneous Squamous
Cell Carcinoma of the Head and Neck: The Randomized
Phase III TROG 05.01 Trial. J Clin Oncol, 36, 1275-1283.
SMITH, S. K., CABRERA-AGUAS, M., SHAW, J., SHEPHERD, H.,
NAEHRIG, D., MEISER, B., JACKSON, M., SAADE, G., BUCCI,
J., HALKETT, G. K. B., TURNER, R. M., MILROSS, C. & DHIL-
LON, H. M. 2018. A low literacy targeted talking book
about radiation therapy for cancer: development and ac-
ceptability. Support Care Cancer. *
SMITH, S. K., NATHAN, D., TAYLOR, J., VAN GELDER, E., DIX-
ON, A., HALKETT, G. K. B., MILROSS, C. & DHILLON, H. M.
2017. Patients' experience of decision-making and receiv-
ing information during radiation therapy: A qualitative
study. Eur J Oncol Nurs, 30, 97-106.
SUNDARESAN, P., KING, M., STOCKLER, M., COSTA, D. & MIL-
ROSS, C. 2017. Barriers to radiotherapy utilization: Con-
sumer perceptions of issues influencing radiotherapy-re-
lated decisions. Asia Pac J Clin Oncol, 13, e489-e496.
TIO, M., WANG, X., CARLINO, M. S., SHIVALINGAM, B., FOG-
ARTY, G. B., GUMINSKI, A. D., LO, S., HONG, A. M., MEN-
ZIES, A. M. & LONG, G. V. 2018. Survival and prognostic
factors for patients with melanoma brain metastases in
the era of modern systemic therapy. Pigment Cell Melano-
ma Res, 31, 509-515.
VAREY, A. H. R., GOUMAS, C., HONG, A. M., MANN, G. J.,
FOGARTY, G. B., STRETCH, J. R., SAW, R. P. M., SPILLANE, A.
J., SHANNON, K. F., LEE, K. J., QUINN, M. J., THOMPSON,
J. F. & SCOLYER, R. A. 2017. Neurotropic melanoma: an
analysis of the clinicopathological features, management
strategies and survival outcomes for 671 patients treated
at a tertiary referral center. Mod Pathol, 30, 1538-1550. *
YAO, M., ROGERS, L., SUCHOWERSKA, N., CHOE, D.,
AL-DABBAS, M. A., NARULA, R. S., LYONS, J. G., SVED, P.,
LI, Z. & DONG, Q. 2018. Sensitization of prostate cancer
to radiation therapy: Molecules and pathways to target.
Radiother Oncol, 128, 283-300.
* Publication shared with other Chris O'Brien Lifehouse
department
RESEARCH REPORT 2017 & 2018
Gynaecological Oncology
CARTER, J., HAMMOND, I. & SMITH, M. 2017. The renewal
of the National Cervical Screening Program. Med J Aust,
206, 274.
CARTER, J., PATHER, S. & NASCIMENTO, M. 2018. Current
status of ovarian cancer surgical management. Argument
for centralisation of care in Australia. Aust N Z J Obstet
Gynaecol, 58, 474-477.
CIBULA, D., ABU-RUSTUM, N. R., FISCHEROVA, D., PATHER,
S., LAVIGNE, K., SLAMA, J., ALEKTIAR, K., MING-YIN, L., KO-
CIAN, R., GERMANOVA, A., FRUHAUF, F., DOSTALEK, L.,
DUSEK, L. & NARAYAN, K. 2018. Surgical treatment of
"intermediate risk" lymph node negative cervical cancer
patients without adjuvant radiotherapy-A retrospective
cohort study and review of the literature. Gynecol Oncol,
151, 438-443.
EA, G. 2018. Diabetes and its role in gynaecological ma-
lignancies. O&G Magazine RANZCOG, 20, 48-49
FARRELL, R., DIXON, S. C., CARTER, J. & WEBB, P. M. 2017.
Lymphadenectomy in Early-Stage Intermediate-/High-Risk
Endometrioid Endometrial Cancer: Clinical Characteris-
tics and Outcomes in an Australian Cohort. Int J Gynecol
Cancer, 27, 1379-1386.
GANE, E. M., STEELE, M. L., JANDA, M., WARD, L. C., REUL-
HIRCHE, H., CARTER, J., QUINN, M., OBERMAIR, A. & HAYES,
S. C. 2018. The Prevalence, Incidence, and Quality-of-Life
Impact of Lymphedema After Treatment for Vulvar or
Vaginal Cancer. Rehabilitation Oncology, 36, 48-55.
HAYES, S. C., JANDA, M., WARD, L. C., REUL-HIRCHE, H.,
STEELE, M. L., CARTER, J., QUINN, M., CORNISH, B. & OBER-
MAIR, A. 2017. Lymphedema following gynecological
cancer: Results from a prospective, longitudinal cohort
study on prevalence, incidence and risk factors. Gynecol
Oncol, 146, 623-629.
JANDA, M., GEBSKI, V., DAVIES, L. C., FORDER, P., BRAND,
A., HOGG, R., JOBLING, T. W., LAND, R., MANOLITSAS, T.,
NASCIMENTO, M., NEESHAM, D., NICKLIN, J. L., OEHLER,
M. K., OTTON, G., PERRIN, L., SALFINGER, S., HAMMOND,
I., LEUNG, Y., SYKES, P., NGAN, H., GARRETT, A., LANEY, M.,
NG, T. Y., TAM, K., CHAN, K., WREDE, C. D., PATHER, S., SIM-
COCK, B., FARRELL, R., ROBERTSON, G., WALKER, G., ARM-
FIELD, N. R., GRAVES, N., MCCARTNEY, A. J. & OBERMAIR,
A. 2017. Effect of Total Laparoscopic Hysterectomy vs
Total Abdominal Hysterectomy on Disease-Free Survival
Among Women With Stage I Endometrial Cancer: A Rand-
omized Clinical Trial. Jama, 317, 1224-1233.
KARAMI JH, L. K., FUNG T, CARTER J, DING Z. 2017. An
investigation of survival following ovarian cancer. Malays
J Med Biol Res 4 27-34.
MORTON, R., ANDERSON, L., CARTER, J., PATHER, S. & SAI-
DI, S. A. 2017. Intraoperative Frozen Section of Ovarian
Tumors: A 6-Year Review of Performance and Potential
Pitfalls in an Australian Tertiary Referral Center. Int J Gyne-
col Cancer, 27, 17-21.
PATHER, S., TEJADA BERGES, T., SAIDI, S. & CARTER, J. 2018.
Re: Neoadjuvant chemotherapy for advanced ovarian
cancer. Who really benefits? Aust N Z J Obstet Gynaecol,
58, E25-e26.
PHILP, S., BARNETT, C., D'ABREW, N. & WHITE, K. 2017.
Nurse confidence in gynaecological oncology practice
and the evaluation of a professional development mod-
ule. Contemp Nurse, 53, 203-216.
PHILP, S., MELLON, A., BARNETT, C., D'ABREW, N. & WHITE,
K. 2017. The road less travelled: Australian women's ex-
periences with vulval cancer. Eur J Cancer Care (Engl), 26.
PLAYDON, M. C., NAGLE, C. M., IBIEBELE, T. I., FERRUCCI, L.
M., PROTANI, M. M., CARTER, J., HYDE, S. E., NEESHAM, D.,
66
CHRIS O'BRIEN LIFEHOUSE
67
NICKLIN, J. L., MAYNE, S. T. & WEBB, P. M. 2017. Pre-diag-
nosis diet and survival after a diagnosis of ovarian cancer.
Br J Cancer, 116, 1627-1637.
TONG, P. S. Y., CONG, A. & PATHER, S. 2018.
Hysteroscopy for Pyometra - Treading on
Treacherous Grounds. Gynecol Minim Invasive
Ther, 7, 185-186.
Breast
ATARA POSNER, F. A., DAVID GOLTSMAN AND SANJAY WAR-
RIER. 2017. Practicing changing cases using ICG technol-
ogy in Breast Reconstruction. BJSTR, 1.
FROIS, A. O., HARBOUR, P. O., AZIMI, F., YOUNG, J., CHAN,
B., MAK, C. & WARRIER, S. 2018. The Role of Antibiotics in
Breast Pocket Irrigation and Implant Immersion: A System-
atic Review. Plast Reconstr Surg Glob Open, 6, e1868.
GOLTSMAN, D., YONG CHEONG, J., POSNER, A., ABRAHAM,
E., AZIMI, F. & WARRIER, S. 2018. The Role of Negative
Pressure Wound Therapy for Salvaging Implant-Based
Breast Reconstruction.
OTHMAN, J., ROBBINS, E., LAU, E. M., MAK, C. & BRYANT,
C. 2017. Tattoo Pigment–Induced Granulomatous Lym-
phadenopathy Mimicking Lymphoma. Annals of Internal
Medicine, 167, 830-831.
SYMONDS, J. G., GRANT, A., NEWMAN, A., MIRTO, R. &
WARRIER, S. 2018. PO10 Management outcomes in lac-
tational breast abscesses: 10-year tertiary centre review.
Uro-Oncology
CALOPEDOS, R. J. S., CHALASANI, V., ASHER, R., EMMETT,
L. & WOO, H. H. 2017. Lutetium-177-labelled anti-pros-
tate-specific membrane antigen antibody and ligands for
the treatment of metastatic castrate-resistant prostate
cancer: a systematic review and meta-analysis. Prostate
Cancer Prostatic Dis, 20, 352-360.
CALOPEDOS, R. J. S., GARCIA, C., RASHID, P., MURPHY, D.
G., LAWRENTSCHUK, N. & WOO, H. H. 2017. Citation indi-
ces for social media articles in urology. BJU Int, 119 Suppl
5, 47-52.
DUCHESNE, G. M., WOO, H. H., KING, M., BOWE, S. J.,
STOCKLER, M. R., AMES, A., D'ESTE, C., FRYDENBERG, M.,
LOBLAW, A., MALONE, S., MILLAR, J., TAI, K. H. & TURN-
ER, S. 2017. Health-related quality of life for immediate
versus delayed androgen-deprivation therapy in patients
with asymptomatic, non-curable prostate cancer (TROG
03.06 and VCOG PR 01-03 [TOAD]): a randomised, mul-
ticentre, non-blinded, phase 3 trial. Lancet Oncol, 18,
1192-1201. *
* Publication shared with other Chris O'Brien Lifehouse
department
RESEARCH REPORT 2017 & 2018
ELSNER, K., NAEHRIG, D., HALKETT, G. K. B. & DHILLON, H.
M. 2017. Reduced patient anxiety as a result of radiation
therapist-led psychosocial support: a systematic review. J
Med Radiat Sci, 64, 220-231.
ELSNER, K. L., NAEHRIG, D., HALKETT, G. K. B. & DHILLON,
H. M. 2018. Development and pilot of an international
survey: 'Radiation Therapists and Psychosocial Support'. J
Med Radiat Sci, 65, 209-217.
ESTOESTA, R. P., ATTWOOD, L., NAEHRIG, D., CLAR-
IDGE-MACKONIS, E., ODGERS, D., MARTIN, D., PHAM, M.,
TOOHEY, J. & CARROLL, S. 2017. Assessment of voluntary
deep inspiration breath-hold with CINE imaging for breast
radiotherapy. J Med Imaging Radiat Oncol, 61, 689-694.
*
GRANT, S. J., HUNTER, J., BENSOUSSAN, A. & DELANEY, G. P.
2018. Guidance for establishing an integrative oncology
service in the Australian healthcare setting-a discussion
paper. Support Care Cancer, 26, 471-481.
GRANT, S. J., MARTHICK, M. & LACEY, J. 2018. Establishing
an integrative oncology service in the Australian health-
care setting-the Chris O'Brien Lifehouse Hospital experi-
ence. Support Care Cancer.
HERRMANN, E., NAEHRIG, D., SASSOWSKY, M., BIGLER, M.,
BUIJSEN, J., CIERNIK, I., ZWAHLEN, D., PELLANDA, A. F.,
MEISTER, A., BRAUCHLI, P., BERARDI, S., KUETTEL, E., DU-
FOUR, J. F. & AEBERSOLD, D. M. 2017. External beam radi-
otherapy for unresectable hepatocellular carcinoma, an
international multicenter phase I trial, SAKK 77/07 and
SASL 26. Radiat Oncol, 12, 12.
LEVY, D., DHILLON, H. M., LOMAX, A., MARTHICK, M., MC-
NEIL, C., KAO, S. & LACEY, J. 2018. Certainty within uncer-
tainty: a qualitative study of the experience of metastatic
melanoma patients undergoing pembrolizumab immu-
notherapy. Support Care Cancer. *
M. EDWARDS, K., THOMAS, V., SEET-LEE, C., CHEEMA, B.,
BOYER, M. & MARTHICK, M. 2018. Piloting the Effect of
Aerobic Exercise during Chemotherapy Infusion in Pa-
tients with Cancer: 1653 Board #3 May 31 3.
MARTHICK, M., DHILLON, H. M., ALISON, J. A., CHEEMA,
B. S. & SHAW, T. 2018. Development of a Web Portal for
Physical Activity and Symptom Tracking in Oncology Pa-
tients: Protocol for a Prospective Cohort Study. JMIR Res
Protoc, 7, e136.
MARTHICK, M., DHILLON, H. M., ALISON, J. A., CHEEMA, B.
S. & SHAW, T. 2018. An Interactive Web Portal for Track-
ing Oncology Patient Physical Activity and Symptoms:
Prospective Cohort Study. JMIR Cancer, 4, e11978.
MARTHICK M, A. J., CHEEMA BS, DHILLON H, SHAW T
2018. Pulmonary rehabilitation and eHealth practices for
patients undergoing surgical treatment for lung cancer :
a survey of multidisciplinary team sites in Australia. Aus-
tralian Journal of Cancer Nursing, 19, 14-20.
SMITH C, H. J., USSHER J. M, DELANEY G. P, GRANT S. J,
TEMPLEMAN K., KELLETT A 2017. Integrative Oncology in
Australia 2016: Mapping Service Provision and Exploring
Unmet Needs. Western Sydney University.
SMITH, C. A., HUNTER, J., DELANEY, G. P., USSHER, J. M.,
TEMPLEMAN, K., GRANT, S. & OYSTON, E. 2018. Integra-
Supportive Care and Integrative Medicine
68
CHRIS O'BRIEN LIFEHOUSE
69
tive oncology and complementary medicine cancer ser-
vices in Australia: findings from a national cross-sectional
survey. BMC Complement Altern Med, 18, 289.
SMITH, S. K., CABRERA-AGUAS, M., SHAW, J., SHEPHERD, H.,
NAEHRIG, D., MEISER, B., JACKSON, M., SAADE, G., BUCCI,
J., HALKETT, G. K. B., TURNER, R. M., MILROSS, C. & DHIL-
LON, H. M. 2018. A low literacy targeted talking book
about radiation therapy for cancer: development and ac-
ceptability. Support Care Cancer. *
* Publication shared with other Chris O'Brien Lifehouse
department
RESEARCH REPORT 2017 & 2018
Simes J, Boyer MJ, Young J, Thomas D, Butow P, Vadas M.
Translational Cancer Centre Grant, NSW Cancer Institute.
$6,500,000. (2016-2021).
Barratt A, McCaffery K, Carter S, Glasziou P, Kerridge I,
Semsarian C, Howard K, Doust J, Elshaug A, Moynihan (AI
- Tattersall, M). NHMRC - Centres for Research Excellence
(APP1104136). Creating sustainable healthcare: ensuring
new diagnostics avoid harms, improve outcomes, and di-
rect resources wisely. $2,400,000 over 5 years. (2017-
2021).
Sanson-Fisher R, Butow P, Tattersall M, D'Este C, Doran C,
Martin J. CCNSW Program Grant. Improving and maintain-
ing holistic cancer survivor outcomes. A system-based
program. $2,234,524.91 over 5 years. (2018-2022).
Juraskova I, Butow P, Laidsaar-Powell R, Boyle F, Yates P,
Schofield P, Kay J, Costa D. AI: Tattersall, M. NHMRC Pro-
ject Grant (APP1146383). Empowering the clinician-pa-
tient-carer TRIO: RCT of a novel online education modules
to facilitate effective family carer involvement in oncolo-
gy. $593,201.60 over 3 years. (2018-2020).
CI: Hui, M. NBCF Investigator Initiated Research Scheme.
Discovering new therapeutic strategies for metastatic tri-
ple negative breast cancer at cellular resolution. (2018).
Hui, M. Sydney Breast Cancer Foundation Research Fellow-
ship. (2017).
CI: Hui, M. Roche Research and Development Grant.
(2017).
Hui, M. Sydney Catalyst Prof Rob Sutherland Travel Award.
(2017).
Lindeman G, Mann G, Desai J, Forbes J, Fox S, Liew D,
Mcarthur G, Simes J, Sutherland R, Visvader J. Centre of
Research Excellence for Translational Breast Cancer Re-
search. From Discovery to Better Health Outcomes.
$2,500,000. (2012-2017).
Simes J, Keech A, Gebski A, Stockler M, Caterson I, Cola-
giuri S, Schofield D, Marschner I. Advancing the Evidence
Base for Care and Policy in Priority Health Areas (Program
Grant) 1037786. $10,643,000. (2013-2017).
Simes J. Research Fellowship, 1121008. $863,910.
(2017-2021).
Simes J. Program Grant, 1150467. $12,215,472. (2019-
2023).
Anderson RL, Swarbrick A, Johnstone R, Chua B, Gill A,
Khanna K, Lakhani S, Loi S, O'Toole S, Saunders C. AI 4: Be-
ith J. Development of a national resource of primary and
secondary metastatic breast cancers to test new drugs
and identify the genetic changes that drive breast can-
cer growth and metastasis. NBCF National Infrastructure
Grant. $1,834,335 (2015-2019) AI 4
Mahon, K. Movember Prostate Cancer Foundation of Aus-
tralia Clinician Scientist Award. $450,000. (2016-2018)
Movember Revolutionary Team Award. $3 million. (2015-
2020).
Butler L, Hoy A, Swinnen J, Wittert G, Scott A, Tilley W.
Exploiting alterations in lipid metabolism to improve di-
agnosis, treatment and molecular imaging of prostate
cancer. Role: Team member – Kate Mahon
CIs: Butler L, Horvath L, Tilley W, Stricker P. Cancer Austral-
ia/Prostate Cancer Foundation of Australia. 1050880. A
pharmacodynamics study of the heat shock protein 90
(Hsp90) inhibitor, AUY922, in high-risk, localized prostate
cancer. $590,000. (2013-2019).
Medical Oncology
72
CHRIS O'BRIEN LIFEHOUSE
73
CIs: Thomas D, Horvath LG. Cancer Gene Discovery and
Validation Program. RT Hall. $334,425. (2016-2018).
CI: Horvath LG. Peer-reviewed Astellas research project
grant. Exploiting lipid metabolism to predict response
to treatment in advanced prostate cancer. $200,000.
(2016-2018).
CIs: von Itzstein M, Horvath LG. Peer-reviewed grant from
private foundation. The Cancer Glycome Project. $2.54
million. (2016-2018).
CIs: Hart D, Clark G, Horvath L. CINSW Translational Pro-
gram Grant. Therapeutic Antibody Translation into Pa-
tients. $3.45 million. (2017-2022).
Horvath L. Below the Belt ANZUP. Statins in metastat-
ic castration-resistant prostate cancer study. $36,000.
(2017-2019).
CIs: Stricker PD, Clark SJ, Hayes VM, Horvath LG, Kench JG,
Rasiah K, Joshua A. Australian Government Department
of Health and Aging. Australian Prostate Cancer Research
Centre - NSW. Integrating research into clinical practice in
prostate cancer. $1.5 million. (2017-2018).
CIs: Horvath LG, Stricker PD, Kench J, Joshua A, Clark S,
Emmett L, Hayes V. CINSW Translational Program Grant.
TPG172146. $3.75 million. (2018-2023).
CIs: Butler L, Lynn D, Hayes V, Horvath L, Mills I, Centen-
era M. PdCCRS Cancer Australia Project Grant. Novel
co-extinction strategies for treatment of prostate cancer.
$596,409. (2018-2020).
CIs: Sandhu S, Horvath LG. Prostate Cancer Founda-
tion Challenge Award. Harnessing synergies between
177Lu-PSMA therapy and olaparib to improve clinical out-
come of men with metastatic castration resistant pros-
tate cancer (CRPC). (2017-2019).
Butler LM, Swinnen JV, Tilley WD, Scott AM, Hoy AJ, Wittert
GA, Horvath LG. Movember Foundation / Prostate Can-
cer Foundation of Australia (Revolutionary Team Award).
Exploiting alterations in lipid metabolism to improve
diagnosis, treatment and molecular imaging of pros-
tate cancer. Phase I: 2015-2018, $3,250,000. Phase II:
2019-2020, $2,000,000.
Fazekas de St Groth B, Kao S, Brown M, de Souza P, Grimison
P, Ormerod J, McGure H. Predicting responses to cancer
immunotherapy. Cancer Council Australia Project Grant,
$599,705. (2018-2020).
Keebone A, Samra J, Le H, Nguyen N, Goldstein D, Apte M,
Barbour A, Oar A, Chander S, Espinoza D. AI Grimison, P.
mFOLFIRINOX And STEreotactic body Radiotherapy (SBRT)
for Pancreatic cancer with high-risk and Locally AdvaNced
disease (MASTERPLAN): a multicentre, randomised phase
II study of the Australian Gastrointestinal Trials Group
(AGITG). NHMRC MRFF Low Survival Cancers and Diseases
(LSCD) Grant, $1,470,201. (2018 - 2022).
Rasko J, Sandroussi C, Grimison P, Adelstein S. Cellular im-
muno-gene therapy for pancreatic cancer. Cancer Coun-
cil NSW Pathways to a cancer-free future Grant Scheme,
$2,000,000. (2018 - 2022).
Grimison P, Haber P, Stockler M, Lintzeris N, Simes J,
McGregor I, Oliver I, Allsop D, Gedye C, Kirby A. Pilot
and definitive randomised double-blind placebo-
controlled trials evaluating an oral cannabinoid-rich
THC/CBD cannabis extract for secondary prevention of
chemotherapy-induced nausea and vomiting. NSW Health.
$2,792,269. (2015 – 2021).
Goldstein D, Friedlander M, Kiernan M, Krishnan A, Boyle
F, Moalem-Taylor G, Haas M, Cohn R, Farrar M. AI Grimison
P. Chemotherapy-induced Peripheral Neuropathy: Assess-
ment strategies, Treatments and Risk Factors. Cancer In-
stitute NSW Program Grant for Excellence in Translational
Research. $3,040,000. (2015 – 2019).
Butow P, Andrews G, Kelly B, Girgis A, Aranda S, Viney R,
Clayton J, Hack T, Price M, Beale P. AI Grimison P. A sus-
tainable and supported clinical pathway for managing
anxiety and depression in cancer patients: Developing and
evaluating components and testing implementation strat-
egies. Cancer Institute NSW Program Grant for Excellence
in Translational Research. $3,643,992. (2015 - 2019).
Grimison P, Toner G, Stockler M, Friedlander M, Thomson D,
Gebski V, King M, Quinn D, Singhal N. Accelerating first-line
chemotherapy to improve cure rates for advanced germ
cell tumours: an Australian-led, international randomised
trial. Cancer Australia and Cancer Council Australia Project
Grant, $595,342. (2013 - 2018).
RESEARCH REPORT 2017 & 2018
Kao S. Cancer Council NSW Competitive Grant 2018. Pre-
dicting response to checkpoint therapy in lung cancer pa-
tients as CIB. $758,033.50 over 5 years.
Kao S. Cancer Institute Research Infrastructure Grant
2015: "Expanding the Asbestos Diseases Research Insti-
tute (ADRI) biobank to create a state-wide repository for
research into thoracic cancers" as CIA. $300,000. (2015
- 2018).
Head and Neck
CI: Luk P. Sydney Catalyst 2018. Understanding the Body's
Response to Cancer Invasion and Progression: Towards
Assisting the Body's Defence System in Fighting Cancer.
$50,000.
CI: Gupta R. ANZHNCS 2018. Can Clinical Validation of
Biologic Predictors of Metastases in Head and Neck Cu-
taneous Squamous Cell Carcinoma be Achieved by Tran-
scriptomic Profiling. $10,000.
CI: Clark J. ANZHNCS Reconstructive Surgery Grant 2018.
The Bionic Lid Implant for Natural Eye Closure (BLINC).
$10,000.
Awarded to Beyond Five. NSW Department of Health
2018. Developing a sustainable structure for Beyond
Five. $15 000.
Awarded to Beyond Five. Brady Cancer Support Founda-
tion 2018. Development of Head and Neck Cancer Pod-
casts. $10,000.
CI: Vasan K. General Surgeons Australia 2018. Young pa-
tients with head & neck squamous cell carcinoma – Iden-
tification of mismatch repair gene mutations. $1,000.
CI: Satgunaseelan L. RCPA Foundation Postgraduate Re-
search Fellowship 2018. Identifying actionable mutations
in young patients with oral cavity squamous cell carcino-
ma. $25,000.
Awarded to Beyond Five. Dry July 2018. Dry July Founda-
tion grant to develop evidence based and easy to follow
animations that help patients maintain good nutrition
and stay well hydrated before, during and after treat-
ment. $34,000.
CI: Clark J. ANZHNS Reconstructive Surgery Grant. The Bi-
onic Lid Implant for Natural Eye Closure (BLINC). $10,000.
Venchiarutti R. COSA Travel Grant. $425.
Venchiarutti R. Cancer Research Network University of
Sydney. Cancer Research Network Postgraduate Student
Conference Travel Grant. $1,716.
Venchiarutti R. Primary Care Collaborative Cancer Clinical
Trials Group (PC4): Self-reported management of possi-
ble symptoms of head and neck cancer: a primary care
vignette survey. $4,000.
Satgunaseelan L. RCPA Foundation Research Postgradu-
ate Fellowship. $25,000.
CI: Clark J. Equity Trustees. Identifying the genetic drivers
of Metastasis in skin cancer. $30,000.
CI: Findlay M. Sydney Research Health Informatics Re-
searcher PhD Scholarship. Towards Value-Based Compre-
hensive Cancer Care: Development and Implementation
of a Next Generation Nutrition Care Analytical Dashboard
for Patients with Head and Neck Cancer. $120,000.
CI: Findlay M. Australia and New Zealand Head and Neck
Cancer Society Research Foundation. Enhanced Recovery
After Surgery: Feasibility of Pre-operative Carbohydrate
Loading in Patients Undergoing Major Head and Neck
Cancer Surgery with Free Flap Reconstruction. $5,000.
CI: Bhadri V. Australian Young Cancer Patient Clinical Trials
Initiative 2018 – Ewing sarcoma. $522,000.
CI: Bhadri V. Australian Young Cancer Patient Clinical Trials
Initiative 2018 – Medulloblastoma. $965,000.
AI: Bhadri V. Australian Young Cancer Patient Clinical Trials
Initiative 2018 – Genomic Screening. $950,000.
74
CHRIS O'BRIEN LIFEHOUSE
75
CI: Clark J. University of Sydney: Biomedical Research Col-
laboration Scheme. $15,000. (2017-2018).
CI: Nadia Rosin. Tour de Cure 2018. Australia and New
Zealand's first Head and Neck Cancer Patient Support
Group Portal. $31,000.
CI: Clark J. Sydney Local Health District. Building the IT
Infrastructure Needed to Support the SHNCI Research Pro-
gram and to Improve Outcomes in Head and Neck Can-
cers. $300,000.
CI: Clark J. Sydney Local Health District. Identification of
therapeutic targets, prognostic and predictive markers in
high grade head and neck cancers that currently lack sec-
ond line therapies. $300,000.
CI: Clark J. Sydney Local Health District. The Bionic Lid Im-
plant for Natural Lid Closure (BLINC) for facial paralysis.
$150,000.
CI: Bruce Ashford. Genomic Landscape of metastatic cu-
taneous squamous cell carcinoma ANZHNCS Research
Grant. $5,000. (2016-2017).
CI: Clark J. Australian and New Zealand Head and Neck
Cancer Society Foundation 2016: Markers of metastases
in cutaneous SCC using Nanostring. $5,000.
CI Findlay M. NHMRC-Cancer Institute NSW Translating
Research Into Practice Fellowship. Best evidence to best
practice: Implementing an innovative model of care for
nutritional management of patients with head and neck
cancer. $272,911. (2015-2017).
Prostate Cancer Foundation of Australia. Biologically Smart
Radiotherapy: killing more prostate cancer by stimulating
immune responses. $98,180.
University of Sydney ECR/MCR Seed Grant. Improving pa-
tient outcomes in radiation therapy: does imaging dose
affect the tumour response. $10,000.
University of Sydney Research Equipment Grant. To deter-
mine the impact of an additional imaging CBCT dose on
cell survival following radiation therapy. $9,906.
Radiation Oncology
CI: Suchowerska N. Prostate Cancer Foundation of Aus-
tralia. Biologically Smart Radiotherapy: killing more pros-
tate cancer by stimulating immune responses. $98,180.
CI: Suchowerska N. University of Sydney ECR/MCR Seed
Grant. Improving patient outcomes in radiation therapy:
does imaging dose affect the tumour response. $10,000.
CI: Suchowerska N. University of Sydney Research Equip-
ment Grant. To determine the impact of an additional
imaging CBCT dose on cell survival following radiation
therapy. $9,906.
CI: Suchowerska N. Sydney Breast Cancer Foundation.
Breast cancer research. $10,000. 2017.
Gynaecological Oncology
ASCCP. A cohort of patients with HPV negative, High
grade cervical dysplasia. $10,000.
RESEARCH REPORT 2017 & 2018
Lacey J. MSD. Living well with melanoma. $135,000.
(2017-2018).
Marthick M. Donor. Livingroom@home. $100,000.
Lacey J, Marthick M, Templeton S. Dry July. Lymphoedema
(LEAP). $30,000.
Lacey J, Marthick M, Dickson C. Donor. Mindfulness@
home. $10,000.
Lacey J, Marthick M, Dickson C. Tour de Cure 2018. Mind-
fulness@home. $70,000.
Lacey J, Grant S, Spiegel G. Donor. Reflexology and Acu-
puncture in day therapy unit. $20,000.
Lacey J. Donor. Supportive care study. $100,000.
Lacey J, Grimmison P. NSW Health. Medicinal Cannabis
NSW health observational and PK study. $3,600,000.
Lacey J. Bioceuticals. Medicinal Cannabis: Recurrent GBM.
$500,000.
Supportive Care and Integrative Medicine
Breast
AirXpander: Satisfaction of Carbon Dioxide Based Tissue
Expander for Breast Reconstruction. $5,000.
76
CHRIS O'BRIEN LIFEHOUSE
Featured Artist: Julia Westwood
All artworks in this report are acrylic on canvas
paintings by Julia Westwood. Julia, a National
Art School graduate, was Artist In Residence
at Chris O'Brien Lifehouse in 2019. The Artist
in Residence program is an initiative by Arterie
that brings practising artists to demonstrate
in the main foyer of Chris O'Brien Lifehouse.
www.juliawestwood.com.au.
Chris O'Brien Lifehouse
119 - 143 Missenden Road
Camperdown NSW 2050
PO Box M5 Missenden Road
Camperdown NSW 2050
www.mylifehouse.org.au
General Enquiries
T: (02) 8514 0000
Donations & Support
T: (02) 8514 0006
ABN 70 388 962 804
Registered Charity Number CFN 17573
Hospital Provider Number 0027350Y
© 2019 Chris O'Brien Lifehouse
Report produced by Professor Lisa Horvath,
Sarah Charlton Li and Juliette O'Brien.
Designed by Juliette O'Brien.
Printed by Vertifix Printing.