Annual Review - My Lifehouse
Transcript of Annual Review - My Lifehouse

2018/19
Annual Review
Artist: Julia Westwood
TREATING PEOPLE,
NOT JUST CANCER

- Professor Chris O'Brien AO
If you have a critical mass of people with a unity of purpose, then you must be
successful.
“
”

To transform cancer treatment for Australian cancer patients through an environment thriving on discovery, research and uncompromising care.
Our Vision
To improve the quality of life for Australian cancer patients, carers and their families by advancing the understanding, diagnosis, treatment, care, cure and prevention of cancer.
Our Mission
Chris O’Brien Lifehouse combines cancer surgery, chemotherapy, radiation therapy, complementary therapy, research and emotional support in one facility. Our integrated model of care allows specialist cancer services to be delivered by a multidisciplinary team, as much as possible under one roof, eliminating the need for patients to navigate a complex series of appointments at different locations.
Our Model of Care
We acknowledge and pay respect to the traditional owners of the land on which Chris O’Brien Lifehouse is built: the Gadigal people of the Eora nation. As we share our knowledge, teaching, learning and practices, may we also pay respect to the
knowledge embedded forever within the Aboriginal Custodianship of Country.

ContentsPa
rt 1
Snap
shot
sPa
rt 2
Feat
ures
Part
3U
pdat
es

How to read this report
At Chris O’Brien Lifehouse, we strive to be patient-centred in every respect — including this document. Therefore the focus here is patient voices and experiences, which provide a gateway into care highlights and service updates. These can be found in Features (part 2). We extend our deep thanks to the patients and families who gave permission for their stories and images to be published. This report also includes an executive summary (snapshots - part 1) and full updates of services and departments (part 3). All elements are indexed to the right.
Snapshots68 Welcome message from Chair and CEO10 Data snapshot14 Financial snapshot15 Philanthropy snapshot18 Leadership team33 Research snapshot
Features2022 This is comprehensive, multidisciplinary care
26 This is compassionate, uncompromising care
28 This is collaborative care
32 In focus: Comprehensive Sarcoma Centre
34 This is research-driven care
36 In focus: Pharmacy and clean room
38 This is patient-centred care
41 In focus: Regional, rapid and specialty care clinics
44 This is holistic care
46 In focus: Music therapy
48 This is a caring community
Updates5052 Medical oncology54 Radiation oncology56 Nursing57 Head and Neck59 Breast60 Gynae-oncology61 Neuro-oncology62 Uro-oncology63 Upper GI63 Gastroenterology64 Colorectal surgery64 Thoracic surgery65 Supportive Care and Integrative Medicine67 Allied Health68 Music in Health69 Patient Advocacy70 Patient Advisory Council (PAC) 71 Volunteers72 Arterie


Summary
Snapshots

8
Welcome and Thank you
We are delighted to present to you the Chris O’Brien Lifehouse Annual Review.
This report covers a period that included two important milestones for our organisation: November 2018 marked five years since the facility opened to patients, and June 2019 was 10 years since Chris O’Brien AO died.
So it is fitting that this period itself ushered in a new beginning - one in which we moved from consolidation to emergence as a constructive contributor to cancer care, benefiting the community.
We have become a hub of innovation and discovery, both through structured research and as a by-product of the complexity of the work done by our clinicians.
We are now one of the biggest cancer clinical trials centres in NSW. Our researchers have contributed to practice-changing research in several areas.
The hospital has reached full operating capacity. Volume and complexity increased in most services.
Data from Cancer Institute NSW showed our patients have better outcomes in crucial moments. These include higher survival and lower mortality rates after surgery for breast, ovarian and head and neck cancers. Details about this
data can be found in the snapshots on the following pages.
We believe this is emerging evidence of the value of the comprehensive cancer centre model in Australia. Our integrated, holistic, patient-centred model of care is focussed on improving patient outcomes.
But it is also about bringing a human touch to cancer care. Our patient experience outcomes are very positive, with Cancer Institute data and Net Promoter Scores showing high rates of approval. (Details in data snapshots).
Unequivocally, all of these achievements are attributable to the professionalism and dedication of our people. Attracting and retaining an outstanding workforce
Doug SneddenChair
Eileen HannaganChief Executive Officer

9
is a consequential focus, as well as creating an environment where patient-centred care can flourish. We’re pleased to report that a survey examining culture showed staff engagement is high.
We cannot emphasise enough that Chris O’Brien Lifehouse is a collaborative and community-based organisation. Our relationships with Royal Prince Alfred Hospital, the University of
Sydney, Sydney Local Health District and NSW Ministry of Health are our pillars. The State and Federal Health Ministers have also been a tremendous support over the past year.
Besides our partnership organisations and staff, our thriving community is made up of collaborating colleagues (both in clinical work and research), invaluable and generous donors, volunteers, patients and families along with their representatives and advocates, and our local neighbourhoods. It truly is a ‘critical mass of people with a unity of purpose’.
We would like to extend a warm welcome to our new patron, Her Excellency the Honourable Margaret
“Six years ago, we set out to deliver a new model of cancer care, combining comprehensive, integrated clinical services with research and education. Today, as we see evidence of improved patient outcomes and practice-changing research, the benefits of that model of care are starting to become clear.”— Professor Michael Boyer AM Chief Clinical Officer
Beazley AO QC Governor of NSW, as she joins this community also.
There are more important milestones on the horizon. In the second half of 2019 we underwent an external accreditation process under new patient-focussed quality measures. The results will be reported in full in the next annual review, but suffice to say that assessors deemed Chris O’Brien Lifehouse a leader in patient-centred care.
We put patients and families at the centre of everything we do. That is why this annual review is told primarily through their eyes and voices. We are grateful to them for allowing us to tell their stories.
— Doug and Eileen

10
We are hereData snapshot
Total bed days Total operations
Examples of growth across tumour streamsData: admitted patients, including overnight and same day stays. Public and private.
Growth in services
Source: Internal data
In the past year, the hospital has reached full operating capacity. Most services have seen significant increases in volume and complexity of clinical work.

11
A - Worries or fears completely discussed by health professionalsB - Informed of wait time (when had appointment and had to wait)C - Completely given enough information to manage side effectsD - No attendance of emergency in past 3 months due to complicationsE - Care received at clinic was very well organised
Better patient experience
Consumer NPS
Our consumer Net Promoter Score (NPS) is now averaging 90. Data from Cancer Institute NSW* showed our patients reported better responses to aspects of care as compared with the wider state.
Avg > 90
Patient reported responses to aspects of care for patients attending an outpatient cancer clinic in NSW, November 2017.
* Source: Cancer Institute NSW, ‘Reporting for Better Cancer Outcomes Performance Report 2018’ (‘the RBCO 2018 report’). This report uses data from 2017 and 2018. Later data will be available in our next annual review.
The very best. Every-body truly cares for
you. They treat you as if you were the most important person in the world. Business
Class service.
You could not have done more. Everyone was great. Thanks so much for taking me from the dark space
to the sunshine.
— Patient feedback

12
90 day mortality
Length of stay greater than 14 days
Unplanned readmissions within 28 days
Surv
ival
rat
e %
Head and neck surgical outcomes Highest number of resections in NSW with among the lowest rates of mortality.
Ovarian cancer surgical outcomes Better outcomes immediately following surgery.
Improved patient outcomes
Data from Cancer Institute NSW showed better patient outcomes in crucial moments, including higher survival and lower mortality rates after surgery for breast, ovarian and head and neck cancers.
Breast surgical outcomes Second highest number of resections in NSW with highest one-year survival rate following mastectomy.
Perc
enta
ge %
Perc
enta
ge %
Mor
talit
y ra
te %
Mor
talit
y ra
te %
30 day mortality
30 day mortality
Mor
talit
y ra
te %
One year survival

13
Strong culture of engaged staff
Source: Best Practice Australia survey
‘I would recommend my organisation to a friend or family
member as a good place to work.’
‘I would recommend my organisation to a friend or family member as the
best choice if they required thetype of service we provide.’
Despite the pressures of working in a facility dedicated solely to treating people with cancer, staff morale is high and our culture is positive when compared with sector benchmarks.
“Thanks so much to the nurse who helped calm my nerves when I was scared about my surgery. I was so grateful she explained everything so well and clearly. Got me a warm blanket and settled me in to have my operation.”— Patient feedback

14
As a not-for-profit, benevolent institution, Chris O’Brien Lifehouse treats both public and private patients. Our revenue is derived from a combination of Medicare, NSW case-mix funding, privately or self-funded patients and a devoted, generous philanthropic community.
Profit for all
Hospital revenue Philanthropy revenue*
*Philanthropy revenue before 2016 used different fundraising arrangements.
“We often refer to our business model as public-private. But that’s not entirely accurate. It’s not two Ps, but three: public, private and philanthropy.” — Mrs Gail O’Brien AO
Financial snapshot

15
Philanthropy achieved significant growth in fundraising activity in FY18/19. Many of our donors are individuals — patients, former patients or family members — who have had first-hand experience of Chris O’Brien Lifehouse care. Philanthropy plays a vital role in our ability to provide a holistic and patient-centred model of care. Support from our donors goes directly to funding research, clinical care and equity of access to treatment, ultimately improving outcomes for patients and families. Here are some ways in which philanthropy has had a real impact in the last year.
Gifts that count
100% philanthropically-funded positions
NEURO-ONCOLOGY Head of Brain Cancer Research
The neuro-oncology research program focuses on GlioNET — a longitudinal study of brain cancer specimens that will support a number of specific sub-studies, including the translation of a non-invasive blood test for monitoring glioma tumour progression. This position will drive this research forward.
HEAD AND NECK Research Fellow
This fellowship focuses on genome sequencing that examines the relationship between DNA mutations and tongue cancer in young people.
GYNAE-ONCOLOGY Deputy Director and Dedicated Research
The Deputy Director role, which includes dedicated research, works with the Royal Prince Alfred and Chris O’Brien Lifehouse Peritonectomy MDT. This research focuses on Heated Intraperitoneal Chemotherapy (HIPEC).
SARCOMA Clinical Trials Coordinator
Chris O’Brien Lifehouse has the largest clinical trials program for sarcoma in NSW, with 11 clinical trials currently open to patients. This position coordinates those trials and patients taking part.
SARCOMA AND LUNG Clinical Nurse Specialists
Clinical Nurse Specialists have specialised knowledge and experience (at least two years), and are qualified to coordinate treatment, develop treatment plans and deliver advanced care. They are the primary point of contact for patients and vital to delivering uncompromising, patient-centred care.
“Our donors help to drive research that can make paradigm shifting changes in the way we treat cancer and ultimately, improve outcomes for patients.”— Dr Kim Kaufman, Head of Brain Cancer Research
MUSIC THERAPY 3 x Music Therapists (1.8 full time equivalents)
Our entire Music in Health program is philanthropically funded, bringing therapeutic music, song-writing and live performance in shared spaces to patients and families.
Philanthropy snapshot

16
THE PATIENT AND
PHILANTHROPIST
Jennie Connolly THE CLINICIAN AND
RESEARCHER
Dr Rhonda Farrell
THE
PATIENT TODAY AND TOMORROW
Ivana Rapajic-Moran
How philanthropy, research and care are linked
Jennie was treated for ovarian cancer by the gynae-oncology group.
She was an active member of the Chris O’Brien Lifehouse community, especially Arterie.
Jennie bequeathed a donation to Lifehouse with instructions that the funds should be used for gynaecological cancer research. Jennie passed away in June, 2018.
Dr Rhonda Farrell is Deputy Director of gynae-oncology and an active researcher.
While Rhonda’s position is funded overall by philanthropy, Jennie’s bequest is funding Rhonda’s research into Heated Intraperitoneal Chemotherapy (HIPEC) — a form of heated chemotherapy that is delivered in a targeted way.
Ivana was diagnosed with ovarian cancer in 2019.
Her treatment was a peritonectomy followed by HIPEC — the latest and most advanced available.
Ivana’s outcomes form part of Rhonda’s research, meaning she is being treated in a scientific-based, research-driven context that will ultimately lead to better outcomes for patients in her position in the future.
“One of my aims is to gather and improve current evidence, and work out which women really do benefit from this treatment.”— Dr Rhonda Farrell

Philanthropy supports several funds that ensure equity of access to services and treatments.
Equity of Access Funds
“Knowing I am a beneficiary of the fund that held me in my lowest moments, that relieved my existential crisis of being able to keep myself and my daughter afloat by shouldering some of the financial burden and continues to support me as I am ‘put back together — body, mind and soul’, has been one of the greatest gifts of my life.”— Victoria Spence, who has received support from the Head and Neck Cancer Hardship Fund, which covers out-of-pocket expenses such as nutrition, accommodation, transport, pharmacy, LivingRoom services and treatment not covered by insurance.
• Surgery, including robotic surgery
• Pharmacy costs• Radiation therapy• Transport and
accommodation• Supportive Care and
Integrative Oncology
The number of patients who access complementary therapies through the LivingRoom Equity of Access Fund
55
Keith Cox OAM ScholarshipIn February 2018, we launched the Keith Cox Clinical Education Fund, named in honour of Keith Cox OAM, a pioneer in cancer nursing.
The purpose of the fund is to support nurses and allied health staff in their professional development to enhance patient care. It gives grants of up to $10,000.
In the last financial year, we:
“The experience allowed me to liaise and network with other sarcoma nurses across Australia.”— Katie Thomson, sarcoma clinical nurse specialist, who used her scholarship to attend the Australian Sarcoma Group 2018 Annual Scientific Meeting.
• raised $178,000
• received 39 applications
• awarded grants to 27 nurses and allied health staff
/ month

18
Doug SneddenChair
Appointed to the board in November, 2013. Appointed Chair of the Board in February, 2014. Appointed a member of the company on 13 February 2014. Member of the Foundation Committee.
Rebecca Davies AODeputy Chair
Appointed to the board in April, 2014. Chair of the Board of Clinical Governance Committee.
David Brettell
Appointed to the board in October, 2014. Chair of the Foundation Committee.
Ian Hammond
Appointed to the board in April, 2015. Chair of the Audit & Risk Management Committee. Appointed as a member of the company on 28 June 2016.
Prof Diana Horvath AO
Appointed to the board in May, 2009. Chair of the Market Positioning & Business Development Committee and the Quality & Safety Committee.
A/Prof Brian McCaughan AM
Appointed to the board in February, 2016. Member of the Market Positioning and Business Development Committee. (Brian is on the left).
Directors and executive
The leadership teamBoard of Directors

19
Robert McMillan OAM
Appointed to the board in February, 2005. Appointed as a member of the company on 6 July 2012. Member of the Foundation Committee.
Max Moore-Wilton AC
Appointed to the board in July, 2007.
Gail O’Brien AO
Appointed to the board in September, 2009. Member of the Foundation Committee. Patron of the Chris O’Brien Bequest Society.
Briony Scott
Appointed to the board in February, 2019.
Prof Michael Boyer AMChief Clinical Officer
Appointed to the board in August, 2003. Member of the Audit & Risk Management Committee, the Market Positioning & Business Development Committee and the Board Clinical Governance Committee.
Eileen HannaganChief Executive Officer
Appointed as CEO and to the board in April, 2014. Member of the Audit and Risk Management Committee, the Market Positioning & Business Development Committee, the Board Clinical Governance Committee and the Foundation Committee.
Eileen Hannagan CEO
Hospital Executive Committee
Prof Michael Boyer AMChief Clinical Officer
Catherine LambertDirector, Nursing and Clinical Operations
Rodney GreenDirector, Corporate Services
Kristin CarneyGeneral Manager, Services Development
A/Prof Chris MilrossDirector, Radiation Oncology

20

21
Features

22
This is
Comprehensive, Multidisciplinary Care
Dr Liz Connolly and Dr Mun Hui in the Breast Multidisplinary Team (MDT) meeting.

23
Lindsay Foster, a Judge in the Federal Court, was treated for a rare type of
salivary gland cancer. His story illustrates wide-ranging, comprehensive care by a
multidisciplinary team.
Lindsay Foster’s cancer story begins like many others: he noticed a lump. It was on the left side of his neck.
A biopsy and CT scan indicated a type of salivary gland cancer called mucoepidermoid carcinoma. Salivary gland cancers are considered rare. Mucoepidermoid carcinoma is the most common among them.
A head and neck surgeon at another large Sydney hospital quickly scheduled surgery of the neck, however another scan (this time a PET) revealed activity in two other parts of the body. Most concerning of these was under Lindsay’s tongue.
“Every piece of news was getting worse,” said Lindsay.
Complex floor-of-mouth surgery appeared likely. The surgeon referred Lindsay to Chris O’Brien Lifehouse, which specialises in treating complex and rare cancers.
At his first consultation, A/Prof Carsten Palme, Director of the Head and Neck Service, explained the multidisciplinary team approach to Lindsay.
“He told me that they workshop the cases,” Lindsay said. “He said ‘there
will be a room full of doctors, as well as nurses and allied health. You’ll sit in my room while we discuss your case.’”
The following Monday, that is what happened. Lindsay waited in the head and neck rooms for Carsten to arrive with three colleagues — surgeons Prof Jonathan Clark AM and Dr Anthony Clifford, and Radiation Oncology Director A/Prof Chris Milross.
Each of them examined Lindsay and raised questions. They left and a few moments later, Carsten returned alone and asked Lindsay, “How does Saturday sound?”

24
He told Lindsay that the operation would require two separate surgical teams. The first, led by himself, would remove the cancer and lymph nodes. The second, led by Jonathan, would manage the floor-of-mouth reconstruction including a free flap reconstruction, which means transferring skin and blood supply from another area of Lindsay’s body such as the forearm or groin.
“It’s a very long operation. We’ve done it before. We feel confident,” Carsten said.
The operation lasted 9.5 hours.
“I had two specialist teams of surgeons working together, after due consideration in a workshop of eminent doctors ... it was complicated, and they needed all their brilliance which they have in spades,” Lindsay said.
During surgery, anaesthetist Dr Murray Stokan rang Lindsay’s wife, Anne, twice with updates. He also sent regular text messages. Nurse Practitioner Sarah Davies worked with ward staff to monitor Lindsay’s recovery, particularly the condition of the free flap.
In the weeks after surgery, Lindsay underwent concurrent radiotherapy and chemotherapy.
Dietitian
Two surgeons, leading consecutive
surgical teams
Director of radiation oncology
Nurse practitioner specialising in
Head and Neck
Anaesthetist
Speech pathologist
Medical oncologists
Lymphoedema physiotherapist
Exercise physiologist
RPA Dental Clinic
Before surgery, seven different members of a multidisciplinary team contacted Lindsay:
During and after this treatment, Lindsay accessed holistic care from a network of integrated services. In addition to those already mentioned, these included:

25
Throughout the entire period, Sarah, was always contactable by Lindsay. “I had a nurse practitioner, Sarah, who has looked over me the entire time, in all respects. If I sent her a text, she would come straight back,” Lindsay said.
In late February, as swelling and soreness around Lindsay’s jaw worsened, Lindsay was re-admitted to hospital for an advanced infection.
“As I’ve had these ongoing issues with the infection, I’ve had Carsten, Jonathan and Chris seeing me at regular intervals depending on my needs at the time. Carsten would see me every week. Carsten, Jonathan and Chris talk to each other. It’s very reassuring.”
Collaborative care
In the initial stages of treatment planning, Chris Milross referred Lindsay to the RPA Dental Clinic. While Lindsay did not need dental work ahead of surgery, the service was a crucial part of monitoring throughout his treatment.
About six months after surgery, the dental oncology team found a hole in the flap front that exposed bone underneath Lindsay’s molar. Later, a large area of exposed bone towards the back of the left side of his jaw became visible. It was osteoradionecrosis — deadening of the bone caused by radiation therapy and probably the infection.
Through collaboration between the dental clinic at RPA, the head and neck service and the radiation oncology unit, the osteoradionecrosis is being managed cautiously with further surgery a potential outcome.
SERVICE HIGHLIGHTS
Head and Neck
• Data from CancerInstitute NSW (RBCOreport 2018) showedthe head and neckservice performsthe largest numberof head and neckcancer surgeries inNSW, doing moreresections than thenext two busiesthospitals combined.
• Data also showedbetter patientoutcomes for headand neck patientstreated at ChrisO’Brien Lifehouse (seeSnapshots p13).
• We have expandedregional and specialtyclinics (see page41 for details aboutclinics).
Full update p 57
SERVICE HIGHLIGHTS
Breast
• Data from theCancer Institute NSWshowed Chris O’BrienLifehouse was thesecond largest breastcancer unit in NSW byvolume of surgery.
• The team achieved50% femalerepresentation insurgical staff (i.e.five female breastsurgeons).
• The team performedthe first ‘awake’mastectomy inAustralia.
Full update p 59
SERVICE HIGHLIGHTS
Allied Health
• All services have seenconsiderable growthin the context ofincreased hospitalactivity.
• Clinics developed invoice, swallowing andpost-surgical follow-up.
• Two new positionswere created:— Discharge PlanningService commencedin April 2019,working closely withSocial Work andNursing management— OccupationalTherapy servicecreated in February2018.
• Physiotherapyrecruited its first newgraduate.
• Speech Pathologyservices have grownwith a majority ofwork in the headand neck serviceand expansioninto neurosurgicalpatients.
Full update p 67

26
“Healthcare is so complex to navigate, but it was so nice to
see other organisations working with us to achieve that patient-
centred goal.”— Kristina Parungao, Nurse Unit Manager
of surgical ward 8 North (pictured)

27
Mark* was far from home when disaster struck. He and his wife had set off from Queensland to caravan through NSW, when he suddenly lost movement on his left side. He was rushed to RPA, where a tumour was discovered in his brain. Head of neurosurgery Dr Brindha Shivalingham operated on him at Chris O’Brien Lifehouse.
Following surgery, Mark was immobile and confused. As his condition moved from acute to rehabilitative, he needed help getting home.
The family learned that the aero-medical support he needed would cost $12,000.
“It was probably the most challenging discharge I’ve ever faced,” said Kristina Parungao, Nurse Unit Manager of surgical ward 8 North.
The situation was so stressful for Mark’s family his wife suffered a strain-related attack and was admitted to RPA herself. His son flew to Sydney.
The family felt they had no choice but to pay the extraordinary cost. But Kristina assured them she would do everything she could to help.
“They said, ‘maybe we’ll just have to pay’, and I said ‘no, let’s try another way’.”
Kristina worked with Brindha and the neurosurgical registrar, Kaishin Tanaka, to escalate Mark’s case through the Queensland Ambulance Service (QAS) for special consideration.
“It was such an emotional and stressful time for the family,” said Kristina. “I was speaking to QAS on the phone and saying, ‘If there’s any way I can get an idea so that there’s light at the end of the tunnel …’.”
The team put Mark’s case in writing, and it was escalated to the QAS commissioner. It was approved.
“His son was in tears,” said Kristina. “They were so thankful to this place. In the end they didn’t pay anything.”
“Healthcare is so complex to navigate but it was so nice to see other organisations working with us to achieve that patient-centred goal.”
* Name changed to protect patient privacy
This isCompassionate,
Uncompromising Care
We strive to deliver compassionate, uncompromising and dignity-conserving care. This is done not only
through clinical practice, but through our attitudes, behaviour and dialogue with patients, families, carers
and fellow healthcare professionals.
SERVICE HIGHLIGHTS
Nursing
• Consistent positive feedback from Patient Experience Program with an average Net Promoter Scores (NPS) of 90 (see p 13).
• New specialist nurse positions created in lung cancer and pain management. The positions are funded through philanthropic support.
• With 60% of respondents to a staff survey being under 35 years old, our nursing team is particularly career and development orientated. See education and training initiatives in full update.
Full update p 56

28
The love story of Maria Calibag and Julian Orjuela began in the kitchen of an upmarket Rose Bay restaurant, where Julian was a pastry chef and Maria a trainee. Neither of them had family in Sydney with hers being primarily in the Philippines and his in Colombia.
They married and she fell pregnant. Sometime during her pregnancy, she began suffering acute stomach pains.
“It was really painful like I wanted to die – it was too much pain,” she told Jo Wallace for the Instagram account @HumansofNewtown.
Maria was diagnosed with stage 4 colorectal cancer. She was 29 years old and 32 weeks pregnant.
Two days later, in mid-September, a team of medical specialists
across maternal and foetal health at RPAH and oncology at Chris O’Brien Lifehouse made urgent arrangements for Maria to deliver her child.
Her baby was born at RPA Women and Babies. She was a girl. Maria and Julian named her Maria Natalia, to be known as Natalia.
More than eight weeks premature, Natalia stayed in the care of the RPA Neonatal Intensive Care Nursery.
Meanwhile, the new mother came into the immediate care of Chris O’Brien Lifehouse across the road, to start palliative chemotherapy and radiation treatment.
Chris O’Brien Lifehouse and Royal Prince Alfred Hospital are connected in many ways. One physical manifestation of this is a
Royal Prince Alfred Hospital and Chris O’Brien Lifehouse journey together, responsively and
compassionately, with patients and their families. Collaboration lies at the heart of this life-enhancing
partnership between these two institutions.
This isCollaborative
Care
tunnel that runs under Missenden Road, joining the two institutions together.
When Julian was at the hospital, he and Maria walked through this tunnel to visit their baby. RPA’s neonatal care team liaised with Maria’s Lifehouse care team to arrange visits around her treatment.
One day, Maria was getting ready to visit Natalia and bathe her for the first time. St Andrews College Choir, a choral group at the University of Sydney which regularly sings to patients and families, was at Lifehouse that day. They sang to Maria and Julian as they left.
Isn’t she lovely?Isn’t she wonderful?Isn’t she precious?Less than one minute old.

29
“I just want my baby to grow strong. You know, like a really
tough girl.”

30
Under the care of RPA’s neonatal unit, Natalia gained strength and was discharged — not to her home, but to Lifehouse. The cancer centre was the baby’s first home environment.
Staff from across Lifehouse rushed to create a baby’s nursery on the ward. The director of medical oncology gathered clothes and a bouncer. ICU nurses brought in more clothes and practical items. The RPA team that had cared for Natalia collected money to buy a bassinet. It was delivered to Lifehouse where the facilities team pieced it together. Head and neck surgeon A/Prof Michael Elliott dragged in bags of sheets, towels and clothes, which his wife Angela, a volunteer, had collected from staff and friends and washed at home. Prof Diana Horvath AO, a member of the board of directors of Chris O’Brien Lifehouse, later came in each day to help bathe Natalia.
The day Natalia arrived, Maria held her daughter in her arms as Julian stood by them. She lowered herself into a chair by the window and sang to her baby.
The sun’ll come out, tomorrowBet your bottom dollar, That tomorrowThere’ll be sun.
Julian often slept in the hospital with his wife and daughter. Maria’s aunties regularly flew in from the Philippines and USA and gathered in the family’s makeshift home on the ward.
Natalia was baptised by Fr Joseph, a regular pastoral visitor at Lifehouse and RPA, at St. Joseph’s Camperdown. Gail O’Brien and Lorainne Brecard, the volunteers manager, became Natalia’s godmothers.
Maria and Natalia were briefly discharged. Not long afterwards Maria was readmitted.
She died on February 2, 2019.
Paul Lahood, a funeral director and Chris O’Brien Lifehouse supporter, undertook the repatriation of Maria’s body back to the Philippines, with Paul Lahood Jnr personally overseeing her journey.
Staff from across both hospitals came together for a memorial service to celebrate Maria’s life. The St Andrews College Choir sang again.
I am waiting for youFor only to adore youMy heart is for youMy love, My love, My love
This is my grief for you For only the loss of you The hurting of you My love, My love, My love

31
Jude Butcher describes his experience at Chris O’Brien Lifehouse and Concord
Hospital as ‘collaborative healing’.
Jude Butcher was treated for Non-Hodgkin’s Lymphoma by A/Prof Chris Milross at Chris O’Brien Lifehouse and Dr Emma Verner at Concord Hospital.
Prof Br Jude Butcher cfc AM deeply appreciates the collaborative care and treatment he experienced, saying, “When I meet with Chris, or when I meet with Emma, I know that I am meeting with both of them ... I’m meeting the two of them together. They bring their different lenses and capacities together into a new whole.
“The beauty of this is that it does create a new whole.” Jude said Chris and Emma’s regular joint meetings about his health show a shared and deep commitment to the ‘collaborative healing’ of his cancer and enhancing his health and wellbeing.
Reflecting upon the collaborative healing he experienced, Jude emphasised that it incorporates a genuine and deep collaboration:
‘The focus and commitment of collaborative healing are holistic (mind, body and spirit) and promote and build upon life and hope.
Collaborative healing incorporates a genuine and deep collaboration between the patient and the doctors, health units and hospitals involved.
This collaboration is life-focussed, hope-inspired and characterised by a deep mutuality and inherent reciprocity between all involved.
Collaborative healing provides a sound holistic basis for health professionals to speak with one voice which is welcomed by the patients and evidenced in their confidence in, and focus upon, life and hope.’
Prof Br Jude Butcher was a member of staff of the Australian Catholic University and its predecessor college for 44 years, during which time he held leadership roles in education and community engagement.
SERVICE HIGHLIGHTS
Radiation Oncology
• One of the busiest private radiation therapy practices in NSW, treating more than 1,800 patients in 2018.
• The second Varian TrueBeam Linear Accelerator was installed in early 2019, with state-of-the-art 6-degree of freedom couch. This is the most up-to-date X-ray imaging for patient setup and new high-dose rate X-ray beams. The technology allows for greater precision and shorter treatment times.
• VectorLAB acquired a customised 3D printer from the start-up company AON3D in Montreal.
• See MDT and patient-centred iniatives in full update.
Full update p 54
SERVICE HIGHLIGHTS
Colorectal
• Growth in volume of colorectal procedures, including more radical resections and robotic surgery.
• Increased integration with specialty clinics like Post-Cancer Sexual Intimacy For Women run by the Gynaecological Oncology Group.
• Development of bowel screening program via the Rapid Access Endoscopy Clinic.
Full update p 64

32
IN FOCUS > COLLABORATIVE CARE
Comprehensive Sarcoma CentreChris O’Brien Lifehouse is the state-wide referral centre for sarcoma. This is a joint campus initiative with Royal Prince Alfred Hospital (the surgical centre) and the University of Sydney.
Chris O’Brien Lifehouse is an accredited, specialist centre for the treatment and care of people with sarcoma, a group of rare cancers that develop in bone and connective tissue. We see 90% of all bone sarcoma patients in the state, and the majority of soft tissue sarcomas.
We have established an exceptional multidisciplinary team of surgeons, specialists, nurses and allied health professionals dedicated to the care and support of people with sarcoma, the majority of whom are adolescents and young adults.
This concentration of expertise, experience, knowledge and compassion provides the best possible environment for people with sarcoma, the very best treatment and the best chance of a good outcome.
The Comprehensive Sarcoma Centre is also a focal point of learning and discovery, with dedicated researchers and the largest clinical trials program for sarcoma in the state, with 11 trials currently open to patients. This active research program is
FACTS ABOUT SARCOMA• There are 2 main types of sarcoma: bone sarcomas and sarcomas
that develop in connective tissue such as muscle, fat, tendons and cartilage.
• There are more than 50 distinct types of sarcoma and many more sub-types. Each develops differently and responds differently to treatment.
• Sarcomas comprise 1% of all cancers, but up to 10% of cancers in young adults and up to 20% of cancers in children.
• 2 in 5 people with sarcoma will die from their disease.
also evaluating areas of acute impact to patients, such as the benefits of advanced pelvic reconstruction techniques.
Our sarcoma services are funded by philanthropy. With the growth of these services and the strides we are taking towards better prognoses for people with sarcoma, we have been able to leverage the support of our donors to secure two significant partnerships.
In July 2019, the Federal Government announced a $6 million grant to establish a sarcoma surgical research centre at Chris O’Brien Lifehouse. This state-of-the-art facility will harness recent advances in technology, such as customised 3D printed bone prostheses and precision haptic robotic surgery, that have the potential to radically alter the lives of people with sarcoma.
In late 2019, the Sony Foundation announced their commitment to build a You Can Centre at Chris O’Brien Lifehouse. This purpose-built space, built in partnership with Sydney Local Health District, will address the unique needs of adolescents and young adults with cancer and their families. More details will be included in the next annual report.
Dr Vivek BhadriPaediatric and adolescent
medical oncologist, COBLH
A/Prof Paul Stalley AM Orthopaedic surgeon,
RPAH
SOME OF OUR SARCOMA CENTRE LEADERS
A/Prof Peter Grimison Medical oncologist, COBLH

33
“Collaboration remains the cornerstone of Chris O’Brien Lifehouse research. Our researchers have many roles, often numerous affiliations and do their research as part of networks.” — Professor Lisa Horvath, Director of Research
Chris O’Brien Lifehouse is one of the largest cancer clinical trials units in NSW. Full details of our research program can be found in the current research report, covering years 2017 and 2018 at mylifehouse.org.au.
Burn on discovery
Immunotherapy in metastatic lung cancer
Extracorporeal radiotherapy for sarcomas
Improved patient decision-making in cancer therapy
Preoperative nutritional support and exercise program Techniques to address fear of cancer recurrence
Our researchers have been part of a wide range of practice-changing studies —
SERVICE HIGHLIGHTS
Medical Oncology
• Dr Kate Mahon was appointed Deputy Director of Medical Oncology.
• A/Prof Peter Grimison was appointed Director of Physician Training.
• The Medical Oncology Fellowship program is expanding with a new sarcoma fellowship to commence in 2020.
• The Medical Oncology department has excelled in research over this period. The current research report (2017 & 2018) lists more than 160 publications across a wide range of research areas including clinical trials, biomarkers, cancer biology, health economics and quality of life.
Full update p 52
SERVICE HIGHLIGHTS
Neuro-oncology
• Increased surgical activity and expansion of services as the neurosurgical service enters 2nd and 3rd years of service.
• Launched as a collection site for the Sydney Brain Tumour Bank, in partnership with Brainstorm Brain Cancer Research at the Brain and Mind Centre, Sydney University and RPA Neuropathology Department.
• Research program launched, with development of GlioNET, a prospective bio/database in collaboration with RPA and USyd. See full update for details.
Full update p 61
Research snapshot

34
At any one time, there are more than 100 clinical trials being undertaken by or in collaboration with our researchers and clinicians.Not only does this mean patients have more access to the latest therapies, it helps move us toward answers for treating the patients of tomorrow.
This isResearch-
DrivenCare

35
When George Reed was diagnosed with stage four prostate cancer he was given ‘months to live’. He sought a second opinion from Prof Lisa Horvath, Director of Medical Oncology and Research.
“She told me, ‘You’re only early stage four. I think I can give you some more time.’ Just those words meant everything to me. They meant hope.”
George was administered a chemotherapy drug called Docetaxel, which is the subject of a collaborative study led by Prof Horvath and medical oncologist Dr Kate Mahon.
The research has confirmed that a blood marker, mGTSP1, can predict outcomes after Docetaxel in men with metastatic castrate resistant prostate cancer.
This research may accelerate future clinical trials of new therapies and be useful in the clinic to guide treatment decisions. The academic paper reporting these findings was the subject of an editorial in the journal European Urology.
George said he experiences fatigue and pain as side-effects of the treatment. “But I am incredibly thankful for the precious extra time I have been given to spend with my wife and family.”
SERVICE HIGHLIGHTS
Uro-oncology
• Expansion of services and department.
• Coming from a base of zero in 2015, we are now the highest volume centre in the country for robotic retroperitoneal lymph node dissection for advanced testicular cancer (using the da Vinci XI). Based on medical literature, Chris O’Brien Lifehouse is the fourth largest centre in the world for this procedure.
• Performed the first case in NSW of robotic inguinal lymph node dissection for treatment of penile cancer, integrating a multidisciplinary collaboration with breast cancer surgical colleagues (using SPY technology which tests vascular activity to assess risk of necrosis).
• Research program launched.
Full update p 62

36
IN FOCUS > RESEARCH-DRIVEN CARE
PharmacyWe have our own clean room onsite where chemotherapy, immunotherapy and clinical trial drugs are compounded and distributed. It is not common for a hospital to have its own clean room, but this area has improved responsiveness to patients, as well as financial outcomes.
More than 20 pharmacists and technicians work in the pharmacy and clean room to prepare and dispense medications daily. It is currently participating in approx. 95 clinical trials with more on the horizon.
In the past year, an external audit by Slade Pharmacy benchmarked us against their hospital pharmacies across the country. It showed we are above average in manufacturing services and on par with their national benchmarks in pharmacy management practices.
The unit is currently implementing ‘i-pharmacy’, a dispensing software used by all NSW public hospitals and private hospital pharmacy groups. This aims to simplify the process of dispensing medications and enhance safety features.
We marked World Pharmacist Day 2019 with ‘Behind the Scenes’, a demonstration in the Day Therapy waiting area on how chemotherapy is compounded, and conducted tours for staff and patients through the pharmacy demonstrating dispensary, clinical trials and clean room operations.
As pharmacy has grown, we are sharpening our focus on innovation and driving growth in ways that are not contingent on an increasing workforce.
Pharmacy continues to supervise students from the University of Sydney and UTS. These arrangements have developed into a strong partnership where students work on solutions-based projects related to defined problems in pharmacy. We look forward to sharing the outcomes in the future.
The Future
Biosimilars are generic equivalents of immunotherapy medications. The public is familiar with generic medicines in a pharmaceutical context, but generics in oncology are new in Australia. Biosimilars present large potential benefits and savings for Chris O’Brien Lifehouse and the Pharmaceutical Benefits Scheme.
In late 2019, we started to use our first biosimilar. This has involved educating patients, haematologists and the hospital executive about biosimilars.
We have worked with students from the University of Sydney on their capstone projects to create education packages for patients about biosimilars and why we are adopting them.

37

38

39
This isPatient- Centred
CareA patient-centred approach has
been our vision from the beginning. We put the patient and family at the heart of everything we do.
SERVICE HIGHLIGHTS
Gynae-oncology
• Dr Rhonda Farrell appointed as Deputy Director and commenced formal duties in early 2019. This role is philanthropically funded.
• The department saw continued development and expansion with increased patient volume across both inpatients and outpatients.
• Data from Cancer Institute NSW showed one of the highest number of ovarian cancer resections in the state and among the best surgical outcomes.
• Robotic surgery continues to give uterine and endometrial patients the best chance of recovery in the shortest period of time.
Full update p 60
SERVICE HIGHLIGHTS
Partnership Advisory Council (PAC)
• The PAC grew in the relevant period, adding three new members and electing a co-chair.
• Increased activity during the accreditation process as the PAC participated in surveyors’ meetings and formed documentation that demonstrated the significant consumer engagement embedded at Chris O’Brien Lifehouse.
• Led the gym garden development including concept, landscape design and installation.
Full update p 70

40
In 2018, Australian media briefly turned its eye to two babies, Vander Clark and Baxter Browne, and the remarkable circumstances around their births.
Their mothers, Jenna-Lea Clark and Kirsty Browne, had both been treated for cervical cancer. Instead of undergoing hysterectomies (the usual approach which involves removing the cervix and uterus), Jenna-Lea and Kirsty both opted for trachelectomies.
A trachelectomy involves the removal of the cervix and lymph nodes, but the body of the uterus is
retained and attached to the top of the vagina.
“This gives women at least the opportunity to carry a child,” said Dr Trevor Tejada-Berges, gynaecologic oncologist and Kirsty’s surgeon.
“Over the last 10 to 20 years, there have been increasing numbers of women who have had a trachelectomy,” Trevor said.
“It carries surgical risks. It carries the possibility of pain, discomfort from the surgery, irregular bleeding … There is still a concern of prematurity in pregnancy. There is a high risk of miscarrying. So a lot of women still don’t pursue it.”
“But even being able to provide that option, where the doors have not completely shut, goes a long way towards making women feel comfortable.”
Throughout Kirsty’s pregnancy following her surgery, Trevor worked with RPA’s foetal medicine team to monitor her progress.
“It was such a unique situation,” he said. “It involved referring Kirsty
Kirsty Browne was supported by an open and collaborative relationship with her surgeon, Dr Trevor Tejada-Berges, throughout exceptionally unique circumstances.
to them early on, when she was thinking of becoming pregnant. There was prenatal consultation. They would call me and discuss the case.”
“We would have conversations about how things are going, what to do. When there were any complications, we would ask if they were related to the surgery.”
“I think there can be a tendency to silo care ... This was a good collaboration.”
“Kirsty was also a part of that. She was very proactive, emailing with any questions she had.”
Trevor stayed involved throughout the pregnancy, even to the point of being present in the delivery room.
“As a gynae-oncologist, so much of what we do is destructive. It’s about taking out a uterus that has cancer, or removing the ovaries if there’s a risk of cancer,” he said. “To actually do something that is both curative and offers a level of restoration of normalcy was really nice for us.”

41
IN FOCUS > PATIENT-CENTRED CARE
Clinics to enhance regional, rapid and specialty careClinics are the key touchpoint between clinicians and patients. Our program of clinics has expanded to offer enhanced care to patients.
REGIONAL CLINICSWith increasing numbers of referrals from outside the metropolitan centre, we are focused on working with local communities to form stronger ties between GPs, specialists and the infrastructure that Chris O’Brien Lifehouse offers.
This has led to us forming satellite clinics in regional areas, with more planned for the future.
SPECIALTY CLINICSPatients with complex cancers have unique needs. The development of walk-in clinics for singular issues allows a unique level of specialty care.
• The Sydney Facial Nerve Clinic — the first specialist multidisciplinary clinic for patients with malignant facial nerve disorders in Australia
• Speech and Swallow clinic — multidisciplinary management of common side-effects of mouth and throat cancer treatment
• Facial Prosthetic Reconstruction Clinic — arranges initial prosthetic assessment and prosthesis
• Post Cancer Sexual Intimacy Clinic For Women — addresses the many unexpected effects gynaecological cancers can have on relationships
TamworthHead and neck
Upper GI Port MacquarieHead and neck
Breast
OrangeHead and neck
Wagga WaggaUpper GI
Uro-oncology Canberra
Gynae-oncology
Nowra Head and neck
Sydney
Coffs HarbourUpper GI
“If people can receive a diagnosis and follow-up treatment in Port Macquarie and not have to travel to the city, I really feel like half their battle has been won.” - Elaine Madden, head and neck patient (Focus Port Macquarie magazine)

42
SYMPTOM MANAGEMENTGoal — give patients with concerns or complications a same-day, walk-in service that reduces hospital admissions and emergency presentations.
Palliative Radiotherapy Rapid Access Clinic
November, 2018: radiation oncologists Dr Georgia Harris and Dr Ee Siang Choong established the Palliative Radiotherapy Rapid Access Clinic to provide faster access to radiotherapy and streamlined treatment pathways for patients who have incurable cancer and high symptom burdens.
For these patients, palliative radiotherapy has been demonstrated to improve symptom control and quality of life. Often this can be given very effectively in a single fraction, which is much more convenient for patients and their families.
How it works: a walk-in clinic appointment with the radiation oncologist, followed immediately by a radiotherapy planning session and usually treatment delivery on the same day (provided this suits the patient).
This aims to improve the current
DIAGNOSISGoal — minimise harmful delays, waiting times and test-related anxiety.
After-hours hotlines exist across all major specialities. These hotlines give GPs direct access to clinicians.
We aim to contact every patient within 24 hours and assess them within one week of referral.
Regularly scheduled Rapid Access Clinics exist in several specialties:
• Endoscopy — streamlined screening and cancer exclusion service (gastroscopy and colonoscopy).
• Hysteroscopy — patients can be referred for a single visit assessment which includes consultation, biopsy and hysteroscopy at the same visit. This is the first such service in New South Wales.
• Prostate Cancer Screening• Head and Neck cancer
diagnosis• Neurosurgery
service model for patients needing palliative radiotherapy, as well as facilitate referral pathways to community palliative care and other supportive services, promote multidisciplinary management in the palliation of cancer symptoms and research in this area of cancer care.
A 12-month audit showed 65% of patients received same day radiotherapy and 50% of patients received single fraction of radiotherapy.
Future: the team is focussed on opening up the clinic to external referrals from community palliative care and GPs over the next six months.
Rapid Access Assessment Head and Neck Clinic
July, 2018: nurse practitioners Sarah Davies and Justine Oates established the Rapid Access Assessment Head and Neck Clinic, for head and neck patients with questions or concerns. Issues raised have included bleeding wounds, airway obstructions, pain management, and infections.
“The service has streamlined the process for our patients.” said NP Justine Oates.
RAPID ACCESS CLINICS
“The Rapid Access Head and Neck Clinic helps patients avoid being admitted to hospital. It not only saves them distress and time, but it eases the burden on emergency departments and wards.”— Nurse Practitioner Justine Oates

43
The story of Denise’s father* shows that patient-centred care means genuine listening and responsiveness to an individual’s needs. Sometimes, this looks different from what we might expect.
Denise describes her father as “fastidious” and “not a man easily pleased”.
He was treated for inoperable metastatic oral cancer, with a combination of radiation therapy and an immunotherapy medication.
After five treatments, tests showed it was having minimal to no effect on the cancer, but was affecting his liver function.
Denise’s father decided he did not want to continue treatment, nor return to hospital.
“Dad had his own ideas,” she said. “He would make up his own mind.”
“Professor Boyer was great in the sense that he said ‘it’s your dad’s choice. It’s his call. He can decide what he wants to do.’
“He spoke on the phone to Dad and explained what would happen if Dad did come back and what would happen if he didn’t. Dad listened. And said ‘OK, I don’t want to come back.’
“He was in a lot of pain and was seeing a pain management specialist. But he was never able to get the pain under control. He said,
‘I’ve got no quality of life.’”
Over the next three or four weeks, Denise’s father became sleepier, and more confused.
He wanted to die at home.
“On the day he died, he collapsed and my daughter found him at home,” she said. “He was lying on the floor. We called the ambulance and brought him upstairs.
“He mustered every little ounce of strength to say, ‘no more’.
“I said, ‘Dad, you understand it’s not too late to go to hospital and get this addressed?”
“He said, ‘Let’s not go over it.’”
He died July 28, 2019, at 87 years old.
“In the end, it was a really good passing. He was in his room. His family was around. It was on his terms. He didn’t seem to be in pain. It was a peaceful, good way to go.
“That was pleasing for me. I knew that’s what he wanted.
“We were prepared. We had a direction for the paramedics to say he didn’t want to be taken to hospital. We’d had these
conversations in advance. So we knew what Dad wanted.
“Professor Boyer filled in many gaps, just off-the-cuff. He was always contactable to give advice.”
After this experience, Denise’s daughter, a medical student, said she wanted to specialise in oncology. “They’re just special people, Mum,” she said.
A/Prof Chris Milross, who managed the radiation treatment, said, “he had wonderful kids in the sense of being supportive of him and respectful of his decision-making.
“They understood him. And they strongly protected his right to self-determination.
“In all the discussions, we gave him all the options. And he chose what he chose.”
* Name not printed to protectpatient privacy.
“lt’s an example of how the right care is that care which the
informed patient will accept. And we have to accept that.”
— A/Prof Chris Milross

44
It’s all about caring for the whole person and not just treating the disease.
This is
Holistic Care
Margie Moore AM was diagnosed with HER2+ breast cancer — a type of cancer that tests positive to a protein that boosts cancer cell growth, and therefore is often more aggressive.
Margie has undergone two surgeries, chemotherapy, radiotherapy and immunotherapy.
Throughout her treatment, she has made frequent use of the LivingRoom, accessing therapies that help alleviate side-effects like nausea, fatigue and anxiety.
“Every person treating me has been meaningful and they’ve all added wellbeing to my journey,” said Margie.
“The treatment unfortunately makes you feel pretty rotten. But the LivingRoom gives a balance.
“I’ve found acupuncture
“This end of the medical spectrum is about wellbeing and support.” — Dr Paul Hutchins AM

45
particularly useful because I’ve had neuropathy in my fingers and toes. Lymphoedema massage has been most helpful and Jessica has been training Paul to continue it daily for me at home. Mindfulness and counselling have been amazing. It all helps to keep you going.” Jessica Kyneur is a physiotherapist who specialises in lymphoedema massage.
“They give you signposts for how to move through your journey and that’s so valuable. The cancer experience is something completely new and you know it’s not going to be all that good, and you don’t know how to prepare for each new step and symptom.
“Just having someone who cares about you tell you something, like ‘oh you’re doing radiotherapy next, make sure to moisturise your skin’, is just so meaningful and helpful.
There is a sense of ongoing care as well as working with you on a specific treatment basis.”
Margie’s husband, Dr Paul Hutchins AM, a retired developmental paediatrician, said “the human body, brain and soul is so complex that many different systems of understanding, treatment and support can be effective.”
“I am so impressed by how the whole LivingRoom team, both clinical and administrative, works together to tailor support to the individual and their partners, and to evaluate the impact of this support.
“This end of the medical spectrum is about wellbeing and support.
“It’s about keeping you going from the beginning through to the future as patient and partner, however much or little you can manage to do.”
SERVICE HIGHLIGHTS
Supportive Care and Integrative Oncology
• Currently approx. 10% -15% of Chris O’Brien Lifehouse patients come through the LivingRoom as outpatients for supportive care or complementary medicine.
• Approx. 55 patients are treated each month under equity of access funds which are philanthropically funded.
• Recognised by peers as one of the most comprehensive integrative oncology services in Australia.
• Philanthropic funding has enabled part-time research fellow position and day therapy intervention program and research.
Full update p 65
“Integrative oncology uses evidence-based interventions to keep
people living well from the time of diagnosis of
cancer and beyond.”— A/Prof Judith Lacey

46
“I’ve learnt that holistic medicine is about treating a human, rather than a machine. Treating a machine says ‘here’s the broken part, let’s fix that.’ Holistic medicine treats all the human bits.”— Jack Thomas, senior music therapist

47
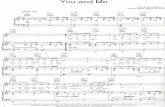
IN FOCUS > HOLISTIC CARE
How music therapy worksThe Music in Health program is entirely philanthropically funded. Music therapy offers choice and control, in a situation where much of it has been removed. It disturbs the routine of sitting, waiting, thinking and getting treatment with moments of deep engagement and generous encouragement.
Music therapy aims to improve quality of life by reducing stress and anxiety, providing peace and comfort, and boosting confidence and self-esteem.
The sessions use therapeutic live music, guided songwriting techniques, improvisation, music skill building, and music and relaxation.
The Guided Original Lyrics and Music (GOLM) therapeutic songwriting method, developed by Music Therapy Fellow Dr Emma O’Brien OAM, guides patients through the creative process of writing a song.
Using their own lyrics and ideas is the most important part.
Sessions begin with an open conversation and move toward lyric composition.
About 500 songs have been written with this method between primarily Royal Melbourne Hospital and Chris O’Brien Lifehouse.
Rapunzel (pictured) is an English teacher, so writing lyrics came naturally to her. “We began with a normal conversation,” said music therapist Jack Thomas. “She was talking about her body: her fingertips, the colour of her fingernails changing, hair falling out, feeling frail.”
“But she wanted it to be relatable for anyone. So the metaphor idea came up. Her body became a house, feeling the strain of two unwelcome tenants — cancer and chemotherapy. She also decided to make the owner of the house a man, so it created a disconnection from her.”
“The looks on people’s faces, when their words turn into a song, when they hear it back for the first time, that’s an incredible moment.”
“A song allows people to say things they don’t know how to say, in a really safe, supportive environment. Then they can share it.”
“It creates the opportunity for achievement, which plays a big role in wellbeing, even if that is to learn a chord on the guitar or ukelele.
“And, it creates something real that will last, a legacy.
Watch our music therapists perform Rapunzel’s song, ‘Home’
URL: vimeo.com/378187203 Password: stoodstrong
SERVICE HIGHLIGHTS
Music in Health
• Expansion of team with appointment of two more part-time therapists (Total 1.8 FTE).
• Overall increase in services including more referrals, more occasions of service, higher choir numbers.
• 2x increase in number of inpatients seen by music therapists in 2019 (compared with 2018).
• Strong focus on building the program for adolescent and young adult sarcoma patients.
• A new Sony Foundation You Can Centre at Lifehouse for adolescents and young adults with cancer will include a dedicated music room and recording studio.
Full update p 68

48
Chris O’Brien Lifehouse volunteers are the lifeblood of a community that runs deep. Here is one example.
Each day, the Chris O’Brien Lifehouse patient car collects patients from across the inner west, brings them to their appointments at the hospital then drops them home again.
One of these people was Helen, who had glioblastoma multiforme, a type of brain cancer.
Janice is a Chris O’Brien Lifehouse volunteer. She drives the patient car at least once a week.
Janice and Helen came to know each other through these trips. The two of them chatted, and Helen often spoke about her daughter, Sonja.
Sonja was living in Melbourne and grappling with her own cancer diagnosis. When she relocated back to Sydney, she was also treated at Lifehouse and subscribed to the patient transport service.
One day, Sonja was staying at Lifehouse as an inpatient when she received the news her mother was going to
pass away imminently.
Helen’s treatment had moved into a palliative stage and she was at that time living in an aged care facility in Rockdale.
The ward made arrangements for Sonja to be discharged for the day so she could see her mother. The volunteer manager, Lorainne Brecard, arranged for the patient car to make this special trip.
In a moving example of the richness of the Lifehouse community, and its capacity to support patients in the physical sense but also at a more profound level, the driver that day was Janice. As they drove to Rockdale together, Sonja was able to talk with someone who knew her mother.
Janice helped Sonja out of the car and walked with her to Helen’s room. She waited outside as Sonja said goodbye to her mother, then brought her back to the care of the ward staff.
SERVICE HIGHLIGHTS
Volunteers
• Approx. 67 volunteers (including Arterie) currently active.
• Approx. 55 volunteers working each week (average).
• Each day, the patient car picks up approx. seven patients from their homes (mainly in the inner west), drives them to appointments and back home.
• Each day, the shuttle bus runs seven trips between Central Station and Chris O’Brien Lifehouse.
• We have seen an increase in volunteers with a volunteer recruitment process underway.
• New corporate support program launched.
Full update p 71
This isA CaringCommunity

“I call this my safety zone. My home. My safe place … The ladies in craft have been just beautiful. They’ve been my little soul mates.”
“We never could have anticipated the love, understanding and nurturing with which we were surrounded from these beautiful souls. The support from you, the volunteers, allowed us to breathe.”
“Sometimes, I just sit here in Lifehouse, because I like to be here ... It’s a place of getting better and healing ... It’s the people here. Everyone has genuinely cared.”
— Lois Byrne, patient
— Kim Sue, patient
— Family member who wishes to remain anonymous

50

51
Updates

52
LEADERSHIP
• Prof Lisa Horvath - Director
SNAPSHOT
• One of the busiest day therapy, medical oncology, chemotherapy and intravenous cancer treatment facilities in NSW.
UPDATES
• Dr Kate Mahon was appointed Deputy Director of Medical Oncology.
• A/Prof Peter Grimison was appointed Director of Physician Training.
• The medical oncology fellowship program is expanding with a new sarcoma fellowship to commence in 2020.
RESEARCH HIGHLIGHTS
• The Medical Oncology department has excelled in research over this period. The current research report (2017 & 2018) lists more than 160 publications across a wide range of research areas including clinical trials, biomarkers, cancer biology, health economics and quality
of life. Patients were recruited to more than 100 clinical trials (Phase I-III trials).
• Dr Kate Mahon was awarded the ANZUP Poster Prize for her work on blood markers and their potential to guide treatment of prostate cancer. Dr Mahon led a study in which it was confirmed that a blood marker, mGTSP1, predicts outcomes after docetaxel chemotherapy in men with metastatic castrate resistant prostate cancer. This paper was the subject of an editorial in the journal European Urology.
• Prof Lisa Horvath, Prof Martin Stockler and Dr Alison Zhang presented the results of a ground-breaking Phase III clinical trial that discovered Enzalutamide can prevent cancer cells from using testosterone to grow in patients with metastatic prostate cancer. Adding Enzalutamide to current treatments (eg. testosterone suppressing therapy) has the capacity to slow cancer growth and increase overall survival of patients by 33%. The results were published in the New England Journal of Medicine and presented at American Society of Clinical Oncology plenary session.
• Prof Michael Boyer AM was a co-author in a global study that identified the immunotherapy, Pembrolizumab, added to chemotherapy, improves survival in patients with newly diagnosed non-small cell lung cancer. (Published in New England Journal of Medicine). This study has resulted in immunotherapy
with chemotherapy as a new standard of care for lung cancer.
• For further details about the medical oncology research program, see the Chris O’Brien Lifehouse Research Report 2017/2018 at mylifehouse.org.au.
EDUCATION SNAPSHOT
• 3 x clinical / research fellows.
• 3 x advanced trainees in medical oncology.
• 2 x Resident Medical Officers.
• 2 x Basic physician trainees.
• The RMOs and physician trainees rotate from RPAH, exposing junior doctors to medical oncology ahead of choosing their specialties.
• 3 x PhD candidates.
• Medical students from the University of Sydney oncology bloc are taught and supervised for five weeks, co-ordinated by Prof Martin Stockler.
EDUCATION HIGHLIGHTS
Fellowships: The medical oncology department currently has 3 active clinical / research fellows:
• Phase 1 clinical trials fellow.
• Lung cancer fellow.
• Rural Specialist Training Program (in conjunction with Dubbo Base Hospital).
• With the appointment of A/Prof Peter Grimison to Director of Physician Training, there is now a stronger focus on expanding the fellowship program. This includes training fellows to be
Service Update
MedicalOncologyMedical Oncology

53
Service Update
Nursing
experts in cancer research and expanding Lifehouse’s capacity to do research.
• 2020 will see the inauguration of the Sarcoma Research Fellow, a new position that will strengthen multidisciplinary sarcoma research.
• The Rural Specialist Training Program, which allows a trainee to be placed at Chris O’Brien Lifehouse 3 days / week and Dubbo Base Hospital 2 days / week, is continuing and developing. This program enhances training for a doctor who wants to work long-term
in regional or rural NSW, and ensures that Lifehouse strengthens affiliations with these areas.
FUTURE
• Building the research program further by developing integrative research programs between medical oncology and surgical units.
• Managing a growing workforce - especially among VMOs - with a focus on ensuring all medical oncologists are well-integrated, included and contributing to the hospital.
• In collaboration with the well-established peritonectomy program at RPAH, Dr Kate Mahon will lead efforts to drive service and research in the use of heated chemotherapy for patients with bowel or appendix cancers following peritonectomy. This field currently suffers from a significant gap in knowledge. Dr Mahon’s work will include the supervision of a PhD candidate.

54
LEADERSHIP
• A/Prof Chris Milross - Director (pictured)
• Kristin Carney - General Manager of Ambulatory Care and Support Services
• Dr Robin Hill - Director of Radiation Oncology Medical Physics
• Ms Joanne Page - Director of Radiation Therapy
• Mel Grand - Radiation Oncology Clinical Trials Manager
• A/Prof Natalka Suchowerska - Director of VectorLAB
• Linda Rogers - Radiobiology Laboratory Manager
SNAPSHOT
• 5 Linear Accelerators - 2 Varian TrueBeam Linear Accelerators.
• Specialist radiation treatments include: - total body irradiation - HDR brachytherapy for gynaecological cancers - superficial x-rays for skin cancers - treatments for mesothelioma patients.
HIGHLIGHTS
• Chris O’Brien Lifehouse is one of the busiest private radiation therapy practices in NSW, treating more than 1,800 patients in 2018.
• The second Varian TrueBeam Linear Accelerator was installed in early 2019, with state-of-the-art 6 degree of freedom couch. This is the most up-to-date X-ray imaging for patient setup and new high-dose rate X-ray beams. The technology allows for greater precision and shorter treatment times.
• A total body irradiation treatment couch, designed by our medical physics team and RPAH BME staff won an award at the NSW BME meeting for quality.
• The number of patients in clinical trials increased for a number of different cancer sites (for details about the radiation oncology research program, see the Chris O’Brien Lifehouse Research Report 2017/2018 at mylifehouse.org.au > about publications).
• Multidisciplinary care: The Stereotactic Radiosurgery (SRS) program continued to grow and is the busiest in the state. This program relies on teamwork between radiation oncology and neurosurgical staff. The latest iteration — BrainLab Elements — was implemented for the treatment of brain metastases and other benign cranial tumours. Planning time for patients was reduced in many instances by 50% and treatment times reduced considerably. We are now able to treat all cerebral metastases with one treatment when patients previously had to return and have each metastasis planned and treated separately.
PATIENT-CENTRED INITIATIVES
• A RAPID access clinic for palliative patients commenced involving simulation and treatment, allowing patients to be seen, planned and treated in the same day.
• A ‘Who’s Who’ team member identification board on each treatment machine allows patients to know the radiotherapists who are giving their treatment that day.
• ‘Walk in my shoes’ orientation tours.
• Patient information sessions for radiation therapy treatment presented by the radiation therapists and medical physicists.
PEOPLE
• The department welcomed three new staff specialists: Dr Georgia Harris, Dr Ee Siang Choong and Dr Raymond Wu.
• Mel Grand was recruited to the role of Clinical Trials Manager.
• We recruited our first on-site services engineer for linear accelerator faults.
ACHIEVEMENTS
• Nursing team leader Adama Briffa was awarded a Keith Cox Scholarship to complete her Nurse Practitioner Masters at the University of Sydney.
• Senior Medical Physicist Elizabeth Claridge Mackonis became an official assessor for the ACDS (Australian Clinical Dosimetry Service), enabling her to perform radiotherapy dosimetry audits in Australia and New Zealand.
• Senior medical physicist Dr Johnny Morales was awarded his PhD in medical physics.
Service Update
Radiation Oncology
UPDATE
Radiation Oncology

55
EDUCATION AND TRAINING
• A number of staff (radiation oncologists, medical physicists, radiation therapists) are involved in teaching activities in radiation oncology through the various professional bodies and the University of Sydney.
• Many of the radiation oncology staff continue to be enrolled in postgraduate studies including PhD, Masters degrees and courses.
• A number of radiation oncology registrars recently passed their RANZCZ Part 1 exam.
• The radiation therapist educator provided clinical training to the radiation therapists and supported students to undertake clinical placement at Lifehouse.
• The department hosted a senior Radiation Oncologist from Myanmar as part of an IAEA training fellowship.
ORGANISATIONAL UPDATES
• A 3-5 year strategic plan was developed with outcomes that include: - Radiation Oncology Clinical Governance framework - Patient advocacy involvement - Implementation of private patient practice
• The department went through recertification of the Novalis Circle accreditation program for its SRS service. We were the first department in NSW to be recertified in this international audit.
• Set up a radiotherapy Planning Dashboard to improve planning processes and efficiencies.
• Increased IMRT/VMAT techniques from to 75% allowing more precise treatments to the tumour volumes.
• The use of the RapidPlan software continued to be expanded. This software relies on machine learning to help develop specific treatment templates for planning of a number of radiotherapy techniques. This relies on extensive testing by the radiation therapists and medical physicists. Recent templates developed included a head and neck template with VMAT treatments.
• The department continues to participate in various audits and quality activities. We participate in annual dosimetry audits for all linear accelerators through the Australian Clinical Dosimetry Service. We passed all of these audits in 2018 and 2019.
VECTORLAB
SNAPSHOT
• VectorLab at combines medicine, physics, biology and chemistry in order to solve some of the most urgent problems in cancer. Comprised of a diverse team of specialist scientists and clinicians, VectorLAB aims to translate advances in science and technology to help people with cancer.
• 1.8FTE funded positions.
• Up to 10 scientists collaborate with the lab at any one time.
• Research funding from Prostate Cancer Foundation Australia was used to subsidise the salary of an additional employee to the end of 2018.
HIGHLIGHTS
• In 2018, VectorLAB acquired a customised 3D printer from the start-up company AON3D in Montreal. This is the only printer of this type in this part of the world. It was made
possible through philanthropic support.
• PhD candidate Georgio Katsifis from the School of Physics, University of Sydney, used the printer to build bone scaffolds using a strong polymer fibre Poly-ethyl-ethyl ketone (PEEK). The scaffolds were then treated using a plasma gas method to attract bone growth. He was awarded the Robinson Prize by ACPSEM for the best biomedical engineering project in 2018 for this work. This study will ultimately enable patients who have lost bone to receive a customised scaffold implant to support regrowth of the patients’ own cells.
• In collaboration with UNSW, VectorLAB has worked on developing antimicrobial treatments that aim to reduce risk of infection during surgery and treatment.
• Funds from Tour de Cure were used to create a magnetic nanoparticle treatment that can carry therapeutic molecules into cancer cells. This is part of the exciting and developing field of advanced targeted treatment delivery to cancer cells.
• Spatially and temporally modulated radiation therapies were studied in a collaboration between VectorLAB and the School of Physics and the NMR Facility in the Faculty of Science, University of Sydney.
• The effect of a cone beam CT imaging dose in addition to the therapeutic dose was studied in collaboration with Dr Peter Kench of the Brain and Mind Institute. The work was funded by the Faculty of Health Science and University of Sydney.
• For details about the VectorLAB research program, see the Chris O’Brien Lifehouse Research Report 2017/2018 at mylifehouse.org.au.

56
LEADERSHIP
• Catherine Lambert - Director of Clinical Services
SNAPSHOT
• Nursing team of approx. 310.
• Continued focus on ensuring patients, families and carers experience ‘Lifehouse Care’ as described in our Nursing Mission statement:
We provide excellence in patient-centred care, offering hope, kindness and compassion.
We listen and support your unique care needs, both physical and emotional with respect and dignity.
We are there for you, your family, and carers when you need us.
• Key objectives: continuity of care, consistency and competency of the workforce.
HIGHLIGHTS
• Nurse Practitioner Shannon Philp, Australia’s only gynae-oncology nurse practitioner, became the first nurse to be awarded the Jeannie Ferris Cancer Australia Recognition Award. (Pictured right).
• Specialist Nurse Program: New specialist nurse positions created in lung cancer and pain management. The positions are funded through philanthropic support.
RESEARCH
• A 3-year retrospective review of head and neck surgical flap surgery, led by Nurse Practitioners Justine Oates and Sarah Davies, demonstrated better outcomes for patients at Chris O’Brien Lifehouse when compared internationally. This work included theatre, wards, ICU and Nurse Practitioners and culminated in a presentation at the Cancer Nurses Society of Australia in June, 2019.
• The nursing team worked closely with the consumer advisory group on a pilot study that tested reframed handovers with the team on Ward 8 North. After positive feedback, it will be rolled out to all wards.
EDUCATION
• With 60% of respondents to a staff survey being under 35 years old, our nursing team is particularly career and development orientated. Education and training focuses on resources and
programs to develop skills and competencies, with programs in:
- team leader workshops
- specialist tumour stream education days
- opportunities to develop skills working with Specialist Nurse and Nurse Practitioner teams.
• Programs led by Clinical Nurse Educators support recruitment strategy, consistent staffing and low agency utilisation. They include:
- Under-graduate placements from 3 universities
- TAFE undergraduate EN placements
- Graduate program annually (155 applicants for 2020 program when writing)
- International student placements from Denmark, Taiwan and UK
- Aboriginal trainee program for AINs 2019
- Orientation with 173 people attending to date in 2019.
• Collaborations with Sydney University and The University of Tasmania have enabled more than 35 nurses to undertake postgraduate studies over the last 12 months in oncology and management.
FUTURE
• We are in the process of further developing patient experience measures. This includes exploring the inclusion of specific compassionate care measures.
UPDATE
Nursing

57
LEADERSHIP
• A/Prof Carsten Palme - Director (pictured)
• Prof Jonathan Clark AM - Director of Research
• Dr James Wykes - Director of International Fellowship Program
• Dr Hubert Low - Education Lead• A/Prof Ruta Gupta -
Translational Research Lead
HIGHLIGHTS
• Data from Cancer Institute NSW showed the head and neck service at Chris O’Brien Lifehouse performs the largest number of head and neck cancer surgeries in NSW, doing more resections than the next two busiest hospitals combined. (Graph A, next page. Also below, growth in admitted head and neck patients.)
• Cancer Institute data also showed better patient outcomes for head and neck patients treated at Chris O’Brien Lifehouse, demonstrating the clinical advantages of a multidisciplinary team setting at a dedicated high volume cancer centre (see Executive Summary).
• Justine Oates and Sarah Davies became Head and Neck Nurse Practitioners. Nurse Practitioner is the highest qualification in nursing.
• Prof Jonathan Clark (pictured) was recognised as a Member of the Order of Australia for services to Head and Neck Cancer.
CLINICS - REGIONAL
• We expanded our regional clinic program, continuing to improve diagnostic and treatment pathways and outcomes for people living in rural and regional Australia. Our existing clinics in Nowra, Orange and Port Macquarie grew. A new clinic is commencing in Tamworth early in the new financial year.
CLINICS - SPECIALTY
• Sydney Facial Nerve Clinic continued - the first specialist multidisciplinary clinic for patients with malignant facial nerve disorders in Australia.
• Dedicated multidisciplinary speech and swallow clinic commenced to manage common side-effects of mouth and throat cancer treatment.
• Facial Prosthetic Reconstruction Clinic approved and commenced to arrange initial prosthetic assessment and prosthesis.
RESEARCH
• The high volume of patients generates invaluable data. Our research institute, the Sydney Head and Neck Cancer Institute (SHNCI), holds the largest head and neck patient research database and biobank in Australia, with over 14,000 registered patients.
• We are currently conducting or collaborating on more than 50 scientific and clinical research projects in conjunction with University of Sydney, The Garvan Institute of Medical Research, The Illawarra Health and Medical Research Institute, and other academic and research facilities. This includes supervising a number of PhD, Masters, Honours and MD students.
• Research priorities are advanced and metastatic cutaneous squamous cell carcinoma, investigating the rising incidence of oral cancer (particularly in young
UPDATE
Head and Neck

Fellowship position was created to work with A/Prof Sydney Ch’ng.
Courses & Workshops
Members of our department organised several professional development courses across the relevant period, including:
• Head and Neck Cancer Oncology Nurse Education Day - 100 attendees nationally (organised by NPs Sarah Davies and Justine Oates).
• First Sydney Neck Dissection Course (facilitated by Dr Hubert Lowe).
• International Perforator Flap course (facilitated by A/Prof Sydney Ch’ng).
• Microsurgical course - multi-day laboratory based microsurgical course aimed to educate the next generation of microsurgeons (facilitated by A/Prof Sydney Ch’ng and Gareth Crouch).
• Sydney Advanced Stroboscopy workshop for ENTs and speech pathologists in conjunction with the Australian Voice Association (facilitated by A/Prof Daniel Novakovic).
• Thyroid Education Events (facilitated by A/Prof Michael
Elliot).
MDT
• The faculty ran monthly multidisciplinary head and neck teaching for clinicians and academics across Sydney.
Symposium
• The faculty hosted the Chris O’Brien Symposium - On The Shoulders Of Giants: Past, Present and Future in Head and Neck Cancer with a full-day of eminent speakers from around the world and Australia.
• From overseas, we welcomed: Prof Patrick Gullane CM (University of Toronto), Prof Jatin P. Shah MD (Sloan Kettering Memorial), Prof Randal Weber MD (MD Anderson) and Dr Graham Smith (St George’s Hospital, London). From among our Australian colleagues we welcomed: Prof William B. Coman AM (University of Queensland), Prof Suren Krishnan (Royal Adelaide Hospital), A/Prof Julia McLean (St George Hospital and ANZHNCS President), Prof Sandro Porceddu (Princess Alexandra), Prof Danny Rischin (Peter MacCallum Cancer Centre) and Prof Elizabeth Salisbury (Royal Prince Alfred Hospital).
patients who have never smoked), aggressive salivary gland cancers, reconstructive approaches to assist patients with advanced facial cancers and facial paralysis, and patient education for head and neck cancer.
• In an example of research underpinning nursing care, Nuse practitioners Justine Oates and Sarah Davies led a retrospective review of head and neck microvascular free flap surgical outcomes. The study showed excellent outcomes in all areas.
• For details about the head and neck research program, please see Research Report 2017 & 2018 at mylifehouse.org.au.
EDUCATION
Fellowships
• Dr James Wykes continues to manage the heavily subscribed, competitive SHNCI fellowship program, which has grown in popularity. Fellows are appointed at least two years in advance and come from multidisciplinary and international backgrounds.
• In 2018 a dedicated Facial Surgical Oncology and Reconstructive Surgery
Chris O'Brien Lifehouse
Graph A: Annual average resectionsBy NSW public and private hospitals, head and neck cancer, 2016-17

59
LEADERSHIP
• Dr Cindy Mak - Director
HIGHLIGHTS
• 50% female representation in surgical staff (i.e. five female breast surgeons).
• Data from the Cancer Institute NSW showed Chris O’Brien Lifehouse was the second largest breast cancer unit in NSW by volume of surgery.
Above, Growth in head and neck patients (admitted).
• A/Prof Sanjay Warrier was elected President of Breast Surgeons of Australia New Zealand (BreastSurgANZ). (Pictured right).
• Dr Cindy Mak chairs Breast Journal Club meeting held in conjunction with Westmead Hospital and the Mater. This one of a kind meeting in Sydney aims to gather a group of like-minded surgeons to collaborate on latest research and ideas.
• The team performed the first ‘awake’ mastectomy in Australia (A/Prof Sanjay Warrier and anaesthetist Dr Ryan Downey). The patient, Moray Gallacher, was not able to have general anaesthetic. The case took a year of planning and drew on research from other cases across the world.
• The surgical team began using 3D-printing technology to produce 3D models of breast tumours to help visualise and plan surgery.
• The SPY Elite System is the most advanced fluorescence imaging system technology available to accurately detect unhealthy or dead skin cells, known as necrosis. Anecdotally, rates of necrosis have decreased since its introduction in late 2017. A prospective trial is underway to determine the full impact of this technology.
EDUCATION
• 2019 Breast Surgery Fellow Dr Anannya Chakrabarti successfully presented research at several meetings. 2018 Fellow Dr Nita Bartlett became a consultant surgeon in Townsville.
RESEARCH
• We are working on several new trials that evaluate efficacy and safety of neoadjuvant therapies in breast cancer treatment, as this is an area that continues to evolve rapidly.
• Researchers led by RPAH have initiated a database through Chris O’Brien Lifehouse and the operative procedures and multi-modality care that it supports. The database captures outcome data and will inform future research primarily for the purpose of evaluating patient characteristics and management of lactational breast abscesses (a serious complication of mastitis that can lead to hospitalisation).
• For details about the breast research program, please see Research Report 2017 & 2018 at mylifehouse.org.au.
FUTURE
• Dr Cindy Mak has submitted a proposal to Medicare for an item number for fat grafting. This will enable surgeons all around the country to obtain rebates for this procedure.
UPDATE
Breast

60
LEADERSHIP
• Prof Jonathan Carter - Director (pictured)
• Dr Rhonda Farrell - Deputy Director
SNAPSHOT
• Dr Rhonda Farrell appointed as Deputy Director and commenced formal duties in early 2019.
• Nurse Practitioner Shannon Philp, Australia’s only gynae-oncology nurse practitioner, became the first nurse to be awarded the Jeannie Ferris Cancer Australia Recognition Award. This prestigious award recognises outstanding contributions to improving the lives of women affected by gynaecological cancer.
• The department saw continued development and expansion with increased patient volume across both inpatients and outpatients. (Right, growth in admitted gynae-oncology patients).
• Data from Cancer Institute NSW showed one of the highest number of ovarian cancer resections in the state and among best surgical outcomes.
• Robotic surgery continues to give uterine and endometrial patients the best chance of recovery in the shortest period of time.
RESEARCH AND SIGNIFICANT
CONTRIBUTIONS
• Dr Rhonda Farrell is conducting research into the role of HIPEC (Heated Intraperitoneal Chemotherapy) in ovarian cancer treatment. This research is philanthropically funded by a Gift in Will from the late Jennie Connolly.
• Prof Jonathan Carter was invited to present at the Beijing Obstetrics and Gynaecology Hospital Annual Scientific Symposium.
• A/Prof Selvan Pather was an invited speaker at the 38th National Congress of the South African Society of Obstetricians and Gynaecologists (SASOG).
• A/Prof Selvan Pather was organiser for the XXXIVth Scientific Meeting of the Australian Society Gynaecologic Oncologists (ASGO), Sydney 2019.
• For full details about the gynae-oncology research program, see the Chris O’Brien Lifehouse Research Report 2017 / 2018 at mylifehouse.org.au.
EDUCATION AND TRAINING
• A Fellows: Dr Emma Allanson and Dr Michael Burling.
• Gynaecologic Oncology Registrar: Dr. Elizabeth Goulding.
• Dr. Elizabeth Goulding, Gynaecologic Oncology Registrar, was accepted for CGO training 2019, completed a Masters Degree in Public Health and Tropical Medicine, delivered several presentations and lectures.
FUTURE
• Prof Selvan Pather to collaborate on the first uterus transplant clinical trial in Australia, led by Dr Anthony Marren and Royal Prince Alfred Hospital.
• Focus on fostering collaboration in research across different areas of cancer.
Gynae-oncology

61
LEADERSHIP
• Dr Brindha Shivalingam - Director (pictured)
• Dr Kim Kaufman - Head of Brain Cancer Research
SNAPSHOT
• Department expanded to five dedicated surgeons with all VMOs running outpatient clinics on a weekly basis and MDT held each fortnight at RPA.
• Neurosurgical registrar appointed in clinical and research capacity.
• Research program in neuro-oncology launched, with the aim of improving clinical management and outcomes for patients diagnosed with primary brain cancer.
• Rapid Access Brain Tumour Hotline continuing to provide on-call and rapid access to patients.
• Research funding secured thanks to key benefactors.
HIGHLIGHTS
• Increased surgical activity and expansion of services as the neurosurgical service enters 2nd and 3rd years of service (Right, growth in admitted neurosurgery patients).
• Launched as a collection site for the Sydney Brain Tumour Bank, in partnership with Brainstorm Brain Cancer Research at the Brain and Mind Centre, Sydney University and RPA Neuropathology Department.
• Development of GlioNET, a prospective bio/database in collaboration with RPA and USyd. This ambitious project will track Australian patients diagnosed with glioma over the entire course of their cancer journey. This will be the first concerted effort to record complete longitudinal clinical and pathological information, bio-specimens (blood, tumour tissues and cells), imaging and patient and caregiver centred data (self-reported quality of life questionnaires, sleep and exercise data).
• GlioNET longitudinal data and specimens will support a
number of specific sub-studies, including the translation of a non-invasive blood test for monitoring glioma tumour progression, published by our group in 2018 (https://www.nature.com/articles/s41698-018-0071-0).
• For details about the neurosurgical research program, please see Research Report 2017 & 2018 at mylifehouse.org.au.
FUTURE
• Launch of GlioNET (October 2019).
• Roll out GlioNET to other teaching hospitals to increase the resource.
• Continue to expand and concentrate services with vision of forming a centre of excellence.
‘The biggest unquantifiable factor that I have noticed is that patients feel a great sense of comfort and confidence in being treated here. Treatment of brain cancer was so fragmented and patients felt very insecure and lost. Collectively, we’re doing a lot to turn this around.’— Dr Brindha Shivalingam
UPDATE
Neuro-oncology

62
LEADERSHIP
• Professor Henry Woo - Director
HIGHLIGHTS
• Expansion of services and department as more patients access surgery, robotic surgery, chemotherapy, radiation therapy and brachytherapy for urological, bladder and prostate cancer treatment.
• Robotic surgery: Coming from a base of zero in 2015, Chris O’Brien Lifehouse has become the highest volume centre in the country for robotic retroperitoneal lymph node dissection for advanced testicular cancer. This surgery involves removing lymph nodes at the back of the abdomen that may contain cancer cells.
• Performed the first case in NSW of robotic inguinal lymph node dissection for treatment of penile cancer, integrating a multidisciplinary collaboration with breast cancer surgical colleagues to use SPY technology to test vascular activity to assess risk of necrosis.
• We have become one of the highest volume centres in testicular cancer surgery in NSW.
• Rapid Access Prostate Cancer Assessment Service: continues to streamline cancer screening services, minimising harmful waiting times and related anxiety by delivering diagnostic procedures within one to two weeks of referral.
Uro-oncology
• For details about research undertaken by the uro-oncology service, see the Chris O’Brien Lifehouse Research Report 2017/2018 at mylifehouse.org.
FUTURE
• Patient Access: urological surgery is currently only available to private patients. Efforts to build a dedicated hardship fund will cover or subsidise the cost of this surgery for public patients.
• Improve and streamline diagnostic procedures, giving patients the most efficient, painless and safe diagnostic pathways.
• Transperineal template prostate biopsy is a diagnostic procedure that is reported to have fewer complications than transrectal biopsy. This procedure has a significantly lower rate of complication. Through research, we are seeking ways to make transperineal prostate biopsies safer and more viable, performing them under local anesthetic and without the risk of impact on sexual function.

63
HIGHLIGHTS
• The Upper GI service has expanded substantially with large increases in overall numbers of surgeries and performance of more complex surgeries. Pancreatic and oesophageal surgery numbers are especially high.
• Commencement of upper robotic GI surgery.
• Expansion of MDTs, attended by specialists from Chris O’Brien Lifehouse and Royal Prince Alfred Hospital. These include:
1. Upper Gastrointestinal/Hepatobiliary (HPB) MDT, discussing approx. 30 patients each week (approx. 1,200 - 1,500 patients in the year) .
HIGHLIGHTS
• Surgeons are focused on performing minimally invasive procedures to offer symptomatic relief for cancer patients, and enabling patients to avoid major surgery and external drains/tubes.
• Focus on development of pancreatic cancer screening services for high-risk individuals.
• An Advanced Endoscopy Fellow is assisting A/Prof Payal Saxena in clinical work and performing research across Chris O’Brien Lifehouse and Royal Prince Alfred, contributing towards research collaborations.
Upper Gastro-intestinal (GI)
Gastroenterology
2. Neuroendocrine MDT.
3. Abdominal Sarcoma MDT is starting imminently.
FUTURE
• As the hospital continues to manage and accommodate rapid expansion of the Upper GI service, the leadership is committed to recruiting more exceptional Upper Gastrointestinal and Hepatobiliary surgeons, and vigorously supporting them in their aspirations to achieve better clinical, research and education outcomes.
• We will continue our focus on developing research collaborations between Lifehouse and RPAH.
• Surgeons performed Hybrid Argon Plasma Coagulation in patients with dysplastic Barrett Esophagus in a novel treatment that is only available at Chris O’Brien Lifehouse.
FUTURE
• We will continue our focus on developing the gastroenterology service and bolstering clinical and research collaborations between Lifehouse and RPAH.

64
ColorectalHIGHLIGHTS
• Growth in volume of colorectal procedures, including more radical resections and robotic surgery.
• Increased integration with specialty clinics like the Post Cancer Sexual Intimacy For Women run by the Gynaecological Oncology Group.
• Focus on upskilling of ward staff and consolidating outpatient pathways for stoma care and management of indwelling catheter on discharge.
• Stronger cross-disciplinary collaborations including:
1. pelvic exenterations in conjuction with gynae- and uro-oncology.
2. cytoreductive surgery with gynae-oncology (no HIPEC).
3. abdopelvic sarcoma and retroperitoneal sarcoma MDT.
• Clinicians contributing to novel research in Abdominopelvic Sarcoma and Retroperitoneal Sarcoma.
• Development of bowel screening program via the Rapid Access Endoscopy Clinic.
FUTURE
• To develop and implement an advanced GI program incorporating maximally and minimally invasive surgeries for the complete management of primary and recurrent malignancies.
• We are looking forward to participating in the ovarian HIPEC trial - a randomised, multicentre trial.
Thoracic surgeryLEADERSHIP
• Professor Tristan Yan was appointed as Head of the Department of Thoracic Surgery.
• Professor Yan brings extensive experience in the management of thoracic malignancies, including lung cancer and mesothelioma with a particular interest in minimally invasive surgery.
• This appointment is intended to enhance existing clinical and research for the management of thoracic cancers.
• Lung cancer patients can access keyhole, open and robotic thoracic surgery, chemotherapy, radiation therapy and clinical trials.

65
Integrative oncology and supportive cancer care are rapidly developing areas nationally and internationally. This service (housed in the LivingRoom) and its research strategy aims to develop a strong evidence base to support the integration of holistic medical care, complementary therapies and exercise into standard cancer care. Furthermore, as people live longer with cancer, there is a growing need to develop programs that help them live well.
LEADERSHIP
• A/Prof Judith Lacey - Director
SNAPSHOT
• Currently approx. 10% -15% of Chris O’Brien Lifehouse patients come through the LivingRoom as outpatients for supportive care or complementary medicine.
• Our outreach program is growing thanks to philanthropic support with significantly increasing numbers receiving therapies on the wards and in day and radiation therapy spaces.
• Approx. 55 patients are treated each month under Equity of Access funds which are philanthropically funded.
• The service has been recognised by peers as one of the most comprehensive integrative oncology services in Australia.
• Philanthropic funding has enabled part time research fellow position and day therapy intervention program and research.
• Team members hold leadership positions in the field of integrative oncology and their area of expertise nationally and internationally.
SERVICES
• Holistic medical consultation• Acupuncture• Exercise physiology• Mindfulness meditation group
and 1 to 1 therapy• Oncology massage• Qigong• Reflexology• Yoga : group and one-to-one
therapy• Lymphoedema service,
including early intervention screening
• Physiotherapy : including pelvic physiotherapy expertise
LivingRoom services work alongside Allied Health services such as psycho-oncology, speech therapy and dietetics. See the Allied Health update on the following pages.
UPDATES
• Ongoing developments of service provision and research in the space.
• Successful embedding of patient voice through the use of patient reported outcome measures has improved our understanding and response to patient supportive care needs.
• The early lymphoedema program has seen rapid growth amidst rising demand, growing from to five sessions per week at full capacity. It offers early lymphoedema assessment for high-risk patients (primarily from head and neck, breast and gynae-oncology).
• New program in Yoga for Lymphoedema launched.
• New program in gentle Chair Yoga launched.
• Focus on team-building with experts in oncology and ensuring all practitioners are well-supported and showcasing their skills.
HIGHLIGHTS
Development of service and the field of integrative oncology:
• Strong focus on evaluating the entire service and how we benchmark against larger integrative oncology services internationally.
• Focus on sharing knowledge about the establishment of an
Supportive Care and Integrative Medicine

66
integrative oncology service in the Australian healthcare setting.
RESEARCH
• The majority of the team is engaged in research and/or teaching.
• Research focus on evaluating the benefit of individual and multimodal interventions in holistic supportive care including exercise and complementary therapies.
• The lymphoedema service is developing research protocols and collaborative university and multidisciplinary partnerships around intervention for patients with gynaecological cancers at risk of developing bilateral lymphoedema.
• Acupuncturist Dr Victoria Choi has completed her PhD in the mechanism of acupuncture and is embarking on post-doctoral research in acupuncture for neuropathy. We also welcome a new acupuncturist Emma Wong who has commenced her PhD
in the area of acupuncture and prostate cancer related erectile dysfunction.
• Research fellow Dr Diana Naehrig is working with Dr Lacey and a multidisciplinary hospital-wide team evaluating the unmet supportive care needs of cancer patients at Chris O’Brien Lifehouse. This will inform interventions and service development and enabling benchmarking.
• Our researchers initiated a practice-changing study into living well with melanoma and immunotherapy.
• For full details about the Supportive Care and Integrative Oncology research program, see the Chris O’Brien Lifehouse Research Report 2017 & 2018 at mylifehouse.org.au.
• Dr Lacey is involved in NSW Health and other funded research as a co-investigator in medicinal cannabis.
FUTURE
• Integration of digital screening and patient-reported outcome measures to improve timely access to helpful interventions.
• Expand our exercise programs through collaborative multidisciplinary research in most cancer groups as part of larger multisite studies and new initiatives.
• Partner with academic centres of excellence, eg USyd and WSU (NICM) in implementation and other research.
• Development of stronger partnerships nationally in research and strategic developments in this field.
• Development of a national education program on integrative oncology services.
• We welcome Dr. Shelley Kay as Exercise Physiologist and acupuncturist Emma Wong to our team and farewell Michael Marthick.

67
LEADERSHIP
• Dr Toni Lindsay - Allied Health Manager
SERVICES
• Dietetics• Discharge Planning• Music Therapy• Occupational Therapy• Physiotherapy• Psycho-Oncology• Social Work• Speech Pathology
HIGHLIGHTS
• All services have seen considerable growth in the context of increased hospital activity. (Below, growth in physiotherapy service.)
• Clinics were developed in voice, swallowing and post-surgical follow-up.
• Two new positions were created: - Discharge Planning Service commenced in April 2019, working closely with Social Work and Nursing management - Occupational Therapy service created in February 2018.
• Physiotherapy: - recruited its first new graduate - focussed on programs that facilitate exercises on the wards through gentle exercise classes, etc - increased equipment such as Continuous Passive Motion (CPM) machine thanks to funding from Dry July.
• Jacqueline Baker, a senior dietitian, was one of two Australians invited to attend an international conference in nutritional needs for cancer patients.
• Dietetics continued its strong clinical expertise in complex head and neck cases, as well as gastrointestinal tract complexities around feeding and total parenteral nutrition (a method of feeding that bypasses the gastrointestinal tract).
• Speech pathology services have grown with a majority of work in the head and neck service and expansion into neurosurgical patients.
EDUCATION
• Speech pathologist Emma Charters is a PhD candidate studying advances in head and neck cancer treatment impact on swallowing.
• Senior physiotherapist Leah
Steele started the Health Leadership program through UTAS.
• Leah Steele and Justin Cheong were granted Honorary titles in Physiotherapy at the University of Sydney.
• Several team members were awarded Keith Cox Educational Scholarships for conference and professional development attendance.
• Funding secured for Tracheostomy Observation Models models (a head and neck model of a patient with a tracheostomy in situ) for education/teaching for patients, families and staff.
• Training for students in Physiotherapy (clinical and project based placements) and Clinical Psychology.
ACHIEVEMENTS
• Dr Toni Lindsay’s book, ‘Cancer Sex Drugs and Death: A Clinician Guide to the Psychological Management of Young People with Cancer’ was published to help health professionals working with young people with cancer understand their emotional and psychological needs.
• Speech Pathologist Emma Charters recognised for best research proposal at the Chris O’Brien Lifehouse Concept Development Workshop 2018.
FUTURE NOTES
• The Speech Pathology team has completed a Head and Neck Support Group Project
Allied Health

68
- Jack Thomas, Senior Music Therapist
that lays the foundations for beginning such a group at Chris O’Brien Lifehouse. The project has gathered data from 119 patients to inform the sustainability and function of a Head and Neck support group. We are in the process of receiving feedback for publication and developing a working party.
MUSIC IN HEALTHLEADERSHIP
• Dr Emma O’Brien OAM - Music Therapy Fellow and Program Founder
• Dr Toni Lindsay - Allied Health Manager
• Jack Thomas - Senior Music Therapist
• Robert Teicher - Choral Director
SERVICES
• Clinical bedside music therapy• Outpatient services• Live music in public and shared
hospital spaces• Chris O’Brien Lifehouse Choir
HIGHLIGHTS
• Expansion of team, with promotion of Jack Thomas to Senior Music Therapist and appointment of two more part-time therapists (Total 1.8 FTE).
• Overall increase in services including more referrals, more occasions of service, higher choir numbers.
• 2x increase in number of inpatients seen by music therapists in 2019 (compared with 2018).
• Strong focus on building the program for adolescent and young adult sarcoma patients.
• Fifth birthday celebrations: The Music In Health service played a significant role in the celebrations with a small choral rendition of the official anthem ‘You Raise Me Up’, bringing together singers and accompanists from the Chris O’Brien Lifehouse ‘family’ for a one-off performance.
• Choir: continued to grow with approx. 27 attendees (avg)
each Thursday in the main foyer and once per month in Radiation Oncology. We introduced monthly rehearsals to help build confidence and expand repertoire and arrangements.
FUTURE
• A new Sony Foundation You Can Centre at Lifehouse for adolescents and young adults with cancer will include a dedicated music room and recording studio.
• Bringing music to more shared spaces: Launching Live Music Volunteer Program, with a roster of volunteers to play high-quality live music in various public and shared spaces around the hospital. This will positively enhance the atmosphere, environment and experience for patients, families, visitors and staff.
• Philanthropically-funded research assistant and program to commence, leading research into the benefits of music therapy and songwriting.

69
LEADERSHIP
• Mrs Gail O’Brien AO - Patient Advocate
SNAPSHOT
• Gail continued in her role as Patient Advocate Liaison for the second and third years.
• Support provided is multifactorial. It includes: - Emotional or logistical support for patients and families. - Supporting clinicians and nurses as an intermediary for communication, particularly with respect to complex medical issues and life expectancy.
HIGHLIGHTS
• The service saw an increase in referrals.
• The role became more embedded throughout the hospital.
• Clinicians and nurses more readily took up the opportunity to involve a Patient Advocate Liaison.
• A high-visibility communications campaign encouraged patients to reach patient advocacy via a direct phone number.
• A focus has been on identifying as early as possible patients and families most in need.
• The role has evolved to complement various allied health and supportive services.
• End-of-life patients have presented acute needs.
FUTURE
• Lorainne Brecard joins Gail as as Patient Liaison.
Patient Advocacy

70
LEADERSHIP
• Shirley Baxter - Co-chair• Claude Gauchat - Co-chair
Council members:• Bev Noble• Maryanne Gauchat• Raymond Chan• Jane Cockburn• Brian Dalton (new member)• Polly Kolotas (new member)• Sue Floro (new member)
Chris O’Brien Lifehouse representatives:• Catherine Lambert - Director of
Clinical Services• Xanthe Jones - Assistant
Director of Nursing, Governance & Quality
• Karen Heath - Manager, Volunteer Services (incoming member in FY19/20)
SNAPSHOT AND HIGHLIGHTS
• The PAC grew in the relevant period, adding 3 new members and electing a co-chair.
• The PAC saw increased activity during the accreditation process as it participated in surveyors’ meetings and forming documentation that demonstrated the significant consumer engagement embedded at Chris O’Brien Lifehouse.
• Led the gym garden development including concept, landscape design and installation.
• Participated in the patient-led handover project.
• Represented the consumer voice at all new employee orientations.
• Engaged in environmental design and refurbishment of
Radiation Oncology waiting area.
• Worked with Day Therapy staff on a project to reduce waiting times.
• Represented consumers to the Board of Directors and on multiple governance committees, including the Board Clinical Governance Sub-Committee and strategic planning meetings and events.
• Reviewed patient literature to ensure health literacy.
• Continued to review patient feedback and outcomes.
FUTURE
• Strategy 2019-21 is being executed and will have mid-term review in 2020. The focus will be on STD2 but starting to develop plans for STD5 engagement.
The voice of the patient has always been at the heart of the design and development of Chris O’Brien Lifehouse. The Partnership Advisory Council was formed in September 2013 and is made up of cancer survivors, carers and consumers. The council informs the development of Chris O’Brien Lifehouse policies, procedures and communication that impact on the patient experience, and represents the patient voice in governance committees.
Partnership Advisory Council (PAC)

71
LEADERSHIP
• Lorraine Brecard - Manager, Volunteer Services
• We welcome Karen Heath as the new Manager, Volunteer Services in 2019.
SNAPSHOT
• Approx. 67 volunteers (including Arterie) currently active.
• Approx. 55 volunteers working each week (average).
• Each day, the patient car picks up approx. seven patients from their homes (mainly in the inner-west), drives them to appointments and back home.
• Each day, the shuttle bus runs seven trips between Central Station and Chris O’Brien Lifehouse.
SERVICES
• Inpatient support: visiting patients and families on wards, giving reading materials, offering refreshments, tidying rooms, cleaning ward kitchens.
• Outpatient support: visiting patients in day therapy and clinic waiting rooms for refreshments, company and support for patients who are undergoing chemotherapy or waiting for appointments.
• Concierge: greet patients, assisting with navigation and mobility.
• Wig Library: helping patients with fitting and maintaining wigs and scarf styling .
• Administration: administrative support to all departments as needed.
• Spiritual Care: support in spiritual care and support to patients, carers and families.
• Patient Transport: bus and car transporting patients from homes and public transport links.
UPDATES
• We have seen an increase in volunteers with a volunteer recruitment process underway.
• New corporate support program launched.
• New volunteer roles were introduced to give additional support to new departments.
• New data system for volunteers implemented.
Volunteers

72
LEADERSHIP
• Deborah Burdett - Director• Nicole Hutton - Carterist
SERVICES
• Non-intrusive, inclusive and supportive opportunities for patients and their families to connect through art and craft programs.
• Carterie mobile studio: offering arts and crafts to patients on wards and in waiting areas.
• Weekly Open Studio: free all day informal art drop in support group to Lifehouse Community.
• Artist-in-Residence program: three-week residencies to different practising artists each month. The artist demonstrates in the main foyer. (Pictured top right, Nicholas Harding).
• Year-long Year 10 Sydney Secondary College, Leichhardt Campus weekly support program.
SNAPSHOT
• Arterie operates three days per week.
• 20 x active volunteers each week across artists, architects, art educators, and pit crew support.
• Supports 10 x students each week.
• 1 x Master of Art Therapy - Practical Placement student.
• 10 x Artists in Residence.
• 3 x carterists per day, with each carterist having approx. 5-10 engagements with patients either on the wards or in waiting areas.
HIGHLIGHTS
• Collaborations with Dry July, Quilt NSW, Australian Tapestry Workshop, Australian Design Centre, Lyndal T Crockery, Inky Playtime, Denyse Whelan.
• Weaving into Wellbeing (collaboration with Australian Tapestry Workshop Melbourne) is now on display in Radiation Oncology.
• 80 dolls were handmade by Open Studio participants and sent to the Uthando Orphanage.
• Completion of the Listening Chairs involving approx. 80 patients included (Pictured middle right).
• Completion of the Sargasso Curtain Project involving approx. 40 patients.
• The Pepi Project stitching project involved approx. 60 patients.
• Arterie’s Blue Hexagon project was displayed at the 2019 Annual Quilt Show, Darling Harbour - more than 17,000 hexagons received via the wider community of NSW (Pictured bottom right).
• Production and collaboration of ‘Hope’ plates and crockery with
Lyndal T Crockery.
• Craft Up Late - Evening Open Studio in Foyer was run in collaboration with Quilt NSW and Australian Design Centre.
• Support and completion from the Pollys Club via the Pollys Headdress Project.
• Completion of the Chen Residency - Drawing Carterie Program in honour of patient Joyce Chen.
Arterie

73
Featured Artist: Julia Westwood
All artworks in this report are acrylic on canvas paintings by Julia Westwood.
Julia is a figurative artist working in Sydney. With a background in symbolism, semiotics and social research, Julia’s work is characterised by themes of family, memory, nostalgia and mortality. Her professional practice includes drawings and paintings in oil, acrylic and ink on a variety of different surfaces such as canvas, board and paper. She graduated in 2019 with a Bachelor of Fine Arts from National Art School.
Julia was Artist in Residence at Chris O’Brien Lifehouse in 2019, and has subsequently painted several commissioned works for the hospital.
www.juliawestwood.com.au

74
Chris O'Brien Lifehouse119 - 143 Missenden RoadCamperdown NSW 2050PO Box M5 Missenden RoadCamperdown NSW 2050
www.mylifehouse.org.au
General EnquiriesT: (02) 8514 [email protected]
Media EnquiriesT: 0429 846 [email protected]
Donations & SupportT: (02) 8514 [email protected]
Registered Charity Number CFN 17573 Hospital Provider Number 0027350Y© 2019 Chris O'Brien Lifehouse
Artwork by Julia WestwoodPhotography by Mark ChewProduced by Juliette O’BrienPrinted by Vertifix Printing












![Quick Start Guide - HealthLink · [Type here] Best Practice Edition Quick Start Guide Chris O’Brien Lifehouse Referral SmartForm The Chris O’Brien Lifehouse Hospital Referral](https://static.fdocuments.us/doc/165x107/5ad050af7f8b9ac1478dd551/quick-start-guide-type-here-best-practice-edition-quick-start-guide-chris-obrien.jpg)