Repetitive strain injury in computer keyboard users: Pathomechanics and treatment principles in...
-
Upload
katy-keller -
Category
Documents
-
view
241 -
download
4
Transcript of Repetitive strain injury in computer keyboard users: Pathomechanics and treatment principles in...

[ SCIENTIFIC/CLINICAL ARTICLES J Repetitive Strain Injury in Computer
Keyboard Users: Pathomechanics and Treatment Principles in Individual and
Group Intervention
Katy Keller, MS, PT West Side Dance Physical Therapy New York, New York
Julie Corbett, MS, OTR, CHT Hudson River Hand Rehabilitation Fishkill, New York
Diane Nichols, ACSW Performing Arts Psychotherapy Center New York, New York
H ealth practitioners in occupational medicine are faced with a new challenge: how
to treat the rising number of patients presenting with Repetitive Strain Injury (RSI). Also known as cumulative trauma disorder, repetitive motion disorder, and overuse syndrome, RSI is characterized by a series of interrelated musculoskeletal and neurovascular conditionsl
-4 and is associated with
workplace risk factors such as repetitive motion and awkward joint postures.5-13 According to the Bureau of Labor Statistics (BLS), the number of such work-related injuries more than doubled in 5 years, from 140,000 cases in 1989 to 281,000 cases in 1993.14
The highest percentage of work injuries resulting from repetitive motion occurs in the manufacturing sector, where assembly-line work is common.14,15 Keyboard users, however, are emerging as a significant segment within the overall RSI-afflicted work population.8.16-20 In a BLS survey of nearly 90,000 work injuries resulting from repetitive motion, 12% were attributed to the repetitive motion of "typing or key entry."14 The number of workers with keyboard-related injuries can be expected to rise; already 60 million Americansnearly half the V.S. work force-use computers on a daily basis in the workplace or at home. 16,17,21,22
Correspondence and reprint requests to Katy KeJier, MS, PT, Westside Dance Physical Therapy, 2lO9 Broadway, Suite 204, New York, NY lO023.
ABSTRACT: Computer users experience high rates of injury and disability, broadly termed repetitive strain injury (RSI). With more than 60 million Americans using computers in offices and homes, the potential magnitude of the RSI problem indicates a need for increased attention to prevention and treatment. The purpose of this article is to: 1) present a conceptual model of RSI as a kinetic-chain, multifactorial disorder; 2) outline the salient features of the clinical evaluation of the RSI patient; 3) describe the role of postural deviation in the pathogenesis of RSI; 4) present the principles of individual manual therapy; and 5) discuss the rationale, admission criteria, educational principles, and outcome of a multidisciplinary group intervention. J HAND THER 11:9-26, 1998.
The BLS reported in 1993 that "repetitive motion cases typically resulted in the lengthiest absences from work of any work-related injury," with "carpal tunnel syndrome requiring the longest recuperation."14 Related worker's compensation and absenteeism cost U.S. employers more than $20 billion in 1990, and this figure is increasing each year. IO,18,19,22-24
Because the syndrome is relatively new and because its incidence has risen so quickly, the development of treatment approaches to RSI is still in the early stages and standard protocols are not yet in place. A multi disciplinary team approach to RSI was developed at The Miller Institute* starting in 1992. This approach has been utilized elsewhere by the medical community in its application to back injury and chronic pain, but only recently has it been applied to work-related RS1.1,25 The team consists of a physician, psychotherapist, technique retraining specialist, and physical, occupational, and massage therapists.
Many of the concepts developed in treating overuse26-30 and technique faults31 - 34 in performing arts patients are applied to treating computer keyboard-injured patients. As with the performing art-
'The Miller Institute for Performing Artists, at st. Lukes/Roosevelt Hospital in New York City, was established in 1985 as a treatment center for performance-related injuries of musicians, dancers, and actors.
January-March 1998 9

ist, a principal challenge in treating the keyboard user is dealing with the patient's realistic anxiety about whether the physicial limitations of RSI will compromise the previous level of performance, and the fear of re-injury and setbacks once the course of treatment is completed. Toward this end, the group process focuses on educating patients in strategies for self-management of the condition, resolving conflicts at work while recovering, and negotiating re-entry into work after a prolonged absence. Most important, the group process utilizes the participants' shared "professional culture" and strong work ethic to redirect the loss of meaningful and affirming work into the work of recovering from RSI proactively. The concepts presented in this paper represent information collected from the treatment of approximately 75 patients with keyboard-intensive occupations (e.g., journalists, editors, writers, and data-entry operators) over a period of three years.
The objective of this article is to present a conceptual framework for understanding the pathomechanics of RSI, based on the clinical evaluation and composite clinical profile of the typical computer-keyboard-injured RSI patient. Principles for treating patients both one-to-one and as part of a multidisciplinary group are outlined.
PATHOMECHANICAL DEFINITION OF RSI
Repetitive strain injuryt is not a diagnosis but rather an umbrella term for a number of related upper-quadrant disorders of the hands, arms, shoulders, neck, and backJ -3,1O,J3,35 The disorders involve the musculoskeletal and neurovascular systems to varying degrees. They share similar pathologic processes, including microtrauma, inflammation, scar formation, and ischemia in response to precipitating biomechamical forces.5,6,J3,J5,28,36-39 The neurovascular disorders, characterized by circulatory compromise and nerve entrapments, occur at multiple sites along the cervical spine, brachial plexus, and median, ulnar and radial nerve pathways.
Examples of musculoskeletal disorders and neurovascular disorders are listed in Table 1.40-43
tSynonymous terms for RSI in the literature include cumulative trauma disorder (CTD), repetitive motion disorder (RMD), and occupational overuse syndrome (OOS), among others, These designations describe mechanisms of injury but not diagnostic entities, and anyone of them needs to be accompanied by one or more medically recognized sub types (e.g., carpal tunnel syndrome, cubital tunnel syndrome, epicondylitis), While nomenclature does contribute to confusion about the condition, the substantive controversy in the literature revolves around issues of medical legitimacy and of overuse and occupation as etiologiC factors, Use of the term RSI in the context of this paper does not indicate a preference for one designation over another. However, RSI was the term most frequently used by the physicians who referred patients to us from a predominantly computer-based population, In other industries (e.g., manufacturing), CTD has become the more prevalent term.
10 JOURNAL OF HAND THERAPY
Clinically, RSI patients may be referred to therapy with any number or combination of these disorders simultaneously.4J Raynaud's disease is included in the list with the caution that thoracic outlet syndrome or myofascial trigger point disorders may mimic the classic triad of symptoms associated with Raynaud's-Le., cyanosis, blanching and erythemia of the hand.44A5 It is important for the clinician to recognize that these disorders, like Raynaud's, can also produce vasomotor changes manifested in the hands.45
Medical references to RSI typically describe the components of this condition as separate disordersYA,8,39A6 It is the contention of the authors, however, that all the disorders included under the RSI designation are dynamically interrelated by an upper-quadrant kinetic-chain response to adverse mechanical forces and behavioral stressors, A kinetic chain is defined as a series of joints interconnected by soft tissues, in which altered structural or functional relationships in one region influence adjacent and distant areas in the chain.47 (See a chart summarizing interrelationships of the upper-quarter kinetic chain in Table 3.) The pathomechanical chain response can originate in one or several areas. The common points of origin in computer keyboard users include the fingers and wrist, the shoulder girdle, and the head and neck. The particular sequence in the chain and potential for injury are determined by an individual's unique neuromusculoskeletal compensatory response to altered forces on the tissuesYA8A9
TABLE 1. Musculoskeletal and Neurovascular Disorders Found in Repetitive Strain Injury (RSI)
Musculoskeletall- 4.s,39
1. Tenosynovitis of the flexor tendon mechanism (trigger fin-ger)
2. Myositis of the wrist flexors 3. Tenosynovitis of the wrist extensors 4. Ganglion cysts 5. de Quervain's syndrome (first dorsal compartment) 6. Intersection syndrome 7. Extensor pollicis longus tenosynovitis (third dorsal com-
partment) 8. Lateral epicondylitis (tennis elbow) 9. Shoulder tendinitis and impingement syndrome 10. Cervicobrachial myofascial pain disorders 11. Cervical spondylosis
Neurovascular 1.3,4.32,40 - 43
1. Cervical radioculopathy 2. Thoracic outlet syndrome consisting of compression of the
upper and/or lower nerve trunks of the brachial plexus and the subclavian vessels
3. Median nerve syndromes, including pronator syndrome, anterior interosseous nerve syndrome, and carpal tunnel syndrome
4. Ulnar nerve entrapments, including compression in the forearm, cubital tunnel, and Guyon's canal
5. Radial nerve entrapments, including compression in the radial tunnel, dorsal forearm, and posterior interosseous nerve syndrome
6. Sympathetic overactivity 7. Raynaud's disease

TABLE 2. Risk Factors Associated with RSI in Computer Keyboard Users
Temporal
Lack of rest breaks and recovery (work pace)
Task repetition High rate of typing Deadlines
Environmental Ergonomic
Incompatible work surface heights
Poor lighting Inadequate chair
support
Biomechanical
Excess force (e.g., keystrike)
Increased static loading
Localized compression
Tension! friction
Pathomechanics of N onneutral Postures
Nonneutral alignment is defined here as a preference for movements that over use end-range joint positioning or consistently deviate from the midrange position of function.2,32 The position of function for the upper extremity at the keyboard is described as follows: The midline of the hand is aligned with the midline of the forearm, the wrist is in approximately 20° of extension, and the fingers maintain a natural curve with the metacarpophalangeal joints in approximately 50° of flex ion and the thumb in line with the radius.32 The elbow is flexed in the midrange between full flex ion and extension, and the shoulder is positioned midway between internal and external rotation,2
Nonneutral alignment compromises joint mechanics and optimal muscle length-tension relationships. At the keyboard it can be seen in cyclic end-range positions and static postures, such as the combination of forward head, shoulder internal rotation, acute elbow flexion, forearm pronation, and wrist ulnar deviation with an alternating cycle of wrist hyperextension and flexion. Nonneutral positions (joint angle beyond its midpoint)/ whether maintained statically or performed repetitively, are a key precipitating factor in the development of RSI at the keyboard.2,s,6,36,38 Nonneutral positioning of joints alters chain biomechanics, compressing nerves and soft tissues against adjacent bony prominences, fibrous bands, and tunnels.38,42,43,50,S1 Repetitive motion causes shearing and irritation of the compressed tissues.52 The nerves and their microcirculation are especially vulnerable to tension, friction, and compressive forces generated at multiple sites along their pathways in the kinetic chain.43,53,54 Nerve injury at a proximal site disrupts the pressure gradient ofaxoplasmic flow and may lessen a nerve's ability to withstand adverse forces at a more distal site, as described in the "double-crush" or "multiple-crush" phenomena.53 -57 Pathomechanically, intraneural scarring or tethering of a nerve decreases the nerve's mobility along its entire length, making it more vulnerable to additional injuries during repetitive movements.53 Multiple crush implies that once nerve injury has occurred, normal movements of the arm can precipitate additional injury to other sites along the susceptible nerve. For instance, when the fingers and wrist move in typing, sliding of the nerves not only oc-
Behavioral
Unrealistic selfexpectations
Type A personality Psychosocial job
stress Job insecurity Productivity
demands
Physical! Anthropometric
Anatomic predisposition
High elbow-carrying angle
Ligament laxity Deconditioning Age
Postural!Keyboard Technique
Forward head and shoulders
Non-neutral joint positioning (e.g., ulnar deviation)
Finger splay Keyboard style
(e.g., "clacker" [Pascarelli])
curs at the wrist but extends into the upper arm. If the peripheral nerves can no longer slide freely in their respective canals because of the proximal entrapments, shearing and microtrauma will result from the normal movements of typing.37,58 The multiple-crush syndrome helps explain the complex and often confusing array of coexisting symptoms characteristic of RSL42,53,54,57
Muscles, tendons, ligaments, synovia, and joint capsules are subject to mechanical deformation and adaptive shortening in response to prolonged static and dynamic loading in maladaptive postures, 38,45,48,59-64 Upper-quadrant muscles in particular are susceptible to overload and fatigue45 and respond in a predictable pattern of hypertonicity and inhibition.49,61,62 The overall change in tissue tone thereby alters joint play, which in turn alters arthrokinematic function and force transmission.38,48,65,66 The resulting joint dysfunctions and faulty movement patterns further compromise nerve pathways and blood flow. Remote trigger points and brachial plexus compression can have distal effects including edema, fibrosis, and temperature changes.41 ,44.45 Ischemic nerves, hypertonic muscles, and sensitized mechanoreceptors of the involved tissues and joints bombard the nervous system with abnormal impulses, creating hyperalgesia in the segmentally related muscles and reference zones.50 Pain initially generated from mechanical irritation is maintained chemically by the metabolites of continuing muscle hypertonus63.67
and overactivation of the gamma motor neuron system,48.68
Many biomechanical, temporal, postural, ergonomic, behavioral, and physical predisposing risk factors can precipitate a pathologic response along the kinetic chain. Examples of these risk factors are listed in Table 2. Predisposing medical considerations such as diabetes mellitus, thyroid disease, smoking, and obesity are also important considerations in regard to the patient's sensitivity to ergonomic or other risk factors.3 Once injured, the tissues are more vulnerable to stresses of lower intensity,8,38.53,69 such as the "repetitive submaximal loading" that occurs in typing.3,15 In summary, normal muscle-tendon extensibility, joint mobility, nerve gliding, nociceptive signaling, and axoplasmic, blood, lymphatic, and synovial fluid dynamics are distorted by altered mechanical forces at the skeletal-soft tissue interfaces, setting up a cycle of pain and dysfunction.
January-March 1998 11

POSTURAL DEVIATION IN RSI PATHOGENESIS
It is the contention of the authors that characteristic postural deviations in the upper-quadrant kinetic chain (see Table 3), when combined with prolonged, sedentary keyboard operation, play a central role in the pathogenesis of RSI.:f: These postural deviations include forward displacements of the head and shoulder girdle, scapular protraction, elbow flexion and adduction, forearm pronation, ulnar deviation at the wrist with hyperflexion or hyperextension, and numerous hand and finger malalignments. Over time, the soft tissues adapt to these postural malalignments by myofascial shortening or lengthening.45,n Changes in the length of the tissues are associated with muscle imbalances, joint dysfunctions,48 and nerve entrapments64 and potentially lead to pain45 and functional impairment.48,49,61 The authors subscribe to Janda's theory of imbalance between postural and phasic muscle groups, exemplified at the shoulder girdle by the "upper crossed syndrome."6o-62 Specifically, there is an imbalance between the shortened upper trapezius, levator scapulae, scalenes, pectorals, and neck extensors on the one hand, and the weakened lower trapezius, serratus anterior, interscapular muscles, and deep neck flexors on the other.61,62,65,66 The shortened muscles tend to be recruited first in movement patterns, perpetuating overuse and chronic loading within the upper quadrant.49,61,66
In the following section, the interactions of postural deviation and pathomechanics are separated out by anatomic region. Table 3 shows the clinical problems associated with nonneutral alignments at each of these joints.
Head and Neck
Anterior displacement of the head excessively lengthens the prevertebral neck flexors and shortens the neck extensors, upper trapezii, and levator scapulae.48,49 The shortened muscles, unopposed by the mechanically disadvantaged flexors, pull on the cervical segments to which they attach, cfeating midcervical strain and increased loading of the joints. Over time, degenerative changes in the cervical spine and periarticular structures can lead to posterior nerve root irritation and cervical radicu-10pathy.48 McKenzie's conceptual model of spinal disorders63 categorizes this mechanical response to poor postural habit as a progression from a "postural syndrome" to "dysfunction" to "disc derangement," In a postural syndrome, pain arises from prolonged loading and overstretching of capsuloligamentous tissues. The postural pain is alleviated by shifting position, which releases tension on the tissues. Protracted anterior displacement of the head causes microtearing and fibrosis of the
tReferences 1, 15, 38, 45, 48, 66, 70, 71.
12 JOURNAL OF HAND THERAPY
strained tissues and leads to a loss of full range of motion. If the annulus fibrosis becomes involved, disc displacement and derangement ensue. The resulting neurogenic pain, as opposed to "the pain of overstretching," is no longer alleviated by changes in position and alignment.63
Forward head posture also causes shortening of the suboccipital muscles with potential for impingement of the occipital nerves, vertebral artery, and dorsal roots of the first cervical nerves.73 The hyperactive response of the scaleni to the forward head posture predisposes to entrapments of the cervicobrachial plexus and the dorsal scapular nerve in their paths through the scaleniYA2A4A5A8 The resulting pattern of motor weakness, pain, and paresthesias radiating to the shoulder, arm, and hand depends on the specific sites of entrapment. Excessive forces placed on the midcervical spine from the pull of the hypertonic upper trapezius and levator scapulae, unopposed by the inhibited lower trapezius, decreases the midcervical lordosis and impairs normal cervicothoracic joint mechanics.48,49,65,74 Specifically, the compensatory motions of upper thoracic contralateral sidebending and ipsilateral rotation that normally accompany cervical rotation and arm elevation are lost in the presence of forward head posture.48,49
Shoulders
The forward-drawn posturing of the shoulders is associated with shortening of the pectoral muscles.41 ,74 The tight pectorals pull on their humeral and coracoid attachments, causing increased glenohumeral internal rotation and scapular protraction.48 The altered position of the scapulae distorts the course of the suprascapular nerve, placing it at risk for traction injury during upper-extremity movements.40-42 Hypertonicity of the levators, upper trapezii, and scaleni, generated from head and neck deviations, causes malalignment at the shoulder girdle, by elevating the scapulae, clavicles, and upper ribs.42A8,49 These altered anatomic relationships decrease the width of the thoracic inlet, rendering the brachial plexus vulnerable to further compressionYA4,75 Weakness of the scapular stabilizers from compression of the dorsal scapular nerve and brachial plexus trunks, combined with hypertonicity of the shoulder elevators, results in altered scapulohumeral rhythm and impingement during upper-extremity movements at the workstation.43A9 The combination of postural dysfunction and muscle hypertonicity can alter and adversely affect patterns of respiration.75
Elbow
At the elbow, the flexed and adducted typing posture is reinforced from above by humeral internal rotation and scapular elevation, which increase musculotendinous tension on the elbow flexors from their origins. The tension is transmitted to the elbow, . thereby increasing resistance to movement and joint play.38,66 Elbow flex ion also increases the

tension of the fibrous arch that connects the two heads of the flexor carpi ulnaris muscle, which can compress the ulnar nerve.40 The combination of joint-play restriction and sustained flex ion at the elbow decreases the volume within the cubital tunneVD
,43 potentially compressing the ulnar nerve against the retrocondylar groove and causing paresthesias and weakness in the ulnar nerve distribution.40
In the cubital fossa, shearing between the bi-
cipital aponeurosis and pronator teres can lead to median nerve irritation.43
,54 Prolonged contraction of the pronator teres can also cause mechanical compression of the median nerve secondary to static stenosis.40 In our patient population, a positive pronator teres test correlated with paresthesias in the median nerve distribution with prolonged active supination. Paresthesias with prolonged supination further implicates the shortened pronators as a source of median nerve compression.
TABLE 3. Postural Deviations Associated with RSI in Computer Keyboard Users
Muscle Imbalance·
Hypertonic
Extensor digitorum communis
Extensor carpi uInaris / radialis
Pronators
Biceps
Subscapularis Upper trapezius
Levator scapulae
Pectorals
Scalenes Levator scapulae Upper trapezius
Neck extensors Suprahyoids
Suboccipitals
Weak
Intrinsics
Supinators
Triceps
Infraspinatus Lower trapezius Middle trapezius
Rhomboids
Deep neck flexors Infrahyoids
Kinetic Chain
HAND
WRIST
FOREARM
ELBOW
SHOULDER
HEAD
Postural Deviation from Neutral
Extended/abducted thumb Finger zig-zag deformity:
DIP hyperextension PIP flexion MCP hyperextension
Finger splaying Alienated little finger
Ulnar deviation Wrist hyperflexion/hyperextension
Pronation
>90· flexion
Adducted Anterior humeral head Internally rotated
Protracted, elevated, & tipped Winging inferior scapular angle
Elevated first rib Depressed sternum
Upper cervical extension Flattened midcervicallordosis Elevated hyoid
Forward head Craniocervical compression
Injury Potential
De Quervain's disease Trigger finger Tenosynovitis Intrinsic muscle shortening Pisohamate ligament
contracture
Guyon's canal syndrome Carpal tunnel syndrome FCU / extensor tenosynovitis Transcarpalligament contracture Ganglion cysts
Intersection syndrome Pronator teres syndrome Anterior /posterior interosseous
nerve syndrome
Radial tunnel syndrome
Cubital tunnel syndrome Medial/lateral epicondylitis Biceps contracture Thoracic outlet syndrome Bicipital tendinitis/bursitis Postural syndrome63
Acromial impingement Suprascapular nerve entrapment
Costoclavicular syndrome
CT joint dysfunction Suboccipital nerve compression
Anterior / middle scalene syndrome Cervical dysfunction/derangement Cervical radiculopathy Degenerative joint disease
TMJ dysfunction/headaches VISion disturbances / eye strain
NOTES: DIP = distal interphalangeal; PIP = proximal interphalangeal; MCP = metacarpophalangeal; FCU = flexor carpi uInaris; er = cervicothoracic; TMJ = temporomandibular joint. ·Described according to Janda's "upper crossed syndrome"6(H;Z (see text).
January-March 1998 13

The radial nerve and its branches are subject to similar mechanisms of injury.9,40,64,76 Localized compression of the radial nerve may occur between the triceps heads, under the extensor carpi radialis brevis, or in the supinator arcade of Frohse.40,43,64 During keyboard activity, increased traction and frictional forces as well as increased compartment pressures provide the mechanical conditions for neurovascular injury.3,38,58,64
Forearm
The pronated forearm position, combined with elbow flexion, wrist extension, and cyclic finger flexion and extension, creates shearing and compressive forces at several soft-tissue interfaces in the forearm.3,5,8,32,54,59 The pronators and extensor digitorum communis adaptively shorten over time because of prolonged contractions in their most shortened positions.1,27,37,38,59,n Adaptive shortening of the extensor digitorum communis can be objectively measured by comparing active wrist-flexion range of motion with and without fist closure. The nonneutral position of the extended wrist places the finger and wrist extensors at a mechanical disadvantage, requiring more exertion in order to type.2,38
Microtrauma to forearm and wrist musculature from increased force and repetitive motions in deviated postures indicates the inflammatory process leading to tendinitis.§ Lateral epicondylitis is a characteristic finding in our RSI patient population, and careful evaluation distinguishes it from radial tunnel syndrome.40A3,54 Another tendinitis, known as intersection syndrome, may develop in the distal third of the forearm, where the abductor pollicis longus and extensor pollicis brevis cross diagonally over the common wrist extensors.3,59,77 Their oblique course gives rise to frictional forces and subsequent inflammation with repeated thumb motions when the spacebar is struck.8,59,78
The brachioradialis and extensor carpi radialis longus tendons press on the radial sensory nerve in a scissors-like fashion when the forearm is pronated and the wrist is repetitively ulnar deviated.3,8,43,54,59,76 The nerve entrapments restrict the longitudinal sliding potential of the nerve along its entire bed, accentuating the shearing process and causing micro trauma with the movements of computer keying.37,38,53,58,59 As always, the multiple crush phenomenon53,56 may be involved, with local injuries superimposed on brachial plexus or cervical nerve entrapmentsY,42,50,54,57 The clinical presentation and symptomology of nerve compression at multiple levels often occurs in the absence of definitive electrodiagnostic findings.43,44
Wrist and Hand
At the wrist and hand, tendons, synovia, and nerves are at risk from biomechanical stresses,6
§References 1, 3, 6, 8, 27, 37, 38, 40, 59, 76.
14 JOURNAL OF HAND THERAPY
which include rapid repetitive movements from high keystroke rates, forceful movements of keystrike,7-9,12,17,38,52 awkward positioning of the thumb and fifth finger in reaching for function keys/v9 and static loading of the wrist in nonneutral positions of extension, flexion, or ulnar deviation?5,36,38,51 Nonneutral positions subject nerves to prolonged stretch and periods of high pressure.53 The nonneutral positions also place muscles at inefficient length-tension relationships/,32,38 resulting in decreased transmission of contractile forces to the fingers.2,38 With the hand in the position of function, the intrinsic and extrinsic musculature maintains the three-joint system of the digits in balance.78
Conversely, with repetitive keystrike in nonneutral positions-such as striking in intrinsic minus, intrinsic plus, or zigzag collapse postures-the intrinsics can shorten from muscle imbalances. The intrinsic muscles of the hand can also shorten from fibrosis that occurs in the cycle of inflammation, healing, scar tissue formation, and remodeling associated with cumulative microtrauma.5,6,13,36-38,59 In our patient population, we noted a prevalence of positive intrinsic tightness tests.
Wrist angulation in ulnar deviation increases shearing in the first dorsal compartment, predisposing to de Quervain's syndrome.3,5,77 Entrapment of the superficial radial nerve by dorsal forearm muscles may mimic the symptoms associated with de Quervain's.54 Lateral deviation of the fifth finger in reaching for function keys contributes to the problem. Excessive force (i.e., higher than the minimum required for key contact closuref and arc of motion by the thumb in performing the spacebar function predispose to extensor pollicis longus tenosynovitis. Similarly, forceful and repetitive keystrike creates friction in the tendon sheaths, impairs synovial diffusion, and ultimately restricts differential gliding between the superficialis and profundus tendons.80 The force pattern of keystroke, which requires rapid deceleration of the "down'swing" as the key bottoms out, adds to the adverse tendon forces.2o
Wrist motion occurs in conjunction with movement of individual carpal bones?8 The lunate, for example, rotates during palmer flex ion so that it projects into the volar tissues, decreasing volume in the carpal tunnel and subjecting the median nerve to compression.81 Similarly, pronation shifts the carpal tunnel contents adversely toward the median nerve.32 Compression in the carpal tunnel is compounded by an increase in synovial fluid pressure and tendon tension that occurs with forceful and repetitive contraction of the finger flexorS.z°,37,59 Demand for tendon lubrication overwhelms the ability of the sheath to respond. 59 The resulting friction between tendon and sheath precipitates an inflammatory reaction.3,59,80-82 A decreased ability of the carpal tunnel walls to adapt to the changing volume of its contents, under the varying conditions of strain and movement, leads to carpal tunnel syndrome.1,6,8,27,66,81 External me-cllanical pressure at the wrist from leaning on hard surfaces (such as the desk top, chair arms, or wrist rests) can exacerbate the neurovascular compres-

sion.8,12 The multiple-crush syndrome and coexisting disorders are a characteristic clinical finding at the wrist and hand in our RSI patient population.53,54,57 Localized injuries are compounded by proximal nerve entrapments with the characteristic signs of diffuse pain, aching, paresthesias, and weakness.
CLINICAL EVALUATION
Clinical evaluation by the physician and physical and occupational therapists includes patient history, physical examination, and specific tests that are standard components of any thorough neuroorthopedic upper-quadrant assessment.48,78 Assessment of vocational and avocational limitations, as well as a keyboard activity analysis, are essential to the evaluation and treatment planning process.
The physician performs the RSI diagnostic evaluation/,8,32,39,79 ruling out non-work-related medical conditions such as rheumatoid arthritis, diabetes mellitus, fibromyalgia, gout, and hypothyroidism and other hormonal disorders.8,39,89 The medically controversial83 and chronic nature of the RSI syndrome often requires the physician to function as a patient advocate, helping the patient obtain a medical leave from work or mediating judicious work re-entry.8,84 The physician also may be called upon to represent the patient in legal issues and disability determinations.3,84,85
Given the number of diagnoses associated with RSI and the complexity of their interrelationships, the clinical evaluation conducted by the physical therapist (PT) and occupational therapist (OT) requires skillful interpretation of the clinical signs and symptoms. The manual therapy approach to clinical evaluation, pioneered by Maitland,86 serves to identify the structures, functional interrelationships, and predisposing physical factors responsible for the patient's symptoms. Knowledge of work-related risk factors and pathomechanics must be correlated with specific findings of abnormal soft tissue, joint, and nerve mobility. Therapists may find it helpful to refer to sensory charts showing distribution of peripheral nerves, dermatomes, and trigger-point referral areas. Diagrams illustrating the distribution of nerve pathways in the cervical-brachial plexus and potential areas of distal entrapment4.43 are also helpful in leading the therapist to the pathomechanical origins of the clinical presentation and in establishing a hypothesis for treatment.
The manual therapist does not determine treatment strategy on the basis of diagnoses alone, but rather on the positions, movements, and functional activities that affect the clinical signs and symptoms.53,86,87 Manual therapy techniques incorporate "hands-on" mobilization of soft tissues and joints to improve the mechanical relationship and function of the involved structures. 11 Treatment ap-
IIReferences 27, 29, 30, 49, 53, 54, 63, 64, 73, 78, 86, 87.
TABLE 4. Provocative Tests Useful in RSI Evaluation
Upper Limb Tension Tests (ULTTs)50,53,54,89: Specific, sequenced positioning of the shoulder girdle, arm, and head with addition of sensitizing maneuvers to selectively traction peripheral nerves in relation to their adjacent structures. The tests assess mobility of the cervical nerve roots, brachial plexus, median, radial, and ulnar nerves. A limited range of motion and/ or reproduction of the patient's pain/paresthesia pattern is considered indicative of "adverse neural tension."
Thoracic Outlet Tests": For example, Adson's, costoclavicular, and hyperabduction maneuvers; the scalene cramp test; and the Roos three-minute elevated arm exercise test.
Sustained-Position Tests3,?": For example, Phalen's wrist flexion test, Buehler and Thayer's elbow flexion test,"9 combined forearm pronation, wrist flexion, and ulnar deviation.
Nerve Irritability Tests3,90:
For example, Tinel's percussion along nerve pathways and tunnels, vibration threshold and sensibility testing.
Musculotendinous Provocative Tests45,82,92,93: Resisted muscle contraction and passive elongation tests to elicit musculotendinous sources of pain and compression according to tissue differentiation principles; e.g., Finkelstein's test for de Quervain's tenosynovitis,93 resisted forearm pronation, passive elongation of wrist extensors by overpressure to fisted wrist flexion with elbow extension.
proaches limited to localized intervention at the site of symptoms, such as application of iontophoresis to a lateral epicondylitis, fail to address the interplay between distant structures in the kinetic chain. Taking the example of lateral epicondylitis, the clinician must consider that elbow pain can be referred from entrapment of cervical nerve roots, brachial plexus nerve trunks, and the radial nerve40,41,43,53,55 as well as trigger points,45 myofascial restrictions, and joint dysfunctions64
,66 along the kinetic chain. Localized symptoms at the elbow may also result from typing when the attenuation of forces from this "repetitive submaxial loading" activity are not dissipated evenly through the linkages of the upper extremity.3,6,88 Proximal muscle imbalances combined with nonneutral positioning of the upper-extremity joints act together to disrupt the attenuation of forces, resulting in force concentration and microtrauma to the tendons at the elbow.3,37 A hypotheSis-oriented treatment approach addresses the patterns of symptoms and the multiple structures affected along the kinetic chain.48,53,54,64
Provocative Tests
Of the many components of the physical evaluation, provocative tests (Table 489-93) are particularly useful for a number of reasons. The tests objectively reproduce the patient's subjective symptoms and provide insight into the underlying pathomechanics.5o,53,54,86 Unlike subjective pain-assessment tools (e.g., visual analogue scales and questionnaires), the provocative tests enable the clinician to gain specific information on abnormal pain responses to reproducible movements. The tests can be used to reassess a patient's status during the course of treatment and to direct treatment
January-March 1998 15

choices and strategies. Maitland86 originated the term "comparable movement signs" to designate the positions and active, passive, or functional movements that reproduce the patient's symptoms.54,94 The practice of reassessment to guide treatment intervention has been eloquently detailed by Butler53 and is fundamental to a "structure selective" and "multifactorial" approach to effective treatment.
Keyboard Analysis
Analysis of keyboard activity is an essential component of the evaluation. Head, neck, back, shoulder, and upper extremity positioning and movement patterns are observed during keyboard activity, and postural deviations, deficiencies in joint stabilization, nonneutral joint positioning and adverse forces such as excessive keystrike impact are noted.7,71,79 Ideally, the evaluation is performed at the patient's own workstation; however, practical considerations often make it necessary to evaluate the patient at a workstation in the clinic set up for this purpose. Videotaped evaluation of computer keyboard activity and function at the workstation enhances the initial analysis and subsequent reevaluations. Specification of the workstation layout, the character and quantity of work/9 and the patient's work-rest cycle69,84,95,96 provide valuable information for treatment and work re-entry consideration. Table 5 provides an evaluation checklist for workstation setup and technique analysis.
ONE-TO-ONE PHYSICAL THERAPY AND OCCUPATIONAL THERAPY
One-to-one treatment planning for the RSI patient takes into consideration the multiple structures affected along the kinetic chain. The sources of the patient's pain must be differentiated from the site-of-pain perception.53 A hypothesis regarding where the problem originates helps direct the treatment plan. Frequent re-evaluation using the provocative tests will validate and redirect the manual therapist'S treatment.
Patients with RSI rarely seek treatment in the early phase of the condition. This may be because of lack of concern for symptoms that initially subside with rest, denial of the potential disabling progression of the condition39 or, as is often the case, frustration in obtaining a diagnosis, effective treatment, and legitimization of the problem from the medical community. Delay in obtaining treatment may also be attributed to a patient's realistic concern that admission of a work-related injury might jeopardize his or her career. Thus, by the time patients enter treatment, their conditions are often chronic and multilayered. A system of functional grading, based on pain response to specific activity, has been proposed by Fry26 and modified by Lowe.27 It is also important to determine the stability, irritability, or progressive nature of the condition and include this in the grading system.53,86,87
16 JOURNAL OF HAND THERAPY
This, in turn, guides the choice of treatment approach and intensity. For example, more aggressive soft tissue and joint mobilization techniques may be used with a stable condition, whereas in an irritable condition an emphasis on reducing pain and inflammation and the use of nerve mobilization techniques "out of tension" are more appropriate.53,54 In a nonresponsive condition the patient risks permanent neurologic and motor impairment. Referral back to the physician for careful consideration of treatment options, including surgery, is imperative.
Treatment by manual methods is central to one-to-one intervention. Manual therapy treatment techniques include soft-tissue, joint, and nerve mobilization,53,64,86.87 trigger point release,45 postisometric relaxation,66 craniosacral therapy, postural and neuromuscular re-education and muscle energy techniques.65.87 Modalities such as moist heat, ultrasound, electric stimulation, iontophoresis, and ice application are sometimes used in conjunction with manual techniques to reduce inflammation and promote circulation, tissue extensibility, and pain control. Biofeedback is a useful tool in reducing muscle hypertonicity and re-educating efficient movement patterns and postures.97 Surface electrodes are placed, for example, on the patient's upper trapezii and forearm flexors and extensors during keyboard retraining, to provide feedback on adverse muscle tension and co-contraction patterns. The practice of reassessing the patient's status after each treatment is fundamental to monitoring the appropriateness of treatment choices.53.54,86,87
Detailed discussion of treatment techniques and parameters is beyond the scope of this article; however, several general principles are mentioned here.
Muscle Balance
Muscle imbalances, particularly the "upper crossed syndrome" of the shoulder girdle, must be corrected if postural and functional movement reeducation is to be effective.61.65.66 Muscle balancing involves stretching of tight, hypertonic muscles followed by strengthening of weak, hypotonic groupS.65.74 The shoulder elevators, for example, are stretched before the shoulder depressors are strengthened. Multiple positions are used in strengthening, such as sidelying or physioball rolling, particularly if habitual upright movement patterns impair an efficient muscle firing sequence. Strengthening of the hands and forearms is not a focus in the initial phase of a manual therapeutic approach, given the appreciation of the double- and multiple-crush phenomena, since the more distal structures cannot be re-conditioned secondary to proximal neurovascular compromise.4,10,49 When the brachial plexus is entrapped, strengthening in positions with the arms elevated above shoulder level is avoided to Rrevent risk of further plexus injury from traction. 1 Stretching of the scalene muscle "entrappers,,,45 mobilization of joints and soft tissues adjacent to the plexus,M and nerve gliding

TABLE 5.
Fault
Visual Field Monitor positioned to side of keyboard Stationary monitor Screen too high or too low Copy on desk surface Glare from direct and reflected light Overhead fluorescent lights Incorrect focal distance for visual acuity
Posture Head forward Shoulders elevated Scapular winging Hypertonic upper trapezii Shoulder protraction/ internal rotation Elbow flex ion >90° Elbow f1exion <80° Wrist flex ion or extension Elbows locked at sides Wris ts against keyboard or desk edge Wrist extension Wrist ulnar deviation Finger MCP joint hyperextension Fla t of kyphotic back Sta tionary chair back and seat pan
Hips lower than knees
Feet dangling
Keyboard Technique Wrist extensor/flexor cocontraction Wrist ulnar deviation Intrinsic plus keystrike } Intrinsic minus keystrike (zig-zag) Digital extensor habitus Thumb held in horizontal abduction and
extension Excessive force of keystrike Ulnar deviation at wris t and fingers
with lateral key strike Excessive leaning on wrist rests Fifth finger lateral reach and strike Hand splay with combination keystrikes Typing too fast Infrequent breaks/poor work-rest cycles
N OTE: MCP, metacarpophalangeal.
Workstation Setup and Keyboard Technique Checklist
Correction
Monitor directly in front of chair and parallel to keyboard Monitor mounted on adjustable support 10°-15° downward viewing angle to the center of the screen Copy secured along side of monitor Clean antiglare screen (glare filter, angle screen away from window) Task-appropriate lighting Focal distance (eyeglasses) corrected for computer use (i.e., 20" - 24")
Ears aligned with shoulders; chin retracted Shoulder girdle muscle balance Scapulothoracic proximal stability Lower keyboard or desk height Neutral shoulder alignment Keyboard parallel to or slightly below elbow level (i.e., 80°-90° elbow flexion) Keyboard moved closer to minimize reach Height of keyboard or chair adjusted to achieve wrist in position of function* Arms stabilized from scapulothoracic region Hard keyboard or desk edge padded Keyboard positive incline eliminated; flat keyboard or negative incline Re-educate neutral wrist positioning; split keyboard Fingers in position of function Back supports in chair to match individual spinal contours Versatile chair allowing forward, upright, and reclined postures; seat pan inclined
forward with " waterfa ll" edge Seat height raised; seat pan inclined to position hips slightly higher (5°_10°) than
knees Feet £la t on floor or foot rest
Light key-touch; relaxation/biofeedback training Wrist aligned with forearm
Hand postures in position of function
Thumb lightly resting on spacebar; spacebar use with thumb press vs. lift and strike
Keystrike with finger press vs. lift and strike; key strike with arm bounce Wrist aligned with forearm; use of external rotation / abduction at shoulder for lat-
eral key reach Wrist glide vs. wrist rest technique Index finger use for lateral keystrike; slight supination with fifth finger keystrike Combination key command efficiency; macro-program development Kinesthetic awareness training Periodic rest breaks/ task rotation; computer programmed to signal rest breaks
*Position of function: forearm, wrist, and hand aligned, 20°_30° wrist extension, natural curve to digits with MCP joints at about 50° of £lexion, and thumb in line with radius."
"out of tension,,94 are indicated instead. In all instances, nerve gliding and muscle stretching in the upper quarter must be performed carefully, limiting the extent and force of treatment to minimize the risk of exacerbating the patient's symptoms and worsening the condition.s
Mobilization
Mobilization of soft tissues, joints, and nerves reduces excess tension, compression, and frictional forces and restores normal mobility between interfacing tissues and structures.53.5M4 The upperlimb-tension test maneuvers are used to treat mobility problems of peripheral nerves and adjacent soft tissues.53,54 Depending on the degree of nerve irritability, treatment is modulated by the addition or deletion of sensitizing components,53,89,94 such as cervical lateral flexion. Increased tension on the
nervous system is associated with forward head posture.53 Accessory joint motion (e.g., radioulnar, carpal bones) and soft tissue mobility (e.g., differential gliding of the flexor digitorum profundus and superficialis)98 must be restored before the patient can be expected to achieve correct postural alignment and keyboard technique. Improvement in joint function, soft tissue extensibility, muscle tonus, and nerve mobility resulting from mobilization techniques increases the neuromuscular adaptive potential to mechanical stress and thereby reduces the possibility of re-injury.53.54.87
Postural Retraining
Restoring proximal stabilization of the trunk, shoulder girdle, and scapulothoracic muscles is a critical component of movement re-education for the RSI patient. Proximal stability is then carried
January-March 1998 17

over into functional, postural, and technique retraining.54.66.87 Postural and technique retraining is based on principles of neutral joint alignment and proximal stabilization for distal mobility.27.74.87 Utilization of neutral joint positioning during performance of therapeutic exercise and keyboarding tasks is a dynamic adaptation.
The initial phase of retraining develops an awareness of head and trunk plumbline alignment and wrist and shoulder neutral positioning. The neutral wrist position is demonstrated by letting the arm hang by the side such that it is not flexed, hyperextended, or deviated side-to-side.5.32 Movement dynamics are then added such that the patient performs the exercises and tasks utilizing neutral alignment as the starting and ending points. If posture is taught statically, instead of dynamically, with plumbline alignment as a constant, the carryover into function will be extremely limited and the patient is likely to develop myofascial pain and trigger points in response to the overstrain of prolonged rigid posture.45.63.66
Preventive Education
Instruction in adapted activities of daily living (ADLs), pacing strategies, and home/workplace exercises are components of preventive education. The multidisciplinary group treatment approach described below provides a framework for efficient delivery of additional patient education material.
GROUP TREATMENT THEORY
The authors developed a multidisciplinary group treatment approach after observing that the RSI syndrome results from a complex interaction of extrinsic, work-related demands and intrinsic, physical and psychologic characteristics. The group format offers an efficient means of addressing all these factors as well as obvious advantages over one-to-one treatment in terms of cost containment, patient load management, and dissemination of information. The multidisciplinary team comprises the referring physician, OT, PT, psychotherapist, and keyboard retraining specialist.
Studies on the benefits of the group approach emphasize that the group process can be a vehicle to teach patients to take control of their own health.99
•lOo Feurstein et al.25 reported that for pa
tients with chronic work-related upper-extremity disorders, psychologic interventions directed at changes in attitudes and health behaviors, coupled with physical conditioning and safe work practices, may contribute to a greater sense of control over pain and distress, which in turn increases returnto-work potential.
In planning the RSI teaching and feedback process, the therapists subscribed to Yalom's group process modePOl and the theory of self-efficacy described by Bandura.102 Although Yalom described 11 elemental factors in the therapeutic process, the
18 JOURNAL OF HAND THERAPY
therapists adopted only five factors into our timelimited group process; namely, the imparting of information, catharsis, universality, instillation of hope, and imitative behavior. Yalom asserts that the therapeutic factors operate in every type of therapy group but their interplay and differential importance may vary widely from group to group. The remaining six factors-altruism, recapitulation of the primary family group, development of socializing techniques, interpersonal learning, group cohesiveness, and existential factors-are more relevant to long-term therapy groups.
A planned sequence of teaching and guided interaction was developed to provide support in the recovery process and validation for a disorder that is not readily recognized in the medical community. A commonality among our RSI patients was their lack of knowledge about the etiology of RSI; therefore, the introductory session was designed to impart this information. In the initial group meeting to explore the psycho logic dimensions of RSI, bridges were made between the participants by sharing their early histories of diagnosis. Sharing of their stories led to a reduction in feelings of isolation and pent-up frustration. The cathartic ventilation of anger that was accepted and understood by group members led to identification with one another. The group offered problem-solving techniques for managing anger and depression. Examples included learning to express negative feelings in the work environment before feelings led to acting out, and using exercise as a constructive release to counter depression. Continuing contact with group members and therapists in the protracted recovery process provided an instillation of hope.
Bandura 102 states that perceived self-efficacy is the cognitive process by which an individual judges his or her ability (self-efficacy expectations) to learn the behavior required to produce predefined outcomes. Perceived self-efficacy has been found to influence psychologic well-being and to be a significant predictor of the individual's likelihood of actually performing the learned skills and behaviors once outside the supervised clinic setting.103 Bandura argues that individuals with low confidence in their self-efficacy are severely limited in the acquisition process. Conversely, individuals with strong efficacy expectations will persevere in the face of adversity, because they believe that they will ultimately achieve their desired outcome.103
The most effective means of enhancing perceived self-efficacy of group members is through performance-based activities102.103 or imitative behavior. 101 Therefore, the minimal behavioral expectation of the RSI group members was to demonstrate compliance by accurately performing prescribed preventive exercises. Participants were taught a specific set of RSI-preventive exercises (e.g., eye exercises; diaphragmatic breathing; neck, shoulder, and forearm stretches; nerve-gliding sequences; postural dynamics; and scapulothoracic str~ngthening) and were observed for competency in their performance during each of the five group sessions.

Group Admission Criteria
Group admission criteria were established to facilitate selection of a homogeneous group of patients. Minimizing the variables patients bring to a group can expedite the interactional group therapy process. The admission criteria are aimed at identifying RSI patients with mild signs and excluding severely involved patients who would derive more benefit initially from one-to-one intervention. The criteria are based on functional capacity rather than normal grades of range of motion (ROM), sensation, and dynamometer measurements. For those patients who do not meet the group admission criteria, one-to-one "pre-group" treatment is indicated. The objective of one-to-one treatment is to improve the patient's neuromuscular function, ROM, and pain threshold to a level where active exercise can be tolerated and the patient can utilize the information and "self-help" strategies presented in the group. In addition to physical criteria, patients must also be psychosocially able to engage in a group process.
The group admission criteria are as follows:
• Recent onset of RSI symptoms (six months maximum) for patients with a keyboard-intensive occupation,
• Referral to the group by a physician after ruling out cervical disc herniation, adhesive capsulitis, and post-traumatic shoulder subluxation/ dislocation,
• Psychosocial ability to engage in group process (e.g., severe clinical depression ruled out by the psychotherapist), and
• A minimal typing/writing activity tolerance of ten minutes.
One or more of the following criteria must also be met:
• No less than 40° active ROM of wrist flexion with fist and wrist extension without fist,
• Diminished light touch sensation of not less than 3.61 on the Semmes-Weinstein monofilament test/I
• Grip weakness on dynamometer testing of not less than 25% of average values based on normative studies lO4 (approximately 100 lbs. for men and 60 Ibs. for women),
• Decreased scapulothoracic and shoulder mobility (e.g., restricted Apley's scratch test) but within functional limits for performance of active exercise,
• Ability to perform active exercise of upper extremities, shoulders, and neck within a tolerable pain threshold, and
• Freedom from pain at rest and/ or level 3 maximal pain rating on the Fry pain scale.26
,27
The Fry pain scale is a functional grading system based on pain experienced during and after a specific activity.26
,27 The five-level scale was originally developed for musicians in relation to playing
an instrument. For our patient population, pain was graded in relation to typing at the keyboard. Grade 3, for example, represents pain in multiple sites that progresses while typing and persists for a short period even after the typing has ceased. Grade 2 indicates that there is pain in one site during typing, which stops when typing is stopped. The most severe grade is 5, in which there is continuous pain that prevents typing and most other uses of the hands.
Multidisciplinary Group Process
The goal of the group approach is to provide patients with education and strategies for selfmanagement of their condition in a supportive environment. This goal incorporates educational, behavioral, and psychologic objectives to help participants achieve a more informed, active, and hopeful stance in the recovery process.
The principles for self-management of RSI are presented in five weekly 90-minute group sessions. Groups are limited to ten participants to facilitate peer interaction, and they range in size from six to ten members. The group sessions are led by a multidisciplinary team consisting of an OT, PT, psychotherapist, and technique retraining specialist. Each of the five sessions has a specific agenda to ensure that the group process is directive and not simply a forum for emotional venting. The PT and OT attend all five sessions to provide continuity and reinforce the physical principles underlying the concepts presented by the other group leaders.
The first and third group sessions are cotaught by the OT and PT and cover basic functional anatomy and pathomechanics, principles of neutral joint alignment and dynamic posture, adaptive products for home and workstation modification, and pain management and pacing strategies. The first session, like all subsequent sessions, includes instruction and refinement of group performance of specific stretching, nerve-gliding, muscle-balancing, and postural exercises. The second and fifth sessions are led by the psychotherapist and explore the emotional response to injury, issues of self-esteem (e.g., the need to expand one's definition of self beyond work roles), and strategies to cope with and gain control over the condition. Reiteration of information on pain management, pacing, and protective exercise by the OT and PT contributes to development of practical coping strategies. The fourth session, conducted by the retraining specialist, elaborates on postural principles, adaptive equipment, workstation setup, and specific methods for improving keyboard technique. In this session, factors that precipitate RSI (e.g., force, repetitive motion, poor posture, and lack of rest) are explored more closely in relation to the task of typing at the workstation.
Sessions are sequenced to build practical information and individual solutions on a knowledge base of RSL-related anatomy and pathomechanics. At the completion of the five sessions, patients fill
January-March 1998 19

out feedback questionnaires, which are later reviewed by the group leaders. The sequencing of the sessions remains constant for all groups; however, content may vary in response to the feedback questionnaires and the particular concerns raised by participants in the different groups. The group format combines didactic instruction, demonstration, and directed group discussion with active participation in evaluations, exercise, and retraining labs.
Throughout the five sessions, the principles presented, all beginning with the letter P, are postural retraining, protective exercise, pain management, positioning, products, pacing, and psychologic strategies. The concept of the "seven Ps" was developed by the authors as a mnemonic to help patients organize the information for easy recall and to highlight the multifactorial nature of RSI recovery. These principles, which are meant to be integrated into daily life, are also reinforced in oneto-one therapy sessions.
The Seven Ps
Postural Retraining. Postural retraining is achieved through muscle balancing and body awareness exercises. Maintenance of the normal spinal curves and plumbline alignment, in which the weight of the head and trunk are vertically aligned over the base of support, is fundamental. Also emphasized is the concept of dynamic posture, in which the body constantly adapts to task demands promoting circulation, joint nutrition, and efficiency of movement. In layman's terms it is explained how malaligned posture, especially forward head and shoulders, subjects capsuloligamentous systems to static overload, fatigue, strain, and compression. Patients learn to utilize movement strategies and cues from the environment to modify posture and promote safe positioning.
Protective Exercise. Protective exercises maintain the correct muscle balance for dynamic posture. The exercises focus on stretching habitually tight, hypertonic muscle groups and strengthening selected proximal, scapulothoracic stabilizers to provide stability for distal fine motor activities and keyboarding. Specific auto-mobilization, nerve, and muscle-tendon stretching sequences are taught. Explanation of the pathomechanical processes of inflammation, scar tissue formation, and nerve entrapment reinforce patient compliance with the home and workplace exercise program. Patients' resistance to exercise-stemming from feelings of hopelessness and anxiety about the future, fear of engendering more pain, or reluctance to draw attention to the injury-are explored with the psychotherapist in the group process.
The sedentary nature of a predominantly computer-based occupation contributes to physical deconditioning and weight gain. Patients are encouraged to commit to a regular walking program outdoors or on a treadmill. Explaining the beneficial effects of cardiovascular conditioning and weight reduction on RSI symptoms supports patients' commitment to a conditioning regime. Car-
20 JOURNAL OF HAND THERAPY
diovascular conditioning activities that require gripping with the hands, such as bicycling, use of handheld weights, or use of the upper body ergometer, can perpetuate overuse and are not advocated.
Pain Management Techniques. Demystifying the sequelae of repetitive strain provides the patients with a framework to interpret and select the appropriate pain management techniques. The benefits of heat, cold, contrast baths, postural adjustment, stretch, exercise, and rest are explored in the group process. The injurious effects of immobilization from prolonged wrist-splint usage are discussed. Splints are advocated only for maintenance of neutral wrist positioning during sleep or retraining exercises. Discussion of participants' individual measurements in clinical tests-such as the Apley's scratch test, wrist flex ion active ROM with and without fist closure, and dynamometer grip strength - helps the participants look to objective signs of improvement rather than focusing on pain.
The psychosocial ramifications of pain in regard to role expectations and interpersonal communication are addressed by the psychotherapist. The reduction of mobility and continuous pain has far-ranging effects on the patient's role in his or her family as well as at work. Learning to delegate responsibility and inform superiors, coworkers, and significant others of the physical limitations and changes that are necessary during the recovery period gives power to the patient and reduces confusion and resentment. The group members offer support in managing resentment of co workers when the patient has a diminished work load. At home, patients are encouraged to discuss with their significant other how painful it is emotionally to have to accept help and not pull one's load. The tendency is to withdraw and not bring attention to the problem. Assertion when one feels ashamed feels paradoxic. The group supports assertion. The therapist helps each patient examine the definition of self and rethink values during this time of reduced capacity. Group members share strategies and advice on how to regain a sense of strength in the family and at work. Original, creative solutions emerge from suggestions in the group.
Positioning. Positioning refers to the relationship of the body to the workstation. Principles of correct keyboard technique and workstation setup are presented by the retraining specialist. The concept of using a wrist rest as a guide to glide the wrists along instead of a support to lean on is explained. Excessive leaning on a wrist rest, arm rest, or the edge of a desk encourages weight-bearing on the vulnerable carpal tunnel. Of even greater concern, leaning on wrist or forearm rests to support the trunk draws the body forward, encouraging a forward head, rounded shoulders, and kyphotic posture. This poor posture decreases the width of the thoracic inlet,48.75 with potential compression of the brachial plexus and subclavian vessels. The additive effects of proximal and distal nerve compression from misuse of wrist or forearm rests can contribute to multiple crush. By anchoring the arms in a static position, excessive leaning also encour-

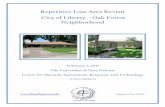
FIGURE 1. Alignment at the workstation. (Copyright 1992 Time Inc. Reprinted by permission.)
HEAD Directly over shoulders. without straining forward or backward. about an arm's length from screen.
NECK Elongated and relaxed
SHOULDERS Kept down. with the chest open and wide.
BACK Upright or inclined slightly forward from the hips. Maintain the slight natural curve of the lower back.
ELBOWS Relaxed. at about a nght angle.
WRISTS Relaxed and In a neutral posItion. without fleXing up or down
KNEES Slightly lower than the hips.
CHAIR Sloped slightly forward to facIlitate proper knee posItion.
ages incorrect keyboarding technique, which isolates the movements of typing and keyreach to the wrist and fingers without appropriate involvement of the upper extremity and proximal scapulothoracic muscles. Patients are taught to maintain a "V" relationship of the forearms (apexed at the finger tips with elbows lateral to wrists) while typing at the keyboard. They are taught to stabilize the upper extremity proximally from the scapulothoracic region and allow the shoulders to rotate and abduct actively, externally and internally. Scapular stability combined with shoulder mobility assists correct movement of the hands across the keyboard without repetitive deviations from the vulnerable wrist or splaying of the fingers. Exercises for reconditioning the scapulothoracic muscles are reviewed by the OT and PT to reinforce efficient function at the workstation. Neutral positioning of the wrist-in which the midline of the fingers and hand are aligned with the midline of the wrist and forearm -is taught as the "home base" for typing.
Patients are instructed in a progression of computer typing skills and tension-reduction strategies that promote biomechanical efficiency. Strategies to avoid multikey and repeat commands in editing and other such repetitive operations are taught. An eye examination and adjustment of corrective lenses for computer screen distance (20" - 24") is recommended, as incorrect focal distance contributes to eye strain and forward head posture. The emphasis is on identifying and modifying risk factors and technique faults that predispose to keyboardrelated injury. The most common faults in posture, joint alignment, force distribution, and fingering are listed in Table 5. The checklist is intended to highlight specific faults; it does not, however, convey the importance of movement dynamics and kinesthetic awareness in keyboard retraining.
Workstation setup includes consideration of the spatial relationship of the desk, keyboard, screen, and chair to each other and to the user. Figure 1, which is used as a teaching tool in the
KEYBOARD
SCREEN At eye level or shghtly lower.
FINGERS Gently curved.
Best when kept flat (for proper wrist positioning) and at or Just below elbow level. Computer keys that are far away should be reached by moving the entire arm. starting from the shoulders. rather than by twisting the wrists or straining the fingers. Take frequent rest breaks.
FE£T Firmly planted on the floor. Shorter people may need a footrest.
SoUft! Mllle,lnslrlule 51 lu ·s·Roosevell HOSPItal
groups, diagrams these considerations. Desk height should enable the elbows to function in an 800 -900
range of flexion without shoulder elevation. The keyboard should be at the same level as the elbows or slightly below them. The screen should be directly in front of the user and 20" - 24" from the eyes, at the optimal focal distance for the individual user. The top of the screen should be even with the top of the head, permitting a 10°-150 viewing angle to the center of the screen. Chair height should position the knees at a 90°-95° angle, with the hips slightly higher than the knees. The backrest should permit a supported upright trunk position during typing and a more reclined posture during rest breaks. The feet should be flat on the floor or foot rest. 1
,5,1U2,35,51 Additional considerations are outlined in Table 5.
Principles for correct positioning are generalized to other ADLs. Patients are encouraged to hold the automobile steering wheel in a 5- and 7-0'clock position, because vascular perfusion of the median nerve is decreased when elevation is superimposed on the clenched fist position. Patients are advised to avoid sleeping on the upper arm or forearm or in the fetal position, to prevent neurovascular compression. The intrinsic-plus grasp, as in holding a book or in writing, can cause the proximal origin of the lumbricals to occupy the distal end of the carpal tunnel; therefore, patients are instructed to relax the fingers into a flexed position during these activities.
Products. Adaptive products are introduced for the patient to select and integrate into daily life. These products are intended to simplify common activities and make them less stressful. Grip and pinch strengths are typically below average in RSI patieI\ts. Selection of a rolling ball pen and buildup of the pen with a pressure-absorbing, high-friction grip can, for example, reduce the muscle energy expenditure for pen retention. Key and doorknob extensions eliminate forearm, wrist, and digit torque requirements and transfer the mechanical advan-
January- March 1998 21

tage to stronger, more proximal muscles. Many activities can be modified by use of commercially available products to reduce prehension overuse patterns in the workplace and the home (e.g., rubber-tipped telephone dialers and page turners, electric staplers). Low-profile, portable products such as an incline seat cushion, wrist rest, collapsible foot rest, telephone headset, copy holder, and screen glare filter are also available and assist in adapting a keyboard workstation.
Patients are instructed in the correct application of these products to reduce postural strain from awkward positions or reaching beyond the primary work zone. The incline seat cushion, for example, reduces posterior tilt of the pelvis and concomitant flexion of the lumbar spine. By raising the pelvis 50_100 above the level of the knees, the incline seat cushion also shifts weight-bearing from the ischial tuberosities to a more even, tripod distribution shared between the femurs and feet. 51 The telephone headset eliminates the need to cradle the phone between an elevated shoulder and sidebent neck when the hands are engaged at the keyboard. The telephone should be within easy reach for dialing. The copy holder supports documents at a comfortable reading angle, reducing awkward head and neck postures. Wrist rests serve several purposes. They cushion the forearms against hard edges, provide surfaces to glide the wrists along, and elevate the forearms to minimize wrist extension in typing. Creative solutions for reducing manual strain and repetitiveness in daily tasks are elicited in the group process.
Pacing. Pacing principles are extrapolated from the arthritis self-management doctrines of joint protection and energy conservation. The principle of work-rest balance is based on studies demonstratin~ oxygen debe and decreased synovial diffusion 0 in overused soft tissue and the detrimental potential for deformation of tissues. Participants in the RSI group are instructed to determine their typing activity tolerance and then reduce that activity duration by 10%. Additionally, participants are instructed to use activity rotation, exercise, stretching, and relaxation techniques as breaks from repetitive keyboarding. While pacing may initially decrease productivity, ultimately it is found to increase productivity by reducing performance decrements that result from eye strain and musculoskeletal fatigue at the computer workstation.105
Psychologic Strategies. Discussion of the psychologic dimensions of RSI is led by the team psychotherapist. In the initial group meeting bridges are made between the participants by sharing their early histories of diagnosis. Inevitably many have worked through pain and denied the significance of their bodies' discomfort. Early difficulties in legitimizing the problem within the medical community have elicited frustration and anger. When a patient is finally diagnosed with RSI-a condition without a definitive treatment and no promise of recovery to full work potential -the denial and confusion move into fear and anxiety. The treatment team is faced with individuals
22 JOURNAL OF HAND THERAPY
with chronic pain who seem to have moved into a dependent position relying on the medical team to cure them.
The sharing of their stories and the ventilating of anger and hopelessness help foster identification within the group. The catharsis and identification enables the group members to acknowledge their sense of anxiety about the future. Guided by the psychotherapist, the despair expressed by group members is connected to fear of outcome, paving the way for exploration of personal and professional role expectations. Education about the nonlinear nature of RSI recovery, characterized by improvements, plateaus, and setbacks, is described for the purpose of shifting focus from the frustration of unpredictable fluctuations to gaining control over symptoms by using strategies of pain management.
Offering an accepting environment within which patients can struggle to gain some autonomy creates a "reality check" on isolation, rage, and despair. Individuals in the group share strategies on how to manage at work and advice on how to handle self-esteem issues. They also regain a sense of strength in the family, where one has suddenly become a "patient," and perhaps most importantly they learn tricks to manage the many indignities of the problem, such as not being able to shake hands, open doors, or drive. Many of the group members are Type A personalities, who have prided themselves on how hard they work and what they have achieved. Within the group they face a reality that they now must consider other aspects and values in life during a period when their sense of identity cannot come from work. By facilitating the strong work ethic within the group, the leaders' goals are to transfer this shared value into the work of recovering as a proactive individual and help group members regain a missing sense of self-efficacy. These goals have been achieved, according to a pilot outcome analysis of individuals treated at the Miller Institute.
Feedback Analysis
Over a period of two years, eight groups of patients participated in the five-session multidisciplinary intervention. Feedback questionnaires were distributed to the patients after the last session of each group. Of the 47 questionnaires distributed, 36 were returned immediately or by mail. The questionnaire (Table 6) included a self-report scale to rate the usefulness of the topics presented, as well as open-ended questions intended to elicit statements regarding perceived self-efficacy. Questionnaires do not provide objective outcome measures like ROM measurements or provocative test results; however, self-report has been demonstrated to be accurate. 106
One educational objective of the group process-to demystify the etiology of RSI-appeared t-o be successfully met; 99% of respondents rated as highly useful the anatomy instruction and presentation on the contributing factors to RSI. Other ed-

ucational topics correlated with the seven principles of RSI management. Responses on the topics of postural awareness and neutral joint positioning confirmed participants' appreciation of the importance of postural retraining: 100% of the respondents rated this information as highly useful.
Group participants' feedback on the topics of pain management and positioning indicated that 75% found the information useful, whereas 25% felt they needed further instruction. Within the pain management topic, the subcategory of adaptive devices was unanimously rated as highly useful. Ninety-eight percent of the participants responded that information on pacing techniques was useful, with 2% requesting further elaboration, specifically on activity tolerance determination. On the topic of psycho logic aspects of RSI, 13% requested further information on how self-esteem and identification of workplace stressors could affect their health.
The behavioral objective of the group process was the accurate performance of a specific set of RSI preventive exercises and postural modifications. Exercises were introduced, performed, and corrected over the course of the five group sessions, and all the participants were observed to have
TABLE 6. Multidisciplinary Group Intervention Feedback Questionnaire
Please complete this feedback form so that we can continue to improve our RSI groups. Rating scale: 3 = highly useful; 2 = useful; 1 = need further instruction or information; 0 = not applicable.
Educational topics Anatomy Contributing factors to RSI Postural awareness Concept of neutral joint positioning
Instructional topics Stretching/ strengthening exercises Postural alignment exercise
Pain management Use of heat/ cold Splint usage Adaptive devices
Positioning/Technique Retraining Daily activities Workstation modifications Keyboard retraining concepts
Pacing techniques Importance of rest/exercise breaks Timing of breaks Determination of activity tolerance
Psychological aspects Self-esteem issues Coping with external factors Identifying workplace stressors
Please comment on the following: What aspects of the group were particularly helpful to you? Do you feel you have gained increased control and coping strategies for your RSI? Suggestions for improving the group content?
achieved the behavioral objective of performing them correctly. According to Bandura,102 successful performance can positively influence group members to raise their self-efficacy expectations, increasing the likelihood of continuing a health-promoting behavior outside the supervised clinic setting. Thirty-five of the 36 questionnaire respondents rated the stretching, strengthening, and postural alignment exercises as useful. Only one participant indicated that further information was needed, specifically on strengthening exercises.
Achievement of the psychologic objective of enhancing perceived self-efficacy was reflected in the subjective comments section of the questionnaire. For the majority of respondents, recurrent themes in subjective comments implied increased confidence in their own ability to manage the condition (statements of self-efficacy), underscoring the therapeutic benefit of the group process. In response to the question, "00 you feel you have gained increased control and coping strategies?," 85% responded affirmatively. Most striking was the number of positive comments that referred to the emotional benefit of meeting other people with similar struggles and health concerns, exemplifying Bandura's observation of the value of catharsis and universality in the group process.102
CONCLUSIONS
In treating the RSI patient it is critical to address all the structures affected along the kinetic chain-from the hand and upper extremity to the shoulders, back, and neck-as well as to analyze the postural, temporal, mechanical, ergonomic, and psychologic factors that contribute to the disturbance in function. Treatment approaches that are dependent on a single diagnosis and limited to localized intervention at the site of symptoms will fail to address the interplay between distant structures and the pathomechanics of symptom generationthe hallmark of complex conditions such as RSI.
The intention of this paper is to provide the clinician with an appreciation of the role of postural deviation in the pathogenesis of RSI and the dynamic interrelationship of the diverse neurovascular and musculoskeletal components of the condition. A composite profile of the characteristic clinical presentation of a computer keyboard-injured RSI patient, unified by the common denominators of postural deviation, muscle imbalance, and nerve entrapment, is offered to counter the conception of RSI as a random grouping of diverse diagnostic entities. Psychologic commonalities are presented to complete the profile. Treatment principles for individual and group intervention are offered as practical guidelines for addressing this condition.
The authors have developed this multidisciplinary model of treatment as a result of observing that the RSI syndrome results from a complex interaction of extrinsic, work-related demands and intrinsic, physical, and psycho logic characteristics. The treatment team, consisting of a physician, er-
January-March 1998 23

gonomist, psychotherapist, PT, and OT, collaborates to help patients recognize and modify these extrinsic and intrinsic causes of injury. The goal of treatment is to restore function and prevent re-injury by giving patients strategies for self-management and increased control over their condition. Outcome analysis of the group intervention, based on a simple feedback questionnaire, has offered a preliminary indication of the therapeutic benefit of the group processes and the usefulness of the information presented as perceived by group participants.
Although clinical experience and theory support the treatment principles and kinetic chain model of RSI presented in this paper, the validity of this hypothesis based on treatment outcome remains to be tested. Clearly, more sophisticated tools and objective measures are needed to determine functional outcomes of the multidisciplinary intervention. Outcome variables might include specific provocative test results, modifications in posture and keyboard technique, typing tolerance, and perceived self-efficacy. Followup studies are needed to determine the effectiveness of manual therapy and multidisciplinary intervention on the long-term reduction of symptoms, resumption of lifestyle, return-to-work capacity, and the relationship of perceived self-efficacy to long-term adherence to health-promoting behaviors.
Acknow ledgments
The authors thank John Kella, PhD, for his invaluable contribution to the group intervention and development of keyboard retraining methods and workstation adaptations; the patients and staff of the Miller Institute, Westside Dance Physical Therapy, and Hudson River Hand Rehabilitation; and Christine Bratton, for skillful editing of this manuscript.
REFERENCES
1. Williams R, Westmorland M: Occupational cumulative trauma disorders of the upper extremity. Am J Occup Ther. 1994; 48(5):411-20.
2. Putz-Anderson V (ed): Cumulative Trauma Disorders: A Manual for Musculoskeletal Diseases of the Upper Limbs. Bristol, PA: Taylor & Francis, 1988.
3. Eversmann W: DiagnOSiS of cumulative trauma disorders. In: Advances in Operative Orthopedics, I. St. Louis, MO: c.v. Mosby, 1993:227-42.
4. Mosley LH, Kalafut RM, Levinson PD, Mokris SA: Cumulative trauma disorders and compression neuropathies of the upper extremities. In: Kasdan ML (ed.): Occupational Hand and Upper Extremity Injuries and Diseases. Philadelphia, PA: Hanley & Belfus, 1991:353-402.
5. Armstrong TJ: Ergonomics and cumulative trauma disorders of the hand and wrist. In: Hunter JM, Schneider LH, Mackin EJ, Callahan AD (eds.): Rehabilitation of the Hand. 2nd ed. St. Louis, MO: c.v. Mosby, 1984:1175-91.
6. Armstrong TJ, Fine LJ, Goldstein SA, Lifshitz YR, Silverstein BA: Ergonomic considerations in hand and wrist tendonitis. J Hand Surg. 1987;12A:830-7.
7. Rempel D, Gerson J, Armstrong T, Foulke J, Martin B: Fingertip forces while using three different keyboards. In: Proceedings of the 35th Annual Meeting of the Human Factors Society, 1991.
8. Rempel 0, Harrison R, Barnhart S: Work-related cumulative trauma disorders of the upper extremity (special communication). JAMA. 1992;267(6):838-42.
24 JOURNAL OF HAND THERAPY
9. Feldman R, Goldman R, Keyserling W: Classical syndromes in occupational medicine: peripheral nerve entrapment syndromes and ergonomic factors. Am J Ind Med. 1983;4:661-81.
10. Parker KG, Inbus HR: Cumulative Trauma Disorders. Current Issues and Ergonomic Solutions: A Systems Approach. Boca Raton, FL: Lewis Publishers/CRC Press, 1992.
11 . Joseph BS, Bloswick DS: Ergonomic considerations and job design. In: Kasdan ML (ed.): Occupational Hand and Upper Extremity Injuries and Diseases. Philadelphia, PA: Hanley & Belfus 1991:539-67.
12. Keyserling WM, Armstrong TJ, Pun nett L: Ergonomic job analysis: a structured approach for identifying risk factors associated with overexertion injuries and disorders. Appl Occup Environ Hygiene. 1991;6:353-63.
13. Mackinnon S, Novak C: Repetitive strain in the workplace. J Hand Surg. 1977;22A(I):2-18.
14. Bureau of Labor Statistics: Survey of occupational injuries and illnesses by selected characteristics. Washington, DC: US. Department of Labor, 1994. Publication no. USDL94-213.
15. Fine LJ, Silverstein BA, Armstrong TJ, et al.: Detection of cumulative trauma disorders of the upper extremities in the workplace. J Occup Med. 1986;28(8):674-8.
16. Horowitz, JM: Crippled by computers. Time MagaZine. 1992 Oct 12:70-2.
17. Bammer G: How technologic change can increase the risk of repetitive motion injuries. Semin Occup Med. 1987;2: 25-31.
18. Strause S: Cumulative trauma disorders in the workplace. Am Occup Ther Assoc. June 1995;9(2). Special interest section newsletter.
19. Banham R: The new risk in ergonomic solutions. Risk Management. 1994;41(5):22-30.
20. Dennerlain JT, Serina ER, Mote CD, Rempel D: Fingertip kinematics and forces during typing. In: Proceedings of the 17th Annual Meeting of the American Society of Biomechanics, 1993.
21. Leavitt SB, Taslitz NJ: Computer-related injuries: legal and design issues, I: Designing healthier computerized offices. Managing Office Technology [newsletter]. 1993.
22. Wolkomir R: When the work you do ends up costing you an arm and a leg. Smithsonian. 1994;6:90-101.
23. Heilbronner DL: The handling of an epidemic. Working Woman. 1993;2:60-5.
24. Freudenheim M: Costs soar for on the job injuries. The New York Times. 1991 April 11:05-6.
25. Feurstein M, Callan-Harris S, Kickey P, Dyer D, Armbruster W, Carosella AM: Multidisciplinary rehabilitation of chronic work-related upper extremity disorders. J Occup Med. 1993;35(4):396-403.
26. Fry HJ: Incidence of overuse syndrome in the symphony orchestra. Med Probl Perform Art. 1986;1:51-5.
27. Lowe C: Treatment of tendinitis, tenosynovitis and other cumulative trauma disorders of musicians' forearms, wrists and hands: restoring function with hand therapy. J Hand Ther. 1992;5:84-90.
28. Lederman R, Calabrese L: Overuse syndromes in instrumentalists. Med Probl Perform Art. 1986;3:7-11.
29. Molnar M: Rehabilitation of the injured dancer. In: Ryan A, Stephens R (eds.): Dance Medicine: A Comprehensive Guide. Chicago, IL: Pluribus Press, 1987:302-19.
30. Marshall P: The rehabilitation of overuse foot injuries in athletes and dancers. Clin Sports Med. 1988;7(1):175-91.
31. Hamilton L, Hamilton W: Classical ballet: balancing the costs of artistry and athleticism. Med Probl Perform Art. 1991;6:39 -44.
32. Markison RE: Treatment of musical hands: redesign of the interface. In: Amadio PC (ed.): Hand Injuries in Sports and Performing Arts. Hand Clin. 1990;6(3):525-42.
33. Keller K, West JC: Functional movement impairment in dancers. J Back Musculoskel Rehab. 1995;5:219-33.
34. Berardi G: Technique and the physics of dance. Kines Med Dance. 1991;13(2):25-34.
35. Armstrong TJ: Ergonomics and cumulative trauma disorders. Hand Cl in. 1986;2(3):553-65.
36. Armstrong T, Chaffin D: An investigation of the relationship between displacements of the finger and wrist joints

and extrinsic finger flexor tendons. J Biomech. 1978;11: 229-38.
37. Gross MT: Chronic tendinitis: pathomechanics of injury, factors affecting the healing response and treatment. J Orthop Sports Phys Ther. 1992;16(6):248-6l.
38. Kiser DM: Physiological and biomechanical factors for understanding repetitive motion injuries. Semin Occup Med. 1987;2(7):11-7.
39. Keith MW: Medical management of cumulative trauma disorders. In: Proceedings of the 14th Annual Meeting of the American Society of Hand Therapists, 1991:1-9.
40. Pecina M, Krmpotic-Nemanic J, Markiewitz A: Tunnel Syndromes. Boca Raton, FL: CRC Press, 1993.
41. Schwartzman RJ: Brachial plexus traction injuries. Hand Clin. 1991;7(3):547-56.
42. Pratt NE: Neurovascular entrapment in the regions of the shoulder and posterior triangle of the neck. Phys Ther. 1986;66(12):1894-9.
43. Vennix MJ, Werstsch JJ: Entrapment neuropathies about the elbow. J Back Musculoskel Rehabil. 1994;4(1):31-43.
44. Howell JW: Evaluation and management of thoracic outlet syndrome. In: Donatelli R (ed.): Clinics in Physical Therapy: Physical Therapy of the Shoulder. 2nd ed. New York: Churchill-Livingstone, 1991:151-91.
45. Travell JG, Si mons DG: Myofascial Pain and Dysfunction. The Trigger Point Manual: The Upper Extremities. Baltimore, MD: Williams & Wilkins, 1983.
46. Muffly-Elsey D, Flinn-Wagner S: Proposed screening tool for the detection of cumulative trauma disorders of the upper extremity. J Hand Surg. 1987;12A:931-85.
47. Donatelli R, Wilkes S: Lower kinetic chain and human gait. J Back Musculoskel Rehabil. 1992;2(4):1-1l.
48. Greenfield B: Upper quarter evaluation: structural relationships and interdependence. In: Donatelli R, Wooden M (eds.): Orthopedic Physical Therapy. New York: ChurchillLivingstone,1989:43-58.
49. Kuzmich D: The levator scapulae: making the con-necktion. J Manual Manip Ther. 1994;2(2):43-54.
50. Quinter J, Elvey R: Understanding "RSI": a review of the role of peripheral neural pain and hyperalgesia. J Manual Manip Ther. 1993;1(3):99-105.
51. Chaffin DB, Andersson GB: Occupational Biomechanics. New York: John Wiley & Sons, 1991.
52. Spaulding SJ: The biomechanics of prehension. Am J Occup Ther. 1989;43(5):302 -7.
53. Butler DS: Mobilization of the Nervous System. New York: Churchill-Livingstone, 1991.
54. Anderson M, TIchenor CJ: A patient with De Quervain's tenosynovitis: a case report using an Australian approach to manual therapy. Phys Ther. 1994;74(4):314-26.
55. Mackinnon SE: Double and multiple "crush" syndromes: double and multiple entrapment neuropathies. Hand Clin. 1992;8:369-90.
56. Upton AR, McComas AJ: The double crush in nerve entrapment syndromes. Lancet. 1973;2:359-62.
57. Pfeffer G, Osterman AL: Double crush syndrome: cervical radiculopathy and carpal tunnel syndrome (abstract). J Hand Surg. 1986;11:766.
58. McLellan DL: Longitudinal sliding of the median nerve during hand movements: a contributory factor in entrapment neuropathy. Lancet. 1975;1:633-4.
59. Rowe L: The diagnosis of tendon and tendon sheath injuries. Semin Occup Med. 1987;1(2):1-6.
60. Janda V: Muscles, central nervous motor regulation and back problems. In: Korr I (ed.): The Neurobiological Mechanisms in Manipulative Therapy. New York: Plenum Press, 1977:27-4l.
61. Janda V: Muscle Function Testing. London: Butterworth, 1983.
62. Janda V, Jull GA: Muscles and motor control in low back pain: assessment and management. In: Twomey L (ed.): Physical Therapy of the Low Back. New York: ChurchillLivingstone, 1987:253 -78.
63. McKenzie RA: The Cervical and Thoracic Spine: Mechanical Diagnosis and Therapy. Waikanae, New Zealand: Spinal Publications, 1990.
64. Leahy M, Mock LE: Myofascial release technique and mechanical compromise of peripheral nerves of the upper extremity. Chiropractic Sports Med. 1992;6(2):139-49.
65. Bookhout MR: Examination and treatment of muscle imbalances. In: Bourdillon JF, Day EA, Bookhout MR: Spinal Manipulation. 5th ed. Oxford, England: Butterworth-Heinemann, 1992:312-22,335-56.
66. Lewit K: Manipulative Therapy in Rehabilitation of the Locomotor System. 2nd ed. Oxford, England: ButterworthHeinemann, 1991.
67. Wyke B: Neurology of the cervical spine joints. Physiotherapy. 1979;85:3.
68. Sunderland S: Traumatized nerves, roots and ganglia: musculoskeletal factors and neuropathic consequences. In: Korr M (ed.): The Neurobiologic Mechanisms in Manipulative Therapy. New York: Plenum Press, 1987:87.
69. Rodgers S: Recovery time needs for repetitive work. Semin Occup Med. 1987;2(1):19-24.
70. Wiker 5, Chaffine DB, Langoff G : Shoulder posture and localized muscle fatigue and discomfort. Ergonomics. 1989;32:211-37.
71. Brown S: The Hand Book: Preventing Computer Injury. New York: Ergonome, 1993.
72. Gossmand MR, Sahrmann SA, Rose SJ: Review of lengthassociated changes in muscle. Phys Ther. 1982;62:1799-808.
73. Grieve GP: Common Vertebral Joint Problems. Edinburgh, Scotland: Churchill-Livingstone, 1981.
74. Kendall FP, McCreary EK: Muscles Testing and Function. 4th ed. Baltimore, MD: Williams & Wilkins, 1993.
75. Greenfield B, Syen D: Evaluation and treatment of brachial plexus lesions. In: Donatelli R (ed.): Clinics in Physical Therapy: Physical Therapy of the Shoulder. 2nd ed. New York: Churchill-Livingstone, 1991.
76. MacKinnon SE, Dellon AL: Surgery of the Peripheral Nerve. New York: Thieme Medical, 1988.
77. Muckart R: Stenosing tendovaginitis of abductor pollicis longus and extensor pol\icis brevis at the radial styloid . Clin Orthop. 1964;33:201.
78. Magee DJ: Orthopedic Physical Assessment. Philadelphia, PA: W.B. Saunders, 1987.
79. Pascarelli E, Kella J: Soft-tissue injuries related to use of the computer keyboard. J Occup Med. 1993;35(3):522-32.
80. Evans RB, Hunter JM, Burkhalter WE: Conservative management of the trigger finger: a new approach. J Hand Ther. 1988;1(1):59-68.
81. Robbins H: Anatomical study of the median nerve in the carpal tunnel and etiologies of the carpal tunnel syndrome. J Bone Joint Surg. 1963;45(A):953.
82. Brand P, Hollister A: Clinical Mechanics of the Hand. 2nd ed. St. Louis, MO: CV. Mosby, 1993.
83. Hadler NM: Cumulative trauma disorders: an iatrogenic concept. J Occup Med. 1990;32:38-4l.
84. Bruening LA, Beaulieu D: The return to work phase for the patient with cumulative trauma. In: Hunter JM, Schneider LH, Mackin EJ, Callahan AD (eds.): Rehabilitation of the Hand: Surgery and Therapy. 3rd ed. St. Louis, MO: Cv. Mosby, 1990:1192-6.
85. Dobyns JH: Role of the physician in worker's compensation injuries. J Hand Surg. 1987;12A(5):826-9.
86. Maitland GD: Vertebral Manipulation. 5th ed. London, England: Butterworths, 1986.
87. Basmajian J, Nyberg R (eds.): Rational Manual Therapies. Baltimore, MD: Williams & Wilkins, 1993.
88. Moran C: Using myofascial techniques to treat musicians. J Hand Ther. 1992;5(2):97-101.
89. Elvey RL: Brachial plexus tension tests and the pathomechanical origin of arm pain. In: Glasgow EF, Twomey LT (eds.): Aspects of Manipulative Therapy. Melbourne, Australia: Churchill-Livingstone, 1979:105-10.
90. Buehler MJ, Thayer DT: The elbow flexion test: a clinical test for the cubital tunnel syndrome. Clin Orthop. 1988; 233:213-6.
91. Bell J: Sensibility testing. Current concepts. In: Hunter JM, Mackin EJ, Callahan AD (eds.): Rehabilitation of the Hand: Surgery and Therapy. 4th ed. St. Louis, MO: Cv. Mosby, 1995:115.
92. Cyriax JH: Textbook of Orthopaedic Medicine, I: Diagnosis and Soft Tissue Lesions. 7th ed. London, England: Bailliere Tindall, 1978.
93. Finkelstein H: Stenosing tendovaginitis at the radial styloid process. J Bone Joint Surg. 1930;12:509-40
January-March 1998 25

94. Koury M, Scarpelli E: A manual therapy approach to evaluation and treatment of a patient with chronic lumbar nerve root irritation. Phys Ther. 1994;7(6):548-60.
95. Key JL: Work capacity analysis. In: Scully RM, Barnes MR (eds.): Physical Therapy. Philadelphia, PA: J.B. Lippincott, 1989.
96. Arndt R: Work pace, stress and cumulative trauma disorders. J Hand Surg. 1987;12A(suppl):866-9.
97. Reynolds C: Electromyographic biofeedback evaluation of a computer keyboard operator with cumulative trauma disorder. J Hand Ther. 1994;1:25-7.
98. Wehbe M: Tendon gliding exercises. Am J Occup Ther. 1987;41(3):164-7.
99. Feurstein M, Hickey P: Ergonomic approaches in the clinical assessment of occupational musculoskeletal disorders. In: Turk DC, Melzack R (eds.): Handbook of Pain Assessment. New York: Guilford Press, 1992:71-99.
100. Hollis L, Hollis E: Teaching what you know. Occupational
26 JOURNAL OF HAND THERAPY
Therapy Week. 1995;Mar 9:18-9. 101. Yalom ID: The Theory and Practice of Group Psychother
apy. 3rd ed. New York: Basic Books, 1975. 102. Bandura A: Self-efficacy: toward a unifying theory of be
havioral change. Psycho Rev. 1977;84:191-215. 103. Gage M, Polatajko H: Enhancing occupational perfor
mance through an understanding of perceived self-efficacy. Am J Occup Ther. 1991;48(5):452-61.
104. Mathiowetz V, Kashaman N, Valland G, et al.: Grip and pinch strength: normative data for adults. Arch Phys Med Rehab. 1985;66:69-74.
105. Swanson NG, Sauter SL, Chapman LF: The design of rest breaks for video display terminal work: a review of relevant literature. Washington, DC: US. Government Printing Office, 1992. Publication no. 648-179/40018.
106. Godin G, Jobin J, Bouillon J: The reliability validity of selfreported exercise. Can J Public Health. 1986;77:359-62.