Proliferative periosteal processes of phalanges: a unitary hypothesis
Click here to load reader
-
Upload
michael-yuen -
Category
Documents
-
view
218 -
download
3
Transcript of Proliferative periosteal processes of phalanges: a unitary hypothesis

Skeletal Radiol (1992) 21:301 303 Skeletal Radiology
Proliferative periosteal processes of phalanges: a unitary hypothesis Michael Yuen, M.B., B.S., F.R.C.R. l, Lawrence Friedman, M.B.B.Ch., F.R.C.P.(C.)1, William Orr, M.D., F.R.C.P.(C.) 2, W. Peter Cockshott, M.D., F.R.C.P.C.(Ed. & C.), F.R.C.R. 1
Departments of 1 Radiology and 2 Pathology, McMaster University, McMaster University Medical Centre, Hamilton, Ontario, Canada
Abstract. A unitary hypothesis is offered to explain the various proliferative processes occurring around the phalanges. In the past, these have been separately desig- nated as proliferative periostitis, bizarre parosteal osteo- chondromatous proliferation, and turret exostosis. Be- cause the appearances of these entities depend on tempo- ral factors, breaching of the pcriosteum, and local ana- tomic features, we suggest a single term, proliferative periosteal processes of phalanges.
Key words: Phalangeal periostitis - Florid reactive per- iostitis - Bizarre parosteal osteochondromatous prolifer- ation - Proliferative periosteal processes of phalanges (PPPP)
Publications over the past 2 decades describing bony proliferative lesions related to the periosteum of the pha- langes of the hands and feet suggest that both patholo- gists and radiologists recognise two major distinct enti- ties: florid reactive periostitis and bizarre parosteal os- teochondromatous proliferation [1 5]. This communica- tion is based on a review of published cases, cases sccn in this hospital, and others referred to us by the Canadi- an Bone Tumour Review Panel. We propose a unitary hypothesis for these lesions since, in practice, there ap- pears to be considerable overlap between florid reactive periostitis and bizarre parosteal osteochondromatous proliferation.
The contrived nosological distinctions of these pro- cesses may be fuelling confusion rather than shedding wisdom.
The hypothesis
Common to all these lesions is an initial stimulus, often related to trauma, that leads to hemorrhagic subperios-
Address reprint requests to: W. Peter Cockshott, M.D., Department of Radiology, McMaster University Medical Centre, 1200 Main Street West, P.O. Box 2000, Hamilton, Ontario L8N 3Z5, Canada
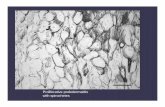
teal proliferation which then matures. If the reaction remains contained within the periosteum, a localised fu- siform periostitis develops in which the underlying cor- tex remains intact in the early stages. Later, as the focus of ossification matures, this periostitis becomes incorpo- rated into the cortex and with remodelling may ultimate- ly resemble a broad-based cancellous protuberance (Fig. 1). The radiologic and histologic features depend on the stage of maturation and organisation, but there may be cellular atypia. A combination of fibrosis, carti- lage, and bony elements confined within the thickened vascular periosteum is noted (Fig. 2) and fits the descrip- tion of florid reactive periostitis.
If the periosteum is breached, the reactive process can then extend into the loose areolar tissues around the fingers, producing a lobular rather than a fusiform lesion attached to the intact cortex (Fig. 3). With the passage of time the base organises into lamellar cancel- lous bone, but the peripheral aspects fail to undergo complete ossification, and islands of cartilage persist (Fig. 4). This failure is probably related to a relative deficiency of blood supply. The fusiform type, florid reactive periostitis, previously described has a blood sup- ply derived from the subperiosteal plexus, whereas the peripheral aspects of reactive processes extending beyond the breached periosteum do not acquire any par- asitic blood supply from the relatively avascular areolar fatty tissue. Therefore, lesions of bizarre parosteal osteo- chondromatous proliferation fail to develop comple te endochondral ossification, and cartilage focil persist. Lo- cal anatomical factors can modify the process. It is note- worthy that no case has been reported developing on the volar aspect of the terminal phalanx (Fig. 5). This is to be expected with the proliferative mechanism we postulate. The multiple septa present in the pulp of the fingers and toes bind the tissues tightly to the periosteum so that no potential subperiosteal expansive space can develop there. On the dorsum of the terminal phalanx, however, the nail bed modifies the development of the proliferative reaction, giving rise ultimately to a subun- gual exostosis or, if the nail is lost, to a turret exostosis or ostler's toe.
�9 1992 International Skeletal Society

Fig. 1. A 30-year-old woman with a 9-month history of painful finger swelling showing classic features of so-called florid perios- titis
Fig. 2. Low power magnification of florid periostitis showing pro- cesses limited by periosteum
Fig. 3. Adult woman with a 2-year history of increasing painless swelling at the proximal phalanx simulating an osteochondroma of the bizarre parosteal osteochon- dromatous proliferation variety. The lesion recurred after partial excision
Fig. 4. Cartilage cells in the exo- phytic process of the bizarre par- osteai osteochondromatous prolif- eration type
Fig. 5. A 9-year-old child trodden on by a horse on great toe. Note the subungual turret exostosis. In the terminal phalanx, the lesions are always dorsal because of the anatomic arrangement of septa on the volar aspect

M. Yuen et al. : Proliferative processes of phalanges 303
Clinically, it has been noted that the subperiosteal form, florid reactive periostitis, is painful, whereas the lobular form bizarre parosteal osteochondromatous pro- liferation, is not. This may be related to the fact that the first entity stretches the vascular periosteum and sti- mulates nerve endings, whereas the lobulated form, hav- ing breached the periosteum, is decompressed and does not produce pain of the same severity.
The rate of recurrence is related to the maturity of the lesion. As the reaction organises into bone and the periosteum becomes less intimately bound to the reactive process, a plane of cleavage forms between the new bone and the periosteum. If excision is carried out early or if the periosteum is not fixed, recurrence is likely. Recur- rence is more frequent in the exophytic type of complete- ly ossified lesions (bizarre parosteal osteochondroma- tous proliferation).
These proliferative parosteal processes of phalanges have occasionally been termed osteochondroma or myositis ossificans. Neither term is acceptable. Anatomi- cally, osteochondromata develop in relation to meta- physes and have a cartilage cap covered by periosteum or perichondrium and so do not resemble proliferative periosteal processes of phalanges. Myositis ossificans
cannot develop around phalanges as there is no muscle, only tendon. However, tendons can be implicated by the exophytic form if the periosteum is breached.
We propose that a unitary view of these lesions be adopted since the specific appearance depends on factors related to breaching of the periosteum, the stage of evo- lution and maturation of the process, and local anatomic factors.
References
1. Holmes WS, Pope TL, Lange EE de, Fechner RE, McDowell CL, Keats TE (1987) Case report 413. Skeletal Radiol 16:163
2. Lange EE de, Pope TL, Fechner RE, Keats TE (1987) Case report 428. Skeletal Radiol 16 : 481
3. Nora FE, Dahlin DC, Beabout JW (1983) Bizarre parosteal os- teochondromatous proliferations of the hands and feet. Am J Surg Pathol 7 : 245
4. Spjut HJ, Dorfman HD (1981) Florid reactive periostitis of the tubular bones of the hands and feet. A benign lesion which may simulate osteosarcoma. Am J Surg Pathol 5:423
5. Wissinger HA, McClain EJ, Boyes JH (1966) Turret exostosis. Ossifying hematoma of the phalanges. J Bone Joint Surg [Am] 48:105