Program & Abstractsregist2.virology-education.com/abstractbook/5th_TB_PK.pdf Program & Abstracts...
Transcript of Program & Abstractsregist2.virology-education.com/abstractbook/5th_TB_PK.pdf Program & Abstracts...

Program & Abstractswww.virology-education.com
Biltstraat 1063572 BJ Utrechtthe Netherlandswww.virology-education.com
SAN FRANCISCO, CA 8 September 2012 USA
5 th

5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs
8 September 2012San Francisco, CA, USA
PROGRAM & ABSTRACT BOOK
SAN FRANCISCO, CA 8 September 2012 USA
5 th

Acknowledgements
This workshop has been made possible by our sponsors.
Financial support for the 5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs has been provided by:
Silver Level Sponsor
Supporter: National Institutes of Health OfficeofAIDSResearch
Contributor: TB Alliance
ScientificSupporters
Program
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs - 8 September 2012 - San Francisco CA, USA
ii

Program iii
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Content • Acknowledgement p. ii
• Content Index p. iii
• General Information p. iii
• Organizing Committee p. iv
• Scientific Committee p. v
• Program p. vi
• Invited Speakers p. ix
• Abstracts p. 01
• Author Index p. 27
General Information Badge Policy
All registered delegates are provided with an identity badge. Please wear it at all times to ensure admission to the meeting.
Certificate of Attendance The certificates can be picked up during lunch.
Conference Materials Presentations will be posted on www.virology-education.com shortly after the workshop.
Date and Venue The date of the meeting is Saturday 8 September, 2012 The meeting is held in The Sheraton Fisherman’s Wharf Hotel, 2500 Mason Street, San Francisco, CA.
Language The official language of the workshop is English.
Social Program A workshop dinner is scheduled for Saturday evening 8 September for those delegates who have pre-registered.
Workshop Secretariat
The registration desk is located near the plenary meeting room. The conference organizers can be addressed for all questions concerning the logistics of the meeting.

Program iv
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Organizing Committee
Rob Aarnoutse, PharmD, PhD Senior Hospital Pharmacist Radboud University Nijmegen Medical Centre Nijmegen, The Netherlands
Geraint Davies, MD Senior Lecturer and Honorary Consultant in Infectious Diseases University of Liverpool Liverpool, United Kingdom
Helen McIlleron, MBChB, PhD Head of the Pharmacokinetic Research group, Division of Clinical Pharmacology University of Cape Town Cape Town, South Africa
Khisi Mdluli, PhD Senior Project Leader, Biology Global Alliance for TB Drug Development New York NY, USA
Eric Nuermberger, MD Associate Professor of Medicine and International Health Johns Hopkins School of Medicine Baltimore MD, USA
Charles Peloquin, PharmD Professor of Pharmacy and Medicine University of Florida Gainesville FL, USA

Program v
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Scientific Committee
Dakshina Chilukuri, PhD FDA, Silver Spring. MD, USAVeronique Dartois, PhD Public Health Research Institute, Newark, NJ, USA Kelly Dooley, MD, PhD John Hopkins University, Baltimore,MD, USAJan Gheuens MD, PhD Bill & Melinda Gates Foundation, Seattle, WA, USATawanda Gumbo, MD Southwestern Medical Center, Dalla, TX, USARichard Hafner, MD National Institutes of Health, Bethesda, MD, USAChristian Lienhardt MD, PhD WHO - Stop TB Department, Geneva, SwitzerlandAnnie Luetkemeyer, MD University of California, San Franciscio, CA, USAGary Maartens, MD University of Cape Town, Cape Town, South AfricaWilliam MacKenzie, MD CDC/CCID/NCHHSTP, Atlanta, GA, USASusan Swindells, MBBS University of Nebraska Medical Center, Omaha, NE, USAAndrew Vernon, MD CDC TBTC, Atlanta, GA, USARobert Wallis, MD, FIDSA Pfizer, New London, MS, USA
This Workshop is organized by
Biltstraat 106, 3572 BJ Utrecht, the NetherlandsPhone: + 31 30 230 7140 Fax: +31 30 230 7148Email: [email protected] / www.virology-education.com

Program vi
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Program - Saturday 8 September 2012 08:30h Opening Workshop chair
Session 1 Pharmacokinetics & pharmacodynamics of approved TB drugs (I)
Chairs: Rob Aarnoutse & Robert Wallis
08:40h Invited lecture: Pharmacokinetics and Pharmacodynamics of Fluoroquinolones in TB meningitis
S. Bhavnani
09:10h
Optimization of the rifampin dosage to improve the therapeutic efficacy in tuberculosis treatment, using a murine model
G. de Knegt
O_01
09:20h
What is the “right” dose of rifampin? An interim report.
M. Boeree
O_02
09:30h
A randomized trial comparing pharmacokinetics, safety and patient survival of standard versus intensified antibiotic treatment for TB meningitis
R. Aarnoutse
O_03
09:40h
Effect of dose size and food on pharmacokinetics of isoniazid in Peruvian TB patients
A. Requena Mendez
O_04
09:50h
Discussion and Q&A
10.15h
Coffee break
Session 2 Pharmacokinetics & pharmacodynamics of approved TB drugs (II) Chairs: Khisi Mdluli & Anne Luetkemeyer
10.35h
Invited lecture: Pyrazinamide, an amazing old drug as corner stone in novel TB drug regimens?
K. Mdluli
11:05h
Rifapentine Pharmacokinetics and Tolerability in Children and Adults Treated Once Weekly with Rifapentine/Isoniazid for Latent Tuberculosis Infection
M. Weiner
O_05
Population pharmacokinetics of once weekly rifapentine in children and adults
R. Savic
O_06
11:20h
Pharmacokinetics of anti-tuberculosis drugs in Venezuelan children: supportive evidence for the revised WHO dosing recommendations
R. Aarnoutse
O_07
11:30h
Clarithromycin shows a trend towards increase of linezolid exposure in multidrug-resistant tuberculosis
M. Bolhuis
O_08
11:40h
Evaluation of Co-trimoxazole in treatment of multidrug resistance tuberculosis
A. Pranger
O_09
11:50h
Discussion & Q&A
12:10h
Lunch
Session 3 Pharmacokinetics & pharmacodynamics of new TB drugs Chairs: Gerry Davies & Dakshina Chilukuri
13:25h
Invited lecture: Oxazolidinones, incorporating the concept of WBA studies
R. Wallis
13:55h
Activity of the Nitroimidazole TBA-354 Alone and in a Novel Drug Regimen in Two Murine Models of Tuberculosis
E. Nuermberger
O_10
14:05h
Population pharmacokinetics (PK) of bedaquiline (TMC207) and its M2 and M3 metabolites with efavirenz (EFV) demonstrate reduced exposure
E. Svensson
O_11

Program vii
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
14:15h
Whole blood mycobactericidal activity in a phase I trial of oral bedaquiline (TMC 207) alone and in combination with rifampin or rifabutin
C. Good
O_12
14:25h
Activity of PNU-100480 and its major metabolite in whole blood and broth culture models of tuberculosis
E. Nuermberger
O_13
14:35h
Pharmacokinetics and safety of moxifloxacin: preliminary results of a dose escalation study in tuberculosis patients
A. Pranger
O_14
14:45h
Discussion and Q&A
15:10h
Coffee break
Session 4 Population pharmacokinetics & pharmacokinetic-pharmacodynamic modeling Chairs: Charles Peloquin & Susan Swindells
15:30h
Invited lecture: Penetration and imaging of TB drugs in lesions – extending PK-PD beyond the central compartment
V. Dartois
16:00h
Population pharmacokinetics of rifampicin, pyrazinamide and isoniazid in children with tuberculosis. Model-based evaluation of currently recommended doses.
S. Zvada
O_15
16:10h
PK/PD of first-line antituberculosis drugs and concentrations associated with optimal efficacy in combination therapy regimens in patients
J. Pasipanodya
O_16
16:20h
The effect of antitubercular drug exposure on disease regression in South African tuberculosis patients
E. Chigutsa
O_17
16:30h
Pharmacokinetic-pharmacodynamic modelling of tuberculosis treatment response in Malawian adults with smear positive pulmonary tuberculosis
G.R. Davies
O_18
16:40h
Discussion and Q&A
Session 5 Drug development tools & methods Chairs: Eric Nuermberger & Helen McIlleron
17:10h
Moxifloxacin PK/PD properties and the role of efflux pumps in a novel hollow fiber model of Mycobacterium kansasii.
S. Srivastava
O_19
17:20h
An International Interlaboratory Quality Control (QC) Program for Bio-analysis of Tuberculosis Drugs
R. Aarnoutse
O_20
17:30h
Dried blood spot analysis for PK/PD optimization of linezolid in MDR-TB treatment
D.H. Vu
O_21
Robust and throughput method for simultaneously determination rifampicin, clarithromycin and metabolites in dried blood spots using LC-MS/MS
D.H. Vu
O_22
17:40h
Effect of limit of detection on analyses of bacteriological biomarkers in TB clinical trials
G.R. Davies
O_23
17:50h
Discussion and Q&A
18:00h
Adjournment

Program viii
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA

Program ix
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs
Invited Speakers

Program x
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Pharmacokinetics & Pharmacodynamics of Fluoroquinolones in TB meningitis
Sujata Bhavnani, PharmD, MSInstitute for Clinical Pharmacodynamics, and School of Pharmacy and Pharmaceutical Sciences, University at Buffalo, USA
Dr. Bhavnani’s scientific interests include anti-infective translational science and antimicrobial resistance. Her interest in anti-infective translational science involves the integration of pre-clinical pharmacokinetic-pharmacodynamic and early clinical pharmacokinetic data to identify dosage regimens that optimize the probability of positive clinical outcomes and minimize the potential of drug toxicities. Dr. Bhavnani also has extensive experience evaluating exposure-response relationships in infected patients, the results of which have been used to support decisions for dose selection and in vitro susceptibility test interpretive criteria for numerous new drug applications. Utilizing antimicrobial surveillance and drug usage databases, Dr. Bhavnani has also identified institutional- and patient-specific factors predictive of infection with resistant isolates. Identification of such factors aids in the clinical study of antimicrobial agents for resistant pathogens. Dr. Bhavnani is the author or co-author of over 150 peer-reviewed scientific publications, book chapters, or scientific abstracts and an Associate Editor for Diagnostic Microbiology and Infectious Disease. She received her B.Sc. in Pharmacy (1991) from the University of Toronto, Canada, her Pharm.D. (1994) from the Albany College of Pharmacy, New York, completed a two-year post doctorial fellowship in infectious diseases and pharmacokinetics (1996) at Millard Fillmore Hospital in Buffalo, New York, and her M.S. in biometry (2003) from the University at Buffalo, New York.
Pyrazinamide, an amazing old drug as corner stone in novel TB drug regimens?
Khisi Mdluli, PhDTB Alliance
Khisi Mdluli, joined the TB Alliance R&D team in May 2011 as the Project Leader of Research, working closely with Dr. Zhenkun Ma, Head of Research. Dr. Mdluli brings over 10 years of drug discovery expertise, particularly in assay development and high throughput screening, to help build and advance the TB Alliance’s portfolio.
A native of Swaziland, Dr. Mdluli is a highly regarded expert in the microbiology, molecular biology and biochemistry of Mycobacterium tuberculosis. A three-year visiting fellowship at the U.S. National Institutes of Health resulted in several important publications describing the mechanism of action of two currently used drugs, including isoniazid. Dr. Mdluli also spent two years at Cumbre Inc., a Texas based biotech, and six years at Chiron Corporation as a Senior Scientist where he helped establish and manage a major antimicrobial discovery program.

Program xi
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Oxazolidinones, incorporating the concept of WBA studiesRobert S. Wallis, MD, FIDSAPfizer, USA
Robert Wallis received his B.A. (1978) from Antioch College, and M.D. (1982) from Case Western Reserve University School of Medicine. He completed a Residency in Internal Medicine and postdoctoral Fellowship in Infectious Diseases at the University Hospitals of Cleveland, and then became a member of the faculty of the Department of Medicine at CWRU in 1987. In 2000, he moved his laboratory to the University of Medicine and Dentistry of New Jersey, where he directed clinical and research activities of the Division of Infectious Diseases of the New Jersey Medical School. His academic career focused on laboratory-based studies of mycobacterial pathogenesis and immunity, and international clinical trials of tuberculosis diagnosis, treatment, and monitoring, and of the co-pathogenesis of HIV and tuberculosis. In 2004, Dr. Wallis became Medical Director at PPD, Inc., a global contract research organization that provides discovery, development and post-approval services for industry, academia, and government. In 2008, he took a position as Senior Director at Pfizer, where he is presently Clinical Lead for Pfizer’s TB oxazolidinone program. Dr. Wallis maintains adjunct Professorships at both his former universities. Dr. Wallis has published over 120 scientific papers in journals such as the Lancet Infectious Diseases, Journal of Immunology, the Journal of Infectious Diseases, Blood, The Journal of Clinical Investigation, The Proceedings of the National Academy of Science, and Infection and Immunity, and has authored chapters in textbooks such as Tuberculosis and the Tubercle Bacillus (ASM Press), Tuberculosis Drug Development (Nova Science Publishers), and Tuberculosis: A comprehensive clinical treatise (Elsevier). He serves as Associate Editor for BMC Infectious Diseases, and as an Editorial Advisory Board member of several journals, including the Journal of Infectious Diseases, Tuberculosis, and Clinical and Laboratory Immunology.
Penetration and imaging of TB drugs in lesions – extending PK-PD beyond the central compartment
Véronique Dartois, PhDThe Public Health Research Institute Center at ICPH, UMDNJ, USA
Véronique Dartois recently joined the Public Health Research Institute in Newark (NJ), with an academic appointment in the Department of Medicine at UMDNJ. She studied Biology and Genetics at the University of Louvain (Belgium) where she received her Ph.D. in Molecular Microbiology. She spent a few postdoctoral years at the Scripps Research Institute (California) and Pasteur Institute (Paris), studying the regulatory networks that control cell differentiation and sporulation in Bacillus subtilis. She then joined a California-based start-up company to discover novel natural product antibiotics. Attracted to the field of neglected diseases, Véronique joined the Novartis Institute for Tropical Diseases in 2005, where she has assembled a team of scientists to conduct pharmacokinetic and efficacy studies supporting hit-to-lead, lead optimization and preclinical stages of drug discovery programs in Tuberculosis, Dengue fever and Malaria. Her current research interests include the pharmacokinetics and imaging of anti-tuberculosis drugs in pulmonary lesions, the molecular mechanisms driving intracellular accumulation of TB drugs, and the optimization of predictive animal models and in vitro assays to study these questions. Her key objective is to guide a more rational approach to TB treatment regimens that ensure optimal drug exposure at the site of infection.

Program xii
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA

Abstracts 1
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs
Abstracts

Abstracts 2
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA

Abstracts 3
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_01 PK/PD of approved TB drugs Optimization of the rifampin dosage to improve the therapeutic efficacy in tuberculosis treatment, using a murine model G.J. de Knegt1, R.E. Aarnoutse2, M.T. ten Kate1, M.J. Boeree3, D. van Soolingen4, I.A.J.M. Bakker-Woudenberg1, J.E.M. de Steenwinkel1
1Erasmus Medical Center, Medical Microbiology and Infectious Disease, Rotterdam, The Netherlands; 2Radboud University Nijmegen Medical Centre, Department of Pharmacy, Nijmegen, The Netherlands; 3Radboud University Nijmegen Medical Centre, Department of Pulmonary Diseases, Nijmegen, The Netherlands; 4National Institute of Public Health and the Environment & Centre for Infectious Disease Control, National Tuberculosis Reference Laboratory, Bilthoven, The Netherlands Introduction: Rifampicin is the cornerstone drug in view of its bactericidal and especially its sterilizing activity in the treatment of tuberculosis (TB). The rifampicin dosage of 10 mg/kg/day in the standard TB treatment appears to be at the lower end of the dose-response curve. This study in murine TB was performed to investigate whether increased rifampicin dosages could improve therapeutic efficacy and prevent the emergence of drug resistance. Furthermore, we assessed pharmacokinetics/pharmacodynamics (PK/PD) parameters to determine the human pharmacokinetic-equivalent dose. Material & Methods: Experimental TB in mice was established by intratracheal inoculation of a Mycobacterium tuberculosis strain of the Beijing genotype. In study 1, rifampicin as single-drug treatment was administered for 3 weeks. The maximum tolerated dose (MTD), steady-state pharmacokinetics and antimycobacterial effect in lung, spleen and liver were assessed. Mean CFU counts between groups were compared using one-way ANOVA. In study 2 we assessed the therapeutic efficacy of a range of rifampin (R) dosages added to a base regimen of isoniazid (H) and pyrazinamide (Z). Results: Study 1: The MTD of rifampicin in mice was 160 mg/kg/day. Rifampicin at dosage of 10 mg/kg/day or 160 mg/kg/day resulted in a 15-fold
increase in exposure (AUC0-24h) from 125.1 to 1854.8 h*mg/L. Cmax increased almost 9-fold, from 16.2 to 157.3 mg/L. Single-drug treatment for 3 weeks with rifampicin showed a strong dose-response correlation (p=0.0001). Study 2: By increasing the rifampicin dosage from 10 mg/kg/day to 80 mg/kg/day in the HRZ regimen, therapy duration could be reduced from 6 to 2 months. Therapeutic efficacy of the 2 months combination treatment was shown by complete mycobacterial elimination from infected organs, prevention of relapse of TB at 3 months post-treatment and avoidance of emergence of drug resistance. Pharmacokinetic data for rifampicin were similar in study 1 and 2, suggesting that co-administration of isoniazid and pyrazinamide does not affect the pharmacokinetics of rifampicin. Administration of 10 mg/kg and 160 mg/kg rifampicin yielded a protein binding of 3.2% and 2.6% respectively, which indicates that protein binding is not strongly dependent on the total concentration of rifampicin. Moreover, the results show that the dose of 10 mg/kg/day rifampin is indeed a human pharmacokinetic-equivalent dose. Conclusions: Our findings indicate that the currently used rifampin dosage in the therapy of TB is too low. In our murine TB model a rifampin dosage of 80 mg/kg/day enabled a significant reduction in therapy duration without adverse effects. No conflict of interest

Abstracts 4
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_02 Toxicity and Safety What is the “right” dose of rifampin? An interim report. M. Boeree1, A. Diacon2,3, R. Dawson4, J. du Bois3, K. Narunsky4, A. Venter2, S. Gillespie5, T. McHugh6, M. Hoelscher7, N. Heinrich7, A. Nunn8, P. Phillips8, G. Plemper van Balen1, R. Aarnoutse9
1Department of Lung Diseases, Radboud University Nijmegen Medical Centre, Nijmegen, The Netherlands; 2Department of Medical Biochemistry, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa; 3Task Applied Science, Bellville, Cape Town, South Africa; 4University of Cape Town Lung Institute, Division of Pulmonology, Cape Town, South Africa; 5 Medical School, University of St Andrews, St Andrews, UK; 6 Department of Infection, University College London, London, UK; 7 Department for Infectious Diseases & Tropical Medicine, University of Munich (LMU), Munich, Germany; 8 Clinical Trials Unit, Medical Research Council, London, UK ; 9 Department of Pharmacy, Radboud University Nijmegen Medical Centre, Nijmegen, The Netherlands Background: The pivotal anti-tuberculosis (TB) drug rifampin was introduced in 1971. In retrospect, the rifampin dose of 10 mg/kg was selected mainly based on cost, efficacy and (fear for) toxicity, but actual evidence underpinning this dose is scant. A maximum tolerable dose (MTD) study was never performed. Currently, available data in mice and humans show that an increase in dose of rifampin may significantly shorten the TB treatment duration. The primary aim of this study was to assess the MTD of rifampin to enable study of the “right” dose of rifampin in follow-up studies. Materials and methods: We performed a 14-day MTD study in treatment-naive adult smear-positive tuberculosis patients. Groups of 8 (control group: 10 mg/kg) and 15 patients received 10 and 20, 25, 30 and 35 mg/kg rifampin once daily for days 1-7, complemented with standard doses of isoniazid, pyrazinamide and ethambutol for days 8-14. Safety/tolerability assessments included physical examinations, vital signs, adverse event assessments, ECG-recordings, clinical chemistry/hematology/coagulation tests and urinanalysis. Therapy was under full DOT. The plasma pharmacokinetics of rifampin was assessed by intensive sampling at days 7 and 14. Microbiological evaluations included
consecutive colony forming units counts in H11 Middlebrook medium and time-to-positivity in MGIT cultures. After day 14, all subjects continued with standard anti-TB treatment. After each dose step a trial steering committee evaluated the incidence and severity of adverse events and determined whether the study could be continued. Results: The control group (10 mg/kg) and all four consecutively recruited groups with daily doses of 20, 25, 30 and 35 mg/kg rifampin completed the study. We recorded 163 adverse events in 68 patients, and 110 were possibly related (102) or related (8) to rifampin: 88 were grade 1, 19 were grade 2, and 3 were grade 3. All 8 events considered related to rifampin were rated grade 1. Grade 3 events included a case of transient hyperkalaemia (20 mg/kg; onset days 3 and 6) and two cases of elevated liver enzymes (30 and 35 mg/kg; onset days 21 and day 17). The geometric mean AUC 0-24 at day 14 was 26.3 h*mg/L in the 10 mg/kg control group, increasing to 112.6, 134.5 and 189.4 h*mg/L in the 20, 25 and 30 mg/kg groups respectively, showing an initial non-linear increase followed by a more proportional increase in exposure. Geometric mean Cmax values were 7.4, 21.6, 25.1 and 33.1 mg/L in the 10, 20, 25 and 30 mg/kg groups respectively. Pharmacokinetic data on the 35 mg/kg group, pharmacodynamic parameters and early bactericial activity results of all groups are pending. Conclusions: Rifampin up to 35 mg/kg was safe and tolerable in this MTD study. There is an increase in exposure to rifampin after several dose increases without an apparent ceiling effect in exposure. We will extend this study with higher doses until the stopping criteria are met. Based on the result of this trial we will evaluate 35 mg/kg rifampin in a multiple arm, multiple stage design within the PanACEA consortium.

Abstracts 5
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_03
PK/PD of approved TB drugs
A randomized trial comparing pharmacokinetics, safety and patient survival of standard versus intensified antibiotic treatment for TB meningitis R. Ruslami1, A.R. Ganiem2, S. Dian2, L. Apriani3, T.H. Achmad4, A.J. van der Ven5, G. Borm6, R.E. Aarnoutse7, R. van Crevel5
1Universitas Padjadjaran/Hasan Sadikin Hospital, Dept. of Pharmacology and Therapy, Bandung, Indonesia; 2Universitas Padjadjaran/Hasan Sadikin Hospital, Dept. of Neurology, Bandung, Indonesia; 3Universitas Padjadjaran/Hasan Sadikin Hospital, Health Research Unit, Bandung, Indonesia; 4Universitas Padjadjaran/Hasan Sadikin Hospital Bandung Indonesia, Dept. of Biochemistry, Bandung, Indonesia; 5Radboud University Nijmegen Medical Centre, Dept. of Internal Medicine, Nijmegen, The Netherlands; 6Radboud University Nijmegen Medical Centre, Dept. of Epidemiology Biostatistics and Health Technology Assessment, Nijmegen, The Netherlands; 7Radboud University Nijmegen Medical Centre, Dept. of Pharmacy, Nijmegen, The Netherlands Background: Tuberculous meningitis (TBM) leaves up to 50% of patients dead or neurologically disabled. Intensified antibiotic treatment may improve outcome of TBM. The current dose of rifampicin is at the lower end of the dose-response curve and the penetration of rifampicin to cerebrospinal fluid (CSF) is limited. Moxifloxacin shows good penetration in CSF, but available data suggest that the optimal dose of moxifloxacin for TB may be higher than the usual dose of 400 mg QD. Co-administration of rifampicin decreases exposure to moxifloxacin by about 30%. We examined pharmacokinetics (PK), safety and clinical benefit of treatment regimens including high-dose rifampicin and high dose moxifloxacin for TBM in a hospital setting in Indonesia. Materials and methods: Sixty TBM patients, aged >14 years, were randomized to standard 10 mg/kg p.o. or 13 mg/kg rifampicin administered i.v., and (in a second randomization) to ethambutol 750 mg, moxifloxacin 400 mg or moxifloxacin 800 mg QD, resulting in 6 groups of patients. All patients received standard dose isoniazid, pyrazinamide and adjunctive corticosteroids. After 14 days of treatment all patients continued with standard TB treatment. PK assessments were performed in
blood (at 1, 2, 4, 6 and 24 h post dose) and in CSF (at 3-6 and 6-9 h post dose) within the first critical days of treatment. In the first 2 weeks of treatment, clinical condition and possible drug-related adverse events were monitored daily. ECG and blood examination were performed twice weekly. Adverse events attributable to TB treatment were assessed, and survival up to six months was evaluated as secondary endpoint. PK and safety data were presented descriptively. A Cox regression analysis was performed to assess the effects of possible predictors on survival. Results: Sixty patients were randomized, most with British Medical Research Council grade 2 (82%) or grade 3 (12%) TBM, and 12% with concurrent HIV infection. After combining of groups in view of limited between-group PK differences, it appeared that a 30% higher dose of rifampicin i.v. led to much higher geometric mean AUC0-6 (78.7 vs. 26.0 mg*h/L), Cmax (22.1 vs. 6.3 mg/L), and CSF peak concentrations of rifampicin (0.62 vs. 0.27 mg/L). Doubling the dose of moxifloxacin resulted in a two-fold increase in plasma AUC0-24, AUC0-6, and Cmax and a 1.6 fold increase in CSF peak concentrations. 34 patients (57%) experienced adverse events that were possibly or probably related to study medication. Hepatotoxicity of all grades and mild QTc prologation appeared to be equally distributed over the study groups. Six-month mortality was substantially lower in patients receiving high dose rifampicin intravenously (HR 0.42, 95% CI 0.20-0.87), and was not explained by HIV-status or severity of disease at time of presentation. Use of moxifloxacin did not appear to improve survival in this population. Conclusions: Intensified antibiotic treatment for TBM leads to more favorable PK with acceptable toxicity. Our study, although not primarily designed for this purpose, suggests that high-dose rifampicin administered for the first two weeks i.v. improves survival of patients with severe TBM. No conflict of interest

Abstracts 6
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_04 PK/PD of approved TB drugs Effect of dose size and food on pharmacokinetics of isoniazid in peruvian TB patients A. Requena-Méndez1, G. Davies2, D. Waterhouse3, A. Aardrey3, O. Jave4, S. Ward3, D. Moore5
1Barcelona Centre for International Health Research (CRESIB, Hospital Clinic-Universitat de Barcelona); 2Institutes of Global Health & Translational Medicine. University of Liverpool; 3Liverpool School of Tropical Medicine, Liverpool, UK; 4Hospital Dos de Mayo, Lima, Peru; 5Department of Clinical Research, Faculty of Infectious and Tropical Diseases, London; School of Hygiene and Tropical Medicine Introduction: Antituberculosis drug pharmacokinetics (PK) could be altered by several factors, including age, sex, ethnicity, malnutrition, drug formulation, drug interactions and different disease presentations. Accordingly, patients with DM and HIV/AIDS have been suggested to have impaired absorption. Isoniazid, one of the essential drugs of first line tuberculosis (TB) treatment, has highly polymorphic metabolism controlled by expression of N-acetyltransferase-2 (NAT-2). Food may also delay and reduce of absorption of isoniazid, particularly high-fat meals. This study, aimed to determine the pharmacokinetics of isoniazid in a Peruvian TB population with and without co-morbidities. Methods: TB patients receiving directly observed first line TB therapy through the National TB programme in health centers of Lima and with more than 15 days of treatment were invited to participate. Two different blood samples taken at two time-points (2 and 6 hours after the drug intake) were collected and sent them to the Liverpool School of Tropical Medicine (LSTM) where isoniazid levels were quantified in human plasma using liquid chromatography coupled with tandem mass spectrometry (LC/MS). For each patient the maximum serum drug concentration (Cmax) was estimated as the higher of the two measured concentrations; Tmax for each patient was the time-point at which the Cmax occurred. Data were analyzed using Stata version 12.
Results: Of 113 patients recruited to the study, PK data was available for 107 (mean age 36.7 years, 63.6% male). Sixty-two patients were in the intensive phase and they were receiving isoniazid at a median daily dose of 5.14 mg/kg/day (range 3.37-10-13) and 45 patients were in the maintenance phase and they received isoniazid twice a week at a median dose of 12.9 (7.62-18.12) mg/kg/day which was significantly lower than expected (p<0.001). Overall median Cmax levels of isoniazid were 2.77 mg/L (range 0.01-22.44) in the intensive-phase group and 8.71 mg/L (0-59.33) in the maintenance-phase group. Neither intensive nor maintenance-phase group of patients with co-morbidities had different Tmax results compared to TB-patients without co-morbidities. There were also no differences in Cmax of males compared to female patients in both intensive and maintenance-phase groups. Tmax predominantly occurred at 2 hours instead of 6 hours (86.4% in the intensive-phase and 90.7% in the maintenance-phase group) and it was not associated with gender, age group, DM or HIV co-morbidity, phase of treatment, intestinal parasitic infection or dose received. Information on oral intake was only available for 48 patients, 12 of who fasted for at least 2 hours before taking the treatment. Food intake was weakly associated with a reduced Cmax in the 5mg/kg/day-patients group (p=0.03) but not in the maintenance-phase group. Conclusion: We could not demonstrate any differences in the PK of isoniazid in TB patients with co-morbidity compared to those without co-morbidity. The known effect of food upon the PK of isoniazid was shown at least in those patients receiving daily dose of isoniazid. Although genotyping for NAT2 was not carried out, the percentage of patients with Tmax at 6 hours represents a minimum estimate for the frequency of slow acetylation in Peruvian patients.

Abstracts 7
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_05 PK/PD of approved TB drugs Rifapentine Pharmacokinetics and Tolerability in Children and Adults Treated Once Weekly with Rifapentine/Isoniazid for Latent Tuberculosis Infection M. Weiner1, R. Savic2, D. Wing3, W.R. Mac Kenzie4, C.A. Peloquin5, M. Engle1, E. Bliven4, A. Borisov4, S.M. Abdel-Rahman6, G.L. Kearns6, W. Burman7, T.R. Sterling8, M.E. Villarino4, . Tuberculosis Trials Consortium Study 26PK Group4
1University of Texas Health Science Center and VAMC, Medicine, San Antonio TX, USA; 2UCSF School of Pharmacy, Bioengineering and Therapeutic Sciences, San Francisco CA, USA; 3University of Texas Health Science Center, Medicine, San Antonio TX, USA; 4Centers for Disease Control and Prevention, Division of Tuberculosis Elimination, Atlanta GA, USA; 5University of Florida, College of Pharmacy, Gainesville FL, USA; 6Children's Mercy Hospitals and Clinics, Pediatrics, Kansas City MO, USA; 7Denver Health, Denver Public Health, Denver CO, USA; 8Vanderbilt University, Medicine, Nashville TN, USA Introduction: In a Phase-3, randomized clinical trial (PREVENT-TB) of 8,053 persons with latent tuberculosis infection (LTBI), 12 once-weekly doses of rifapentine and isoniazid demonstrated efficacy and tolerability comparable to nine months of daily isoniazid. A prior Phase-1, single-dose rifapentine pharmacokinetic study suggested that higher rifapentine dosages (mg/kg) in young children were needed to achieve an area under the concentration curve (AUC) comparable to adults administered a standard dose. In the PREVENT-TB trial, children were administered higher rifapentine mg/kg dosages than adults, and pharmacokinetic values in children were compared to adults. Material & Methods: 80 children (age 2 to < 12 years) and 77 adults (> 18 years) were enrolled in the pharmacokinetic substudy of the PREVENT-TB trial. Rifapentine doses in children ranged from 300 to 900 mg (depending on weight) while adults received 900 mg. Pharmacokinetic samples were taken after at least three weeks of therapy. Children who could not swallow tablets were administered a suspension of crushed rifapentine and isoniazid tablets in either liquid or a soft food. Because historical rifapentine pharmacokinetic data
demonstrated high correlations between AUC obtained by intensive sampling and a single concentration 24-hours after drug administration, the sparse sampling design used a plasma sample collected 24-hours after administration of study drugs (C24). Using NONMEM software, a nonlinear, mixed effects regression model was developed from historical pharmacokinetic data from 38 pediatric and 36 adult patients with intensive sampling, and the model was further developed with data from this substudy. Results: In the pharmacokinetic substudy, the median ages of children and adults were 4.5 years and 40.0 years, respectively. There were 40 children ages 2-4 years; 22, 5-8 years; and 18, 9-11 years. The geometric mean (GM) rifapentine dosage in children was 23 mg/kg vs. 11 mg/kg in adults. Rifapentine GM AUC0-inf was 33% greater in children compared to adults (GM, [90% CI], 650 [604-699] vs. 489 [451-529] mcg*h/mL, P<0.0001, ANOVA, Contrast t-test). The GM AUC0-inf in children administered crushed rifapentine tablets was lower than in children administered whole tablets (GM, [90% CI], 588 [538-643] vs. 809 [733-894] mcg*h/mL, P=.03). The rifapentine and isoniazid regimen appeared well tolerated by children. Three patients in this pharmacokinetic substudy were discontinued from 3HP treatment due to adverse events attributed to study medications. One child developed grade-1 emesis with administration of crushed isoniazid tablets in liquid and in food suspensions, while two adults were identified with grade-3 events; urticaria and angioedema in one and dyspnea in the other. In the 24-hours after drug administration during the pharmacokinetic substudy, grade-1 signs or symptoms were identified in 6% of children and 17% of adults. Conclusions: With the weight-based, rifapentine dosing algorithm in children, rifapentine AUC0-inf was higher than the AUC0-inf in adults receiving a 900 mg dose. The higher rifapentine dosages in children were clinically well tolerated. This study of 3HP treatment of LTBI demonstrates that comparable rifapentine AUC0-inf was achieved between adults and HIV-seronegative, young children with weight-based, higher dosage rifapentine. Support was provided by the Centers for Disease Control and Prevention through the Tuberculosis Trials Consortium, Sanofi-aventis, the Veterans Administration, and the National Center for Research Resources (Award Number UL 1RR025767) of the National Institutes of Health.

Abstracts 8
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_06 PK/PD of approved TB drugs Population pharmacokinetics of once weekly rifapentine in children and adults R.M. Savic1, M. Weiner2, W. Mac Kenzie3, E. Bliven-Sizemore3, C.A. Peloquin4, K. Dooley5, S.M. Abdel-Rahman6, G.L. Kearns6, W. Burman7, T.R. Sterling8, M.E. Villarino3, and the Tuberculosis Trials Consortium 1University of California San Francisco, San Francisco, CA; 2University of Texas Health Science Center and VAMC, San Antonio TX; 3Centers for Disease Control and Prevention, Atlanta, GA; 4University of Florida, Gainesville, FL; 5Johns Hopkins University School of Medicine, Baltimore, MD; 6Children's Mercy Hospitals and Clinics, Kansas City, MO; 7Denver Public Health, Denver CO; 8Vanderbilt University, Nashville TN Background: A 12-dose, once weekly regimen of rifapentine and isoniazid (3HP) has been recommended by the CDC as an alternative treatment of latent tuberculosis infection (LTBI) in adults. Previous studies in adults showed that rifapentine pharmacokinetics are influenced by food, dosage and time, and one PK study suggested that young children may need higher mg/kg dosages of rifapentine to achieve the exposure comparable to adults receiving a standard dose. To help guide dosing of rifapentine in children and adults with LTBI, we developed a population pharmacokinetic (PPK) model. Methods: The PPK model used pharmacokinetic data from four studies of children and adults with rifapentine administered as either a single dose or as part of a once weekly regimen: (A) 35 intensively sampled adult patients receiving 600–1200 mg of rifapentine once weekly; (B) 23 intensively sampled children (2-14 years old) receiving a single 150-300 mg dose of rifapentine; (C) 12 intensively sampled adolescents (12–15 years old) receiving a 450-600 mg single dose of rifapentine; and (D) a PK substudy of 3HP treatment with 81 sparsely sampled children (2-12 years) receiving 300-900 mg rifapentine and 77 adults receiving 900 mg. Model development involved sequential development of models for children and adults, followed by the joint analysis of all available data. The developmental changes in rifapentine clearance in young children were investigated as
well as the effect of covariates, including food, tablet integrity, weight and dose. The analysis was performed in NONMEM 7. Results: The database included 837 concentration-time measurements from 230 subjects (116 children). A one-compartment model with allometrically scaled parameters described the data well. Apparent oral clearance per kilogram of body weight was significantly higher in children compared to adult. This relationship was described by a maturation function, where clearance for the youngest child (2 years) was estimated to be 0.038 L/h/kg, decreasing to the fully matured value of 0.029 L/h/kg by age of 10 (half-life of 1.65 years). This relationship was confirmed by estimated lower parent/metabolite exposure ratios in very young children compared to adults, indicating higher metabolic activity in very young children. The between-subject variability in clearance was 44%. Rifapentine relative bioavailability decreased by 5% for each 100 mg increase in dose higher than 600 mg. Food was found to increase relative bioavailability by 68%. Children who could not swallow the whole tablet, and received the formulation crushed, showed a 30% decrease in relative bioavailability. There was no evidence of auto-induction with once weekly dosing. Conclusions: Our population pharmacokinetic model of once weekly rifapentine in children and adults shows that clearance in children is higher than in adults, but decreases with age; therefore children < 10 years require higher dosages per kilogram of body weight to reach the equivalent adult exposure. The reduction in AUC0-inf with administration of crushed tablets emphasizes the need for a novel rifapentine formulation for children who cannot swallow whole tablets. Food effect and decreased bioavailability at rifapentine doses > 600 mg deserve consideration in the development of dosage guidelines.

Abstracts 9
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_07 PK/PD of approved TB drugs Pharmacokinetics of anti-tuberculosis drugs in Venezuelan children: supportive evidence for the revised WHO dosing recommendations L.M. Verhagen1, D. López2, P.W.M. Hermans3, A. Warris3, R. de Groot3, J.F. García2, J.H. de Waard1, R.E. Aarnoutse4
1Instituto de Biomedicina, Laboratorio de Tuberculosis, Caracas, Venezuela; 2Hospital de Niños J.M. de los Ríos, Departamento de Pediatría Infectología, Caracas, Venezuela; 3Radboud University Nijmegen Medical Centre, Department of Pediatrics, Nijmegen, The Netherlands; 4Radboud University Nijmegen Medical Centre, Department of Pharmacy, Nijmegen, The Netherlands Background: Dosage recommendations for anti-tuberculosis (TB) drugs in children (expressed in mg/kg) have been deducted from dosages used in adults for decades, without considering that (young) children may need higher drug doses in mg/kg in view of different pharmacokinetics (PK) compared to adults. In 2009, the WHO has issued revised, higher dosage recommendations for first-line anti-TB drugs in children. However, the revised dosage recommendations are still under consideration in many settings and there is a complete lack of PK data for children from South America, either on old or new dosage recommendations. We studied the PK of first-line anti-TB drugs in Venezuelan children who received these drugs following the old dosage recommendations. Materials and Methods: Venezuelan HIV-negative TB patients aged 1 to 15 years were included during the intensive phase of daily anti-TB treatment following old WHO dosing guidelines. Plasma concentrations of first-line anti-TB drugs were assessed at 0, 2, 4 and 8 h after intake of anti-TB drugs with a standardized meal, which reflected the usual drug intake procedure. PK parameters were assessed using noncompartmental PK. For pyrazinamide, which shows a long elimination half-life in children, the plasma concentration at T=0 was assumed to reflect the concentration at 24 h post dose at steady-state, to enable calculation of AUC0-24. Acetylator status for isoniazid was determined
phenotypically from the half-life of isoniazid. Cmax values were compared to the typical reference values associated with adequate response in the majority of adult patients. In view of a possible effect of food on Cmax , AUC0-24 values were also compared to data from adult studies performed in The Netherlands, Tanzania and Indonesia. Results: Thirty patients were included: 63% were boys, median age was 3 years (IQR 2-8), 57% was aged 0-4 years and 43% was 5-15 years. Twenty-five children (83%) had an isoniazid Cmax below the reference range of 3-6 mg/L and 23 children (77%) had a rifampicin Cmax below 8-24 mg/L. Only one patient (3%) had a pyrazinamide Cmax below 20-50 mg/L. The low number of patients on ethambutol (n=5) precluded firm conclusions. Comparison of geometric mean AUC0-24 values to those in adults from The Netherlands, Tanzania and Indonesia showed lower exposures in Venezuelan children compared to adults, especially for rifampicin. AUC0-24 and Cmax of all four drugs were significantly and positively correlated with age and body weight. Children aged 1-4 years had significantly lower AUC0-24 and Cmax values for isoniazid and rifampicin and a trend to lower values for pyrazinamide compared to those aged 5-15 years. The geometric mean AUC0-24 for isoniazid was much lower in fast acetylators than in slow acetylators (5.2 vs. 12.0 h*mg/L, p<0.01). Conclusions: This is the first PK study from the South American region focusing on pediatric TB. The data provide supportive evidence for the implementation of the revised WHO guidelines for isoniazid and rifampicin in children in South America. Follow-up studies are needed to describe exposures in children who take the recommended increased doses of anti-TB drugs. No conflict of interest

Abstracts 10
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_08 Therapeutic Drug Monitoring Clarithromycin shows a trend towards increase of linezolid exposure in multidrug-resistant tuberculosis M.S. Bolhuis1, R. van Altena2, W.C.M. de Lange2, A.D. Pranger1, D.R.A. Uges1, T.S. van der Werf3, J.G.W. Kosterink1, J.W.C. Alffenaar1
1University of Groningen University Medical Center Groningen, Hospital and Clinical Pharmacy, Groningen, The Netherlands; 2University of Groningen University Medical Center Groningen, Tuberculosis Center Beatrixoord, Haren, The Netherlands; 3University of Groningen University Medical Center Groningen, Internal Medicine and Pulmonary Disease and Tuberculosis, Groningen, The Netherlands Background: Linezolid (LZD) is a promising antimicrobial agent for the treatment of multidrug-resistant tuberculosis (MDR-TB). Unfortunately, adverse events, such anemia and peripheral neuropathy limit the use of LZD. Dose reduction of LZD has resulted in lower frequency of adverse events. Recently we reported a pharmacokinetic drug-drug interaction between LZD and clarithromycine (CLR), another WHO Group 5 anti-TB drug. The drug-drug interaction resulted in increased LZD exposure, which could lead to increased toxicity with the need to cease treatment with LZD. This severely limits the treatment options left. Therefore, the aim of this prospective pharmacokinetic study is to quantify the possible interaction between LZD and CLR. Materials & Methods: All study subjects included in this open-label, prospective single-center, 1-arm, fixed-order, interventional pharmacokinetic interaction study, were aged ≥18 years old and were diagnosed with MDR-TB. The criteria for exclusion were based on the contraindications and known drug-drug interactions of both drugs. Subjects that concomitantly received P-glycoprotein modulators were excluded. All study subjects received LZD 300mg twice a day during the entire study. Serum curves were obtained at three time points: at baseline without CLR, after two weeks of 250mg CLR once daily and after two weeks of 250mg CLR once daily, consecutively. LZD and CLR serum concentrations were analyzed using a validated
method and results were used to calculate pharmacokinetic (PK) parameters. Differences between PK parameters were calculated with the Mann-Whitney-Wilcoxon test. Linear regression is calculated between LZD AUCs at different CLR doses. Results: The median LZD AUC0-12h was 48.4 mg*h/L (ICR: 34.0-66.5) at baseline, 63.9 mg*h/L (ICR: 61.0-98.2) after co-administration with 250mg CLR and 75.8 mg*h/L (ICR: 67.2-85.4) after co-administration with 500mg CLR. The geometric means were 48.5, 68.2, and 70.8 respectively. Statistical analysis with Mann-Whitney-Wilcoxon test revealed no statistically significant increase after 250mg (P=0.225), but showed a trend towards increase of LZD AUC0-
12h after co-administration of 500mg CLR compared to baseline (P=0.08). Dose dependency was tested by Friedmans related samples test and showed a trend (P=0.17) Co-administration of CLR and LZD was well tolerated in general. None of the patients experienced severe adverse effects such as anemia, peripheral neuropathy, optic neuritis, or thrombocytopenia. Two patients reported nausea from the administered CLR, a well known side-effect. One of these patients withdrew from the study after 2 weeks of 250mg CLR once daily due to the gastro-intestinal side effects. Conclusion: In this study, we evaluated a possible interaction between CLR and LZD and showed that CLR did not significantly increase LZD serum AUC0-12h in MDR-TB patients. CLR showed a trend towards a dose dependent increase in LZD AUC0-12h after co-administration. .Based on the presented data, further exploration in a larger cohort or with a higher CLR dose of 1000mg is needed. Preemptive dose-reduction of LZD after co-administered with CLR is currently not advised but monitoring drug levels when LZD and CLR are combined is suggested. No conflict of interest

Abstracts 11
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_09 Treatment of MDR-TB and XDR-TB Evaluation of Co-trimoxazole in treatment of multidrug resistance tuberculosis N. Alsaad1, R. Altena2, A.D. Pranger1, D. Soolingen3, W.C.M. de Lange2, T.S. van der Werf4, J.G.W. Kosterink5, J.W.C. Alffenaar5
1University Medical Center Groningen, Hospital and Clinical Pharmacy, Groningen, The Netherlands; 2University Medical Center Groningen, Tuberculosis Centre Beatrixoord, Haren, The Netherlands; 3Institute for Public Health and the Environment, National Tuberculosis Reference Laboratory, Bilthoven, The Netherlands; 4University Medical Center Groningen, Department of Pulmonary Diseases and Tuberculosis, Groningen, The Netherlands; 5University Medical Center Groningen, Hospital and Clinical Pharmacy, Groningen, The Netherlands Introduction: Co-trimoxazole (SXT), a combination of sulfamethoxazole (SMX) and Trimethoprim (TMP) has shown in vitro activity against Mycobacterium tuberculosis (i.e. SMX). However, the pharmacokinetic (PK) and pharmacodynamic (PD) parameters of SXT in multidrug-resistant (MDR) tuberculosis (TB) are so far lacking. Therefore we evaluated the pharmacokinetics and drug susceptibility along with its tolerability in MDR-TB treatment. Material & Methods: MDR-TB patients who were referred to the Tuberculosis Center Beatrixoord between the 1st January 2006 and the 1st July 2012 and for whom drug susceptibility testing (DST) for SXT was performed, were eligible for evaluation. Patient characteristics and medical history were evaluated for patients that received SXT. Blood samples were collected at steady state; before and at 0, 1, 2, 3, 4 and 8 h after SXT administration and analysed using LC/MS-MS. PK parameters of SMX were determined with a standard non-compartmental PK method using the KINFIT and an one compartmental PK population model with first order absorption without lag time was developed using an iterative two-stage Bayesian procedure (MW/Pharm 3.60, Mediware, Groningen, The Netherlands). The model was cross validated and tested using Bland Altman analysis. To determine MIC values, the patients? M. tuberculosis isolates were subjected to drug susceptibility testing
which was performed on the Middelbrook 7H10 agar dilution method at the Dutch national Mycobacterium Reference Laboratory (National Institute for Public Health and the Environment, RIVM).Tolerability during TB treatment was evaluated by assessing the reported side effects of SXT with specific attention for gastrointestinal side effects (nausea, vomiting and diarrhea), hepatotoxicity, anemia and blood count abnormalities. Results: Ten MDR-TB patients (1 of whom had XDR-TB) received 480 mg of SXT with median dose of 6.5 mg/kg of SXT once daily for a median treatment period of 381 days. PK parameters of SMX could be evaluated in only 8 of the 10 patients because in the other two patients no plasma sampling was performed during the treatment period with SXT. Median AUC was 371.5 (IQR 360-574.8) mg*h/L, median Cl was 0.9 (0.5-1) L/h, median Vd was 11.5 (9.2-14.9) L and median t ½ 10.1 (8.7 -10.8) h. Geometric mean values of the POP-PK model were Cl (1.14 ± 0.43)L/h/1.85 m2, Vd (0.24± 0.05) L/Kg LBMc, Ka-po (0.43±0.17) and F=1. The drug susceptibility testing show that MIC values of SMX for M. tuberculosis varied with median ranges of 9.5 (IQR, 4.8 - 25) mg/L. In two patients, the dose was escalated to 960 mg with median value of 13.6 mg/kg. The ƒAUC0-
24h/MIC ratios after receiving 480 mg for SMX was 11.1 (IQR, 8 -16.4) and exceeded 25 in only one patient. SXT was safe and well tolerated except for one patient who had gastrointestinal side effects after receiving 960 mg of SXT. Conclusions: Our study showed that MDR-TB patients seem to display a consistent PK profile for SMX. Interesting is that the PK values are lower compared to patients with other infectious diseases. Evaluation in a hollow fiber infection model or mouse model is warranted to establish target AUC/MIC value to predict the efficacy of SXT in the treatment of TB. No conflict of interest

Abstracts 12
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_10 PK/PD modeling Activity of the Nitroimidazole TBA-354 Alone and in a Novel Drug Regimen in Two Murine Models of Tuberculosis E. Nuermberger1, K. Williams1, O. Amoabeng1, R. Tasneen1, A. Minkowski1, K. Mdluli2, A. Upton2, Z. Ma2
1Johns Hopkins University, Baltimore, MD, USA; 2Global Alliance for TB Drug Development, New York, NY, USA Background. Two nitroimidazoles, OPC-67683 and PA-824 (Pa), are tuberculocidal in animal models and now in clinical trials for tuberculosis (TB). TBA-354 (T) is a next generation nitroimidazole identified through a medicinal chemistry effort. It is more potent than Pa in vitro against both replicating and hypoxic, non-replicating cultures of Mycobacterium tuberculosis. It is also more active than Pa when administered at the same dose against acute and established TB in BALB/c mice after low-dose aerosol infection. To further evaluate the in vivo potency and efficacy of T, we compared the dose-ranging activity of T and Pa during the initial phase of treatment against a high-dose aerosol infection in BALB/c mice and during the continuation phase of treatment (after 4 wks of standard therapy) in C3HeB/FeJ mice which, unlike BALB/c mice, develop necrotic lung granulomas. Materials & Methods. The dose-ranging study in BALB/c mice used aerosol infection with ~4 log10 CFU of Mycobacterium tuberculosis H37Rv. Daily treatment began 2 wks later and lasted for 8 weeks. The continuation phase experiment used aerosol infection with 2.25-3.0 log CFU and treatment with Pa or T began 10 wks later, after 6 wks of infection and 4 wks of treatment with rifampin, isoniazid, and pyrazinamide (RHZ). Treatment with Pa or T lasted for 8 weeks. Doses were: Pa, 15-600 mg/kg, and TBA-354, 1-100 mg/kg. In the continuation phase experiment, Pa 50 mg/kg and T 10 mg/kg were also administered with bedaquiline (J) 25 mg/kg to evaluate the combined effects. Lung CFU count was the outcome measure in all experiments.
Results. Pa and T had dose-dependent activity in the initial phase in BALB/c mice and the continuation phase in C3HeB/FeJ mice. In the initial phase experiment, T was consistently 10 times more potent than Pa (eg, 2 log kill observed with Pa 100 mg/kg and T 10 mg/kg). However, the maximal effect (~3 log kill) was similar for both drugs. The highest doses selected for cross-resistant organisms after 8 wks of initial phase treatment. In the continuation phase experiment, the mean lung CFU count after RHZ treatment was 4.83. T was more than 5 times more potent than Pa in both mouse strains. Overall effect sizes were similar to those seen in the initial phase of treatment. T 100 mg/kg was at least as active as J 25 mg/kg. No significant antagonism was observed and a trend towards additive activity was observed in C3HeB/FeJ mice. Conclusions. TBA-354 is more potent than PA-824 in initial and continuation phases of treatment, and in pathologically distinct murine models of TB. Novel drug combinations are currently under study. Given the promising clinical activity of Pa observed in trials thus far, T warrants further development for tuberculosis.

Abstracts 13
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_11 PK/PD modeling Population pharmacokinetics (PK) of bedaquiline (TMC207) and its M2 and M3 metabolites with efavirenz (EFV) demonstrate reduced exposure E.M. Svensson1, K.E. Dooley2, F. Aweeka3, J.G. Park4, M.O. Karlsson1
1Uppsala University, Pharamceutical Biosciences, Uppsala, Sweden; 2Johns Hopkins University School of Medicine, Medicine, Baltimore, USA; 3University of California, Clinical Pharmacy, San Francisco, USA; 4Harvard School of Public Health, Center for Biostatistics in AIDS Research, Boston, USA Introduction: Co-infection with HIV and tuberculosis (TB) is common and treatment is complicated by drug-drug interactions. Bedaquiline is an investigational anti-TB agent metabolized to an N-monodesmethyl metabolite (M2) by CYP3A4, an enzyme induced by EFV. M2 is further N-demethyated to M3. Both M2 and M3 are less active in vitro against M. tuberculosis than the parent drug. Methods: Data were obtained from a Phase I pharmacokinetic (PK) trial in 33 healthy volunteers (ACTG Study A5267, JAIDS 2012;59). Subjects were given two single doses of bedaquiline 400 mg, the first alone and the second administered together with EFV after two weeks of EFV 600 mg daily. PK samples were collected over 14 days after each bedaquiline dose. Non-linear mixed effects modeling was performed using NONMEM 7.2 and used to predict relative steady state conditions. The model selection was based on the objective function value and graphical analysis (goodness of fit plots and visual predictive checks). Results: Bedaquiline PK were best described by a 3-compartment disposition model with absorption through a transit compartment model. M2 and M3 were described by 2-compartment models with bedaquiline clearance as input to the M2 central compartment and M2 clearance as input to the M3 central compartment. Oral clearance (CL/F) of bedaquiline was estimated to 2.9 L/h (relative standard error, RSE, 10.8%).
For the metabolites the fraction converted (fm) to respective metabolite was included in the clearance terms which were estimated to 12.2 L/h (RSE 11.3 %) for M2 (CL/F/fmTMC207-M2) and to 39.6 L/h (RSE 10.3%) for M3 (CL/F/fmTMC207-
M2/fmM2-M3). The impact of induction was described as an immediate change in clearance one week after start of EFV treatment. The change in clearance was not significantly different for bedaquiline and M2 and estimated to an increase of 107% (RSE 3.8%). For M3 the change in clearance was smaller but significant, an increase of 11.5% (RSE 3.1%). Relative steady state exposure with and without EFV induction was calculated under different assumptions about the fractions of bedaquiline converted to M2 and of M2 converted to M3, the time for onset of induction, and the induction effect on bioavailability. Under all assumptions, exposure was decreased by 40-50% for both bedaquiline and M2 and while M3 exposure varied between 80 and 110% of the non-induced condition. Conclusions: Based on these analyses, EFV may reduce exposure to bedaquiline and M2 by up to 50% upon chronic co-administration under a range of plausible model assumptions, which is more than previously concluded from the single-dose data (JAIDS). The result was the same with or without M3 data included in the analysis. Given the long terminal half-lives, extrapolation from single dose to steady state is limited by the incomplete PK profiles of bedaquiline and metabolites. Nevertheless, this model-based analysis provides important additional information compared to the non-compartmental analyses. No conflict of interest

Abstracts 14
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_12 PK/PD of new TB drugs Whole blood mycobactericidal activity in a phase I trial of oral bedaquiline (TMC 207) alone and in combination with rifampin or rifabutin C.E. Good1, A.M.B. Healan2, J.L. Blumer3, S.A. Fulton4, M.R. Jacobs5, K. Kreller6, R.A. Salata4, R.S. Wallis7
1University Hospitals Case Medical Center, Pathology, Cleveland, USA; 2Case Western Reserve University, Infectious Disease, Cleveland, USA; 3University of Toledo, Infectious Disease, Toledo OH, USA; 4UHCMC and CWRU, Infectious Disease, Cleveland, USA; 5UHCMC and CWRU, Pathology, Cleveland, USA; 6Clin RM, Project Management, Hinkley OH, USA; 7CWRU and Pfizer, Infectious Disease, Cleveland OH and Groton CT, USA Background: Bedaquiline (BDQ) is a novel diarylquinoline antimycobacterial agent that is metabolized by CYP3A4. This study used the whole blood mycobactericidal assay (WBA) as an index of intracellular activity in a Phase I trial of single BDQ 400 mg doses given both alone and combined either with rifampin (RIF) 600 mg or rifabutin (RBT) 300 mg after 10 days of daily rifamycin dosing. The WBA is an elegant method for assessing in vivo intracellular efficacy of antimycobactericidal agents, using both neutrophils and monocytes. Materials & Methods: Healthy volunteer subjects received BDQ orally on days 1 & 29 and either RIF or RBT for days 20-29. Blood for WBA was obtained at intervals before and after dosing on days 1 & 29. WBA was measured in cultures of 1:1 diluted whole blood as follows. Heparinized whole blood (300 µL) was added to a standardized suspension of Mtb H37Rv in 300 µL RPMI with added 15nM vitamin D3. After 3 days incubation at 35ºC with constant rotation, human cells were lysed, and bacilli were recovered and inoculated into MGIT (Becton Dickinson), where time to positivity was monitored. Log change in viability was calculated per day of whole blood culture, with negative values indicating killing. AUC was calculated by the trapezoidal method.
Results: WBA data were analyzed for 33 subjects. There was mycobacterial growth of 0.19 ± 0.3 log/d at baseline. Maximal killing (log/d±SD), 4-6 hrs after dosing, was -0.32 ± 0.15, -0.92 ± 0.12 and -0.86 ± 0.14 for BDQ, BDQ + RIF, and BDQ + RBT, respectively (P<0.001 for BDQ + RIF and BDQ + RBT vs. BDQ alone by ANOVA). Total killing (AUC0-12hr), was -0.95 ± 0.96, -6.17 ± 1.5, and -8.57 ± 1.2, respectively (P<0.001 for BDQ + RIF and BDQ + RBT vs. BDQ alone and for BDQ + RIF vs. BDQ + RBT by ANOVA). Conclusions: RIF and RBT both significantly added to the intracellular antimycobacterial activity of BDQ. The total activity of BDQ + RBT was superior to BDQ + RIF, presumably reflecting differences in potencies, pharmacokinetics, and intracellular penetration of these rifamycins. No conflict of interest

Abstracts 15
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_13 PK/PD modeling Activity of PNU-100480 and its major metabolite in whole blood and broth culture models of tuberculosis P. Converse1, J. Lee1, R. Tasneen1, K. Williams1, K. Dionne1, N. Parish1, R. Wallis2, E. Nuermberger1
1Johns Hopkins University School of Medicine, Baltimore, MD; 2Pfizer Inc., Groton, CN Background: PNU-100480 (PNU) is an oxazolidinone in Phase 2 trials for tuberculosis (TB). It is rapidly metabolized in vivo to PNU-101603 (PNU’603), which comprises ~85% of the total plasma oxazolidinone exposure after PNU administration in mice and humans. PNU and PNU’603 MICs are 1 dilution lower and equal to, respectively, the linezolid (LZD) MIC against Mycobacterium tuberculosis H37Rv (Mtb). However, despite achieving lower serum drug exposures, PNU has more potent activity than LZD against Mtb infection in mice and in ex vivo cultures of whole blood (WB) from healthy volunteers dosed with either drug. We sought to compare the respective contributions of PNU and PNU’603 to the overall activity of PNU using broth, WB, and J774 macrophage-like cell culture-based TB models. Materials & Methods: Time-kill studies were performed in complete 7H9 broth, as were cell kill experiments in a hollow fiber system (HFS) in which PNU’603 and LZD were dosed alone once daily to mimic the combined steady state PK profile observed after administration of PNU 600 mg twice daily (ie, Cmax = 5.4 ug/ml, AUC0-24h = 29.3 ug-h/ml). WB from healthy volunteers and J774 cell cultures were spiked with Mtb and with PNU, PNU’603 or LZD over a range of concentrations. Results: All 3 compounds showed similar potency in the broth time-kill experiments. PNU’603 and LZD had similar potency in the HFS. However, PNU was at least 10 times more potent than PNU’603 or LZD in WB and J774 culture models. Using plasma PK profiles for PNU and PNU’603 from Phase 1 trials, we calculated cumulative broth and WB activity and
determined that, despite comprising only ~15% of plasma exposure, PNU accounts for 75-80% of the total observed WB activity. In contrast, PNU’603 drives the activity in broth cultures, commensurate with its higher concentrations. These data suggest that the superior activity of PNU over LZD in ex vivo WB and other intracellular infection models (including mice) is driven by the PNU component, which comprises 75-80% of the area under the WBA curve. In contrast, against extracellular Mtb, where PNU and PNU’603 have similar activity (as in broth culture), the overall activity of PNU is likely driven by PNU’603, the dominant species in terms of concentration. Conclusions: If supported by further studies, these results suggest that the relative efficacy of PNU and LZD varies according to the location of infecting bacilli and raise important new questions about the significance of extracellular and intracellular bacillary populations in human TB outcomes.

Abstracts 16
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_14 Toxicity and Safety Pharmacokinetics and safety of moxifloxacin: preliminary results of a dose escalation study in tuberculosis patients A. Pranger1, W.C.M. de Lange2, R. van Altena2, P. van der Harst3, M.P. van den Berg3, D. van Soolingen4, D.R.A. Uges1, J.G.W. Kosterink1, T.S. van der Werf5, J.W.C. Alffenaar1
1University Medical Center Groningen, Hospital and Clinical Pharmacy, Groningen, The Netherlands; 2University Medical Center Groningen, Tuberculosis Centre Beatrixoord, Haren, The Netherlands; 3University Medical Center Groningen, Cardiology, Groningen, The Netherlands; 4National Institute for Public Health and the Environment, National Tuberculosis Reference Laboratory, Bilthoven, The Netherlands; 5University Medical Center Groningen, Internal Medicine and Pulmonary Diseases, Groningen, The Netherlands Background: Moxifloxacin (MFX) has a high in vivo and in vitro activity against Mycobacterium tuberculosis and therefore fulfils an important role in tuberculosis (TB) treatment. For optimal killing of active-dividing M. tuberculosis an AUC0-
24h/MIC ratio of 100 is required. A daily dose of 600-800 mg MFX can be considered to reach this target along with prevention of resistant mutant selection. However, safety data to support this dose escalation in TB patients is limited. We therefore compared pharmacokinetics and safety/tolerability of a standard dose (400 mg) to an escalated dose (600 mg; 800 mg) of MFX as part of the TB regimen in a prospective clinical trial. Material and Methods: Patients received 400 mg MFX once daily as part of their TB regimen at the Tuberculosis Centre Beatrixoord, University Medical Center Groningen (Groningen, The Netherlands) in directly observed treatment (DOT). MFX dose was escalated on the 8th and 15th day of treatment to 600 mg and 800 mg, respectively. Pharmacokinetic sampling (t = 0, 1, 2, 3, 4, 5, 8, 12 and 24h) was performed at steady state (i.e. 7th day of each dose period) along with drug susceptibility testing of patients' M. tuberculosis isolate to determine AUC0-24h, MIC and AUC0-
24h/MIC. During each dose step, safety/tolerability of the escalated dosage,
including AUC0-24h value, QTc prolongation, vital signs (blood pressure, heart rate, and temperature), electrocardiography and laboratory tests (clinical chemistry, urinalysis; including electrolytes (K, Mg, Na, Ca), transaminase values, serum creatinine and bilirubin) were evaluated to prevent toxic exposure or an increased risk of QT prolongation. MFX plasma concentrations were determined by a validated LC-MS/MS method. Drug susceptibility testing was performed using the internationally standardised MGIT (BD) method. Results: We report on the first three patients with MDR-TB, included at the time of writing – three female patients, with extra-pulmonary TB aged 19 - 30 years. The patients were infected with isolates for which the MIC of MFX was 0.125 – 0.25 mg/L. MFX AUC0-24h values of 27, 29 and 31 mg*h/L at 400 mg, of 37, 60 and 37 mg*h/L at 600 mg and of 52, 89 and 80 mg*h/L at 800 mg were calculated. A disproportional AUC0-24h increase was thereby observed in 2/3 patients after escalating the dose to 600 mg and/or 800 mg. No serious clinical adverse effects (including diarrhoea, vomiting, renal or hepatic injury ≥ 2 CTC) with a clear time relationship to MFX were observed. Neither QTc interval > 500 msec, >10% increase of QTc compared to baseline or other abnormalities were identified on the Holter registration. Furthermore, vital signs, ECG monitoring and laboratory tests were normal. Finally, all three patients received 400 mg as part of standard care based on individual AUC0-24/MIC values > 100 (range: 108- 248). Conclusions: Although TDM–guided therapy is still recommended in patients at risk for inadequate treatment at a standard dose, these first data on high dose MFX (600 mg; 800 mg) are promising as a safe option as part of TB regimens but clearly more data are needed. No conflict of interest

Abstracts 17
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract O_15 PK/PD modeling Population pharmacokinetics of rifampicin, pyrazinamide and isoniazid in children with tuberculosis. Model-based evaluation of currently recommended doses. S. Zvada1, P. Denti1, P. Donald2, H. Schaaf2, S. Thee2,3, J. Seddon2,4, H. Seifart5, P. Smith1, H. McIlleron1, U. Simonsson6
1Division of Clinical Pharmacology, University of Cape Town, South Africa; 2Desmond Tutu TB Centre, Department of Paediatrics and Child Health, Faculty of Health Sciences, Stellenbosch University, Tygerberg, South Africa; 3Department of Paediatric Pneumology and Immunology, Charite´, Universitatsmedizin Berlin, Germany; 4Clinical Research Department, Faculty of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London, United Kingdom; 5Division of Pharmacology, Stellenbosch University, Tygerberg, South Africa; 6Department of Pharmaceutical Biosciences, Uppsala University, Sweden. Background: To treat tuberculosis in children, using the dose per kilogram proposed in adults is inadequate and the World Health Organisation recently revised its recommendations to suggest higher daily doses of antituberculosis drugs for children. Materials & Methods: Firstly, we used previously published data to describe the population pharmacokinetics of rifampicin, pyrazinamide and isoniazid in a population of 76 South African children hospitalized for treatment of tuberculosis. Their median age (5th,95th percentile) and median weight (5th,95th percentile) were 2.0 (0.4,7.9) years and 12.5 (5.5,22.7) kg, respectively. Concentration-time data, basic anthropometric information and N-acetylytransferase 2 acetylator status were available on two sampling occasions and were analysed using NONMEM. Secondly, we used the models developed to simulate steady state maximum plasma concentrations and exposures resulting from the World Health Organisation interim dosing guidelines and the newly revised guidelines. Reference plasma concentrations and exposures in adults were derived using
previously published models and the current World Health Organisation guidelines for adults. Results: Rifampicin population pharmacokinetics was best described using a one-compartment model with transit compartment absorption (previously presented at the 3rd International Workshop on Clinical Pharmacology of TB Drugs). Pyrazinamide was best described by one-compartment model, with first-order absorption, while isoniazid was best fitted with a two-compartment model with transit absorption. Allometric scaling based on total body weight was applied on clearance and volume of distribution in all the models to account for body size. In addition, age maturation was supported on clearance and bioavailability for isoniazid and on clearance and absorption mean transit time for rifampicin. The typical oral clearances of rifampicin and pyrazinamide, respectively, were estimated to be 8.05 and 1.12 L/h. Isoniazid typical oral clearances were predicted to be 4.32, 9.09 and 11.7 L/h, respectively, for slow, intermediate, and fast acetylators. These values are for a child weighing 12.5 kg with median age of 2 years. Furthermore, intermediate and fast acetylators were shown to have 20% lower isoniazid bioavailability. For rifampicin, simulations following both interim and newly revised dosing guidelines based on weight bands for the currently available fixed dose combination products showed adequate but more variable exposures than in ethnically similar adults with tuberculosis. However, for pyrazinamide or isoniazid, different exposures to those reported in ethnically similar adults were shown in some weight bands following interim or newly recommended higher doses. Conclusions: Our models describe the population pharmacokinetics of rifampicin, pyrazinamide and isoniazid in children with tuberculosis. Simulations based on our models suggest that for some weight bands, both the recently recommended higher doses and interim guidelines result in different pyrazinamide and isoniazid exposures to those reported in an ethnically similar adult population. No conflict of interest

Abstracts 18
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_16 PK/PD of approved TB drugs PK/PD of first-line antituberculosis drugs and concentrations associated with optimal efficacy in combination therapy regimens in patients J.G. Pasipanodya1, H. McIlleron2, A. Burger3, P.A. Wash3, P. Smith2, T. Gumbo1,4
1Office of Global Health, UT Southwestern Medical Center, Dallas, Texas, USA; 2Division of Pharmacology, Department of Medicine, University of Cape Town, Observatory, South Africa; 3Brewelskloof Hospital, Worcester, South Africa; 4Department of Medicine, UT Southwestern Medical Center, Dallas, Texas, USA Background: Hollow fiber system studies of rifampin, isoniazid, and pyrazinamide monotherapy have suggested that their efficacy, post-antibiotic effects, and prevention of acquired drug resistance (ADR) are linked to area under the concentration-time curve (AUC) and peak (Cmax) to the minimum inhibitory concentration (MIC). Moreover, these studies, together with computer-aided clinical trial simulation, these studies have suggested that the most proximate cause of microbiologic failure and ADR is pharmacokinetic variability. The in silico studies predicted that ADR would be encountered in 0.68% of totally adherent patients within the first 2 months, given the pharmacokinetics described in patients from the Western Cape, South Africa. We examined if this was true in adult patients treated with drug-susceptible tuberculosis. Materials and Methods: Drug concentrations were prospectively collected at 9 different time points during a 24hr period at the end of two months of the initial phase of therapy in 142 patients at the Brewelskloof Hospital, Western Cape Province, South Africa. The patients were then followed for up to two years for relapse, death, and microbiological failure. Poor outcomes were defined as death, relapse or microbiological failure; while, microbiological cure or treatment completion were designated the good outcomes. Compartmental pharmacokinetic analysis was performed for the antituberculosis compounds in ADAPT 5, using
the maximum-likelihood expectation maximization algorithm. The best number of compartments was chosen using Akaike Information Criteria. Next, we performed classification and regression tree (CART) analysis to identify and rank clinical predictors of poor long-term outcome and the two month sputum conversion. Clinical predictors examined included weight, age, gender, and HIV status together with drug Cmax, AUC, and trough concentrations. Results: Isoniazid pharmacokinetics were best described by a two compartment model, while both rifampin and pyrazinamide were best described by a one compartment model. Eleven percent of patients still had positive sputum cultures at two months. The top predictors of two month sputum conversion, in order of importance, were pyrazinamide Cmax, rifampin Cmax, and isoniazid Cmax. Twenty five percent of all patients had poor long-term outcome. The top predictors of poor long term outcome, in order of importance, were pyrazinamide AUC, rifampin AUC, and isoniazid AUC. Threshold AUC and peak concentrations associated with the poor outcomes were selected by CART. Using standard statistical approaches, the odds ratio of poor long term outcomes in patients with the AUC to at least one of these drugs below AUC threshold versus without was 14 (95% confidence interval: 4-49). Altogether Ž91% of patients with poor long-term outcomes had at least one drug with a low AUC. ADR was encountered in 2% of all patients and 0.7% during the first 2 months. All ADR patients had low concentrations of at least one drug. Conclusion: Pharmacokinetic variability drives anti-tuberculosis treatment failure and ADR in patients on a first line anti-tuberculosis regimen. As predicted by pre-clinical models, the PK/PD drivers are AUC and Cmax. Drug concentrations are good early “biomarkers” of long-term outcome in patients treated with multi-drug regimens. We propose that they be used for patient care.

Abstracts 19
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_17 PK/PD modeling The effect of antitubercular drug exposure on disease regression in South African tuberculosis patients E. Chigutsa1, P. Denti1, G. Maartens1, C.M.J. Kirkpatrick2, H. McIlleron3, M. Karlsson4
1University Of Cape Town, Medicine, Cape Town, South Africa; 2Monash University, Centre for Medicine Use and Safety Faculty of Pharmacy and Pharmaceutical Sciences, Melbourne, Australia; 3Monash University, Medicine Division of Clinical Pharmacology, Cape Town, South Africa; 4Uppsala University, Pharmaceutical Biosciences, Uppsala, Sweden Background: In vitro and animal data shows the importance of drug exposure on kill rates of Mycobacterium tuberculosis. However, clinical analyses are limited to comparison of regimens rather than evaluation of the effect of individual drug exposures within regimens. We have previously described the decline in viable Mycobacterium tuberculosis in the sputum during the intensive phase of standard short course chemotherapy in patients with sputum smear-positive pulmonary tuberculosis using the quantitative measure of days to positivity in liquid culture. We have also described the pharmacokinetics of rifampicin and pyrazinamide in the same group of patients. The aim of this work now is to investigate the effect of the pharmacokinetics of the first line antitubercular drugs on the rate of decline of Mycobacterium tuberculosis in sputum from patients. Materials and Methods: Seventy-three patients starting a 5 day per week drug regimen containing rifampicin, isoniazid, pyrazinamide and ethambutol who had both pharmacokinetic and pharmacodynamic data were investigated. Sputum was collected from patients before they started treatment, and then once weekly for 8 weeks. Sputum was processed for culture on liquid media (BACTEC MGIT 960; Becton Dickinson, Sparks, MD) and the days to a positive result were recorded. If no growth was observed after 42 days of incubation, the result was recorded as negative. A non-linear mixed effects time to event model was used to describe the progression of the days to positivity with time
on treatment. Drug plasma concentrations for all the 4 drugs were available and pharmacokinetic models were built to obtain the area-under-the-curve (AUC(0-24)) for each drug. The AUCs were then investigated separately as linear covariates on the kill rates of the bacteria in the sputum. Results: A biexponential decay model was used to characterise decline in bacillary burden of Mycobacterium tuberculosis in patients over the 8 weeks of treatment. The AUC of rifampicin had a significant effect on the alpha slope of the biexponential decay model (p<0.05), with a 2.2% increase in the slope for every AUC unit above the median (45 mg.h/L) and a corresponding decrease for an AUC below the median. Pyrazinamide AUC had a significant effect independently on the beta slope but this did not reach statistical significance when jointly introduced in the model with rifampicin on the alpha slope. Neither isoniazid nor ethambutol exposure significantly influenced the slopes. Conclusion: Rifampicin exposure significantly influences disease regression in patients and this is the first report to quantify the effect in a routine clinical setting. Since the SLCO1B1 rs4149032 polymorphism reduces rifampicin bioavailability, this polymorphism may affect the time it will take a patient to be cured. Studies in a larger patient population are required to confirm our findings. No conflict of interest

Abstracts 20
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_18 PK/PD modeling Pharmacokinetic-pharmacodynamic modelling of tuberculosis treatment response in Malawian adults with smear positive pulmonary tuberculosis D. Sloan1,2,3, H. Mwandumba1,2, E. Corbett1,2, A. Butterworth2, G. Chipungu2, R. Heyderman1, A. Ardrey3, D. Waterhouse3, S. Ward3, S. Khoo3, G. Davies3 1Malawi-Liverpool-Wellcome Trust Clinical Research Programme, Malawi; 2Department of Microbiology, College of Medicine, University of Malawi; 3University of Liverpool, UK Background: Development of new treatments for tuberculosis is limited by a lack of early surrogate markers of outcome for use in Phase II clinical studies. Measuring changes in the sputum bacillary load during the first eight weeks of therapy may help to generate surrogate markers. However, relationships between changes in bacillary load, pharmacokinetic parameters of drug exposure and clinical outcomes are unclear. Pharmacokinetic-pharmacodynamic (PK-PD) modelling can be used to improve understanding of therapeutic response. We present preliminary data from a longitudinal PK-PD study of short course chemotherapy in a cohort of Malawian adults with pulmonary tuberculosis and investigate relationships between clinical presentation, quantitative bacteriology, plasma drug concentrations, and treatment outcome. Materials & Methods: Adults with a first presentation of smear ‘++’ or ‘+++’ pulmonary TB were recruited and treated with standard 6 month therapy. At 5 time-points during the first 8 weeks, decontaminated sputum was set up for liquid culture. Time-to-positivity (TTP) of these cultures was recorded in days and used as an inverse measure of bacillary load. Blood was collected at 0, 2 and 6 hours post-dose on day 14 or 21 of therapy for measurement of the plasma concentration of sterilising drugs (rifampicin and pyrazinamide) by High Performance Liquid Chromatography (HPLC) Patients were followed until 1 year post-treatment and classified as “responders” (sustained cure) or “non-responders” (treatment
failure or relapse). Modelling changes in TTP during therapy was done using a linear mixed effects model. Pharmacokinetic parameters (Cmax and AUC) were calculated from individuals with valid concentration-time profiles. Relationship between study parameters and treatment outcome was done by logistic regression. All data analysis was done in ‘R’. Results: 169 eligible patients were recruited. 95 (56%) were HIV infected. From 138 patients who completed follow-up, there were 11 (8%) non-responders (9 failures and 2 relapses). Amongst responders, the median TTP of sputum culture was 7.9 (range: 5.9-11.5) days at baseline and increased by 0.41 (range: 0.01-0.92) days per day of treatment. Amongst non-responders, the median TTP at baseline was 7.2 (range: 5.86-8.13) days and the rate of increase during treatment was 0.21 (range: -0.01-0.42) days per day. A slower rate of change in TTP during therapy was associated with non-response (OR: 118.5, 95% CI: 2.49-5630.01, p=0.009). Pharmacokinetic data from the first 33 patient suggests that median plasma concentrations of sterilising drugs were low (Rifampicin Cmax: 3.47µg/l, AUC0-6h 14.66 µg-h/l, AUC0-infinity: 20.01 µg-h/l, Pyrazinamide Cmax: 22.6µg/l, AUC0-6h: 155.54 µg-h/l, AUC0-Infinity: 410.33 µg-h/l. Initial analysis suggests no association between the AUC of these drugs and treatment outcome, but full assessment awaits analysis of samples from the entire study cohort. Conclusions: In a mixed cohort of HIV-infected and uninfected patients, a slower rate of change in TTP of liquid culture during therapy was predictive of response. This is important and will be useful in developing surrogate markers of outcome for Phase II clinical trials. Plasma drug concentrations of rifampicin and pyrazinamide from a subset of patients were low but an association between pharmacokinetic parameters and treatment outcome has not been demonstrated so far.

Abstracts 21
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_19 PK/PD of approved TB drugs Moxifloxacin PK/PD properties and the role of efflux pumps in a novel hollow fiber model of Mycobacterium kansasii. S. Srivastava1,2, C. Sherman2, T. Gumbo1,2
1Office for Global Health, UT Southwestern Medical Center, Dallas, Texas; 2Department of Medicine, UT Southwestern Medical Center, Dallas, Texas Background: Mycobacterium kansasii (Mkn) is the second most common cause on non-tuberculous mycobacterial lung disease in the USA. Treatment is patterned on that of tuberculosis, with rifampin, isoniazid, and ethambutol administered for 12 months after negative sputum. Frequently, the therapy duration is longer. Shorter courses are associated with high relapse rates. Nevertheless, the duration of therapy is too long. We are interested in reducing the duration of therapy to six months, or less, via design of new drug regimens and pharmacokinetic/ pharmacodynamics (PK/PD) based dose optimization. Moxifloxacin is being investigated in a role to shorten anti-tuberculosis therapy regimens; we wanted to examine its PK/PD properties against Mkn. We also wanted to examine the role of efflux pumps in Mkn resistance emergence. Materials and Methods: Extracellular and intracellular minimum inhibitory concentrations (MICs) were determined by broth dilution and resazurin colorimetric assays. Next we created a novel hollow fiber system (HFS) model of intracellular Mkn. THP-1 macrophages were infected with Mkn, and then inoculated into peripheral compartment of HFS that had RPMI-1640 and 2% FBS. The HFS model was used in moxifloxacin PK/PD studies of human dose equivalents of 0, 25, 50, 100, 200, 400, 600 and 800 mg a day for 14 days. In addition, two extra systems also received the efflux pump inhibitor reserpine plus either moxifloxacin 400 mg or 200 mg/day. A moxifloxacin half-life of 12 hrs was utilized, as well as concentrations achieved in epithelial lining fluid and alveolar macrophages. The central compartment was sampled at 7 time
points to validate moxifloxacin pharmacokinetics. Samples from the peripheral compartment were collected on day 0, 3, 7, 10 and 14 to enumerate total as well as moxifloxacin-resistant sub-population. Macrophage counts were performed at each sampling time. Results: Moxifloxacin MIC was 0.03 mg/L based on all methods, including the resazurin assay. For the HFS studies, the inhibitory sigmoid Emax relationship between moxifloxacin (dose in mg/day) and Mkn on day 14 was: Effect (log10 CFU/ml)=9.8-9.8*Dose2.0/(69.82.0 + Dose2.0) where the ED50 is 69.8 mg/kg and the Hill-factor is 2.0 (r2=0.998). The doses 400 mg/day plus reserpine and 800 mg/day had sterilized HFS by day 7; 200 mg/day plus reserpine; and 400 and 600 mg/day had sterilized HFS by day 14. Conclusion: First, the standard laboratory strain demonstrated an MIC greater than the MIC50 of clinical isolates, and 1-tube dilution lower than the MIC90, so that our isolate has a higher MIC than majority of clinical strains. Nevertheless, moxifloxacin was associated with rapid kill of the Mkn strain in the HFS. The ED90 dose calculates as 215 mg/day. A moxifloxacin containing combination regimen with rifampin should be further investigated and compared to the standard regimen in the HFS.

Abstracts 22
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_20 Therapeutic Drug Monitoring An International Interlaboratory Quality Control (QC) Program for Bio-analysis of Tuberculosis Drugs R. Aarnoutse1, M.G.G. Sturkenboom2, K. Robijns3, A. Harteveld3, B. Greijdanus2, D.R.A. Uges2, D.J. Touw3, J.W. Alffenaar2
1Radboud University Nijmegen Medical Centre, Department of Pharmacy, Nijmegen, The Netherlands; 2University Medical Centre Groningen, Department of Hospital and Clinical Pharmacy, Groningen, The Netherlands; 3Association for Quality Assessment in TDM and Clinical Toxicology, Bureau of the Association for Quality Assessment in TDM and Clinical Toxicology, The Hague, The Netherlands Introduction: Analytical methods for tuberculosis (TB) drugs are being applied in pharmacokinetic (PK) studies and in Therapeutic Drug Monitoring (TDM) for TB drugs. Intralaboratory (internal) method validation, intralaboratory QC procedures and participation in an interlaboratory (external) QC program (or proficiency testing program) are required to ensure that these analytical methods have sufficient accuracy. So far there has been no interlaboratory QC program for TB drugs. The Association for Quality Assessment in TDM and Clinical Toxicology in The Netherlands has extensive experience in offering international QC programs for antiretroviral drugs and antifungal drugs. We started an international interlaboratory quality control (QC) program for first-line and second-line TB drugs in serum. Results of the pilot round are presented. Methods: Drug-free human serum was spiked with isoniazid, rifampicin, pyrazinamide, ethambutol, moxifloxacin and linezolid to obtain two QC samples, each containing the 6 drugs in either a low or median/high concentration. All drug substances were of analytical quality and had a high and specified purity. Samples were freeze-dried because of the instability of some of the drugs involved and to decrease shipping costs. Stability under these circumstances had been validated before. Seven laboratories in Europe and the USA participated in this first pilot round of the program. They were requested to
analyze the samples within 6 weeks after dispatch. Considering the limited number of participants and measurements in this pilot round, results were only presented descriptively. Twenty percent limits around the weighed-in concentrations (i.e. an accuracy between 80 and 120% ) were considered to be appropriate thresholds for a satisfactory measurement. These thresholds are derived from guidelines for analytical method validation, in which 20% deviations are often used as a fixed criterion for inaccuracy at the lowest level of quantitation. Results: Two laboratories were able to measure all 6 TB drugs, one laboratory measured 5 drugs, two laboratories measured 4 drugs and the remaining laboratories analyzed less drugs. A total of 58 analyses were performed, with satisfactory results reported for 48 measurements (83%). Measurements of isoniazid, rifampicin, pyrazinamide, ethambutol, moxifloxacin and linezolid yielded satisfactory results in 14/14 (100%), 5/12 (42%), 10/10 (100%), 9/12 (75%), 6/6 (100%) and 4/4 (100%) of the analyses respectively. Three out of 7 laboratories performed all measurements within 20% inaccuracy limits. The concentration level did not appear to affect accuracy, as 24/29 (83%) of the measurements was performed satisfactorily both at the low and median/high concentration levels. Rifampicin concentrations were too low in 3 laboratories both at the low and median/high concentration, suggesting systematic errors in one direction. All laboratories were informed about their own performance to enable them to optimize their analytical methods or other QC procedures (eg dilutions, pipetting, calculations, clerical reporting) if applicable. Conclusions: An interlaboratory QC program for TB drugs was developed. The program alerted some laboratories to previously undetected problems and will enable them to improve their assays or procedures. The program will be open for more laboratories to participate. No conflict of interest

Abstracts 23
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_21 Therapeutic Drug Monitoring Dried blood spot analysis for PK/PD optimization of linezolid in MDR-TB treatment D.H. Vu1, M.S. Bolhuis2, R.A. Koster2, B. Greijdanus2, W.C.M. de Lange3, R. Altena3, J.R.B.J. Brouwers1, D.R.A. Uges2, J.W.C. Alffenaar2
1Groningen Institute for Drug Studies, Department of Pharmacotherapy and Pharmaceutical Care, Groningen, The Netherlands; 2University Medical Center Groningen, Department of Hospital and Clinical Pharmacy, Groningen, The Netherlands; 3University Medical Center Groningen, Tuberculosis Center Beatrixoord, Groningen, The Netherlands Introduction: Linezolid is a promising antimicrobial agent for the treatment of multidrug-resistant tuberculosis (MDR-TB), but its use is limited by severe toxicity. Therapeutic drug monitoring (TDM) may help to minimize toxicity whilst adequate drug exposure is maintained. Conventional plasma sampling and monitoring might be hindered by logistic problems in most parts of the world. The use of dried blood spot (DBS) sampling may provide a helpful alternative to conventional plasma sampling. The aim of this study is to develop and validate a novel method for TDM of linezolid in MDR-TB patients using DBS. Materials & Methods: Plasma, venous DBS (VDBS) and capillary DBS specimens were obtained simultaneously from eight MDR-TB patients receiving linezolid. VDBS specimens were prepared by pipetting 50µL venous blood onto paper. To quantify DBS samples, a disc was punched out of each blood spot. After a newly developed extraction, the samples were analysed using a validated LC-MS/MS method. The DBS method was validated in accordance with the recommendation of US Food and Drug Administration's Guidance for Industry Bioanalytical Method validation. Additionally, the impact of hematocrit (Hct) and blood spot volume were evaluated. The DBS method was clinically validated by comparing DBS with plasma results using Passing Bablok regression and Bland-Altman plot. The AUC0-12h/MIC values were also calculated from each type of sample.
Results: The DBS assay method showed linearity over the analytical concentration range (r2=0.9947). DBS analysis method proved to be reproducible and robust. DBS specimens were stable at 370C for 2 months and at 500C for one week. Variation of blood spot volume between 30-90µL had a minor impact on the assay accuracy. Variation in Hct from 20% to 50%, an even broader range than clinical Hct values found in TB patients, resulted in acceptable biases. The concentration ratio of DBS/plasma was 1.2 (95%CI: 1.12-1.27) and of VDBS 1.36 (95%CI: 1.32-1.40). When the AUC0-12h values of DBS and VDBS were calculated, using these conversing factors, all values were within the 95% limit of agreement. Furthermore, a high correlation of AUC0-24h/MIC values between conversed DBS and plasma (Spearman's rho=0.97, n=8) was observed. Conclusions: This study presents a validated analysis of linezolid in DBS specimens that is suitable for optimization of linezolid treatment of MDR-TB. Advantages include a very simple, low biohazard risk sampling method using a finger prick, easy logistics and very good stability of DBS specimens. With a simple instruction, the DBS samples can be performed easily and sent to equipped facilities for analysis by mail. This could enable the TDM in TB-programs worldwide including resource limited settings where MDR/XDR-TB epidemic is a growing problem. No conflict of interest

Abstracts 24
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_22 Therapeutic Drug Monitoring Robust and throughput method for simultaneously determination rifampicin, clarithromycin and metabolites in dried blood spots using LC-MS/MS D. Vu1, M. Bolhuis2, R. Koster2, B. Greijdanus2, W. de Lange3, R. Altena3, J. Brouwers1, D. Uges2, J.W. Alffenaar2
1Groningen Institute for Drug Studies, Department of Pharmacotherapy and Pharmaceutical Care, Groningen, The Netherlands; 2University Medical Center Groningen, Department of Hospital and Clinical Pharmacy, Groningen, The Netherlands; 3University Medical Center Groningen, Tuberculosis Center Beatrixoord, Groningen, The Netherlands. Introduction: Rifampicin (RIF) is the most important first-line drug for the treatment of tuberculosis. However, the inter-patient variability in its bioavailability suggested that therapeutic drug monitoring (TDM) is benefit to maintain efficacy and avoid emerge of drug resistance. In addition, clarithromycin (CLR) is used to treat MDR-TB and combine with rifampicin in the treatment of Mycobacterium ulcerans. The drug interaction through cytochrome P450 3A4 was warrant in which rifampicin may cause the decrease in CLR blood concentration. It is noticed that the conventional TDM using plasma sampling is limited due to number of logistic difficulties. Dried blood spot (DBS) sampling is easy to implement and transport with high stability may be a better choice to extend TDM to rural area where epidemic is more frequent. The aim of this study was to develop a robust and throughput analytical method to simultaneously determine rifampicin and clarithromycin and their active metabolites, desacetyl rifampicin (DAc-RIF) and hydroxyl clarithromycin (14OH-CLR), in DBS and clinically validate the method on TB/MDR-TB patients. Materials & Methods: A simple DBS analytical method was develop to avoid the interference of endogenous components and produce a quick and reliable result. To quantify DBS samples, a disc was punched out of each blood spot,
extracted by an optimize procedure and analyzed using LC-MS/MS. The method was validated according to the US Food and Drug Administration's Guidance for Industry Bioanalytical Method validation. Furthermore DBS method was clinically validated by comparing analytical result of DBS and plasma sample attaining from TB and MDR-TB patients by ordinary linear regression. Results: The DBS analytical method was linear over the analytical concentration range (RIF: 0.15-30mg/L, DAcRIF, CLR, 14OH-CLR: 0.05-10mg/L). The three day validation showed that the accuracy (presented as bias) and within-day, between-day precision (presented as covariation coefficient) was less than 15%. CLR and 14OH-CLR in DBS were stable after storing at 500C, 370C and room temperature for at least 15days, 30days and 2 months, respectively. RIF and DAc-RIF were stable for 3 days at 500C, 10 days at 370C and 2 months at room temperature. The linear regression equation between DBS (y) and plasma (x) concentrations were: CLR: y=0.80x-0.13, r2=0.9785, n=10; 14OH-CLR: y=1.1x-1.1, r2=0.9421, n=10; RIF: y=0.86x+0.17, r2=0.9067, n=33; DAc-RIF: y=0.78x+0.18, n=25. Identical result from DBS and plasma samples in which analytes concentration lower than lower limited of quantification suggested that DBS can be used to detect the non-adherence to the treatment or the mal-absorption patients. Conclusions: We successfully developed and validated a robust and throughput method to simultaneously determine rifampicin and clarithromycin and metabolites in DBS. The method was clinically validated on TB and MDR-TB patients. The high stability of the samples enables the application of DBS sampling on the TDM of these drugs in rural resources-limited areas. The DBS analytical result can be used to estimate the drugs exposure and therefore to ensure the efficacy, avoid the toxicity and detect the non-adherence.

Abstracts 25
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Abstract: O_23 Toxicity and Safety Effect of limit of detection on analyses of bacteriological biomarkers in TB clinical trials G. Davies1, T. Mthiyane2, C. Lienhardt3, A. Martineau4
1Institutes of Infection and Global Health and Translational Medicine, University of Liverpool UK; 2South African Medical Research Council, Durban, South Africa; 3Stop TB Partnership, World Health Organization, Geneva, Switzerland; 4Centre for Primary Care and Public Health, Barts and The London School of Medicine and Dentistry Background: Longitudinal measurements of bacteriological biomarkers are increasingly advocated in early phase clinical trials to facilitate PK-PD analysis and enhance the power of dose-finding and screening of combinations of drugs. Currently the two most commonly reported such endpoints are serial sputum colony counts on selective solid medium and time-to-positivity in automated liquid culture systems. Mixed effects modelling techniques have proven to be a suitable approach to these data, flexibly capturing the pattern of treatment response while accounting effectively for high inter-individual variability. However, there is uncertainty concerning the effect of the potentially substantial proportion of data that may be unobserved during these studies due to the limit of detection (LOD) of the bacteriological method. We have applied two different analytical approaches to this missing data problem, one based on conditioning the likelihood of the model according to the LOD and one on a Bayesian approach to interval censoring, with a view to assessing whether statistical inferences about treatment effect are robust in this situation. Materials & Methods: Longitudinal bacteriological biomarker data was available from two clinical trials: Study 1 (OFLOTUB IIB) was a four arm study based on serial colony counting on solid media and Study 2 (AdjuVIT) was a two arm study based on serial time-to-positivity in automated liquid culture (MGIT). To account for the effect of censoring due to limit-of-detection issues, these data were re-analysed using the conditional likelihood approach (M3 method) in NONMEM VI v2 and the I() function in WinBUGS 1.4.
Results: Study 1 was re-analysed using both the NONMEM and WinBUGS approaches. The magnitude of treatment effect estimated by NONMEM, ignoring data below the LOD was larger than suggested by the original analysis. The M3 approach resulted in an altered absolute trajectory for the parameter ?4 but the same relative magnitude of treatment effect as the original analysis. The Bayesian formulation of the model for Study 1 produced predictions of response that were slightly different from the pure likelihood methods but reassuringly similar estimates of treatment effect. The method incorporating left-censoring supported a steeper profile of response with a numerically larger estimate of treatment effect. Study 2 was reanalysed using the WinBUGS method alone due to the right rather than left censoring which is not suitable for the unmodified M3 method on the original scale of response. The Bayesian model produced a less steep profile of response overall but a similar inference about lack of treatment effect. Conclusions: As longitudinal analyses become more commonplace in Phase II trials in TB and bacteriological biomarkers with differing sensitivities are applied to regimens of improved potency, dealing correctly with data below the LOD will become increasingly important. The conditional likelihood and Bayesian methods evaluated here are regarded as rigorous and non-arbitrary approaches to this problem. These preliminary results suggest however that naive inferences about treatment effect are reasonably robust even in the presence of substantial proportions of observations below the LOD.

Abstracts 26
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA

Abstracts 27
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Author Index
Author Abstract Title Abstract # Page # Aarnoutse, R.
A randomized trial comparing pharmacokinetics, safety and patient survival of standard versus intensified antibiotic treatment for TB meningitis
O_03
05
Aarnoutse, R.
Pharmacokinetics of anti-tuberculosis drugs in Venezuelan children: supportive evidence for the revised WHO dosing recommendations
O_07
09
Aarnoutse, R.
An International Interlaboratory Quality Control (QC) Program for Bio-analysis of Tuberculosis Drugs
O_20
22
Boeree, M.
What is the “right” dose of rifampin? An interim report.
O_02
04
Bolhuis, M.
Clarithromycin shows a trend towards increase of linezolid exposure in multidrug-resistant tuberculosis
O_08
10
Chigutsa, E.
The effect of antitubercular drug exposure on disease regression in South African tuberculosis patients
O_17
19
Davies, G.R.
Pharmacokinetic-pharmacodynamic modelling of tuberculosis treatment response in Malawian adults with smear positive pulmonary tuberculosis
O_18
20
Davies, G.R.
Effect of limit of detection on analyses of bacteriological biomarkers in TB clinical trials
O_23
25
de Knegt, G.
Optimization of the rifampin dosage to improve the therapeutic efficacy in tuberculosis treatment, using a murine model
O_01
03
Good, C.
Whole blood mycobactericidal activity in a phase I trial of oral bedaquiline (TMC 207) alone and in combination with rifampin or rifabutin
O_12
14
Nuermberger, E.
Activity of the Nitroimidazole TBA-354 Alone and in a Novel Drug Regimen in Two Murine Models of Tuberculosis
O_10
12
Nuermberger, E.
Activity of PNU-100480 and its major metabolite in whole blood and broth culture models of tuberculosis
O_13
15
Pasipanodya, J.
PK/PD of first-line antituberculosis drugs and concentrations associated with optimal efficacy in combination therapy regimens in patients
O_16
18
Pranger, A.
Evaluation of Co-trimoxazole in treatment of multidrug resistance tuberculosis
O_09
11
Pranger, A.
Pharmacokinetics and safety of moxifloxacin: preliminary results of a dose escalation study in tuberculosis patients
O_14
16
Requena Mendez, A.
Effect of dose size and food on pharmacokinetics of isoniazid in peruvian TB patients
O_04
06
Savic, R.
Population pharmacokinetics of once weekly rifapentine in children and adults
O_06
08
Srivastava, S.
Moxifloxacin PK/PD properties and the role of efflux pumps in a novel hollow fiber model of Mycobacterium kansasii.
O_19
21
Svensson, E.
Population pharmacokinetics (PK) of bedaquiline (TMC207) and its M2 and M3 metabolites with efavirenz (EFV) demonstrate reduced exposure
O_11
13
Vu, D.H.
Dried blood spot analysis for PK/PD optimization of linezolid in MDR-TB treatment
O_21
23

Abstracts 28
5th International Workshop on Clinical Pharmacology of Tuberculosis Drugs – 8 September 2012 – San Francisco CA, USA
Author Abstract Title Abstract # Page # Vu, D.H.
Robust and throughput method for simultaneously determination rifampicin, clarithromycin and metabolites in dried blood spots using LC-MS/MS
O_22
24
Weiner, M.
Rifapentine Pharmacokinetics and Tolerability in Children and Adults Treated Once Weekly with Rifapentine/Isoniazid for Latent Tuberculosis Infection
O_05
07
Zvada, S.
Population pharmacokinetics of rifampicin, pyrazinamide and isoniazid in children with tuberculosis. Model-based evaluation of currently recommended doses.
O_15
17

Program & Abstractswww.virology-education.com
Biltstraat 1063572 BJ Utrechtthe Netherlandswww.virology-education.com
SAN FRANCISCO, CA 8 September 2012 USA
5 th





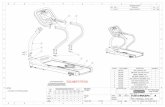



![3572 [PDF Library]](https://static.fdocuments.us/doc/165x107/577d28e91a28ab4e1ea58739/3572-pdf-library.jpg)









