Primary colorectal tumors and their metastasis are genetically not the same: Implication for choice...
-
Upload
raymond-bond -
Category
Documents
-
view
212 -
download
0
Transcript of Primary colorectal tumors and their metastasis are genetically not the same: Implication for choice...

Primary colorectal tumors and their metastasis are genetically not the same: Implication for choice of targeted therapy? ASCO 2011 Abstract #3535
Joost Vermaat1*, Isaac Nijman2*, Marco Koudijs1, Frank Gerritse1, Stefan Scherer3 , Michal Mokry2, Wijnand Roessing1, Nico Lansu2, Ewart de Bruin2, Richard van Hillegersberg4, Paul van Diest5, Edwin Cuppen2,6, Emile Voest1
Department of 1Medical Oncology, 4Surgery , 5Pathology, 6Human Genetics; University Medical Center Utrecht, 2Hubrecht Institute Genome Biology and Bioinformatics group, The Netherlands; 3Hoffman-La Roche Inc. / Genetech, NJ, USA [email protected]
STUDY DESIGN
BACKGROUND
CONCLUSIONS
RESULTS (1): Technical Overview of Sequenced Data RESULTS (3): Dissimilarities between Primary CRC tumor and liver metastasis
PATIENTS AND METHODS
• On average 83 mutations were gained in the metastasis and 70 variations were lost (Figure-3).
• No differences in the overall number of genetic variations between primary tumor and liver metastasis were detected.
• Non-tumor tissue of five patients, obtaining 192 variants (2%) which were commonly found.
• Chemotherapy between removal of the primary tumor and the metastasis did not further increase the amount of genetic variation.
• In almost all 21 CRC patients, we found aberrations in the coding regions of the KRAS and EGFR gene (both>90%) either in the primary tumor and/or liver metastasis.
• Dissimilarities of the KRAS and EGFR mutational status between both tumor entities were detected in 57% and 62% of the 21 CRC patients (Table-2). High concordance for codon 12 and 13 mutations!
• In all patients protein-altering genetic aberration in genes downstream of EGFR were identified, including MAP3K1, MAPK10, PLCG1, PIK3CG, PRKCB, and RAF1.
• In total, 118 variations in 32 genes were validated with a true-positive rate of 84%.
• As depicted in Figure-2, in total 8,405 genetic variations were detected in 1,264 diverse genes.
• 8,001 Single Nucleotide Variations (SNV’s) and 404 small (5%) insertions or deletions were identified.
• 16% of genetic variations were novel variations.
• In total, 1,414 non-synonymous mutations were detected including 281 which were predicted as probably damaging (p>0,85, using polyphen2).
RESULTS (2): Total Number of Identified Genetic Variations
Acknowledgements
In the era of personalized cancer care, the analysis of the tumor genome will become an important aid in clinical decision making for patients with cancer. In colorectal cancer (CRC), KRAS and BRAF mutations are already incorporated in algorithms for treatment with EGFR antibodies. This supports the notion that the mutational status of a gene in the primary tumor can guide therapeutic strategies. However, given the genomic instability of tumors, it can be questioned whether the primary tumor reflects the genetic background of the metastases. We therefore embarked on a study to compare the primary tumor with its subsequent metastases for 1264 genes with ´next generation sequencing´ technology in a cohort 21 CRC patients.
• We selected 21 metastatic colorectal cancer (mCRC) patients who underwent resection of the primary tumor and at a later stage resection of their liver metastasis. All patients were treated at the University Medical Center of Utrecht (UMC Utrecht) between 1999 and 2009.
• FFPE tissue of the primary tumor and its corresponding liver metastatis was collected.
• Time between the resection of the primary tumor and the liver metastasis was at least 6 months.
• 11 mCRC patients received chemotherapy (5-Fluorouracil combined with Oxaliplatin) between both resections where the other 10 mCRC patients were not treated with chemotherapy between the surgical interventions.
• We have successfully sequenced the exons of 1,264 crucial genes relevant to the biology and treatment of cancer of the primary tumor and the corresponding liver metastasis of FFPE material from 21 mCRC patients.
• Significant losses and gains of genetic variations in relevant genes demonstrated that there are significant differences between the primary tumor and its corresponding liver metastases. This suggests that a genetic analysis of the metastasis at the start of treatment may be preferred over archived material of the primary tumor in developing treatment algorithms.
• This study was supported by grants from Roche and the Dutch Foundation ‘Barcode for Life’.
• Variation candidates were strictly filtered to suppress the false positive rates.
• Genetic variations were considered when the regions were covered for at least 10x and non-reference calls were supported by two indepedent reads on each strand.
• A genetic variation was determined in the non-reference allel with a frequency of at least 35%.
• Next, a random assigned subset of our identified candidate genetic varations was validated with conventional sequencing techniques to elucidate false positive and negative rates.
• ‘Cancer Mini-Genome’We have composed a ‘Cancer Mini-Genome’ consisting of 1,264 genes including relevant kinases and pathways important for carcinogenesis and targeted treatment.
• Genome Sequencing PipelineWe have validated a genome sequencing pipeline (Figure 1) using fresh frozen and formalin-foxed paraffin-embedded (FFPE) of healthy tissue.
• TechniquesFor the selection of the exonic regions of our ‘Cancer Mini-Genome’ we used common CGH-capture arrays (Agilent). Subsequently, samples were sequenced by the SOLiD 3+ system (Applied Biosystems).
• Data-Analysis Sequence data is mapped against the human reference genome (GRCh 37, www.ensembl.org) using BWA. To limit the influence of SNV caller artifacts, we applied three different SNV callers (custom PERL script, VarScan and the GATK toolkit) and considered the overlapping variants (33±10% ) as high-confidence variants. To predict the possible impact of the identified variation on amino acid structure and thus the protein function, PolyPhen-2 (Polymorphism Phenotyping version2) was used.
• Functional AnalysisOnly predicted variations with a probable consequence on protein level (non-synonymous, frameshift, essential splice sites and stop-gain/lost) were considered as relevant aberrations in our study and named ‘functional’ genetic variations.
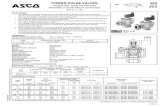
Healthy Tissue
Primary Colorectal
TumorLiver
MetastasisOverall mean
Overall Range
N=5 N=21 N=21 N=46 N=46
Mean number of reads 29,206,762 34,031,468 38,671,220 35,591,282 21-70 x 106
mapping percentage 59.00 62.71 62.57 62.26 51-80 x 106
Mean number of mapped reads 14,151,812 22,571,654 26,435,760 23,402,441 12-51 x 106
Percentage on target 48.60 66.33 66.95 64.72 42-85 % Mean number of reads on target 6,955,220 15,167,653 18,504,941 15,785,119 5-43 x 106
Mean target sequence (Mbp) 348 758 925 789 250-2150 Mean coverage of requested target 97.60 156.76 183.86 162.57 81-359 Median coverage of requested target 63.00 85.43 94.14 86.94 52-217 Percentage of requested target covered 98.94 98.68 98.69 98.71 97-99 % Percentage of designed target covered 94.17 93.62 93.58 93.66 91-96 % Percentage of requested target covered >=20x 78.68 79.03 79.70 79.29 71-88 % Percentage of designed target covered >=20x 85.38 85.74 86.45 86.02 77-95 %
Table 1 – General sequencing results per individual tissue
Figure 2: Overview of identified Genetic Variations
Figure 3: Genetic differences between primary tumors and their comparative liver metastases. Results are presented as loss or gain of relevant mutations per individual patient.
Table 2: Comparison of SNV’s of relevant CRC genes between primary tumor and liver metastasis
Gene
No. of patients with identified SNV's in either primary tumor, liver metastasis, or both
No. of patients with identified SNV's not identical in primary tumor and liver
metastasisKRAS 19 / 21 (90%) 12 / 21 (57%)
EGFR 20 / 21 (95%) 13 / 21 (62%)
PI3K 14 / 21 (67%) 3 / 21 (14%)
Flt-1 16 / 21 (76%) 4 / 21 (19%)
KDR 4 / 21 (19%) 1 / 21 (5%)
PTEN 4 / 21 (19%) 1 / 21 (5%)
BRAF 7 / 21 (33%) 3 / 21 (14%)