Overproduction of inter-a-trypsin inhibitor heavy chain 1 after ...However, phospho-Akt was notably...
Transcript of Overproduction of inter-a-trypsin inhibitor heavy chain 1 after ...However, phospho-Akt was notably...

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
METABOL I SM
1College of Pharmacy and Research Institute of Pharmaceutical Sciences, SeoulNational University, Seoul 08826, Korea. 2Department of Biochemistry, BK21 PLUSProgram for Creative Veterinary Science Research and Research Institute for Vet-erinary Science, College of Veterinary Medicine, Seoul National University , Seoul08826, Korea. 3Korea Mouse Metabolic Phenotyping Center, Lee Gil Ya Cancer andDiabetes Institute, Gachon University School of Medicine, Incheon 21999, Korea.4College of Korean Medicine, Daegu Haany University, Gyeongsan, Gyeongsang-buk-do 38610, Korea. 5Department of Pharmacology, Institute of Biomedical Sci-ence, College of Medicine, Hanyang University, Seoul, Korea. 6Endocrinology,Internal Medicine, Gachon University Gil Medical Center, Incheon 21565, Korea.7Interdisciplinary Program in Genetic Engineering, Seoul National University,Seoul 08826, Korea. 8Division of Gastroenterology and Hepatology, Departmentof Internal Medicine, College of Medicine, Seoul National University, Seoul Metro-politan Government Boramae Medical Center, Seoul, Korea.*Corresponding author. Email: [email protected] (S.G.K.); [email protected] (W.K.)
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019
Copyright © 2019
The Authors, some
rights reserved;
exclusive licensee
American Association
for the Advancement
of Science. No claim
to original U.S.
Government Works
http://stm.scien
Dow
nloaded from
Overproduction of inter-a-trypsin inhibitor heavy chain 1after loss of Ga13 in liver exacerbates systemic insulinresistance in miceTae Hyun Kim1, Ja Hyun Koo1, Mi Jeong Heo1, Chang Yeob Han1, Yong-In Kim2, Shi-Young Park3,Il Je Cho4, Chang Ho Lee5, Cheol Soo Choi3,6, Jung Weon Lee1,7, Won Kim8*,Je-Yoel Cho2, Sang Geon Kim1*
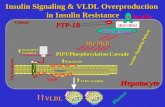
The impact of liver disease on whole-body glucose homeostasis is largely attributed to dysregulated release of secre-tory proteins in response to metabolic stress. The molecular cues linking liver to whole-body glucose metabolismremain elusive. We found that expression of G protein a-13 (Ga13) was decreased in the liver of mice and humanswith diabetes. Liver-specific deletion of theGna13 gene inmice resulted in systemic glucose intolerance. Comparativesecretome analysis identified inter-a-trypsin inhibitor heavy chain 1 (ITIH1) as a protein secreted by liver that wasresponsible for systemic insulin resistance inGna13-deficient mice. Liver expression of ITIH1 positively correlatedwithsurrogate markers for diabetes in patients with impaired glucose tolerance or overt diabetes. Mechanistically, adecrease in hepatic Ga13 caused ITIH1 oversecretion by liver through induction of O-GlcNAc transferase expres-sion, facilitating ITIH1 deposition on the hyaluronan surrounding mouse adipose tissue and skeletal muscle. Neutral-ization of secreted ITIH1 ameliorated glucose intolerance in obese mice. Our findings demonstrate systemic insulinresistance in mice resulting from liver-secreted ITIH1 downstream of Ga13 and its reversal by ITIH1 neutralization.
ce
at Seoul National U
niversity Library on Novem
ber 17, 2019m
ag.org/
INTRODUCTIONThe metabolic network among tissues is mediated by hormones, cyto-kines, or other secretory proteins that have paracrine or endocrineactions on other organs, maintaining systemic nutrient and energyhomeostasis. Perturbations in this cross-talk can provoke disorders inglucose metabolism, often accompanied by insulin resistance and dia-betes. Insulin resistance is characterized by impaired insulin signaling inmultiple metabolic organs including liver, adipose tissue, and skeletalmuscle. Most of the nutrients absorbed by the intestine first passthrough the liver, where two-thirds of blood glucose is assimilated.Hence, the liver senses and responds quickly to nutritional changes, reg-ulating systemic glucosemetabolism. Therefore,metabolic disturbancesin the liver (e.g., steatosis) commonly precede the development of obe-sity, as well as insulin resistance in other organs (1, 2).
Numerous genes encoding extracellular proteins are expressed in theliver. Recent advances in comprehensive gene expression analysis andproteomic technology have contributed to the consideration of liver asan endocrine and secretory organ (3, 4). Abnormalities in liver functionmay have a detrimental effect on glucosemetabolism in other organs, asindicated by changes in the protein secretory profile of steatotic liver inassociation with glucose intolerance and insulin resistance (5). More-over, several liver-derived secretory factors affect the metabolism of
peripheral organs, supporting the hypothesis that proteins secreted byliver control whole-body energymetabolism (5–7). However, the effectsof metabolic challenges on liver-secretory proteins and their modes ofaction remain elusive.
G protein a subunits share the common biological feature of beingactivated in response to environmental changes sensed by G protein–coupled receptors (GPCRs) (8). Given thatmyriadGPCRs directly bindto a relatively small number of Ga proteins for signal transmission, Gaproteins regulate the complexity of diverging and converging signaltransducing systems. Thus, Ga protein expressionmay have a profoundeffect on modulating physiological and biochemical activities. AmongthemajorGa protein familymembers,Ga13 ismore highly expressed inliver than in other insulin target tissues (9). However, the biologicalfunction of Ga13 in the liver and its effects on whole-body energy me-tabolism have not been explored.
This study investigated the underlying basis of aberrant expressionof liver-secreted proteins in mice under metabolic stress. The goal wasto identify a mediator affecting glucose metabolism in extrahepatic tis-sues upon the onset of hyperglycemia. To define the hepatocyte-specificrole of Ga13 in systemic glucosemetabolism, we generated liver-specificGna13 knockout (G13 LKO) mice and attempted to identify a molec-ularmediator and understand its effects on peripheral insulin resistanceusing proteomic techniques. Here, we report that Ga13 expression wasmarkedly lower in the livers of mice or patients with hyperglycemia ordiabetes.We demonstrate that selective ablation ofGna13 inmouse he-patocytes caused glucose intolerance and insulin resistance in otherorgans through overproduction of inter-a-trypsin inhibitor heavy chain1 (ITIH1), a liver-derived secretory protein. In subjects with impairedglucose tolerance or type 2 diabetes, ITIH1 production was enhanced.
RESULTSGa13 is down-regulated in the liver of diabetic miceFirst, we examined Ga13 expression inmajor metabolic organs. In micerendered obese through a high-fat diet (HFD), Ga13 was decreased in
1 of 17

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
the liver and hepatocytes, whereas no difference was found in Ga13 ex-pression in adipose tissue or skeletal muscle (P < 0.01; Fig. 1, A to C).The phenotypic changes were confirmed in genetically obese mice(P < 0.01; Fig. 1D). A strong inverse correlation existed between hepaticGa13 expression and fasting blood glucose concentrations in bothanimal models (P < 0.01; Fig. 1E). A similar correlation was confirmedin the overall analysis for the obese diabeticmice in both animalmodels(P < 0.05; Fig. 1E), suggesting that decreased hepatic Ga13 was asso-ciated with hyperglycemia. To validate this association, we monitoredhepatic Ga13 in human subjects with non-alcoholic fatty liver disease(NAFLD), in accordance with the degree of glucose tolerance (cohort#1). When compared to human subjects with normal glucose tolerance(fasting blood glucose below 110mg/dl), there was a decrease inGa13 inthe liver of subjects with impaired glucose tolerance (fasting blood glu-cose ranging between 110 and 126 mg/dl) (Fig. 1F and table S1). Thedecrease in Ga13 was even greater in patients with overt type 2 diabetes(fasting blood glucose over 126 mg/dl) (Fig. 1F and table S1). A similaroutcome was obtained with liver biopsy specimens stained immuno-histochemically for Ga13. Liver biopsy specimens from patients withimpaired glucose tolerance or type 2 diabetes showed negative-to-faintGa13 staining compared to weak-to-moderate Ga13 staining intensityfor liver specimens from subjects with normal glucose tolerance(Fig. 1G). Consistently, hepatic Ga13 expression was inverselycorrelated with indices of diabetes such as the HOMA-IR (homeostaticmodel assessment of insulin resistance) test, insulin and glucose concen-trations, HbA1c, adipose tissue insulin resistance, and C-peptide(P < 0.05; Fig. 1H).When the samples were divided into two subgroupsby the median value of hepatic Ga13 expression, clinical indices ofdiabetes were elevated in subjects with lower hepatic Ga13 (P < 0.01;fig. S1A). In another cohort study, similar results were found in pa-tients with chronic hepatitis C virus infection who had clinical char-acteristics of type 2 diabetes (cohort #2) (P < 0.05; fig. S1, B to D). Nosignificant correlations existed between hepatic Ga13 expression andlipid profiles assessed in the subjects in cohort #1 or cohort #2 (fig. S2,A to D). These results suggested that a decrease in Ga13 in the livermay affect glucose homeostasis.
Liver-specific ablation of Ga13 exacerbates diet-inducedinsulin resistance in mouse peripheral tissuesTo identify the pathophysiological role of hepatic Ga13 in systemicglucose metabolism, we generated a mouse strain with liver-specificablation of Gna13 (G13 LKO) by breeding Gna13flox/flox mice withalbumin-Cre transgenic mice (fig. S3A). qRT-PCR and immuno-blotting analyses of different organs and primary hepatocytes verifiedspecific deletion of Ga13 in hepatocytes (fig. S3B). Thereafter, wesubjected wild-type and G13 LKO mice to a high-fat diet for 9 weeksand monitored metabolic profiles. No significant difference in diet-induced obesity was observed between genotypes (fig. S3, C and D).Liver morphology and serum biomarkers for hepatocellular injuryremained unchanged (fig. S3, E and F). With respect to lipid metabo-lism, triglyceride content in both liver and serum was unaffected,whereas serum total cholesterol and low-density lipoproteinwere slight-ly decreased in G13 LKO mice compared to wild-type mice (fig. S3G).Our results indicated that hepatocyte-specific deletion ofGna13 did notexacerbate liver steatosis in mice with diet-induced obesity.
Given the inverse relationship between hepatic Ga13 and hyper-glycemia, we next explored the effects of liver-specific ablation ofGa13 on blood glucose and insulin concentrations in mice. Fasting glu-cose was higher in G13 LKOmice fed a high-fat diet compared to wild-
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019
type mice fed a high-fat diet, but this effect was absent in animals fed anormal diet (Fig. 2A and fig. S4A). In G13 LKOmice fed either a high-fat diet or normal diet, however, both glucose and insulin tolerancewereimpaired (Fig. 2, B and C, and fig. S4, B and C), whereas serum insulinconcentrations after glucose challenge were not significantly differentbetween genotypes (Fig. 2D and fig. S4D). Similarly, neither insulinnor C-peptide showed significant decreases in G13 LKO mice underfasted or fed conditions compared towild-typemice; this was consistentwith comparable pancreatic islet sizes observed during histological ex-amination (Fig. 2, E to G, and fig. S4, E to G). These results suggestedthat glucose intolerance manifested in G13 LKO mice might be due toimpaired systemic insulin sensitivity rather than a defect in glucose-stimulated insulin secretion.
To better understand the effects on insulin signaling of Gna13 de-letion in mouse hepatocytes, we measured phosphorylated Akt(phospho-Akt) as an insulin sensitivity marker in major metabolicorgans ofmice subjected to insulin challenge or a fasting and refeedingregimen. Wild-type and G13 LKO mice were fed a high-fat diet for5 weeks to evaluate the metabolic impact of hepatic Gna13 deficiencyon systemic insulin sensitivity without the possible confounding effectof inflammatory mediators induced by a long-term high-fat diet (1, 5).Phospho-Akt expression was unchanged in the liver or in primary he-patocytes isolated frommice fed a high-fat diet or normal chow (Fig. 2,H and I, and fig. S4, H and I). Glucose production inmouse hepatocyteswas also comparable (Fig. 2J), presumably due to similar expression ofgluconeogenic genes (fig. S4J). However, phospho-Akt was notablydiminished in adipose tissue and skeletal muscle of G13 LKO micefed either a high-fat diet or normal diet (Fig. 2K and fig. S4K). Con-sistently, liver-specific ablation of Ga13 completely abolished insulin-stimulated 2-deoxyglucose uptake in epididymal fat pad and skeletalmuscle in ex vivo cultures (Fig. 2L). Moreover, the outcome of glucosetolerance assays after lentiviral overexpression of Ga13 in the liver ofwild-type mice further confirmed the hypothesis that loss of Ga13 inhepatocytes caused systemic glucose intolerance (Fig. 2, M and N), po-tentially due to impaired insulin sensitivity in extrahepatic tissues. Dur-ing challenge with a high-fat diet, Ga13 overexpression in the liveraffected none of the parameters measured including body weight gain,food consumption, and liver and epididymal fat weight (fig. S4, L to O).Ga13 expression did not change in adipose tissue and skeletal muscle(fig. S4P), highlighting the potential role of hepatic Ga13 in systemicglucose tolerance. These results prompted us to investigate the potentialliver-secreted molecules causing systemic insulin resistance.
Ablation of Ga13 promotes the secretion of ITIH1 frommouse liverTo identify the hepatocyte-derived factors induced by ablation ofGna13, we prepared conditionedmedia fromculturedhepatocytes fromeither G13 LKO or wild-type mice fed a high-fat diet for 5 weeks.Conditioned media from G13 LKO hepatocytes inhibited insulin-dependentAkt phosphorylation in differentiated 3T3-L1 orC2C12 cellscompared to conditioned media from wild-type mouse hepatocytes(Fig. 3A). To elucidate the hepatocyte-derived soluble factors in theconditionedmedia, we performed semi-quantitative secretome analysisusing conditioned media depleted of abundant plasma proteins (albu-min and immunoglobulin). Of a total of 530 proteins detected, 104weredesignated “secreted,” whereas others were grouped as “non-secreted,”based on the possession of an N-terminal signal sequence and the crite-ria annotated by UniProt (Fig. 3B). Of the secreted protein candi-dates, 67 were annotated as “liver-enriched” by UniProt or the
2 of 17

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
Kim et al., Sci. Transl. Med. 11, eaan4
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
ND HFD (9 weeks)
Liver
Adipose tissue
Skeletal muscle
G 13
-Actin
-Actin
-Actin
G 13
G 13
Mouse metabolic organsA B
C
E
D
ND HFD (9 weeks)
G13
Mouse liver
G
-Actin
-Actin
-Actin
G 13
Primary hepatocytes
ND HFD
Mouse liver
WT ob/ob
G 13
WT db/db
G 13
F H
Liver
0
0.5
1.0
1.5
2.0 WTob/ob
0
0.5
1.0
1.5
2.0Liver
WTdb/db
Adipose tissue
N.S.
0
0.5
1.0
1.5
2.0
Liver
0
0.5
1.0
1.5
2.0
0
0.5
1.0
1.5
2.0
Skeletal muscle
N.S.
NDHFD
NGT
G 13
-Actin
-Actin
IGT T2DM
Patient no. 1 2 3 4 5 1 2 3 4 1 2 3 4
NGT IGT T2DM
Patient no. 6 7 8 9 10 5 6 7 8 5 6 7 8 9
Log 2 h
epat
ic G
13 e
xpre
ssio
n(n
orm
aliz
ed to
-a
ctin
)
–2
–1
0
1
2
NGT IGT T2DM
NGT T2DM
H&
E
NGT T2DMIGT
G13
–6 –5 –4 –3 –2 –1 0 10
100
200
300
400
500
600
Log2 hepatic G 13 expression (fold)
WTob/ob
P < 0.01r = –0.833
–2.0 –1.5 –1.0 –0.5 0.0 0.50
100
200
300
400
500
600
Log2 hepatic G 13 expression (fold)
WTdb/db
P < 0.01r = –0.839
P < 0.01r = –0.614
–1.2 –0.9 –0.6 –0.3 0 0.3 0.60
100
200
300
400
500
Log2 hepatic G 13 expression (fold)
Glu
cose
(mg/
dl)
NDHFD (9 wks)
G 13
200250300350400450500550600
Glu
cose
(mg/
dl)
–6 –5 –4 –3 –2 –1 0 1
P < 0.05r = –0.423
Log2 hepatic G 13 expression (fold)
NAFLD human samples (cohort #1)NGT IGT T2DM
WT-HFD(9 wks)ob/obdb/db
(12 weeks)
–2.0 –1.5 –1.0 –0.5 0 0.5 1.00
5
10
15
20
25
P = 0.000r = –0.667
HO
MA
-IR
05
10152025303540
P = 0.000r = –0.808
–2.0 –1.5 –1.0 –0.5 0 0.5 1.050
100
150
200
250
300
350
P = 0.008r = –0.500
–2.0 –1.5 –1.0 –0.5 0 0.5 1.0
Glu
cose
(mg/
dl)
456789
1011
P = 0.037r = –0.404
HbA
1c (%
)
–2.0 –1.5 –1.0 –0.5 0 0.5 1.00
10
20
30
40
P = 0.000r = –0.632
–2.0 –1.5 –1.0 –0.5 0 0.5 1.0
Adi
pose
tiss
ue IR
0
2
4
6
8
10
P = 0.000r = –0.684
C-p
eptid
e (n
g/m
l)
–2.0 –1.5 –1.0 –0.5 0 0.5 1.0
735 (2019) 9 October 2019 3 of 17
-s
-
s
Fig. 1. Decrease in hepatic Ga13
in obese mice and patients withdiabetes. (A) Immunoblot analysesfor Ga13 expression of protein ly-sates of liver, adipose tissue (epi-didymal fat), and skeletal muscle(gastrocnemius) collected fromC57BL/6 mice fed a normal diet(ND) or a high-fat diet (HFD) for9 weeks. The relative band intensi-ties of the immunoblots were quan-t i f ied by dens i tometry andexpressed as relative intensity nor-malized to b-actin (n = 4 per group).(B) Representative images of liversections from C57BL/6 mice fed anormal diet (ND) or a high-fat diet(HFD) for 9 weeks [as in (A)] immu-nostained for Ga13 (brown) using apolyclonal antibody against Ga13(n = 3 to 4 per group). (C) Immuno-blot analysis for Ga13 expression inprotein lysates of primary hepato-cytes isolated from C57BL/6 micefedeither anNDorHFDfor12weeks.The relative band intensities of theimmunoblots were quantified bydensitometry andexpressed as rela-tive intensity normalized to b-actin(n = 4 per group). (D) Immunoblotanalyses for Ga13 expression in pro-tein lysates of liver collected fromwild-type (WT), obese ob/ob (top),and diabetic db/db (bottom) micefed normal chow. Quantification ofdensitometry analyses for immuno-blots is shown below the represent-ative gels (n = 5 per group). Therelative band intensities of the im-munoblots were quantified bydensitometry and expressed as in-tensity relative to b-actin. (E) Corre-lation analyses between hepaticGa13 expression and fasting bloodglucose concentrations in C57BL/6mice fed a normal diet (ND) orhigh-fat diet (HFD) for 9 weeks (left,n= 8or 13per group) andwild-type(WT), obese ob/ob, or diabetic db/dbmice (middle and right, n = 5 pergroup) fed a normal diet. An identi-cal correlation was reanalyzed (farright box) using combined data forthe same obese ob/ob and diabeticdb/dbmice (n=23). (F) Immunoblotanalyses for Ga13 expression in pro-
tein lysates of liver specimens from individuals with normal glucose tolerance (NGT), impaired glucose tolerance (IGT), and overt diabetes (T2DM) (NAFLD cohort #1). Quantification of densitometry analyses for immunoblots relative to b-actin is shown below the representative gels (n = 8 to 10 per group). (G) Representative images of liver sectionobtained from the same individuals described in (F) stained for Ga13 expression (brown) using a polyclonal antibody against Ga13 (left, n = 3 to 4 per group) or stained withhematoxylin and eosin (H&E) (right, n = 1 to 2 per group). Scale bars, 100 mm. (H) Correlation analyses between hepatic Ga13 expression and diabetic indices such as the homeostatic model assessment of insulin resistance (HOMA-IR) test, insulin, fasting glucose, HbA1c, adipose tissue insulin resistance index (adipose tissue IR), and C-peptide insubjects with non-alcoholic fatty liver disease (NAFLD) or normal controls (n= 27, total number of subjects including normal controls andNAFLDpatients). Values are expressed ameans ± SEM. (**P < 0.01 versus ND or WT). Data were analyzed by two-tailed Student’s t test (A and D) or Pearson correlations (E and H). N.S., not significant.

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
Kim et al., Sci. Transl. Med. 11, eaan47
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
C DBA
IH
L
J
M N
K
0 30 60 90 120405060708090
100110
Glu
cose
(% in
itial
)
Time (min)
Insulin tolerance test (HFD 13 weeks)
0
4
8
12 AUC
(x10
3 )
WTG13 LKO
0
1
2
3
4
5
0 15 30 45 60 75 90
Insu
lin (n
g/m
l)
Time (min)
050
100150200250300350
N.S.AUC
Glucose-stimulatedinsulin secretion (HFD 10 weeks)
WTG13 LKO
0
2
4
6
8
InsulinBasal
Glu
cose
pro
duct
ion
(m
g/m
g pr
otei
n/ho
ur)
N.S.
N.S.
Primary hepatocytes (HFD 5 weeks)
WTG13 LKO
050
100150200250300
Glu
cose
(mg/
dl)
HFD (9 weeks)
WTG13 LKO
0 15 30 45 60 75 900
100200300400500600700 WT
G13 LKO
Glu
cose
(mg/
dl)
0
2
4
6 AUC
(x10
4 )
Time (min)
Glucose tolerance test (HFD 10 weeks)
20
40
60
80
100
0InsulinBasal
Skeletal muscle (HFD 5 weeks)
WTG13 LKO
020406080
100120140160
InsulinBasal(nm
ol/m
g pr
otei
n/15
min
)
Adipose tissue (HFD 5 weeks)
Primary hepatocytes
G 13
HFD (5 weeks)
WT G13 LKO
Akt
+ + ––Insulin
p-Akt (Thr308)
p-Akt (Ser473)
Adipose tissue
HFD (5 weeks)
Fasted Refed Fasted RefedG13 LKOWTG13 LKO
HFD (5 weeks)
G 13
Akt
InsulinWT
p-Akt (Thr308)
p-Akt (Ser473)
Skeletal muscle
WT G13 LKO
HFD (5 weeks)
G 13
Akt
Insulin
p-Akt (Thr308)
p-Akt (Ser473)
HFD (5 weeks)
Fasted Refed Fasted RefedG13 LKOWT
Liver
HFD (5 weeks)
WT G13 LKO
-Actin
-Actin -Actin
-Actin
G 13
Akt
Insulin
p-Akt (Thr308)
p-Akt (Ser473)
G13 LKOWT
HFD (5 weeks)
Fasted Refed Fasted Refed
00.20.40.60.81.01.21.4
Insulin
p-Akt(Ser473)
p-Akt(Thr308)
00.20.40.60.81.01.21.4
Refed
p-Akt(Ser473)
p-Akt(Thr308)
00.20.40.60.81.01.21.4
Insulin
p-Akt(Ser473)
p-Akt(Thr308)
00.20.40.60.81.01.21.4
Refed
p-Akt(Ser473)
p-Akt(Thr308)
HFD (9 weeks)
WT G13 LKO
0
1
2
3
4
N.S.
N.S.
Insu
lin (n
g/m
l)
RefedFasted
WT-HFD (5 weeks)G13 LKO-HFD (5 weeks)
C-p
eptid
e (p
M)
N.S.
N.S.
0
500
1000
1500
2000
2500
RefedFasted
GFE
Glucose tolerance test (HFD 8 weeks)
0 15 30 45 60 75 900
100
200
300
400
500
Time (min)
Glu
cose
(mg/
dl)
0
AUC
1
2
3
4
4 )
Lv-ConLv-G 13
Insulin tolerance test (HFD 9 weeks)
0 30 60 90 1205060708090
100110120
Time (min)
Glu
cose
(% in
itial
)
0
5
10
15 AUC
3 )
Lv-ConLv-G 13
RefedFasted
Glu
cose
(mg/
dl)
0
50
100
150
200
250
Rel
ativ
e in
tens
ity(n
orm
aliz
ed to
Akt
)
Rel
ativ
e in
tens
ity(n
orm
aliz
ed to
Akt
)
Rel
ativ
e in
tens
ity(n
orm
aliz
ed to
Akt
)
Rel
ativ
e in
tens
ity(n
orm
aliz
ed to
Akt
)
2-D
eoxy
gluc
ose
upta
ke
35 (2019) 9 October 2019 4 of 17
fl
,
Fig. 2. Impaired glucose homeo-stasis and insulin resistance inG13 LKOmice fed a high-fat diet.(A) Measurement of fasting bloodglucose concentrations in wild-type(WT) mice or mice with liver-specificablation of Gna13 (G13 LKO) fed ahigh-fat diet (HFD) for 9 weeks(n = 5 per group). (B) Results of theglucose tolerance test (glucose ga-vage; 2 g/kg body weight) in WTand G13 LKO mice fed an HFD for10 weeks (n = 6 per group). (C) Re-sults of the insulin tolerance test (in-sulin injection; 1.5 insulin units/kgbodyweight) in WT and G13 LKO mice fedan HFD for 13 weeks (n = 12 pergroup). (D) Measurements of ser-um insulin concentrations duringthe glucose tolerance test in WTand G13 LKO mice fed an HFD for10weeks (n = 6 per group). (E) Mea-surements of fasting blood glucoseconcentrations in WT or G13 LKOmice fed an HFD for 5 weeks (n = 4or 5 per group). Mice were sub-jected to fasting and then refeeding(fasted for 16 hours and then refedfor 4 hours). (F) Measurements ofserum insulin and C-peptide con-centrations in the same mice as in(E) (n = 6 per group). (G) Represent-ative images of pancreas sectionsfrom WT and G13 LKO mice fed anHFD for 9 weeks and stained for he-matoxylin and eosin (n = 3 to 4 pergroup). (H ) Immunob lo t s fo rphosphorylated-Akt (p-Akt) and totalAkt expression in protein lysatesof the livers from WT or G13 LKOmice fed an HFD for 5 weeks andinjected with a single dose of insu-lin (2 insulin units/kg body weight;i.p., 15 min) or fromWT or G13 LKOmice subjected to fasting and thenrefeeding (fasted for 16 hours andthen refed for 4hours). (I) Immunoblotsfor phosphorylated-Akt (p-Akt) andtotal Akt expression in protein ly-sates of primary hepatocytesisolated from WT or G13 LKO micefed an HFD for 5 weeks and treatedwith a single dose of insulin (100 nM,15min). (J) Measurement of glucoseproduction rate inhepatocytes fromWT or G13 LKOmice fed an HFD for5weeks (n=3pergroup, experimentsperformed in triplicate). (K) Immuno-
blots for phosphorylated-Akt (p-Akt) and total Akt expression in protein lysates of epididymal fat tissue or soleus muscle from the same mice as in (E). Quantification odensitometry analyses for immunoblots relative to b-actin is presented below each blot (n = 3 per group). (L) Measurement of 2-deoxyglucose uptake rate in epididymafat tissue or soleusmuscle fromWT or G13 LKOmice fed anHFD for 5weeks (n= 4 or 6 per group). (M andN) The effect of hepatic Ga13 overexpression onglucosemetabolismwas determined by analyzing glucose (M) or insulin tolerance (N) in C57BL/6 mice injected via the tail vein with control lentiviruses (Lv-Con) or lentiviruses expressing mouseGa13 (Lv-Ga13) (1.1 × 107 transduction units). Injectedmice were subsequently subjected to HFD feeding for 8 or 9 weeks (n = 6 or 7 per group). For (B) to (D) and (M) and (N)insets represent area under the curve (AUC). Values are expressed asmeans ± SEM. *P < 0.05, **P < 0.01 for G13 LKO versusWT (A to C and K) or Lv-Ga13 versus Lv-Con (M andN). Data were analyzed by two-tailed Student’s t test (A to D, K, M, and N) or one-way ANOVA followed by Bonferroni post hoc tests (E, F, J, and L). N.S., not significant.
SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
Human Protein Atlas. The secretion of 42 proteins was increased in re-sponse to liver-specific ablation of Gna13, whereas secretion of 25 pro-teins was decreased. Of the top differentially secreted proteins showingtwofold or more increased or decreased abundance, we narrowed ourfocus to ITIH1 because of its marked increase and potential effect ondiabetes (Fig. 3C). In mice fed a high-fat diet, liver-specific ablation ofGna13 augmented hepatic and serum ITIH1 expression (Fig. 3, D to F),confirming the results obtained from proteomic analyses. Plasma pro-tease C1 inhibitor was not examined due to the lack of a direct role inthe development of diabetes and its controversial expression pattern de-pending on diabetes type (10, 11).
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019
Hepatic and serum ITIH1 are increased in subjects withimpaired glucose tolerance or diabetesTo validate possible correlations between Ga13 and ITIH1 in clinicalspecimens, we analyzed ITIH1 expression in specimens from humansubjects with diabetes where Ga13 expression was markedly decreased.In the first cohort of patients (cohort #1), ITIH1 was elevated in liverand serum samples from subjects with impaired glucose tolerance andin patients with overt diabetes (Fig. 4, A to C). Serum ITIH1 concentra-tions exhibited a strong negative correlation with hepatic Ga13(r = −0.776, P < 0.01; Fig. 4D), suggesting an inverse relationship be-tween hepatic Ga13 and ITIH1 production. Moreover, serum ITIH1
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
BA
0100200300400500600
104
426
Secreted
Notsecreted
Total detected proteins
Num
ber o
f pro
tein
s
020406080
100120
Liver-enriched
Non-liver- enriched
Secreted proteins
67
37
Differentially secreted proteins (G13 LKO vs WT)
0
20
40
60
80
25
42 Increased
Decreased
CSemi-quantitative secretome anlaysis of CM from HFD-fed primary hepatocytes
1
Differentially secreted proteins Fold change
Plasma protease C1 inhibitorAccession number = IC1_Mouse GN=Serping1 3.229
2 Heavy chain H1Accession number = ITIH1_Mouse GN=Itih1
2.691
3 AngiotensinogenAccession number = Q3UTR7_Mouse GN=Agt
2.583
4 CeruloplasminAccession number = CERU_Mouse GN=Cp 2.217
5 SerotransferrinAccession number = TRFE_Mouse GN=Tf
2.061
(G13 LKO / WT)
FED
WT G13 LKO
Mouse liver
-Actin
ITIH1
HFD (9 weeks)
Alpha-2-HS-glycoproteinXanthine dehydrogenase/oxidaseComplement component C8 gamma chainHemopexinAlpha-1-acid glycoprotein 1SerotransferrinCeruloplasminAngiotensinogen
–2 –1 0 1 2Log2 fold change (G13 LKO / WT)
Fold change >2
Plasma protease C1 inhibitor
Pigment epithelium-derived factorVitamin D–binding protein 4
Retinol-binding protein 4Serum amyloid A-2 proteinMannose binding protein C
Apolipoprotein A-IIComplement C4-B
0
1
2
3
4
ITIH1
HFD (9 weeks)
R
elat
ive
inte
nsity
(nor
mal
ized
to
-act
in)
WTG13 LKO
00.050.100.150.200.250.300.35
HFD (9 weeks)
Mouse serum
ITIH
1 (O
.D. 4
50/6
20) WT
G13 LKO
Mouse serum
ITIH1
HFD (12 weeks)
WT G13 LKO
Albumin
CM from primary hepatocytes (fed HFD for 5 weeks)
WT-CM KO-CM
C2C123T3-L1
-Actin
p-Akt
Akt
+ + + + ––––InsulinWT-CM KO-CM
Fig. 3. Identification of ITIH1 as a hepatocyte-secreted protein enhanced by loss of Ga13. (A) Immunoblots for phosphorylated-Akt (p-Akt) and total Akt expres-sion in protein lysates of 3T3-L1 and C2C12 cells incubated with conditioned media (CM) that were collected from primary hepatocytes isolated from WT or G13 LKOmice fed a high-fat diet (HFD) for 5 weeks. (B) The numbers of proteins in primary hepatocyte conditioned media from WT and G13 LKO mice in (A) that weredifferentially secreted (n = 3). (C) List of top differentially secreted proteins from (B) detected by semi-quantitative secretome analysis. (D) Immunoblots for ITIH1expression in protein lysates from the livers of WT or G13 LKO mice fed an HFD for 9 weeks. Quantification of densitometry analysis for bands is shown next tothe immunoblot (n = 7 per group). b-Actin was the loading control. (E) Measurements for serum ITIH1 concentrations for WT or G13 LKO mice fed an HFD for 12 weeks.Albumin was used as the loading control. (F) Quantitative analysis of ELISA for serum ITIH1 for the same mice as in (E) (n = 7 per group). Values are expressed as means ± SEM.**P < 0.01 for G13 LKO versus WT mice (D and F). Data were analyzed by two-tailed Student’s t test (D and F). N.S., not significant.
5 of 17

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
concentrations were highly associated with various diabetic parametersirrespective of lipid profiles (Fig. 4, E andF, and fig. S5, A andB). Similarresults were observed in patients with hepatitis C virus infection (cohort#2), who showed a stepwise increase in ITIH1 production in both liverand plasma samples that was associated with the HOMA-IR test, amethod used to assess insulin resistance (fig. S6, A and B). In contrast,expression of ITIH2, another liver-enriched member of the inter-a-trypsin inhibitor (ITI) protein family, was not elevated in the liverof diabetic subjects or G13 LKO mice (Fig. 4A and fig. S6, A and C).In addition, Itih1 and Itih2mRNA expression was not significantly dif-ferent between genotypes (fig. S6D), suggesting possible post-transcriptional regulation of ITIH1 by Ga13.
Liver-secreted ITIH1 binds to hyaluronan surroundingmouse adipose tissue and skeletal muscleCirculating ITIH1 is synthesized exclusively in hepatocytes and secretedinto the bloodstream, stabilizing the extracellular matrix by covalentbinding to hyaluronan (12–14). Considering recent studies demonstrat-ing excessive hyaluronan accumulation in insulin-resistant tissues(15, 16), we examined whether ITIH1 oversecreted in response to he-patic Ga13 deficiency might bind to hyaluronan surrounding adiposetissue and skeletal muscle in mice with impaired insulin sensitivity.ITIH1 expression in adipose tissue and skeletal muscle was higher inG13 LKO mice compared to wild-type mice both fed a high-fat diet(Fig. 5A), with no change in hyaluronan (Fig. 5B). Immunohisto-chemical studies on adipose tissue and skeletal muscle from G13LKO mice showed enhanced ITIH1 immunoreactivity (Fig. 5C),whereas ITIH1 staining was reduced in tissues from mice with hepaticGa13 overexpression (Fig. 5D), verifying the hepatic origin of ITIH1 se-cretion. In addition, ITIH1 staining in the mouse tissues was abrogatedby pretreatment with hyaluronidase (Fig. 5C), demonstrating thatITIH1 required hyaluronan for binding to the tissues. Moreover, wefound that ITIH1 depositionwas augmented by hepatic Ga13 deficiencyin extracellular matrix–enriched fractions from adipose and skeletalmuscle tissues (Fig. 5E). Detection of fibronectin, but not b-tubulin, in-dicated appropriate enrichment of extracellular matrix proteins (fig.S7). In immunofluorescence assays, we corroborated the enhanced in-teraction of ITIH1 with hyaluronan in response to hepatic Ga13 defi-ciency (Fig. 5F, left andmiddle). Similar results were obtained in 3T3-L1and C2C12 cells incubated with conditioned media from cultured G13LKO hepatocytes (fig. S8). In liver tissue, ITIH1-hyaluronan complexeswere not readily detected in either group, although ITIH1 staining in-tensity wasmarkedly enhanced by hepatic Ga13 deficiency, presumablydue to the lack of hepatic deposition of hyaluronan (Fig. 5F, right).Together, these results indicate that overproduction of ITIH1 byGa13-deficient liver may result in ITIH1 deposition in adipose tissueor skeletal muscle through its interaction with hyaluronan.
ITIH1 secretion in response to Gna13 ablation is dueto O-GlcNAC transferase inductionTo elucidate the molecular basis underlying overproduction and secre-tion of ITIH1 under the conditions of Ga13 deficiency or diabetes, weexamined the effect of hyperglycemia on hepatic Ga13 expression inmice after an oral glucose gavage. A single glucose gavage in mice no-tably diminished Ga13 in the liver in conjunction with an increase incirculating ITIH1 (fig. S9A). A similar result was observed in culturedmouse hepatocytes exposed to high glucose concentrations (fig. S9B),supporting the causative effect of hyperglycemia on Ga13 repressionin hepatocytes. Considering that most secretory proteins are modified
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019
by glycosylation to ensure protein stabilization and solubility (17, 18),we focused on the possibility of glycosyl modification of ITIH1. In par-ticular, O-GlcNAcylation is one of the major posttranslational modifi-cations elicited by high glucose concentrations due to hyperglycemiaor diabetes (19). The loss of Ga13 in liver hepatocytes intensifiedO-GlcNAcylation of proteins along with increased ITIH1 production(Fig. 6, A and B). O-GlcNAcylation was markedly enhanced in G13LKO mouse hepatocytes compared to wild-type mouse hepatocytesunder normal glucose concentrations (Fig. 6B and fig. S9B), raisingthe possibility that O-GlcNAcylation might be directly controlled byGa13 signaling.
Given that O-GlcNAC transferase, an enzyme catalyzing proteinO-GlcNAcylation, is up-regulated in the clinical settings of insulinresistance such as hyperglycemia and diabetes (20, 21), we examinedwhether Ga13-dependentmodification ofO-GlcNAcwasmediated byO-GlcNAC transferase. After a glucose gavage, G13 LKO mice dis-played augmented expression of O-GlcNAC transferase in the liver,which was accompanied by increased ITIH1 in liver and serum relativetowild-type controlmice (Fig. 6, C andD). Similar results were found inliver or cultured hepatocytes of G13 LKO mice fed a high-fat diet (Fig.6E). We corroborated increases in ITIH1 and O-GlcNAC transferaseassociated with Ga13 repression in mice subjected to streptozotocin-induced diabetes (fig. S9, C to E).O-GlcNAC transferase expressionwassuppressed by Rho signaling downstream of Ga13, as evidenced by theoutcomes using cultured primary hepatocytes exposed to chemical in-hibitors and AML12 cells transfected with a constitutively active Rhomutant protein (fig. S9, F and G). In addition, lentiviral vector–mediated overexpression of Ga13 inhibited O-GlcNAC transferaseexpression in mouse liver in tandem with diminished ITIH1 in liverand serum (Fig. 6F and fig. S9H). Infection of culturedmouse primaryhepatocytes with adenovirus carrying a constitutively active mutantform of Ga13 (Ad-G13QL) had a similar effect (Fig. 6, G and H). More-over, immunoblotting of ITIH1 immunoprecipitates from liver orserum samples for O-GlcNAcylation verified ITIH1 O-GlcNAcylation(Fig. 6I). We further examined ITIH1 O-GlcNAcylation by liquidchromatography–tandem mass spectrometry (LC-MS/MS) usingcultured HEK293A cells overexpressing FLAG-tagged human ITIH1(fig. S10, A and B). We identified several putative O-GlcNAcylationsites on conserved amino acid residues including Ser590, Ser608, Ser820,and Ser824 (fig. S10, C and D). Of these, Ser590 and Ser608 residues werelocated on the C-terminal domain of ITIH1, whereas the other residueswere located on the propeptide domainwhere the corresponding regionwas cleaved in theGolgi apparatus during the process ofmaturation andsecretion of ITIH1.
O-GlcNAcylation may control protein stability by affecting proteinubiquitination (22). O-GlcNAC transferase overexpression increasedITIH1 stability along with a decrease in ITIH1 ubiquitination (fig.S11, A and B). Likewise, O-GlcNAC transferase knockdown using anshRNA-expressing plasmid against O-GlcNAC transferase (shOGT)suppressed ITIH1 O-GlcNAcylation and stabilization in culturedAML12 cells exposed to high glucose concentrations or overexpres-sing ITIH1 (fig. S11, C and D). Treatment of the AML12 cells withST045849, an inhibitor of O-GlcNAC transferase, had a similar effect(fig. S11E), suggesting that ITIH1 was stabilized by O-GlcNAcylation.Given the role ofO-GlcNAC transferase–mediated proteinO-GlcNAcylationin the etiology of insulin resistance anddiabetes (19, 21), we further testedthe effect of hepatic O-GlcNAC transferase on systemic glucose toler-ance in vivo. Treatment of G13 LKO mice with ST045849 (20 mg/kgper day, for 4 consecutive days) not only prevented an ITIH1 increase
6 of 17

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
HO
MA
-IR
0
5
10
15
20
25
LowSerum ITIH1concentration
High
Insu
lin (
IU/m
l)
0
10
20
30
40
50
Low High
Glu
cose
(mg/
dl)
50
100
150
200
250
300
350
Low High
HbA
1c (%
)
4
5
6
7
8
9
10
11
Low High
Adi
pose
tiss
ue IR
0
10
20
30
40
50
60
Low High
C-p
eptid
e (n
g/m
l)
0
2
4
6
8
10
Low High
NGT IGT T2DM
Patient no. 6 7 8 9 10 5 6 7 8 5 6 7 8 9
NGT
ITIH1
IGT T2DM
ITIH2
Patient no. 1 2 3 4 5 1 2 3 4 1 2 3 4
-Actin
-Actin
ITIH1
ITIH2
NGT IGT T2DM
ITIH
1D
AP
IM
erge
d
020406080
100120140160180
NGT IGT T2DM
–2.0 –1.5 –1.0 –0.5 0 0.5 1.00
20406080
100120140160180 NGT IGT T2DM
0 10 20 30 40 500
20406080
100120140160180
HbA1c (%)4 5 6 7 8 9 10 11
020406080
100120140160180
Adipose tissue IR0 10 20 30 40 50 60
020406080
100120140160180
HOMA-IR0 5 10 15 20 25
020406080
100120140160180
50 100 150 200 250 300 3500
20406080
100120140160180
Glucose (mg/dl)
0 2 4 6 8 100
20406080
100120140160180
C-peptide (ng/ml)
NGT IGT T2DM
Fig. 4. Increased hepatic and serum ITIH1 concentrations in NAFLD subjects with diabetes. (A) Immunoblot analyses for ITIH1 and ITIH2 expression in protein lysates ofliver specimens from subjects with normal glucose tolerance (NGT), impaired glucose tolerance (NGT), or type 2 diabetes (T2DM) (NAFLD cohort #1). (B) Representativeimmunofluorescence images of liver sections fromNAFLD patients with diabetes stained for ITIH1 (red) withDAPI counterstain (blue) (n= 3 to 4 per group, 60×magnification).(C) Quantitative analysis of ELISA for serum ITIH1 from the same subjects as in (A) (n = 7 per group). (D and E) Correlation analyses between serum ITIH1 concentrations andhepatic Ga13 expression (D, n= 17) and serum ITIH1 concentrations and insulin resistance–related indices including HOMA-IR, insulin, glucose, HbA1c, adipose tissue IR, andC-peptide (E, n = 21) in subjects with NAFLD or normal controls. (F) Changes in diabetic indices in relation to serum ITIH1 concentrations for human subjects categorized into twosubgroups by themedian value of serum ITIH1 (n= 10 per group). Data are shown as box andwhisker plots. Box, interquartile range (IQR); whiskers, 5 to 95 percentiles; horizontallinewithin box,median. Values are expressed asmeans ± SEM. Datawere analyzed by one-wayANOVA followedby Bonferroni post hoc tests (C), Pearson correlations (D and E), orMann-Whitney tests (F).
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019 7 of 17

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
A
B
F
D
HFD (9 weeks)
Liver
WT G13 LKO
Adipose tissue
WT G13 LKO
ITIH
1H
AB
PM
erge
d
Skeletal muscle
WT G13 LKO
C
EAdipose tissue
ITIH1
Coo
mas
sie
blue
stai
ning
HFD (9 weeks)
WT G13 LKO
70
100
130170
70
(kDa)
ECM-enriched fraction
HFD (9 weeks)0
0.020.040.060.080.100.120.140.16
∗
ITIH
1 (O
.D. 4
50/6
20)
Adipose tissue
0
0.05
0.10
0.15
0.20
0.25
∗
Skeletal muscle
HFD (9 weeks)
WTG13 LKO
1
Adipose tissue
0
50
100
150
200N.S.
HA
(ng/
mg
prot
ein)
HFD (9 weeks)0
Skeletal muscle
20
4060
80
00N.S.
WTG13 LKO
HFD (9 weeks)
Adipose tissueWT G13 LKO
HFD (9 weeks)
Vehi
cle
Hya
luro
nida
se
Skeletal muscleWT G13 LKO
HFD (9 weeks)
Adipose tissue
noC-vL
Skeletal muscle
G-vLα
31
HFD (11 weeks)
Skeletal muscleWT G13 LKO
70
100
130170
70
(kDa)HFD (9 weeks)
ITIH1
Coo
mas
sie
blue
stai
ning
Fig. 5. Increased ITIH1 deposition onto hyaluronan surrounding peripheral tissues in G13 LKO mice. (A) Quantitative analyses of ELISA for ITIH1 in homogenates ofepididymal fat tissue (n = 8 or 10 per group) and gastrocnemius muscle (n = 12 or 13 per group) from wild-type (WT) or G13 LKO mice fed a high-fat diet (HFD) for 9 weeks.(B) Quantitative analyses of ELISA for hyaluronan (HA) in the homogenates of epididymal fat tissue and gastrocnemius muscle of the same animals as in (A) (n = 8 pergroup). (C) Representative images of epididymal fat tissue and gastrocnemiusmuscle sections frommice as described in (A) stained for ITIH1 (brown) (n = 4 per group). Theslideswerepretreatedwithhyaluronidase (20U/ml) or vehicle for 2 hours at 37°C. Scale bars, 100mm. (D) Representative images of epididymal fat tissue andgastrocnemiusmusclesections fromwild-type (WT) C57BL/6mice injected via the tail veinwith control lentiviruses (Lv-Con) or lentiviruses expressingmouseGa13 (Lv-Ga13) (1.1 ×10
7 transductionunits).The injectedmicewere subsequently fed a high-fat diet (HFD) for 11weeks (n=4per group). Scale bars, 100 mm. (E) Immunoblot analyses for ITIH1 expression in fractions enrichedfor extracellular matrix (ECM) prepared from epididymal fat tissue or tibialis anterior muscle of the samemice as in (A). ECM proteins were normalized to tissue weight and werestained with Coomassie blue stain after SDS-PAGE separation. (F) Representative immunofluorescence images of epididymal fat tissue, gastrocnemius muscle, and liver sectionsfrom the samemice as in (C) stained for ITIH1 (red) and hyaluronan binding protein (HABP) (green) (n = 3 per group). For liver tissue, blue color inmerged images represents DAPIstaining for nuclei. Arrowheads indicate merged color (yellow/orange). Scale bars, 25 mm. For (A) and (B), values are expressed as means ± SEM. *P < 0.05 for G13 LKO versus WTmice (A). Data were analyzed by two-tailed Student’s t test. N.S., not significant.
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019 8 of 17

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
HFD (5 weeks)
(C
TD11
0.6)
G13 LKOWTFasted Refed Fasted Refed
Liver
70
55
40
100
170
130
ITIH1
-Actin-Actin
-Actin
-Actin -Actin
-Actin -Actin
-Actin-Actin
(kDa)
+ –– Ad-G13QL
ITIH1
WT G13 LKO
Albumin
CM from primary hepatocytes
G 13
OGT
Ad-Con Ad-G13QL
Primary hepatocytes
ITIH1
OGT
Vehicle Glucose GlucoseVehicle
WT G13 LKOLiver
ITIH1
G 13
ITIH1
Serum
Albumin
Glucose Glucose
WT G13 LKO
00.20.40.60.81.01.2
OGT
Lv-ConLv-G 13
00.20.40.60.81.01.2
HFD (10 weeks)
ITIH1
0
0.5
1.0
1.5
2.0G 13
WTG13 LKO
< 0.05
02468
101214
ITIH1
< 0.05
< 0.01
< 0.05
< 0.01
0
1
2
3
4
5
VehicleGlucose
VehicleGlucose
OGT
< 0.05
(R
L2)
Liver
WT G13 LKO
70
55
100
170
130
(kDa)
HFD (5 weeks)
Primary hepatocytes
(C
TD11
0.6)
WT G13 LKO5 25 5 25 Glucose
(mM)
70
55
100
170
130
ITIH1(kDa)
HFD (5 weeks)
(R
L2)
WT G13 LKO5 25 5 25 Glucose
(mM)
70
55
100
170130
(kDa)
Primary hepatocytes
HFD (5 weeks)
Lv-Con Lv-G 13
ITIH1
OGT
Liver
G 13
HFD (10 weeks)
G 13
OGT
Liver
WT G13 LKO
Primary hepatocytes
WT G13 LKO
HFD (9 weeks) HFD (5 weeks)
WT G13 LKO
(CTD110.6)
ITIH1
IP: I
TIH
1Ly
sate
s
OGT
Liver
HFD (9 weeks)
Serum
(CTD110.6)
IP: ITIH1WT G13 LKO
HFD (9 weeks)
Vehicle Vehicle
VehicleGlucose
VehicleGlucose
Fig. 6. Increase inO-GlcNAc transferase–mediatedO-GlcNAcylationofproteins after loss of Ga13. (A) Immunoblot analyses forO-GlcNAcproteins (CTD110.6 or RL2 clones)or ITIH1 expression in protein lysates of livers from WT or G13 LKO mice fed a high-fat diet (HFD) for 5 weeks. (B) Immunoblot analyses for O-GlcNAc proteins (CTD110.6 or RL2clones) or ITIH1 expression in protein lysates of primary hepatocytes isolated fromWT or G13 LKO mice fed an HFD for 5 weeks. Primary hepatocytes were incubated with highglucose (25mM) for 24 hours. (C andD) Immunoblot analyses for ITIH1 orO-GlcNAc transferase (OGT) expression in protein lysates of the liver (C) or in sera (D) fromWTorG13 LKOmice. Glucose (2 g/kg body weight) was orally administered to mice, and the liver tissues were harvested after 6 hours. The relative band intensities were quantified by densi-tometry analyses for the immunoblots (n=3per group). b-Actin and albuminwere the loading controls for liver and serum samples, respectively. (E) Immunoblot analyses for OGTin the protein lysates of liver or hepatocytes isolated from WT or G13 LKO mice fed an HFD for 9 or 5 weeks, respectively. (F) Immunoblot analysis for OGT and ITIH1 in proteinlysates of liver fromC57BL/6mice injected via the tail veinwith control lentiviruses (Lv-Con) or lentiviruses expressingmouseGa13 (Lv-Ga13) (1.1 × 107 transduction units). Injectedmice were subsequently fed an HFD for 10 weeks. Immunoblots were quantified by densitometry (n = 3 per group). (G) Immunoblot analysis for OGT and ITIH1 expression inprotein lysates of primary hepatocytes infected with adenoviruses carrying an active mutant of Ga13 (Ad-G13QL) or green fluorescent protein (Ad-GFP) as a control. (H) Immu-noblot analysis for ITIH1 expression in conditioned media (CM) from the same primary hepatocytes as in (G). Albumin was the loading control for conditioned mediasamples. (I) Immunoblot analyses forO-GlcNAc proteins (CTD110.6 clone) orO-GlcNAc transferase (OGT) in ITIH1 immunoprecipitates from the liver homogenates or sera ofmice fed a high-fat diet (HFD) for 9 weeks. Values are expressed asmeans ± SEM. *P < 0.05, **P < 0.01 for Lv-Ga13 versus Lv-Con (F). Data were analyzed by one-way ANOVA,followed by least significant difference (LSD) post hoc test (C) or two-tailed Student’s t test (F).
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019 9 of 17

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
and O-GlcNAcylation in the liver and serum (Fig. 7, A and B) butalso improved glucose tolerance (Fig. 7C). Likewise, overexpression ofO-GlcNAC transferase in hepatocytes in vivo using a hydrodynamic in-jection technique enhanced bothhepatic ITIH1 and serumO-GlcNAcylatedITIH1, whereas knockdown of hepatic O-GlcNAC transferase re-sulted in the opposite effects (fig. S11F). O-GlcNAC transferase ex-pression was not changed in the other tissues examined, indicativeof efficient and selective O-GlcNAC transferase gene delivery intothe mouse liver (fig. S11G). Consistently, O-GlcNAC transferase knock-down lowered ITIH1 in the liver and serum of injected mice and rescuedthe glucose-intolerant phenotype of G13 LKOmice (fig. S11, H to J).To strengthen our hypothesis, we used a lentiviral vector carrying thehuman OGT gene and an albumin promoter. Specific O-GlcNACtransferase overexpression in hepatocytes increased ITIH1 in liverand serum compared to control mice (Fig. 7D) and impaired glucoseand insulin tolerance (Fig. 7, E and F). EnhancedO-GlcNAcylation andstabilization of ITIH1 were verified in cultured primary hepatocytes(Fig. 7G).O-GlcNAC transferase expressionwas comparable in adiposetissue and skeletal muscle (Fig. 7H).
Antibody neutralization of ITIH1 overcomes systemicglucose intolerance and insulin resistance in miceHaving identified ITIH1 overproduction in response to a decrease inGa13 in mouse liver and the consequent induction of insulin resistancein different organs, we finally examined whether antibody neutraliza-tion of ITIH1 had a beneficial effect on systemic glucose homeostasisin mice. C57BL/6 mice were placed on a high-fat diet or normal dietfor 8 to 9 weeks, followed by daily injections of a custom-synthesizedrabbit anti-ITIH1–neutralizing antibody or preimmune IgG as a con-trol for an additional 2 weeks, and the metabolic outcomes weremonitored. In this experiment, ITIH1 neutralization did not alter bodyweight or liver and epididymal fat weight (Fig. 8, A to C). Antibodyneutralization normalized glucose disposal and insulin sensitivity witha decrease in serum ITIH1 (Fig. 8, D to F). Phospho-Akt was altered in3T3-L1 or C2C12 cells incubated with conditioned media from G13LKO hepatocytes in the presence of anti-ITIH1–neutralizing antibody(fig. S12A). We further examined the role of ITIH1 in insulin respon-siveness using conditioned media from G13 LKO cultured primary he-patocytes deficient in ITIH1. siRNA-mediated Itih1 gene silencingabrogated the inhibitory effect of liver-specific Ga13 ablation onphospho-Akt expression and 2-deoxyglucose uptake (fig. S12, B andC). Immunoblotting assays using peptide competition and siRNA tar-geting of endogenous ITIH1 confirmed specificity of our custom-madeantibody (fig. S12, D and E). ITIH1 neutralization using the anti-ITIH1antibody, confirmed by a decrease in circulating ITIH1, improved glu-cose and insulin tolerance inG13 LKOmice fed a high-fat diet (Fig. 8, Gto I), with no changes in body weight or fasting blood glucose concen-trations (Fig. 8, J and K). Insulin-stimulated glucose uptake was im-proved in adipose tissue or skeletal muscle of wild-type mice fed ahigh-fat diet (Fig. 8L).
DISCUSSIONGiven that insulin resistance precedes the development of diabetes andetiologically determines metabolic syndrome in multiple organs, thera-peutic approaches targeting single organs or a subset of intracellularsignaling pathways have shown limited success or considerable sideeffects (23). The liver regulates overall glucose metabolism in responseto changes in extracellular nutritional availability. Hepatic steatosis,
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019
which frequently accompanies insulin resistance, usually occurs beforemetabolic dysfunction in other organs (1, 2), suggesting the causal effectof liver pathophysiology on overall metabolic disturbances. Never-theless, the notion of the liver as the origin and driver of global meta-bolic defects in the setting of hyperglycemia has drawn little attention.Our current findings show that hyperglycemia decreases Ga13 in hepa-tocytes, which exacerbates glucose intolerance and insulin resistance inextrahepatic organs through an O-GlcNAC transferase–dependent in-crease in circulating ITIH1. Our results suggest that there may be anincrease in ITIH1 upon hyperglycemic challenge.
Studies investigating Ga13 have been limited as mice lacking Ga13show a defect in angiogenesis during embryonic development resultingin lethality (24). We generated hepatocyte-specific Gna13 knockoutmice using the Cre-loxP system. Upon feeding these G13 LKO micea high-fat diet, the mice exhibited impaired glucose tolerance andmarked insulin resistance in the absence of changes in obesity and lipidprofiles, suggesting that metabolic abnormalities manifested by G13LKO mice could be attributed to a defect in glucose disposal. Our datashowing that the metabolic profiles of liver were unaffected by hepaticablation of Ga13 support the notion that the Ga13 decrease in hepato-cytes due to hyperglycemia was directly linked to enhanced secretion ofliver-derived soluble factors but not to the initiation of hepatocyte mal-function or injury.
Insulin resistance, observed in subjects with glucose intolerance, en-tails a compensatory hyperinsulinemia in the diet-induced obesitymouse model that enables pancreatic b cells to overcome a decreasein insulin sensitivity in the peripheral tissues. Although it is wellestablished that feeding mice a long-term high-fat diet induces inflam-mation and impairs pancreatic beta cell function, we assumed that thefailure of beta cells might not have occurred in our model given themarked increase in insulin upon glucose challenge in mice fed ahigh-fat diet. In our study, wild-type and G13 LKO mice fed either ahigh-fat diet or normal diet showed comparable serum insulin concen-trations when subjected to glucose gavage, which might reflect a mildeffect of high-fat diet challenge on pancreatic beta cells in our mousemodel. However, ITIH1 may also contribute to pancreatic beta cellfunction. A recent study showed higher accumulation of IaI (inter-a-trypsin inhibitor that comprises ITIH1, ITIH2, and bikunin) andhyaluronan in the pancreatic islets of patients with type 1 diabetes(25). Thus, we propose that increased ITIH1 may affect beta cell func-tion under more severe diabetic conditions (e.g., pancreatitis and type1 diabetes). Moreover, we cannot exclude the potential involvement ofother factors affecting plasma insulin concentrations (e.g., insulin clear-ance by either liver or kidney).
Given that most GPCRs exist in various oligomeric complexes (26),it is improbable that a singleGPCRor ligandmight account for a varietyof metabolic consequences. Moreover, some GPCRs can interact withmore than one Ga protein, indicating possible engagement of severalGa proteins upon ligand binding. Considering the complex nature ofGPCR-Ga protein coupling, certain ligands may activate several typesofGPCRs/Ga proteins, transducingmixed signals to downstream effec-tors. In the current study, G13 LKO mice revealed a cell type–specificrole for Ga13 and excluded interference from other G proteins. More-over, Ga13 in liver was decreased under hyperglycemic conditions re-gardless of ligand activation of corresponding GPCRs. Therefore, it ispossible that a high glucose concentration functions as a nutritionalenvironment or putative ligand for glucose-sensing orphan GPCRs po-tentially affecting intracellular signals modulating Ga13, but this re-mains to be established in future experiments. Overall, the results
10 of 17

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
Lv-ConLv-OGTalb
OGT(Liver)
FE
Lysa
tes
IP :
ITIH
1
Lv-OGTalb
Lv-Con
Primary hepatocytes
ITIH1
OGT
(CTD110.6)
OGTOGT
(Skeletal muscle)
0
0.5
1.0
1.5
2.0
N.S.
0
0.5
1.0
1.5
2.0
N.S.
OGT(Adipose tissue)
D
HG
ITIH1
Glucose (mM) 5 25 5 25
Primary hepatocytesLv-Con
Lysa
tes
Lv-OGTalb
OGT
IP: ITIH1
(CTD110.6)
ITIH1
Lv-Con Lv-OGTalb
Albumin
ITIH1
Liver
Serum
00.51.01.52.02.53.03.5
Lv-Con Lv-OGTalb
OGT
OGT
Liver
Skeletal muscle
Adipose tissue
OGT
B
C
A
Time (min)0 15 30 45 60 75 90
0
50
100
150
200
250
300
Glu
cose
(mg/
dl) Lv-Con
Lv-OGTalb
Glucose tolerance test (ND)
AUC (GTT)
02468
10121416
3 )
-Actin
-Actin
-Actin
-Actin
-Actin
-Actin
-Actin
-Actin
ITIH1
(C
TD11
0.6)
70
55
100
170130
(kDa)
Vehicle ST045849Vehicle
WT G13 LKOLiver
ITIH1
Vehicle ST045849Vehicle
WT G13 LKO
Glucose gavage (2 g/kg)
Serum
Albumin
ITIH1
(C
TD11
0.6)
7055
100
170130
(kDa)
Liver
Vehicle ST045849VehicleWT G13 LKO
Glucose gavage (2 g/kg)
0
0.5
1.0
1.5
2.0
2.5 WT+VehicleG13 LKO+VehG13 LKO+ST045849
ITIH1
0
0.5
1.0
1.5
2.0
2.5 WT + VehicleG13 LKO + VehG13 LKO + ST045849
Glucose gavage (2 g/kg)
ITIH1
0 15 30 45 60 75 900
50100150200250300350
Time (min)
Glu
cose
(mg/
dl)
##
##
##
WT+VehicleG13 LKO + vehicleG13 LKO + ST045849
Glucose tolerance test (ND)
05
10152025
AUC (GTT)
##
Insulin tolerance test (ND)
AUC (ITT)
02468
1012
3 )
0 30 60 90 12050
60
70
80
90
100
110
Time (min)
Lv-ConLv-OGTalb
Glu
cose
(% in
itial
)
R
elat
ive
inte
nsity
(nor
mal
ized
to
-act
in)
R
elat
ive
inte
nsity
(nor
mal
ized
to
-act
in)
R
elat
ive
inte
nsity
(nor
mal
ized
to
-act
in)
R
elat
ive
inte
nsity
(nor
mal
ized
to
-act
in)
Fig. 7. Overproduction and O-GlcNAcylation of ITIH1 induced by O-GlcNAc transferase. (A) Immunoblot analysis for O-GlcNAc proteins (CTD110.6) or ITIH1 expression inprotein lysates of livers fromWT or G13 LKOmice injectedwith ST045849, an inhibitor ofO-GlcNAc transferase (OGT; 20mg/kg bodyweight). Micewere subjected to vehicle (left,n= 2per group) or glucose gavage (right, n= 3 to 4 per group). Glucose (2 g/kg bodyweight) was orally administered tomice, and the liver tissueswere harvested after 6 hours.(B) Immunoblot analysis for ITIH1 in serum samples from the same mice as in (A). (C) Analysis of the glucose tolerance test (2 g/kg body weight) in WT and G13 LKO miceinjectedwith ST045849 (OGT inhibitor, 20mg/kg bodyweight) (n= 6 per group). Inset represents area under the curve (AUC) for the glucose tolerance test (GTT). (D) Immunoblotanalysis for ITIH1 expression in protein lysates of liver or in sera from 8-week-old C57BL/6 mice injected with lentiviral vector carrying the human OGT gene with an albuminpromoter (Lv-OGTalb) or empty control vector (Lv-Con) via the tail vein (2 × 107 transduction units each). Albuminwas the loading control for serum samples. (E and F) The effect ofhepatic Ga13 overexpression on glucosemetabolismwas determined using a glucose test (E, n = 10 per group) or insulin tolerance test (F, n = 9 to 10 per group) in the samemiceas in (D). Insets show the area under the curve (AUC) for the glucose tolerance test (GTT) or insulin tolerance test (ITT). (G) Immunoblot analyses for ITIH1 and O-GlcNAc ITIH1 inprimary hepatocytes isolated from 8-week-old C57BL/6 mice injected via tail vein with lentiviral vector carrying the human OGT gene with an albumin promoter (Lv-OGTalb) orempty control vector (Lv-Con) (2 × 107 transduction units). Immunoblotting for O-GlcNAc proteins (CTD110.6 clone) was performed on immunoprecipitates of ITIH1 in primaryhepatocyte cell lysates. (H) Immunoblot analyses for OGT in protein lysates of liver, epididymal fat tissue, and gastrocnemius muscle of 8-week-old C57BL/6 mice injected via tailveinwith lentiviral vector carrying the humanOGT genewith an albumin promoter (Lv-OGTalb) or empty vector control (Lv-Con) (2 × 107 transduction units) (n= 3 per group). Therelative band intensities were quantified by densitometry analyses for the immunoblots. Values were expressed as means ± SEM. *P < 0.05 for G13 LKO + vehicle versus WT + ve-hicle; ##P < 0.01 for G13 LKO + ST045849 versus G13 LKO + vehicle (C); and *P < 0.05, **P < 0.01 for Lv-OGTalb versus Lv-Con (E, F, and H). Data were analyzed by one-way ANOVA,followed by least significant difference (LSD) (A), Bonferroni post hoc tests (C), or two-tailed Student’s t test (E, F, and H). N.S., not significant.
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019 11 of 17

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
IH
J K
G
4
0
1
2
3
4
#
AUC (GTT)
FE
0
0.5
1.0
1.5
2.0
2.5
ITIH
1 (O
.D. 4
50/6
20)
Serum (HFD 12 weeks)
NDHFD
HFD–pre-IgGHFD-ITIH1 Ab
01020304050607080
Day 0 Day 14
Bod
y w
eigh
t (g)
Pre-IgGITIH1 Ab
G13 LKO-HFD
AUC (ITT)
02468
1012
3 )
02468
101214
AUC (ITT)3 ) #
05
101520253035
AUC (GTT)
00 20 40 60 80 100 12405060708090
100110
#
Glu
cose
(% in
itial
)
Time (min)
WT–pre-IgGG13 LKO–pre-IgGG13 LKO-ITIH1 Ab
0
0.1
0.2
0.3
0.4
0.5
ITIH
1 (O
.D. 4
50/6
20)
##
G13 LKO–pre-IgGG13 LKO-ITIH1 Ab
WT–pre-IgG
HFD
L
A B C
Rat
io
Liver/body weight
00.010.020.030.040.050.06
N.S.
Tiss
ue w
eigh
t (g)
Epidydimal fat
N.S.
00.51.01.52.02.53.03.5
NDHFD
HFD–pre-IgGHFD-ITIH1 Ab
NDHFD
HFD–pre-IgGHFD-ITIH1 Ab
WT–pre-IgGG13 LKO–pre-IgGG13 LKO-ITIH1 Ab
0 15 30 45 60 75 900
100
200
300
400
500
600
Glu
cose
(mg/
dl)
###
Time (min)
0
50
100
150
200
250
300
Day 0 Day 14
Glu
cose
(mg/
dl)
Pre-IgGITIH1 Ab 1
0
20
40
60
80
00
Skeletal muscle
Basal Insulin0
100
200
300
400
Adipose tissue
2-D
eoxy
gluc
ose
upta
ke(n
mol
/mg
prot
ein/
15 m
in)
Basal Insulin
Pre-IgGITIH1 Ab
Pre-IgGITIH1 Ab
Glucose tolerance test (HFD 11 weeks)
Insulin tolerance test (HFD 12 weeks)
Serum (HFD 13 weeks)
DFH-TW DFH-TW DFH-OKL 31G ITIH1 Ab treatment
ITIH1 Ab treatment
0 1 2 3 4 5 6 7 8 9 10 112025303540455055
NDHFD
HFD–pre-IgGHFD-ITIH1 Ab
Ab neutralization
N.S.
Bod
yw
eigh
t(g)
Weeks
D
0 15 30 45 60 75 900
100
200
300
400 NDHFDHFD–pre-IgGHFD-ITIH1 Ab
###
#
Glucose tolerance test (HFD 10 weeks)
Time (min)
Glu
cose
(mg/
dl)
#
0 20 40 60 80 100 12050
60
70
80
90
100
110 NDHFDHFD–pre-IgGHFD-ITIH1 Ab
#
#
Insulin tolerance test (HFD 11 weeks)
Time (min)
Glu
cose
(% in
itial
)
Fig. 8. Recoveryof impairedglucose tolerance inHFD-fedG13LKOmice treatedwithanti-ITIH1antibody. (A toC)Measurements for bodyweight gain and epididymal fatweights for 6-week-oldC57BL/6mice subjected to ahigh-fat diet (HFD) or normal diet (ND) for 10weekswithdaily injections of rabbit polyclonal anti-ITIH1 antibodyor control pre-IgGantibody for the last 2weeks of theHFDorNDdiet (n=7 to 8per group). Bodyweight gain (A), liver–to–bodyweight ratio (B), andepididymal fatweight (C). (D,E,G, andH) Effectsof anti-ITIH1 antibody treatment on the results of the glucose tolerance test (1.5 g/kg bodyweight) or insulin tolerance test (0.75 insulin units/kg bodyweight) in C57BL/6mice fed anHFDorND (D and E) andWTorG13 LKOmice fed anHFD (G andH).Micewere injected dailywith purified anti-ITIH1 antibody or pre-IgG (i.p., 250 mg each) for the last 2weeks ofHFDor ND feeding. (D) Analysis of the glucose tolerance test in C57BL/6mice fed anNDor HFD for 10weeks (ND, n=7; HFD, n=8; HFD–pre-IgG, n=7; HFD–anti-ITIH1 antibody, n= 8). (E)Analysis of the insulin tolerance test in C57BL/6mice fed anNDorHFD for 11weeks (ND,n=7;HFD,n=8;HFD–pre-IgG,n=6;HFD–anti-ITIH1 antibody,n=6). (F) Quantitative analysisof ELISA for ITIH1 in serum (ND,n=7; HFD,n=8; HFD–pre-IgG, n=7; HFD–anti-ITIH1 antibody, n=8). (G) Analysis of the glucose tolerance test inWTandG13 LKOmice fed anHFD for11weeks (n=7per group). (H) Analysis of the insulin tolerance test inWTandG13LKOmice fedanHFD for 12weeks (n=6per group). (I) Quantitative analysis of ELISA for serum ITIH1in WT and G13 LKO mice fed an HFD (WT–pre-IgG or G13 LKO–pre-IgG, n = 7; G13 LKO–anti-ITIH1 antibody, n = 6). (J and K) Body weight gain (J) or fasting blood glucose con-centrations (K) in G13 LKO mice fed an HFD for 13 weeks and treated with anti-ITIH1 antibody or control IgG as in (A) (n = 5 per group). Days 0 and 14 represent before and aftertreatments, respectively, with anti-ITIH1 antibody or pre-IgG control antibody. (L) Measurements of 2-deoxyglucose uptake in epididymal fat tissue ofWTmice fed an HFD for16 weeks. (Left) Basal 2-deoxyglucose uptake (n = 3 mice) and uptake after glucose gavage (n = 3 mice) in adipose tissue frommice treated with pre-IgG antibody control oranti ITIH1 antibody (right). Basal 2-deoxyglucose uptake (n = 3 mice) and uptake after glucose gavage (n = 3 mice) in skeletal soleus muscle of mice treated with pre-IgGantibody control or anti-ITIH1 antibody. For (D), (E), (G), and (H), insets represent area under the curve (AUC). Values are expressed asmeans ± SEM. *P< 0.05, **P< 0.01 for HFDversus ND (A, D, and E) or G13 LKOmice treated with pre-IgG versusWTmice treated with pre-IgG (G to I); #P < 0.05, ##P < 0.01 for mice fed anHFD and treatedwith anti-ITIH1antibody versus mice fed an HFD and treated with pre-IgG antibody (D and E) or G13 LKO mice treated with anti-ITIH1 antibody versus G13 LKO mice treated with pre-IgGantibody (G to I). Data were analyzed by one-way ANOVA followed by Bonferroni (A to K) or least significant difference (LSD) (L) post hoc tests. N.S., not significant.
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019 12 of 17

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
from theGa13 knockoutmice need to be interpreted separately from theoutcomes using common Ga13-activating ligands. Other approachessuch as Ga13-selective designer GPCRs are needed to corroborate ourproposed mechanism.
Toobtainmechanistic insights into howhigh glucose concentrationsmay down-regulate Ga13, we examined whether O-GlcNAcylationaffects Ga13 stability. A switch from high glucose (25 mM, 24 hours)to low glucose (5mM, 12 hours) caused the recovery ofGa13 toward thatof control in AML12 cells or primary hepatocytes (fig. S13, A and B).However, O-GlcNAcylation staining remained higher than control inboth AML12 and primary hepatocytes. Nonetheless, the effect of highglucose onGa13O-GlcNAcylationwas not clear in immunoprecipitationassays (fig. S13A). In addition, shOGT transfection did not prevent highglucose concentrations from repressing Ga13 (fig. S11C). Thus, Ga13stability seems to be affected by glucose concentrations in a dynamicfashion andmay not solely depend onO-GlcNAcylation. Further studiesare necessary to understand the possible effects of O-GlcNAcylation onGa13 signaling.
In the present study, proteomics-based approaches using semi-quantitative, label-free LC-MS/MS identified differential abundanceof secreted proteins in their nascent form regulated by hepatic Ga13.Labeling of peptides and proteins through either isobaric tagging(e.g., iTRAQ) or metabolic labeling (e.g., SILAC) allows more sensitivedetection of differential abundance than the present method. However,the label-freemethod enables detection of proteins in their original formfor MS-based abundance measurements and, thus, is suitable for bio-marker discovery and validation in terms of better quantification capa-bility and reproducibility (27, 28). Of the top-ranked liver-enrichedsecretory proteins affected by a decrease in Ga13, ITIH1 was identifiedas a key molecule accounting for metabolic dysfunction. ITIH1 ispredominantly synthesized and secreted from hepatocytes with varyingexpression under pathological conditions (e.g., ITIH1 was lower in pa-tients with liver fibrosis or hepatocellular carcinoma) (29, 30). Althoughwe do not necessarily exclude local ITIH1 expression in adipose tissueand skeletal muscle, our results indicate that a larger amount of liver-derived ITIH1 is incorporated into the extracellular matrix of adiposetissue and skeletal muscle in G13 LKO mice compared to wild-typemice, as indicated by the outcomes of experiments using extracellularmatrix–enriched fractions and immunohistochemistry.
Extracellularmatrix is composed ofmyriad extracellular proteins se-creted by various cell types andmodulates not only biological processesbut also intercellular communication. Growing evidence suggests thatextracellular matrix remodeling in peripheral tissues is of potential im-portance for glucose metabolism and insulin signaling under diabeticconditions (15, 16). Hyaluronan, one of the major components of ex-tracellular matrix, is an anionic nonsulfated glycosaminoglycan, whosecontent and density are increased in insulin-resistant tissues (15, 16).The stiffness or rigidity of hyaluronan, which is affected by variousinteracting proteins and proteoglycans, determines cellular function(31–33). Here, we postulated that binding of liver-derived ITIH1 tohyaluronan results in extracellular matrix remodeling in the patho-genesis of insulin resistance and diabetes. In our study, hepatic Ga13ablation had no effect on hyaluronan content in adipose tissue andskeletal muscle in mice. Instead, our findings indicated enhanced co-localization and interaction of ITIH1 and hyaluronan in the tissues ofG13 LKOmice, highlighting the role of ITIH1 as a hyaluronan-bindingprotein that contributes to peripheral insulin resistance. In the liver,both glucose metabolism and insulin sensitivity were not affected byGa13 deficiency, implying the marginal effect of ITIH1 on hyaluronan-
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019
mediated insulin resistance in the liver, presumably because hyaluronanis metabolized and degraded specifically by liver sinusoidal endothelialcells via endocytosis (34). In line with this, it is reported that hepaticstellate cells are the unique cell type responsible for hyaluronan syn-thesis in the liver, supporting the contention that excessive accumula-tion of hyaluronan is observed mostly in fibrotic/cirrhotic liver (35).Consistently, ITIH1-hyaluronan complexes were not readily detectedin the liver of G13 LKOmice despite the marked staining intensity forITIH1 in liver. Our results demonstrate that the liver contributes to themaintenance of systemic glucose homeostasis by regulating insulinsensitivity in other metabolic organs through ITIH1 secretion.
O-GlcNAcylation of proteins as a dynamic posttranslational modi-fication may enable cells to sense and respond quickly to glucose avail-ability (19–21). O-GlcNAcylation of protein extracellular domains hasbeen found in a variety of organisms (36–38). Similarly, secreted mac-rophage migration inhibitory factor is O-GlcNacylated by O-GlcNACtransferase, which affects its ability to regulate tumorigenesis (39),consistent with the observation that O-GlcNAcylation was aberrantlyincreased in several secretory proteins lacking an epidermal growthfactor (EGF)–like domain (40). Our data showed that ITIH1 oversecre-tion due to Ga13 deficiency or hyperglycemia was accompanied byO-GlcNAC transferase expression induction in hepatocytes. We alsodiscovered the ability of O-GlcNAC transferase to increase ITIH1 sta-bility with diminished ubiquitination of ITIH1 by either immuno-precipitation or immunoblotting assay, which is in line with thereport that O-GlcNAcylation controls protein stability through proteinubiquitination (22). The outcomes from LC-MS/MS analysis providedfurther evidence for O-GlcNAc modification of ITIH1. We addressedthe engagement of Rho in our proposed signaling pathway, althoughthe detailed mechanistic insight by which loss of Ga13 up-regulatesO-GlcNAC transferase remains to be investigated. We demonstratedthe inhibitory effect of hyperglycemia on Ga13 in mouse hepatocytesand the resultant overproduction of ITIH1 mediated by O-GlcNACtransferase–catalyzed O-GlcNAcylation. In our study, we cannot ruleout the possibility that Ga13 signaling modulates O-GlcNAcase or itsactivity, which opposes O-GlcNAC transferase function. In addition,our results do not necessarily exclude the potential involvement ofother liver-derived secretory proteins in the development of systemicinsulin resistance as O-GlcNAC transferase overexpression might re-sult in a generalized increase in protein O-GlcNAcylation that is notlimited to ITIH1.
Collectively, our findings revealed that a decrease in hepatic Ga13promoted overproduction of O-GlcNAcylated ITIH1 in hepatocytesand its secretion into the systemic circulation. The hypothesis thatITIH1 binds directly to hyaluronan on the surface of adipose tissueand skeletal muscle resulting in extracellular matrix stabilization andconsequent insulin resistance provides a new conceptual frameworkby which the liver may regulate systemic glucose homeostasis in re-sponse to varying glucose concentrations.
There are some limitations to our study. First, we used several in vivogene transfer techniques in G13 LKO mice to modulate Ga13/O-GlcNAC transferase expression. A genetic loss-of-function approachtargeting ITIH1 in the liver is needed to provide support for our pro-posed mechanism. Second, despite our attempt to examine the possiblerole of O-GlcNAcylation on Ga13 function, the basis underlying howthe hyperglycemic condition represses Ga13 needs to be investigatedfurther. Third, the candidate GPCR/corresponding ligands responsiblefor the observed signaling and functional pathways were not identifiedhere. Another approach is needed to identify the candidate GPCR
13 of 17

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
ligands and study them in depth (e.g., high-throughput ligand screen-ing). Fourth, a detailed experimental approach is necessary to under-stand the biology of ITIH1 and hyaluronan in insulin desensitization.Last, ITIH1 concentrations in patients with impaired glucose toleranceor type 2 diabetes were quite high (23 to 166 mg/ml), which wouldmakeit difficult to use a neutralizing antibody to reduce circulating ITIH1 inclinical situations due to the high antibody dosage thatwould be needed.Thus, other therapeutic options would be needed to efficiently accom-plish the tight management of blood ITIH1 concentrations, such assiRNA/shRNA-based gene therapy.Nevertheless, our findings suggestthat ITIH1 should be investigated further as a target for developingnew treatments for diabetes.
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
MATERIALS AND METHODSStudy designThe objective of the study was to determine the effects of hepatic Ga13on whole-body glucose metabolism in mice. We aimed to elucidatethe underlying mechanisms of Ga13’s potential effects using primaryhepatocytes and G13 LKO mice. We used lentiviral or hydrody-namic injection–mediated in vivo delivery of genes encoding Ga13or O-GlcNAc transferase to mice with diabetes induced by feedingthemice a high-fat diet, gavaging themwith glucose, or treating themwith streptozotocin.We validated the clinical relevance of our preclinicalfindings in two independent cohorts of human subjects, who had im-paired glucose tolerance or overt diabetes induced by NAFLD (cohort#1) or chronic hepatitis C virus infection (cohort #2). Secretome analysisusing LC-MS/MS technology was conducted to identify putative targetsresponsible for the development of systemic insulin resistance in G13LKO mice. Overall, glucose tolerance in the mice was analyzed byperforming a glucose tolerance test, an insulin tolerance test, and fastingblood glucose/insulinmeasurements. The studywas extended to examineantibody neutralization of ITIH1 inmice to assess the potential of ITIH1as a therapeutic target. For in vivo experiments, age-matched mice wererandomly allocated to different groups, but the experimenters were notblinded. Only mice in poor health or with an insufficient metabolic re-sponse to diabetic insults were excluded from data analysis (one or twomice per group for Figs. 7F and 8E).
AnimalsAnimal experiments were conducted under the guidelines of the Insti-tutional Animal Use and Care Committee at Seoul National University.All animals were maintained in a 12-hour light/dark cycle and fed adlibitum. All mice used were male and had C57BL/6 background.C57BL/6, ob/ob, or db/db mice were purchased from the Jackson Lab-oratory (Bar Harbor, ME). Gna13flox/flox mice (a gift from S. Offer-manns, Max Planck Institute, Germany) (41) were crossed withalbumin-Cre transgenic mice (the Jackson Laboratory) to generateG13 LKO mice. Gna13flox/flox mice without detectable Cre gene wereused as wild-type (WT) littermates. For diet-induced obesityexperiments, mice at the age of 8 to 12 weeks were fed either a high-fat diet (HFD; 60% kcal fat; Research Diets D12492, New Brunswick,NJ) or a normal chow diet (ND) for 5 to 16 weeks. For an acute insulininjection experiment, mice were fasted overnight and intraperitoneallyinjected with insulin (2 insulin units/kg body weight; Humalog, Lilly,Indianapolis, IN) and subsequently euthanized 15 min afterward. Fora fasting/refeeding transition model, mice were fasted for 24 hours,followed by refeeding for 4 hours. For a streptozotocin-induced diabe-tes model, 10-week-old C57BL/6 mice were intraperitoneally injected
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019
with 200 ml of either citrate buffer (pH 4.5) (Sigma-Aldrich, St. Louis,MO) or streptozotocin [50 mg/kg in citrate buffer (pH 4.5)] (Sigma-Aldrich) once a day for 5 consecutive days andwere euthanized 4weeksafterward. For an oral glucose gavage experiment, 10-week-old C57BL/6 mice were fasted overnight, were given a single bolus of glucose (2 g/kgbody weight) by gavage, and euthanized at indicated times thereafter. Inanother set of experiments,WTorG13LKOmice at 12weeks of agewereinjected with ST045849 (TimTec, Newark, DE) at the dose of 20 mg/kgbody weight, as resolved in a 2.5% DMSO/2.5% Tween 20/95% PBSsolution, once a day for 4 consecutive days and euthanized 6 hoursafter the last treatment. Glucose tolerance test or glucose gavageexperiments were performed in an identical manner, where the as-says were initiated 6 hours after the last injection.
Human samplesWritten informed consent was obtained from all subjects before par-ticipating in research studies. Studies using human samples were re-viewed and approved by the independent Institutional Review Boardof the Seoul Metropolitan Government Seoul National University Bor-amae Medical Center. The subject cohort included patients from twoclinical studies (cohorts #1 and #2). Liver biopsies and serum/plasmasamples were obtained from diabetic patients with NAFLD (cohort#1) or chronic hepatitis C virus infection (cohort #2). For subjects withbiopsy-proven NAFLD (cohort #1), measurements of serum bio-chemical parameters, type 2 diabetes status, and histological assessmentwere carried out for 31 human subjects. These subjects included thosewith normal glucose tolerance (fasting blood glucose concentrationswere lower than 110mg/dl, n = 11), impaired glucose tolerance (fastingblood glucose concentrations ranged between 110 and 126 mg/dl,n = 10), or overt type 2 diabetes (fasting blood glucose concentrationsweremore than 126mg/dl, n= 11). Together, these subjects had a broadrange of values on the HOMA-IR test (ranging from 0.49 to 22.01).None of the human subjects were taking antidiabetic medications.Three or five subjects in each group (n = 3 for normal glucose toleranceand impaired glucose tolerance; n = 5 for type 2 diabetes) were takingantihyperlipidemic medications (statins) at the time the measurementswere taken (see table S1 for the characteristics of these individuals). Forsubjects with chronic hepatitis C virus infection (cohort #2), serum bio-chemical parameters and glucose tolerance status were assessed in25 subjects (13 males, 12 females) with a broad range of HOMA-IRvalues (ranging from 1.3 to 21.0). The patients were subdivided andanalyzed according to the HOMA-IR index. Subjects in cohort #2had an average age of 57.0 ± 2.0 years, with a body mass index (BMI)of 24.8 ± 0.8 kg/m2 and with a fasting blood glucose concentration of119.4 ± 8.7 mg/dl.
Glucose tolerance test and insulin tolerance testFor glucose tolerance tests (GTT), mice were orally administered withglucose (1.5 to 2 g/kg body weight) after overnight fasting, and bloodwas drawn to measure glucose concentrations at indicated times there-after. For insulin tolerance tests (ITT), insulin (0.75 to 1.5 insulin units/kgbody weight; Humalog, Lilly) was intraperitoneally injected into miceafter fasting for 6 hours, and bloodwas drawn tomeasure blood glucoseat indicated times. Insulin concentrations were measured at each indi-cated time in serum collected from the mice subjected to GTT.
Glucose production assays in primary hepatocytesThe glucose concentration was determined using the Amplex RedGlucose/Glucose Oxidase Assay Kit (Invitrogen) according to the
14 of 17

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
manufacturer’s instructions. The cells were lysed, and the proteinconcentration was determined to normalize the values for glucoseproduction.
Conditioned media preparation from primary hepatocytesCultured primary hepatocytes frommice fed an HFD for 5 weeks werewashed with PBS and incubated in serum-free Opti-MEM medium(Gibco BRL). Conditioned media (CM) were collected after 24 hoursand centrifuged at 3000g for 5 min, and the supernatant excluding de-bris was stored at −80°C until use. For secretome analysis, CM was de-pleted of abundant serumproteins (e.g., albumin and immunoglobulin)using commercially available immunodepletion resin (MIDR002-020,R&D Systems), followed by concentration at 4800g centrifugation for90 min at 4°C with Amicon Ultra centrifugal filter units (10 kDaMWCO; Millipore, Burlington, MA).
Sample preparation for proteomics of hepatocyteCM samplesFor liquid chromatography–tandem mass spectrometry (LC-MS/MS)analysis of CM samples from primary hepatocytes, protein concentra-tion of CM was measured using Quick Start Bradford 1 × Dye Reagent(Bio-Rad Laboratories, Hercules, CA). Then, a fraction of proteins(100 mg) was prepared in 50 mM ammonium bicarbonate and was re-duced and alkylated by treatment with dithiothreitol (Bio-Rad Labora-tories) and iodoacetamide (Sigma-Aldrich, St. Louis, MO). Trypsin(Promega, Madison, WI) was added to digest samples at a protein-to-enzyme ratio of 50:1 (w/w), and the solution was incubated at 37°C for16 hours. Digested samples were separated into 12 fractions using highpH on a C18 column as the first dimension.
ITIH1-enriched sample preparation for proteomicsof O-GlcNAcylationHEK293A cells overexpressed with human ITIH1 (Origene, Rockville,MD, USA) were subjected to SDS-PAGE. ITIH1 bands were cut fromthe SDS-PAGE gel for LC-MS/MS analysis of ITIH1O-GlcNAcylation.Briefly, a fractionof proteins prepared in 50mMammoniumbicarbonatewas successively reduced and alkylated by treatment with dithiothreitol(Sigma-Aldrich) and iodoacetamide (Sigma-Aldrich). In-gel digestionwas conducted by incubation with trypsin at 37°C overnight, and thesamplewas subsequently resolved by online reversed-phase chromatog-raphy using a C18 column as a cleanup procedure.
LC-MS/MS analysis for hepatocyte secretomeSpectra raw data were acquired on a linear trap quadrupole (LTQ)–Orbitrap (Thermo Fisher, San Jose, CA) with EASY-nLC II (ThermoFisher Scientific). An autosampler was used to load 6-ml aliquots ofthe peptide solutions into an EASY-Column; C18 Trap column withan inner diameter of 100 mm, a length of 20mm, and a particle size of5 mm (Thermo Fisher Scientific). The peptides were desalted and con-centrated on the trap column for 15min at a flow rate of 2ml/min. Then,the trapped peptides were separated on an EASY-Column; C18 analyticcolumn with an inner diameter of 75 mm, a length of 100 mm, and aparticle size of 3 mm(120Å; fromThermoFisher Scientific). Themobilephases were composed of 100%water (A) and 100% acetonitrile (ACN)(B), and each contained 0.1% formic acid. The voltage applied to pro-duce the electrospray was 2.0 kV. During the chromatographic separa-tion, the LTQ-Orbitrap was operated in a data-dependent acquisitionmode. The MS data were acquired using the following parameters: fullscans were acquired in Orbitrap at a resolution of 60,000 for each MS/
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019
MS measurement, and six data-dependent collision-induced dissocia-tion (CID) MS/MS scans were acquired in LTQ with 10-ms activationtime performed for each sample, 35% normalized collision energy(NCE) in CID, and ±1.5 Da isolation window. Previously fragmentedions were excluded for 180 s. Then, the datasets generated by LTQ-Or-bitrap were analyzed using the Proteome Discoverer (version 1.3.0.339,Thermo Fisher Scientific) and Scaffold (version 4.4.1, ProteomeSoftware Inc., Portland, OR) Platform and searched against theUniProtmouse protein database (release 2014_06) using SEQUEST and X!tan-dem. Peptide identifications were accepted if they could be establishedat greater than 90% probability by the Scaffold Local FDR algorithm.Protein identifications were accepted if they could be established at agreater than 95%probability. Thesewere also accepted if they containedat least two identified unique peptides. Protein probabilities were as-signed by the Protein Prophet algorithm.
Secreted proteins were defined as either the presence of N-terminalsignal peptide or the annotation in UniProt by Gene Ontology cellularcompartment (GO:0005615 orGO:0005576) or the keyword for cellularcomponents (secreted). Liver-enriched proteins were considered asthose annotated as “tissue-enriched in liver” or “liver-specific” inUniProtand/or Human Protein Atlas.
ITIH1-neutralizing antibody treatmentThe rabbit polyclonal antibody against mouse ITIH1 was producedby immunization with a KLH-conjugated synthetic peptide pre-dicted from mouse ITIH1 sequence (C-DKAREVAFDVE). The an-tibody was then purified from the serum of final bleed through IgGpurification. Preimmune IgG (pre-IgG) was similarly purified andused as a control. Mice were daily injected with purified antibody orpre-IgG (diluted in sterile PBS, i.p., 250 mg each) for the last 2 weeksduring the diet feeding.
Statistical analysesValues are expressed asmeans ± SEM. Statistical significance was testedusing a two-tailed Student’s t test or one-way ANOVAwith Bonferronior least significant difference (LSD)multiple comparisonswhere appro-priate. Differences were considered significant at P < 0.05.
SUPPLEMENTARY MATERIALSstm.sciencemag.org/cgi/content/full/11/513/eaan4735/DC1Materials and MethodsFig. S1. Decrease in hepatic Ga13 in patients with diabetes.Fig. S2. Correlations between hepatic Ga13 and lipid profiles in patients with diabetes.Fig. S3. A metabolic and liver function profile in G13 LKO mice fed a high-fat diet.Fig. S4. Impaired glucose homeostasis and insulin resistance in G13 LKO mice fed anormal diet.Fig. S5. Correlations between serum ITIH1 concentrations and lipid profiles in patientswith NAFLD.Fig. S6. ITIH1 and ITIH2 concentrations in the liver of patients with diabetes or G13 LKO micefed a high-fat diet.Fig. S7. Immunoblotting for extracellular matrix and cytoplasmic protein markers.Fig. S8. Immunofluorescence staining for ITIH1-hyaluronan complexes in vitro.Fig. S9. Increase in O-GlcNAC transferase–mediated O-GlcNAcylation and ITIH1 concentrationsafter loss of Ga13.Fig. S10. LC-MS/MS analysis of O-GlcNAc modification of human ITIH1.Fig. S11. O-GlcNAC transferase–mediated stabilization of ITIH1 through suppression ofproteasomal degradation.Fig. S12. The effect of ITIH1 silencing on insulin sensitivity in vitro and effects of anti-ITIH1antibody treatment of mice in vivo.Fig. S13. The effect of a high to low glucose transition on O-GlcNAcylation and Ga13concentrations in mice in vivo.Table S1. Characteristics of subjects with NAFLD in cohort #1.
15 of 17

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
Data file S1.References (42–51)View/request a protocol for this paper from Bio-protocol.
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from
REFERENCES AND NOTES1. N. Turner, G. M. Kowalski, S. J. Leslie, S. Risis, C. Yang, R. S. Lee-Young, J. R. Babb,
P. J. Meikle, G. I. Lancaster, D. C. Henstridge, P. J. White, E. W. Kraegen, A. Marette,G. J. Cooney, M. A. Febbraio, C. R. Bruce, Distinct patterns of tissue-specific lipidaccumulation during the induction of insulin resistance in mice by high-fat feeding.Diabetologia 56, 1638–1648 (2013).
2. V. T. Samuel, Z.-X. Liu, X. Qu, B. D. Elder, S. Bilz, D. Befroy, A. J. Romanelli, G. I. Shulman,Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease. J. Biol. Chem.279, 32345–32353 (2004).
3. H. Misu, T. Takamura, N. Matsuzawa, A. Shimizu, T. Ota, M. Sakurai, H. Ando, K. Arai,T. Yamashita, M. Honda, T. Yamashita, S. Kaneko, Genes involved in oxidativephosphorylation are coordinately upregulated with fasting hyperglycaemia in livers ofpatients with type 2 diabetes. Diabetologia 50, 268–277 (2007).
4. K. K. Y. Lai, D. Kolippakkam, L. Beretta, Comprehensive and quantitative proteomeprofiling of the mouse liver and plasma. Hepatology 47, 1043–1051 (2008).
5. R. C. Meex, A. J. Hoy, A. Morris, R. D. Brown, J. C. Y. Lo, M. Burke, R. J. A. Goode,B. A. Kingwell, M. J. Kraakman, M. A. Febbraio, J. W. Greve, S. S. Rensen, M. P. Molloy,G. I. Lancaster, C. R. Bruce, M. J. Watt, Fetuin B is a secreted hepatocyte factor linkingsteatosis to impaired glucose metabolism. Cell Metab. 22, 1078–1089 (2015).
6. S. Vernia, J. Cavanagh-Kyros, L. Garcia-Haro, G. Sabio, T. Barrett, D. Y. Jung, J. K. Kim, J. Xu,H. P. Shulha, M. Garber, G. Gao, R. J. Davis, The PPARa-FGF21 hormone axis contributes tometabolic regulation by the hepatic JNK signaling pathway. Cell Metab. 20, 512–525(2014).
7. H. Misu, T. Takamura, H. Takayama, H. Hayashi, N. Matsuzawa-Nagata, S. Kurita, K. Ishikura,H. Ando, Y. Takeshita, T. Ota, M. Sakurai, T. Yamashita, E. Mizukoshi, T. Yamashita,M. Honda, K. Miyamoto, T. Kubota, N. Kubota, T. Kadowaki, H.-J. Kim, I.-K. Lee,Y. Minokoshi, Y. Saito, K. Takahashi, Y. Yamada, N. Takakura, S. Kaneko, A liver-derivedsecretory protein, selenoprotein P, causes insulin resistance. Cell Metab. 12, 483–495(2010).
8. W. M. Oldham, H. E. Hamm, Heterotrimeric G protein activation by G-protein-coupledreceptors. Nat. Rev. Mol. Cell Biol. 9, 60–71 (2008).
9. M. P. Strathmann, M. I. Simon, G alpha 12 and G alpha 13 subunits define a fourth class ofG protein alpha subunits. Proc. Natl. Acad. Sci. U.S.A. 88, 5582–5586 (1991).
10. Q. Zhang, T. L. Fillmore, A. A. Schepmoes, T. R. W. Clauss, M. A. Gritsenko, P. W. Mueller,M. Rewers, M. A. Atkinson, R. D. Smith, T. O. Metz, Serum proteomics reveals systemicdysregulation of innate immunity in type 1 diabetes. J. Exp. Med. 210, 191–203 (2013).
11. P. Ghosh, R. Sahoo, A. Vaidya, M. Chorev, J. A. Halperin, Role of complement andcomplement regulatory proteins in the complications of diabetes. Endocr. Rev. 36,272–288 (2015).
12. L. Zhuo, V. C. Hascall, K. Kimata, Inter-a-trypsin inhibitor, a covalent protein-glycosaminoglycan-protein complex. J. Biol. Chem. 279, 38079–38082 (2004).
13. A. Hamm, J. Veeck, N. Bektas, P. J. Wild, A. Hartmann, U. Heindrichs, G. Kristiansen,T. Werbowetski-Ogilvie, R. Del Maestro, R. Knuechel, E. Dahl, Frequent expression loss ofinter-alpha-trypsin inhibitor heavy chain (ITIH) genes in multiple human solid tumors: Asystematic expression analysis. BMC Cancer 8, 25 (2008).
14. L. Huang, M. Yoneda, K. Kimata, A serum-derived hyaluronan-associated protein (SHAP) isthe heavy chain of the inter alpha-trypsin inhibitor. J. Biol. Chem. 268, 26725–26730(1993).
15. L. Kang, L. Lantier, A. Kennedy, J. S. Bonner, W. H. Mayes, D. P. Bracy, L. H. Bookbinder,A. H. Hasty, C. B. Thompson, D. H. Wasserman, Hyaluronan accumulates with high-fatfeeding and contributes to insulin resistance. Diabetes 62, 1888–1896 (2013).
16. A. S. Williams, L. Kang, D. H. Wasserman, The extracellular matrix and insulin resistance.Trends Endocrinol. Metab. 26, 357–366 (2015).
17. C. Wang, M. Eufemi, C. Turano, A. Giartosio, Influence of the carbohydrate moiety on thestability of glycoproteins. Biochemistry 35, 7299–7307 (1996).
18. G. Walsh, R. Jefferis, Post-translational modifications in the context of therapeuticproteins. Nat. Biotechnol. 24, 1241–1252 (2006).
19. G. W. Hart, M. P. Housley, C. Slawson, Cycling of O-linked b-N-acetylglucosamine onnucleocytoplasmic proteins. Nature 446, 1017–1022 (2007).
20. J. Ma, G. W. Hart, Protein O-GlcNAcylation in diabetes and diabetic complications.Expert Rev. Proteomics 10, 365–380 (2013).
21. L. K. Kreppel, M. A. Blomberg, G. W. Hart, Dynamic glycosylation of nuclear and cytosolicproteins. Cloning and characterization of a unique O-GlcNAc transferase with multipletetratricopeptide repeats. J. Biol. Chem. 272, 9308–9315 (1997).
22. H.-B. Ruan, Y. Nie, X. Yang, Regulation of protein degradation by O-GlcNAcylation:Crosstalk with ubiquitination. Mol. Cell. Proteomics 12, 3489–3497 (2013).
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019
23. A. K. Rines, K. Sharabi, C. D. J. Tavares, P. Puigserver, Targeting hepatic glucosemetabolism in the treatment of type 2 diabetes. Nat. Rev. Drug Discov. 15, 786–804(2016).
24. S. Offermanns, V. Mancino, J.-P. Revel, M. I. Simon, Vascular system defects and impairedcell chemokinesis as a result of Ga13 deficiency. Science 275, 533–536 (1997).
25. M. Bogdani, P. Y. Johnson, S. Potter-Perigo, N. Nagy, A. J. Day, P. L. Bollyky, T. N. Wight,Hyaluronan and hyaluronan-binding proteins accumulate in both human type 1 diabeticislets and lymphoid tissues and associate with inflammatory cells in insulitis. Diabetes 63,2727–2743 (2014).
26. K. Palczewski, Oligomeric forms of G protein-coupled receptors (GPCRs). Trends Biochem. Sci.35, 595–600 (2010).
27. N. Q. Liu, L. J. M. Dekker, C. Stingl, C. Güzel, T. De Marchi, J. W. M. Martens, J. A. Foekens,T. M. Luider, A. Umar, Quantitative proteomic analysis of microdissected breast cancertissues: Comparison of label-free and SILAC-based quantification with shotgun, directed, andtargeted MS approaches. J. Proteome Res. 12, 4627–4641 (2013).
28. B. Domon, R. Aebersold, Options and considerations when selecting a quantitativeproteomics strategy. Nat. Biotechnol. 28, 710–721 (2010).
29. F. Caillot, M. Hiron, O. Goria, M. Gueudin, A. Francois, M. Scotte, M. Daveau, J.-P. Salier,Novel serum markers of fibrosis progression for the follow-up of hepatitis C virus-infectedpatients. Am. J. Pathol. 175, 46–53 (2009).
30. H. G. Hass, J. Jobst, U. Vogel, M. Scheurlen, O. Nehls, Overexpression of tumor-associatedtrypsin inhibitor (SPINK1/TATI) in hepatitis C-associated hepatocellular carcinoma: Potentialimplications for viral hepatocarcinogenesis. Oncol. Res. Treat. 37, 732–738 (2014).
31. S. Garantziotis, E. Zudaire, C. S. Trempus, J. W. Hollingsworth, D. Jiang, L. H. Lancaster,E. Richardson, L. Zhuo, F. Cuttitta, K. K. Brown, P. W. Noble, K. Kimata, D. A. Schwartz,Serum inter-a-trypsin inhibitor and matrix hyaluronan promote angiogenesis in fibroticlung injury. Am. J. Respir. Crit. Care Med. 178, 939–947 (2008).
32. L. Zhuo, M. Yoneda, M. Zhao, W. Yingsung, N. Yoshida, Y. Kitagawa, K. Kawamura,T. Suzuki, K. Kimata, Defect in SHAP-hyaluronan complex causes severe femaleinfertility. A study by inactivation of the bikunin gene in mice. J. Biol. Chem. 276,7693–7696 (2001).
33. C. B. Knudson, W. Knudson, Hyaluronan-binding proteins in development, tissuehomeostasis, and disease. FASEB J. 7, 1233–1241 (1993).
34. S. Eriksson, J. R. E. Fraser, T. C. Laurent, H. Pertoft, B. Smedsrod, Endothelial cells are a siteof uptake and degradation of hyaluronic acid in the liver. Exp. Cell Res. 144, 223–228(1983).
35. A. M. Gressner, R. Haarmann, Hyaluronic acid synthesis and secretion by rat liver fatstoring cells (perisinusoidal lipocytes) in culture. Biochem. Biophys. Res. Commun. 151,222–229 (1988).
36. A. Matsuura, M. Ito, Y. Sakaidani, T. Kondo, K. Murakami, K. Furukawa, D. Nadano,T. Matsuda, T. Okajima, O-linked N-acetylglucosamine is present on the extracellulardomain of notch receptors. J. Biol. Chem. 283, 35486–35495 (2008).
37. Y. Sakaidani, T. Nomura, A. Matsuura, M. Ito, E. Suzuki, K. Murakami, D. Nadano, T. Matsuda,K. Furukawa, T. Okajima, O-linked-N-acetylglucosamine on extracellular protein domainsmediates epithelial cell-matrix interactions. Nat. Commun. 2, 583 (2011).
38. J. F. Alfaro, C.-X. Gong, M. E. Monroe, J. T. Aldrich, T. R. W. Clauss, S. O. Purvine, Z. Wang,D. G. Camp II, J. Shabanowitz, P. Stanley, G. W. Hart, D. F. Hunt, F. Yang, R. D. Smith,Tandem mass spectrometry identifies many mouse brain O-GlcNAcylated proteinsincluding EGF domain-specific O-GlcNAc transferase targets. Proc. Natl. Acad. Sci. U.S.A.109, 7280–7285 (2012).
39. Y. Zheng, X. Li, X. Qian, Y. Wang, J.-H. Lee, Y. Xia, D. H. Hawke, G. Zhang, J. Lyu, Z. Lu,Secreted and O-GlcNAcylated MIF binds to the human EGF receptor and inhibits itsactivation. Nat. Cell Biol. 17, 1348–1355 (2015).
40. P. Netsirisawan, D. Chokchaichamnankit, C. Srisomsap, J. Svasti, V. Champattanachai,Proteomic analysis reveals aberrant O-GlcNAcylation of extracellular proteins from breastcancer cell secretion. Cancer Genomics Proteomics 12, 201–209 (2015).
41. A. Moers, B. Nieswandt, S. Massberg, N. Wettschureck, S. Grüner, I. Konrad, V. Schulte,B. Aktas, M.-P. Gratacap, M. I. Simon, M. Gawaz, S. Offermanns, G13 is an essentialmediator of platelet activation in hemostasis and thrombosis. Nat. Med. 9, 1418–1422(2003).
42. S. H. Hwahng, S. H. Ki, E. J. Bae, H. E. Kim, S. G. Kim, Role of adenosinemonophosphate-activated protein kinase-p70 ribosomal S6 kinase-1 pathway inrepression of liver X receptor-alpha-dependent lipogenic gene induction and hepaticsteatosis by a novel class of dithiolethiones. Hepatology 49, 1913–1925 (2009).
43. Y. M. Yang, S. Y. Seo, T. H. Kim, S. G. Kim, Decrease of microRNA-122 causes hepatic insulinresistance by inducing protein tyrosine phosphatase 1B, which is reversed by licoriceflavonoid. Hepatology 56, 2209–2220 (2012).
44. J. H. Koo, T. H. Kim, S. Y. Park, M. S. Joo, C. Y. Han, C. S. Choi, S. G. Kim, Ga13 ablationreprograms myofibers to oxidative phenotype and enhances whole-body metabolism.J. Clin. Invest. 127, 3845–3860 (2017).
45. Y. M. Yang, W. H. Lee, C. G. Lee, J. An, E.-S. Kim, S. H. Kim, S.-K. Lee, C. H. Lee,D. N. Dhanasekaran, A. Moon, S. Hwang, S. J. Lee, J.-W. Park, K. M. Kim, S. G. Kim, Ga12 gep
16 of 17

SC I ENCE TRANS LAT IONAL MED I C I N E | R E S EARCH ART I C L E
at Seo
http://stm.sciencem
ag.org/D
ownloaded from
oncogene deregulation of p53-responsive microRNAs promotes epithelial–mesenchymaltransition of hepatocellular carcinoma. Oncogene 34, 2910–2921 (2015).
46. K.-J. Shin, E. A. Wall, J. R. Zavzavadjian, L. A. Santat, J. Liu, J.-I. Hwang, R. Rebres,T. Roach, W. Seaman, M. I. Simon, I. D. Fraser, A single lentiviral vector platform formicroRNA-based conditional RNA interference and coordinated transgene expression.Proc. Natl. Acad. Sci. U.S.A. 103, 13759–13764 (2006).
47. P. Kelly, L. N. Stemmle, J. F. Madden, T. A. Fields, Y. Daaka, P. J. Casey, A role for the G12
family of heterotrimeric G proteins in prostate cancer invasion. J. Biol. Chem. 281,26483–26490 (2006).
48. T. K. Kwak, H. Kim, O. Jung, S.-A. Lee, M. Kang, H. J. Kim, J.-M. Park, S.-H. Kim,J. W. Lee, Glucosamine treatment-mediated O-GlcNAc modification of paxillindepends on adhesion state of rat insulinoma INS-1 cells. J. Biol. Chem. 285,36021–36031 (2010).
49. T. H. Kim, J. S. Eom, C. G. Lee, Y. M. Yang, Y. S. Lee, S. G. Kim, An active metabolite ofoltipraz (M2) increases mitochondrial fuel oxidation and inhibits lipogenesis in the liverby dually activating AMPK. Br. J. Pharmacol. 168, 1647–1661 (2013).
50. W. Yingsung, L. Zhuo, M. Morgelin, M. Yoneda, D. Kida, H. Watanabe, N. Ishiguro, H. Iwata,K. Kimata, Molecular heterogeneity of the SHAP-hyaluronan complex. Isolation andcharacterization of the complex in synovial fluid from patients with rheumatoid arthritis.J. Biol. Chem. 278, 32710–32718 (2003).
51. A. Naba, K. R. Clauser, R. O. Hynes, Enrichment of extracellular matrix proteins fromtissues and digestion into peptides for mass spectrometry analysis. J. Vis. Exp. 2015,e53057 (2015).
Acknowledgments: We thank S. Offermanns for providing the Gna13flox/flox mice. Funding:S.G.K. was supported by the National Research Foundation (NRF) funded by the Koreangovernment (Ministry of Science, ICT and Future Planning) (no. 2017K1A1A2004511). W.K. wassupported by the Korea Health Technology R&D Project through the Korea Health IndustryDevelopment Institute funded by the Ministry of Health & Welfare, Republic of Korea(no. HI17C0912). C.S.C.was supported by a grant from theBio andMedical TechnologyDevelopmentProgram of the NRF, funded by the MSIP (no. 2014M3A9D5A01073886). T.H.K. was supported bythe Basic Science Research Program of the Ministry of Education (NRF no. 2016R1A6A3A01011043and NRF no. 2018R1A6A3A11048112). This study was supported, in part, by a fund from the KoreaInstitute of Oriental Medicine (no. K16820). Author contributions: T.H.K. and S.G.K. conceived theproject, designed overall in vivo and in vitro experiments, and wrote the manuscript. T.H.K.
Kim et al., Sci. Transl. Med. 11, eaan4735 (2019) 9 October 2019
performed most of the experiments and data analysis with contributions from J.H.K., M.J.H., andC.Y.H., who performedglucose and insulin tolerance tests and virus and hydrodynamic tail vein injectionexperiments. S.-Y.P. and C.S.C. performed exploratory experiments for metabolic phenotyping ofanimals and assisted in the analysis and interpretation of data. T.H.K. and M.J.H. performed primaryhepatocyte isolation and preparation of conditioned media samples for LC-MS/MS analysis.Y.-I. K. and J.-Y. C. performed and analyzed LC-MS/MS for secretome studies. I.J.C. and C.H.L.generated adenoviral Ga13 active mutant. J.W.L. provided input on O-GlcNAc transferaseexperiments and constructs. W.K. collected, analyzed, and provided human samples. S.G.K.supervised the overall study and provided funding. All authors discussed the results andcommented on themanuscript. Competing interests: S.G.K. is a consultant for Pharmaking Co. andWooshin Labotachi Co. in Korea. W.K. consults and lectures for Gilead, Boehringer-Ingelheim,Eisai, Samil, Ildong, LG Chemistry, CJ Healthcare-Kolmar, GreenCross, BuKwang, and Standigmand receives research support from Pfizer and Roche. C.S.C. has stock options in MD Healthcare.The other authors declare that they have no competing interests. S.G.K., T.H.K., and J.-Y.C. areco-inventors on patent no. 10-2019-0034314 entitled “Method of screening nucleic acid-basedmaterial targeting ITIH1 for treating disease related to hyperglycemia” and patent no. 10-2019-0042917 entitled “Method of screening small molecular material targeting ITIH1 for treatingdisease related to hyperglycemia.” S.G.K., T.H.K., and W.K. are co-inventors on patent no.10-2019-0109433 entitled “Use of ITIH1 for detecting insulin resistance in disease associatedwith glucose intolerance” and patent no. 10-2019-0109892 entitled entitled “Pharmaceuticalcomposition comprising antibody specifically binding to ITIH1 for improving insulin resistance.”Data and materials availability: All data associated with this study are in the paper or theSupplementary Materials. G13 LKO mice with liver-specific ablation of Gna13 are available throughan MTA from Sang Geon Kim.
Submitted 18 April 2017Resubmitted 18 February 2018Accepted 22 March 2019Published 9 October 201910.1126/scitranslmed.aan4735
Citation: T. H. Kim, J. H. Koo, M. J. Heo, C. Y. Han, Y.-I. Kim, S.-Y. Park, I. J. Cho, C. H. Lee,C. S. Choi, J. W. Lee, W. Kim, J.-Y. Cho, S. G. Kim, Overproduction of inter-a-trypsin inhibitorheavy chain 1 after loss of Ga13 in liver exacerbates systemic insulin resistance in mice. Sci.Transl. Med. 11, eaan4735 (2019).
ul N
17 of 17
ational University Library on N
ovember 17, 2019

exacerbates systemic insulin resistance in mice in liver13α-trypsin inhibitor heavy chain 1 after loss of GαOverproduction of inter-
Cheol Soo Choi, Jung Weon Lee, Won Kim, Je-Yoel Cho and Sang Geon KimTae Hyun Kim, Ja Hyun Koo, Mi Jeong Heo, Chang Yeob Han, Yong-In Kim, Shi-Young Park, Il Je Cho, Chang Ho Lee,
DOI: 10.1126/scitranslmed.aan4735, eaan4735.11Sci Transl Med
a new strategy to treat metabolic diseases.developingsystemic insulin resistance and ameliorated glucose intolerance in mice. This finding may contribute to
muscle, making a physical barrier between insulin and its receptor. Neutralization of secreted ITIH1 preventedmodification of ITIH1 facilitated its deposition on the hyaluronan surrounding mouse adipose tissue and skeletal (ITIH1) highly secreted by liver in association with insulin resistance and consequent hyperglycemia. Glycosylin the liver of mice and humans with diabetes. Secretome analysis enabled identification of a specific protein
13α report a decrease in Get al.The liver releases secretory proteins in response to metabolic stress. Kim Targeting ITIH1 in metabolic disease
ARTICLE TOOLS http://stm.sciencemag.org/content/11/513/eaan4735
MATERIALSSUPPLEMENTARY http://stm.sciencemag.org/content/suppl/2019/10/07/11.513.eaan4735.DC1
CONTENTRELATED
http://stm.sciencemag.org/content/scitransmed/10/455/eaah6324.fullhttp://stm.sciencemag.org/content/scitransmed/10/467/eaat4271.fullhttp://stm.sciencemag.org/content/scitransmed/10/472/eaat3392.fullhttp://stm.sciencemag.org/content/scitransmed/11/489/eaav0120.fullhttp://stm.sciencemag.org/content/scitransmed/11/496/eaav1892.fullhttp://stm.sciencemag.org/content/scitransmed/11/510/eaav5055.full
REFERENCES
http://stm.sciencemag.org/content/11/513/eaan4735#BIBLThis article cites 51 articles, 18 of which you can access for free
PERMISSIONS http://www.sciencemag.org/help/reprints-and-permissions
Terms of ServiceUse of this article is subject to the
registered trademark of AAAS. is aScience Translational MedicineScience, 1200 New York Avenue NW, Washington, DC 20005. The title
(ISSN 1946-6242) is published by the American Association for the Advancement ofScience Translational Medicine
of Science. No claim to original U.S. Government WorksCopyright © 2019 The Authors, some rights reserved; exclusive licensee American Association for the Advancement
at Seoul N
ational University Library on N
ovember 17, 2019
http://stm.sciencem
ag.org/D
ownloaded from