Myasthenia Gravis
description
Transcript of Myasthenia Gravis

Myasthenia Gravis
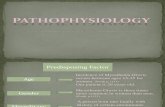
Myasthenia gravis occurs at all ages, sometimes in association with a thymic tumor orthyrotoxicosis, as well as in rheumatoid arthritis and lupus erythematosus. It is commonest inyoung women with HLA-DR3; if thymoma is associated, older men are more commonly affected.Onset is usually insidious, but the disorder is sometimes unmasked by a coincidental infection thatleads to exacerbation of symptoms. Exacerbations may also occur before the menstrual period andduring or shortly after pregnancy. Symptoms are due to a variable degree of block ofneuromuscular transmission caused by autoantibodies binding to acetylcholine receptors; these arefound in most patients with the disease and have a primary role in reducing the number offunctioning acetylcholine receptors. Additionally, cellular immune activity against the receptor isfound. Clinically, this leads to weakness; initially powerful movements fatigue readily. Theexternal ocular muscles and certain other cranial muscles, including the masticatory, facial, andpharyngeal muscles, are especially likely to be affected, and the respiratory and limb muscles mayalso be involved.
Clinical Findings A. Symptoms and Signs: Patients present with ptosis, diplopia, difficulty in chewing orswallowing, respiratory difficulties, limb weakness, or some combination of these problems.Weakness may remain localized to a few muscle groups, especially the ocular muscles, or maybecome generalized. Symptoms often fluctuate in intensity during the day, and this diurnalvariation is superimposed on a tendency to longer-term spontaneous relapses and remissions thatmay last for weeks. Nevertheless, the disorder follows a slowly progressive course and may havea fatal outcome owing to respiratory complications such as aspiration pneumonia.
Clinical examination confirms the weakness and fatigability of affected muscles. In most cases,the extraocular muscles are involved, and this leads to ocular palsies and ptosis, which arecommonly asymmetric. Pupillary responses are normal. The bulbar and limb muscles are oftenweak, but the pattern of involvement is variable. Sustained activity of affected muscles increasesthe weakness, which improves after a brief rest. Sensation is normal, and there are usually noreflex changes.
The diagnosis can generally be confirmed by the response to a short-acting anticholinesterase.Edrophonium can be given intravenously in a dose of 10 mg (1 mL), 2 mg being given initially andthe remaining 8 mg about 30 seconds later if the test dose is well tolerated; in myasthenic patients,there is an obvious improvement in strength of weak muscles lasting for about 5 minutes.Alternatively, 1.5 mg of neostigmine can be given intramuscularly, and the response then lasts forabout 2 hours; atropine sulfate (0.6 mg) should be available to reverse muscarinic side effects.
B. Imaging: Lateral and anteroposterior x-rays of the chest and CT scans should be obtained todemonstrate a coexisting thymoma, but normal studies do not exclude this possibility.
C. Laboratory and Other Studies: Electrophysiologic demonstration of a decrementing muscleresponse to repetitive 2- or 3-Hz stimulation of motor nerves indicates a disturbance ofneuromuscular transmission. Such an abnormality may even be detected in clinically strong

muscles with certain provocative procedures. Needle electromyography of affected musclesshows a marked variation in configuration and size of individual motor unit potentials, andsingle-fiber electromyography reveals an increased jitter, or variability, in the time intervalbetween two muscle fiber action potentials from the same motor unit.
Assay of serum for elevated levels of circulating acetylcholine receptor antibodies is anotherapproach—increasingly used—to the laboratory diagnosis of myasthenia gravis and has asensitivity of 80–90%.
TreatmentMedication such as aminoglycosides that may exacerbate myasthenia gravis should be avoided.Anticholinesterase drugs provide symptomatic benefit without influencing the course of thedisease. Neostigmine, pyridostigmine, or both can be used, the dose being determined on anindividual basis. The usual dose of neostigmine is 7.5–30 mg (average, 15 mg) taken four timesdaily; of pyridostigmine, 30–180 mg (average, 60 mg) four times daily. Overmedication maytemporarily increase weakness, which is then unaffected or enhanced by intravenousedrophonium.
Thymectomy usually leads to symptomatic benefit or remission and should be considered in allpatients younger than age 60, unless weakness is restricted to the extraocular muscles. If thedisease is of recent onset and only slowly progressive, operation is sometimes delayed for a yearor so, in the hope that spontaneous remission will occur.Treatment with corticosteroids is indicated for patients who have responded poorly toanticholinesterase drugs and have already undergone thymectomy. It is introduced with the patientin the hospital, since weakness may initially be aggravated. Once weakness has stabilized after 2–3weeks or any improvement is sustained, further management can be on an outpatient basis.Alternate-day treatment is usually well tolerated, but if weakness is enhanced on the nontreatmentday it may be necessary for medication to be taken daily. The dose of corticosteroids isdetermined on an individual basis, but an initial high daily dose (eg, prednisone, 60–100 mg) cangradually be tapered to a relatively low maintenance level as improvement occurs; totalwithdrawal is difficult, however. Treatment with azathioprine may also be effective. The usualdose is 2–3 mg/kg orally daily after a lower initial dose.
In patients with major disability in whom conventional treatment is either unhelpful orcontraindicated, plasmapheresis or intravenous immunoglobulin therapy may be beneficial. It mayalso be useful for stabilizing patients before thymectomy and for managing acute crisis.