Microbiology of periodontal diseases 1
-
Upload
ashish-bisane -
Category
Documents
-
view
2.999 -
download
7
Transcript of Microbiology of periodontal diseases 1

1
GOOD MORNING

2
MICROBIOLOGY OF PERIODONTAL DISEASES
Presented by
Dr Ashish Bisane
Post Graduate Student
Dept. of Periodontics
Swargiya Dadasaheb Kalmegh Smruti Dental College and Hospital, Nagpur.

3
Introduction• The colonization of the oral cavity also starts close to the
time of birth.
• Within hours after birth, the sterile oral cavity will be
colonized by low numbers of mainly facultative and aerobic
bacteria.
• It is estimated that more than 700 different species are
capable of colonizing the adult mouth and that any
individual typically harbours 150 or more different species.
(Moore WE, 1994)
• Most oral bacteria are harmless commensals under normal
circumstances.

4
Bacterial Classification
• Based on Morphology : Cocci, Bacilli, Spirochetes
• Based on Staining Characteristics• Based on Culturing Characteristics (Aerobes,
Facultative anaerobes, Microaerophiles, Obligate Anaerobes /Anaerobes)

5
Bacterial Classification Based On Shape

6
Gram +ve (Purple/Blue)
Cocci
Catalase +ve (clusters)
Staph.
Coagulase +ve
E.g. S. aureus
Coagulase –ve
E.g. S.epidermis
Catalase –ve
(chains)
Strepto.
Alpha Hemolysis (Green Colonies)
Capsule /Quelling +ve
Optochin Sensitive
e.g. S. Pneumoniae
No capsule, Optochin resistant.
e.g. S. viridans
Beta Hemolysis
(Clear Colonies)
20 Lancefield Groups
Bacitracin Sensitive
E.g. S.pyogenes
Bacitracin Resistant
E.g. S, Agalactiae
No Hemolysis
Enterococci
BacilliE.g.: Clostridium, Corneybacterium

Gram – ve
Pink
Cocci
Maltose fermenter
E.g. N.meningtides
Maltose Non-Fermenter
E.g. N.gonorrhea
Coccobacilli
E.g. H.influenzaBacilli
Lactose Fermenter
E.g. Klebsiella, E.coli
Lactose Non-Fermenters
Oxidase +ve
E.g. Pseudomonas
Oxidase –ve
E.g. Salmonella, Shigella
7

9
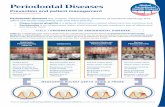
Similarity between Periodontal Diseases and Other Infectious
Diseases• Individuals may be colonized continuously by
periodontal pathogens at or below the gingival margin and yet not show evidence of ongoing or previous periodontal destruction.
• In spite of the presence of periodontal pathogens, periodontal tissue damage does not take place.
• This phenomenon is consistent with other infectious diseases in which it may be observed that a pathogen is necessary but not sufficient for a disease to occur.

10
Unique Features of Periodontal Infection
• The major reason for this uniqueness is the unusual anatomic feature that a mineralized structure, the tooth passes through the integument, so that part of it is exposed to the external environment while part is within the connective tissues.
• The tooth provides a surface for the colonization of a diverse array of bacterial species.
• Bacteria may attach to the tooth itself, to the epithelial surfaces of the gingiva or periodontal pocket, to underlying connective tissues, if exposed, and to other bacteria which are attached to these surfaces.
• Thus, a situation is set up in which microorganisms colonize a relatively stable surface, the tooth and are continually held in immediate proximity to the soft tissues of the periodontium.

11
• The organisms that cause periodontal diseases reside in biofilms that exist on tooth or epithelial surfaces.
• The biofilm provides a protective environment for the colonizing organisms and fosters metabolic properties that would not be possible if the species existed in a free-living (planktonic) state.

12
• Dynamic Equilibrium:
(1) Swallowing, Mastication, Or Blowing The Nose
(2) Tongue And Oral Hygiene Implements
(3) The Wash-out Effect Of The Salivary, Nasal, And Crevicular Fluid Outflow
(4) Active Motion Of The Cilia (Nasal And Sinus Walls).
• Most organisms can only survive in the oropharynx when they adhere to either the soft tissues or the hard surfaces (teeth, dentures, and implants).

13
• Several different types of surfaces are available for bacterial adhesion: soft tissues, such as mucosae, skin, and cornea, and hard tissues, such as teeth and nails.
• On the basis of physical and morphologic criteria, the oral cavity can be divided into six major ecosystems (also called niches), each with the following distinct ecologic determinants:
1. The intraoral, supragingival, hard surfaces (teeth, implants, restorations, and prostheses)
2. Subgingival regions adjacent to a hard surface, including the periodontal/peri-implant pocket (with its crevicular fluid, the root cementum or implant surface, and the pocket epithelium)
3. The buccal, palatal epithelium, and the epithelium of the floor of the mouth
4. The dorsum of the tongue
5. The tonsils
6. The saliva

15
Historical Perspective• Investigators in the period from 1880–1930
suggested four distinct groups of microorganisms as possible etiologic agents; amoeba, spirochetes, fusiforms, and streptococci.
• The basis of this determination was primarily the seeming association of these organisms with periodontal lesions.
• The major techniques : wet mount or stained smear microscopy and limited cultural techniques.

16
Amoeba
• They found higher proportions of amoeba in lesions of destructive periodontal diseases than in samples taken from sites in healthy mouths or mouths with gingivitis.
• Treatment was done using systemic or local Emitin and/or Emitic.
• The role of amoeba in periodontal disease was questioned by some authors because amoeba were found in sites with minimal or no disease and could not be detected in many sites with destructive disease and because of the failure of emitin to ameliorate the symptoms of the disease.

17
Spirochetes• Investigators reported higher proportions of spirochetes
and other motile forms in lesions of destructive disease when compared with control sites in the same or other individuals.
• Neosalvarsan (compound 606), the anti-spirochetal agent used to treat syphilis, coupled with the use of subgingival scaling to control destructive periodontal disease.
• Other investigators employed bismuth compounds to treat oral spirochetal infections.

18
Fusiforms• The third group of organisms that were frequently suggested to
be etiologic agents of destructive periodontal diseases, including Vincent’s infection, were the spindle-shaped fusiforms.
• These organisms were originally recognized on the basis of their frequent appearance in microscopic examination of subgingival plaque samples.
• The organisms were first related to periodontal disease by Plaut (1894).
• Vincent (1899) distinguished certain pseudomembranous lesions of the oral cavity and throat from diphtheria and recognized the important role of fusiforms and spirochetes in this disease.
• In honour of this investigator the infection became known as Vincent’s infection.

19
Streptococci
• These microorganisms were proposed on the basis of cultural examination of samples of plaque from subgingival sites of periodontal disease.
• The selection of the streptococci may have been predicated upon the fact these were the only species that could be consistently isolated from periodontitis lesions using the cultural techniques of that era.

21
• Invasion of the periodontal tissues by bacteria, was thought to
be important in the pathogenesis of periodontal diseases in the early 1900s, forgotten and then rediscovered.
• The initial enthusiasm for the hunt for the etiologic agents of destructive periodontal diseases slowly subsided and by the mid 1930s there were virtually no workers involved in this quest.
• This state was eloquently described by Belding and Belding (1936) in the aptly titled “Bacteria – Dental Orphans”.
• In between 1920 to 1940 it was thought that periodontal disease was due to some constitutional defect on the part of the patient, trauma from occlusion, disuse atrophy or some combination of these factors.

22
Non – Specific Plaque Hypothesis• Clinicians recognized that plaque control was essential in the satisfactory
treatment of periodontal patients.
• According to this “nonspecific plaque” hypothesis, any accumulations of microorganisms at or below the gingival margin would produce irritants leading to inflammation.
• The non specific plaque hypothesis maintains that periodontal disease results from the elaboration of noxious products from the entire plaque flora. (Loesche, 1976)
• The inflammation in turn was responsible for the periodontal tissue destruction.
• The specific species of microorganisms that accumulated on the teeth was not considered to be particularly significant, providing that their numbers were sufficiently large to trigger a destructive process.

23
• At first, a direct relationship was often assumed to exist between the total number of accumulated bacteria and the amplitude of the pathogenic effect; biologically relevant differences in the composition of plaque were not usually considered.
• This bacterial mass, termed plaque, was shown to produce a variety of irritants, such as acids, endotoxins, and antigens, which, over time, invariably dissolved teeth and destroyed the supporting tissues.
• Consequently, the need to discriminate among bacterial deposits from different patients or at healthy or diseased sites was not yet recognized in detail.
• Individuals with extensive periodontal disease were either suspected of having a weak resistance to bacterial plaque as a whole or were blamed for inadequate home care.
• Such a view of dental plaque as a biomass is referred to as the non specific plaque hypothesis. (Theilade 1986).

24
Mixed Infections• In the early 1930s, investigators found that mixtures of microorganisms
isolated from lung infections or subgingival plaque would induce lesions when injected subcutaneously into various experimental animals.
• A combination of a fusiforms, a spirochete, an anaerobic vibrio and an alpha haemolytic streptococcus could cause transmissible infections in the guinea pig.
• Macdonald and co-workers (1956) were later able to produce transmissible mixed infections in the guinea pig groin using combinations of pure cultures.
• The critical mixture of four organisms included a Bacteroides melaninogenicus strain, a Gram positive anaerobic rod and two other Gram-negative anaerobic rods.
• These results led to the concept that mixed infections might be “bacteriologically non-specific but biochemically specific”.

25
Return To Specificity In Microbial Etiology
Of Periodontal Diseases• In the 1960s, interest in the specific microbial etiology of periodontal disease
was rekindled.
• It was demonstrated that periodontal disease could be transmitted in the hamster from animals with periodontal disease to animals without periodontal disease by caging them together.
• Swabs of plaque or faeces from diseased animals were effective in transmitting the disease to animals free of disease. It was demonstrated that a pure culture of a Gram-positive pleomorphic rod that later became known as Actinomyces viscosus was capable of causing destructive periodontal disease in animals free of disease.
• Other species isolated from the plaque of hamsters with periodontal disease did
not have this capability.

26
• At about the same time, it was demonstrated that spirochetes with a unique ultra structural morphology could be detected in practically pure culture in the connective tissue underlying lesions of ANUG and within the adjacent epithelium.
• Control tissue taken from healthy individuals and individuals with other forms of disease did not exhibit a similar tissue invasion.
• To date, the spirochete associated with ANUG has not been cultivated.
• Such findings suggested that there might be more specificity to the microbial etiology of periodontal disease than had been accepted for the previous 4decades.
• Human isolates of Actinomyces species were shown to have this ability in vitro and led to plaque formation and periodontal destruction in animal model systems.
• These findings reinforced the notion that organisms that formed abundant plaque were responsible for destructive periodontal disease.

27
From Non-Specific to Specific Plaque Hypothesis
• By the end of the 1960s it was generally accepted that dental plaque was in some way associated with human periodontal disease.
• It was believed that the presence of bacterial plaque initiated a series of as yet undefined events that led to the destruction of the periodontium.
• It was thought that the major event triggering destructive periodontal disease was an increase in mass of bacterial plaque, possibly accompanied by a diminution of host resistance.
• Indeed, in the mid 1960s the classic studies of Loe et al. (1965, 1967) and Theilade et al. (1966) convincingly demonstrated that plaque accumulation directly preceded and initiated gingivitis.

28
• If all plaques were more or less alike and induced a particular tissue response in the host, why was periodontal destruction localized, taking place adjacent to one tooth but not another?
• If plaque mass was a prime trigger for periodontal destruction, why did certain subjects accumulate much plaque, frequently accompanied by gingivitis, but fail, even after many years to develop destruction of the supporting structures?
• On the other hand, why did some individuals with little détectable plaque or clinical inflammation develop rapid periodontal destruction?
• If inflammation was the main mediator of tissue destruction, why were so many teeth retained in the presence of continual gingivitis ?

29
• One explanation may have been that there were inconsistencies in the host response, or disease required the superimposition of local factors such as trauma from occlusion, overhanging fillings etc.
• Newman et al. (1976, 1977) and Slots (1976) demonstrated that the microbial composition of subgingival plaque taken from diseased sites differed substantially from the samples taken from healthy sites in subjects with localized aggressive periodontitis (LAP).
• Tanner et al. (1979) and Slots (1977) demonstrated that the microbiota recovered from lesion sites from subjects with chronic periodontitis differed from the microbiota from healthy sites in the same subjects and also from lesion sites in LAP subjects.
• Such a view of periodontitis being caused by specific pathogens is referred to as the specific plaque hypothesis (Loesche 1979).

30
Biofilm
• The term biofilm describes the relatively indefinable microbial community associated with a tooth surface or any other hard, non-shedding material (Wilderer & Charaklis 1989).
• Biofilms consist of one or more communities of microorganisms, embedded in a glycocalyx, that are attached to a solid surface.
• The biofilm allows microorganisms to stick to and multiply on surfaces.

31
• This method of growth provides a number of advantages to colonizing species.
• A major advantage is the protection that the biofilm provides to colonizing species from competing microorganisms, from environmental factors such as host defence mechanisms, and from potentially toxic substances in the environment, such as lethal chemicals or antibiotics.
• Biofilms also can facilitate processing and uptake of nutrients, cross-feeding (one species providing nutrients for another), removal of potentially harmful metabolic products (often by utilization by other bacteria), as well as the development of an appropriate physicochemical environment (e.g. a properly reduced oxidation reduction potential).

32
• In the lower levels of most biofilms a dense layer of microbes is bound together in a polysaccharide matrix with other organic and inorganic materials.
• On top of this layer is a looser layer, which is often highly irregular in appearance and may extend into the surrounding medium.
• The fluid layer bordering the biofi lm may have a rather “stationary’’ sub layer and a fluid layer in motion.
• Nutrient components may penetrate this fluid medium by molecular diffusion.

33
• Communication between bacterial cells within a biofilm is also necessary for optimum community development and is performed by production of signalling molecules such as those found in “quorum sensing” or perhaps by the exchange of genetic information.
• The long-term survival of the human species as well as a species in a biofi lm becomes more likely if that species (or the human) colonizes multiple sites.
• Thus, detachment of cells from biofilms and establishment in new sites is important for survival of biofi lm dwellers.
• Thus, we may regard mixed species biofilms as primitive precursors to the more complex organizations observed for eukaryotic species.

34
Structure of Biofilm• Biofilms are composed of micro colonies of bacterial cells (15–20% by
volume) that are non-randomly distributed in a shaped matrix or glycocalyx (75–80% by volume).
• The water channels permit the passage of nutrients and other agents throughout the biofi lm acting as a primitive “circulatory” system.
• Nutrients make contact with the sessile (attached) microcolonies by diffusion from the water channel to the microcolony rather than from the matrix.
• Microcolonies occur in different shapes in biofilms which are governed by shear forces due to the passage of fluid over the biofi lm.
• At low shear force, the colonies are shaped liked towers or mushrooms, while at high shear force, the colonies are elongated and capable of rapid oscillation.

35
Exopolysaccharides – The Backbone of Biofilms
• The bulk of the biofi lm consists of the matrix or glycocalyx and is composed predominantly of water and aqueous solutes.
• The “dry” material is a mixture of Exopolysaccharides, proteins, salts, and cell material.
• Exopolysaccharides (EPS), which are produced by the bacteria in the biofilm, are the major components of the biofi lm making up 50–95% of the dry weight.
• They play a major role in maintaining the integrity of the biofi lm as well as preventing desiccation and attack by harmful agents.
• In addition, they may also bind essential nutrients such as cations to create a local nutritionally rich environment favouring specific microorganisms.
• The EPS matrix could also act as a buffer and assist in the retention of extracellular enzymes (and their substrates) enhancing substrate utilization by bacterial cells.
• The EPS can be degraded and utilized by bacteria within the biofi m.• One distinguishing feature of oral biofilms is that many of the
microorganisms can both synthesize and degrade the EPS.

36
• Bacterial cells within biofilms can produce enzymes such as beta-lactamase against antibiotics, catalases, and superoxide dismutases against oxidizing ions released by phagocytes.
• These enzymes are released into the matrix producing an almost impregnable line of defense.
• Bacterial cells in biofilms can also produce elastases and cellulases which become concentrated in the local matrix and produce tissue damage.

37
Quorum Sensing and Exchange of Genetic Information
• Quorum sensing in bacteria “involves the regulation of expression of specific genes through the accumulation of signalling compounds that mediate intercellular communication” (Prosser 1999).
• Quorum sensing is dependent on cell density.• Once the signalling compounds reach a threshold level
(quorum cell density), gene expression is activated. • Quorum sensing may give biofilms their distinct properties.• For example, expression of genes for antibiotic resistance at
high cell densities may provide protection Or influence community structure by encouraging the growth of beneficial species (to the biofilm) and discouraging the growth of competitors.

39
• The high density of bacterial cells growing in biofilms facilitates exchange of genetic information between cells of the same species and across species or even genera.
• Conjugation, transformation, plasmid transfer, and transposon transfer have all been shown to occur in naturally occurring or in vitro prepared mixed species biofilms.

40
Attachment of Bacteria
• The key characteristic of a biofilm is that the microcolonies within the biofilm attach to a solid surface.
• In the mouth, there is a wide variety of surfaces to which bacteria can attach including the oral soft tissues, the pellicle coated teeth, other bacteria, as well as prosthetic replacements such dentures and implants.
• Many bacterial species possess surface structures such as fimbriae and fibrils that aid in their attachment to different surfaces.
• Fimbriae have been detected on a number of oral species including Actinomyces naeslundii, P. gingivalis, A. actinomycetemcomitans and some strains of streptococci such as Streptococcus salivarius, Streptococcus parasanguinis, and members of the Streptococcus mitis group.

41
Dental Plaque• Dental Plaque is defined clinically as a structured, resilient,
yellow-grayish substance that adheres tenaciously to the intraoral hard surfaces, including removable and fixed restorations. (W H Bowen, 1976)
• Dental plaque may accumulate supragingivally, i.e. on the clinical crown of the tooth, but also below the gingival margin, i.e. in the subgingival area of the sulcus or pocket.
• Differences in the composition of the subgingival microbiota have been attributed in part to the local availability of blood products, pocket depth, redox potential, and pO2.
• Supragingival plaque typically demonstrates a stratified organization of a multilayered accumulation of bacterial morphotypes.
• Gram-positive cocci and short rods predominate at the tooth surface, whereas gram-negative rods and filaments, as well as spirochetes, predominate in the outer surface of the plaque mass.

42

43
• In the tooth-associated cervical plaque, filamentous microorganisms dominate, but cocci and rods also occur.
• This plaque is dominated by gram-positive rods and cocci, including S. mitis, S. sanguinis, Actinomyces oris (a new species containing strains that were formerly classified as A. naeslundii), A. naeslundii, and Eubacterium spp.
• However, in the deeper parts of the pocket, the filamentous organisms become fewer in numbers, and in the apical portion they seem to be virtually absent.
• Instead, the microbiota is dominated by smaller organisms without a particular orientation.
• The apical border of the plaque mass is separated from the junctional epithelium by a layer of host leukocytes, and the bacterial population of this apical tooth associated region shows an increased concentration of gram-negative rods.

44
• The layers of microorganisms facing the soft tissue lack a definite inter-microbial matrix and contain primarily gram-negative rods and cocci, as well as large numbers of filaments, flagellated rods, and spirochetes.
• Studies on plaque associated with crevicular epithelial cells indicate a predominance of species such as S. oralis, S.intermedius, Parvimonas micra (formerly Micromonas micra and Peptostreptococcus micros), P. gingivalis, Prevotella intermedia, Tannerella forsythia and F. nucleatum.(S Dibart,1998)
• Host tissue cells (e.g. white blood cells and epithelial cells) may also be found in this region.
• Bacteria are also found within the host tissues, such as in the soft tissues and within epithelial cells. as well as in the dentinal tubules. (F R Saglie, 1982,1988)
• The composition of the subgingival plaque depends on the pocket depth. The apical part is more dominated by spirochetes, cocci and rods, whereas in the coronal part more filaments are observed.

45
Dental Plaque as a Biofilm
• Dental plaque has structure similar to biofilms.• It is heterogeneous in structure with open fluid filled channels running
through plaque mass.• These water channels permit the passage of nutrients and other agents
throughout the biofilm.• The bacteria exist and proliferate within the intercellular matrix
through which these water channels run.• In the lower levels, a dense layer of microbes is bound together in a
polysaccharide matrix with other organic and inorganic materials.• On top of this layer is a looser layer, which is often highly irregular in
appearance and may extend into the surrounding medium. • The fluid layer bordering the biofilm may have a rather “stationary’’
sub layer and a fluid layer in motion.

46
• Immediately upon immersion of a solid substratum into the fluid media of the oral cavity, or upon cleaning of a solid surface in the mouth, hydrophobic and macromolecules begin to adsorb to the surface to form a conditioning film termed the acquired pellicle.
• This film is composed of a variety of salivary glycoproteins (mucins) and antibodies.
• The conditioning fi lm alters the charge and free energy of the surface, which in turn increases the efficiency of bacterial adhesion. Bacteria adhere variably to these coated surfaces.

47
Inter-Cellular Matrix• It consists of organic and inorganic materials derived from
saliva, GCF and bacterial products.
• Organic components: Polysaccharides (Mainly Dextran) Proteins Glycoproteins Lipid material (from debris of membranes of disrupted
bacterial and host cell membranes)
• Inorganic components: Calcium Phosphorus Traces of sodium, potassium and fluoride

50
Formation of Plaque

51
Phase – I
• Immediately upon immersion of a solid substratum into the fluid media of the oral cavity, or upon cleaning of a solid surface in the mouth, hydrophobic and macromolecules begin to adsorb to the surface to form a conditioning film termed the acquired pellicle.
• This film is composed of a variety of salivary glycoproteins (mucins) and antibodies.
• The conditioning film alters the charge and free energy of the surface, which in turn increases the efficiency of bacterial adhesion.

52
Phase – II
• Bacteria adhere variably to these coated surfaces.
• Some possess specific attachment structures such as extracellular polymeric substances and fimbriae, which enable them to attach rapidly upon contact.
• Other bacteria require prolonged exposure to bind firmly.

53
Phase – III
• Behaviour of bacteria change once they become attached to surfaces.
• This includes active cellular growth of previously starving bacteria and synthesis of new outer membrane components.

54
Phase – IV
• The bacterial mass increases due to continued growth of the adhering organisms, adhesion of new bacteria, and synthesis of extracellular polymers.
• An oxygen gradient develops as a result of rapid utilization by the superficial bacterial layers and poor diffusion of oxygen through the biofi lm matrix.
• Completely anaerobic conditions eventually emerge in the deeper layers of the deposits.

55
Colonization and Plaque Maturation
• When the firmly attached micro-organisms start growing and the newly formed bacterial clusters remain attached, microcolonies or a biofilm can develop.
• Here onwards bacteria exhibit the phenomena of Coaggregation (cell to cell recognition of genetically distinct partner cell types) (Kolenbrander 1993)

56

57
Primary Colonizers
1. Streptococcus gordonii2. Streptococcus intermedius3. Streptococcus mitis4. Streptococcus oralis5. Streptococcus sanguinis6. Actinomyces gerencseria7. Actinomyces israelii8. Actinomyces naeslundii9. Actinomyces oris10.Aggregatibacter actinomycetemcomitans serotype a11. Capnocytophaga gingivalis12.Capnocytophaga ochracea13.Capnocytophaga sputigena14.Eik enella corrodens15.Actinomyces odontolyticus16.Veillonella parvula

58
SecondaryColonizers
1. Campylobacter gracilis2. Campylobacter rectus3. Campylobacter showae4. Eubacterium nodatum5. Aggregatibacter actinomycetemcomitans
serotype b6. Fusobacterium nucleatum ssp nucleatum7. Fusobacterium nucleatum ssp vincentii8. Fusobacterium nucleatum ssp polymorphum9. Fusobacterium periodonticum10. Parvimonas micra11. Prevotella intermedia12. Prevotella loescheii13. Prevotella nigrescens14. Streptococcus constellatus15. Tannerella forsythia16. Porphyromonas gingivalis17. Treponema denticola

59
Coaggregation• Coaggregation is a direct interaction and is distinct from agglutination,
which occurs when cells are stuck together by molecules in solution. • At least 18 genera from the oral cavity have shown some form of
Coaggregation.(P E Kolenbrander, 1993)• All oral bacteria possess surface molecules that foster some sort of cell-
cell interaction.• The initial stages of coaggregation or co adhesion are essentially the same
as the first steps involved in bacterial binding to surfaces: bacterial cells come into contact through passive or active transport and bind weakly through nonspecific hydrophobic, electrostatic, and Vander Waals forces.
• Strong cell-cell binding is then determined by the presence of adhesin proteins or carbohydrates on one partner and complementary receptor proteins or carbohydrates on the other.
• Many coaggregations between strains of different genera are mediated by lectin-like adhesins (proteins that recognize carbohydrates) and can be inhibited by lactose and other galactosides.

60
• Fusobacteria coaggregate with all other human oral bacteria.
• Veillonella spp., Capnocytophaga spp. and Prevotella spp. bind to streptococci and/or Actinomyces.
• F. nucleatum with S. sanguinis• Prevotella loescheii with A. oris• Capnocytophaga ochracea with A. oris
• In some instances, coaggregation between non-coaggregating species may be mediated by cellularconstituents (e.g. vesicles) of a third species (Ellen & Grove 1989; Grenier & Mayrand 1987b).
• In certain instances more than one type of adhesin–receptor interaction has been detected between a species pair.

61
Adhesins
• Some of the adhesins that havebeen identifi ed on subgingival species include
1. Fimbriae (cisar et al. 1984; clark et al. 1986; sandberg et al. 1986, 1988; isogai et al. 1988)
2. Cell-associated proteins (murray et al. 1986, 1988; mangan et al. 1989; weinberg & Holt 1990).
• Receptors on tissue surfaces include
1. Galactosyl residues (cisar et al. 1984; murray et al. 1988; sandberg et al. 1988; mangan et al. 1989),
2. Sialic acid residues (murray et al. 1986),
3. Proline-rich proteins or statherin (clark et al. 1986),
4. Type I or IV collagens (Naito & Gibbons 1988; Winkler et al. 1988).

63

64
Supragingival Plaque
• During the first 24 hours starting from a clean tooth surface, plaque growth is negligible from a clinical viewpoint.
• During the following 3 days, coverage progresses rapidly to the point where, after 4 days, on average 30% of the total coronal tooth area will be covered with plaque.
• In parts of the plaque with the presence of Gram-negative organisms, the inter microbial matrix is regularly characterized by the presence of small vesicles surrounded by a trilaminar membrane, which is similar in structure to that of the outer envelope of the cell wall of the Gram-negative microorganisms .
• Such vesicles probably contain endotoxins and proteolytic enzymes, and may also be involved in adherence between bacteria (Hofstad et al. 1972; Grenier & Mayrand 1987).

65
Subgingival Plaque
• Between subgingival plaque and the tooth an electron- dense organic material is interposed, termed a cuticle.
• This cuticle probably contains the remains of the epithelial attachment lamina originally connecting the junctional epithelium to the tooth, with the addition of material deposited fromthe gingival exudate (Frank & Cimasoni 1970; Lie &
• Selvig 1975; Eide et al. 1983). It has also been suggested• that the cuticle represents a secretory product• of the adjacent epithelial cells (Schroeder & Listgarten• 1977).

66
• The subgingival plaque structurally resembles supragingival plaque, particularly with respect to plaque associated with gingivitis without the formation of deep pockets.
• A densely packed accumulation of microorganisms is seen adjacent to the cuticular material covering the tooth surface.
• The bacteria comprise Gram-positive and Gram-negative cocci, rods, and filamentous organisms.
• Spirochetes and various flagellated bacteria may also be encountered, especially at the apical extension of the plaque.
• The surface layer is often less densely packed and leukocytes are regularly interposed between the plaque and the epithelial lining of the gingival sulcus.
• However, in the deeper parts of the periodontal pocket, the filamentous organisms become fewer in number, and in the apical portion they seem to be virtually absent.
• Instead, the dense, tooth-facing part of the bacterial deposit is dominated by smaller organisms without particular orientation (Listgarten 1976)

67
• The surface layers of microorganisms in the periodontal pocket facing the soft tissue are distinctly different from the adherent layer along the tooth surface, and no definite inter microbial matrix is apparent.
• The microorganisms comprise a larger number of spirochetes and flagellated bacteria. Gram-negative cocci and rods are also present.
• The multitude of spirochetes and flagellated organisms are motile bacteria and there is no inter microbial matrix between them.
• This outer part of the microbial accumulation in the periodontal pocket adheres loosely to the soft-tissue pocket wall (Listgarten 1976).
• Subgingivally located bacteria appear to have the capacity to invade dentinal tubules, the openings of which have become exposed as a consequence of inflammatory driven resorptions of the cementum (Adriaens et al. 1988). Such a habitat might serve as the source for bacterial recolonization of the subgingival space following treatment of periodontal disease.
• The mechanisms involved in such reversed invasion of the subgingival space are unknown.

68
Thank You !!!