Management of sepsis
-
Upload
ankur-gupta -
Category
Health & Medicine
-
view
1.071 -
download
1
description
Transcript of Management of sepsis

MANAGEMENT OF SEPSIS AND SEPTIC SHOCK
Dr. Ankur Gupta

INTRODUCTION• Rapid diagnosis (within the first 6 hours) and
expeditious treatment are critical, since early, goal directed therapy can be very effective.
• Multiple approaches are necessary in the treatment of sepsis and shock.
• It is important to select patients for each given therapy with great care, because the efficacy of treatment — as well as the likelihood and type of adverse results — will vary, depending on the patient.

EPIDEMIOLOGY
• Major cause of morbidity and mortality worldwide.
• Sepsis ranks in the top 10 causes of death.• Mortality in Septic Shock ranges from 40 to
60% .• Mortality rate is proportional to the number
of organ systems that fail.• Less defined in developing countries.

EPIDEMIOLOGY
• Increasing incidence of severe sepsis in the USA is attributable to the aging of the population, the increasing longevity of patients with chronic diseases, and the relatively high frequency with which sepsis develops in patients with AIDS.
• Widespread use of antimicrobial agents, glucocorticoids, indwelling catheters and mechanical devices, and mechanical ventilation also plays a role.

DEFINITIONS
• Bacteremia - Presence of bacteria in blood, as evidenced by positive blood cultures.
• Septicemia - Presence of microbes or their toxins in blood.
• Systemic Inflammatory Response syndrome(SIRS) - Two or more of the following conditions: – (1) fever (oral temperature >38C) or hypothermia (<36C);– (2) tachypnea (>24 breaths/min);– (3) tachycardia (heart rate > 90 beats/min); – (4) leukocytosis (>12,000/L), leukopenia (<4,000/L), or 10%
bands; may have a noninfectious etiology

• Sepsis - SIRS that has a proven or suspected microbial etiology.
• Severe sepsis (similar to“sepsis syndrome”) Sepsis with one or more signs of organ dysfunction—for example:
1. Cardiovascular: Arterial systolic blood pressure ≤ 90 mmHg or mean arterial pressure ≤ 70 mmHg that responds to administration of intravenous fluid2. Renal: Urine output < 0.5 mL/kg per hour for 1 h despite adequate fluid resuscitation

• 3. Respiratory: PaO₂ /FIO₂ ≤ 250 or, if the lung is the only dysfunctional organ, ≤ 200
• 4. Hematologic: Platelet count < 80,000/L or 50% decrease in platelet count from highest value recorded over previous 3 days
• 5. Unexplained metabolic acidosis: A pH ≤ 7.30 or a base deficit ≥ 5.0 mEq/L and a plasma lactate level > 1.5 times upper limit of normal for reporting lab.

Septic shock - Sepsis with hypotension (arterial blood pressure < 90 mmHg systolic, or 40 mmHg less than patient’s normal blood pressure) for at least 1 h despite adequate fluid resuscitation;Or Need for vasopressors to maintain systolic blood pressure ≥ 90 mmHg or mean arterial pressure ≥ 70 mmHg

• Refractory septic shock - Septic shock that lasts for 1 h and does not respond to fluid or pressor administration
• Multiple-organ Dysfunction Syndrome (MODS) Dysfunction of more than one organ, requiring intervention to maintain homeostasis


Inflammatory response of sepsis

Proinflammatory response in sepsis



Diagnostic criteria - SSCG

Diagnostic criteria - SSCG

Diagnostic criteria - SSCG

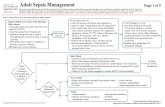
MANAGEMENT
• cornerstone of emergency management of sepsis is early, goal-directed therapy, plus lung-protective ventilation, broad-spectrum antibiotics.

Early, Goal-directed Therapy
• decreased mortality at 28 and 60 days as well as the duration of hospitalization.
• mechanisms of the benefit of EGDT are unknown but may include reversal of tissue hypoxia and a decrease in inflammation and coagulation defects.

EGDT – River`s trial
• Crystalloids were administered to maintain CVP at 8 to 12 mm Hg.
• Vasopressors were added if the MAP was less than 65 mm Hg.
• If central venous oxygen saturation was less than 70%, erythrocytes were transfused to maintain a hematocrit of more than 30%.
• Dobutamine was added if the CVP, MAP, and hematocrit were optimized yet venous oxygen saturation remained below 70%.

Surviving Sepsis Campaign: International guidelines - SSC
• Initial resuscitation (first 6 hrs) – hypotension or elevated serum lactate 4 mmol/L. Resuscitate using crystalloids or colloids
• Resuscitation goals – CVP 8–12 mm Hg– Mean arterial pressure ≥ 65 mm Hg.– Urine output ≥ 0.5 mL/kg/hr.– Central venous (superior vena cava) oxygen
saturation ≥ 70% or mixed venous ≥ 65%.

Vasopressors - SSCG
• Maintain MAP > 65 mm Hg.• Norepinephrine and dopamine centrally
administered are the initial vasopressors of choice.
• Use epinephrine as the first alternative agent.• Do not use low-dose dopamine for renal
protection

VASOPRESSIN• I.V. infusion of low-dose vasopressin (0.03 to
0.04 U per minute) has been reported to increase BP, urinary output, and creatinine clearance, permitting a dramatic decrease in vasopressor therapy.
• Side effects – – intestinal ischemia, – decreased cardiac output, – skin necrosis, – cardiac arrest

VENTILATION
• lung-protective ventilation (TV of 6 ml/kg or as low as 4 ml if the plateau pressure exceeds 30 cm H2O) decreases mortality and is beneficial in septic acute lung injury.
• Advantages – – decrease the mortality rate (from 40 to 31%),– lessen organ dysfunction, – lower levels of cytokines.
• PEEP – no significant difference in mortality

VENTILATION
• Patients receiving ventilation require appropriate but not excessive sedation.
• Titrating sedation and interrupting sedation daily until patients are awake decrease the risks associated with sedation.
• Neuromuscular blocking agents should be avoided.

SSCG
• Diagnosis - Obtain appropriate cultures before starting antibiotics.– Obtain two or more BCs – One or more BCs should be percutaneous – One BC from each vascular access device in place
> 48 hrs .– Culture other sites as clinically indicated

ANTIBIOTICS - SSCG
• Begin intravenous antibiotics as early as possible and always within the first hour of recognizing severe sepsis and septic shock.
• Reassess antimicrobial regimen daily to optimize efficacy, prevent resistance, avoid toxicity, and minimize costs.

ANTIBIOTICS
• Immunocompetent adult – – ceftriaxone (2 g q24h) or ticarcillin-clavulanate
(3.1 g q4–6h) or piperacillin-tazobactam (3.375 g q4–6h).
– imipenem-cilastatin (0.5 g q6h) or meropene (1 g q8h) or cefepime (2 g q12h).
– Gentamicin or tobramycin (5–7 mg/kg q24h).– Ciprofloxacin (400 mg q12h) or levofloxacin (500–
750 mg q12h) plus clindamycin (600 mg q8h).

ANTIBIOTICS
• Neutropenia (500 neutrophils/L) – – imipenem-cilastatin (0.5 g q6h) or meropenem (1
g q8h) or cefepime (2 g q8h).– ticarcillin-clavulanate (3.1 g q4h) or piperacillin-
tazobactam (3.375 g q4h) plus tobramycin (5–7 mg/kg q24h).

• Splenectomy – – Cefotaxime (2 g q6–8h) or ceftriaxone (2 g q12h).– vancomycin (15 mg/kg q12h) plus ciprofloxacin
(400 mg q12h) or levofloxacin (750 mg q12h) or aztreonam (2 g q8h).
• AIDS – – Cefepime (2 g q8h), ticarcillin-clavulanate (3.1 g
q4h), or piperacillin tazobactam (3.375 g q4h) plus tobramycin (5–7 mg/kg q24h).
– ciprofloxacin (400 mg q12h) or levofloxacin (750 mg q12h) plus vancomycin (15 mg/kg q12h) plus tobramycin

ACTIVATED PROTEIN C
• Therapy with APC (24 μg / kg / hr for 96 hours) has been reported to decrease mortality and to ameliorate organ dysfunction in patients with severe sepsis.
• Approved for administration to patients with severe sepsis and an increased risk of death.
• Absolute decrease in the mortality rate of 13%.

ACTIVATED PROTEIN C
• Contraindications – PROWESS trial– Recent trauma or surgery (within 12 hours), – Active hemorrhage, – Concurrent therapeutic anticoagulation,– Thrombocytopenia (defined as a platelet count of
less than 30,000 per cubic millimeter), – Recent stroke

ACTIVATED PROTEIN C
• Mechanism of action – – increase protein C. – decrease markers of thrombin generation.– prevents hypotension.

ANEMIA IN SEPSIS
• Mediators of sepsis (TNF-α and interleukin-1β) decrease the expression of the erythropoietin gene and protein.
• Rivers et al. used a hematocrit of 30% and Hebert et al. compared hemoglobin values of 70 and 100 g per liter as a threshold for transfusion.
• SSCG - Give RBC`s when Hb decreases to 7.0 g/dL (70 g/L) to target a Hb of 7.0–9.0 g/dL in adults .

STEROIDS• SSCG – – Consider i.v. hydrocortisone for adult septic shock
when hypotension responds poorly to adequate fluid resuscitation and vasopressors.
– Hydrocortisone is preferred to dexamethasone. – Hydrocortisone dose should be 300 mg/day .– Do not use corticosteroids to treat sepsis in the
absence of shock

STEROIDS
• Important adverse effects in patients with sepsis – – Neuromyopathy – Hyperglycemia, – Decreased numbers of lymphocytes, – Immunosuppression (leading to nosocomial
infection and impaired wound healing ), – Loss of intestinal epithelial cells.

HYPERGLYCEMIA AND INTENSIVE INSULIN THERAPY
• Hyperglycemia - acts as a procoagulant, induces apoptosis, impairs neutrophil function, increases the risk of infection, impairs wound healing.
• Insulin - control hyperglycemia and improve lipid levels , has anti inflammatory, anticoagulant, and anti apoptotic actions.

HYPERGLYCEMIA AND INTENSIVE INSULIN THERAPY
• The appropriate target glucose range and insulin dose in patients with sepsis are unknown.
• SSCG - Aim to keep blood glucose 150 mg/dL (8.3 mmol/L).
• Although intensive insulin therapy appears to be beneficial in surgical patients, the lack of efficacy in medical patients, indicates clinical equipoise and the need for a randomized, controlled trial in patients with Sepsis.

RENAL DYSFUNCTION AND DIALYSIS
• ARF is associated with increased morbidity, mortality. • Continuous renal-replacement therapy decreases the
incidence of adverse biomarkers, but there is little evidence that it changes outcomes.
• Low-dose dopamine (2 to 4 μg / kg / min) neither decreases the need for renal support nor improves survival and, consequently, is not recommended.
• Lactic acidosis is a common complication of septic shock; however, sodium bicarbonate improves neither hemodynamics nor the response to vasopressor medications.

Deep vein thrombosis prophylaxis - SSCG
• Use either low-dose UFH or LMWH, unless contraindicated .
• Use a mechanical prophylactic device, such as compression stockings or an intermittent compression device, when heparin is contraindicated.

Stress ulcer prophylaxis - SSCG
• Provide stress ulcer prophylaxis using H2 blocker or proton pump inhibitor.

NUTRITION
• Enteral nutrition is important because it is generally safer and more effective than total parenteral Nutrition.
• However, total parenteral nutrition may be required in patients who have had abdominal sepsis, surgery, or trauma.

INEFFECTIVE THERAPIES
• Anti lipopolysaccharide therapy was ineffective.
• Therapies that block proinflammatory cytokines have failed.
• Excessively immunosuppressive , Ibuprofen, platelet-activating factor acetylhydrolase, bradykinin antagonists, and other therapies have not improved survival among patients with sepsis.

POTENTIAL NEW THERAPIES• Interferon gamma improved macrophage function and
increased survival in one study.• Inhibition of apoptosis (e.g., with anticaspases)
improved survival in an animal model.• Lipid emulsion (which binds and neutralizes
lipopolysaccharide) is being evaluated in a phase 3 trial.
• Superantigens and mannose.• Inhibition of tissue factor, a proximal target, might
mitigate excessive procoagulant activity.• Strategies to boost immunity could improve the
outcome of sepsis when applied early in sepsis

PROGNOSIS
• Approximately 20 to 35% of patients with severe sepsis and 40 to 60% of patients with septic shock die within 30 days.
• Septic shock is also a strong predictor of short- and long-term mortality.
• Case-fatality rates are similar for culture-positive and culture-negative severe sepsis.

SUMMARY
• Optimal management of sepsis requires early, goal directed therapy; lung-protective ventilation; antibiotics; and possibly activated protein C.
• corticosteroids, vasopressin, and intensive insulin therapy requires further study.
• Later in the course of sepsis, appropriate management necessitates organ support and prevention of nosocomial infection.
• Studies focused on novel targets, mechanisms of action, and combination therapy may improve current treatment.

SEPSIS BUNDLE
• Sepsis resuscitation bundle – (within 6 hrs )– Measure s.lactate.– Obtain blood culture prior starting antibiotics.– Give BS ABT within 3 hrs of ED admission/1 hr of
non ED admission.– Treat hypotension and/or elevated lactate with
fluids (20 ml/kg crystalloids).– Apply vasopressors for ongoing hypotension.– Maintain adequate CVP (>8) and ScvO2 (>70%).

SEPSIS BUNDLE
• Sepsis management bundle – (within 24 hrs of presentation), in accordance with ICU policy.– Give low dose steroids for septic shock.– Give rhAPC.– Maintain glucose control lower limit of normal ,
but < 180 mg/dl.– Maintain inspiratory plateau pressure < 30 cm H₂0
for ventillated patients.


THANK YOU