Management of Nonfebrile Seizures Eileen P. G. Vining and ... · Eileen P. G. Vining, MD,* and John...
Transcript of Management of Nonfebrile Seizures Eileen P. G. Vining and ... · Eileen P. G. Vining, MD,* and John...

DOI: 10.1542/pir.8-6-1851986;8;185Pediatrics in Review
Eileen P. G. Vining and John M. FreemanManagement of Nonfebrile Seizures
http://pedsinreview.aappublications.org/content/8/6/185the World Wide Web at:
The online version of this article, along with updated information and services, is located on
Print ISSN: 0191-9601. Village, Illinois, 60007. Copyright © 1986 by the American Academy of Pediatrics. All rights reserved.trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove
andpublication, it has been published continuously since 1979. Pediatrics in Review is owned, published, Pediatrics in Review is the official journal of the American Academy of Pediatrics. A monthly
at UNIV OF CHICAGO on May 23, 2013http://pedsinreview.aappublications.org/Downloaded from

EDUCATIONAL OBJECTIVE
98. Appropriate ability to assessthe risk of recurrent seizures aftera single nonfebrile convulsion (Re-cent Advances, 86/87).
pediatrics in review #{149} vol. 8 no. 6 december 1986 PIR 185
Management of Nonfebrile SeizuresEileen P. G. Vining, MD,* and John M. Freeman, MDt
“Dr Robinson, help-Johnny’s on thefloor jerking-I think he’s having a sei-zure!”
How often have you had a call sim-ilar to this? Because febrile seizuresoccur in 3% to 4% of your patientsand nonfebrile seizures occur in 0.5%of children in your practice, calls likethis must occur frequently.
What should you do for the parenton the phone? How should you helpJohnny? Both are your patients, par-ticularly at this time. A seizure is oneof the most frightening things a par-ent can observe. What tests shouldyou order? What can you tell theparent about the future? Should youtreat and with what?
The approach to seizures (febnleand nonfebrile) has changed dramat-ically in the past 20 years. At onetime, physicians were advised thatphenobarbital therapy should be in-stituted for all children with a firstseizure and therapy continued for theforeseeable future. For febrile sei-zures, that meant until they were 5or 6 years old. For nonfebrile sei-zures, that meant forever, or at leastuntil they were adults making theirown decisions. Such teaching is outof date. The approach to febrlle sei-zures has clearly changed, eliminat-ing therapy for the vast majority ofchildren.1 Not all first afebrile seizuresrequire treatment according to con-cepts of modern management. Whentreatment is instituted for a first orsecond seizure, it should be basedon the type of seizure, the carefulweighing of the risks of seizure re-currence, and the benefits and sideeffects of medication.2 Careful atten-tion must be paid to the cognitive andbehavioral effects of anticonvulsantdrugs, and they should be adminis-tered for the least time required.
Changes in the workup of patientswith nonfebrile seizures have also oc-curred as new data and approachesto evaluation have become available.
* Assistant Professor of Neurology and Pediat-rics, The Johns Hopkins University School ofMedicine, Baltimore.t Professor of Neurology and Pediatrics, TheJohns Hopkins University School of Medicine,Baltimore.
This article will update current think-ing on the approach to the first non-febrile seizure and its management.
WHAT DO YOU DO FOR MRSJONES ON THE PHONE?
Generalized tonic-clonic seizuresare exceedingly frightening to every-one who witnesses them. The childarches his back (tonic), turns some-what blue, and then begins therhythmic (clonic) jerking. There is
foam at the mouth. Many inexperi-enced observers are sure that thepatient will die or, at least, swallowhis tongue. The most important inter-vention at this point is reassurancethat these things will not happen. Anindividual cannot swallow the tonguebecause it is attached to the back ofthe throat. The blueness comes dur-ing the tonic phase in which respira-tion is inhibited. In addition, skin cir-culation may decrease while bloodgoes to the head. However, if thepatient becomes sufficiently hypoxic(a very rare event), the seizure willstop, and breathing will resume.Keeping the observers calm, havingthem turn the patient on his or herside, protecting him or her from sharpobjects, putting something soft suchas a pillow or a jacket under the headis all that is necessary. Most 9ener-alized tonic-clonic seizures last onlya few minutes, and the ambulanceneed not be called. The patientshould be observed for further sei-zures or other neurologic symptoms.An ambulance should be called onlyif a seizure lasts more than 1 5 mm-utes. If the seizure is still continuingwhen the child has been transportedto the emergency room, then it hasprobably reached a limit of approxi-mately 30 minutes (defined as statusepilepticus) and should be treatedwith intravenous medication. There isno evidence that a seizure lasting lessthan 30 minutes produces permanentbrain damage. There is evidence fromanimal experiments that a seizurelasting 30 minutes or longer beginsto produce changes in the brainwhich, if continued, might result inpermanent brain damage. Notice theitalicized words. Education of parents
and others to these facts can mark-edly reduce the cost and inconveni-ence faced by people with epilepsywho are taken to an emergency roomevery time they have a seizure.
When the seizure has stopped byitself, commonly ending with a deepsigh, the patient is usually in a sleepy(postictal) state. This will last five to1 5 minutes. When the patient wakesup, he or she may be confused and,therefore should be attended until heor she is alert and aware enough toreturn to work, home, or normal life.
Because status epilepticus is rarelythe initial episode, the seizure wouldusually have stopped before the par-ent calls. If the seizure is continuingthe first-aid measures descibed be-fore will be helpful. Most pediatricianswould want to see the child as soonas possible after the seizure to en-sure that the child has returned tonormal and that the episode is not asymptom of an acute disturbance af-fecting the CNS.
EVALUATION OF A FIRSTSEIZURE
The most important aspect of theevaluation of a seizure is the history.3There is no way to diagnose a seizureexcept by the correct interpretationof the events that occurred. Fortu-nately, with children, most events areobserved by an adult who should becontacted for the detailed observa-tion of what went on during the epi-sode. The history is vital to differen-tiating seizures from other episodesthat may alter consciousness in a
at UNIV OF CHICAGO on May 23, 2013http://pedsinreview.aappublications.org/Downloaded from

TABLE 1. ClassifIcation of Seizures
International Classification Old Terminology
Focal or local seizures
Jacksonian seizuresFocal sensory
Partial seizuresSimple partial seizures (consciousness
not impaired)With motor symptomsWith somatosensory or special
sensory symptomsWith autonomic symptomsWith psychic symptoms
Complex partial seizures (withimpairment of consciousness)Simple partial onsetWith impairment of consciousness at
onsetPartial seizures that secondarily
generalizeGeneralized seizures (convulsive or
nonconvulsive)Absence
AbsenceAtypical
MyoclonicClonicTonicTonic-clonicAtonic (astatic)
Psychomotor or temporal lobeseizures
Petitmal
Minor motorGrand melGrand malGrand malAkinetic, drop attacks
Nonfebrile Seizures
PIR 186 pediatrics in review #{149} vol.8 no. 6 december 1986
child, particularly fainting and breathholding, both of which may be accom-panied by tonic-clonic movement.Both cyanotic and “pallid” breath-holding spells are common inchildren. Classic (cyanotic) breath-holding spells involve a prolonged ex-piration phase usually precipitated bycrying. The child may become blueand sufficiently hypoxic to precipitatea brief tonic-clonic seizure. Pallidbreath-holding spells are really achildhood form of vasovagal syncopeand can often be simulated whilemonitoring the child by applying pres-sure to the eyeballs with productionof a vagal discharge. The heart rateis slowed and an occasional period ofbrief asystole may be seen. Precipi-tating events such as fear, anxiety,hyperventilation, and crying shouldbe sought. The history will also es-tablish if the seizure was associatedor concomitant with acute headtrauma, possible hypoglycemia, in-fection, cardiac problems, or drugingestion. No laboratory test can es-tablish with certainty that a child hada seizure. Information about focality,incontinence, alterations or loss ofconsciousness, and the postictal
state may help to differentiate a trueseizure from these other entities. Thepresence of fever in the appropriatelyaged child may help to separate fe-brile seizures from nonfebrile sei-zures. However, a seizure triggeredby fever cannot be accurately sepa-rated from a febrile seizure until theindividual goes on to have nonfebrileseizures.
After this careful and detailed his-tory, the physician usually should beable to separate nonseizure eventsfrom true seizures. However, occa-sionally, one cannot be certain. If thechild is otherwise doing well, it is farbetter to adopt an expectant attitudeand wait and see whether the epi-sode recurs. The parent can be edu-cated to gather more specific infor-mation to better define the nextevent. This is more important thanprematurely deciding that a child hashad a seizure.
Classification of the different typesof seizures is important to the clini-cian. There are certain types of sei-zures that will routinely recur. In ad-dition, it is important to determinewhether there is any element of fo-cality because this implies the possi-
bility of a localizable abnormalitywithin the brain. Certainly, it is alsonecessary to determine what type of
seizure a child had in order to makea more logical choice of drug. Finally,there is evidence that prognosis fordifferent types of seizures may bedifferent. The current system dividesseizures into partial (focal) and gen-eralized (including absence and tonic-clonic seizures). The currently usedterms are shown in parallel with theold terminology (Table 1).
A complete physical and neurologicexamination is always mandatory.Seizures may be associated with sys-
� temic illness, renal disease, hyperten-� sion, or metabolic conditions. A care-� ful neurologic examination should beI performed both to detect focal neu-� rologic deficit and to establish, when� possible, whether this deficit is new� or old. If new focal deficits are found,� more immediate diagnostic evalua-� tions should be performed. This ex-� amination should also form a baseline� for follow-up examination to detect
any evidence of a progressive neu-rologic deficit.
Which laboratory tests to obtainwill depend on the history and physi-cal examination findings (Table 2).There is no routine laboratory workupfor the patient who has had a seizure.Because hypoglycemia and hypocal-cemia can, on occasion, cause sei-zures without any otherwise detect-able disease, we favor blood testingfor glucose (after an overnight fast)and calcium levels. Tests for liverchemistries and a complete blood cellcount are particularly useful as base-line evaluations before starting anti-epileptic drugs.
An electroencephalogram (EEG)should be part of the initial workup ofa patient with seizures (Table 3).However, an EEG does not provideevidence to diagnose a seizure un-less a seizure occurs during the EEG.It is still the clinical description of anevent that is important. AbnormalEEG results are compatible with sei-zures, as are normal EEG findings.One treats the patient with seizures,not the EEG. The EEG does, how-ever, provide a baseline for furtherevaluation should the seizures be-come recurrent or change in pattern.Certain words in the EEG report areof special importance.4 Focal slowing
at UNIV OF CHICAGO on May 23, 2013http://pedsinreview.aappublications.org/Downloaded from

TABLE 2. Laboratory Evaluation TABLE 3. Electroencephalo-gram Findings and Importance
FastingOccasionally
helpfulRarely helpfulConsider as
baseline
Focal slowing
Focal spikes
Generalizedslowing
Spike-wave
Blood glucoseCa2�
Mg, P04, NaComplete
blood cellcount
Liver function
Lumbar punc-ture
Skull x-ray filmComputed to-
mography
EEG
Acute focaldisturb-ance-en-cephalitis,stroke, tu-mor, etc
Long-standingfocal proc-ess
Acute or long-standing
3/s seen in ab-sence,slower pat-tern seen inatypical ab-sence
NEUROLOGY
pediatrics in review #{149} vol. 8 no. 6 december 1986 PIR 187
on the EEG is important because itusually indicates an acute focal dis-turbance. It does not tell you the typeof disturbance. A finding of focalslowing is compatible with focal en-cephalitis, a stroke, a tumor, andother local disturbances. Focal slow-ing warrants further evaluation. Focalspikes, however, indicate a long-standing lesion and are of muchless diagnostic concern. Generalizedslowing may indicate an acute dis-turbance such as encephalopathy ormay be long-standing. A spike-wavepattern on the EEG is, however, use-ful in distinguishing absence seizures(formerly referred to as petit mal) fromother forms of epilepsy and fromother conditions such as daydream-ing. Spike-wave abnormalities canoften be precipitated by hyperventi-lation.
If an EEG is to be performed, itshould be complete and include hy-perventilation, photic stimulation, andsleep (spontaneous or induced withhypnotic agents).
When should an EEG be performedin relationship to the seizure? Underideal circumstances, it should bedone during a seizure, but such ser-endipity is unusual. It would be ofvalue to have an EEG immediatelyafter a seizure to confirm postictalphenomena such as slowing. If slow-ing is seen, the EEG should also berepeated two or more days after theseizure to establish whether theslowing was related to a temporaryphysiologic disturbance or underlyinganatomic abnormality. However, ingeneral, we obtain a routine, com-plete EEG during the interictal state,several days to several weeks afterthe seizure.
Skull x-ray films are not useful inthe evaluation of a patient who hashad a seizure. Only if the seizure isrelated to trauma and one is worriedabout a depressed skull fractureshould a skull film be performed. Acomputed tomographic (CT) scan isnot a routine part of the initial workupfor every child who has had a seizure.CT scans are far more useful thanskull x-ray film in looking for intracra-nial abnormalities, tumors, or vascu-lar problems, but these conditions arerare causes of epilepsy in children.We would reserve use of the CT scanfor the child who has had a focal
of Seizures
Test Comment
Consider asbaseline
Consider-es-pecially ifpossible in-fection orprodromalchanges inbehavior
NoNot routine-
useful ifclearfocality
Yes-getcompletestudy
slow-wave abnormal finding on theEEG, for one who has acquired focaldeficit, or for the child who has con-tinuing focal seizures. A CT scan mayalso be useful in the child whose sei-zure pattern is worsening or chang-ing. To reiterate, a CT scan need notbe obtained as part of the initialworkup of the child who has had aseizure.
TO TREAT OR NOT TO TREAT
The decision to initiate therapyafter a single seizure must includeconsiderations of such factors as theage of the patient, the type of seizure,predisposing factors, the psychologicand social consequences of furtherseizures, and the chance of recur-rence of seizures. These risk factorsshould be weighed against the risksand consequences of the medicationthat will be used. These risks andconsequences include the effects ofmedication on learning and behavior,the need to take daily medication, andthe effect of labeling (Figure).5
In this discussion, we are concen-trating on generalized tonic-clonicseizures and partial (focal) seizures.Absence seizures, myoclonic sei-
Findings Meaning
zures and infantile spasms, are rarelyseen at the time of the initial singleseizure.
WHAT ARE THE RISKS OFRECURRENCE AFTER A SINGLESEIZURE?
Among the first questions the par-ent asks are, “Why did he have aseizure?” and “Will it happen again?”Because more than half of childhoodseizures are idiopathic, the likelihoodof discovering the etiology for theseizures is small. Despite differing re-ported estimates of recurrence rates,due to variability in methodology, weare beginning to accumulate data thatgive us guidelines as to who is mostlikely to experience a recurrence (Ta-ble 4).
Hauser et a16 reported on 238 peo-pIe (75% older than 19 years of age)who had a single, nonsymptomaticseizure. Of these 238 individuals,27% experienced a recurrence by 36months of follow-up. Approximatelyone fourth of the patients had hadsome remote neurologic insult towhich the seizure was attributed, andthose patients had a higher recur-rence rate (31 %) than those in whomno etiology could be determined andfor whom the recurrence rate wasonly 20%. EEGs were obtained inalmost all patients and were onlyhelpful in predicting recurrence in thesmall group (5%) with spike-wave ab-normalities. In this group, the recur-
at UNIV OF CHICAGO on May 23, 2013http://pedsinreview.aappublications.org/Downloaded from

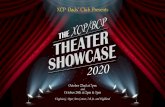
RISKS AND BENEFITS OF DRUG THERAPY
Non- Treatment Treatment
Figure. Balancing risks and benefits of treatment.
Nonfebrile Seizures
PIR 188 pediatrics in review #{149} vol. 8 no. 6 december 1986
rence rate was 50%. There were noEEG data to compare abnormal focalfindings. When a sibling had seizures(7%), the recurrence rate was 35%.Abnormal neurologic examinationfindings were not associated with asignificantly increased recurrencerisk.
Treatment with anticonvulsantdrugs did not affect the recurrencerate. Treatment was recommendedin 69% of patients, but the choice ofdrugs and compliance are unknown.One could certainly question whetherthose with known previous neuro-logic insult (remote symptomatic)were more concerned about the de-velopment of seizures because theyknew they had a potential cause andwere, therefore, more prone to havemedications prescribed and to com-ply.
The study by Hirtz et a17 used thedata from the National CollaborativePerinatal Project (NCPP) in which ap-proximately 54,000 children were fol-lowed from birth to 7 years of age.They reviewed the records obtainedat the routine follow-up visits, whichwere a year apart after 2 years ofage. There were 518 children identi-fied as having one or more nonfebrileseizures. One or more recurrenceswere experienced by 313 (61%). Inthe group of 435 who did not have
absence, myoclonic seizures, or in-fantile spasms, the recurrence ratewas 55%. Unfortunately, 6% of thesechildren had atypical staring spells,many of which may have been thefrequently recurring absence sei-zures. It is difficult to compare thisgroup to that of Hauser et al but, asin the work of Hauser et al, there isthe sense that those with generalizedmotor seizures (tonic-clonic) hadfewer recurrences (48%). No EEGdata are available and a significantpercentage (27%) may have beentreated.
In the most recent study, by Cam-field et al,#{176}children were identifiedfrom EEG records. Of children with afirst seizure, 86% were scheduled tobe studied by EEG. Of 757 possiblepatients, 1 76 had experienced a sin-gle, unprovoked seizure before theEEG and 168 were available for fol-low-up. More than one seizure wasexperienced before the EEG by 141patients, suggesting that somewhatless than 86% of children actuallyhave an EEG performed after the firstseizure. There were 428 children whowere believed not to have experi-enced a seizure at all but were be-lieved to have had pallid syncope orbreath-holding spells. Unlike thestudy by Hirtz et al, there were nochildren with symptomatic seizures.
Seizures were considered focal ifthere were focal EEG changes, evenif only tonic-clonic symptoms werereported. Children were believed to
� have abnormal neurologic examina-� tion findings if there were excessive
soft signs. Unlike the studies by Hau-ser et al and Hirtz et al, children withabnormal neurologic examinationfindings were believed to have morefrequent recurrences; ie, 73%. Ther-apy was recommended for 70% ofthe children; compliance was not as-certained.
Camfield et al have generatedprognostic data by combining prog-nostic factors. The best prognosisexisted if there were normal neuro-logic examination findings, a nonepi-leptiform EEG tracing, and a gener-alized tonic-clonic seizure. In thispopulation, only 30% recurrence isexpected. On the other hand, a childwith a partial complex seizure, focalepileptic EEG change, and abnormalneurologic examination findings ex-perienced a 96% recurrence rate.
A fourth study in progress sug-gests that, in a less biased, prospec-tive population, the risk of recurrenceafter a first seizure is less than 20%.8a
One constant theme that runsthrough these three studies is that, ifthere is a second seizure, the likeli-hood of a third is 50% to 75%, re-gardless of other factors. In all threestudies, it is clear that, if recurrencetakes place, it tends to be within thefirst 6 months to 1 year after the initialseizure and that recurrence virtuallynever occurs beyond 2 to 3 years.
Because the generalized tonic-clonic seizure has a reasonably lowchance of recurrence (20% to 48%),and because of the consequences ofmedications, we do not usually initiatetherapy after a single seizure.
Is medication mandatory after asecond seizure? Decisions about em-barking on therapy after a secondgeneralized tonic-clonic seizureshould include consideration of thetime span between the two seizures,the age of the child, and the potentialconsequences should another sei-zure occur. Because these conse-quences may be different, and per-haps less for the younger child ascompared with the older child or theadolescent, one cannot make a fixedrule about who should be treated.
at UNIV OF CHICAGO on May 23, 2013http://pedsinreview.aappublications.org/Downloaded from

Hauseret al�
<19 yr(27%)
27 (36me)
Idiopathic (73)Generalized tonic-
Remote symptomatic(27)
31 Age at first seizureSex
(N = 238) donic (45)Complex partial (7)Simple partial (20)
Idiopathic & spike-wave (5)
Idiopathic & siblingwith seizures (7)
50
35
Seizure typesOnset with statusIdiopathicAbnormal neurobgic
examination findingsTreatment
Hirtzet al7
I mo-7 yr
Until 7 yr 55 Generalized motor(72)
48 Focal motor (21)AtypiCal staring (6)
6593
Age at first seizureAbnormal neurologic
(N = 435) Symptomatic (3) 23 lkiprovoked (70)Previous febrile
seizure (7)Prior neonatal
seizure (7)
6965
74
examination findingsFamily history of non-
febrile seizure
Camfieldet al�
1 mo-16 yr
31 .4 ±
16 mo52 Normal neurologic
examination find-47 Abnormal neurologic
examination find-73 History of febrile
seizure (17)(N = 168) ings (82)
Tonic-clonic (45) 44ings (1 8)
Partial complex (19)Focal epileptic dis-
charge (30)Focal seizure without
2#{176}generalization(20)
ftjlfocalwith2#{176}gen-eralization (50)
7968
75
60
Spike-wave EEG (14)
NEUROLOGY
pediatrics in review #{149} vol. 8 no. 6 december 1986 PIR 189
TABLE 4. Recurren ce After First Nonfebnle Seizure
StudyAge
(% ofPatients)
Duration ofFOllOW-lip
Recur-ring
Favorable Predictors Unfavorable Predictors
NeutralCat�.�(% of Patients)
%R�-
ring
Category� Patients)
%R�-�
22 mo 20
Certainly, a child who has had two ormore generalized tonic-clonic (grandmal) seizures should be consideredfor therapy. The risks accompanyingrecurrent seizures and the benefits oftherapy should be fully discussedwith the family. The risks of use ofanticonvulsant agents include bothallergic and idiosyncratic reactions,chronic side effects on many organsystems, and the effects on the de-veloping brain. Children with seizuresthat impair consciousness, such asabsence and partial complex sei-zures, should probably be treatedbecause these types tend to recurfrequently, and there may be manysubclinical electrical events that caninterfere with learning and behavior.
WHY DO YOU TREATSEIZURES?
Most seizures are treated primarilybecause of their psychosocial risks,and these risks are clearly age de-pendent. Although there is a some-what increased mortality associatedwith seizures, it is not clear that thisis less in patients who are on medi-cation. The risks of status epilepticus
occurring are small, and there are nodata to suggest that they are sub-stantially lessened by anticonvulsantmedication.8b The effectiveness ofanticonvulsant drugs in preventingthe recurrence of seizures has alsobeen questioned.9 Apparently, pre-vention of recurrence does not takeas smooth and easy a course as wehad once thought. Parents need tobe aware that medication and dosagemust be tailored on an individual ba-sis and that a quick remedy is notalways possible.
WHAT ANTICONVULSANTAGENT TO CHOOSE?
For patients with generalized tonic-clonic seizures and simple partial sei-zures, the standard anticonvulsantdrugs are phenobarbital, phenytomn,and carbamazepine. Phenobarbitalhas been used for generations. It isthe cheapest and one of the safestanticonvulsants available. There arerare allergic or idiosyncratic side ef-fects. The major disadvantage ofphenobarbital is a 30% to 40% mci-dence of hyperactivity, behavioraldisorders, and sleep disorders in
younger children. Sedation, althoughusually tolerated, is common, and itseffects are often not fully recognizeduntil the medication is discontinued.A recent study indicates that pheno-barbital may interfere with learningand behavior even in the absence ofobservable side effects.1#{176}For thesereasons, it is rarely our first choicedrug except when cost or single dailydosing becomes a significant consid-eration.
Phenytoin is slightly more expen-sive but also effective. In addition todrug rashes and occasional liver orhematologic side effects, its majorunpleasant side effects are gum hy-perplasia, occurring in as many as90% of children, hirsutism, and coar-sening of features. Gum hyperplasiamay be diminished by good dentalhygiene, but there may be major ef-fects on permanent dentition. Be-cause of these side effects, we prefernot to use phenytomn for our initialdrug. If phenytomn is used, it shouldbe recognized that generic forms ofphenytoin are as effective in control-ling seizures as Dilantin, but thesegeneric forms have different rates ofabsorption and bioavailability. There-
at UNIV OF CHICAGO on May 23, 2013http://pedsinreview.aappublications.org/Downloaded from

Nonfebrile Seizures
PIR 190 pediatrics in review #{149} vol. 8 no. 6 december 1986
fore, care must be taken to assuresimilar blood levels when switchingfrom Dilantin to generic phenytomn orwhen switching between genericphenytoin preparations. The genericform should be used twice a day,whereas Dilantin may be used oncea day, except in small children.
Carbamazepine (Tegretol) is saidto cause hematologic problems anda host of other side effects. Althoughthe Physicians’ Desk Reference(PDR) recommends checking thedrug frequently for multiple hemato-logic and hepatic parameters, the fre-quency of problems is small and notdissimilar to those found with otheranticonvulsant drugs. Although oc-casional allergic and idiosyncratic re-actions may occur, the major dose-related side effects are blurred visionor double vision occurring about 1hour after a dose. Because the half-life of the drug is short, it is recom-mended that it be given three or fourtimes a day but we have found thattwice daily dosing is usually adequateand tolerated. It would appear thatthere is less effect of carbamazepineon neuropsychologic function. Weprefer it as our initial anticonvulsantmedication for most partial seizuresand for generalized tonic-clonic sei-zures.
Sodium valproate (Depakene, De-pakote) is a useful drug for patientswith tonic-clonic seizures and may behelpful in patients with partial com-plex seizures. The side effect of mostconcern is severe hepatotoxicity.This occurs more frequently in thevery young child receiving more thanone medicine. The most frequentlydescribed side effects are gastroin-testinal disturbances (alleviated bythe enteric coated preparation),tremor, and alopecia. Behavioral andcognitive disturbances appear to beinfrequent and generally mild. Half-lifeis generally believed to be less than
1 2 hours, but twice daily dosing isusually appropriate. It is our drug ofchoice for patients with atypical ab-sence, myoclonic and atonic sei-zures.
MONITORING
The scope of this paper pertains tothe more immediate situations of di-agnosis, evaluation, and initiation oftherapy. It would be remiss, however,not to mention the excellent prog-nosis for most children. This messageshould be conveyed to parents andto the children themselves. If seizurescan be controlled for 2 years, 75% ofchildren can be slowly weaned fromthe medication without experiencingrecurrence. The decision to withdrawtherapy is just as important as thedecision to prescribe it.11
While the child is on anticonvulsantdrugs, it is important to monitor thechild for medication side effects andlearning and behavioral problems andto be sure that overprotection andpsychologic and social problems arenot occurring. Monitoring serum 1ev-els of the medication can be usefulbut serves only as a guide. A medi-cation is effficacious when seizuresare controlled without toxicity to thepatient; a drug is toxic when the pa-tient experiences side effects. Toxic-ity does not exist solely on the basisof a reported drug level. It must becorrelated with the patient’s condi-tion.12
SUMMARY
Single, nonfebrile seizures are notepilepsy, and although they oftencause a major psychic trauma to thefamily they do not necessarily requirehospitalization, CT scanning, or ex-tensive workup. Anticonvulsant treat-ment is not obligatory and should, ifused, be individualized. Only 30% of
tonic-clonic seizures will recur, andmost children who do require therapycan have it discontinued after 2 years.
REFERENCES
1 . Freeman JM: Febrile seizures: An end toconfusion. Pediatrics 1978;61 :806-808
2. Vining EPG, Freeman JM: Where, why andwhat type of therapy. Pediatr Ann1985;1 4:741-745
3. Vining EPG, Freeman JM: Classificationand evaluation of seizures. Pediatr Ann1985;1 4:730-732
4. Lewis DV, Freeman JM: The electroen-cephalogram in pediatric practice: Its useand abuse. Pediatrics 1977;60:324-330
5. American Academy of Pediatrics, Commit-tee on Drugs: Behavioral and cognitiveeffects of anticonvulsant therapy. Pediat-rics 1985;76:644-647
6. Hauser WA, Anderson VE, LoewensonRB, et aI: Seizure recurrence after a firstunprovoked seizure. N Engl J Med 1982;307:522-528
7. Hirtz DG, Ellenberg JH, Nelson KB: Therisk of recurrence of non-febnle seizuresin children. Neurology 1984;34:637-41
8. Camfield PR, Camfield CS, Dooley JM, etal: Epilepsy after a first unprovoked sei-zure in childhood. Neurology 1985;35:1657-1660
8a. Shinnar 5, Zeitlin-Gross L, Moshe 5, etal: The low risk of seizure recurrence fol-lowing a first unprovoked seizure in chil-dren and adolescents: A prospectivestudy, abstracted. Ann Neurol 1986;20:388
8b. Freeman JM, Tibbles J, Camfield C, etal: Benign epilepsy of childhood: A spec-ulation and its ramifications. Pediatrics, inpress, 1987
9. Camfield PR, Camfield CS, Smith EC, etal: Newly treated childhood epilepsy: Aprospective study of recurrences and sideeffects. Neurology 1985;35:722-725
10. Vining EPG, Mellits ED, Dorsen MM, et aI:Effects of phenobarbital and sodium val-proate on neuropsychological functionand behavior, abstracted. Ann Neurol1983;1 4:360
11. Shinnar 5, Vining EPG, Mellits ED, et al:Discontinuing antiepileptic medication inchildren with epilepsy after two years with-out seizures: A prospective study. N EnglJ Med 1985;313:976-980
12. Vining EPG, Freeman JM: Monitoring: Themost important role of the pediatrician.Pediatr Ann 1985;1 4:747-756
at UNIV OF CHICAGO on May 23, 2013http://pedsinreview.aappublications.org/Downloaded from

DOI: 10.1542/pir.8-6-1851986;8;185Pediatrics in Review
Eileen P. G. Vining and John M. FreemanManagement of Nonfebrile Seizures
ServicesUpdated Information &
http://pedsinreview.aappublications.org/content/8/6/185including high resolution figures, can be found at:
Permissions & Licensing
/site/misc/Permissions.xhtmlits entirety can be found online at: Information about reproducing this article in parts (figures, tables) or in
Reprints/site/misc/reprints.xhtmlInformation about ordering reprints can be found online:
at UNIV OF CHICAGO on May 23, 2013http://pedsinreview.aappublications.org/Downloaded from