Immunohistology - Vidrolab 2 SA
Transcript of Immunohistology - Vidrolab 2 SA

ImmunohistologyBreast pathology
Detection of invasion/myoepithelial markers
The expanding role of immunohistochemistry in breast pathology is enabled by a growing list of available antibodies. Immunohistochemistry can help to distinguish usual ductal hyperplasia
from atypical ductal hyperplasia or low-grade carcinoma in situ, to subtype a carcinoma as ductal or lobular, basal or luminal, and to detect invasive carcinomas.
Almost all benign glands and in situ carcinomas are surrounded by a myoepithelial cell layer and an intact basal membrane. The presence of myoepithelial cells has always been considered to be an important criterion that separates in-vasive from non-invasive neoplasms. In case of invasive carcinomas malignant epithelial cells penetrate the myoepithelial cell layer as well as the basal membrane and invade the stroma.
Smooth muscle Actin (SMA), Calponin and smooth muscle Myosin heavy chain (SMMHC) are typical myoepithelial cell markers used in immunohistochemistry. Myoepithelial cells (or basal cells) are also positive for typical basal cell markers like Cytokeratin 5 (CK5), CK14, CK HMW
(clone 34ßE12) as well as p63. In immunohisto-chemistry antibodies against these markers are often used in form of cocktails. Because of its low sensitivity and specificity S-100 is no longer recommended for detecting myoepithelial cells. It is also considered critical to use basal mem-brane markers like Laminin and Collagen IV for detecting invasion because invasive tumour cells can synthesise basal membrane structures themselves.
Recent publications also describe NGFR (Nerve Growth Factor Receptor), P-Cadherin, Maspin and WT-1 as useful markers for myoepithelia. Nevertheless, some of them show a reaction with myoepithelial cells.
Benign and malignant breast lesions – therapeutically relevant antibodies
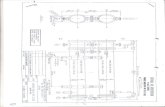
The picture shows a typical structure of epithelium in thoracic ducts and glands. The epithelium consists of basal membrane, myoepithelial cells,
and luminal epithelial cells. This structure is also found in all benign lesions and in situ carcinomas of the breast. The only known exception is the
microglandular adenosis, a benign lesion which contains no myoepithelial cell layer (Lerwill, 2004)
Luminal epithelial cellsCK7, CK8, CK18, CK19, GATA-3
Basal membraneLaminin, Collagen IV
Myoepithelial cellsCK5, CK14, CK HMW, SMA, Calponin, SMMHC, p63, CD10
Stromaincluding myofibroblasts and vessels
Myosin SMMHC stained on normal breast tissue (MSK081)
p63 stained on breast carcinoma (MSK087)
Differentiation of benign and in situ proliferations from invasive carcinomas

ImmunohistologyBreast pathology
p63
The advantage of p63 as myoepithelial cell marker is its high specificity. Unlike other smooth muscle markers p63 is not expressed in myofibroblasts and blood vessels. Very rarely p63 stains positive in usual ductal hyperplasia (UDH) and invasive carcinomas but the staining is restricted to few cells and considerably weaker compared to the stain in myoepithelial cells. Dedifferentia-ted carcinomas and carcinomas with squamous cell differentiation frequently show p63 staining.
Myosin SMMHC (smooth muscle myosin heavy chain)
Myosin SMMHC is a marker for smooth muscle cells with sensitivity similar to SMA or Calponin. In contrast to SMA or Calponin SMMHC shows only minor cross-reactivity with myofibroblasts. Thus SMMHC is a sensitive and specific myoepithelial marker although it also stains blood vessels.
SMA (smooth muscle Actin)
SMA strongly stains myoepithelial cells of the breast but also reacts with myofibroblasts in reac-tive stroma on invasive breast carcinomas, DCIS and sclerotic lesions. Blood vessels are positive too. SMA is rarely positive in scattered epithelial cells of UDH.
Calponin
Calponin is a contraction protein which is expressed in differentiated smooth mucle cells. It shows lower cross-reactivity with myofibroblasts when compared with SMA. Calponin stains blood vessels and shows focal positivity in invasive tumour cells in rare cases.
Expression of several myoepithelial markers
Marker Localisation Myoepithelial cells
Myofibro-blasts
Vascular SM/vessels
Luminal cells
Epithelial cells
Tumour cells
SMA Cytoplasmic +++ ++ +++ - rarely + -
Calponin Cytoplasmic +++ + +++ - rarely + rarely +
SMMHC Cytoplasmic ++ + +++ - -
p63 Nuclear ++ - - + occasionally + rarely +
CD10Cytoplasmic and
membranous+ + - + +
S100 Cytoplasmic + +/- - + variable
Basal CK Cytoplasmic ++ - - + +
Bibliography
Lerwill MF. Current practical applications of diagnostic immunohistochemistry in breast pathology. Am J Surg Pathol 28:1076-1091, 2004 (Review)
Moriya T et al. Usefulness of immunohisto-chemistry for differential diagnosis between benign and malignant breast lesions. Breast Cancer 16:173-178, 2009
Werling RW et al. Immunohistochemical dis-tinction of invasive from noninvasive breast lesions: a comparative study of p63 versus calponin and smooth muscle myosin heavy chain. Am J Surg Pathol 27:82-90, 2003
Yeh IT, Mies C. Application of immunohisto-chemistry to breast lesions. Arch Pathol Lab Med. 132:349-358, 2008 (Review)
E-Cadherin
Staining of E-Cadherin to distinguish invasive lobular from invasive ductal carcinomas is often considered to be the “Gold Standard” of the question DCIS versus LCIS. DCIS usually shows memb-ranous staining of the neoplastic cells whereas LCIS is negative for E-Cadherin in almost all cases. In benign glands E-Cadherin shows a strong membrane staining in luminal cells and a granular staining pattern in myoepithelial cells.
Due to the different therapies for ductal and lobu-
lar carcinomas of the breast it is of great impor-
tance to reliably diagnose these two carcinoma
types. In cases of ambiguous morphology of the
H&E stain the immunohistochemistry can be very
useful. However, one must be aware of different
hybrid forms which show invasive lobular as well
as invasive ductal characteristics.
Invasive ductal versus invasive lobular carcinoma (DCIS vs. LCIS)
E-Cadherin, clone EP700Y (Cat. No. RBK043)

ImmunohistologyBreast pathology
DCIS versus LCIS – reactivity of several markers
Marker DCIS LCIS
E-Cadherin + -
Catenin (delta) p120 membranous Cytoplasmic
CK HMW 34ßE12 mostly – or strongly diminished mostly +
CK8 diffuse cytoplasmic perinuclear
Bibliography
Acs et al. Differential expression of E-cadherin in lobular and ductal neoplasms of the breast and its biologic and diagnostic implications. Am J Clin Pathol 115:85-98, 2001
Bratthauer GL et al. Combined E-cadherin and high molecular weight cytokeratin immunoprofile differentiates lobular, ductal, and hybrid mammary intraepithelial neo-plasias. Hum Pathol 33:620-627, 2002
Goldstein NS et al. E-cadherin reactivity of 95 noninvasive ductal and lobular lesions of the breast. Implications for the interpretati-on of problematic lesions. Am J Clin Pathol 115:534-542, 2001
The usual ductal hyperplasia UDH, the atypical duc-
tal hyperplasia ADH, as well as the ductal carcinoma
in situ DCIS and the lobular neoplasia are all beni-
gn or pre-invasive lesions of the breast according
to the German guideline S3. UDH is classified as
benign lesion whereas the ADH is categorised as
pre-invasive or suspiciously malignant with further
consequences for the patient.
According to the S3 guideline the detection of ADH
in a biopsy is an indication for an operation. Pati-
ents with UDH face a 1.5 fold higher risk for a car-
cinoma; patients with ADH have to face a 4-5 fold
higher risk for a carcinoma than other people. ADH
is regarded as potential precursor lesion of carcino-
ma (Hartman et al., 2005).
UDH can be distinguished from ADH by immunohis-
tochemistry using the marker constellation of the
involved cell types. These are luminal epithelial cells
and myoepithelial (or basal) cells. In UDH both cell
types are involved whereas in ADH (or low-grade
DCIS) mostly the luminal epithelial cells play a role.
Thus, the “polymorph” UDH can be characterised by
using the typical basal cell markers like Cytokeratin
5 (CK5), CK14 or the high-molecular weight CK (CK
HMW, 34ßE12).
90–100 % of the UDH cases show these markers but
only 10 % of the ADH cases.
The majority of ADH cases is characterised by the
typical luminal epithelial cell markers which are the
CK7, CK8, CK18, and CK19.
UDH versus ADH/DCIS
Cytokeratin 8/18, clone IVT2000 (Cat. No. MSK035)
Bibliography
Böcker W et al. Usual ductal hyperplasia of the breast is a committed stem (progenitor) cell lesion distinct from atypical ductal hyperplasia and ductal carcinoma in situ. J Pathol 198:458-467, 2002
Hartmann LC et al. Benign breast disease and the risk of breast cancer. N Engl J Med 353:229-237, 2005
Lacroix-Triki M et al. Value of cytokeratin 5/6 immunostaining using D5/16 B4 antibody in the spectrum of proliferative intraepithelial lesions of the breast. A comparative study with 34betaE12 antibody. Virchows Arch 442:548-554, 2003
Catenin (delta) p120
The Catenin (delta) p120 protein forms a complex with E-Cadherin. This complex is associated with the cell membrane and involved in cell-cell contacts and the regulation of the cytoske-leton. P120 shows a membranous staining in normal ducts and ductal carcinomas. In lobular carcinomas, were E-Cadherin is missing or inoperable, p120 is accumulated in the cytoplasm of the tumour cells. Since loss of E-Cadherin is a very early event in the development of LCIS p120 constitutes itself as a positive marker for LCIS.
Cytokeratins
Cytokeratin HMW (34ßE12) can be used as an additional marker to E-Cadherin. DCIS shows no staining or strongly diminished CK HMW staining whereas LCIS is positive for CK HMW (Bratt-hauer, 2002). However, the result of different publications advice to be aware of different hybrid forms which show positivity for both markers. Cytokeratin 8 shows a diffuse cytoplasmic staining in ductal carcinomas whereas lobular carcinomas show a perinuclear staining for CK8.

ImmunohistologyBreast pathology
Antibodies for evaluating breast carcinomas
Description IVD/CE Host Clone Method Pre-treatement Form Dilution Amount Cat. No.
Actin alpha (Smooth Muscle) Mouse 1A4 P None Ready-to-Use - 14 ml BMS001
Actin alpha (Smooth Muscle) ✔ Mouse 1A4 P None
Ready-to-Use - 6 ml MSG030
Concentrate ~ 1:1001 ml MSK030
0.5 ml MSK030-05
Calponin-1 ✔ Rabbit EP789Y P, F CitrateReady-to-Use - 6 ml RBG041
Concentrate ~ 1:50 - 1:200 0.5 ml RBK041-05
Catenin (delta) p120 Rabbit polyclonal P, F CitrateReady-to-Use - 7 ml 503-17531
Concentrate ~ 1:100 1 ml 503-17534
CD4 (T-Cell helper/inducer) Rabbit SP35 P, F CitrateReady-to-Use - 7 ml 503-3351
Concentrate ~ 1:50 1 ml 503-3354
CD8 (T-Cell cytotoxic/suppressor) Rabbit SP16 P, F Citrate Ready-to-Use - 14 ml BRB036
CD8 (T-Cell cytotoxic/suppressor) ✔ Mouse C8/144B P, F EDTA pH 8 or 9
Ready-to-Use - 6 ml MSG011
Concentrate ~ 1:1001 ml MSK011
0.5 ml MSK011-05
CD10 (CALLA) ✔ Mouse 56C6 P, F Citrate
Ready-to-Use - 6 ml MSG070
Concentrate ~ 1:25 - 1:501 ml MSK070
0.5 ml MSK070-05
Cytokeratin (HMW) Mouse 34ßE12 P, F Citrate or Pepsin Ready-to-Use - 14 ml BMS015
Cytokeratin (HMW) ✔ Mouse 34ßE12 P, F Citrate or Pepsin
Ready-to-Use - 6 ml MSG027
Concentrate ~ 1:25 - 1:501 ml MSK027
0.5 ml MSK027-05
Cytokeratin 5/6 Mouse D5/16B4 P, F Citrate Ready-to-Use - 14 ml BMS017
Cytokeratin 5/6 ✔ Mouse D5/16B4 P Citrate
Ready-to-Use - 6 ml MSG034
Concentrate ~ 1:50 - 1:1001 ml MSK034
0.5 ml MSK034-05
Cytokeratin 5/14 Mouse XM26 & LL002 P, F Citrate Ready-to-Use - 14 ml BMS023
Cytokeratin 7 Mouse OV-TL 12/30 P, F Citrate Ready-to-Use - 14 ml BMS030
Cytokeratin 7 ✔ Mouse OV-TL 12/30 P, F Citrate
Ready-to-Use - 6 ml MSG032
Concentrate ~ 1:100 - 1:2001 ml MSK032
0.5 ml MSK032-05
Cytokeratin 8/18 Mouse IVT2000 P Citrate
Ready-to-Use - 6 ml MSG035
Concentrate ~ 1:100 - 1:2001 ml MSK035
0.5 ml MSK035-05
Cytokeratin 19 ✔ Mouse A53-B/A2.26 P, F Citrate
Ready-to-Use - 6 ml MSG017
Concentrate ~ 1:200 - 1:3001 ml MSK017
0.5 ml MSK017-05
E-Cadherin Mouse ECH-6 P Citrate Ready-to-Use - 14 ml BMS031
E-Cadherin ✔ Mouse ECH-6 P Citrate
Ready-to-Use - 6 ml MSG033
Concentrate ~ 1:1001 ml MSK033
0.5 ml MSK033-05
E-Cadherin ✔ Rabbit EP700Y P, F Citrate
Ready-to-Use - 6 ml RBG043
Concentrate ~ 1:50 - 1:2001 ml RBK043
0.5 ml RBK043-05
Myosin SM Heavy Chain (SMMHC) ✔ Mouse SMMS-1 P, F CitrateReady-to-Use - 6 ml MSG081
Concentrate ~ 1:100 - 1:500 0.5 ml MSK081-05
p63 Mouse Y4A3 P, F Citrate Ready-to-Use - 14 ml BMS020
p63 Mouse 4A4 P, F Citrate Concentrate ~ 1:50 - 1:751 ml MSK087
0.5 ml MSK087-05
Anhaltinerstraße 16 | 14163 Berlin | Fon +49 30 804 984 990 | Fax +49 30 804 984 999 [email protected] | www.zytomed-systems.com Breast pathology-Mai 2013-E
Distribuído por:
E
Vidrolab 2, S.A. www.vidrolab.pt
















![[XLS]Grants & Fellowships Admin: Excel Download · Web viewDetecting Iron Content of Multiple Sclerosis Lesions Through Techniques in Immunohistology and Immunoflourescence with Dr.](https://static.fdocuments.us/doc/165x107/5ae59b367f8b9a87048ccdbc/xlsgrants-fellowships-admin-excel-download-viewdetecting-iron-content-of-multiple.jpg)

