Heart Failure and Coronary Artery Disease€¦ · Heart Failure and Coronary Artery Disease...
Transcript of Heart Failure and Coronary Artery Disease€¦ · Heart Failure and Coronary Artery Disease...
37th Panhellenic Congress of Cardiology
Heart Failure and Coronary Artery
Disease
Filippos Triposkiadis, MD, FESC, FACC Professor of Cardiology Director, Department of Cardiology Larissa University Hospital Larissa, Greece
Athens, October 20-22, 2016
Characteristics of Hospitalized Patients with HF
LVEF ≥ 50% (n=40,354)
40%≤LVEF<50% (n=15,184)
LVEF<40% (n=55083)
Age (years) 78 (67-85) 76 (65-84) 70 (58-80)
Female sex (%) 63 47 36
Body mass index>30 kg/m2 (%)
33 29 25
Anemia 22 20 14
Hypertension 80 77 72
Diabetes (oral therapy) 24 24 22
Diabetes (insulin) 22 22 18
Chronic/recurrent atrial fibrillation
34 34 28
Coronary artery disease 44 54 52
Pulmonary disease 33 30 27
Chronic kidney disease 52 52 48
Steinberg B, et al. Circulation 2012;126:65-75
Hypertension, Obesity, Diabetes, and MI are the
Major Determinants of HF Phenotype1019 consecutive HF patients (age 71.7±12.3 years, male 56.9%, mean LVEF 42.8±14.4%, HFpEF 46.6%) referred to the outpatient HF Clinic of a tertiary University Hospital were screened for major HF comorbidities, from January 2014 to December 2015.
Giamouzis G, et al. Heart Failure 2016, Florence
Chart Title
Anemia
CKD
Obesity
COPD
Diabetes
Atrial fibrillation
Myocardial infarction
Hypertension
0 20 40 60 80
72,3
39,8
26,2
21,3
13,6
39,4
18,9
28,2
Comorbidities
Prevalence (%)
Variable Odds ratios* (95% CI) P value
Hypertension 9.43 (5.85, 15.17) <0.0001
Myocardial infarction 0.06 (0.04, 0.09) <0.0001
Obesity 3.24 (2.23, 4.69) <0.0001
Diabetes 0.57 (0.37, 0.90) 0.01
*Higher odds for: i) HFpEF, if OR>1.0; ii) HFrEF, if OR<1.0
Determinants of the HF Phenotype
Giamouzis G, et al. Heart Failure 2016, Florence
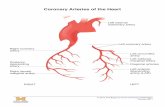
Definition of Ischemic Cardiomyopathy (?) (Ischemic HFrEF) for Use in Clinical Research
The clinical history and coronary anatomy of pts with symptomatic HF and LVEF ≤40% undergoing diagnostic coronary angiography between 1986 and 1999 (n =1,921) was assessed. Five classification schemes were tested to develop the best definition of ischemic cardiomyopathy for prognostic purposes. Patients with ≥ 75% stenosis of the LMCA or proximal LAD were included in the ischemic group.
Years Years
Surv
ival
Surv
ival
Felker GM, et al. J Am Coll Cardiol 2002;39:210–8
Non ischemic
Ischemic
1 VD
2 VD
3 VD
No significant CAD
Patients with single-vessel disease (no LMCA or proximal LAD) and no history of MI or revascularization should be classified as nonischemic for prognostic purposes.
Ischemic Cardiomyopathy (Ischemic HFrEF): Independent Predictors of Survival in the Best
Multivariable Model
Felker GM, et al. J Am Coll Cardiol 2002;39:210–8
Εffect of Coronary Artery Disease in HFpEF Survival
Hwang SJ, et al. J Am Coll Cardiol 2014;63:2817–27
Patients discharged (2004-2012) from Mayo Clinic with HFpEF (n=376) who had coronary angiography within 1 year of hospital discharge (CAD, n=255, 68%) and echocardiography within 6 months before angiography. Median follow up was ≈1500 days
Operating Characteristics of Stress Testing in HFpEF
Hwang SJ, et al. J Am Coll Cardiol 2014;63:2817–27
N=376, Treadmill ECG 16%, Stress echocardiography 39%, nuclear studies 45%
Development of Ischemic Heart Failure as a Time-Dependent Phenomenon
Schuster A, et al. J Am Coll Cardiol 2012;59:359–70
Rienks M, et al. Circ Res. 2014;114:872-888
Complex Cardiac ECM with Potential Functions of Some Residing Matrix Elements
Myocardial InfarctionHealthy Myocardium
Left Ventricular Wall Stress, Geometry, and Remodeling in Myocardial Infarction
D’Elia N, et al. J Am Coll Cardiol Img 2015;8:1430–43
Velazquez EZ, et al. N Engl J Med 2016;374:1511-20
The STICH Extension Study: CABG in Patients with LV Systolic Dysfunction /Long-Term
Outcomes Outcomes
The median duration of follow-up, including the current extended-follow-up study, was 9.8 years.
Impact of Revascularization on Survival in Patients With HFpEF With
CAD
Hwang SJ, et al. J Am Coll Cardiol 2014; 63 :2817–27
Long-term Outcomes with EES vs. CABG in the Propensity Score Matched Cohort
Bangalore S, et al. Circulation 2016, in press
Pts with multivessel CAD and LVEF≤35% who underwent either PCI with everolimus-eluting stent (EES) or CABG selected from New York registries. Primary outcome was all-cause death. Secondary outcomes were MI, stroke and repeat revascularization. Among pts who fulfilled inclusion criteria (1,351 EES and 3,265 CABG), propensity score matching identified 2,126 pts with similar propensity scores.
Two-Year Outcomes of Surgical Treatmentof Moderate Ischemic Mitral Regurgitation
301 patients randomly assigned to undergo either CABG alone or CABG plus mitral valve repair. Patients were followed for 2 years for clinical and echocardiographic outcomes.
Michler RE, et al. N Engl J Med 2016;374:1932-41
Two-Year Outcomes of Surgical Treatmentof Severe Ischemic Mitral Regurgitation
251 patients randomly assigned to mitral-valve repair or replacement. Patients were followed for 2 years, and clinical and echocardiographic outcomes were assessed
Goldstein D, et al. N Engl J Med 2016;374:344-53
Pathophysiological Targets of Differing Imaging Modalities
Schuster A, et al. J Am Coll Cardiol 2012;59:359–70
Magnetic Resonance Imaging in Myocardial Infarction
Marra MP, et al. European Heart Journal 2011; 32: 284–293
Algorithm for the Assessment of Myocardial Viability using
CMR
Nagel E, Schuster A. JACC Cardiovasc Imaging 2012;5:509–12
Positron Emission Tomography and Recovery Following Revascularization-2 (PARR-2) Study
Beanlands RSB, J Am Coll Cardiol 2007;50:2002–12
The STICH Trial: Myocardial Viability and Survival in Ischemic Left Ventricular
Dysfunction
Bonow RO, et al. N Engl J Med 2011;364:1617-25
Among the 1212 patients enrolled in the randomized trial, 601 underwent assessment of myocardial viability. Of these patients, 298 were randomly assigned to receive medical therapy plus CABG and 303 to receive medical therapy alone. Median follow-up 5.1 years.
• Limitations of overall trial -Crossover in 17% of patients assigned to medical therapy and 9% of patients assigned to CABG -Randomization of a very small proportion of eligible patients -Average of only 2 patients per site per year at 127 sites in 26 countries over 5 years -Outcome of the large number of patients screened but not randomized not reported
• Lack of randomization in viability substudy
• Optional viability testing performed at clinician’s discretion
• Only about one-half of eligible patients from the main trial
• Significant differences in baseline characteristics between those with versus those without viability testing
• Nonsignificant trend toward higher rates of CABG among patients with viability testing on the day of randomization or on the following day than among those who had testing before randomization
• Acceptable viability tests do not have highest sensitivity or negative predictive value for identifying viable myocardium
• Binary classification of viability with controversial thresholds for extent and uptake
• Stress-induced ischemia not consistently addressed by viability testing
• Revascularization not guided by the presence of viable myocardium
• Small sample size of the group with nonviable myocardium
Limitations of the STICH Trial
Chareonthaitawee P, et al. J Am Coll Cardiol Img 2012;5:550-558
Myocardial Viability Testing and Impact of Revascularization
on Prognosis in CAD and LV Dysfunction: A Meta-Analysis24 viability studies reporting patient survival using thallium perfusion imaging, F-18 fluorodeoxyglucose metabolic imaging or dobutamine echocardiography. There were 3,088 patients (2,228 men), LVEF 32±8%, followed for 25±10 months.
Allman KC, et al. J Am Coll Cardiol 2002;39:1151– 8
Impact of Ischaemia and Scar on Therapeutic Benefit from Myocardial Revascularization vs. Medical therapy
13 969 pts who underwent adenosine or exercise stress SPECT myocardial perfusion scintigraphy (MPS) were identified. The percent myocardium ischaemic (%I) and fixed (%F) were calculated using 5 point/20-segment MPS scoring. Pts lost to follow-up (2.8%) excluded leaving 13 555 patients [35% with history of known coronary artery disease (CAD), 65% exercise stress, 61% male, age 66+12]. Follow-up was performed at 12–18 months for early revascularization (n=1226) and at > 7 years for all-cause death (mean follow-up 8.7+3.3 years).
Hachamovitch R, et al. European Heart Journal 2011; 32, 1012–1024
No prior CAD Prior revascularization/No MI
Prior MI < 10% fixed defect
Therapeutic Benefit from Revascularization
in Patients With LV Systolic DysfunctionThe extent of perfusion defects and metabolism-perfusion mismatch was measured in 648 consecutive pts (age, 65±12 years; 23% women; mean LVEF, 31±12%) undergoing PET. Early revascularization was performed within 92 days of positron PET in 199 patients (33%). Follow-up time (2.8±1.2 years, 165 deaths) began at 92 days to avoid waiting-time bias.
Ling LF, et al. Circ Cardiovasc Imaging 2013;6:363-372
HM≈5% HM≈10%
HM≈15% HM≈20%
Ottawa-FIVE Substudy of the PARR 2 Trial
Included were pts with LV dysfunction and suspected CAD being considered for revascularization. The patients had been randomized in PARR 2 to PET-assisted management (group 1) or standard care (group 2) and had been enrolled in Ottawa after August 1, 2002 (the date that on-site 18F-FDG was initiated) (n = 111). The primary outcome was the composite endpoint of cardiac death, myocardial infarction, or cardiac rehospitalization within 1 y. Data were compared with the rest of PARR 2 (PET-assisted management [group 3] or standard care [group 4]).
Abraham A, et al. J Nucl Med 2010; 51:567–574
http://revived.lshtm.ac.uk, NCT01920048
REVascularisation for Ischaemic Ventricular Dysfunction- British Cardiovascular Intervention Society-2: REVIVED-BCIS-2 Trial
Alternative Imaging Modalities in Ischemic Heart Failure (AIMI-HF) IMAGE HF Project I-A
O’Meara et al. Trials 2013; 14:218
• Severe renal insufficiency • LVESVI < 79 ml/m2
• LVEF>28 % • Single vessel CAD • Significant (> 10%) scar • Limited functional capacity -6MWD < 300m -KCCQ Physical ability score ≤ 55
• Competent surgeon • Significant myocardial viability • Increased MI risk • Increased risk of SCD • Moderate/severe MR • LVESVI ≥ 79 ml/m2
• LVEF ≤ 27 % • Multivessel CAD • Preserved functional capacity -6MWD ≥ 300m -KCCQ Physical ability score ≥ 55
Modified from: Velazquez EJ, Bonow RO. J Am Coll Cardiol 2015;65:615–24 Anavekar, N.S. et al. J Am Coll Cardiol 2016;67:2874–87
Medical Treatment with or without Revascularization
• CAD is a contributing factor in approximately 50% cases of HF and adversely affects survival.
• Stunned and hibernating (viable) myocardium together with myocardial necrosis and scar tissue contribute to the development of LV remodelling and ischemic HF.
• The results of the STICH Extension Study support a significant benefit of CABG plus medical therapy over medical therapy among patients with ischemic HF and multivessel CAD.
• Although RCTs dispute the value of viability testing, several observational studies suggest that patients with viable myocardium may benefit after revascularization.
• Myocardial viability is one of the several factors to be considered in order to determine whether a patient with ischemic HF needs a revascularization procedure in addition to optimal medical treatment.
The STICH Trial: Kaplan-Meier Analysis of Mortality
Rates in Patients With Myocardial Viability
Bonow RO, et al. J Am Coll Cardiol Img 2015;8:1121–9
The STICH Trial: Kaplan-Meier Analysis of Mortality Rates in
Patients With Myocardial Viability in
3 Subgroups of ESVI
Bonow RO, et al. J Am Coll Cardiol Img 2015;8:1121–9
Anti-Inflammatory Therapy in Myocardial Infarction: Pre-Clinical
Evidence
Montecucco F, et al. European Heart Journal 2016; 37: 1268–1283
Velazquez EJ, Bonow RO. J Am Coll Cardiol 2015;65:615–24
Medical Treatment with or without Revascularization
Reasons viable myocardium may
not recover function following
revascularization
Pre-procedural factors
Post-procedural factors Post-procedural factors
Shah BN, et al. Eur Heart J 2013;34:1323–1334
15th Cardiology Congress of Northern Greece
Thessaloniki, May 26-28, 2016
Ischemic Heart Failure
Filippos Triposkiadis, MD, FESC, FACC Professor of Cardiology Director, Department of Cardiology Larissa University Hospital Larissa, Greece
Critical Determinants of Myocardial Infarction Injury
Montecucco F, et al. European Heart Journal 2016; 37: 1268–1283
The STICH Trial: Patients, Randomization, and Follow-up Between July 2002 and007, 1212 pts with an LVEF≤ 35% and CAD amenable to CABG were randomly assigned to medical therapy alone (n=602) or medical therapy plus CABG (n=610). The primary outcome was the rate of death from any cause. Major secondary outcomes included the rates of death from CV causes and of death from any cause or hospitalization for CV causes.
Velazquez EZ, et al. N Engl J Med 2011;364:1607-16
The STICH Trial: CABG in Patients with LV Systolic Dysfunction/Intermediate Subgroup
Analyses of Death from Any Cause
Spectrum of Myocardial Dysfunction in
Ischaemic Heart Failure
Shah BN, et al. Eur Heart J 2013;34:1323–1334
The STICH Trial: Myocardial Viability and Survival in Ischemic Left Ventricular
Dysfunction
Bonow RO, et al. N Engl J Med 2011;364:1617-25
Infarct Size Reduction by Pre- and Postconditioning
Zhao Z-Q, et al. Am J Physiol Heart Circ Physiol 2003;285:H579–H588
The STICH Trial: Extent of Viability and ESV Expressed as Continuous Variables
Bonow RO, et al. J Am Coll Cardiol Img 2015;8:1121–9
The Conditioning Stimulus and the Impact of Co-Morbidity and Drug
Therapies
Bell RM, et al. Basic Res Cardiol 2016; 111:41
Park M, et al. Am J Physiol Heart Circ Physiol 297:H785–H791
Apoptosis Predominates in Nonmyocytes in Heart Failure
The Heart Failure Revascularization Trial (HEART) Trial
Multicenter RCT, SRV (n=69) vs OMT (n=69) in persons with LVEF < 35% and CAD. Inclusionary prerequisite was ≥5 viable LV segments with reduced contractility using a 17-segment DSE model. Results: After a median follow-up of 59 (inter-quartile range: 33-63) months, there were 51 (37%) deaths; 25 (37%) in those assigned to the conservative strategy, and 26 (38%) in those assigned to the invasive strategy, 13 (29%) of whom had been revascularized. Limitations • Underpowered secondary to a relatively small sample size. • Primary modality of viability assessment was DSE (lower sensitivity for viability detection relative to other imaging
modalities) • Randomization had not occurred prior to viability assessment, therefore clouding the impact of viability assessment on
treatment outcomes . Cleland JG, et al. Eur J Heart Fail 2011;13:227-33
The PET and Recovery Following Revascularisation-2 (PARR-2) trial
Efficacy evaluation of perfusion FDG-mediated PET imaging in risk stratification and identification of patients (n=430, LVEF <35% and suspected or confirmed CAD) who would benefit most from SRV. Results At 1 year, the cumulative proportion of patients who had experienced the composite event (CV death, MI, or recurrent hospital stay for cardiac cause, within 1 year) was 30% (PET arm) versus 36% (standard arm) (relative risk 0.82, 95% confidence interval [CI] 0.59 to 1.14; p = 0.16). Limitations • Poor adherence to therapeutic strategy, with only 75% of participants treated accordingly to viability imaging.
Beanlands RSB, et al. J Am Coll Cardiol 2007;50:2002–12
The STICH Extension Study: CABG in Patients with LV Systolic Dysfunction/Long-Term
Subgroup Analyses of Death from Any Cause
Velazquez EZ, et al. N Engl J Med 2016;374:1511-20
The STICH Trial: Myocardial Viability and Survival in Ischemic Left Ventricular
Dysfunction
The comparison shown not adjusted for other prognostic baseline variables. After adjustment on multivariable analysis, the between-group difference was not significant (P = 0.21).
Bonow RO, et al. N Engl J Med 2011;364:1617-25
Among the 1212 patients enrolled in the randomized trial, 601 underwent assessment of myocardial viability. Of these patients, 298 were randomly assigned to receive medical therapy plus CABG and 303 to receive medical therapy alone. Median follow-up 5.1 years.
Temporal Trends in Ischemic Heart Disease Mortality
in 21 World Regions, 1980 to 2010 The Global Burden of Disease 2010 Study
Moran AE, et al. Circulation. 2014;129:1483-1492
Males Females
Endothelium
Cardiomyocytes
ONOO- NO
VCAM E-selectinROS
TGF-β
Fibroblasts Myofibroblasts
Leukocytes
Collagen
• IL-6 • TNF-α • sST2 • Pentraxin 3
Fpassive PKG
cGMP
sGC
Hypertrophy
A Novel Paradigm for HFpEF: Comorbidities Drive Myocardial Dysfunction and Remodeling Through Coronary Microvascular Endothelial Inflammation
Paulus WJ, Tschoepe C. JACC 2013; 62:263-71
• Hypertension • Overweight/Obesity • Diabetes Mellitus • Kidney disease • Iron deficiency • COPD
Endothelium
Cardiomyocytes
Myocardial Remodeling in HFREF
Paulus WJ, Tschoepe C. JACC 2013; 62:263-71
Autophagy Apoptosis Necrosis
Collagen
ROS
• Ischemia • Infection • Toxicity
Positive and Negative Arterial Remodelling Influences the Consequences of Atherosclerosis
Heusch G, et al Lancet 2014; 383(9932): 1933–1943
Heusch G, et al. Circulation 2009; 120:1822–1836
Role of Microembolisation in Coronary Vascular Remodelling
Enrolment and Outcomes in the STICH Trial
Jones RH, et al. N Engl J Med 2009;360:1705-17
Velazquez EZ, et al. N Engl J Med 2011;364:1607-16
Bonow RO, et al. N Engl J Med 2011;364:1617-25
HYPOTHESIS 1 HYPOTHESIS 2
Viability Sub-study (n=601)
Main trial (n=1212)
Interactions of end-systolic volume index (ESVI), myocardial viability, and treatment with respect to survival were assessed in patients in the prospective randomized STICH (Comparison of Surgical and Medical Treatment for Congestive Heart Failure and Coronary Artery Disease) trial of CABG versus medical therapy who underwent viability assessment (n = 601; age 61 9 years; ejection fraction #35%), with a median follow-up of 5.1 years.
The STICH Trial: Severity of Remodeling, Myocardial Viability, and Survival
Bonow RO, et al. J Am Coll Cardiol Img 2015;8:1121–9
Optimal Healing Post Myocardial Infarction
Francis Stuart SD, et al. Journal of Molecular and Cellular Cardiology 2016; 91: 114–122
The STICH Trial: Myocardial Viability and Survival in Ischemic Left Ventricular
Dysfunction
The comparison shown not adjusted for other prognostic baseline variables. After adjustment on multivariable analysis, the between-group difference was not significant (P = 0.21).
Bonow RO, et al. N Engl J Med 2011;364:1617-25
Among the 1212 patients enrolled in the randomized trial, 601 underwent assessment of myocardial viability. Of these patients, 298 were randomly assigned to receive medical therapy plus CABG and 303 to receive medical therapy alone.
Prognostic Significance of Biomarkers in Patients With CAD and LV Dysfunction: STICH HYPOTHESIS
1
Feldman AM, et al. Circ Heart Fail 2013;6:461-472
Biphasic Monocyte Response During Early Myocardial Remodeling
Swirski FK, Nahrendorf M. Science 2013 ; 339(6116): 161–166
Prognostic Significance of Biomarkers in Patients With CAD and LV Dysfunction: STICH HYPOTHESIS
2
Feldman AM, et al. Circ Heart Fail 2013;6:461-472
Ischaemia/Reperfusion Injury and the Different Forms of Cell Death
Bell RM, et al. Basic Res Cardiol 2016; 111:41
Wu E, et al. Heart 2008;94:730–6
Relationship Between Initial Infarct Size (% LV Mass) and Subsequent Change in LVEDV
Index
Impact of Revascularization on Longitudinal Changes in LVEF in
HFpEF
Hwang SJ, et al. J Am Coll Cardiol 2014; 63 :2817–27
Relationship Between Baseline LVEF and Subsequent Change in LVESV and LVEDV
Schächinger V, et al. Eur J Heart Fail 2009;11:973–9