Ekg Cases 7 15 09 Level 2 Part 1
-
Upload
michael-lacombe -
Category
Business
-
view
5.774 -
download
2
description
Transcript of Ekg Cases 7 15 09 Level 2 Part 1

Case-oriented EKG’s(level 2- less easy)
MDFMR/UNECOMJuly 15, 2009M. LaCombe

By Way of Review:

The normal EKG waveform

A normal EKG

The frontal plane (QRS) axis:

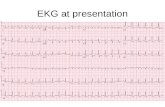
Let’s take a moment to review the steps you should follow every time you read an ECG.
Try to get into the habit of following the steps in the same order each time:1. Check the standardization and quality of the ECG (The usual calibration is 25 mm/sec and 10mm/mV)2. Calculate the heart rate3. Analyze the rhythm (Is it sinus; sinus plus ectopic beats; or some entirely non-sinus mechanism such as atrial fibrillation, ventricular tachycardia or a junctional escape rhythm?)4. Check the PR interval5. Check the P wave size6. Check the QRS width7. Check the QT interval8. Check the mean QRS electrical axis9. Check the QRS voltage10. Check the R wave progression in the chest leads11. Look for abnormal Q waves12. Look for ST segment abnormalities13. Look for T wave abnormalities14. Look for prominent U waves

Case #26:
21-year-old female with a history of "seizure"
disorder. She is on no medications and her
electrolytes are normal.


Dx: Congenital long QT syndrome. The ECG demonstrates a prolonged QT interval of 0.6 seconds. Note the broad T waves with notching (or
possibly U waves) in the precordial leads. This characteristic may identify patients with long QT syndrome at increased risk for
torsade de pointes and syncope and sudden death. Patients at high risk
of recurrent syncope or sudden death are usually considered for
implantable cardioverter defibrillator therapy along with
beta-blockade. A number of different "channelopathies" have
been identified in the pathogenesis of congenital long QT syndrome. (Ref: Kass RS, Moss AJ. Long QT
syndrome: J Clin Invest 2003;112:810-5.)

Case #27:18-year-old pre-op ECG for
knee surgery

Limb lead reversal.
The left and right arm leads are reversed. The clue is inversion of the P wave and QRS complex
in lead I. Whenever you see a negative P wave and QRS complex in lead I the likely diagnosis is limb lead reversal. Dextrocardia is another
possibility, but in dextrocardia there is loss of R wave progression in the left chest leads which is not seen in this tracing. Another clue is the
dissimilarity of the morphology of the QRS complexes in lead I and V6. (The variability in
heart rate here is due to respiratory sinus arrhythmia, a physiologic finding that is most
apparent in younger healthy subjects.)

Case #28: 85-year-old male without symptoms on no significant cardiac
medications. What is the diagnosis and does it necessitate a pacemaker?

Sinus rhythm with 2:1 AV heart block.
The ECG shows a bradyarrhythmia with non-conducted sinus P waves alternating with normally conducted P waves. It is not possible to reliably identify the
point of block (nodal vs. infranodal) from this single ECG with 2:1 conduction. There is no evidence of acute inferior ischemia, either. The site of block could be proximal (in the AV node) or more distal, in the His-
Purkinje system. In general, with 2:1 block, involvement of the AV node is favored by a narrow QRS complex and a prolonged PR interval, or by the presence of intermittent AV Wenckebach. Block (nfranodal) in the His-Purkinje system would be favored by a concomitant bundle branch block and/or with a PR interval of 160 ms or less. A possibly useful bedside diagnostic test for chronic 2:1 block (in the absence of active ischemia) would be to increase the sinus rate (mild exercise). A resumption of 1:1 conduction favors AV node block while worsening of block strongly favors infranodal disease. Pacemaker placement is indicated for symptomatic 2:1 block without reversible cause (e.g., drug effect) and generally for asymptomatic 2:1 block due to infranodal disease. Intracardiac His bundle electrogram would
definitively identify the site of block. This patient had intermittent 3:2 AV Wenckebach at other times, and
then resumed 1:1 conduction on subsequent ECGs, consistent with AV node disease..

Case #29:49-year-old woman having palpitations.

AV nodal reentrant tachycardia (AVNRT).
This tracing demonstrates a REGULAR narrow complex tachycardia at a rate of 150. The differential diagnosis of this supraventricular tachycardia
includes: sinus tachycardia, AVNRT, automatic atrial tachycardia, atrio-ventricular reentrant tachycardia
(AVRT), involving retrograde conduction over a "concealed" bypass tract, or atrial flutter with 2:1 block. If P waves can be located it can be helpful in determining the mechanism of the tachycardia. In this tracing P waves can be located at the end of the QRS in lead II and aVF, producing a "pseudo S" wave. Absence of P waves or a "pseudo S" pattern in II, III, or aVF, or a "pseudo R prime" pattern in V1 is characteristic of AVNRT due to near simultaneous activation of the atrium and the ventricle from the AV node. If the
diagnosis is still in doubt, adenosine may be useful in slowing conduction in the AV node. Reentrant rhythms (AVNRT or AVRT) may "break" abruptly, converting to sinus; the ventricular response of other atrial
tachcyardia or atrial flutter will slow often revealing underlying atrial activity. (Note: the final wide
complex waveform is either an artifact or a ventricular premature beat.)

Case #30:The patient is an elderly man who presented to the emergency ward with dizziness and new renal
failure

Dx: Hyperkalemia (7.6 mEq/L) secondary to renal failure.
The ECG demonstrates findings consistent with severe hyperkalemia -- most importantly marked
widening of the QRS complex. The QRS complex here shows a left bundle branch block (LBBB)
morphology with left axis deviation. However, the QRS duration (about 240 ms) is much wider than seen with an "uncomplicated" LBBB or just with left anterior fascicular block due to intrinsic conduction disease. There is also peaking of the T waves with prolongation of the PR interval and flattening of the P waves. If the hyperkalemia is
left untreated, the ECG will progress to a sinusoidal pattern and eventually asystole with
subsequent hemodynamic collapse and death.

Case #31:60-yr-old female with a history of anti-
phospholipid syndrome who presented with chest pain.

Sinus rhythm with AV Wenckebach with 4:3 conduction in the setting of an acute inferior wall infarction. The ECG
demonstrates Q waves and ST elevation in leads 2, 3, and aVF. There are also reciprocal ST segment depressions in leads 1, aVL and V2-3. The rhythm is
Wenckebach showing progressive prolongation of the PR intervals,
shortening of the R-R intervals and block of every fourth P wave. The presence of "group" beating is easily recognized and characteristic of Wenckebach and is often associated with high vagal tone or nodal ischemia in the setting of an inferior wall myocardial infraction (MI). The block is at the level of the AV node.

Wait! Not so fast!
What is the anti-phospholipid antibody
syndrome?

Antiphospholipid syndrome (APS) is a disorder characterized by recurrent venous or arterial thrombosis
and/or fetal losses associated with typical laboratory abnormalities. These include persistently elevated levels
of antibodies directed against membrane anionic phospholipids (ie, anticardiolipin [aCL] antibody,
antiphosphatidylserine) or their associated plasma proteins, predominantly beta-2 glycoprotein I (apolipoprotein H), or evidence of a circulating
anticoagulant.Multiple terms exist for APS. Unfortunately, some synonyms can be confusing. Lupus anticoagulant
(LA) syndrome, for example, is misleading because patients may not necessarily have systemic lupus
erythematosus (SLE) and LA is associated with thrombotic rather than hemorrhagic complications. In an attempt to avoid further confusion, APS is the currently preferred
term for the clinical syndrome (as described below).APS can occur in patients without evidence of any definable associated disease (primary APS). It may also occur in
association with SLE or another rheumatic or autoimmune disorder (secondary APS). Although antiphospholipid
(aPL) antibodies are clinically linked to APS, whether they are involved in the pathogenesis or are an
epiphenomenon is unclear. (aPL antibodies are known to occur in up to 5% of healthy individuals.)

Case #32: 79-year-old woman with shortness of breath requiring intubation.

Atrial fibrillation with a rapid ventricular response. Right axis
deviation. Intraventricular conduction delay. Right ventricular hypertrophy (RVH). This patient has
severe mitral stenosis with pulmonary congestion, pulmonary hypertension, and right heart
failure. A qR in lead V1 is one of the most specific signs for right ventricular hypertrophy. Other causes of a qR in V1 include a
right bundle branch block (RBBB) in patients with an anterior
myocardial infarction or normal patients who have a QS in V1 and subsequently develop a RBBB. This patient has right axis deviation in
addition to the qR in V1 which suggests RVH.

Given atrial fibrillation and RVH one should strongly consider mitral stenosis. Additional note on differentiating right
ventricular hypertrophy (RVH) from lateral MI: In some cases of severe (RVH) with marked right axis deviation, leads I and aVL may show rS or even QS waves,
simulating lateral MI. In this case, lead V1 notably shows a narrow qR complex (not just a tall R wave) strongly suggestive of RVH, rather than posterior-lateral MI. Also, the lateral precordial leads here show rS type complexes, not QR waves.
Physical examination, echocardiogram and other imaging modalities also provide important information about RVH vs. lateral MI in cases where the ECG is
ambiguous.

Major Segues:
Homework Assignments

Who is Diana Prince?

Yes, Wonder Woman’s alter-ego

Who is Linda Danvers?

Supergirl’s secret identity

What is Hestia chiefly noted for?

Wonder Woman’s Lasso of Truth receives its power from the Fires of Hestia

What is Ondine’s Curse?

Congenital Central Hypoventilation Syndrome

Which 3rd year resident lived here?

Gretchen Andrews, who taught an Outward Bound course on Hurricane Island

Name one member of the band Circle of Willis.

Dan Gibbons

Who goes by Red, plays the saxaphone, and likes Ursula Le Guin?

Selma Holden

Case #33:58-year-old man with chest pain.

The ECG reveals an acute anteroseptal myocardial infarction
(MI) in the setting of a (preexisting) right bundle branch block (RBBB). This is a dramatic example of the fact that ischemia
and infarction can still be diagnosed, even in the setting of conduction abnormalities. The
anterior precordial leads reveal a qR pattern (analagous to an RSR'
with the R replaced by a pathologic Q), marked ST elevation, and
upright T waves. This pattern is essentially pathognomonic for an
acute infarction.

Three points are worth making with regard to a RBBB:
1) Secondary T wave inversions are typically seen in the right precordial
leads (only in those leads with a terminal R'). Upright T waves in such leads might indicate ischemia, etc. T
wave inversions in leads with no terminal R' might also be ischemic.
2) ST elevations are not normally seen in RBBB.
3) Right precordial Q waves may be seen in RBBB without an infarct (especially in the setting of acute right ventricular
overload), but if the Q waves extend past V2 or if they are slurred or wide, they suggest pathology. Bottom Line: Bundle branch block, especially RBBB does not
render the ECG uninterpretable!!

First Aside:
How can we diagnose an acute infarction in the presence of a
bundle branch block?
(this is level 4 stuff, but now you are
ready for it)

Recognition of a myocardial infarction in the presence of RBBB is feasible, since
the former deforms the initial part of QRS, and the latter alters only the late part of the QRS. Thus, Q waves in inferior leads
suggest an inferior myocardial infarction, while Q waves in precordial and lateral
leads are due to myocardial infarctions in these two territories. PMI is cited as the
single exception, since it is thought to affect the terminal part of the QRS
complex and thus it is masked by RBBB. Normally the posterior/basal myocardial region is the last to be depolarized, and
consequently the PMI is expected to deform the late part of QRS, rather than to
generate early QRS abnormalities.

RBBB With Primary ST-T Wave AbnormalitiesRBBB is recognized by 1) rR' in V1; 2) QRS duration >0.12s; 3) terminal QRS forces oriented rightwards and anterior. In RBBB
the ST-T waves should be oriented opposite to the terminal QRS forces. In this example there are "primary ST-T wave
abnormalities" in leads I, II, aVL, V5, V6. In these leads the ST-T orientation is in the same direction as the terminal QRS forces.


RBBB and Inferior MI
Note the developing Q’s in II, III, AVF

Pathologic Q waves are seen in leads II, III, aVF (inferior MI) and in leads V1-3 (anteroseptal MI). RBBB is recognized by the wide QRS (>0.12s)
and the anterior/rightwards orientation of terminal QRS forces. When an anteroseptal MI
complicates RBBB (or visa versa) the rSR' complex in V1 (typical of RBBB) becomes a qR
complex.

Anteroseptal MI With RBBB: Precordial Leads

Deep Q waves in II, III, aVF plus tall R waves in V1-2 are evidence for this infero-posterior MI. The wide QRS
(>0.12s) and RR' complex in V1 are evidence for RBBB. Any time RBBB has an initial R in V1 equal to or greater
than the R', true posterior MI must be considered. Q waves in V5-6 suggest an apical lateral wall extension of this
large MI.

Infero-posterior MI with RBBB
This is an unusual RBBB because the initial R wave is taller than the R' wave in lead V1. This is the clue for true
posterior MI. The tall initial R wave in V1 is a "pathologic R" wave analagous to the "pathologic Q" wave of an anterior
MI.

RBBB and Posterior MI

Another TPMI in presence of RBBB

As for LBBB and acute myocardial infarctions
on EKG...

Three electrocardiographic criteria were found to have independent value in the
diagnosis of acute infarction in the presence of left bundle-branch block:
ST-segment elevation equal to or greater than 1 mm in the presence of a positive
QRS complex;
ST-segment depression equal to or greater than 1 mm in lead V1, V2, or V3;
and ST-segment elevation equal to or greater than 5 mm in the presence of a
negative QRS complex.

The ‘old’ criteria

Flow Chart for the Prediction of Acute Myocardial Infarction in the Presence of Left Bundle-Branch Block, with the Use of All Possible Combinations of the Three Independent
Electrocardiographic Criteria

...so here is LBBB with no
injury...

Electrocardiogram Meeting All Three Independent Criteria for the Diagnosis of Acute Myocardial Infarction in a Patient from the GUSTO Trial with left bundle-Branch Block.The electrocardiogram shows ST-segment elevation of at least 1 mm that is concordant with the QRS complex (lead II),
ST-segment depression of at least 1 mm in leads V2 and V3, and ST-segment elevation of at least 5 mm that is discordant with the QRS complex (leads III and aVF)
(You are now in possession of the worst EKGtracing in medical history)

Acute myocardial infarction in the presence of left bundle branch blockFeatures suggesting acute MI•ST changes in the same direction as the QRS (as shown here)•ST elevation more than you'd expect from LBBB alone (e.g. > 5 mm in leads V1 - 3)•Q waves in two consecutive lateral leads (indicating anteroseptal MI)

LBBB with lateral wall infarct:
note the Q’s in I, AVL

Atypical LBBB with Primary T Wave Abnormalities
Primary T wave abnormalities in LBBB refer to T waves in the same direction as the major deflection of the QRS.
These are seen in leads I, III, aVL, V2-4. Most likely diagnosis is myocardial infarction.