DIS News - health.umt.eduhealth.umt.edu/pharmacypractice/Alum and Prac/DIS/Sept 2015.pdfCommon side...
Transcript of DIS News - health.umt.eduhealth.umt.edu/pharmacypractice/Alum and Prac/DIS/Sept 2015.pdfCommon side...

PATIENT INFORMATION:
Swimmer’s Itch
What is Swimmer’s Itch?
Swimmer’s itch is a rash that appears as red,
itchy bumps on the skin after swimming. It
can occur hours or days after someone has
been swimming in certain bodies of water,
such as lakes. Swimmer’s itch is caused by
the human body’s reaction to a parasite that
lives in the water. The parasite does not sur-
vive in humans, and the rash will clear up
within a couple of weeks.
Who is at Risk for Swimmer’s Itch?
Anyone who swims in non-chlorinated water
that is home to large groups of birds (such as
ducks or gulls) and a specific type of snail is at
risk. The parasite lives in shallow shore areas
with warmer water temperatures. Water
known to be a source of the parasite will often
have signs posted by public health officials to
warn swimmers of the risk.
How to Prevent Swimmer’s Itch
Avoid water that is known to contain the para-
site. If you don’t know if the water contains
the parasite, rinse with clean water or towel
off immediately after exiting the water.
How to Treat Swimmer’s Itch
Treatment is focused on relieving the discom-
fort caused by swimmer’s itch. It is very im-
portant not to scratch the rash to avoid an in-
fection.1
Cold compresses can be applied to affect-
ed areas.
Colloidal oatmeal or Epsom salt baths can
relieve discomfort. Use lukewarm (not
hot) water in the bath.
Baking soda and water can be mixed into
a paste and applied to the itchy skin.
Topical anti-itch creams or lotions (such
as calamine) are available over-the-
counter.
Volume 19, Issue 9
September 2015
We welcome any comments
and suggestions for future
newsletter topics.
Editors in Chief:
Sherrill Brown, DVM, Pharm.D, BCPS
Micah Miller, PharmD
Patient Information: PCSK9 Inhibitors
2
Savaysa™ 3
Patient Information: Mirena® IUD
5
Patient Information: Belsomra®
6
Inside this issue:
DIS News Col lege of Heal th Professions and Biomedica l Sc iences
Drug Informa tion Service
Topical steroid creams are also available
over-the-counter. Use with caution on large
areas in children for extended periods.
When to Contact Your Medical Provider
Talk to your medical provider if the rash skin
does not improve or if it worsens after 3 days of
treatment. If signs of infection (fever, pus,
swelling) develop, contact your medical provider
as soon as possible.
By Kaylyn DesRosier, PharmD Candidate
REFERENCES:
1. Swimmer’s itch FAQs (1/10/2012). CDC
Web site. Available at: http://
www.cdc.gov/parasites/
swimmersitch/faqs.html. Accessed Septem-
ber 8, 2015.
2. Swimmer’s itch (n.d.). American Osteo-
pathic College of Dermatology Web Site.
Available at: http://www.aocd.org/?
page=SwimmersItch. Accessed September
8, 2015.

Nearly 73 million Americans have hy-
percholesterolemia (high cholesterol), a
condition which can double the risk of
heart disease. Less than one-third of
people with high cholesterol have their
low-density lipoprotein (LDL), or bad
cholesterol, well managed. For years,
the standard of therapy has been the
statins, which include Lipitor®
(atorvastatin) and Crestor®
(rosuvastatin). Unfortunately, a disease
called familial hypercholesterolemia
results in highly elevated LDL and re-
sistance to statin therapy for a small
group of patients. Recently, a new class
of drugs called the PCSK9 inhibitors
were approved by the FDA to help treat
this condition. Two drugs, Repatha™
(evolocumab) and Praluent®
(alirocumab), are currently available.
Who may benefit from the PCSK9
inhibitors?
Both Praluent® and Repatha™ are used
as add-on therapy to diet and maximally
tolerated statin therapy in patients with
clinical cardiovascular disease or hetero-
zygous hypercholesterolemia, when
LDL reduction has not been successful
with previous treatments.
Who should not take a PCSK9 inhibi-
tor?
Patients who have had severe hypersen-
sitivity or anaphylactic allergic reactions
to either Praluent® or Repatha™ should
not take these medications.
Which conditions should I tell my doc-
tor about before I start a PCSK9 in-
hibitor?
Prior to starting a PCSK9 inhibitor, tell
your provider if you have a latex allergy,
are pregnant or planning to become
pregnant, or are breastfeeding. The nee-
dle cover of Repatha™ contains dry nat-
ural rubber, so an allergic reaction to
latex may occur. Latex allergies are not
a concern with Praluent®. Though signif-
icant drug interactions have not been
identified with either drug, inform your
doctor about all of your prescription and
over-the-counter medications and sup-
plements.
What are adverse events may occur
while taking PCSK9 inhibitors?
Common side effects include upper res-
piratory infections, influenza, injection
site reactions, muscle pain, urinary tract
infections, and diarrhea.
How do I take my PCSK9 inhibitor?
Both Praluent® and Repatha™ are
administered by the patient as sub-
cutaneous injections into the abdo-
men, thigh, or upper-arm.
Each injection needs to warm up to
room temperature for 30 minutes
prior to administration.
Rotate injection sites.
Repatha™ is given either every two
weeks (140 mg dose) or once a
month (420 mg dose). The once-
monthly 420 mg dose is given as
three 140 mg injections within 30
minutes. Each injection is with a
new syringe or auto-injector.
Praluent® is given every two weeks
and is available in 75 mg and 150
mg doses.
How do I store my PCSK9 inhibitor?
Protect both medications from light
exposure.
Store both medications in the refrig-
Page 2 DIS News
erator at 36-46° F.
Do NOT allow either medication
to freeze or be exposed to temper-
atures above 77° F.
Praluent® should not be exposed
to room temperature (77° F) for
more than 24 hours.
Repatha™ may be kept at room
temperature for up to 30 days.
How much do PCSK9 inhibitors
cost?
Praluent® is estimated to cost $14,600
annually, or $560 per injection. Re-
patha™ has an annual cost of $14,100,
or $542.31 per injection. Although
copays are determined by individual
insurance companies, both drugs have
copay assistance programs.
The patient assistance program for
Repatha™ allows eligible patients cov-
ered by non-government insurance
programs to pay no more than $5 for
each prescription refill.
Praluent® patient support allows eligi-
ble patients with commercial insurance
to receive the first 6 months of therapy
for a $0 copay. After the first 6
months, the copay becomes $10. As-
sistance for eligible patients without
insurance provides 12 months of
Praluent® free of charge.
By Matt Slagle, PharmD Candidate
PATIENT INFORMATION: PCSK9 Inhibitors: New Big Guns in the Arsenal Against High Cholesterol
References on Page 4
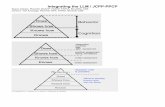
Cholesterol Reductions in Heterozygous Familial Hypercholesterolemia with the PCSK9 Inhibitors
LDL Reduction (%) Total Cholesterol Reduction (%)
Repatha™ (evolocumab) 61-71% 38-42%
Praluent® (alirocumab) 58% 36%
What is the reduction in cholesterol with PCSK9 inhibitors?

Volume 19, Issue 9 Page 3
Savaysa™ (edoxaban) is a new antico-
agulant agent approved in January 2015
by the FDA1
Routine coagulation monitoring is not
needed because edoxaban is a factor Xa
(FXa) inhibitor2-5
Edoxaban is indicated for stroke pre-
vention in nonvalvular atrial fibrillation,
deep vein thrombosis (DVT), and pul-
monary embolism (PE)2
Edoxaban can also be used prophylacti-
cally for postoperative DVT prevention
in patients undergoing total knee arthro-
plasty2
Dosing:
The typical adult dose of edoxaban is 60 mg
by mouth daily for atrial fibrillation, DVT,
and PE.2 Dosing for other different indica-
tions is described in Table 1.
Dose adjustments for creatinine clearance:
>95 mL/min: do not use in patients
with atrial fibrillation due to increased
risk of ischemic stroke
15-50 mL/min: reduce dose to 30 mg
daily
<15 mL/min: not recommended
Patients with hepatic impairment:
Not recommended for patients with
Child-Pugh score B or C
Patients with low body weight (≤60 kg):
Reduce dose to 30 mg daily
Drug Interactions:
Edoxaban is a p-glycoprotein substrate and
can interact with other drugs that use the p-
glycoprotein transport system. These drugs
include azithromycin, clarithromycin, keto-
conazole, and verapamil.2,6 In patients with
a DVT or PE who are taking other drugs that
are p-glycoprotein substrates, the edoxaban
dose should be reduced to 30 mg daily.2,4,5
Unlike rivaroxaban and apixaban, edoxaban
does not interact with cytochrome P450 en-
zymes. This makes edoxaban a good alter-
Savaysa™ (edoxaban)
native for patients on many medica-
tions.2,5 See Table 2 (page 4) for a phar-
macokinetic comparison of anticoagulant
agents.
Adverse Effects:
Bleeding, including in mouth, phar-
ynx, gastrointestinal tract, and skin
Rash
Abnormal liver function tests
Edoxaban Compared to Warfarin:
Edoxaban is comparable in efficacy and
safety to warfarin, the oldest anticoagu-
lant agent.3-6 Warfarin has its peak effect
within four to five days. This time
frame, along with its many drug interac-
tions, make warfarin dosing difficult.
For this reason, coagulation monitoring
of INR is crucial for patient safety and
efficacy.2
Unlike warfarin, edoxaban has fewer
drug interactions. Instead of 4-5 days,
edoxaban reaches its peak effect in ap-
proximately one to two hours. Fewer
interactions and a shorter time to peak
effect makes monitoring less crucial with
edoxaban. However, edoxaban’s half-
life is much shorter than warfarin’s, so
compliance is an important topic to dis-
cuss with patients before starting edoxa-
ban. See Table 3 (page 4) for infor-
mation on switching patients between
edoxaban and warfarin.3,5
Edoxaban was non-inferior to warfarin in
a major study.3,4 The ENGAGE AF-
TIMI 48 study focused on individuals
with moderate-to-high risk atrial fibril-
lation. Primary endpoints included all-
cause stroke events, systemic embo-
lism, and mortality. This study also
looked at safety related to increased
bleeding risk.3,4
In this randomized, double-blind, dou-
ble-dummy trial, 21105 patients were
given either warfarin adjusted to INR
2.0-3.0, edoxaban 60 mg daily, or
edoxaban 30 mg daily. Stroke or sys-
temic embolic events per year were
decreased with edoxaban 60 mg com-
pared to warfarin (1.18% vs. 1.50%).
According to the study results, 197
people need to be treated with edoxa-
ban 60 mg daily instead of warfarin to
prevent one stroke or systemic embolic
event per year. The incidence of major
bleeds was also reduced in patients
treated with edoxaban compared to
patients treated with warfarin.3,4
By Ka Zoua Moua, PharmD Candi-date
Continued on Page 5
Table 1: Edoxaban Dosing
References and Tables on Page 4

Volume 19, Issue 9 Page 4
1. High cholesterol facts (3/17/2015). CDC
Web site. Available at: http://www.cdc.go
v/cholesterol/facts.htm. Accessed Septem-
ber 7, 2015.
2. Weinrauch LA. Familial hypercholesterol-
emia (5/20/2014). Medline Plus Web site.
Available at: https://www.nlm.nih.gov/
medlineplus/ency/article/000392.htm.
Accessed September 7, 2015.
3. Repatha [package insert and patient infor-
mation]. Thousand Oaks, CA: Amgen
Inc.; 2015 August.
4. Praluent [package insert]. Bridgewater,
NJ: Sanofi-Aventis U.S. LLC; 2015 July.
5. Pollack A. New drug sharply lowers cho-
lesterol, but it’s costly (7/24/2015). New
York Times Web site. Available at: http://
www.nytimes.com/2015/07/25/business/
us-approves-drug-that-can-sharply-lower-
Edoxaban (from page 3)
cholesterol-levels.html. Accessed Sep-
tember 7, 2015.
6. Davis K, Hawkins T, Sood A. FDA
approves Amgen’s new cholesterol-
lowering medication Repatha
(evolocumab) (8/27/2015). Amgen
Web site. Available at: http://ww
w.amgen.com/media/media_pr_deta
il.jsp?releaseID=2082837. Accessed
September 7, 2015.
7. Patient assistance and support services
(2015). Repatha Web site. Available
at: https://www.rep atha.com/patient-
services-and-copay-registration/. Ac-
cessed September 9, 2015.
8. Patient support(2015). Praluent Web
site. Available at: https://www.pra
luenthcp.com/cost-support. Accessed
September 9, 2015.
REFERENCES:
1. FDA approves anti-clotting drug Savaysa (1/8/2015). FDA Web site. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm429523.htm. Accessed August 10, 2015.
2. Micromedex® Healthcare Series [internet database]. Greenwood Village, Colo: Truven Health Ana-lytics, 2015. www.micromedexsolutions.com. Accessed August 10, 2015.
3. Giugliano RP, Ruff CT, Braunwalk E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. New Engl J Med 2013;369(22):2093-2104.
4. Ruff CT, Giugliano RP, Braunwalkd E, et al. Association between edox-aban dose, concentration, anti-factor Xa activity, and outcomes: an analysis of data from the ran-domized, double-blind ENGAGE AF-TIMI 48 trial. Lancet 2015;385:2288-2295.
5. Niebecker R, Jonsson S, Karisson MO, et al. Population pharmacoki-netics of edoxaban in patients with symptomatic deep-vein throm-bosis and/or pulmonary embo-lism—the Hokusai-VTE phase 3 study. Br J Clin Pharmacol 2015; 80(6):1374-1387.
6. Lip GYH, Merino J, Ezekowitz M, et al. A prospective evaluation of edoxaban compared to warfarin in subjects undergoing cardioversion of atrial fibrillation: the edoxaban vs. warfarin in subjects undergoing cardioversion of atrial fibrillation (ENSURE-AF) study. Am Heart J 2015;169:597-604.e5.
Warfarin → Edoxaban Discontinue warfarin
Start edoxaban when INR is ≤2.5
Edoxaban → Warfarin Decrease edoxaban dose by 50% and start warfarin
Discontinue edoxaban when INR is stable (≥2) Monitor INR at least weekly once on warfarin therapy
Edoxaban → Warfarin
(With Parenteral
Bridge)
Discontinue edoxaban and start warfarin and parenteral
anticoagulant at next scheduled edoxaban dose Discontinue parenteral anticoagulant once INR is stable (≥2)
Table 2: Anticoagulant Comparison
Table 3: Switching between Warfarin and Edoxaban
PCSK9 Inhibitors References (from page 2)

Volume 19, Issue 9 Page 5
The Mirena® (levonorgestrel) intrauterine
device (IUD) is used for up to 5 years of
contraception and is 99% effective. Mire-
na® is also FDA approved to treat menor-
rhagia.
Mirena® contains synthetic progestin that
inhibits pregnancy by:
Slowing the transport of the sperm
Preventing the implantation of a ferti-
lized egg
Do not use Mirena® if you are pregnant or if
you have any of the following conditions:
Pelvic Inflammatory Disease (PID) or
history of PID
Cervical or uterine cancer
Breast cancer or other progestin sensi-
tive cancer
History of pelvic infections
Hypersensitivity to levonorgestrel or
any component of the IUD
Liver cancer or disease
Precautions:
If pregnancy occurs, IUD must be re-
moved
Bleeding patterns may change and be-
come irregular or amenorrhea (absence
of menstrual bleeding) may occur
Expulsion of IUD may occur
PATIENT INFORMATION:
Mirena® (levonorgestrel) IUD
Adverse Effects:
Bacterial Vaginitis (13.6%)
Vaginal Candidiasis (13.3%)
Acne (12.3%)
Headache (9.8%)
Nausea/Vomiting (7.9%)
Abdominal discomfort or pain
(6.1%)
Pelvic discomfort or pain (6.1%)
Depression (5.4%)
After Mirena® is inserted, your provider
will want to do an exam 4-6 weeks later
and every year while the IUD is in place.
Mirena® was highly effective for up to 3
years in one study. The Mirena® IUD
was associated with a low occurrence of
side effects. Expulsion of the IUD with-
in the first year after placement occurred
in 3.5% of women in the study. Pelvic
infections were not more common in the
first 20 days after IUD insertion. In the
3-year study, only 6 pregnancies oc-
curred in the 1751 women.
Mirena® can also be used to treat abnor-
mal uterine bleeding. In 70 women, use
of Mirena® decreased menstrual blood
loss and improved quality of life.
By Mandy Major, PharmD Candidate
REFERENCES:
1. Mirena® [package insert]. Whip-
peny, NJ: Bayer Healthcare Phar-
maceuticals; May 2014.
2. Micromedex [Internet database].
Greenwood Village, Colo: Truven
Health Analytics, 2015.
www.micromedexsolutions.com
Accessed July 15, 2015.
3. Eisenber DL, Schreiber CA, Turok
DL, et al. Three-year efficacy and
safety of a new 52 mg levonorg-
estrel-releasing intrauterine sys-
tem. Contraception 2015;92(1):10
-16.
4. Dhamangasnkar PC, Anurandha K,
Saxena A. Levonorgestrel intrau-
terine system (Mirena®): an
emerging tool for conservative
treatment of abnormal uterine
bleeding. J Mid-life Health
2015;6:26-30.

The University of Montana
Skaggs School of Pharmacy
32 Campus Drive
Missoula, MT 59812-1522
College of Health Professions and Biomedical Sciences
Drug Information Service
Phone: 406-243-5254
Fax: 406-243-5256
Email: [email protected]
www.health.umt.edu/DIS
PATIENT INFORMATION:
Belsomra® (suvorexant): A Different Look at Treating Insomnia
What is Belsomra®?
Belsomra® (suvorexant) is a new medi-
cation that treats insomnia with fewer
side effects than traditional sleep medi-
cines.
Suvorexant acts differently than other
sleep medications. Suvorexant blocks
hormones called orexins which play a
role in waking you up and keeping you
awake throughout the day.
Researchers believe that people with
insomnia have higher levels of orexins
in their brains. By blocking the orex-
ins in the brain from working, su-
vorexant may help some people get to
sleep and stay asleep.
How do I take suvorexant?
Some people might need more or less
suvorexant depending on how well it
works for them. Suvorexant comes in
three different sized tablets, so you and
your doctor can find which strength
may work best for you.
Take suvorexant a half hour before you
plan to go to bed at night. Suvorexant
may take longer to work if you take it
with food.
Suvorexant is intended to help you get
a full night’s sleep, so you should plan
on having at least seven hours of sleep
before you take suvorexant.
Taking more than one dose of suvorexant
before bed can increase the chances of
side effects and make you very drowsy, so
it is important to take it as prescribed by
your doctor.
What are the side effects of suvorexant?
Suvorexant has fewer side effects than
other available sleep medications. How-
ever, side effects can still happen. Nor-
mal side effects include diarrhea, dry
mouth, and higher risk of flu or strep in-
fection.
Serious side effects can happen with su-
vorexant. You should call your doctor
right away if you:
Feel sleepier than normal during the day
Have problems concentrating
Have episodes of sleep-walking, sleep-
eating, sex while asleep, or sleep-talking
What are the warnings with suvorexant?
Suvorexant can interact with alcohol and
some medications that also make you
tired. When using suvorexant:
Avoid drinking alcohol with suvorexant
Have someone else drive if you have
recently taken suvorexant
Avoid taking other medications at night
that make you drowsy, like pain medi-
cations, anti-anxiety medications, and
some antidepressants
By Barry Bodle, PharmD Candidate
REFERENCES:
1. Belsomra® [package insert].
Whitehouse Station, NJ: Merck &
Co.; 2014 August.
2. Michelson D, Snyder E, Paradis E, et
al. Safety and efficacy of suvorexant
during 1-year treatment of insomnia
with subsequent abrupt treatment
discontinuation: a phase 3 random-
ised, double-blind, placebo-controlled
trial. Lancet 2014;13:461-471.
3. Sun H, Kennedy WP, Wilbraham D,
et al. Effects of suvorexant, an orexin
receptor antagonist, on sleep parame-
ters as measured by polysomnogra-
phy in healthy men. Sleep 2013;36
(2):259-267.
4. Herring JW, Snyder E, Budd K, et al.
Orexin receptor antagonism for treat-
ment of insomnia: a randomized clini-
cal trial of suvorexant. Neurology
2012;79:2265-2274.