DIAGNOSTICS OF KIDNEY DISEASES Ph. D., M D. Svitlana Dzyha.
-
Upload
charlene-pierce -
Category
Documents
-
view
221 -
download
0
Transcript of DIAGNOSTICS OF KIDNEY DISEASES Ph. D., M D. Svitlana Dzyha.

DIAGNOSTICS OF KIDNEY DISEASES
Ph. D., M D. Svitlana Dzyha

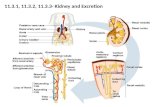
The kidneys are a pair of bean-shaped organs that lie on either side of the spine in the lower middle of the back.
They are connected to the urinary bladder by tubes called ureters
Parenchyma of each kidney
consists of two zones:outer area
called the cortexand inner
region calledthe medulla

The main function of the kidneys is to help keep the body in homeostasis by controling the composition and volume of blood:
Remove waste products (urea, ammonia, drugs, toxic substances) and excess water from the blood in the form of urine
Keep the concentrations of various ions and other important substances constant
Keep the volume of water in the body constant Keep the acid/base concentration of the blood constant The kidneys also produce certain hormones that have
important functions in the body: Renin, which regulates blood volume and blood pressure Erythropoietin, which stimulates the bone marrow to produce
red blood cells Active form of vitamin D, which controls calcium uptake
and helps make strong bones
The functions of kidneys

The functional unit of the kidney is the nephrone
Each nephron is made of
a glomerulus and a tubule
Urine formation requires 3 principal processes:glomerular filtration,
tubular reabsorption,and tubular secretion

The filtering of the blood depends on
a number of opposing pressures
Glomerular blood hydrostatic pressure Blood oncotic pressure Capsular hydrostatic pressure Condition of endothelial-capsular membrane
(depends on amount of functioning capillaries and permeability of basement membrane) PPeffeff = = РРblbl – – (Р(Рonconc+Р+Рcapscaps))
PPeffeff – – effective filtration effective filtration pressurepressure
РРblbl – – gglomerular blood hydrostatic pressure
РРonconc – – bblood oncotic pressure
РРcapscaps – – ccapsular hydrostatic pressure
PeffPeff = 25 = 25 mm Hgmm Hg
Structure of filter
Podocytes
Basement membrane
Endothelium of glomerulus
The consequences of reduced glomerular filtration: azotemia, metabolic acidosis
Abnormalities of Glomerular Function

Protein is normally absent or present in only a trace quantity in the urine
If the integrity of the glomelular filter is impaired, and plasma
proteins can gain access to the capsular space
(proteinuria)
If massive proteinuria (>3,5 g/day),
hypoproteinemia and peripheral edema occur together, this is termed nephrotic
syndrome
Violation of glomerular filtration:proteinuria

These are damaged red blood cells in the urine under
electron microscope
Violation of glomerular filtration:hematuria
Hematuria is the presence of red blood cells in the urine
If the integrity of the glomelular filter is impaired, and red blood cells can gain access to the capsular space
(hematuria)

The worst disorders of sodium and water reabsorption occur in dystrophic and inflammatory changes of tubular epithelium. So kidneys lose the ability to concentrate the urine
Loss of concentration ability is called hyposthenuria, specific gravity of urine is fixed between 1.008 and 1.012 (The specific gravity of normal urine ranges from 1,008 to 1,030)
Isosthenuria is an excretion of urine that has not been concentrated by the kidneys and has the same osmolality as that of plasma. Specific gravity of the urine becomes fixed around 1.010, irrespective of the fluid intake
tubular reabsorption retains substances needed
by the body, including water, glucose, amino acids,
and ions
Violation of tubular reabsorption

Depending on Depending on clinical courseclinical course
aquteaqute chronicchronicprerenal
Depending on etiology of renal failure
renal
postrenal
CLASSIFICATION
Renal failure is a condition in which the kidneys fail to remove
metabolic end-products and maintain the main parameters of homeostasis

It is a clinical syndrome of various ethiology, which is characterized by significant and acute decrease of glomerular filtration rate (GFR)
Acute renal failure develops, when GFR is reduced to 1-10 ml/min (Normal GFR – 100-140 ml/min)
The kidneys fail to remove metabolic end-products from the blood and regulate the fluid, electrolyte, and pH balance of extracellular fluids
The reasons of acute renal failure
are divided into 3 groops
PRERENAL
RENAL
POSTRENAL
Acute Renal Failure:the sudden interruption of renal function

FILTRATION
REABSORPTION
URINARY EXCRETION
The effective filtration pressure Prerenal factors diminish blood flow
to the kidney
Postrenal factors interfere with the
elimination of urine from the kidney
Renal factors lead to damage
to structures within the kidney
Causes of acute renal failure

Hypovolemia Hemorrhage
DehydrationExcessive loss of gastrointestinal tract fluidsExcessive loss of fluid due to burn injury
Decreased vascular fillingAnaphylactic shockSeptic shock
Heart failure and cardiogenic shock Decreased renal perfusion due to vasoactive mediators,
drugs, diagnostic agents
Prerenal failure ensues when a condition that diminishes blood flow to the kidneys leads to hypoperfusion. The impaired blood flow results in decreased glomerular filtration rate
Prerenal ARF accounts for approximately ~55% of ARF cases
Prerenal factors cause hypoperfusion

Acute tubular necrosis (ATN) – is the most common cause of intrinsic renal failureProlonged or severe renal ischemia (the lack of blood flow by ischemia may lead to renal damage; ischemic ATN occurs most frequently in persons who have major surgery, severe hypovolemia, sepsis, trauma, and burns)Exposure to nephrotoxic drugs (antimicrobial agents, particularly aminoglycoside antibiotics, analgesics, anesthetics, chemotherapeutic agents, heavy metals, radiocontrast media, and organic solvents)
Intratubular obstruction resulting from hemoglobinuria, myoglobinuria, uric acid casts
Acute renal disease (acute glomerulonephritis, pyelonephritis)
Obstetric complications (eclampsia, septic abortion, or uterine hemorrage)
Intrinsic ARF directly involve the renal parenchyma ~40% of the cases
Renal factors cause the damage to the filtering structures
of the kidneys

Some of the most notable causes of postrenal ARF include the following:
Bladder outlet obstruction due to an enlarged prostate gland or bladder stone
Kidney stones in both ureters or in patients with one kidney
Tubule obstruction (end channels of the renal nephrons)
Renal injury (usually sustained in an automobile accident or while playing a sport)
Retroperitoneal fibrosis
These factors cause an acute obstruction of urine outflow from the kidneys. The blockage causes pressure to build in all of the renal nephrons (tubular filtering units that produce urine). The excessive fluid pressure ultimately causes the nephrons to shut down
Postrenal ARF accounts for approximately ~5% of the cases
This illustration tells you how kidney stones
could lead to acute renal failure
Postrenal factors cause the obstruction of urine outflow
from the kidneys

Obstruction of urine outflow from the
kidneys
Pathogenesis of acute renal failure
prerenal factors
renal factorspostrenal
factors
Decreased blood flow to the
kidneys
Damage to the filtering structures
of the kidneys
A sharp decrease in effective filtration pressure and glomerular filtration rate
Excretion of nitrogenous wastes is reduced and fluid and electrolyte balance cannot be maintained

The clinical course of acute renal failure is divided into four phases:
Initial phase is a period from the onset of kidney lesion untill oliguria development
Oliguric phase is characterized by marked decrease in the GFR. Serum waste products cannot be removed. Fluid retention gives rise
to edema, water intoxication and pulmonary congestion. The main threat in the oliguric phase is hyperhydration and hyperkalemia
Diuretic phase is characterized by excessive urine output. There is a
gradual return of renal function
Phase of recovery – is the period during which repair of renal tissue takes place. Renal function are restored
Acute renal failure is accompanied by high death, for ischemic and traumatic form approximately 50-70 %, other form – approximately 10-35 %
The clinical course of acute renal failure is divided into four phases:

The end result of progressive and irreversible destruction of kidney structures
Histologic findings of CRF include a reduction in renal capillaries and scarring in the glomeruli (nephrons are replaced with scar tissue, nephrosclerosis develops)
Renal insufficiency (Initial signs of CRF) develops when the nephron amount is between 50-30% of normal (kidney has considerable compensatory ability!)
Renal failure develops when the nephron amount is between 30-10 % of normal
End-stage renal failure – less than 10 % of normal
A decrease in glomerular filtration rate below 10 ml/min leads to the
terminal stage of renal failure
At this final phase treatment with dialysis is necessary for survival
Chronic renal failure

chronic glomerular diseases (chronic glomerulonephritis)
the primary canaliculus diseases (chronic infections (chronic pyelonephritis, tuberculosis), interstitial nephritis)
metabolic disorders (gout, diabetes mellitus) vascular diseases
(arterial hypertension) collagen diseases (systemic lupus erythematosus,
sclerodermia, nodular periarteriitis) obstructive processes (kidney stones, cancer) congenital anomalies
(polycystic kidney disease, Alport syndrome)
Causes of chronic renal failure

The mechanisms of reducing of renal functions include Permanent loss of nephrons A reduction in the GFR in nephrons
These mechanisms result in the retention of waste products in the body, rise in plasma level of creatinine,
blood urea nitrogen (the tert “azotemia” indicates the accumulation of nitrogenous wastes in the blood)
alterations in water, electrolyte and acid-base balance mineral and skeletal disorders anemia and coagulation disorders hypertension and alterations in cardiovascular system neurologic complications etc
Uremia – is the term used to describe the clinical manifestations of end-stage renal failure. Uremic syndrome is caused by accumulation of end products of protein metabolism, so-called ‘middle molecules’ (lipids or peptides with a molecular weight of 300–2000 Da), peptides hormons. They poison the body
Pathogenesis of chronic renal failure

the accumulation
of uremic toxins which suppresses red blood cell production in the bone marrow
erythropoietin deficiency iron deficiency bleeding hemolysis of red blood cells Appearance of
normal red blood
cells
Peripheral blood smear examination
reveals anemia
The clinical manifestations of uremia: Hematologic Disorders
pathogenesis of anemia includes

pathogenesis of hypertension includes
an increased vascular volume
elevation of peripheral vascular resistance
decreased levels of renal vasodilator prostaglandins
increased activity of the reninangiotensin system
The clinical manifestations of uremia: Cardiovascular Disorders

anorexia nausea vomiting diarrhea a metallic taste in the
mouth stomatitis ulcers gastrointestinal bleeding develop due to retained
uremic products
The clinical manifestations of uremia: Gastrointestinal Disorders
The clinical manifestations of uremia: Gastrointestinal Disorders
The clinical manifestations of uremia: Gastrointestinal Disorders

decreased levels of active vitamin D lead to a decrease in intestinal absorption of calcium
stimulation of the parathyroid glands (secondary hyperparathyroidism) leads to demineralization of bone and teeth
there is retention of phosphate, which leads to increased renal excretion of calcium
The clinical manifestations of uremia: Mineral Metabolism and Skeletal Disorders
The bones become more porous, fragile and more likely to break
pathogenesis of renal osteodystrophy includes

Transplantation Hemodialysis
Treatment of uremia
Patients must have kidney dialysis to
cleanse the blood of toxic elements
Treatment of uremia

Thank you for attention!