An Introduction to Cardiotocography – “CTG” Max Brinsmead MB BS PhD May 2015.
CTG introduction
-
Upload
aboubakr-elnashar -
Category
Health & Medicine
-
view
532 -
download
0
Transcript of CTG introduction
1. Fetal response to hypoxia
2. Fetal monitoring in labor
3. Indications
4. Types of CTG monitoring
5. Important considerations
6. Why care about CTG
7. Steps
8. Components of CTG paper
ABOUBAKR ELNASHAR
1. FETAL RESPONSE TO HYPOXIA
Hypoxia ← ↓ Blood Flow
↓↓
↓ PO2 ↑PCO2
↓ ↓
Metabolic acidosis ← Respiratory acidosis
⇓
Redistribution of blood flow to vital organs
Bradycardia, and slightly ↓cardiac output
↓oxygen consumption
ABOUBAKR ELNASHAR
↓ ↓
FHR, variability FHR,↓ variability,
retained / ↑ rate, decelerations
⇓⇓ Compensated State Decompensated State
(Normal cortical functions (Decrease cerebral
cerebral oxygenation oxygenation, eventual
maintained cellular damage
ABOUBAKR ELNASHAR
Important definitions
Hypoxia: Decreased po2 level in tissues.
Hypoxima: Decreased po2 level in blood.
Acidosis: Decreased PH in tissues.
Acidemia: Decreased PH in blood.
Ashyxia: Hypoxia + acidosis.
ABOUBAKR ELNASHAR
2. FETAL MONITORING IN LABOR
1. Intermittent auscultation
2. CTG Fetal electrocardiography
Scalp stimulation
Vibroacoustic stimulation
3. Fetal scalp sampling PH determination
4. Fetal pulse oximetry
ABOUBAKR ELNASHAR
1968:
Hammacher and Hewitt-Packard, developed 1st
commercial fetal monitor.
Assessment of fetal well being during late
pregnancy and labor.
Expectations at the time
it would lead to a decreased incidence of perinatal
death and cerebral palsy.
Reality
has fallen very short of these expectations
ABOUBAKR ELNASHAR
3. INDICATIONS OF CONTINUOUS EFM
1. High-risk pregnancies where there is an
increased risk of perinatal death, cerebral palsy
or neonatal encephalopathy.
2. Where oxytocin is being used for induction or
augmentation of labour.
ABOUBAKR ELNASHAR
The admission CTG test
Commonly used screening test consisting of a short
(usually 20 minutes) recording of FHR and uterine
activity performed on the mother's admission to the labour
ward.
Admission CTG not be used for women who are low risk
on admission in labour. (Cochrane SR, 2012)
{:an increase in the incidence of CS without evidence of
benefit}.
ABOUBAKR ELNASHAR
CTG is best regarded as a screening tool (not
diagnostic)
High negative predictive value (Specificity=
Healthy, 98%)
>98% of fetuses with a normal CTG will be OK
Poor positive predictive value (Sensitivity) with
unnecessary operative intervention for f distress.
50% of fetuses with an abnormal CTG will be
hypoxic and acidotic but 50% will be OK
CTG should always be interpreted in its clinical
context and backed by fetal blood sampling PRN
5. IMPORTANT CONSIDERATIONS
ABOUBAKR ELNASHAR
Normal CTG indicate that there were
no abnormalities
no indication for intervention.
CTG could be viewed as part of Defensive Medicine (permanent record)
Abnormal/suspicious CTG may provide:
an evidence that inappropriate or lack of tt: litigation
In spite of it is poor indicator of overall fetal status but it remains The best we have
ABOUBAKR ELNASHAR
Disadvantages
Insufficient understanding of the (patho-)physiologic background
Confusion due to the many influences on the FH rhythm
Lack of agreement on how, when, and whom to monitor
Lack of uniform classification systems
Poor positive predictive value (Sensitivity): unnecessary operative intervention for f distress.
Substantial intra- and inter-observer variation regarding the interpretation
Contributes to medico-legal vulnerability
Primarily qualitative information (pattern recognition)
ABOUBAKR ELNASHAR
7. STEPS
External monitoring
• Explain the processes and reasons for the CTG, verbal
consent
Ask to empty her bladder
Ascertain the lie, presentation and position of the fetus
Place and secure the FHR ultrasound transducer over the
fetal anterior shoulder
Place and secure the toco-transducer on the fundus
Position the woman: comfortable: sitting upright or laterally
Ensure ultrasound contact is maintained
Document on the FHR pattern: date and time, gestation,
indication for monitoring, maternal pulse/30 min
Record the FHR pattern at the rate of 1cm or 3cm/min
ABOUBAKR ELNASHAR
Internal monitoring
Membranes: absent
Cervix: dilated enough.
1. Fetal scalp electrode:
A device that monitors FHR.
consists of a small clip that is placed on the
fetal scalp.
The electrode is attached to a cable.
ABOUBAKR ELNASHAR
2. Intrauterine pressure catheter (IUPC):
directly measures the strength of contractions
and resting tone in millimeters of Hg.
It provides more accurate information as to the
strength of contractions than an external monitor
(tocodynameter).
can also be used to instill an amnioinfusion.
ABOUBAKR ELNASHAR
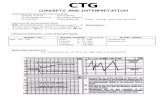
8. COMPONENTS OF FETAL HEART
RATE PAPER
Date
Time
Paper speed: 3 cm/minute. There are 6 in one minute between the dark lines so each little box represents ten (10) seconds.
Dark red lines are one minute apart
Maternal vital signs
ABOUBAKR ELNASHAR
LITIGATIONTraces:
not done.
Unsatisfactory or
Missing: EFM traces should be kept up to 25 ys
Abnormal CTG: ignored or not recognized
ABOUBAKR ELNASHAR
EDUCATION AND TRAINING
If you are going to use the CTG You must be
able to Interpret the trace & respond accordingly
Improves Knowledge/clinical skills for all staff
Training should include
instructions on documenting traces and
storage
appropriate clinical responses to suspicious or
pathological traces
local guidelines
ABOUBAKR ELNASHAR