Clostridium difficile : Biology, Diagnosis and Infection Control Clostridium difficile Disease.
Clostridium difficile Policy Prevention and Control) · PDF fileClostridium difficile Policy...
Transcript of Clostridium difficile Policy Prevention and Control) · PDF fileClostridium difficile Policy...
Clostridium difficile Policy (Prevention and Control)
EQUALITY IMPACT The Trust strives to ensure equality of opportunity for all both as a major employer and as a provider of health care. This policy has therefore been equality impact assessed by the Infection Prevention Committee to ensure fairness and consistency for all those covered by it regardless of their individual differences, and the results are shown in Appendix 7. Version: 5.0
Authorised by: Infection Prevention Committee
Date authorised: 16th September 2015
Next review date: September 2017
Document author: Matron, Infection Prevention / Tissue Viability
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 2 of 23 Check the Intranet for the latest version
VERSION CONTROL SCHEDULE Clostridium difficile Policy (Prevention and Control) Version : 5.0 - draft
Version Number Issue Date Revisions from previous issue
1.0 (final) March 2008
1.2 December 2008 Addition of policy statements on:- Faecal transplants Probiotic use
2.0 June 2009 Addition of responsibilities of the Antibiotic Management Team Addtion of statement on CDAD associated deaths.
3.0 July 2011 Includes the Trusts strategic approach to clinical management and treatment. Review of Policy Statement to reflect management of individual performance
3.1 July 2012 Addition of the updated 2-stage testing process for C. difficile. Addition of paragraph on patients own clothing.
4.0 July 2013 Addition of: Information on GDH positive (colonisation). Paragraph on care plans. SIGHT protocol (2 hour time limit from diagnosis to isolation). Escalation procedures to follow in the event that single room accomadation is unavailable. Isolation cleans of bed spaces / single rooms. Isolation of C.difficile patients throughout the length of their stay in hospital. Use of the Bowel Management System. Updated References.
4.1 December 2013 Addition of: CDI severity assessment guide (Appendix 1). Bristol stool chart (Appendix 2).
4.2 March 2014 Amendment to prescribing guidance for vancomycin from 125mg to 500mg.
5.0 September 2015
C. difficile Clinical Guideline merged with the Policy into one averarching document. Updated and refreshed content as per latest clinical evidence. Updated references and bibliography. Addition of extra appendicies:
Antibiotic Stewardship treatment algorithm
Diarrhoea Assessment Tool
SIGHT Protocol
Clinical Management of patients with C. difficile
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 3 of 23 Check the Intranet for the latest version
INDEX/ TABLE OF CONTENTS EQUALITY IMPACT ................................................................................................... 1 INTRODUCTION ........................................................................................................ 4 PURPOSE .................................................................................................................. 4 SCOPE ....................................................................................................................... 4
DEFINITIONS (in context) .......................................................................................... 5 RESPONSIBILITIES ................................................................................................... 5 POLICY STATEMENT ................................................................................................ 7
THE POLICY .............................................................................................................. 8 Summary: ................................................................................................................ 8 Risk factors ............................................................................................................. 8 Initial management of suspected cases .................................................................. 8
Symptoms ............................................................................................................... 8 SIGHT Protocol ....................................................................................................... 9 Testing for C. difficile .............................................................................................. 9 Procedure for informing results ............................................................................. 10
Antimicrobial Prescribing ....................................................................................... 10 Source Isolation .................................................................................................... 11
Clinical Management of Patients with C. difficile diarrhoea ................................... 11
Assessment of C. difficile Severity and Treatment ................................................ 11
Recurrence ........................................................................................................... 11 Probiotics .............................................................................................................. 12 Information for patients and carers ....................................................................... 13
Period of increased incidence / outbreaks ............................................................ 13 Root Cause Analysis (RCA) investigations ........................................................... 13
Bowel Management System / Faecal Collection Bags .......................................... 13 Hand Decontamination and Enteric precautions ................................................... 14 Environmental Cleaning ........................................................................................ 14 C. difficile Associated Deaths ................................................................................ 15
POLICY DEVELOPMENT & CONSULTATION ........................................................ 15 IMPLEMENTATION .................................................................................................. 15
MONITORING .......................................................................................................... 15 EQUALITY AND DIVERSITY ................................................................................... 16 REFERENCES ......................................................................................................... 16 BIBLIOGRAPHY ....................................................................................................... 16 REVIEW ................................................................................................................... 16
APPENDICES .......................................................................................................... 17 Appendix 1 – Antimicrobial Stewardship .................................................................. 17 Appendix 2 - Diarrhoea Assessment Tool ................................................................ 18 Appendix 3 – SIGHT Protocol ................................................................................... 19 Appendix 4 – Clinical Management of Patients with C. difficile diarrhoea ................ 20
Appendix 5 – Assessment of C. difficile Severity and Treatment .............................. 21
Appendix 6 – Bristol Stool Chart ............................................................................... 22
Appendix 7 - Equality Impact Assessment Tool ........................................................ 23
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 4 of 23 Check the Intranet for the latest version
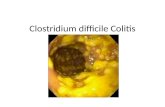
INTRODUCTION Clostridium difficile (C. difficile) is a spore-forming organism that can survive in the healthcare environment and colonisation is usually acquired by ingestion after contact with a contaminated environment, equipment, other patients or the hands of staff. However there are approximately 3% of the population who are naturally colonised with the spores as part of their normal bowel flora. The GDH test explained on page 8 will indicate a colonisation. C. difficile Infection (CDI) occurs when the normal flora of the bowel is disrupted, usually as a consequence of treatment with broad spectrum antibiotics. This is confirmed by the toxin A & B test; explained on page 8. C. difficile infections are most common in people over the age of 65 years but any age group may be susceptible. Illness ranges from mild diarrhoea of short duration to severe and potentially life threatening inflammation of the bowel called Pseudomembranous colitis. Outbreaks of infection can be prolonged and difficult to control. Large outbreaks of C. difficile associated with loss of life have occurred in healthcare facilities and it is therefore essential that the Trust takes appropriate action to minimise the occurrence of C. difficile infection and ensures robust management arrangements are in place at all times to prevent secondary spread.
PURPOSE This policy provides operational guidance for the prevention, control and management of C. difficile associated diarrhoea based on Department of Health guidance. The key elements of this policy are: 1. Early identification of patients at risk 2. Prompt recognition of symptomatic patients 3. Source isolation and implementation of appropriate precautions for symptomatic patients 4. Early clinical and laboratory diagnosis 5. Careful monitoring and symptom management 6. Antibiotic Stewardship 7. High standards of personal and environmental hygiene and cleanliness 8. Ensuring compliance with all aspects of the policy and associated guidance.
SCOPE This policy is applicable to all staff, patients and visitors of Tameside General Hospital.
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 5 of 23 Check the Intranet for the latest version
DEFINITIONS (in context)
Staff All persons employed directly or indirectly by Tameside Hospital NHS Foundation Trust.
Antibioitc Stewardship The thoughtful provision of antibiotic therapy appropriate to assessed clinical need.
Symptomatic C.difficile is suspected in all patients presenting with frequent, watery stool when there is no clear alternative clinical cause.
Spore Forming The organism survives in a differentiated, specialised form that can be used for dispersal, and enables survival in adverse conditions.
Colonisation An individual has the organism in their body but has no symptoms of infection.
Source Isolation The separation of an infectious patient from other patients.
Surveillance On-going monitoring of the occurrence and spread of infection.
Enteric Precautions Infection prevention and control measures taken to control pathogens excreted from the bowel and potentially ingested.
Pro-biotic A food supplement that contains live cultures, formulated to assist rebalance of gut flora.
Faecal transplant The use of stool from a donor to rebalance gut flora.
RESPONSIBILITIES
Chief Executive The Chief Executive has overall responsibility for ensuring that there is a managed environment which minimises the risk of C. difficile infection.
Director of Infection Prevention / Control: The Director of Nursing is the Chief Executives nominated Director for Infection Prevention / Control (DIPC) and is responsible for ensuring that there are effective and appropriate arrangements for the prevention and control of C. difficile throughout the Trust.
Consultant Medical Microbiologists Consultant Medical Microbiologists are responsible for the development and monitoring of a comprehensive antibiotic policy / guideline and for ensuring that all prescribers have access to support and guidance to enable them to prescribe with due caution and to prevent the inappropriate use of antibiotics.
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 6 of 23 Check the Intranet for the latest version
Infection Prevention Team: The Infection Prevention Team report directly to the DIPC and have responsibility for all aspects of surveillance, prevention and control of C. difficile within the Trust. In particular, the Infection Prevention Team is responsible for the implementation of the Trust’s Infection Prevention Programme and for the development and dissemination of this C. difficile policy. Critical functions of the Infection Prevention Team include:-
Prompt and effective identification and control of an outbreak of C. difficile
Education and training of staff in all aspects of the prevention and control of C. difficile associated diarrhoea
Liaison with clinical teams to ensure prompt recognition of and response to cases
Co-ordinate prompt investigation and root cause analysis of individual cases.
Manage data and performance reporting.
Antimicrobial Management Team: The Antimicrobial Management Team are accountable to the DIPC and have delegated authority from the Chief Executive to monitor and regulate the prescription and administration of antimicrobial agents. Directors / Lead Clinicians / Senior Managers All Directors, Lead Clinicians and Senior Managers are responsible for ensuring that this policy is known to their staff and that its requirements are followed at all times, by all staff within their Directorate / Division / Department. In the event of an outbreak Directors, Lead Clinicians and Senior Managers have a responsibility to ensure and facilitate compliance with all control measures including ward closures and restrictions to admissions or discharges as recommended by the Infection Prevention Team. Senior Managers are responsible for ensuring that the Infection Prevention elements / implications of all service developments, structural alterations and environmental changes are duly considered and brought to the attention of the Infection Prevention Team. In the event of an outbreak, Executive Directors and Lead Clinicians will take responsibility for ensuring the prompt implementation of all outbreak controls including ward closure on advice from the Infection Prevention Team. Bed Managers Bed Managers have a responsibility to ensure that patients who are admitted with undiagnosed diarhoea are placed appropriately. Decisions relating to the placement of patients and patient transfers (inter-ward) must include the potential risk of infection and must reflect and make reference to this policy and to the Trust’s Isolation Policy.
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 7 of 23 Check the Intranet for the latest version
Matrons / Ward Managers Matrons and Ward Managers are responsible for ensuring all staff are aware of this policy and comply with all aspects with particular reference to:
Recognising patients at risk Acting promptly in response to patients developing diarrhoea The timely collection of stool specimens Prompt isolation of patients Cleaning of equipment Antibiotic Stewardship Effective hand decontamination Managing the clinical environment to optimise and facilitiate hygiene and
cleanliness
Matrons and Ward Managers also have responsibility for ensuring staff have adequate supplies of equipment, particularly consumables to ensure compliance with this policy. Head of Hotel Services and Hotel Services Manager The Head of Hotel Services and the Hotel Services Manager are responsible for ensuring that all domestic / environmental practices and procedures are carried out in line with the requirements of this policy. The Hotel Services Manager will ensure that any proposed changes to cleaning products or practices will be discussed with the Infection Prevention Team, prior to implementation. All Staff All staff are responsible for following policies, procedures and guidance (written or verbal) relating to the prevention and control of infection, at all times. Staff are responsible for ensuring that they understand the risk of C. difficile infection associated with their activity and that they adopt safe practice and act to prevent inappropriate practice at all times. Any member of staff who has concerns about infection risks or suspicions of an outbreak of infection will discuss their concerns (as a matter of urgency) with their Matron and the Infection Prevention Team.
POLICY STATEMENT Diarrhoea caused by C.difficile toxin may lead to serious and a potentially life threatening illness and as such is to be recognised as a significant clinical condition in its own right. Tameside Hospital NHS Foundation Trust recognises a collective responsibility for the protection of patients by the prevention of C. difficile infection and will actively engage all personnel in strategic risk reduction. Wilful failure of any individual to practice / operate within the Trust’s policy will lead to disciplinary action against that individual.
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 8 of 23 Check the Intranet for the latest version
THE POLICY Summary: The essential components in the prevention and control of C. difficile disease are:
High index of suspicion – C.difficile is to be suspected when there is no clear alternative cause for diarrhoea.
All symptomatic patients must have stool tested promptly.
All symptomatic patients must have each episode of loose stool recorded on a stool chart using the criteria of the Bristol Stool Chart (Appendix 6)
Prudent antibiotic prescribing to reduce the use of antibiotics particularly quinolones and cephalosporin’s.
Prompt isolation (within 2 hrs) of patients with C. difficile diarrhoea and strict infection control practice.
Fastidious hand washing with soap and water (hand sanitiser does not kill the spores of C. difficile) before and after direct patient contact and /or contact with potentially contaminated clothing or equipment, and wearing of gloves and aprons appropriately.
Enhanced environmental cleaning and the prudent use of high level disinfectant products (under the direction of the Infection Prevention Team) where there are cases of C. difficile infection in order to reduce environmental contamination.
Risk factors
Aged > 65 years
Severity of underlying disease
Chemotherapy
Chronic Renal disease
Immunocompromised
Gastrointestinal procedures / Bowel surgery
Enteral feeding / NG tube
Proton Pump Inhibitors (PPI) – and H2 antagonists
Recent healthcare intervention
Antibiotic therapy – Almost all cases of C. difficile infection (CDI) will have had a recent history of antibiotics (NHS England 2015)
Initial management of suspected cases A range of factors may cause diarrhoea and it is therefore essential to identify any underlying causes which are abnormal for the patient and may be indicative of infection. In order to prevent spread to other patients an assessment must be undertaken using the diarrhoea assessment tool (appendix 2) and precautions must be employed promptly. Symptoms
Watery diarrhoea / type 5, 6, 7 on Bristol Stool Chart – stool smells offensive and can contain mucous / be green in colour
Abdominal pain / tenderness
Fever / nausea / loss of appetite
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 9 of 23 Check the Intranet for the latest version
SIGHT Protocol (See also Appendix 3) Clinicians (doctors and nurses) should apply the following mnemonic protocol (SIGHT) when managing suspected potentially infectious diarrhoea (DH 2009):
S Suspect that a case may be infective where there is no clear alternative cause for diarrhoea
I Isolate the patient and consult with the Infection Prevention Team whilst determining the cause of the diarrhoea
G Gloves and aprons must be used for all contacts with the patient and their environment
H Hand washing with soap and water must be carried out before and after each contact with the patient and the patient’s environment
T Test the stool, by sending a specimen immediately
Testing for C. difficile In 2009 evidence was published demonstrating the low sensitivity rates of the C. difficile toxin ELISA kits. In line with many laboratories in the UK this was the method of choice. However both false negative and false positive results may occur: It is estimated that testing for toxin may miss between 1 in 5 to 1 in 10 cases. It is also estimated that the test for toxin only may have an intrinsic false positive rate of up to 3%. Most research and DoH/PHE updates strongly suggest that a 2-step protocol would be the most accurate approach. Stage 1 – a screening test Testing for GDH antigen – this has very good predictive negative rate, that is, if GDH test is negative, C. difficile is not present in the bowel. Stage 2 test - Toxin testing is not required. Stage 2 – a confirmation test GDH antigen positive – Toxin testing performed: Toxin negative – Cl.difficile present in the bowel, but no demonstration of toxin production. Toxin positive – toxin present and laboratory evidence (GDH) confirms C. difficile infection. In March 2012 the Department of Health published updated guidance on the diagnosis and reporting of C. difficile. This included an extensive review of the commercially available testing kits for C. difficile which concluded that toxin EIA’s are not suitable as standalone tests for the diagnosis or detection of C. difficile. Therefore a combination of two tests should be used. Proactively in July 2011 following a laboratory trial and based on the published research the Trust introduced the 2 stage algorithm as the routine laboratory protocol. This protocol consists of stage 1-primary screening by GDH antigen EIA, followed by stage 2- toxin testing (C. difficile toxin A and B EIA) on those samples that were GDH antigen positive.
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 10 of 23 Check the Intranet for the latest version
Procedure for informing results Routine C. difficile testing is performed in the afternoons (Monday – Friday) and the results are reported on the same day via Lorenzo. Samples must be received into the laboratory by 11am to ensure that results can be obtained on the same day. The Infection Prevention Team will:
Notify any positive results to the ward during normal working hours.
Visit the ward to discuss infection prevention / control related issues with staff and the patient / relatives if appropriate.
Add an alert to Lorenzo and to the patient’s medical notes.
Deliver advice sheets, information leaflets and an alert card to the ward.
Send a letter to the patient’s General Practitioner to inform them of the result. Antimicrobial Prescribing Antimicrobial Stewardship is an important element of the UK Five Year Antimicrobial Resistance Strategy (2013-2018). The aim of antibiotic stewardship is to improve the safety and quality of patient care by contributing to reductions in the emergence and spread of resistant organisms. These aims can be achieved by improving antimicrobial prescribing utilising evidence based tools such as the Start Smart – Then Focus (Antimicrobial Stewardship Toolkit – March 2015). The Health and Social Care Act 2008: Code of Practice on the prevention and control of infections and related guidance (updated July 2015); places greater emphasis on antimicrobial resistance and stewardship. Criterion 3 states “Ensure appropriate antimicrobial use to optimise patient outcomes and to reduce the risk of adverse events and antimicrobial resistance.” C. difficile infection is almost always associated with and triggered by the use of antibiotics. The appropriate use of antibiotics will reduce the selection pressure for colonisation and infection with C. difficile. Staff prescribing antibiotics must adhere to the Trusts antibiotic guidelines. Where antibiotic prescription cannot be avoided, the prescription should be reviewed daily to consider whether or not the prescription is still required. Antibiotic use, especially if inappropriate, excessive or prolonged, is the single most important factor in promoting both bacterial antibiotic resistance as well as the development of C. difficile enteric disease. Antimicrobials must only be prescribed in patients who have confirmed evidence (clinical, microbiologic, and radiologic) of a bacterial infection. See Antimicrobial Stewardship Treatment Algorithm – Appendix 1. This does not include antibiotics which are being given as part of prophylaxis. C. difficile infection should be suspected in patients who have abrupt onset of watery, foul smelling diarrhoea. In such patients the following actions should be taken immediately:
Review all antibiotic prescriptions and consider discontinuation or change of antibiotic (most patients symptoms will resolve if antibiotics are stopped)
Discuss with Consultant Medical Microbiologist
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 11 of 23 Check the Intranet for the latest version
Source Isolation Patients who have diarrhoea should be assesed using the diarrhoea assessment tool (appendix 2) and be moved to a single room unless they are known to have a non infectious cause for the diarrhoea. As far as possible the patient should be isolated on the same ward where their symptoms started. When a patient has C. difficle associated diarrhoea it is important that:
On confirmation of the diagnosis of C. difficile colonisation or infection the patient should be isolated preferably within 2 hours if they have not previously been isolated when first symptomatic.
If the patient cannot be isolated on the ward where the symptoms started then the ward staff must escalate this to the Bed Manager.
Any delays in isolation of the patient must be escalated to the Matron and the Deputy Chief Nurse if required.
If single room capacity is exceeded then cohorting of patients must be considered.
The patient must not be transferred to any other ward, hospital or care facility unless the transfer is for urgent treatment and the transfer has been discussed with the Infection Prevention Team.
The patient should not attend other departments for investigative procedures unless the procedure is associated with urgent treatment and has been discussed with the Infection Prevention Team.
The patient must be isolated in a single room for the length of their hospital stay (even when asymptomatic) unless the Infection Prevention Team have been consulted regarding alternative arrangements.
Where isolation would compromise patient safety the clinical team must inform Infection Prevention. A risk assessment must be carried out to establish the safest care for the patient whilst protecting others within that same clinical environment.
Clinical Management of Patients with C. difficile diarrhoea See appendix 4 Assessment of C. difficile Severity and Treatment See appendix 5. Recurrence If not severe, treat first recurrence with the same modality of treatment to which initial symptoms responded. If first relapse was treated with metronidazole and recurrence is severe, use vancomycin. In second relapse if antibiotic is clinically required treatment can be given by tapering and pulsed oral vancomycin as follows: Week 1 Vancomycin 125mg orally four times daily
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 12 of 23 Check the Intranet for the latest version
Week 2 Vancomycin 125mg orally twice daily Week 3 Vancomycin 125mg orally once daily Week 4 Vancomycin 125mg orally alternate days Week 5 and 6 Vancomycin 125mg orally every 3 days Treatment of subsequent relapse is by vancomycin 125mg orally four times daily for up to fourteen days together with rifaximin orally 400mg three times daily for up to fourteen days. In any further relapse, prolonged vancomycin 125mg twice daily. For multiple relapses fidaxomicin 200mg orally bd can be given but only on the advice of the Consultant Medical Microbiologist. For further information please refer to the THFT Antibiotic Guidelines on the intranet.
Probiotics Probiotics are live organisms believed to confer health benefits to the host. They are thought to help with food digestion and in maintaining the balance of gut flora. Antibiotic treatment can disturb the natural balance of organisms in the gut by killing beneficial bacteria which can leave the gut open to colonisation and infection by harmful bacteria. Prophylactic use of probiotics (e.g. Actimel) in patients receiving antibiotic treatment: There is moderate quality evidence which suggests that C.difficile diarrhoea can be reduced with the use of probiotic prophylaxis. In order to prevent the incidence of C.difficile infection, patients who are 65 years or over and are receiving antibiotic treatment for an infection should be given Actimel, one bottle of 100ml, twice a day for the duration of antibiotic treatment and for 7 days after stopping antibiotics. For patients to receive Actimel doctors, pharmacists or nurses must produce a written indication on the medication chart in the regular medicines section. Contraindications: The following patients should not receive probiotics: • Patients who are immunosuppressed • Patients with acute pancreatitis • Patients who have a dairy allergy Interactions: Dairy products reduce absorption of oral ciprofloxacin. Patients receiving oral ciprofloxacin should not take Actimel at the same time and a 2 hour interval should be maintained between the administration of these two agents.
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 13 of 23 Check the Intranet for the latest version
Information for patients and carers All cases identified during an inpatient stay will be visited by a member of the Infection Prevention Team, who will explain about C. difficile and provide them with an advice sheet / patient information leaflet which also contains contact details for the Infection Prevention Team. The patient is also issued with a C. difficile alert card which can be shown by the patient in future contacts with any healthcare providers. Period of increased incidence / outbreaks A period of increased incidence (PII) is identified as 2 or more cases (hospital attributable) in a 28 day period in the same ward. Additional auditing and enhanced monitoring will be undertaken. An outbreak is defined as 2 or more cases which can be linked in time and place which have the same identifiable ribotype and enhanced fingerprint (MLVA). If this occurs the Outbreak Policy will be followed and a multidisciplinary incident meeting will be held – chaired by the Director of Infection Prevention / Control. Root Cause Analysis (RCA) investigations Following a case of C. difficile there is a requirement for the ward where the patient was diagnosed to complete an incident form and an RCA. Each month C. difficile cases are reviewed at the Consultant Review Executive Assurance Meeting (CREAM). This meeting is held in order to:
Seek assurance re the effectiveness of measures implemented to prevent further cases
Learn any lessons to improve patient safety
Identify any ‘lapses in care’
Determine preventability (avoidable / unavoidable) CREAM is a sub group of the Infection Prevention Committee and a RCA summary report is tabled on a monthly basis.
Bowel Management System / Faecal Collection Bags Bowel/faecal management systems have been developed to assist clinicians in the management of faecal incontinence and infection control, and the prevention of associated skin damage. Extensive skin damage can be caused by prolonged contact with excessive moisture from urine or liquid stool incontinence. Additionally, in-patients with infective bacteria present in their faeces, e.g. C. difficile, incontinence may add to the risk of cross infection. A bowel / faecal management system is a temporary containment device consisting of a soft flexible, silicone catheter with a low pressure balloon, which is filled with water to aid retention, and which is easily inserted into the patient’s rectum. The catheter is attached to a closed end collection bag. The device is suitable for the collection of liquid or semi-liquid stools and has a port to allow for flushing of the system if required. At THFT the bowel management system is only to be used in critical care. All other wards have the alternative faecal collection bag which is similar to a stoma bag and attaches around the anus.
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 14 of 23 Check the Intranet for the latest version
Hand Decontamination and Enteric precautions C. difficile is transmitted via the faecal – oral route. This means that the organism is excreted from the bowel of a symptomatic patient and may be picked up on the hands of the affected patient, other patients, staff and visitors.
The risk of transmission is therefore significantly reduced by effective hand decontamination and by the application of enteric precautions. A laminated Infection Prevention / Control precautions sign must be placed on the door of the single room where the patient is nursed. Additional copies of this are available from Infection Prevention. This ensures that all staff / visitors are aware that certain practices must be adhered to before entering / leaving the single room.
All staff must be vigilant in the decontamination of their hands before and after every patient contact. Where staff have contact with patients who have diarrhoea, hands must be washed thorougly with soap and water as alcohol hand sanitiser will not effectively deal with the spores of C. difficile. Appropriate provision must be made to enable patients to clean their hands after using the toilet / commode / bedpan, after episodes of incontinence and before eating drinking and taking medications. Patient visitors should be advised to clean their hands before leaving the isolation room / ward. Staff attending patients with diarrhoea must wear a protective disposable apron and disposable gloves for each care intervention. Contaminated articles of clothing, bedding, commodes, bedpans etc must be removed promptly. Note - Contaminated linen must be placed in a red alginate bag inside a red plastic laundrey bag. Patients must be given their own dedicated BP cuff and tourniquet which should be labelled with their name. On discharge these should be disposed of as clinical waste. Patients own clothing which is contaminated with any body substances including faeces must be placed into the patient’s clothing bag from the ‘dissolvo’ sack range. Friends / family do not then have to touch the clothes as the sack goes straight into the washing machine and dissolves. If the patient is suffering from severe diarrhoea leading to frequent soiling of clothes it is advisable to discuss with friends / relatives that the wearing of hospital nightwear may be preferable. Environmental Cleaning Because C. difficile can survive in spore form for prolonged periods of time, enhanced cleaning and disinfection of the patient environment is required particularly in clinical areas where patients have C. difficile associated diarrhoea. Domestic staff use cleaning products which are suitable for this type of cleaning. Following vacation of a single room or bed space by a patient who has had C. difficile the ward staff must request a Level 3 isolation clean from the Trust domestic service provider. Ward staff must then request that the single room is ‘fogged’ with hydrogen peroxide by the maintenance team. Ward staff must clean the patient bedspace and associated equipment with high level
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 15 of 23 Check the Intranet for the latest version
disinfectant wipes and label ‘I am clean’. Care Plan All patients diagnosed as either GDH positive (colonised with spores) or C. difficile infection (producing toxin) must be commenced on care plans, the latest versions of which can be found on the intranet. The care plans also contain an integral component regarding the recording of patient bed spaces and isolation as well as the date any isolation cleans were carried out. This information is essential for patient care as well as audit and root cause analysis. C. difficile Associated Deaths If a patient with symptomatic C. difficile infection dies the doctor completing the death certificate must consider the significance of C. difficile in the sequence of events leading to the death of the patient. C. difficile should be noted on the death certificate if:
C. difficile directly led to or was the underlying cause of death (include in Part 1 of the certificate)
C.difficile was not the direct or underlying cause of death but contributed to death (include in Part 2 of the certificate)
If there is any doubt relating to the significance of C. difficile at the time of death the doctor must seek the advice and guidance of the Consultant responsible for the patient and/or a Consultant Medical Microbiologist before completing the certificate.
POLICY DEVELOPMENT & CONSULTATION This policy has been considered and ratified by the Infection Prevention Committee and is to be implemented throughout the Trust. Stakeholders are represented on the Infection Prevention Committee.
IMPLEMENTATION This policy will be implemented throughout Tameside Hospital NHS Foundation Trust and brought to the attention of all staff via Trust wide communications using the intranet and the Infection Prevention newsletter. The Infection Prevention Team is available to discuss aspects of the policy at any time. The policy should be read in conjunction with:
Infection Prevention / Control Policy
Hand Hygiene Policy
Bare Below the Elbow Policy
Isolation Policy
Outbreak of Infection Policy
MONITORING Compliance with this policy will be monitored by the Infection Prevention Team. The High Impact Intervention (Care Bundle) included within the Saving Lives programme
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 16 of 23 Check the Intranet for the latest version
will be audited monthly by ward teams in inpatient areas and results monitored by the Infection Prevention Team, Deputy Chief Nurses and Matrons. Where a PII or outbreak occurs, the Infection Prevention Team will undertake a detailed investigation and audits of practice. Where monitoring has identified deficiencies, recommendations and action plans will be developed and changes implemented accordingly. Progress on these will be reported to the Infection Prevention Committee.
EQUALITY AND DIVERSITY (Impact Assessment Tool – Appendix 7)
The Tameside Hospital NHS Foundation Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds.
REFERENCES Department of Health - The Health and Social Care Act 2008 Code of Practice on the Prevention and Control of Infections and related guidance (updated July 2015) Department of Health (2011), Saving Lives: High Impact Interventions – care bundles:
Reducing the risk of infection from the presence of Clostridium difficile
Antibiotic Stewardship Department of Health (2009), Clostridium difficile Infection: How to deal with the problem NHS England (2015), Clostridium difficile infection objectives for NHS organisations in 2015/16 and guidance on sanction implementation Public Health England (2015), Start Smart – Then Focus, Antimicrobial Stewardship Toolkit for English Hospitals
BIBLIOGRAPHY National Institute for Health and Care Excellence (2015), NICE Guideline – Antimicrobial Stewardship: systems and processes for effective antimicrobial medicine use
REVIEW This policy will be formally reviewed in September 2017 or earlier if indicated by the results of monitoring.
TAMESIDE HOSPITAL NHS FOUNDATION TRUST Clostridium difficile Policy (Prevention and Control)
VERSION 5.0 (final) September 2015 Page 17 of 23 Check the Intranet for the latest version
APPENDICES Appendix 1 – Antimicrobial Stewardship
TAMESIDE HOSPITAL NHS FOUNDATION TRUST policy for the prevention and control of clostridium difficile associated diarrhoea
VERSION 5.0 (final) September 2015 Page 18 of 23
Check the Intranet for the latest version
APPENDIX 2 - DIARRHOEA ASSESSMENT TOOL
Has the patient got diarrhoea? Bristol Stool Chart 5 – 7?
Increase in frequency from their normal pattern? Change in odour?
YES
Can diarrhoea be attributed to another cause?
e.g. inflammatory bowel disease, overflow, laxatives, enteral feeding, patient’s normal bowel habit, new medication.
YES NO
Clinical Review Review of clinical indicators, patient’s
general condition, abdominal examination, bloods including WCC &
CRP
Considered non-
infective diarrhoea Infective diarrhoea
suspected
Review / modify treatment e.g. antibiotics, laxatives, feeds etc.
Maintain enteric precautions and review patient’s clinical response in 24hrs
Take specimen Move to single room
Maintain enteric precautions
Senior clinical review must take place
Liaise with IP team and microbiologist re treatment
TAMESIDE HOSPITAL NHS FOUNDATION TRUST policy for the prevention and control of clostridium difficile associated diarrhoea
VERSION 5.0 (final) September 2015 Page 19 of 23
Check the Intranet for the latest version
APPENDIX 3 – SIGHT PROTOCOL
• Suspect infection when there is no clear
alternative cause for diarrhoea (type 5 - 7
Bristol stool chart)
• Isolate the patient within 2 hours if infective
diarrhoea is suspected
• Gloves and aprons must be used for all
contacts with the patient and their environment
• Hand washing with soap and water before and
after each contact with the patient and their
environment
• Test stool - send a specimen immediately
TAMESIDE HOSPITAL NHS FOUNDATION TRUST policy for the prevention and control of clostridium difficile associated diarrhoea
VERSION 5.0 (final) September 2015 Page 20 of 23
Check the Intranet for the latest version
APPENDIX 4 – CLINICAL MANAGEMENT OF PATIENTS WITH C. DIFFICILE DIARRHOEA
Isolate the patient in a single room AND implement enteric precautions
Physical examination (especially abdomen) The patient must be reviewed by the Doctor each day and more frequently if clinically indicated.
Record each review in the case notes.
Monitor stool using the Bristol Stool chart (to be kept at the bedside) recording stool type whenever stool is passed.
Immediate Review of Antibiotics by Consultant / Registrar
*please note mild to moderate symptoms do not require treatment.
Send bloods for WBC ,CRP urea and electrolytes and record results in the case notes. Repeat daily until diarrhoea has subsided.
Check and record vital signs (NEWS) – 4 hourly observations unless criteria changes and amend frequency as required.
Monitor fluid intake and output and record on the fluid balance chart / associated documentation
Clinical Management for Patients with Clostridium Difficile Diarrhoea
August 2015
TAMESIDE HOSPITAL NHS FOUNDATION TRUST policy for the prevention and control of clostridium difficile associated diarrhoea
VERSION 5.0 (final) September 2015 Page 21 of 23
Check the Intranet for the latest version
APPENDIX 5 – ASSESSMENT OF C. DIFFICILE SEVERITY AND TREATMENT
3-5 type 5-7 stools
*, WBC
Not raised treat for Mild. If diarrhoea is debilitating causing poor nutrition, weight loss, poor mobility treat as for moderate
Stop PPI’s if possible
*Using Bristol Stool Chart
No antibiotics required. Rehydrate and correct Electrolyte disturbance
Stool positive for Clostridium difficile toxin
Diarrhoea continues
Patient requires treatment – assess severity
No diarrhoea for at least 24 hr
Nurse patient in side room for the length of their hospital stay
Diarrhoea continues – 2 or more loose stools (entirely liquid – no solid pieces) in 24 hr
Patient asymptomatic (diarrhoea has resolved)
Enteric precautions including environmental cleaning by domestic services using Diff X and high level disinfectant wipes used by nursing staff. Use apron and gloves when caring for patient
Promptly (within 2 hr) transfer to a single room where available
Wash hands using soap and water
Review any current antibiotic treatment and if possible stop. If patient’s condition warrants continuation, seek advice of Microbiologist
Stop any medicines (if possible) that decrease stomach acid (e.g. proton pump inhibitors and H2 antagonists) also stop NSAID unless there is a compelling indication. Avoid enteral feeding if possible
Do NOT prescribe anti-diarrhoeal agents. Correct fluid loss and electrolyte imbalance
Enteric precautions – nurse in single room for length of hospital
stay No treatment required
Do not send further specimens unless symptoms recur, as stool can remain positive for several
weeks
Mild
No raised WBC
< 2 type 5 –7 stools* in 24 hr
Moderate
WBC raised, but < 15 x 10
9/L
> 5 type 5 – 7 stools* in 24 hr
Severe (1 of the following present):
WBC ≥15 x 109/L
Acute rising serum creatinine (>50% increase above baseline)
Temperature >38.5C
Evidence of severe colitis (abdominal or radiological signs)
Life threatening
Hypotension
Partial or complete ileus or toxic megacolon
CT evidence of severe disease
metronidazole 400mg orally (or 500mg 8hrly IV) up to 14 days if necessary. If any deterioration or not responding within 1 week treat as severe. If second relapse or unresponsive add vancomycin 125mg orally (not IV) qds
Vancomycin 500 mg orally 6 hrly for up to 14 days if necessary. Plus metronidazole 500 mg IV by infusion 8 hrly. If not improving consider surgical referral for review regarding colectomy
Involve surgeons for review regarding colectomy. Vancomycin 500 mg orally 6 hrly plus
metronidazole 500 mg IV by infusion 8 hrly for up to 14 days. Plus IV
immunoglobulin 400mg / kg as a single dose.
For multiple relapses fidaxomicin 200mg orallybd only on advice of Microbiologist
TAMESIDE HOSPITAL NHS FOUNDATION TRUST policy for the prevention and control of clostridium difficile associated diarrhoea
VERSION 5.0 (final) September 2015 Page 22 of 23
Check the Intranet for the latest version
APPENDIX 6 – BRISTOL STOOL CHART
Please record type and frequency on a stool chart.
TAMESIDE HOSPITAL NHS FOUNDATION TRUST policy for the prevention and control of clostridium difficile associated diarrhoea
VERSION 5.0 (final) September 2015 Page 23 of 23
Check the Intranet for the latest version
APPENDIX 7 - EQUALITY IMPACT ASSESSMENT TOOL
Yes/No Comments
1. Does the policy/guidance affect one group less or more favourably than another on the basis of:
Race No
Ethnic origins (including gypsies and travellers)
No
Nationality No
Gender No
Culture No
Religion or belief No
Sexual orientation including lesbian, gay and bisexual people
No
Age No
Disability - learning disabilities, physical disability, sensory impairment and mental health problems
No
2. Is there any evidence that some groups are affected differently?
No
3. If you have identified potential discrimination, are any exceptions valid, legal and/or justifiable?
N/A
4. Is the impact of the policy/guidance likely to be negative?
No
5. If so can the impact be avoided? N/A
6. What alternatives are there to achieving the policy/guidance without the impact?
N/A
7. Can we reduce the impact by taking different action?
N/A