Chikungunya PPT_RP
-
Upload
ruchi-pancholy-rehs -
Category
Documents
-
view
1.162 -
download
0
Transcript of Chikungunya PPT_RP

Ruchi Pancholy, MPH, REHSPHC 6002 Infectious Disease Epidemiology
Fall 2015 Disease PresentationOctober 29, 2015
Aurora Sanchez-Anguiano, MD, PhD, CPH
Chikungunya: An Emerging Arboviral Threat

Background Chikungunya (CHIK): Viral, Mosquito-Borne Disease transmitted to humans
Single-Stranded RNA Virus
Class: Arbovirus, Family: Togaviridae, Genus: Alpha virus (3 Known Strains)
Transmitted by: Two mosquito species/FemaleAedes aegypti (Primary Vector)Aedes albopictus
Name derived from Swahili word meaning “that which bends up”, referring to stooped posture of Chik virus patients/”Hallmark of Chik virus”
First isolated from serum of febrile human after a 1952-1953 outbreak in Tanzania
Detected in large outbreaks with high attack rates in Africa, Asia, Indian Ocean Islands, and Italy since 2004
Aggressive Day Time Biters

Disease Transmission Primary Reservoir: Humans Other Reservoirs: Monkeys, Rodents, Birds, & Some Small Mammals Transmission: Mosquito-Human-Mosquito-Human Cycle Primary Mode of Transmission: Mosquito Bite Other Modes of Transmission/ (Uncommon)
-In utero transmission, can cause miscarriage in 1st trimester- Intrabirth transmission, newborn of a viremic mother- Needle prick- Laboratory exposure
No evidence of virus in breast milk
Mosquito-Human-Mosquito-Human

Disease Transmission Human Incubation Period: 1-12 days (Average 3-7 Days), following bite of an infected mosquito Mosquito Incubation Period: Average 7-10 days; Once infected has virus until death (30 days)
Reference: Thinboutot M., et al., (2010). Chikungunya: A Potentially Emerging Epidemic. Neglected Tropical Diseases, 4 (4). Retrieved from:http://www.plosntds.org/article/info%3Adoi%2F10.1371%2Fjournal.pntd.0000623 on October 20, 2015.

Clinical Features Common Symptoms: Joint Pain, Fever (> 38.5 degrees), & Chills
Joint pain: So severe can’t leave bed; Symmetric in both arms/legs 85% of Exposed become Ill/15% are Asymptomatic Very similar to Dengue, except in Chik virus there is No
Hemorrhagic or Shock Syndrome
Other Symptoms: Maculopapular Rash, Headache, Back Pain, Myalgia, Retrorbital Pain, Arthritis, GI Symptoms & Severe Malaise
Two Phases: Acute & Chronic Acute: Generally lasts 1 Week (severe headache & malaise) Chronic: Months or years of rheumatic symptoms, fatigue and
depression; More likely in immunocompromised, elderly, neonates, & very young
Rarely fatal (Mortality<1%) but Morbidity high due to severity of disease

Clinical Features
Reference: Weaver C., Lecuit., M. (2015). Chikungunya Virus and the Global Spread of a Mosquito-Borne Disease. The New England Journal of Medicine, 372 (13), 1231-1239.

Clinical Features
Figure 1. Maculopapular Rash Figure 2. Hyperpigmentation Brownish colored lesions; Seen rarely but in some
cases
Reference: Kandhari R., Khunger N., Singh A. (2012). Flagellate pigmentation and exacerbation of melasma following Chikungunya fever: A less frequently reported finding. Indian Journal of Dermatology, 78 (6), 774.

Treatment & Prognosis To date, no specific treatment for Chik Virus Chik virus is a self-limiting illness with acute symptoms resolved in 7-10 days Recovery is Key! About 3-5% of patients are at risk for developing prolonged arthritis
Recommended Treatments:- Rest & Movement of Joints- Apply cold compresses to inflamed joints- Adequate fluid intake and/or IV fluids- Non-Steroidal Anti-Inflammatory Drugs (NSAIDS) for acute fever & pain** Aspirin use is discouraged due to risk of hemorrhage and Reye’s Syndrome* NSAIDS should be avoided until Dengue fever is ruled out, as NSAIDS are contraindicated in Dengue treatment.

Diagnostic Testing
*Virus should be handled under biosafety level 3 conditions
Diagnostic Assay Timing for Diagnostic Assays/Days Post-Illness Onset
Viral Culture* < 3 days
RT-PCR < 8 days
IgM antibody tests > 4 days (Up to several months after onset)
Where is testing performed?
CDC Arboviral Diseases Branch Several State Health Departments One Commercial Laboratory (Focus Diagnostics)
- Demonstrating four fold or greater rise in antibody titre
- The antibody titre will positive after 5th day of illness only

Case Definition of Chikungunya Suspect Case: Acute onset, high fever, 7 days duration, severe
headache, myalgia, severe arthralgia, with or without rash
Probable Case: Suspect case of Chik virus, high vector density, presence of confirmed case in area.
Confirmed Case:- Isolation of virus in early phase. Serological test for IgM antibody after 5th day of illness. Demonstration of 4 fold or greater rise in IgG antibodies in paired sera

Chik Virus Epidemiological Patterns Age Group: Above 15 Years (Less Common in Infants &
Children)/Although children under 1 are considered a High-Risk Group
Gender: Seen more in Females
Ethnicity/Education/Occupation: To date, limited information exists in literature
Family cluster of cases common
Urban Areas: More Cases Identified
Attack rates vary from 3 to 45% of Population; Average Attack Rate: 10%

Chik Virus Epidemiological PatternsTable 1. Characteristics of Chikungunya
Cases Identified in the US, 1995-2009 (N=109) Characteristic No. of
Cases (%) of cases
Age, Years
0-19 0 (0)
20-39 31 (28)
40-59 57 (52)
> 60 16 (15)
Unknown 5 (5)
Sex
Female 62 (57)
Male 46 (42)
Unknown 1 (1)
Reference: Gibney K., et al. (2011). Chikungunya Fever in the United States: A Fifteen Year Review of Cases. Clinical Infectious Diseases, 52 (5), e121-e126.

Seasonal Distribution of Chik Virus
Figure 2: Month of illness onset of chikungunya fever cases identified in the United States, 1995-2009. Reference: Gibney K., et al. (2011). Chikungunya Fever in the United States: A Fifteen Year Review of Cases. Clinical Infectious
Diseases, 52 (5), e121-e126.

Seasonal Distribution of Chik Virus Heat, Humidity, & Rainfall: Ideal
conditions for mosquito growth & replication
Geographic areas with seasonal variation in temperature have particular months (In US: April through October) during which mosquitoes multiply & survive.
Timing & duration of high-transmission seasons varies substantially across 53 different countries (Figure 1).
Figure 1: Seasonal pattern of projected weekly RO by country, Countries are sorted by the latitudes of their capital citiesReference: Perkins TA., et al. (2015). Estimating Drivers of Autochthonous Transmission of Chikungunya virus in its Invasion of the Americas. PLOS
Current Outbreaks, 1, 1-28.

Chik Virus Affects More than 1 Million Individuals Across the Globe
Figure 3: Countries and territories where chikungunya cases have been reported (as of March 10, 2015), CDC Reference: Centers for Disease Prevention and Control [CDC] (2015). Chikungunya virus. Retrieved from:
http://www.cdc.gov/chikungunya/geo/index.html on October 20, 2015.

Countries with Reported Local Transmission of Chikungunya virus
Figure 4: Countries with Reported Local Transmission of Chikungunya virusReference: CDC (2015). Chikungunya virus. Retrieved from: http://www.cdc.gov/chikungunya/geo/index.html on October 20, 2015.

Chikungunya in USA, 1/1-10/13/15 N=524
Figure 5. States reporting Chikungunya virus disease cases- United States, 2015 (as of October 13, 2015)Reference: CDC. (2015). Arboviral Diseases Branch. October 6, 2015.
*Includes Provisional Data reported to ArboNet
Florida, N=58

Chikungunya in Florida Florida has abundance of principal vector
species, Aedes aegypti
So far in 2015: 61 lab confirmed, Chik virus cases reported in Florida (All travel-associated)
In 2014: Florida was second state reporting largest number of lab confirmed Chik virus cases (N=476); 17 travel-associated, 11 locally acquired
In 2014: Florida was first and only state to report locally acquired cases (N=11)
In 2014: The 11 local cases reported from 4 South Florida counties: Palm Beach (N=4), St. Lucie (N=4), Miami Dade (N=2), & Broward (N=1)

Chikungunya in Florida Florida: US State with highest average
temperature in June with aedesmosquito species
Chik Virus Outbreaks in Florida: Occurred over past three decades
Florida has strong potential for new locally acquired cases & outbreaks
Miami, Florida: Third highest travel volume city in the world, majority travel to Caribbean Island, abundance of Aedes mosquitoes, and climate
Figure 5: Volume of Travellers from Chikungunya Indigenous Areas of the Caribbean to the United States and Canada in May 2012Reference: Bogoch K., et al. (2014). Assessing the Origin of and Potential for International Spread of Chikungunya Virus from the Carribbean.
PLOS, 1, 1-15.

Major Risk Factors Environment: Damp marshy, and/or Mosquito Prone Areas, Areas with
stagnant or collected water (e.g., Household Containers, Pools, etc.)
Climate: Hot, humid rainy season
High Risk Individuals: Immunocompromised, Care Givers of Chik Virus Patients, Pregnant, Women in General, Newborns, Elderly (> 65 Years)
Those with Co-existing Medical Conditions: Diabetes, Cardiovascular, Neurologic, & Respiratory Diseases, High Blood Pressure
Increased Disease Severity

Preventative Measures No vaccine or medication currently available to prevent
infection
Mosquito Control: Most effective preventative measure. BG Sentinel trap most effective for surveillance.
Health Education: Advise high-risk individuals (e.g. immunocompromised) to avoid travelling to areas with ongoing outbreaks
Inform travelers going to regions with known virus transmission about risk of disease
Protect infected individuals from further mosquito exposure during the first week of illness

Mosquito Control PreventionSeal window/door screens and use air conditioning
Apply mosquito repellant on exposed skin
Wear long-sleeved clothing
Empty standing water from containers, old tires, coolers, pools, buckets, etc.
Insecticide treated curtains & clothing

Future DirectionsWhat is Known?
Adequate Knowledge on: Disease Transmission, Biological Plausibility, Risk Factors, Preventative Measures (Vector Control), and Pathogenesis of Chik virus
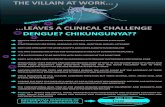
Chik virus: A Relatively Recent Threat; Not as much research conducted on it as Dengue Fever
What is Not Known?
Questions regarding targeted therapeutic and preventative strategies remains unanswered
Chikungunya virus replication and host-cell response Unknown; Key to Development of Antiviral Agents
Forecasting and Prediction of future outbreaks is critical Misdiagnosis with dengue fever common; How to handle concurrent outbreaks Further research to understand adaption of virus to mosquito vectors

Future DirectionsWhere are We Going?
Chik virus likely to spread exponentially across the world, esp. the Americas due to increased air travel, migration, global trade, and denser human and mosquito populations
Previously unexposed individuals will be at greater risk in future
Non-endemic regions will experience new cases (esp. due to climate change and global warming)
What Needs to be Done?
A vaccine, post-exposure prophylaxis, and/or drugs need to be tested & developed soon Further Studies, (e.g., Clinical Trials) Needed: Test efficacy of Potential Drugs & Vaccines Evaluate vector competence of mosquito populations to assess risk of future transmission &
spread Cases frequently underreported and unrecognized Educate healthcare providers Development & Validation of Additional Laboratory and Rapid Point of Care Diagnostics

Rationale/Project
Reference: Ramsaver K., et al. (2015). Immunogenicity, safety, and tolerability of a recombinant measles-virus-based chikungunya vaccine: a randomized, double-blind, placebo-controlled, active-comparator, first-in-man trial. Lancet Infec Dis, 15, 519-27.
Project: Randomised, double-blind, placebo-controlled first-in-man trial of a recombinant measles-virus-based Chik virus vaccine
Why?: No Chik virus vaccine available, severe morbidity, escalating medical costs associated with treating the disease; Investigate safety & efficacy of a live recombinant measles-virus based Chik virus vaccine
Methods: Healthy adults aged 18-45 (N=42), with no comorbidities randomly assigned to receive 1 of 3 doses of measles-virus-based vaccine [low, n=12] [medium, n=12] or [high, n=12] dose
Efficacy of vaccine: Determined by presence of neutralizing anti-chikungunya antibodies on day 28, assessed by 50% plaque reduction neutralization test
Results: Vaccine produced neutralizing antibodies in all dose cohorts after 1 immunization; seroconversion rates of 44% (n=4) low dose group, 92% (n=11) medium dose group, 90% (n=10) high dose group. Overall, vaccine found safe; rate of adverse events increases with vaccine dose & volume.
Significance: First Promising Measles-Virus-Based Vaccine for human beings. Herd immunity important in preventing future outbreaks due to nature of its’ man-to-mosquito-man transmission cycle.

Selected ReferencesBogoch K., et al. (2014). Assessing the Origin of and Potential for International Spread of Chikungunya Virus from the Carribbean. PLOS, 1, 1-15.
Christofferson R., et al. (2014). Chikungunya Viral Fitness Measures within the Vector and Subsequent Transmission Potential. PLOS One, 9 (10), 1-8.
Centers for Disease Control and Prevention [CDC]. (2015). Arboviral Diseases Branch. October 6, 2015.
Centers for Disease Prevention and Control [CDC] (2015). Chikungunya virus. Retrieved from: http://www.cdc.gov/chikungunya/geo/index.html on October 20, 2015.
Gibney K., et al. (2011). Chikungunya Fever in the United States: A Fifteen Year Review of Cases. Clinical Infectious Diseases, 52 (5), e121-e126.
Kandhari R., Khunger N., Singh A. (2012). Flagellate pigmentation and exacerbation of melasma following Chikungunya fever: A less frequently reported finding. Indian Journal of Dermatology, 78 (6), 774.
Kendrick, K., Stanek, D., Blackmore, C. (2014). Notes from the field: Transmission of chikungunya virus in the continental united states—Florida 2014. MMWR Morb Mortal Wkly Rep 2014; 63 (48), 1137.
Mardekian, S., & Roberts, A. (2015). Diagnostic Options and Challenges for Dengue and Chikungunya Viruses. Hindawai Publishing Corporation, 2015, 1-8.
Nasci, R. (2014). Movement of Chikungunya Virus into the Western Hemisphere. Emerging Infectious Diseases, 20(8), 1394-1395.
Perkins TA., et al. (2015). Estimating Drivers of Autochthonous Transmission of Chikungunya virus in its Invasion of the Americas. PLOS Current Outbreaks, 1, 1-28.
Porse C., et al. (2015). Public Health Response to Aedes aegypti and Ae. Albopictus Mosquitoes Invading California, USA. Emerging Infectious Diseases, 21(10), 1827-1829.
Ramsaver K., et al. (2015). Immunogenicity, safety, and tolerability of a recombinant measles-virus-based chikungunya vaccine: a randomized, double-blind, placebo-controlled, active-comparator, first-in-man trial. Lancet Infec Dis, 15 (15), 519-27.
Rudd A., & Mahalinham S. (2015). Fighting back against Chikungunya. Lancet Infec Dis, 15 (15), 488-89.

Selected References, cont’d
Vega-Rua, A., (2014). High level of Vector Competence of Aedes aegypti and Aedes albopictus from Ten American Countries as a Crucial Factor in the Spread of Chikungunya Virus. Journal of Virology, 88 (11), 6294-6304.
Weaver C., & Lecuit., M. (2015). Chikungunya Virus and the Global Spread of a Mosquito-Borne Disease. The New England Journal of Medicine, 372 (13), 1231-1239.
Ruiz-Moreno, D. (2012). Modelling Dynamic Introduction of Chikungunya Virus in the United States. PloS Neglected Tropical Diseases, 6 (11), 1-8. Thiberville, S., et al. (2013). Chikungunya fever: Epidemiology, clinical syndrome, pathogenesis and therapy. Antiviral Research, 99, 345-370.
Kendrick, K., Stanek, D., Blackmore, C. (2014). Notes from the field: Transmission of chikungunya virus in the continental united states—Florida 2014. MMWR Morb Mortal Wkly Rep 2014; 63 (48), 1137.
Sharp T., et al., (2014). Chikungunya Cases Identified Through Passive Surveillance and Household Investigations- Puerto Rico, May 5-August 12, 2014. MMWR Morb Mortal Wkly Rep 2014; 63 (48), 1121-1128.

QUESTIONS