Case presentation pleural effusion
-
Upload
jagadish-mishra -
Category
Health & Medicine
-
view
202 -
download
9
Transcript of Case presentation pleural effusion
CLINICAL CASE PRESENTATION
GROUP-4 ROLL NO:- 16-20
(JAGADISH, JOHN, KULDEEP, MAHESH, MAMTA)
Case:- Pleural effusion
•CR NO:- C-2353• Name - Mr. Rinku Parida • Age - 22yr• Gender - male• Address- Delanga, Puri• Diagnosis- Right side pleural effusion
Patientdetails
CONTD…
•Dept. - Pulmonary Medicine• Ward - Medical Ward• Bed No - 06• Date of Admission - 27/08/2014•Period of observation- 7 Days• Physician- Dr. Manoj Panigrahi
asst. professor Pulmonary medicine
History•Chief complaints:-
High fever – 14 days Right side chest pain- 14 days•History of present illness:- Apparently all right 2 weeks ago high grade fever (remittent)-14 days pain in right side chest-14 days (sharp, stabbing, intensified by deep inspiration/cough) cough-14 days sputum- white, purulent(blood tinged sputum one episode- 10 days back) Loose stool, right lumber pain -10 days
•Past history:- noh/osimilarepisodesinpastnoh/oanychronicdiseases(DM,HTN,thyroiddisorder,CVSdisorder,Bronchialasthma)•History of allergy:- noallergichistory
•Family history:- notsignificant
•Treatment history:- paracetamol(SOS)- 5 days before hospitalization
•Personal history:- nosmokinghistory,bladder&bowelhabitnormal
Examination
•General examination–Thin built–Orientationnormal–Pallor absent–Icterus absent–Cyanosisabsent–Edemaabsent–Clubbingabsent–JVP notraised–Lymphadenopathyabsent–Organomegalyabsent–Temperature :-101F( axillary)
SYSTEMIC EXAMINATION•Respiratory system:- Inspection:-normalshape, RR:-30/min, regular,abdominal-thoracictyperespirationbilateralsymmetricalchestmovement
Palpation:-tracheacentral,apexbeat-5thintercostalspace,symmetricalexpansion
tenderness at right side chest Percussion:- mild dullness over the right chest(infra axillary)
CONTD…
Auscultation:- bilateralvesicularbreathsounds+, diminished in right side(infra axillary), noadditionalsound
•Abdominal examination:- nolump,visiblepulsesorperistalsispresentNoorganomegalypalpable
CONTD….
•CVS:-–Pulse -110bpm,regular,normalvolume,
noradio-radial/radio-femoraldelay,allperipheralpulsespalpable,arterialwallnormal–BP–94/54mmHginrighthandinsupine
position–HeartsoundsS1,S2auscultated–noadditionalsounds
•CNS:- notsignificant
INVESTIGATIONSureaserum-29.00mg/dl(17-43)creatinineserum-1.20mg/dl(0.8-1.25)
LIVER FUNCTION TEST:- S.BILIRUBIN(TOTAL)-1.00mg/dl(0.3-1.2)S.BILIRUBIN(DIRECT)-0.30mg/dl(0-0.2)S.BILIRUBIN(INDIRECT)-0.70mg/dl(0-0.7)ALT- 84 U/L(0-50)AST-39U/L(0-50)ALP- 273 U/L(34-104)TOTALPROTEIN-7.10g/dl(6.5-8.3)Serum albumin- 2.5g/dl(3.5-5.2) Serum globulin- 4.6g/dl(2-3.5) A:G Ratio- 0.54(1.2-2.5)
URINE ROUTINE EXAMINATION:-Colour- pale yellowAppearance- clear pH- 7.00(4.6-8.0)Specific gravity- 1.025(1.001-1.035)Glucose- -veAlbumin- -veWBC/HPF- 2-4/HPFRBC/HPF- NILEPITHELIAL CELL/HPF- 6-8/HPFCASTS- NILCRYSTAL- NIL
CONTD..
•SERUM ELECTROLYTES-Na(ISEindirect)-130mmol/L(135-145mmol/L)K-5.10mmol/L(3.5-5.0mmol/L)Cl-98mmol/L(98-111mmmol/L)
MALARIA ANTIGEN TEST:- -VE SPUTUM ( for AFB):- -VE
COMPLETE BLOOD COUNT:- hemoglobin- 13.10 g/dl (13-17) hematocrit-41% (40-50) RBC count-6.62x10^6/ul (4.5-5.5) MCV-61.91 fl (83-101) MCH-19.80 pg (27-32) MCHC-32.00 g/dl (31.5-34.5) Platelet- 320x10^3/ul (150-410) TLC-10.34x10^3/ul (4.0-11.0) Neutrophil-81% (40-80) Lymphocyte-14% (20-40) Monocyte-2% (2-10) Eosinophil-3% (1-4) Basophil-0% (0-2)
CONTD….
WIDAL(SLIDE AGGLUTINATION TEST):-
Salmonella typhi “o” 1:80Salmonelle typhi “h” 1:40Salmonella paratyphi “A(H)” 1:40Salmonella paratyphi “B(H)” 1:40 TITRE >1:80 IS SIGNIFICANT
CONTD…FBS,RBS:-NORMAL
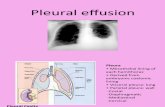
X ray DONE
USG Thorax:- Pleural effusion found
PLEURAL ASPIRATION DONE:- 10 ml straw col. Fluid protein- 5.50 mg/dl
Provisional diagnosis:- Pleural Effusion(EXUDATE TYPE)
Differential diagnosis:- Pneumonia, pulmonary consolidation, Chronic lung abscess
S.No Date Drugsgiven Dose Frequency Route
1. 27.08.2014–02.09.2014
TAB RABEPRAZOLE
40mg OD ORAL
2.27.08.2014–29.08.2014
30.08.2014–02.09.2014
TAB PARACETAMOL
650mgSOS
TDORAL
3. 27.08.2014–02.09.2014
INJ AMOXYCLAV
1.2g TD I.V
4. 28.08.2014–02.09.2014
TAB AZITHROMYCIN
500mg ODORAL
5. 30.08.2014–02.09.2014
INJ LEVOFLOXACIN
500mg OD I.V
6. 31.08.2014–02.09.2014
SYP GRILINCTUS
2TOP BD ORAL
TREATMENT GIVEN
•Summary of treatment given–Symptomatic–Curative
•Advice:- proper diet , medicine on time
•ADR:- noADR
Azithromycin:-(macrolide), better tolerability, rapid oral absorption High activity- against respiratory pathogens ,1st choice in Legionnaire's pneumonia , chlamydia trachomatis, Donovanosis t ½:-.50 hrs
Amoxicillin:- oral absorption good, effective against penicillin resistant Strep. Pneumoniae
Levofloxacin:- active against Strep. Pneumoniae , oral bioavailability 100% indication in community acquired pneumonia and chronic bronchitis
Paracetamol:-analgesic & antipyretic >10 g – toxicity
Rabeprazole:- newer PPI ,fastest acid suppression
DETAILS ABOUT DRUGS:-
Discussion about pharmacotherapy
•Details about the drugs•Details
•Rationale of therapy•The treatment given is Rationale.
•Is there an STG available? Was it followed ?
•An STG is avilable. It was followed.
STG•Treatment: Pleural effusion
•Standard Operating procedure (IN TERTIARY CARE HOSPITAL-
AIIMS)
•a. In Patient
•Pleurodesiswithdoxycycline–recurrentmalignantpleuraleffusion
•Chesttubeinstilledfibrinolytictherapy(streptokinase)-
parapneumoniceffusions
•VATS(thoracotomy,ifVATSnotavailable)-non-resolvingempyema
•b. Out Patient
•Treatmentofprimarysystemicillness
IN SECONDARY CARE HOSPITALPleuraleffusion
Therapeuticthoracocentesis-symptomaticreliefofdyspnea(Caveat:notmorethan1litreofpleuralfluidshouldberemovedtoprevent
postthoracocentesisshockandre-expansionpulmonaryedemainonesitting)Inatransudate,theprimarycausehastobemanaged.
Exudativeeffusions.Tuberculosis:asperRevisedNationalTuberculosisControlProgram
(RNTCP)guidelinesItneedstoberememberedthatincasesofsuspectedempyema,establishingthediagnosisasearlyaspossibleafteradmissionisthekey.AdelayintheinstitutionofICDevenbyafewmorehoursresultsinmorefibrosisandloculations,whichfurthercomplicatethelongtermmanagement.
Atadmission,thefollowingcriteriahelpindecidingtheplaninthesepatients
PFbacteriologyPFpHChesttubedrainageCultureand/orGramstain->7.2NoCultureand/orGramstain+<7.2Yes
Frankpus<7Yes
CONTD…
•Was proper route, dose, frequency and duration followed ?
•Yes
•What was the adherence ?•The patient sticks to the treatment
guidelines
•What was the cost of pharmacotherapy?
•A total of Rs.1500 has been spent by the patient
CONTD..•How you would have treated the case?/ Alternative treatment
• No alternative therapy is required because at present no causative factor/organism is found so only empirical therapy & the symptomatic relief of the patient is to be done which requires the given medicines only.
•Overall comments•The patient is not diagnosed with any
infectious disease which may explain his febrile condition. He has been given symptomatic & curative medication only.
Reference
•Pathological basis of Disease, Robbins and Cotran
•Essential of Medical Pharmacology, KD Tripathy
•Clinical Establishment Act 2010