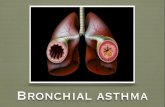
Bronchial Asthma
-
Upload
rohitkumar -
Category
Documents
-
view
10 -
download
0
description
Transcript of Bronchial Asthma

BRONCHIAL ASTHMAPRESENTER : DR. SHREYAMODERATOR : DR. ROHAN

Asthma is a chronic inflammatory disorder of the airways characterized by airway hyperresponsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness, and coughing. These episodes are usually associated with widespread, but variable, airflow obstruction within the lung that is often reversible either spontaneously or with treatment.

300 million affected individuals in the world. global prevalence of asthma ranges from 1% to 18% 15 million disability-adjusted life years(DALYs) are
lost annually due to asthma, 1% of the total global disease burden.

HOST FACTORS◦ Genetic◦ Obesity◦ Sex
ENVIRONMENTAL FACTORS◦ Allergens◦ • Indoor: Domestic mites◦ • Outdoor: Pollens, fungi◦ Infections (predominantly viral)◦ Occupational sensitizers◦ Tobacco smoke◦ Outdoor/Indoor Air Pollution◦ Diet
FACTORS INFLUENCING THE DEVELOPMENTAND EXPRESSION OF ASTHMA

epithelial cells smooth muscle cells Endothelial cells Fibroblasts and myofibroblasts Airway nerves
AIRWAY STRUCTURAL CELLS INVOLVED IN THEPATHOGENESIS OF ASTHMA

Chemokines Cysteinyl leukotrienes: mast cells and eosinophils. Cytokines: IL-1 and TNF-alpha Histamine: mast cells Prostaglandin D2: mast cells
KEY MEDIATORS OF ASTHMA


Airway smooth muscle contraction Airway edema Airway thickening Blood vessels proliferate Mucus hypersecretion Subepithelial fibrosis

episodic breathlessness, wheezing, cough, and chest tightness
seasonal variability of symptoms and a positive family history of asthma and atopic disease
precipitation by non-specific irritants, such as smoke, fumes, strong smells, or exercise; worsening at night; and responding to appropriate asthma therapy.
CLINICALS

H/o recurrent attacks of wheezing• H/o cough at night.• H/o wheeze or cough after exercise• H/o wheezeing, chest tightness, orcough after exposure to airborne allergens or
pollutants• symptoms improved by appropriate asthma
treatment

1.MEASUREMENTS OF LUNG FUNCTIONSPIROMETRY: measurement of forced expiratory volume in 1
second (FEV1) forced vital capacity (FVC) peak expiratory flow (PEF) measurement.
REVERSIBILITY: applied to rapid improvements in FEV1 (or PEF), measured within minutes after
inhalation of a rapid-acting bronchodilation.
VARIABILITY: refers to improvement or deterioration in symptoms and lung function occurring over time

DIAGNOSIS OF ASTHMA: 60 L/min (or 20% or more of prebronchodilatorPEF) improvement after inhalation of aBronchodilator or diurnal variation in PEF of morethan 20% (with twice daily readings, more than 10%.

2.MEASUREMENT OF AIRWAY RESPONSIVENESS levels of exhaled nitric oxide (FeNO) and carbon
monoxide (FeCO)
3.MEASUREMENTS OF ALLERGIC STATUS Skin tests with allergens

CLASIFICATION OF ASTHMA BY SEVERITY

INTERMITTENT Symptoms less than once a week Brief exacerbations Nocturnal symptoms not more than twice a month
- FEV1 or PEF ≥ 80% predicted- PEF or FEV1 variability < 20%
Mild Persistent Symptoms more than once a week but less than once a
day Exacerbations may affect activity and sleep Nocturnal symptoms more than twice a month
- FEV1 or PEF ≥ 80% predicted- PEF or FEV1 variability < 20 – 30%

MODERATE PERSISTENT Symptoms daily Exacerbations may affect activity and sleep Nocturnal symptoms more than once a week Daily use of inhaled short-acting 2-agonist
- FEV1 or PEF 60-80% predicted- PEF or FEV1 variability > 30%
SEVERE PERSISTENT Symptoms daily Frequent exacerbations Frequent nocturnal asthma symptoms Limitation of physical activities
- FEV1 or PEF ≤ 60% predicted- PEF or FEV1 variability > 30%

Characteristic Controlled(All of the following)
Partly Controlled(Any measure present in any week)
Uncontrolled
Daytime symptoms None (twice or less/week)
More than twice/week Three or more features of partly controlledasthma present inany week
Limitations of activities
None Any
Nocturnal symptoms/awakening
None Any
Need for reliever/rescue treatment
None More than twice/week
Lung function (PEF or FEV1)‡
Normal < 80% predicted or personal best(if known)
Exacerbations None One or more/year One in any week
LEVELS OF ASTHMA CONTROL


ACUTE SEVERE ASTHMA

MILD MODERATE SEVERE RESPIRATORY ARREST
BREATHLESS WALKING TALKINGPREFERS SITTING
AT RESTHUNCHED FORWARD
TALKING SENTENCES PHRACES WORDS
ALERTNESS MAY BE AGITATED
AGITATED AGITATED DROWSY OR CONFUSED
RESPIRATORY RATE
INCREASED INCREASED
ACCESSORY MUSCLES AND CHEST RETRACTIONS
NOT SEEN USUALLY SEEN
USUALLY SEEN
PARADOXICAL THORACO ABDOMINAL MOVEMENT
WHEEZE MODERATE, EXPIRATORY
LOUD LOUD ABSENSE OF WHEEZE
SEVERITY OF ASTHMA EXACERBATIONS

MILD MODERATE SEVERE RESPIRATORY ARREST
PULSE < 100 100-120 >120 BRADYCARDIA
PULSES PARADOXUS
ABSENT< 10 mm Hg
MAY BE PRESENT10-25 mmHg
OFTEN PRESENT>25 mmHg
ABSENCE SUGGESTS RESPIRATORY MUSCLE FATIGUE
PEF% predicted
OVER 80% 60-80% < 60%
PaO2 and /orPaCO2
NORMAL
< 45mmHg
60 mm Hg
< 45mmHg
< 60 mmHg
>45mmHg
SaO2 >95% 91-95% <90%

INITIAL ASSESSMENT ◦ History, physical examination (auscultation, use of accessory
muscles, heart rate, respiratory rate, PEF or FEV1, oxygen◦ saturation, arterial blood gas if patient in extremis)
REASSESS AFTER 1 HOUR◦ Physical Examination, PEF, O2 saturation and other tests as
needed
INITIAL TREATMENT• Oxygen to achieve O2 saturation ≥ 90% • Inhaled rapid-acting 2-agonist continuously for one hour.• Systemic glucocorticosteroids if no immediate response,
or if episode is severe.• Sedation is contraindicated in the treatment of an
exacerbation.

REASSESS AFTER 1 HOUR Physical Examination, PEF, O2 saturation and other tests as
neededCRITERIA FOR MODERATE EPISODE:• PEF 60-80% predicted/personal best• Physical exam: moderate symptoms, accessory muscle useTREATMENT:• Oxygen• Inhaled 2-agonist and inhaled anticholinergic every 60 min• Oral glucocorticosteroids• Continue treatment for 1-3 hours, provided there is
improvement

CRITERIA FOR SEVERE EPISODE:• History of risk factors for near fatal asthma• PEF < 60% predicted/personal best• Physical exam: severe symptoms at rest, chest retraction• No improvement after initial treatmentTREATMENT:• Oxygen• Inhaled 2-agonist and inhaled anticholinergic• Systemic glucocorticosteroids• Intravenous magnesium

REASSESS AFTER 1-2 HOURSGood Response within 1-2 Hours:• Response sustained 60 min after last treatment• Physical exam normal: No distress• PEF > 70%• O2 saturation > 90% Improved: Criteria for Discharge Home• PEF > 60% predicted/personal best• Sustained on oral/inhaled medication

INCOMPLETE RESPONSE WITHIN 1-2 Hours: Risk factors for near fatal asthma Physical exam: mild to moderate signs PEF < 60% O2 saturation not improvingADMIT TO ACUTE CARE SETTING• Oxygen• Inhaled 2-agonist ± anticholinergic• Systemic glucocorticosteroid• Intravenous magnesium• Monitor PEF, O2 saturation, pulse

POOR RESPONSE WITHIN 1-2 HOURS:• Risk factors for near fatal asthma• Physical exam: symptoms severe,drowsiness, confusion• PEF < 30%• PCO2 > 45 mm Hg• P O2 < 60mm HgADMIT TO INTENSIVE CARE• Oxygen• Inhaled 2-agonist + anticholinergic• Intravenous glucocorticosteroids• Consider intravenous 2-agonist• Consider intravenous theophylline• Possible intubation and mechanicalventilation

THANK YOU