August / September September is Sepsis Awareness Month SEPTEMBER… · sepsis as a systemic host...
Transcript of August / September September is Sepsis Awareness Month SEPTEMBER… · sepsis as a systemic host...

August / September 2015
INSIDE THIS EDITION:
Dept Meetings/Conf New Appointments
Feature Stories/
Announcements:
ICD-10 Champions
ICD-10 Hotline
ICD-10 Raffle Winners
Valley Receives Gold-
Level Recognition
Physician Inspires
Philanthropy
Update on Dense
Breasts and Screening
On Track with the PAC
Electrophysiology Edu-
cational Event
Save the Date: Valley
Hospital Foundation
Save the Date: The
Holiday Soirée
Editors Elizabeth Leahy [email protected] Margaret (Peggy) Moran [email protected] Joseph Yallowitz, MD [email protected]
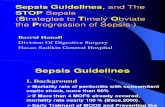
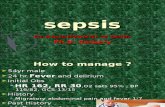
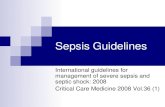
September is Sepsis Awareness Month
Sepsis historically has been a condition that is difficult to identify and diagnose. As far back as 100 BC, Marcus Terentius Varro, the ancient Roman scholar and writer (116 BC–27 BC), was quoted as noting that “small creatures, invisible to the eye, fill the atmosphere, and breathed through the nose cause dangerous diseases.” Perhaps the most prescient description of sepsis was by the historian, philosopher, humanist and Renaissance author Niccolo Machiavelli (1469–1527), as reported in his treatise, The Prince, in 1513. He very eloquently stated that, “hectic fever, at its inception, is difficult to recognize but easy to treat; left unattended it becomes easy to recognize and difficult to treat.” Although hectic fever is not the name by which we know sepsis now, the description of a disease that is difficult to recognize in its early stages, at a time when the condition may be amenable to treatment, and more difficult to treat in its later more obvious stages is a clear description of the more severe forms of sepsis.
In an attempt to better clinically understand sepsis, in the past century, a variety of definitions have been developed. Among the earliest concepts was to consider sepsis as a systemic host response to an infection. In fact, it was classically de-scribed by the eminent American physician William Osler (1849–1919) in his semi-nal observation that the patient appears to die from the body's response to an in-fection rather than from the infection itself.
Ignaz Semmelweis (1818-1865) was an obstetrician at the Vienna General Hospi-tal at a time when the death of women in childbed from puerperal fever was a com-mon complication. Semmelweis discovered that it was common for medical stu-dents to examine pregnant women directly after pathology lessons. Hygienic measures such as hand washing or surgical gloves were not yet customary prac-tice.
Semmelweis deducted that childbed fever was caused by "decomposed animal matter that entered the blood system". He succeeded in lowering the mortality rate by introducing hand washing with a chlorinated lime solution before every gyneco-logical examination. However, in spite of this clinical success, these hygienic measures were not accepted, and colleagues harassed him, forcing him to leave the city. It took him until 1863, more than 15 years after his findings, to publish his work "Aetiology, terminus and prophylaxis of puerperal fever.”
Although antiseptic procedures meant a huge medical breakthrough, it soon be-came apparent that a number of patients still developed sepsis. In this pre-antibiotic time, the death rate was very high. Only with the introduction of antibiot-ics after WW II could the death rate of sepsis be reduced.
While the literature continues to evolve, the mainstay of treating sepsis is prompt recognition and early goal-directed therapy. September is Sepsis Awareness month and you can learn more about efforts to raise awareness at http://www.sepsisalliance.org Joseph Yallowitz, MD Editor

SEPTEMBER 2015 DEPARTMENT MEETINGS
Otolaryngology Thursday, Sept. 3 8:00 a.m. CC-3 Family Practice Friday, Sept. 4 8:00 a.m. CC-6 Anesthesia Tuesday, Sept. 8 7:00 a.m. CC-7 Surgery Tuesday, Sept. 8 7:30 a.m. Board Room Pediatrics Tuesday, Sept. 8 9:00 a.m. Auditorium Medicine – CME Wednesday, Sept. 9 6:00 p.m. CC-7 Neurology Monday, Sept. 14 7:30 a.m. CC-7 Podiatry Tuesday, Sept. 15 7:30 a.m. Medical Library Emergency Medicine Wednesday, Sept. 16 6:00 p.m. CC-7 Neurology Monday, Sept. 21 7:30 a.m. CC-7 Anesthesia Tuesday, Sept. 22 7:00 a.m. Kurth Surgery Tuesday, Sept. 22 7:30 a.m. CC-7 Orthopedic Surgery Tuesday, Sept. 22 7:30 a.m. Auditorium Pediatrics Tuesday, Sept. 22 9:00 a.m. CC-7 Neurology Monday, Sept. 28 7:30 a.m. CC-7 OB/GYN Wednesday, Sept. 30 7:00 p.m. Terrace
SEPTEMBER 2015 COMMITTEE/CONFERENCE MEETINGS
Palliative Care Wednesday, Sept. 2 12:00 p.m. CC-5 Lung Management Conference Thursday, Sept. 3 12:00 p.m. CC-5 Credentials Committee Tuesday, Sept. 8 12:00 p.m. Board Room Endoscopy Committee Tuesday, Sept. 8 12:00 p.m. CC-3 Palliative Care Wednesday, Sept. 9 12:00 p.m. CC-7 Pediatric Critical Care Wednesday, Sept 9 9:00 a.m. Board Room GYN Cancer Conference Wednesday, Sept. 9 5:00 p.m. Luckow Conf. Room Officers’ Council Friday, Sept. 11 7:00 a.m. Admin. Conf. Rm. #1 Breast Management Conference Monday, Sept. 14 12:00 p.m. Luckow Conf. Room Surgical Control Committee Wednesday, Sept. 16 7:00 a.m. CC-7 Cancer Committee Tuesday, Sept. 15 12:00 p.m. Luckow. Conf. Room Patient Safety Tuesday, Sept. 15 4:00 p.m. CC-7 Palliative Care Wednesday, Sept. 16 12:00 p.m. Cheel Conf. Room 2 Infection Committee Wednesday, Sept. 16 12:00 p.m. Board Room Breast Management Conference Monday, Sept. 21 12:00 p.m. Luckow Conf. Room GI Liver Conference Monday, Sept. 21 1:00 p.m. Cheel Conf. Room 2 Medical Board Monday, Sept. 21 4:30 p.m. Board Room Pharmacy and Therapeutics Tuesday, Sept. 22 8:30 a.m. Board Room Palliative Care Wednesday, Sept. 23 12:00 p.m. CC-5 Medical Record Committee Thursday, Sept. 24 7:30 a.m. Board Room Breast Management Conference Monday, Sept. 28 12:00 p.m. Luckow Conf. Room Hematology/Onc. Cancer Conf. Tuesday, Sept. 29 12:00 p.m. Board Room Palliative Care Wednesday, Sept. 30 12:00 p.m. CC-7
SEPTEMBER 2015 PEER REVIEW COMMITTEES
Surgery Tuesday, Sept. 1 7:00 a.m. CC-2 Cardiovascular Monday, Sept. 7 4:00 p.m. Board Room MSQAIC Monday, Sept. 7 6:00 p.m. Board Room Neuroscience Thursday, Sept. 10 7:30 a.m. CC-2 Women & Children’s Services Monday, Sept. 14 8:00 a.m. Board Room Musculoskeletal Thursday, Sept. 17 7:00 a.m. CC-2 Medicine Wednesday, Sept. 23 12:00 p.m. Cheel Conf. Room 2 Anesthesiology Wednesday, Sept. 23 4:30 p.m. CC-3

NEW APPOINTMENTS TO THE MEDICAL STAFF Name: Irwin Z. Benzel, DO Department: Pediatrics Medical School: Touro College of Osteopathic Medicine, NY Residency: Winthrop-University Hospital, NY—Pediatrics Practice: Pedimedica Office: 870 Palisades Avenue, Suite 204, Teaneck, NJ Name: Advay G. Bhatt, MD Department: Medicine Medical School: Albert Einstein College of Medicine, NY Residency: Boston University Medical Center, MA— Internal Medicine Fellowships: Boston University Medical Center, MA—
Electrophysiology, Cardiovascular Disease Practice: VMG Arrhythmia Associates of NY & NJ Office: 1 Linwood Avenue, Paramus, NJ Name: Neha D. Chheda, MD Department: Medicine Medical School: State University of New York School of Medicine,
NY Residency: Thomas Jefferson University Hospital, PA—Internal
Medicine Fellowship: Johns Hopkins Hospital, MD—Nephrology Practice: Bergen Hypertension and Renal Associates Office: 44 Godwin Avenue, Midland Park, NJ Name: Shiau H. Chin, MD Department: Emergency Medicine Medical School: New York Medical College, NY Residency: New York Hospital at Queens, NY—Emergency Medicine Fellowship: New York Hospital at Queens, NY—Ultrasound Practice: Valley Emergency Room Associates Office: 223 North Van Dien Avenue, Ridgewood, NJ Name: Emily F. Fischer, MD Department: Pediatrics College: Temple University School of Medicine, PA Residency: St. Christopher’s Hospital for Children, PA— Pediatrics Practice: North Jersey Pediatrics Office: 17-10 Fair Lawn Avenue, Fair Lawn, NJ
(Continued on next page)

NEW APPOINTMENTS TO THE MEDICAL STAFF (CONT.) Name: Fernande Josias, MD Department: Emergency Medicine College: Drexel University College of Medicine, PA Residency: York Hospital, PA—Emergency Medicine Practice: Valley Emergency Room Associates Office: 223 North Van Dien Avenue, Ridgewood, NJ Name: Dominique Kalil, MD Department: Medicine Medical School: University of Texas Health Science Center, TX Residency: Cabrini Medical Center, NY—Internal Medicine Westchester County Medical Center, NY—Internal
Medicine Practice: Valley Medical Services—Hospitalists Office: 223 North Van Dien Avenue, Ridgewood, NJ Name: Julia J. Lee, MD Department: Pediatrics Medical School: Drexel University College of Medicine, PA Residency: North Shore LIJ, NY—Pediatrics Practice: Valley Pediatric Associates Office: 201 East Franklin Turnpike, Ho-Ho-Kus, NJ Name: Marianne M. Longo, APN Department: Medicine School: Rutgers University, NJ Practice: Valley Physician Services—Valley Heart Group Office: 1200 East Ridgewood Avenue, Ridgewood, NJ Name: Heather Shafi, MD Department: Pediatrics Medical School: University of Medicine and Dentistry of NJ, NJ Residency: Yale-New Haven Hospital, CT—Pediatrics Practice: Pediatricare Associates Office: 20-20 Fair Lawn Avenue, Fair Lawn, NJ

ICD-10 Physician Champions The Clinical Documentation Improvement Department would like you to meet the ICD-10 resource physicians. These physicians recognize the importance of high quality and accurate documentation
and are a contact for questions and clarification for their peers.
Nicholas Alexander, M.D. Years at Valley: 21 years, Education: University of Pennsylvania, PA, University of Medicine and Dentistry, NJ, Board Certification: American Board of Orthopedic Surgery, Specialty: Orthopedic Surgery
Jeffrey P. Barasch, M.D. Years at Valley: 31 years, Education: Yale University, CT, New York University School of Medicine, NY, Board Certification: American Board of Internal Medicine, Subspecialty Board of Pulmonary Disease, American Board of Sleep Medicine, American Board of Int. Med. Sub of Sleep Medicine, Specialty: Pulmonary Medicine, Sleep Studies
Joshua Bernheim, M.D. Years at Valley: 12 Years, Education: Yeshiva University, NY, Albert Einstein College of Medicine, NY, Board Certification: American Board of Surgery, Special Qualifications in Vascular Surgery, Specialty: Vascular surgery
Anthony L. D’Ambrosio, M.D. Years at Valley: 8 Years, Education: University of North Carolina, NC, Vanderbilt University School of Medicine, TN, Board Certification: American Board of Neurological Surgery, Specialty: Neurosur-gery (continued on next page)

Annie Lee, M.D. Years at Valley: 9 years, Education: New York University, NY, Ross University, West Indies, Board Certification: American Board of Internal Medicine, Specialty: Internal Medicine
Jin S. Lee, M.D. Years at Valley: 1 year, Education: Columbus College, GA, Medical College of Georgis, GA, Board Certification: American Board of Internal Medicine, Subspecialty Board of Medical Oncology, Spe-cialty: Oncology
Jonas Mansson, M.D. Years at Valley: 4 years, Education: University of South Florida, Fl, Ross University School of Medi-cine, WI, Board Certification: American Board of Surgery, Specialty: Surgery
John J. McGreal, M.D. Years at Valley: 13 years, Education: Georgetown University, Washington D.C., Georgetown Univer-sity School of Medicine, Washington D.C., Board Certification: American Board of Internal Medicine, American Board of Pediatrics, Specialty: Emergency Medicine
Dan L. Musat, M.D. Years at Valley: 7 years, Education: Carol Davila University of Medicine & Pharmacy, Romania, St. Lukes-Roosevelt Hospital Center, NY, Board Certification: American Board of Internal Medicine, Subspecialty Board of Cardiovascular Disease, Subspecialty Board of Electrophysiology, Specialty: Electrophysiology, Cardiac (continued on next page)

Amit S. Tibb, M.D. Years at Valley: 1 year, Education: Lokmanya Tilak Municipal Medical College, India, Temple Uni-versity School of Medicine, PA, Board Certification: American Board of Internal Medicine, Subspe-cialty Board of Pulmonary Disease, Subspecialty Board of Critical Care, Subspecialty of Hospice & Palliative Care, Specialty: Critical Care, Pulmonary
The ICD-10 Hotline is now open! Monday through Friday 8:00 am—5:00 pm with any ICD-10 related questions. From outside the Hospital, you can call (201)447-8114.
Internally, you can call ext. 8114.
ICD-10 Raffle Winners!!
Jonas Mansson, MD—Department of Surgery and Deborah Ungerleider, MD—Department of Pediatrics
The Valley Hospital Receives Gold-Level Recognition from the U.S. Department of Health and Human Services for Promoting Organ Donation
The Valley Hospital was recently awarded gold-level recognition from the U.S. Department of Health and Human Services (HHS) for the hospital’s efforts in promoting organ donation. The hospital was recognized as part of the national Workplace Partnership for Life Hospital Cam-paign, sponsored by HHS’s Health Resources and Services Administration.
The Valley Hospital’s awareness and registry campaigns educated staff, patients, visitors, and community members on the critical need for organ, eye, and tissue donors and thereby in-creased the number of potential donors on the state’s donor registry.
“Organ donation is such an important issue,” said Bettyann Kempin, Assistant Vice President for Medical and Surgical Services at Valley. “We’re proud to partner with the NJ Sharing Network to be a part of this national campaign to increase awareness about the importance of organ dona-tion.”
Of the 1,856 hospitals and transplants centers enrolled in the campaign, 736 were awarded gold, silver or bronze recognition for effort to promote organ donation during Phase IV of the campaign, between August 1, 2014 and April 30, 2015.

Dr. Grau’s Confidence in Care Inspires Philanthropy
As the scar on her chest gradually fades from her operation performed at Valley over a year ago, Vita Zola reflects on the care and treatment leading up to and following the removal of an aneurysm on her aorta.
It started out as a visit to the eye doctor, which consequentially led to an MRI of the head and chest and resulted in Mrs. Zola landing in Valley's Department of Cardiac
Surgery. “I was shocked!” Mrs. Zola recalls of her first meeting Juan Grau, M.D., a board certified car-diac surgeon for the Valley's Department of Cardiac Surgery and Director of Cardiovascular Transla-tional Research. “When he came into the room with his assistant and told me there was an aneurism on my aorta, I really thought he had the wrong patient.”
Mrs. Zola was not in pain and did not feel symptomatic, which is one of the reasons why this news was so distressing and perplexing. But Dr. Grau’s absolute certainty regarding treatment of this aneurism, involving an aortic procedure to replace the aneurysm while preserving the patient’s native aortic valve, helped her come to grips with the reality that this 5-hour operation was imperative. “My husband and I responded well to Dr. Grau’s assurance,” Mrs. Zola reasons, “and we felt very confident under his care.”
John and Vita Zola have been part of the Valley Hospital family for years, having lived in Ramsey for the past 45 years. The Zolas have tapped into the many services of Valley, including the Emergency Room for stitches and bumps and the Maternity floor for their youngest child, now in her 40s. Through the years, as their three children grew, so has Valley.
The care that Mrs. Zola received from Valley clinicians during this time spanned the gamut from the cardiac consult, to the OR, to home with a visiting nurse, and then through three months of rehabilita-tion. “I cannot say enough about Valley! I recommend Valley Hospital to people all the time.” Mrs. Zo-la adds “When I was going through all of this, the cardiac nurses were unbelievable, so attentive, helped me in and out of bed. Every day I felt a little better.”
Months later, having fully recovered from the successful operation, Vita attended a dinner at Brassarie Brandman restaurant in Park Ridge where Dr. Grau spoke to a room filled with veteran cardiac pa-tients of all ages. “It was quite a night. He seems to know each and every one of his patients.”
Following that evening, Mr. and Mrs. Zola felt inspired to sponsor a grateful patient gift [link to https://www.valleyhospitalfoundation.org/sslpage.aspx?pid=298] to the Valley Hospital Foundation towards Dr. Grau’s Cardiology department. “I am so thankful that it all went so well, and that is what compelled me to give back.”
If you have a grateful patient that you would like the Valley Hospital Foundation to highlight in a story, please contact Trisha
Sullivan, Foundation Writer, at x6377 or [email protected]

Update on Dense Breasts and Supplemental Screening
Lauren Levy, MD Department of Diagnostic Imaging The Valley Hospital and Radiolo-gy Associates of Ridgewood, Member of the NJ Department of Health Breast Imaging Options Workgroup
New Jersey enacted its breast density no-tification law in May 2014. To date, 23 states have laws requiring notification of breast density be given to patients so that they can discuss the option of supplemental imaging with their health care providers. Similar bills are pending in Con-gress. The language of the mandatory notifica-tion legislation varies by state. Approximately 50% of women who undergo screening mammo-grams have dense breasts, therefore a national law would affect tens of millions of women yearly. Dense breast tissue increases breast cancer risk, but more importantly decreases the sensitivity of mammography. Supplemental imaging after a normal mammogram increases cancer detection in dense breasts; however, this is associated with increased false positives and unnecessary biopsies. The breast density debate includes the amount of screening women with dense breasts should get and whether all women with dense breasts should undergo supplemental screening. A recent report in the Annals of Inter-nal Medicine concluded: “breast density should not be the sole criterion for deciding whether supplemental imaging is justified because not all women with dense breasts have high interval cancer rates.” The objective of this study was to identify women who would benefit most from supplemental imaging by determining which combinations of breast cancer risk and BI-RADS density category are associated with high interval cancer rates to better inform the discus-sion of supplemental imaging between clinicians and their patients. This prospective cohort study was set in Breast Cancer Surveillance Consortium (BCSC) facilities over a nine-year period. The data set included 365,426 women from ages 40 through 74 who underwent 831,455 digital screening mammograms. The measured
parameters were BI-RADS breast density, BCSC 5-year breast cancer risk and interval cancer rate (defined as invasive cancer diagnosed in less than or equal to 12 months after a normal mam-mography result). Interval cancers are associat-ed with more aggressive tumor biology. A high interval cancer rate was defined as more than 1 case/1000 exams. The results of this study sug-gest that women with invasive cancer were more likely to be older and white and to have heteroge-neously or extremely dense breasts, a BCSC 5-year risk of at least 1.67%, and a family history of breast cancer. In this study 47% of the women ages 40 -74 had dense breasts. High interval cancer rates were observed for women with a 5-year risk of 1.67% or greater and extremely dense breasts (47% of extremely dense breasts) or a 5-year risk of 2.5% or greater and heteroge-neously dense breasts (19.5% of heterogeneous-ly dense breasts). These two groups comprised 24% of all women with dense breasts or 12% of all women undergoing screening. Half the wom-en with heterogeneously dense and half the women with extremely dense breasts were at low to average 5-year cancer risk (0% - 1.66%). The interval rate of advanced stage disease was highest among women with a 5-year risk of 2.5% or greater and heterogeneously or extremely dense breasts (21% of all women with dense breasts). The current Legislation Notification en-courages all women with dense breasts to dis-cuss supplemental screening with their health care providers. For the vast majority of women undergoing screening digital mammography, the rate of interval cancer is low and not all women with dense breasts have high interval cancer rates as indicated above. However, women with high interval cancer rates are at higher breast cancer risk and are at higher risk for advanced breast cancer. The authors found that using com-binations of breast cancer risk and density to identify those women with a high likelihood of in-terval cancers would more efficiently identify women who are more likely to benefit from sup-plemental imaging after a normal mammogram. Identifying those women with low mammographic sensitivity can also direct a discussion of the benefits of supplemental imaging in extremely dense women even in those women with low rates of interval cancer. (continued on the next page)

High mammographic density does indeed decrease the cancer detection rate of digital mammography and increases the risk that the cancers detected are larger and at a more advanced stage. Women with extremely dense breasts therefore may benefit from supplemental screening exams such as whole breast screening ultrasound or breast MRI. For any woman at high risk for breast cancer (lifetime risk >20%), sup-plemental yearly breast MRI should be consid-ered beginning as early as age 25. Supplemental 3D mammography (a.k.a. tomosynthesis) can be beneficial in women with heterogeneously dense breasts, low to average breast cancer risk and those at higher risk for false positives. Digital mammography has a sufficiently high breast can-cer detection rate and reasonably low rate of false positives for routine screening use even in patients with dense breasts and should be the first line screening exam starting at age 40. The authors suggest that primary care doctors and gynecologists can easily calculate the 5-year breast cancer risk using the BCSC calculator since it requires only 5 risk factors (age, first de-gree relatives with history of breast cancer, histo-ry of breast biopsy, BI-RADS density, and race/ethnicity). The primary doctors can then use this 5-year risk score in conjunction with the mammo-graphic density to guide their patient’s consulta-tion for supplemental imaging for women with dense breasts. One limitation of this study was that it did not specifically assess whether there is a benefit to supplemental screening in women with high rate of interval cancer or false positive mammo-gram result. The authors’ findings provide a start-ing point for identifying women who may have the most to gain from supplemental screening and help inform clinical decision-making about recom-mending supplemental imaging in women with dense breasts. In response to this study, the NY Times published an article in the Health section May 18, 2015, titled: Study Suggests Dense Breast Tis-sue Isn’t Always a High Cancer Risk. A similar article was published in Time Magazine the same day titled: Why Women With Dense Breasts May Not Need More Screening. Both of these articles were geared to the lay public summarizing this study.
An additional controversy raised by dense breast notification legislation is “who” should discuss breast density results with patients – the primary doctor or the radiologist. Since radiolo-gists are assigning the breast density based on the mammogram, many suggest that radiologists notify the patient of her density. Realistically, the vast majority of mammograms in the United States are interpreted after the patient has left the imaging facility. A recent editorial in the Soci-ety of Breast Imaging Newsletter (2015/Issue2), warned: “a recommendation of additional screen-ing by radiologists may be seen as self serving.” Because the assessment of a woman’s risk for breast cancer involves more than breast density, the primary doctor is in the unique position to as-sess multiple risk factors for an individual patient as well as discuss options such as systemic anti-estrogen therapy and prophylactic mastectomy. Unfortunately, educating the primary health care provider has lagged behind mandat-ed legislation. Many primary clinicians are una-ware of legislation in their state or feel uncomfort-able discussing breast density with their patients. The California Breast Density Information Group created an evidence-based website to educate clinicians and patients about breast density, risk assessment and supplemental imaging options. In NJ, the American Congress of Obstetrics and Gynecologists created a tool kit to assist and educate gynecologists in managing their patients with dense breasts. The patient advocacy group, Are You Dense, in conjunction with Dr. Wende Berg, has recently launched a website geared toward patient understanding of breast density and available options. The article referenced above is: Kerlikowske K, Zhu W, Tosteson AN, et.al. Identifying Women With Dense Breasts at High Risk for Interval Can-cer – A Cohort Study. Ann Intern Med. 2015;162:673-681. To learn more about BCSC 5-year risk calculator clinicians can visit http://breastscreening.cancer.gov. The calculator is also available as an app on a mobile device downloadable at the app store.
(continued on the next page)

Resources available on line: www.breastdensity.info - The California Breast Density Information Group website for
physicians and patients www.acr.org - The American College of Radiology (a brochure is available for patients), www.acog.org - The American College of Obstetricians and Gynecologists,
www.Areyoudenseadvocacy.org - Are You Dense Advocacy Group,http://www.densebreast-info.org - Are You Dense and Dr. Wende Berg’s dense breast website geared specifically for patients
Venous Thromboembolism Prophylaxis in Meditech The Valley Hospital faces many challenges related to venous thromboembolism (VTE) management, including identifying patients at highest risk of VTE; prescribing prophylactic and therapeutic antico-agulant therapies for these high-risk patients in a timely manner; and monitoring and reporting the VHS performance on VTE prophylaxis to national agencies. Six VTE measures are currently reported by Valley.
1. Patients receiving VTE prophylaxis 2. ICU patients receiving VTE Prophylaxis 3. VTE patients with anticoagulation overlap therapy 4. VTE patients receiving unfractionated heparin with dosage/platelet monitoring by protocol 5. VTE patients receiving appropriate discharge instructions 6. Incidence of potentially preventable VTEs To identify patients at risk for VTE, the admitting order sets all contain a VTE Risk Assessment screen. This screen provides a list of the risk factors for VTE; prompts the provider to enter the risk level of the patient; and recommends appropriate (mechanical and pharmacologic) prophylaxis based upon national guidelines. The entry of the prophylaxis will generate orders for those VTE prophylaxis measures automatically. Patients are assigned 1 of 3 risk levels based upon their score: low (0–2), medium (3–4), or high (> 4). Risk factors are given a score (using the Caprini scoring sys-tem). Examples are: Age 41–60 = score: 1; age 60–74 = score: 2; age >75 = score: 3; family history of thrombosis = score: 3; recent stroke = score: 5; major lower extremity arthroplasty = score: 5. The VTE assessment screen lists all of the risk factors and their scores to facilitate picking the appropri-ate risk level by the provider. All of the risk factors are summed and based upon the total score of all of the relevant risk factors; the overall risk score is assigned to the patient by the provider. Note that the Meditech screen recommends the appropriate prophylaxis based upon the risk level identified. (continued on next page)

The use of this screen provides four benefits: 1. Provides the information needed to assign a risk score to the patient 2. Provides recommendations on appropriate prophylaxis based upon the patient’s risk score 3. Generates orders for the prophylaxis medications and interventions 4. Provides the data to monitor and report VHS adherence to VTE prophylaxis guidelines Our goal is to use the new Meditech system to improve performance on VTE quality measures. The changes to our VTE approach represent evidence-based guidelines for the best patient care. In the future, we will try to apply rules within Meditech that help the physician to remember to always address prophylaxis.
More from the PAC: Discharge Process As we continue to address issues and improve workflows within the new Meditech system, Infor-mation Systems is addressing the questions and concerns of our physicians regarding the new Dis-charge Process. Below you will see answers and explanations for some of the most frequent inquir-ies we are receiving. Why is the discharge documentation more complicated than it was in the old system? Instead of being spread throughout the system, all discharge activities have been consolidated into a single, more complex document. There are more than a dozen discharge plans, which have been customized to meet the needs of specific services or types of patients. Each discharge plan sup-ports all of the provider steps necessary to perform the discharge (medication reconciliation, dis-charge instructions, diet, activity, the discharge order, problem list, etc.). This streamlined approach will help providers perform the discharge as efficiently as possible. When do I need to dictate a discharge summary? Discharge summary information can be placed by using either traditional dictation or a template in Meditech, with or without the assistance of Dragon Voice Recognition. The discharge summary must contain the following elements (taken from the Medical Staff Rules and Regulations): • the reason for hospitalization; • significant findings; • the final diagnosis; • procedures performed and care, treatment and services provided; • the patient’s condition at discharge; • a complete list of medications; • a medication reconciliation list is communicated to the next healthcare provider (within or outside the organization); • information given to the patient and family (as appropriate); and signature on the medical record(s).
What are the discharge templates and when do I use them? The discharge (D/C) templates that have been designed in Meditech support the different possible methods for discharge summary completion. They are named to represent their purpose. These are designed to contain the mostly commonly needed information presented in a way that expedites the
completion of the steps necessary to perform a patient discharge.
(continued on next page)

D/C Templates available for use:
D/C Plan: This template is used solely to complete the process of discharging the patient. These plans are further customized to streamline discharges from many areas (i.e., “D/C Plan: Endoscopy”). It is important to remember that this is not the discharge summary (per the R&R). D/C Plan with D/C Note: This template is meant for consultants to utilize. It allows the consultant to document their specific discharge plan needs, such as follow up, medications, and prescriptions, but not actually do the discharge. It also allows a brief note that can act as communication to the discharging physician, coordinating the discharge process. This document does not qualify as a discharge summary. D/C Plan with Discharge Summary: This template is meant for the discharging physician to complete both the process of discharge and the true discharge summary at the same time. Completing all of the required components of the discharge summary in this template qualifies as the discharge summary described in the R&R. Discharge Summary: This template is a stand-alone discharge summary template because sometimes the physician will use a D/C Plan to have the patient physically discharged from the hospital, and then, a short time later, return to the chart to complete the discharge summary. What happened to my Endoscopy discharge plan document? In order to streamline discharge documentation for endoscopy patients, the general Endoscopy discharge plan has been broken down into three discharge plans, each of which is specific to the type of procedure: bronchoscopy, colonoscopy and EGD/ERCP. Each document is customized to the procedure that makes the process more efficient for the physician. It includes a pre-entered statement that the medications have been reviewed and that there are no changes when the patient gets discharged home. If the patient is going back to an inpatient floor, these should not be used. Instead, the ‘manage transfer’ should be used to make sure all of the orders remain the same and that the medications do not change. Why am I getting deficiency notices on my discharge summaries? If you are being asked for an addendum to your discharge summary, it is because of missing/incomplete information such as a discharge date, hospital course narrative or physical exam. It is NOT due to missing information such as vitals, lab values or medications. Additionally, if the original discharge summary was dictated/created the day before the patient was discharged, an addendum will be requested. What are the common problems with discharge summary addendums? When entering an addendum to the discharge summary, please make sure that you are adding the addendum to the D/C Plan document (name will be “D/C Plan: XXXX” where XXXX represents the particular type of patient, specialty or diagnosis). The HIM Department has noticed that several addendums have been completed as requested; however, they are on the wrong document, thus requiring another addendum put on the correct document. Also, a Progress Note is not identified or labeled as a D/C Plan anywhere within the system, so it is not a substitute for a discharge summary when requested by the HIM Department. Addenda should not say “see information below” if the information is incomplete.


Gala Planned for the
35th Year Anniversary
of
the Valley Hospital Foundation
On September 25, 2015 at The Skylands Manor , 5 Morris Road in Ringwood, New Jersey, The Valley Hospital Foundation will be celebrating 35 remarkable years of philanthropically
supporting Valley Health System’s vision of providing excellence in patient and family centered care to this region.
The “black tie” gala will begin with cocktail hour at 7 p.m. followed by dinner at 8 p.m.
The Valley Hospital is a fully accredited, acute care, not-for-profit hospital serving more than 440,000 people in 32 towns in Bergen County and adjoining communities. Valley Home Care,
the home health agency of the Valley Health System, provides in-home comprehensive, quality healthcare by professionally trained staff. From the tiniest premature newborn to
the grandmother at the end of life, The Valley Hospital and Valley Home Care provide compassionate and expert care.
As the fundraising body, The Valley Hospital Foundation ensures that The Valley Hospital and Valley Home Care continue to have the essential resources in place to fund the maintenance
of its modern facilities, cutting edge technology, innovative programs, and groundbreaking research.
To celebrate 35 years of success, the Valley Hospital Foundation is inviting individuals, business-es, and interest groups in the Ridgewood vicinity to attend its 35th Anniversary Gala. This black
tie affair promises an exquisite evening of fine dining, cocktails, and live entertainment, while mingling among a unique, local, likeminded audience committed to clinical excellence for this re-gion. All guests will be listed in the Gala journal, a special edition of the donor newsletter Inside
Valley, and on the Foundation website. Businesses interested in demonstrating their commitment to this community are also lining up for corporate sponsorship which creates a unique
promotional opportunity for a captivated local audience.
To find out more about this event, purchase tickets, or become a corporate sponsor,
please visit www.valleyhospitalfoundation.org/35thGala