Approach to endometrial biopsy
-
Upload
prasad-csbr -
Category
Health & Medicine
-
view
477 -
download
5
Transcript of Approach to endometrial biopsy

Approach to Endometrial Biopsy
Dr.CSBR.Prasad, MD.,Professor & HOD
Deptt. of PathologySri Devaraj Urs Medical College
Kolar-563101

What do you think of this EM biopsy?

What is the finding here?

What is your impresion on this biopsy?
http://www.webpathology.com/image.asp?n=1&Case=568

Some fundamentals• Only endometrium from the fundus is suitable for diagnosis• The functionalis layer is particularly ideal• Basalis layer is generally of little diagnostic value except in
two conditions:1. Carcinoma2. Irregular shedding
• Irregular development is best detected in larger fragments of tissue where structural units retain their relationship
• EM from the isthmic region is unsuitable for functional diagnosis as they fail to respond to hormonal changes

Some fundamentals
• Proliferative phase may fluctuate between 10-20days – Dating is not possible
• Secretory phase is fixed and hence dating is possible
• Cystic dilatation of an occasional gland is not necessarily a sign of hyperplasia
• Ovulation may recur sporadically, even years after menopause, the associated corpus luteum is insufficient

EM Biopsy
• Different methods of obtaining endometrial sample– Curetting (D&C)– Pipelle biopsy or other equivalent technique– Hysteroscopy and direct biopsy– Endometrial cytology

Adequacy• There are no definitive guidelines / agreements *• If you can make a diagnosis, it is adequate• Clinical details are very important – Eg: Strips of endometrium in a post menopausal woman
• Don’t write “inadequate”– Sign out
• No stroma• Proliferative without definite stroma• No endometrium• No tissue
*Phillips V, McCluggage WG. Results of a questionnaire regarding criteria foradequacy of endometrial biopsies. J Clin Pathol 2005;58:417–9.

EM biopsy, Post menopausal

Algorithm for assessment of the adequacy of an endometrial biopsy specimen
McCluggage WG. My approach to the interpretation of endometrial biopsies and curettings . J Clin Pathol 2006;59:801–12.

Indications for EM Biopsy*4 Main INDICATIONS Other Indications
Determine the cause of AUB AGC /EM cells in PAP smear
Assessment of response of the EM to hormone Tx
Finding thickened EM in US in post menopausal women
Status of EM in infertile patients / datingEvacuation of POC (Spontaneous or MTP)
*Diagnosis of Endometrial Biopsies and Curettings: A Practical ApproachBy Michael Mazur, Robert J. Kurman

DDs for presence of adipose tissue in EM samples
• Uterine Perforation (Critical value)• Lipoleiomyoma

Myometrium in the curettings
• Notify the clinician how much myometrium was there in the curettings
• This helps in two ways:1. Gives info regarding the consistency of
myometrium2. Gives information about the technique of
curettage

Artefacts
• Telescoping (glands within glands)• Artefactual crowding and compression of
glands • Pseudopapillary architecture of superficial
strips of EM• Crushed endometrial glands and stroma may
be extremely cellular and can cause concern


Telescoping (gland within gland)

Crushed endometrial glands

Pseudopapillary architecture of superficial strips of EM

Normal EM

Proliferative endometrium

Proliferative endometrium

Mitosis - indicator of proliferative activity
• Non-reactive endometrium (No mitosis)• Mitosis in post menopausal EM– May be associated with hyperplasia– If there is no hyperplasia:• Continued estrogen stimulation• Prolapse• EM polyp

EM – Status Post menopusal

Secretory endometrium

EndometritisCommon components in EM:• Lymphocytes, including natural killer cells and lymphoid aggregates• PMNs: Premenstrual and menstrual phasesPlasma cells: *• Plasma cells: Is it always endometritis?• Other morphological features that favour endometritis:
– Disturbance in maturation—focal areas that are out of cycle with other areas
– Stromal edema and – Characteristically, a spindle-cell alteration of the stroma, especially around
glands– Glandular architectural complexity and cytological atypia
*Bayer-Garner IB, Korourian S. Plasma cells in chronic endometritis are easily identified when stained with syndecan-1. Mod Pathol 2001;14:877–9

Lymphoid aggregate

Spindle-cell alteration of the stroma, especially around glands

Endometritis
In the absence of other morphological features
exhaustive search for plasma cells is unnecessary

Endometritis• Focal necrotising endometritis*• Granulomatous endometritis– Tuberculosis– Sarcoidosis– Others
*Bennett AE, Rathore S, Rhatigan RM. Focal necrotizing endometritis: a clinicopathologic study of 15 cases. Int J Gynecol Pathol 1999;18:220–5.

EM polyp• 40-50yrs (rare before menarche, can occur after menopause)• Site: Fundus and cornua• Often pedunculated• Histology:
– Composed of glands and stroma– Mostly proliferative changes (cyclical changes are rare)– Foci of squamous metaplasia– Smooth muscle may form a component– Blood vessels are thick walled and tortuous
• Rarely carcinoma can arise (3%) – Through examination of polyp / stalk is important– Atypicalities in a post menopausal woman warrants hysterectomy

EM polyp• Proliferative activity is common in endometrial polyps,
even in postmenopausal women• A diagnosis of simple hyperplasia should not be made in
the case of an endometrial polyp• Carcinomas may arise in endometrial polyps• Endometrial polyps are particularly common in
association with tamoxifen• There is a peculiar tendency for serous carcinoma and EIC
to arise within endometrial polyps whether sporadic or associated with tamoxifen*
*Silva EG, Jenkins R. Serous carcinoma in endometrial polyps. Mod Pathol1990;3:120–8.

EM polyp

Metaplasias - Epithelial• Epithelial metaplasias: Squamous or mucinous– Associated with hyperplasia / carcinoma
• Ciliated metaplasia: Applicable only when extensive resembling fallopian tube
• Papillary syncytial metaplasia: – May be a reparative response– When florid, this may be suggestive of a serous carcinoma
or an EIC• Mucinous metaplasia• Benign papillary proliferations

Squamous metaplasia

Tubal metaplasia

Benign papillary proliferation

Simple mucinous metaplasia in the basalis of an atrophic endometrium

Include ichthyosis uteri

Metaplasias - Stromal• Formation of smooth muscle, cartilage and
bone
Importance: May be it difficult to assess myometrial invasion in carcinoma.
What are the differentials for stromal metaplasia?Retained fetal parts
Int J Gynecol Pathol 2007;26:115

Metaplasias - Stromal Endometrial stromal nodule with smooth muscle metaplasia

Effects of Tamoxifen on the Endometrium
• Tamoxifen is widely used as adjuvant therapy in the management of breast cancer
• Tamoxifen may exert a proliferative effect on the endometrium• The risk increases with increasing duration and dosage of tamoxifenEFFECTS:• Benign polyps (most common)• Stromal fibrosis• Stromal condensation around glands (DD Adenosarcoma)• Endometrial hyperplasia• Endometrioid and Non-Endometrioid carcinomas• Tamoxifen-associated polyps should be extensively sampled

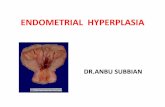
EM Hyperplasia
Def: Endometrial proliferation with an increase in gland to stroma ratio (from 2:1 to 3:1).
Classification of endometrial hyperplasia:– WHO 1994 - Four tier system– WHO 2014 – Two tier system
Atypia:• Vesicular nuclei• Prominent nucleoli• Rounding of nuclei• Increased cytoplasmic eosinophilia

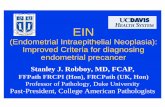
New WHO classification of endometrial hyperplasias - 2014
New term Synonym Genetic changes Coexistent invasive endometrial carcinoma
Progression to invasive carcinoma
Hyperplasia withoutatypia
Non-atypical EM hyperplasias
Low level of somatic mutations
< 1 % RR: 1.01–1.03
Atypical hyperplasia/endometrioid intraepithelial neoplasia
Atypical EM hyperplasias,EIN
Many of the genetic changes typical for endometrioid endometrial cancer are present
25–33 % 259 % 1
RR: 14–45
1. Antonsen S L, Ulrich L, Hogdall C. Patients with atypical hyperplasia of the endometrium should be treated in oncological centers. Gynecol Oncol. 2012;125:124–1282. Zaino R, Carinelli S G, Ellenson L H, Lyon: WHO Press; 2014. Tumours of the uterine Corpus: epithelial Tumours and Precursors; pp. 125–126.

EM hyperplasia

Simple hyperplasia without atypia
http://www.webpathology.com/image.asp?n=1&Case=568

Complex hyperplasia without atypia
http://www.webpathology.com/image.asp?n=1&Case=568

Complex hyperplasia without atypia

Atypical hyperplasia

Atypical hyperplasia

Atypical hyperplasia

Complex hyperplasia without nuclear atypia & Carcinoma

Complex hyperplasia with atypia
• Regresses in about 57% of cases • Progression to adenocarcinoma occurs in
about 30% of cases• Hysterectomy soon after biopsy: between 23%
and 48% harbor EM adenocarcinoma
http://www.webpathology.com/image.asp?n=8&Case=568

Benign mimics of EM hyperplasia
• Artefacts• Endometritis• Endometrial polyp• Arias-Stella reaction• Disordered proliferative endometrium• Benign papillary proliferations• Lower uterine segment endometrium

Disordered proliferative endometrium

Immunohistochemical staining of FOXA1 and AR in normal endometrium, atypical hyperplasias, and endometrial cancer
Qiu, Meiting, Bao, Wei, Wang, Jingyun, Yang, Tingting, He, Xiaoying, Liao, Yun, Wan, Xiaoping . FOXA1 promotes tumor cell proliferation through AR involving the Notch pathway in endometrial cancer BMC Cancer 2014; 14:78 ·

Cyclin D1 staining
1-Surface epithelium 2-Complex hyperpasia
3-Endometrioid adenocarcinoma (+) and adenomyosis(-)

Arias – Stella reaction

Extensive regions of necrosis in curettings - Causes
• Degenerating carcinoma• Septic abortion• Infarcted polyp• Degenerated submucosal leiomyoma

Extensive regions of necrosis better microscopic evidence must be sought before making a definitive diagnosis of
carcinoma

Adenocarcinoma of endometrium• Criteria helpful in distinguishing carcinoma from hyperplasia:
The tumor is probably malignant if:– Glands are closely packed without intervening stroma for at least half
the low power field– If gland Lumina containing multiple thin branching papillary
projections with a collagenous core with neoplastic epithelium occupying more than half of low-power field
– If sheets of squamous cells occupy more than half of low-power field– Bridging between the adjacent glands – Cribriform pattern– Luminal necrosis with PMN infiltration– If stroma between the glands is collagenous

Some tips• Interact with your clinician / History is important for interpretation• Separate the endometrial tissue proper from the blood clots for
processing• Endometrium with surface epithelium is best for interpretation. Absence
of surface epithelium compromises interpretation• Do not report hyperplasia on secretory endometrium• In all cases of abnormal uterine bleeding, consider the possibility of polyp• Finding fat in EM curetting is a critical value. It should be intimated to the
clinician• Aware of the mimics• All endometrial cancers should be typed and, if appropriate, graded, even
for small biopsy specimens

Thank you




![Study of Endometrial Pathology in Abnormal …sitivity of endometrial biopsy for the detection of endo-metrial abnormalities has been reported to be as high as 96% [2, 3]. Table 1](https://static.fdocuments.us/doc/165x107/5ed75e130b858a20966772e6/study-of-endometrial-pathology-in-abnormal-sitivity-of-endometrial-biopsy-for-the.jpg)