Advanced E/M Coding for EHRsstatic.aapc.com/.../d6330504-23fd-488d-8a7c-4aae95647c10.pdf ·...
Transcript of Advanced E/M Coding for EHRsstatic.aapc.com/.../d6330504-23fd-488d-8a7c-4aae95647c10.pdf ·...

AAPC2480 South 3850 West, Suite BSalt Lake City, Utah 84120800-626-CODE (2633), Fax 801-236-2258www.aapc.com
2013
AAPC Workshops
Advanced E/M Coding for EHRs


Advanced E/M Coding for EHRsBy: Stephen R. Levinson, M.D., CHCA

ii AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Introduction
AAPCDisclaimerThis course was current when it was published. Every reasonable effort has been made to assure the accuracy of the information within these pages. Readers are responsible to ensure they are using the codes, and following applicable guidelines, correctly. AAPC employees, agents, and staff make no representation, warranty, or guarantee that this compilation of information is error-free, and will bear no responsibility or liability for the results or consequences of the use of this course. This guide is a general summary that explains guide-lines and principles in profitable, efficient health care organizations.
USGovernmentRightsThis product includes CPT®, which is commercial technical data and/or computer data bases and/or commercial computer software and/or commercial computer software documentation, as applicable, which was developed exclusively at private expense by the American Medical Association, 515 North State Street, Chicago, Illinois, 60610. U.S. Government rights to use, modify, reproduce, release, perform, display, or disclose these technical data and/or computer data bases and/or computer software and/or computer software documentation are subject to the limited rights restrictions of DFARS 252.227-7015(b)(2) (November 1995), as applicable, for U.S. Department of Defense procurements and the limited rights restrictions of FAR 52.227-14 (June 1987) and/or subject to the restricted rights provision of FAR 52.227-14 (June 1987) and FAR 52.227-19 (June 1987), as applicable, and any applicable agency FAR Supplements, for non-Department of Defense Federal procurements.
AMADisclaimerCPT® copyright 2012 American Medical Association. All rights reserved.
Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT®, and the AMA is not recommending their use. The AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for data contained or not contained herein.
CPT® is a registered trademark of the American Medical Association.
The responsibility for the content of any “National Correct Coding Policy” included in this product is with the Centers for Medicare and Medicaid Services and no endorsement by the AMA is intended or should be implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, nonuse or interpretation of information contained in this product.
AbouttheAuthorFollowing medical education at Johns Hopkins and specialty training in head and neck surgery at UCLA, Dr. Levinson had a private practice in Connecticut for 26 years. After training in 1991 by AMA and HFCA as an E/M coding educator, he developed Intelligent Medical Records (IMR) – chart tools for E/M compliance in paper and dictation formats. He has authored Practical E/M: Documentation and Coding Solutions for Quality Patient Care, published by the AMA Press in 2005, with release of a second edition in 2008. In 2008, AMA Press also published his second book, Practical EHR: Electronic Record Solutions for Compliance & Quality Care, which provides the foundation concepts for this workshop.
NoticeRegardingClinicalExamplesUsedinthisBookAAPC believes it is important in training and testing to reflect as accurate a coding setting as possible to students and examinees. All examples and case studies used in our study guides and exams are actual, redacted office visit and procedure notes donated by AAPC members.
To preserve the real world quality of these notes for educational purposes, we have not rewritten or edited the notes to the stringent grammatical or stylistic standards found in the text of our products. Some minor changes have been made for clarity or to correct spelling errors originally in the notes, but essentially they are as one would find them in a coding setting.
© 2013 AAPC2480 South 3850 West, Suite B, Salt Lake City, Utah 84120800-626-CODE (2633), Fax 801-236-2258, www.aapc.com
All rights reserved.CPC®, CPC-H®, CPC-P®, CIRCC®, CPMA®, CPCO™, and CPPM® are trademarks of AAPC.

AdvancedE/MCodingforEHRs www.aapc.com iii
Contents
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .1
TheupsideofEHRs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1
ThedownsideofEHRs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3
HowEHRscandistortthedocumentationandcodingprocess . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .4
ReviewofQuantitativeandQualitativeGuidelines. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
SummaryofEHRDesignIssues. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .9
Add#1:ConsiderationofMedicalNecessity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
Add#2:ThequalitativemeasuresspecifiedinDocumentationGuidelines . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10
Remove#1:Incompleteandnon-compliantE/Mcodingengines. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
Remove#2:Automatedentryofclinicalinformation,resultingin“cloned”documentation. . . . . . . . . . . . . . . . . . . . 12
UserTipsforE/MAuditforms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .15
AppearanceOptionsfortheH&PRecord:HybridModelvs.“Translation”31. . . . . . . . . . . . . . . . . . . . . . .31
Notes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .42
AppendixAAMAstatement . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .45
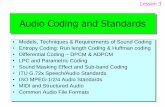
SlidePresentation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .53

Contents

Advanced E/M Coding for EHRs
AdvancedE/MCodingforEHRs www.aapc.com 1
Introduction
“Our recovery plan will invest in electronic health records and new technology that will reduce errors, bring down costs, ensure privacy, and save lives.”
President Barack Obama Address to Joint Session of Congress
February 24, 2009
President Obama’s ambition to see electronic health records (EHRs) universally adopted in medical practices across the country is being realized, as physician practices and hospitals hurry to meet federal deadlines for EHR adoption. Today, the medical marketplace is abuzz with the promise and threat of legislation that provides financial incentives to physicians and facilities that adopt electronic health records before the government deadline of 2015. The Health Information Technology for Economic and Clinical Health (HITECH) Act, under Title XIII of the American Recovery and Reinvestment Act (ARRA) of 2009, provides more than $30 billion for incentive payments to physicians and facilities that adopt EHRs that meet set standards. CMS is administering the program. In addition to subsidizing the cost of EHRs for those who adopt qualifying systems, and inflicting penalties on those who do not, the HITECH act also is a boon to health information technology companies with EHRs that the medical community was previously hesitant to adopt.
TheUpsideofEHRsHITECH’s nudge of physicians and facilities into EHR adoption may herald the biggest change to medical documentation since the advent of the transcription recorder. This change presents the promise, as yet unproven, to streamline processes and save lives. The Office of the National Coordinator for Health Information Technology Electronic Health Record Adoption and Utilization released its 2012 Highlights and Accomplishments in September, and listed examples of EHR benefits:
z “Joplin, Missouri experienced a devastating tornado in 2011. Because St. John’s Regional Medical Center, a 370-bed facility in Joplin, had implemented an EHR system prior to the tornado striking the town, St. John’s was able to use or transfer all patients’ medical records within hours.
z Dr. Jennifer Brull of Kansas realized the benefits of using her EHR system when she proactively identified patients in need of colon cancer screenings. She increased her screening rate from 37% to 81%. While she considered that impressive, she found the real benefit of EHRs came to light when she was able to detect colon cancer early in three patients. The detection was so early the patients did not require chemotherapy or radiation. For them, it made a huge difference between early colon cancer detection and invasive colon cancer.”
The advancements in EHRs are many. Some benefit the patient: the physician can see all health data in one place, know instantly when preventive care is due, and see prescription contraindications more readily. Some benefit the provider: data can be mined across the patient population, Physician Quality Reporting System (PQRS) reporting is simplified, and clinical decision support is provided. The payer also benefits: reduction in redundant services reduces costs, as does fewer errors in medications. Adoption rates for EHRs continue to climb. Many practices have already adopted, or are shopping for new systems. Others are looking for their first system. The Office of the National Coordinator for Health Information Technology Electronic Health Record Adoption and Utilization provides graphs and maps showing growth in the use of EHRs over the past few years:

Advanced E/M Coding for EHRs
2 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
(Source: The Office of the National Coordinator for Health Information Technology Electronic Health Record Adoption and Utilization’s 2012 Highlights and Accomplishments published in September, 2012)
As you can see, hospitals outpace physician practices in adoption, and urbanized states outpace rural ones, as well. What these charts do not capture is those facilities and practices that are currently shopping for EHRs. If those were shown, virtually every state would be blue because the deadline looms for adoption, and the financial incentives
from the federal government are very strong. Those not using an EHR by 2015 sill see a reduction in Medicare payments, and will miss incentive payments provided to those who do adopt EHRs.

Advanced E/M Coding for EHRs
AdvancedE/MCodingforEHRs www.aapc.com 3
TheDownsideofEHRsBut in front of every silver lining there is a dark cloud, and EHRs are no exception. Detractors may talk about cost, or complexities, or implementation timelines that extend beyond promised dates. Congressional committees have also voiced concerns about failure of certified systems to actually achieve true interoperability.
During Hurricane Sandy in 2012, in the face of flooding, two major New York Medical Centers (Belleview & New York University) recognized impending loss of electrical power. News reports revealed that while preparing their patients for transfer to other hospitals, efforts at sending those patients’ records electronically failed, because the EHR systems at those hospitals were not interoperable with their electronic records.
All these may be valid concerns, but are not the topic of today’s workshop, Advanced E/M Coding for EHRs. This workshop will look at the way EHRs are altering the ways in which physicians and other health care professionals document the services they render, specifically their E/M services. We will look at a variety of EHR formats and templates that change the way elements of E/M are docu-mented, and look at the impact those changes have on how CMS and other payers review the documentation gener-ated from an EHR. To do this, we need to understand the government standards affecting evaluation and manage-ment (E/M) elements within an EHR that qualifies under HITECH. We also need to examine the potential impact of non-compliant documentation capabilities on clinicians’ patient care processes.
“Qualifying” and “Compliant” EMRs and E/MThe government requires that EHRs being adopted qualify for “meaningful use” certification in order for benefits to be paid to the physician or facility. “Meaningful use” focuses on issues like interoperability, the ability to e-prescribe, and security -- not on documentation and coding compliance. While the systems are required to include CPT®, ICD-9-CM and HCPCS Level II codes, there is no requirement that the system provide these codes in a manner that is compliant with a coder’s understanding and sensibility of “meaningful use”; i.e., complete and accurate descriptions, compliance with guidelines, consideration of Medical Necessity, etc. For E/M, the only requirement in current “Meaningful Use” certification is that the codes be included. However, this certification includes no criteria for the EHR to be E/M compliant from a documentation or coding standpoint.
Even so, many EHR developers include in their systems components that actively or passively affect documentation and coding of E/M services. Active components include items like templates with checkboxes, used in a review of systems; macros that automatically enter completed entries of history or examination without requiring clinician documentation; or copying forward identical blocks of text from prior visits or even from other patients’ visits. Passive components include a system’s ability to advance to today’s date of service the problem list from the patient’s previous date of service, or the ability to cut-and-paste data within a patient record or between patient records. Medical docu-mentation of the patient encounter has been forever altered by the EHR.
The OIG noted a year ago that the frequency of claims for level 5 services increased from 28 percent to 49 percent between 2001 and 2010, and that CMS saw an overall increase of 48 percent in E/M payments during that same period. Soon, the phenomenon of E/M inflation was in the press, as seen in these two articles from the New York Times:
September 21: “Medicare Bills Rise as Records Turn Electronic”
“This spring, the Office of Inspector General for the federal Health and Human Services Department warned that the coding of evaluation services had been ‘vulnerable to fraud and abuse.’”
“The move to electronic health records may be contrib-uting to billions of dollars in higher costs for Medicare, private insurers and patients by making it easier for hospitals and physicians to bill more for their services, whether or not they provide additional care.”
“Some experts blame a substantial share of the higher payments on the increasingly widespread use of elec-tronic health record systems. Some of these programs can automatically generate detailed patient histories, or allow doctors to cut and paste the same examination findings for multiple patients—a practice called clon-ing—with the click of a button or the swipe of a finger on an iPad, making it appear that the physicians con-ducted more thorough exams than, perhaps, they did.”

Advanced E/M Coding for EHRs
4 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
“Critics say the abuses are widespread. ‘It’s like doping and bicycling,’ said Dr. Donald W. Simborg, who was the chairman of federal panels examining the potential for fraud with electronic systems. ‘Everybody knows it’s going on.’”
http://www.nytimes.com/2012/09/22/business/medicare-billing-rises-at-hospitals-with-electronic-records.html?pagewanted=all
September 25:
“The Obama administration has issued a strong and much-needed warning to hospitals and doctors about the fraudulent use of electronic medical records to ille-gally inflate their billings to Medicare.”
“Attorney General Eric Holder Jr. and the health and human services secretary, Kathleen Sebelius, cited ‘trou-bling indications’ that some providers are billing for ser-vices never provided and vowed to prosecute.”
http://www.nytimes.com/2012/09/22/business/medicare-billing-rises-at-hospitals-with-electronic-records.html?pagewanted=all
The Center for Public Integrity also picked up the story, with this report on September 15:
“A significant portion of the added charges is likely due to ‘upcoding’—charging for more extensive and costly services than actually delivered.”
“The rise in costly coding and billing errors appears to be getting worse amid lax government oversight and the proliferation of electronic medical records systems, which critics say can facilitate abuse.”
The introduction of EHRs has not only presented new challenges to compliant E/M documentation and coding, but it has magnified old challenges that coders and auditors have faced in the world of paper records. These reports have placed the overbilling consequences of these coding discrepancies in the public spotlight. This exposure prompted immediate critical responses from the U.S. Attorney General and Secretary of Health and Human Services, both of whom declared that such improper billing with EHRs for E/M services will not be tolerated. The OIG has also targeted EHR noncompliant coding, and congressional committees have even threatened to disrupt incentive funding for EHRs that were touted as decreasing costs (but have done the opposite). Modern Healthcare reported that audits revealed that improper billing is
commonly not due to physician intent, but by physicians using their EHRs as they were designed to be used.
HowEHRsCanDistorttheDocumentationandCodingProcessThe challenges presented by E/M coding for EHRs are largely the result of programming that recognizes only a selective (i.e., limited) set of established E/M guidelines. Specifically, most certified EHR systems incorporate the quantitative (i.e., counting to determine E/M level, as in counting the systems in ROS) guidelines, but leave out some or all of the qualitative (i.e., medical necessity) guidelines. This selectivity results in a significant number of coding gaps, or “loopholes,” that necessarily lead to non-compliant coding and billing practices by clinicians, who are using these systems according to their designs and training practices.
Addressing these challenges requires a comprehensive application of E/M principles and guidelines, as well as Medicare/Federal regulations. An analysis of the principles for compliant E/M coding proves that the medical necessity (one of the qualitative components of the visit) is the overarching criterion for selection of the E/M level, with the quantitative component (counting) playing a secondary role.
Applying this approach also calls for us to consider using a more sophisticated and complete chart evaluation tool than conventionally employed. Such a tool must incorporate all qualitative and quantitative guidelines, and have the versa-tility to be used for coding, for auditing, and for clinician education.
ReviewofQuantitativeandQualitativeGuidelinesDiscussion below provides a section-by-section analysis of E/M components, and those selected quantitative and qualitative guidelines that are commonly found to create particular challenges for compliant coding of documents created using EHRs. These are based on CPT®, 1995 and 1997 Documentation Guidelines (DGs), CMS guidelines and other federal laws, and the AMA’s publication, Practi-cal E/M Documentation and Coding Solutions for Quality Patient Care, second edition.

Advanced E/M Coding for EHRs
AdvancedE/MCodingforEHRs www.aapc.com 5
Medical History: Past History, Family History, and Social HistoryDocumentation Guidelines cover both quantitative and qualitative elements for determining level of history in CPT® E/M code selection for past, family, and social history (PFSH). Quantitative Documentation Guidelines require:
z At least one specific item from any of the three history areas must be documented for a pertinent PFSH.
z At least one specific item from two of the three his-tory areas must be documented for a complete PFSH for the following categories of E/M services: office or other outpatient services, established patient; emergency department; domiciliary care, established patient; and home care, established patient.
z At least one specific item from each of the three his-tory areas must be documented for a complete PFSH for the following categories of E/M services: office or other outpatient services, new patient; hospital obser-vation services; hospital inpatient services, initial care; consultations; comprehensive nursing facility assess-ments; domiciliary care, new patient; and home care, new patient.
Qualitative Documentation GuidelinesThe ROS and/or PFSH may be recorded by ancillary staff or on a form completed by the patient. To document that the physician reviewed the information, there must be a notation supplementing or confirming the information recorded by others
Based on both clinical standards of care and logical inter-pretation of the DGs, there must be a notation supple-menting any positive findings when recorded/documented by the physician.
Medical History: Review of SystemsDocumentation Guidelines cover both quantitative and qualitative elements for determining review of systems in CPT® E/M code selection.
Quantitative Documentation GuidelinesDGs state, “a problem pertinent ROS inquires about the system directly related to the problem(s) identified in the HPI” and, “The patient’s positive responses and pertinent negatives for the system related to the problem should be documented.”
DGs state, “an extended ROS inquires about the system directly related to the problem(s) identified in the HPI and a limited number of additional systems” and, “The patient’s positive responses and pertinent negatives for two to nine systems should be documented.”
DGs state, “a complete ROS inquires about the system(s) directly related to the problem(s) identified in the HPI plus all additional body systems” and, “at least ten organ systems must be reviewed. Those systems with positive or pertinent negative responses must be individually docu-mented.”
Qualitative Documentation GuidelinesDGs state, “the ROS and/or PFSH may be recorded by ancillary staff or on a form completed by the patient. To document that the physician reviewed the information, there must be a notation supplementing or confirming the information recorded by others.” Based on both clinical standards of care and logical interpretation of the DGs, there must be a notation supplementing positive findings when recorded/documented by the physician.
Medical History: Chief Complaint (CC)The DGs state, “The CC is a concise statement describing the symptom, problem, condition, diagnosis, physician recommended return, or other factor that is the reason for the encounter, usually stated in the patient’s words.”
Qualitative Documentation GuidelinesThe DGs state, “the medical record should clearly reflect the chief complaint.”
Medical History: History of Present Illness (HPI)As defined by the DGs, “The HPI is a chronological description of the development of the patient’s present illness from the first sign and/or symptom or from the previous encounter to the present. It includes the follow-ing elements: location, quality, severity, duration, timing, context, modifying factors, and associated signs and symp-toms.”
Quantitative Documentation Guidelines“A brief HPI consists of one to three elements of the HPI,” according to the DGs, and “The medical record should describe one to three elements of the present illness (HPI).”
“An extended HPI consists of at least four elements of the HPI or the status of at least three chronic or inactive conditions,” according to the DGs, and “the medical record should describe at least four elements of the present

Advanced E/M Coding for EHRs
6 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
illness (HPI), or the status of at least three chronic or inactive conditions.”
Qualitative Documentation GuidelinesAs defined by Documentation Guidelines, “The HPI is a chronological description of the development of the patient’s present illness from the first sign and/or symptom or from the previous encounter to the present.”
Physical Examination
1995 Quantitative Documentation Guidelines In the 1995 DGs, a Problem Focused examination involves only “the affected body area or organ system;” i.e., one organ system.
When a Comprehensive examination is “a general multi-system examination…. the medical record for a general multi-system examination should include findings about eight or more of the 12 organ systems,” the DGs state.
Both expanded problem focused and detailed examinations will involve performing and documenting between two and seven organ systems
1995 Qualitative Documentation GuidelineThe 1995 DGs offer the following definitions:
z “Problem Focused (exam) - a limited examination of the affected body area or organ system”
z “Expanded Problem Focused (exam)- a limited exami-nation of the affected body area or organ system and other symptomatic or related organ system(s)”
z Detailed (exam) - an extended examination of the affected body area or organ system and other symp-tomatic or related organ system(s)”
z “Comprehensive (exam) - a general multi-system examination or complete examination of a single organ system” The DGs also state, “The medical record for a general multi-system examination should include findings about eight or more of the 12 organ systems.”
In these definitions, the terms “limited examination” and “extended examination” are not defined. We must con-clude that “extended” is more complete than a “limited examination.”
Also, the requirement for performing and documenting examination of “other related organ systems” is commonly overlooked in determining whether the medically indicated examination was performed and documented. For example, for patients with a complaint of “chest pain,” the related
organ systems warranting examination include cardiovas-cular, but also constitutional, respiratory, gastrointestinal, musculoskeletal, skin, neurologic, and psychiatric. The DGs clearly indicate that a “comprehensive examination” should be more thorough than a “detailed examination.” Therefore, the general multi-system examination must include an extended examination of eight or more of the 12 organ systems
There are very few published descriptions of the requirements for a “complete examination of a single organ system,” and no evidence that documents a physical examination in accordance with any published complete single organ system exam for 1995 DGs.
The DGs state, “Specific abnormal and relevant negative findings of the examination of the affected or symptomatic body area(s) or organ system(s) should be documented. A notation of ‘abnormal’ without elaboration is insufficient.”
In individually documented (i.e., non-cloned) physical examination sections, it is common to encounter medical records in which documentation may include only the designation, “abnormal,” without including specific details of these findings. This lack of documentation of “specific abnormal findings” is a failure to fulfill this qualitative guideline. More commonly, the examination does include the specific abnormal findings of the symptomatic organ systems, but simply records “normal” for affected or symptomatic organ systems where abnormalities were not found. This lack of documentation of “relevant negative findings” is also a failure to fulfill this qualitative guideline.
The DGs also state, “a brief statement or notation indicating ‘negative’ or ‘normal’ is sufficient (only) to document normal findings related to unaffected area(s) or asymptomatic organ system(s),” and “abnormal or unexpected findings of the examination of the unaffected or asymptomatic body area(s) or organ system(s) should be described.”
1997 Quantitative Documentation GuidelinesIt is noteworthy that the original intent of the 1997 edition of the DGs was to supersede (i.e., replace) the 1995 edition. This plan would have eliminated many of the non-specificity challenges in the physical exam section of the 1995 DGs, as discussed above. However, this intention was reversed in response to physician concerns voiced prior to the 1998 “Fly-In Meeting” held in Chicago regarding the E/M system and DGs. As a result, clinicians were allowed to choose between the two editions.

Advanced E/M Coding for EHRs
AdvancedE/MCodingforEHRs www.aapc.com 7
The 1997 DGs provide specific examination templates for a general multi-system examination and for eleven different single organ system examinations. The DGs list numbers of examination elements to be performed and documented specific for each of these types of examinations to fulfill requirements for Problem Focused, Expanded Problem Focused, Detailed, and Comprehensive examinations.
1997 Qualitative Documentation GuidelinesThe 1997 DGs retain the identical qualitative guidelines published in the 1995 edition.
The 1997 DGs state, “Specific abnormal and relevant negative findings of the examination of the affected or symptomatic body area(s) or organ system(s) should be documented. A notation of ‘abnormal’ without elaboration is insufficient.”
In individually documented (i.e., non-cloned) physical examination sections, it is common to encounter medi-cal records where documentation may include only the designation “abnormal,” without including specific details of these findings. This lack of documentation of “specific abnormal findings” is a failure to fulfill this qualitative guideline. More commonly, the examination does include the specific abnormal findings of the symptomatic organ systems, but simply records “normal” for affected or symp-tomatic organ systems where abnormalities were not found. This lack of documentation of “relevant negative findings” is a failure to fulfill this qualitative guideline.
“The 1997 DGs state, “A brief statement or notation indicating ‘negative’ or ‘normal’ is sufficient (only) to document normal findings related to unaffected area(s) or asymptomatic organ system(s),” and “Abnormal or unexpected findings of the examination of the unaffected or asymptomatic body area(s) or organ system(s) should be described.”
Medical Decision Making (MDM): Number of diagnoses and/or the number of management options that must be considered
Quantitative Documentation Guideline Neither CPT® nor either edition of DGs provides quan-titative values for the qualitative descriptors noted below. However, the AMA publications “Practical E/M” and “Practical EHR” suggest the following quantitative values. These suggestions were approved for the publication by the AMA’s CPT® section9:
CPT® Description of Number of Diagnoses and/or Management Options
Practical E/M’s Numerical Value
Minimal 1
Limited 2
Multiple 3
Extensive 4 or more
Qualitative Documentation GuidelinesThe DGs say, “For each encounter, an assessment, clinical impression, or diagnosis should be documented. It may be explicitly stated or implied in documented decisions regarding management plans and/or further evaluation.” For a presenting problem with an established diagnosis the record should reflect whether the problem is: either improved, well controlled, resolving or resolved; or inad-equately controlled, worsening, or failing to change as expected. For a presenting problem without an established diagnosis, the assessment or clinical impression may be stated in the form of differential diagnoses, or as a “pos-sible,” “probable,” or “rule out” (R/O) diagnosis.”
A common challenge of EHR coding results from systems programmed to replace the differential diagnosis described above with selection from lists of ICD-9 (or, soon-to-be ICD-10) diagnosis codes that are simultaneously used for billing purposes, thereby eliminating the inclusion of the “rule out,” “possible,” and “probable” diagnoses required for this sections of MDM.
Medical Decision Making (MDM): Amount and/or complexity of data to be reviewed
Quantitative Documentation GuidelinesNeither CPT® nor either edition of the DGs provides quantitative values for the qualitative descriptors noted below. However, the AMA publications “Practical E/M” and “Practical EHR” suggest the following quantitative values. These suggestions were approved for the publication by the AMA’s CPT® section10:
CPT® Description of Number of Amount of Data to be Reviewed
Practical E/M’s Numerical Value
Minimal 1
Limited 2
Moderate 3
Extensive 4 or more

Advanced E/M Coding for EHRs
8 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Qualitative Documentation GuidelinesBoth editions of the DGs list a series of guidelines con-cerning review of diagnostic studies and old records that “should be documented.” DG also offer three examples of relative complexity of data review:
z “A decision to obtain and review old medical records and/or obtain history from sources other than the patient increases the amount and complexity of data to be reviewed.”
z “Discussion of contradictory or unexpected test results with the physician who performed or interpreted the test is an indication of the complexity of data being reviewed.”
z “On occasion the physician who ordered a test may personally review the image, tracing or specimen to supplement information from the physician who pre-pared the test report or interpretation; this is another indication of the complexity of data being reviewed.”
Although it is clear that assessment of the complexity of data is best accomplished by the clinician at the point of care, it is noteworthy that the Documentation Guidelines fail to suggest that clinicians should document their pro-fessional assessment of the complexity of data ordered or reviewed. The additional documentation of this qualitative measure through well-designed EHR screens is effective for promoting compliant E/M coding and providing audit protection. In the absence of such clinician documentation, the coder is compelled either to make this determination without clinical guidance or to seek the assistance of an authoritative clinician.
Medical Decision Making (MDM): Risk of significant complications, morbidity, and/or mortality
Quantitative Documentation GuidelinesNeither CPT® nor either edition of DGs provides quanti-tative values for the qualitative (subjective) descriptors of levels of risk provided in the “Table of Risk,” described below. Rather, DGs specify, “Because the determination of risk is complex and not readily quantifiable, the table (of risk) includes common clinical examples rather than abso-lute measures of risk.”
Qualitative Documentation Guidelines Both editions of the DGs provide a “table of risk” with common clinical examples of the three types of risk that are to be assessed:
z A risk of the presenting problem(s) based on the risk related to the disease process anticipated between the present encounter and the next one.
z A risk of selecting diagnostic procedures based on the risk during and immediately following any procedures or treatment.
z A risk of management options based on the risk during and immediately following any procedures or treatment.
Each of the three types of risk is characterized by one of four possible levels of risk, which are described in qualita-tive terms: minimal, low, moderate, and high.
Although it is clear that assessment of the three levels of risk is best accomplished by the clinician at the point of care, it is noteworthy that the DGs fail to suggest that clinicians should document their professional assessment of these three levels of risk. The additional documentation of this qualitative measure through well-designed EHR screens is effective for promoting compliant E/M coding and providing audit protection. In the absence of such clinician documentation, the coder is compelled either to make this determination without clinical guidance or to seek the assistance of an authoritative clinician.
Nature of the Presenting Problem(s) (NPP)CPT® defines the NPP in terms of the probability of the risk of morbidity, mortality, and or prolonged functional impairment without treatment.11 This definition and the Clinical Examples referenced below provide powerful evi-dence that the NPP is the E/M system’s measure of Medi-cal Necessity
Quantitative Documentation GuidelineNeither CPT® nor either edition of DGs provides quantitative values for the qualitative (subjective) descriptors of levels of the NPP
Qualitative Documentation GuidelinesCPT® defines severity of the NPP in five different levels:
z Minimal (usually applies to services provided under supervision without actual presence of the clinician)
z Self-limited or minor

Advanced E/M Coding for EHRs
AdvancedE/MCodingforEHRs www.aapc.com 9
z Low severity z Moderate severity z High severity
In Appendix C, CPT® provides Clinical Examples that illustrate the relationship between NPP and medically indicated levels of coding (and care):
z “As shown in Appendix C of the CPT® codebook, presenting problems with higher severity NPPs war-rant higher levels of E/M care. This concept correlates with the Centers for Medicare and Medicaid Services’ (CMS) mandate for ‘medical necessity’ as a require-ment for reimbursement of services.”12
CPT® documents the direct link between the NPP (as illustrated in Appendix C) and appropriate levels of coding: “Clinical examples…are provided to assist physi-cians in understanding the meaning of the descriptors and selecting the correct code.”13DGs also documents the links between Medical Necessity, Nature of the Presenting Problem(s), and medically appropriate levels of care:
z “Payers…. may request information to validate…. the medical necessity and appropriateness of the diagnostic and/or therapeutic services provided.”14
z “The extent of history of present illness, review of systems and past, family and/or social history that is obtained and documented is dependent upon clinical judgment and the nature of the presenting problem(s).”15
z “The type (general multi-system or single organ system) and content of examination are selected by the examining physician and are based upon clinical judgment, the patient’s history, and the nature of the presenting problem (s)”16
Although it is clear that assessment of the Nature of the Presenting Problem(s) is best accomplished by the clinician at the point of care, it is noteworthy that the CPT® and Documentation Guidelines both fail to suggest that clinicians should document their professional assessment of the NPP. The additional documentation of this qualitative measure through well-designed EHR screens is effective for promoting compliant E/M coding and providing audit protection. In the absence of such clinician documentation, the coder is compelled either to make this determination without clinical guidance or to seek the assistance of an authoritative clinician.
SummaryofEHRDesignIssuesAchieving information integrity in E/M services (i.e., the clinical history and physical) is far more complex than optimizing objective data. This is because clinical data includes both objective (i.e., “quantitative”) and subjective (i.e., “qualitative”) information. This clinical information is individualized rather than “black and white,” and should be documented using appropriate descriptive narratives in addition to straightforward “yes or no” and “normal or abnormal” findings.
The problems with current EHR design efforts to achieve clinical information integrity and documentation compli-ance can be distilled down to five non-compliant designs and functions. These five functions, which are prevalent in almost all current EHR systems, lead not only to loss of E/M compliance, but also to decreased usability, decreased efficiency, diminished clinical data integrity, and poten-tially compromised patient safety. Three of these are design features should be eliminated to promote information integrity, and the other two are design features that are currently missing and must be added. It is noteworthy that compliance with all five of these features is mandated by existing CMS regulations and documents, which are not currently being enforced in the EHR domain nor included in certifications that qualify for “meaningful use” under HITECH. This workbook will address these five problems one at a time, starting with the two features that should be added, then following with the three that should be deleted, rectified, or turned off.
Add#1:ConsiderationofMedicalNecessityMedical necessity is the governing factor in E/M leveling, yet is omitted from the majority of EHRs. The Medicare Claims Processing Manual, Chapter 12, Section 30.6. states: “Medical Necessity is the overarching criterion for pay-ment, in addition to the individual requirements of a CPT® code.”
Furthermore, Social Security Law, section 1862 says, “Medicare will not pay for services that are not medically necessary.”
Documentation Guidelines from 1995 and 1997 also demand that the nature of the presenting problem support the level of service provided. A simple UTI does not warrant a level 4 CPT® code, regardless of the level of exam and history taken. Here are some DG excerpts:
z “The extent of history of present illness, review of systems and past, family and/or social history that is

Advanced E/M Coding for EHRs
10 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
obtained and documented is dependent upon clinical judgment and the nature of the presenting problem(s)” [note: the NPP is the E/M system’s measure of medi-cal necessity].
z “The type (general multi-system or single organ system) and content of examination are selected by the examining physician and are based upon clinical judgment, the patient’s history, and the nature of the presenting problem(s).” [note: the NPP is the E/M sys-tem’s measure of medical necessity].
z “Payers want and “may request documentation to vali-date….the medical necessity and appropriateness of the diagnostic and/or therapeutic services provided.”
What will happen when EHR developers are successful in effectively incorporating the medical necessity guidance on compliance, clinical data quality, and information integrity into EHRs? We will find that the physician will be documenting their thought processes, and treating all the patient’s presenting problem rather than focusing on counting enough “bullets.” This will also assist the physician in establishing a medically indicated level of E/M care for each patient at each encounter, rather than relying on data from past encounters. With paper charts, physicians were counseled to “think in ink” so their medical decision making would be well documented. Perhaps today’s physicians should be counseled to “glean on the screen,” using narrative descriptions rather than pre-loaded menus or codes to ensure their thought processes are well documented. This protects the provider from overcoding and charges of fraud and abuse. It also protects the patient, as focusing on the presenting problems will ensure the patient receives the appropriate level of care.
Add#2:TheQualitativeMeasuresSpecifiedinDocumentationGuidelinesEHR coding engines and electronic H&P data entry screens commonly adopt all of the easily measured quanti-tative requirements of the DGs. Programming to help cli-nicians additionally document and consider the qualitative measures of the DGs requires more sophisticated consider-ation, but it is possible to accomplish this goal
Governing regulations appear in DGs (1995 and 1997). Examples of the qualitative measures are underlined below.
History“DGs state, “The ROS and/or PFSH may be recorded by ancillary staff or on a form completed by the patient. To
document that the physician reviewed the information, there must be a notation supplementing or confirming the information recorded by others.”
Note that most EHRs permit recording of patient responses to PFSH and ROS questions (to “count” the quantitative number of elements) without requiring docu-mentation of the qualitative requirement that the positive responses be supplemented. The resulting insufficient and non-compliant documentation can result in failure to address positive responses for such potentially serious con-cerns as “diabetes,” “chest pain,” “weight loss,” and other potentially morbid conditions. As a result, the medical record can suffer not only non-compliance, but also loss of clinical data integrity, and the potential for significant patient safety issues.
Documentation Guidelines also state, “The HPI (history of present illness) is a chronological description of the development of the patient’s present illness from the first sign and/or symptom or from the previous encounter to the present. It includes the following elements” (eight elements listed).
Most EHRs guide documentation of some or all of the eight elements, often by fill-in-the-blank on pre-loaded templates listing those eight elements or through the use of pre-loaded macros with fill-in-the-blank for those eight elements. However, such designs exclude a requirement for the “chronological description of the course of the illness,” which is the essential element of a history.
Without this critical documentation, the clinical record presents nothing more than an expanded chief complaint, which is frequently inadequate for a precise or accurate differential diagnosis and assessment of the nature of the presenting problem. Absence of a detailed HPI disrupts cli-nicians’ ability to make accurate differential diagnoses and their ability to accurately assess the nature of the present-ing problem (i.e., medical necessity). Loss of these capabili-ties is frequently associated with an increased amount of non-specific testing and associated decrease in cost effec-tiveness
The DGs state, “Specific abnormal and relevant negative findings of the examination of the affected or symptomatic body area(s) or organ system(s) should be documented. A notation of ‘abnormal’ without elaboration is insufficient.”
Most current EHRs permit documentation of examination findings being “abnormal” without requiring individualized documentation describing the specific abnormalities. Most current EHRs also commonly fail to

Advanced E/M Coding for EHRs
AdvancedE/MCodingforEHRs www.aapc.com 11
require individualized documentation of the specific negative findings in all relevant organ systems related to the patient’s presenting problems (For example, relevant organ systems to be thoroughly documented for a presenting problem of chest pain should include detailed description not only the cardiovascular system, but also pulmonary, GI, Musculoskeletal, neurologic, dermatological, and psychiatric). This loss of precision and specificity affects ability for clinicians to achieve accurate diagnoses and information integrity as well as compliance.
Here’s an example from the documentation of a physical exam as recorded in the EHR. The narrative was generated from a checklist filled out by the physician:
As you can see, an abnormal gait was documented, but no further explanation was provided.
In the medical decision making component of the clinical record, “For each encounter, an assessment, clinical impression, or diagnosis should be documented…. For a presenting problem with an established diagnosis the record should reflect whether the problem is: a) improved, well controlled, resolving or resolved; or, b) inadequately controlled, worsening, or failing to change as expected. For a presenting problem without an established diagnosis, the assessment or clinical impression may be stated in the form of differential diagnoses or as a ‘possible,’ ‘probable,’ or ‘rule out’(R/O) diagnosis.”
Most current EHRs replace the qualitative or subjective descriptions required to meet these requirements with simplistic drop down menus of ICD-9 diagnosis codes to facilitate billing requirements. These codes not only fail to meet the descriptive requirements of DGs, but the restrictions for submitting claims for payment prohibit the required differential diagnoses by prohibiting “rule out” diagnoses or other qualifying descriptions. For example, there are no diagnosis codes for “possible hyperthyroidism,” or “probable asthma,” or “life-threatening obstructive sleep apnea.” In summary, there are no “qualitative” (i.e., descriptive) adjectives in the code sets used to submit for payment, and the rules for payment
claims prohibit use of uncertain, or “rule out” diagnoses. Physicians need to be reminded: selection of ICD-9 codes and their accompanying descriptions from a pull-down list in an EHR does not qualify as complete and medically effective documentation of their clinical impressions.
Remove#1:IncompleteandNon-compliantE/MCodingEnginesFrequently-encountered automated “coders” are built on a non-compliant and non-sanctioned (by CMS or by AMA) shortcut “scoring sheet” that first appeared in 1995. The compliance damage caused by these coding engines is magnified by the fact that programmers commonly build their clinical H&P screens 1:1 upon the requirements needed to satisfy these coding engines. As a result, the items missing from the scoring sheet are missing from the data entry screens (e.g., absence of consideration of qualita-tive guidelines), thereby negatively affecting compliance, information integrity, quality of care, and patient safety
This truncated scoring sheet fails to include multiple ele-ments of the E/M system, such as:
z Qualitative DGs for the HPI z Qualitative DGs for the PFSH and ROS z Qualitative DGs for the physical examination

Advanced E/M Coding for EHRs
12 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
z “Number of treatment options” element of medical decision making
z “Complexity of data ordered or reviewed” element of medical decision making
z “Nature of the presenting problem(s),” the E/M sys-tem’s measure of medical necessity
This truncated scoring sheet also includes a non-compliant measure for “number of possible diagnoses.” Specifically, it provides that “one new diagnosis” is the equivalent of “multiple diagnoses” as required in CPT® and the DGs. These sanctioned guidelines do NOT distinguish between number of new diagnoses and number of established diagnoses. Further, this system allowing “one new diagnosis” to be the equivalent of multiple diagnoses permits coding of moderate complexity decision making (supporting level 4 claims) for any new patient complaint, even those as minor as a sprained ankle or a fever blister. This scoring sheet currently appears on six of the nine MAC web sites. At a recent HIMSS roundtable discussion, this inconsistency was presented to CMS leaders as one of the underlying causes of improper upcoding in EHRs. HIMSS is hopeful that this revelation will lead to CMS action to eliminate this aberration in the near future.
Remove#2:AutomatedEntryofClinicalInformation,Resultingin“Cloned”DocumentationMedicare Administrative Contractors have identified the problem with automated entry of clinical information (cloned documentation) for years, saying it “does not meet medical necessity requirements for coverage of services…. Cloning of documentation is considered a misrepresenta-tion of the medical necessity requirement for coverage of services. Identification of this type of documentation will
lead to denial of services for lack of medical necessity and recoupment of all overpayments made.”22
Types of automated clinical data entry functionality that creates “cloned” clinical records include:
z Documentation by exception z Copy forward of previously entered clinical informa-tion
z Copy and paste of generic pre-loaded and non-specific macros
z Generic “pick lists” z Translation of individual documentation by check box into automated generic “pseduo-narrative” descriptions
Cloned documentation is inadequate to substantiate care was actually performed. CMS Carrier Manual, Section 7103.1(i) states: “The following are examples of situations in which the physician is liable for refunding an overpayment… Physician does not submit documentation to substantiate that he performed services billed to program where there is question as to whether they were actually performed.” This section of the CMS Carrier Manual is customarily summarized to mean, “if care wasn’t documented, it wasn’t done.” Applying this regulation to “cloned documentation” leads to the conclusion that portions of the record that have automated entry have not been adequately documented by the physician, and therefore no care can be credited in an audit of these sections. In summary, automation is not documentation.23
Medicare Claims Processing Manual, Chapter 12, Section 30.6.1. states, “Medical Necessity is the overarching criterion for payment, in addition to the individual requirements of a CPT® code.” Because cloned documentation does not meet medical necessity requirements, it fails to fulfill compliance requirements
Here is an excerpt from a date of service in a 2012 EHR:
HPI: Patient is here as an add-on for evaluation of left-sided neck wound site of prior biopsies. Otherwise he also has a lesion involving the right ear with some tenderness that is thought to be inflammatory nodule and not associated with malignancy. No reports of any fever chills nausea or vomiting. The area was examined. No residual sutures noted. Steri-Strips was applied.

Advanced E/M Coding for EHRs
AdvancedE/MCodingforEHRs www.aapc.com 13
This HPI shows a patient whose chief complaint is an inflamed biopsy site on his neck, with an assessment/plan to dress the wound. The following diagnoses were assigned by the EHR to the visit. Note the complex assessment and plan:
A/P: Right ear lesion is thought to be nonmalignant no changes at this time.
Open wounds involving the left neck site of prior incision was examined and dressing was placed.
Diabetes II with diabetic nephropathy and diabetic neuropathy (250.40): Doing moderately well, so far no changes continue with current management.
ED – Impotence of organic origin (607.84): conservative therapy for now
HTN (benign)(401.1): moderately well controlled with current medication; osteoarthritis, multiple sites (715.89): avoid nonseteroidal anti-inflammatory medications
SSS/SINOATRIAL NODE DYSFUNCTION (427.81): doing well since pacemaker placement,
history of anemia (V12.3): doing well so far.
diabetic nephropathy (583.81) : continue with ACE inhibitor therapy
diabetic neuropathy (357.2) : continue with daily foot examination
atherosclerosis disease of aorta (440.0) : No new changes
diverticulosis, without GI bleed (562.10) : denies any changes in his bowel habits
insomnia (780.52) : doing moderately well so far
PERIPHERAL VASCULAR DISEASE, Carotids (443.9) : no major changes noted. Recheck on yearly basis.
AK (702.0) : no acute changes noted
B12 deficiency (266.2) : continue with B12 replacement therapy
Impacted Cerumen (380.4) : no evidence of any reaccumulation at this time
There is little doubt that the diagnoses beyond the neck lesion and healing incision site are cloned (i.e., copied and pasted) from previous encounters. The only way they are mentioned elsewhere in the note is that some of these diagnoses can be lined to a cloned list of prescription medications also appearing as part of this date of service’s documentation.
Remove #3: Integration of billing diagnosis coding func-tionality into documentation of medical decision making
The Medical Decision Making (MDM) component of E/M compliance calls for documentation of the “number of possible diagnoses and/or the number of management options that must be considered.”24 Both clinically and according to DGs, effective documentation of MDM includes listing an appropriate differential diagnosis, including possible or “rule out” diagnoses. However, billing compliance rules prohibit use of “rule out” diagnoses, thereby truncating clinicians’ ability to document their decision making process.
The differential diagnosis also provides clinicians an opportunity to describe the details and nuances that individualize a specific patient’s clinical problems, and also to convey the nature of a patient’s presenting problem(s) (i.e., medical necessity) during each encounter. In addition to the differential diagnoses, clinicians should also be able to document:
z The relative probability of each possible diagnosis; i.e., in addition to stating “rule out,” clinicians should be able to document the descriptive terms “unlikely,” “possible,” “probable,” etc.
z The relative severity of each possible diagnosis; i.e., clinicians should be able to document the descriptive terms “mild,” “moderate,” “severe,” “life-threatening,” etc.
z The relative timing of each possible diagnosis; i.e., clinicians should be able to document the descriptive terms “constant,” “intermittent,” “occasional,” “rare,” “fluctuating,” “unpredictable,” etc.

Advanced E/M Coding for EHRs
14 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
z Special differentiating features of each possible diag-nosis; i.e., clinicians should be able to document the descriptive terms “unusual,” “atypical,” “paradoxical,” “well-differentiated (tumor),” “poorly-differentiated (tumor),” “undifferentiated (tumor),” etc.
Documentation Guidelines state, “For each encounter, an assessment, clinical impression, or diagnosis should be documented… For a presenting problem without an established diagnosis, the assessment or clinical impression may be stated in the form of differential diagnoses or as a ‘possible’, ‘probable’, or ‘rule out’(R/O) diagnosis”25
There are clinical implications of disrupting MDM documentation through the alternative of using of medical codes. Codification of medical records is a process of creating shorthand descriptions needed for payment process or generalized data collection. Such shorthand descriptions are inadequate to characterize the breadth, depth, and/or degree of specificity required to describe the characteristics of individual patients and support their individualized care. ICD-9 and ICD-10 diagnosis codes do not provide this required degree of specificity.
Loss of ability to document the individualized patient-specific and visit-specific features of each encounter also tends to impair clinicians’ diagnostic evaluation and thereby disrupt optimal selection of diagnostic procedure choices, management options, and optimal effectiveness of care. EHR programming that non-compliantly requires the use of diagnosis codes to document clinical impressions both distorts the purpose of coding and interferes with the purpose of MDM documentation. Codes should be a summary overview of the care provided and documented. They should not, however, be used in a manner that dictates and truncates clinicians’ documentation and thereby disrupts the patient care process.

Advanced E/M Coding for EHRs
AdvancedE/MCodingforEHRs www.aapc.com 15
Users’ Tips for the E/M Compliant Coding & Auditing Forms
This color-coded E/M evaluation tool brings coders a structured worksheet that can assist with coding, auditing, and clinician education. For any coder or auditor who has a comfortable working knowledge of E/M’s primary reference sources (CPT® and the Documentation Guidelines), most of the core E/M materials should be familiar. There are added sections addressing the impact of Electronic Health Record (EHR) data entry approaches that have been recognized in a variety of CMS and Medicare Contractor publications as being intrinsically non compliant, due to failure to support Medical Necessity Each page of the forms has its own set of written instructions. Experienced coders should find both the color-coded “counting” sections and the instructions related to quantitative measures similar to many conventional coding approaches, though with only compliant measures. However, CPT and Documentation Guidelines also contain qualitative criteria, including a measure for Medical Necessity, which are grounded in quality care practices. Although often overlooked in conventional coding and documentation approaches (and almost uniformly overlooked in EHR designs), these qualitative criteria bear equal importance with quantitative measures. Form selection As we know, each type of service has a unique coding paradigm for calculating the seven components of E/M coding. Therefore, a unique set of forms must be used for each type of service. This workbook includes form sets for two types of service:
• Initial outpatient visit • Established outpatient visit
Forms for other types of service, such as inpatient care, emergency department, observation, etc. can be obtained from the author if needed Core principles 1) E/M components and sub-components
a) In practical terms, the seven E/M components break down to three sub-components: i) The three “key components” (history, examination, and medical decision
making) (a) These three components are evaluated on the first and second color-coded
forms ii) The “nature of the presenting problem(s),” which is the E/M system’s measure of
Medical Necessity (a) This component is evaluated on the third color-coded form
iii) Time, which is considered only when documentation confirms that more than 50% of the time of the encounter is dominated by counseling and/or coordination of care
(a) This component is evaluated on the fourth color-coded form b) For compliant coding and auditing, the documented levels for each of these three sub-
components must be compared with each other and, if applicable, with the code selected by the clinician. This final step is evaluated on the final page of the coding packet. As a basic principle, coders and auditors should recognize that the level of care calculated by the three “key components” is subordinate to both: i) The level of care determined by time (when documented appropriately); this
principle is presented on the final page of the “Documentation Guidelines” ii) The level of care determined by the Nature of the Presenting Problem(s) – “NPP”

Advanced E/M Coding for EHRs
16 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
(a) Per Medicare policy, “Medical Necessity is the overarching criterion for payment,” and the NPP is the E/M system’s measure of Medical Necessity
(b) Unfortunately, physicians have generally not been taught to document their assessment of the NPP; when using these forms, you should note that fact with an asterisk next to your personal impression of the level of the NPP (on color coded page #3). Hopefully, this will help you encourage the clinicians to document this assessment going forward
2) Coding interplay among quantitative guidelines, qualitative guidelines, and findings of non-compliant EHR data-entry functionality (i.e., “cloned records”) a) Different types of guidelines
i) Quantitative guidelines determine the amount of care that was provided (as indicated by the documentation)
ii) Qualitative guidelines determine the whether that care was provided in a medically complete and medically appropriate manner (as indicated by the documentation)
iii) Medical Necessity indicates whether the amount of care provided was appropriate for the nature of the presenting problems and “in accord with generally accepted standards of practice”1
b) Conventional approaches to E/M commonly focus on the quantitative aspects of the Documentation Guidelines that can easily be counted (and are easily programmed into EHR code calculating engines), to the exclusion of considering the equally significant qualitative Documentation Guidelines and even more significant qualitative NPP
c) These Compliant E/M Coding and Auditing forms incorporate all these qualitative guidelines and the NPP i) These guidelines appear as check boxes beneath the color-coded quantitative
features ii) The basic principle for evaluating these qualitative guidelines is that if the
qualitative features are not properly documented, then no credit should be given for the entire section, regardless of the number of quantitative features present in the documentation (1) For example, in the ROS of an initial patient visit, regardless of the number of
organ systems with documented questions and “yes” or “no” responses from the patients, the qualitative Documentation Guideline requires all positive responses to be “supplemented” (i.e., with additional questions to evaluate the significance of these responses) (a) If supplemental information is not documented, it would be inappropriate to
give any credit for the ROS; this would be indicated by checking the box corresponding to “fails to document supplemental findings of the ROS.” Then the yellow box for “0 systems” would be circled
(b) This action correlates with quality care principles, since patients’ signs and symptoms could indicate significant underlying illness, and this must be evaluated
(c) This action also correlates with potential liability problems if these positive responses (e.g., “chest pain”) are not evaluated and the patient subsequently suffers harm (e.g., heart attack)
(2) For example, in the HPI, if the documentation fails to provide a “chronological description of the course of the illness,” then a history has not been documented.
1 Quoted from the definition of “medical necessity” presented on the AMA web site

Advanced E/M Coding for EHRs
AdvancedE/MCodingforEHRs www.aapc.com 17
(a) In this circumstance, it would be inappropriate to give any credit for the HPI; this would be indicated by checking the box corresponding to “fails to document chronological details of HPI.” Then the red box for “no HPI” would be circled
(b) Note: initially, coders or auditors in their own practice may wish to use judgment to reduce HPI to level of a “brief” HPI, followed by clinician education
(3) For example, in the physical exam section, if the documentation fails to provide “details of abnormal findings and details of normal findings for all organ systems related to the presenting problem(s),” then a satisfactory examination has not been documented
d) In reviews of EHR documentation (or dictated records built on pre-loaded macros or copy forward of information from prior visits), CMS and by MACs have established the policy that the use of data-entry shortcuts that result in “cloned” records lack patient-specific and visit-specific information. As a result such records fail to support medical necessity, and no credit should be given. i) When this type of non-compliant pseudo documentation is identified, please
check the box labeled “EHR documentation compliance issues” and an associated box indicating the type of improper data entry identified (e.g., “documentation by exception”)
ii) Under this circumstance, the red boxes for “no history” or “no exam” should be circled
3) The final (summary) page of the forms compiles all of the components already assessed, and they allow the coder to compare the levels for code submitted, code based on key components, code based on NPP, and code based on time a) For clinician education, this summary page may be placed on the front of the packet and
used to present findings. The remaining pages then provide the detail that builds to these conclusions
4) Added optional features a) The coder may choose to complete the “data gathering form” to indicate which elements
of the PFSH, ROS, and physical examination have been documented b) The check boxes on the left side of the medical history form (page 1) provide the coder
with similar capability to document which of the 8 elements of HPI were identified, as well as whether there is documentation of the “chronology” required for a valid medical history
c) Note that in the medical history section of page 1 of the established outpatient visit form, there is a check box to indicate “level based on documented ‘update’ of PFSH and ROS.” i) This finding is compatible with the qualitative Documentation Guidelines that
permit clinicians to perform an update (i.e., eliciting and documenting changes to PFSH and ROS since last visit) instead of repeating all of these questions completed during initial visit
ii) Also note that, with this approach, the level of PFSH and ROS for the current visit must duplicated the level at the previous visit. When there are updates documented on all established patient visits, then the level of PFSH and ROS are based on the extent of this care documented on the initial visit for that patient

Patient: Name:__________________ Chart #: ________ Date of visit: ___/___/____Reviewed by: __________________ Date of review: ___/___/____
Select the level corresponding to lowest of the components Level of HistoryPFSH HPI
5 3 elements ComprehensiveRelated 4 status of > 3 chronicsE/M level: 3 1 element Detailed
2 0 elements Expanded1 Prob focused
no HPI no historyChronology Fails to document or clearly reflect a chief complaintDuration Fails to document supplemental details of positive findings for PFSHTiming Fails to document supplemental details of positive findings for ROSSeverity Fails to document chronological details of HPI (performing only an "extended" Chief Complaint)Location Fails to document the STATUS of at least 3 chronic or inactive conditionsQuality *EHR documentation compliance issues fail to validate medical necessity &/or that care was performedContext Copy forward functionality Copy-paste of pre-loaded generic text Mod. factors Documentation by exception, automated or single click Assoc signs & Sx Non-specific documentation resulting from use of pick lists
Select the level corresponding to guideline description Level of Exammulti-system
5 2 in each of ComprehensiveRelated 4 9 systems
E/M level: 3 12 elements Detailed2 6-11 elements Expanded1 1-5 elements Prob focused
Fails to document specific abnormal findings no exam Fails to document relevant negative findings of symptomatic organ systems
*EHR documentation compliance issues fail to validate medical necessity &/or that care was performed Copy forward functionality Copy-paste of pre-loaded generic text Documentation by exception, automated or single click Non-specific documentation resulting from use of pick lists
Select the level corresponding to guideline description Level of Exam
5 8 organ systems or complete single organ system exam ComprehensiveRelated 4E/M level: 3 Extended exam of affected & related areas/systems Detailed
2 Limited exam of affected & related areas/systems Expanded1 Limited exam of affected body area or organ system Prob focused
Fails to document specific abnormal findings no exam Fails to document relevant negative findings of symptomatic organ systems
*EHR documentation compliance issues fail to validate medical necessity &/or that care was performed Copy forward functionality Copy-paste of pre-loaded generic text Documentation by exception, automated or single click Non-specific documentation resulting from use of pick lists
Note: Draw a line through all the levels of care and NPP to indicate the E/M code level submitted
in each minor
12 elements6-11 elements1-5 elements
in each minor
9 elements6-8 elements1-5 elements
1 system0 systems
Ophth & Psychall major, one
specialtyall major, one
Practical E/M Audit Form: Initial Outpatient Visit (p.1)
Medical History Review
Physical Exam Review (1997 Guidelines)
Physical Exam Review (1995 Guidelines)
4-8 elements, or
1-3 elementsor no chronology
ROS10 or more
2-9 syst
Created 2009 by ASA, LLC

Instructions, Medical History Section:
1) Circle the number of documented elements of the PFSH; 2) Circle the range containing the number of documented elements of the ROS; 3) Circle the range containing the number of elements of the HPI documented on page 1 Be sure to indicate if these elements include a "chronological description of course of illness" 4) Review the four boxes evaluating the qualitative Documentation Guidelines of the Medical History Document any qualitative features not completed and adjust the quantitative values circled if indicated 5) Review the four boxes evaluating possible non-compliant data entry functions by an EHR (or dictation) Document any non-compliant data entry functions and adjust the quantitative values circled if indicated 6) Then circle the Level of History that corresponds to the lowest of the three key components circled 7) Transfer this Level of History to the Level of History column on page 5
Instructions, Physical Examination Section:
A) 1997 Documentation Guidelines 1) Select the column for the type of examination documented: general multi-system examination, one of the 11 specialty specific examinations other than opthalmology or psychiatry, or ophthalmology or psychiatry 2) Circle the range containing the number of documented examination elements in the appropriate column 3) Review the two boxes evaluating the qualitative Documentation Guidelines of the Physical Examination Document any qualitative features not completed and adjust the quantitative values circled if indicated 4) Review the four boxes evaluating possible non-compliant data entry functions by an EHR (or dictation) Document any non-compliant data entry functions and adjust the quantitative values circled if indicated 5) Circle the Level of Exam that corresponds to this number of exam elements
B) 1995 Documentation Guidelines (if indicated) 1) Circle the appropriate level of examination documented; note that "extended" applies to all organ systems and that all systems potentially related to the presenting problem(s) should be examined and documented 2) Circle the Level of Exam that correspondes to this description 3) Review the two boxes evaluating the qualitative Documentation Guidelines of the Physical Examination Document any qualitative features not completed and adjust the quantitative values circled if indicated 4) Review the four boxes evaluating possible non-compliant data entry functions by an EHR (or dictation) Document any non-compliant data entry functions and adjust the quantitative values circled if indicated
C) Transfer the higher of these two Levels of Exam to the Level of Exam column on page 5
Instructions for Page 1

Section 1: Medical History
HPI: see color sheet for listing of chronologic description & 8 elements of HPI
PFHS: record which elements have documented inquiries & responses(see color sheet for documentation of qualitative factors & EHR data entry issues) Past medical history Family history Social history
Number of elements documented ______
ROS: record which organ systems have documented inquiries & responses(see color sheet for documentation of qualitative factors & EHR data entry issues) Constitutional Gastrointestinal Neurological Eyes Genitourinary Psychiatric Ears, nose, & throat Musculoskeletal Endocrine Cardiovascular Integumentary Hematologic/lymphatic Respiratory (skin and/or breast) Allergic/immunologic
Number of organ systems documented ______
Section 2: Physical Examination
1997 Documentation Guidelines: Types of Examinations: General multi-system exam Genitourinary (female) Neurological Cardiovascular Genitourinary (male) Psychiatric Ears, nose, & throat Hematologic/lymphatic/immunologic Respiratory Eyes Musculoskeletal Skin
see exam details in "Documentation Guidelines for Evaluation & Management Coding" to identify number of designated exam elements documented
1995 Documentation Guidelines: Body areas: Head and face Abdomen Back, including spine Neck Genitalia, groin, buttocks Each extremity Chest, incl. breasts & axillae
Organ systems: Constitutional Respiratory Skin Eyes Gastroinstestinal Neurological Ears, nose, mouth, throat Genitourinary Psychiatric Cardiovascular Musculoskeletal Hematol/lymph/immunol
Documentation Details: All other symptomatic or related organ systems documented All other symptomatic or related organ systems NOT documented LIMITED examination of (all) affected and symptomatic/related organ systems
(includes cases with less than an extended exam of ALL affected & related organ systems) EXTENDED examination of (all) affected and symptomatic/related organ systems COMPLETE examination of a single organ system
Data Gathering Form, History & Exam (p.1B)

Patient: Name: _________________ Chart #: _________ Date of visit: ___/___/____
Select the 2nd lowest of the RED circled levels Level of MDM
Dx or Rx Options Data Reviewed & Ordered Levels of Risk
5 ext 4 ext 4 ext 4 ext ext 4 ext high high high High
Related 4 mult 3 mult 3 mod3 mod mod 3 mod mod mod mod Mod
E/M level: 3 lim 2 lim 2 lim 2 lim lim 2 lim low low low Low
2 min 1 min 1 min 0-1 min min 0-1 min min min min Strtfrwd1
cmplx cmplx pres diag mgmt no MDMDx Rx # rev rev # ord ord probs proc optns
Circle highest in red Circle highest of 4 in red Circle highest of 3 in red
* Indicates sub-component(s) of MDM that were not documented in the medical record
Interpretation: 1) Level of each MDM component is circled in blue or black ink, whether documented or interpreted by reviewer 2) Highest level in each of the three sections is circled in red ink; 3) An asterisk within the circle of any sub-component indicates that it was not documented in the medical record 4) The calculated level of MDM corresponds to the 2nd lowest of the red circles, which appears in the final column Note: Draw a line through all the levels of care and NPP to indicate the E/M code level submitted
Glossary:Dx or Rx OptionsDx: number of diagnoses min: minimumRx: number of treatment options lim: limited
mult: multipleext: extensive
Data Reviewed & Ordered# rev: amount of data reviewed min: minimumcmplx rev: complexity of data reviewed lim: limited# ord: amount of data ordered mod: moderatecmplx ord: complexity of data ordered ext: extensive
Levels of Riskpres probs: risk of the presenting problem(s) min: minimumdiag proc: risk of the diagnostic procedures low: lowmgmt optns: risk of the management options mod: moderate
high: high
Practical E/M Audit Form: Initial Outpatient Visit (p.2)
Medical Decision Making (MDM)
Created 2009 by ASA, LLC

Patient: Name: _________________ Chart #: ________ Date of visit: ___/___/____
Code Level Warranted by NPP
5
Moderate-High 4
3
2
11
* Indicates severity of NPP is not documented in the medical record
Interpretation: 1) Circles indicate severity of NPP and level of code warranted by this degree of severity 2) If severity of NPP not documented in medical record, level of severity and corresponding level of warranted care seem appropriate based on remaining documentation; indicated by asterisk (*) 3) If appropriate severity seems to be "moderate to high," choice of code level 4 or 5 based on level of care suggested as appropriate by the examples in CPT's Appendix C and/or highest documented level of risk Note: Draw a line through all the levels of care and NPP to indicate the E/M code level submitted
CPT Descriptors for Severity of NPP: (* intermediate descriptors interpreted by Practical E/M)
Minor: Problem runs definite and prescribed course, is tansient in nature, and is not likely to permanentlyalter health status; OR, has a good prognosis with management and compliance
Low: Problem where the risk of morbidity without treatment is low; there is little to no risk of mortalitywithout treatment; full recovery without functional impairment is expected
Low - Mod: *Problem where the risk of morbidity without treatment is low to moderate; there is low to moderaterisk of mortality without treatment; full recovery without functional impairment is expected in most cases, with low probability of prolonged functional impairment
Moderate: Problem where the risk of morbidity without treatment is moderate; there is moderate risk of mortality without treatment; prognosis is uncertain, or there is an increased probability of prolonged functional impairment.
Mod - High: *Problem where the risk of morbidity without treatment is moderate to high; there is moderate risk of mortality without treatment; uncertain prognosis or increased probability of prolonged functional impairment
High: Problem where the risk of morbidity without treatment is high to extreme; there is moderate to high risk of mortality without treatment, or high probability of severe prolonged functional impairment.
Practical E/M Audit Form: Initial Outpatient Visit (p.3)
Low-Moderate
LowMinor
Nature of the Presenting Problem(s)
Moderate-High or High
Moderate
Created 2009 by ASA, LLC

Patient: Name: ________________ Chart #: _______ Date of visit: ___/___/____
DOCUMENTATION that > 50% of face-to-face time spent counseling and/or coorinating care DOCUMENTATION of total amount of FACE-TO-FACE time of visit DOCUMENTATION of counseling and/or coordination performed
Initial Visit Code LevelIndicated by
Time
60 mins 99205
45 mins 99204
30 mins 99203
20 mins 9920210 mins 99201
Interpretation: 1) Time considered for code selection ONLY if ALL THREE of the above boxes are checked 2) Time value selected must equal or exceed amount in selected box Note: Draw a line through all the levels of care and NPP to indicate the E/M code level submitted
Practical E/M Audit Form: Time for Counseling / Coordination of Care (p. 4)Initial Outpatient Visit
Time for Counseling / Coordination of Care
Created 2009 by ASA, LLC

Patient: Name: ________________ Chart #: _______ Date of visit: ___/___/____
Code Level Code Level Code Level by Key Warranted Indicated
Components by NPP by Time
Comprehensive Comprehensive High 99205 99205 99205
Moderate 99204 99204 99204
Detailed Detailed Low 99203 99203 99203
Expanded Expanded Strtfrwd 99202 99202 99202Prob focused Prob focused 99201 99201 99201
no history no exam no MDM N/ALevel of Level of Level of History Exam MDM
Interpretation: 1) "Level of history" is value that was determined on page 1 2) "Level of exam" is value that was determined on page 1; selected the higher of 1995 or 1997 Guidelines 3) "Level of MDM" is value that was determined on page 2 4) "Code level by key components" is indicated by the lowest level circled among the 3 key components If the medical record lacks documentation of history, examination, or MDM, then, by CPT definition, an E/M service was not performed; claim for E/M service should be denied 5) "Code level warranted by NPP" is value that was determined on page 3 6) "Code level indicated by Time" is value that was determined on page 4 (if time properly documented) 7) Note: Draw a line through all the levels of care and NPP to indicate the E/M code level submitted
The result of step 4 indicates the level of care performed and documented; The result of step 5 indicates the level of care that is medically necessary / indicated The result of step 6 indicates the level of care that is supported by time of counseling and coordination of care Usually, the code level warranted by the NPP establishes the maximum level of care that should be coded If time properly documented, code level determined by time supercedes key components & NPP if it was higher
Conclusion: code submitted: Code medically indicated based on NPP: Level of care documented:
Code level based on counseling & time: N/A
Select the level corresponding to the lowest component
Select Correct E/M Code
CPT Compliant E/M Audit Tools: Initial Outpatient Visit (Summary)
Created 2009 by ASA, LLC

Patient: Name: _________________ Chart #: _______ Date of visit: ___/___/____Reviewer: ___________________ Date of review: ___/___/____
Select the level corresponding to lowest of the components Level of HistoryPFSH HPI
5 2 elements ComprehensiveRelated 4 1 element >3 chronic conds DetailedE/M level: 3 0 elements Expanded
2 or no chronology Prob focused1
Level based on documented "update" of PFSH /ROS no historyChronology Fails to document or clearly reflect a chief complaintDuration Fails to document supplemental details of positive findings for PFSHTiming Fails to document supplemental details of positive findings for ROSSeverity Fails to document chronological details of HPI (performing only an "extended" Chief Complaint)Location Fails to document the STATUS of at least 3 chronic or inactive conditionsQuality *EHR documentation compliance issues fail to validate medical necessity &/or that care was performedContext Copy forward functionality Copy-paste of pre-loaded generic text Mod. factors Documentation by exception, automated or single click Assoc signs & Sx Non-specific documentation resulting from use of pick lists
Select the level corresponding to guideline description Level of Exammulti-system specialty Ophth & Psych
5 2 in each of 9 all major,1 ea minor all major,1 ea minor ComprehensiveRelated 4 12 elements 12 elements 9 elements DetailedE/M level: 3 6-11 elements 6-11 elements 6-8 elements Expanded
2 1-5 elements 1-5 elements 1-5 elements Prob focused1
Fails to document specific abnormal findings no exam Fails to document relevant negative findings of symptomatic organ systems
*EHR documentation compliance issues fail to validate medical necessity &/or that care was performed Copy forward functionality Copy-paste of pre-loaded generic text Documentation by exception, automated or single click Non-specific documentation resulting from use of pick lists
Select the level corresponding to guideline description Level of Exam
5 8 organ systems or complete single organ system exam ComprehensiveRelated 4 Extended exam of affected & related areas/systems DetailedE/M level: 3 Limited exam of affected & related areas/systems Expanded
2 Limited exam of affected body area or organ system Prob focused1
Fails to document specific abnormal findings no exam Fails to document relevant negative findings of symptomatic organ systems
*EHR documentation compliance issues fail to validate medical necessity &/or that care was performed Copy forward functionality Copy-paste of pre-loaded generic text Documentation by exception, automated or single click Non-specific documentation resulting from use of pick lists
Note: Draw a line through all the levels of care and NPP to indicate the E/M code level submitted
(note: level 1 appropriate when care provided under physician's supervision without physician present)
Physical Exam Review (1995 Guidelines)
0 system1 system2-9 syst
1-3 elements
ROS
Practical E/M Audit Form: Established Outpatient Visit (p.1)Medical History Review
Physical Exam Review (1997 Guidelines)
4-8 elements /10 or more
no HPI
Created 2009 by ASA, LLC

Section 1: Medical History
HPI: see color sheet for listing of chronologic description & 8 elements of HPI
PFHS: record which elements have documented inquiries & responses(see color sheet for documentation of qualitative factors & EHR data entry issues) Past medical history Family history Social history or UPDATE of PFSH from documented previous visit (assess # elements previously)
Number of elements documented ______
ROS: record which organ systems have documented inquiries & responses(see color sheet for documentation of qualitative factors & EHR data entry issues) Constitutional Gastrointestinal Neurological Eyes Genitourinary Psychiatric Ears, nose, & throat Musculoskeletal Endocrine Cardiovascular Integumentary Hematologic/lymphatic Respiratory (skin and/or breast) Allergic/immunologic or UPDATE of ROS from documented previous visit (assess # elements previously)
Number of organ systems documented ______
Section 2: Physical Examination
1997 Documentation Guidelines: Types of Examinations: General multi-system exam Genitourinary (female) Neurological Cardiovascular Genitourinary (male) Psychiatric Ears, nose, & throat Hematologic/lymphatic/immunologic Respiratory Eyes Musculoskeletal Skin
see exam details in "Documentation Guidelines for Evaluation & Management Coding"
1995 Documentation Guidelines: Body areas: Head and face Abdomen Back, including spine Neck Genitalia, groin, buttocks Each extremity Chest, incl. breasts & axillae
Organ systems: Constitutional Respiratory Skin Eyes Gastroinstestinal Neurological Ears, nose, mouth, throat Genitourinary Psychiatric Cardiovascular Musculoskeletal Hematol/lymph/immunol
Documentation Details: All other symptomatic or related organ systems documented All other symptomatic or related organ systems NOT documented LIMITED examination of (all) affected and symptomatic/related organ systems EXTENDED examination of (all) affected and symptomatic/related organ systems COMPLETE examination of a single organ system
Data Gathering Form, History & Exam

Patient: Name: _______________ Chart #: _________ Date of visit: ___/___/____
Select the 2nd lowest of the RED circled levels Level of MDM
Dx or Rx Options Data reviewed & ordered Levels of Risk
5 ext 4 ext 4 ext 4 ext ext 4 ext high high high High
Related 4 mult 3 mult 3 mod3 mod mod 3 mod mod mod mod Mod
E/M level: 3 lim 2 lim 2 lim 2 lim lim 2 lim low low low Low
2 min 1 min 1 min 0-1 min min 0-1 min min min min Strtfrwd1
cmplx cmplx pres diag mgmt no MDMDx Rx # rev rev # ord ord prob proc optns
Circle highest in red Circle highest of 4 in red Circle highest of 3 in red
* Indicates sub-component(s) of MDM that are not documented in the medical record (note - level 1 appropriate only when care provided under physician's supervision without physician present)
Interpretation: 1) Level of each MDM component is circled in blue or black ink, whether documented or interpreted by reviewer 2) Highest level in each of the three sections is circled in red ink; 3) An asterisk within the circle of any sub-component indicates that it was not documented in the medical record 4) The calculated level of MDM corresponds to the 2nd lowest of the red circles, which appears in the final column Note: Draw a line through all the levels of care and NPP to indicate the E/M code level submitted
Glossary:Dx or Rx OptionsDx: number of diagnoses min: minimum Rx: number of treatment options lim: limited
mult: multiple ext: extensive
Data Reviewed & Ordered# rev: amount of data reviewed min: minimum cmplx rev: complexity of data reviewed lim: limited# ord: amount of data ordered mod: moderatecmplx ord: complexity of data ordered ext: extensive
Levels of Riskpres probs: risk of the presenting problem(s) min: minimumdiag proc: risk of the diagnostic procedures low: lowmgmt optns: risk of the management options mod: moderate
high: high
Medical Decision Making
Practical E/M Audit Form: Established Outpatient Visit (p.2)
Created 2009 by ASA, LLC

Patient: Name: ________________ Chart #: _______ Date of visit: ___/___/____
Code Level Supported by NPP
5
Moderate-High 4
3
2
Minimal 1
* Indicates severity of NPP is not documented in the medical record
Interpretation: 1) Circles indicate severity of NPP and level of code warranted by this degree of severity 2) If severity of NPP not documented in medical record, level of severity and corresponding level of warranted care seem appropriate based on remaining documentation; indicated by asterisk (*) 3) If appropriate severity seems to be "moderate to high," choice of code level 4 or 5 based on level of care suggested as appropriate by the examples in CPT's Appendix C and/or highest documented level of risk Note: Draw a line through all the levels of care and NPP to indicate the E/M code level submitted
CPT Descriptors for Severity of NPP: (* intermediate descriptors interpreted by Practical E/M)
Minimal: Problem that may not require the presence of physician, but service is provided under physician's supervision
Minor: Problem runs definite and prescribed course, is tansient in nature, and is not likely to permanentlyalter health status; OR, has a good prognosis with management and compliance
Low: Problem where the risk of morbidity without treatment is low; there is little to no risk of mortalitywithout treatment; full recovery without functional impairment is expected
Low - Mod: *Problem where the risk of morbidity without treatment is low to moderate; there is low to moderaterisk of mortality without treatment; full recovery without functional impairment is expected in most cases, with low probability of prolonged functional impairment
Moderate: Problem where the risk of morbidity without treatment is moderate; there is moderate risk of mortality without treatment; prognosis is uncertain, or there is an increased probability of prolonged functional impairment.
Mod - High: *Problem where the risk of morbidity without treatment is moderate to high; there is moderate risk of mortality without treatment; uncertain prognosis or increased probability of prolonged functional impairment
High: Problem where the risk of morbidity without treatment is high to extreme; there is moderate to high risk of mortality without treatment, or high probability of severe prolonged functional impairment.
Low-Moderate
Low
Minor
Practical E/M Audit Form: Established Outpatient Visit (p.3)
Nature of the Presenting Problem
Moderate-High or High
Moderate
Created 2009 by ASA, LLC

Patient: Name: ________________ Chart #: ________ Date of visit: ___/___/____
Time for Counseling / Coordination of Care
DOCUMENTATION that > 50% of face-to=face time spent counseling and/or coorinating care DOCUMENTATION of total amount of FACE-TO-FACE time of visit DOCUMENTATION of counseling and/or coorination performed
Establ Visit Code LevelIndicated by
Time
40 mins 99215
25 mins 99214
15 mins 99213
10 mins 992125 mins 99211
Interpretation: 1) Time considered for code selection ONLY if ALL THREE of the above boxes are checked 2) Time value selected must equal or exceed amount in selected box Note: Draw a line through all the levels of care and NPP to indicate the E/M code level submitted
Practical E/M Audit Form: Established Outpatient Visit (p.4)
Crated 2009 by ASA, LLC

Patient: Name: _______________ Chart #: ________ Date of visit: ___/___/____
Select Correct E/M Code Code Level Code Level Code Level by Key Warranted Indicated
Components by NPP by Time
Comprehensive Comprehensive High 99215 99215 99215
Detailed Detailed Mod 99214 99214 99214
Expanded Expanded Low 99213 99213 99213
Prob focused Prob focused Strtfrwd 99212 99212 99212no M.D. no M.D. no M.D. 99211 99211 99211
no history no exam no MDM N/ALevel of Level of Level of History Exam MDM
Interpretation: 1) "Level of history" is value that was determined on page 1 2) "Level of exam" is value that was determined on page 1; selected the higher of 1995 or 1997 Guidelines 3) "Level of MDM" is value that was determined on page 2 4) "Code level by key components" is indicated by the next-to-lowest level circled among the 3 key components 5) "Code level warranted by NPP" is value that was determined on page 3 6) "Code level indicated by Time" is value that was determined on page 4 (if time properly documented) Note: Draw a line through all the levels of care and NPP to indicate the E/M code level submitted
The result of step 4 indicates the level of care performed and documented; The result of step 5 indicates the level of care that is medically necessary / indicated The result of step 6 indicates the level of care that is supported by time of counseling and coordination of care Usually, the code level warranted by the NPP establishes the maximum level of care that should be coded If time properly documented, code level determined by time supercedes key components & NPP if it was higher
Conclusion: code submitted: Code medically indicated based on NPP:
Level of care documented:
Code level based on counseling & time: N/A
Select level corresponding to 2nd lowest component
Practical E/M Audit Form: Established Outpatient Visit (Summary)
Created 2009 by ASA, LLC

Advanced E/M Coding for EHRs
AdvancedE/MCodingforEHRs www.aapc.com 31
AppearanceOptionsfortheH&PRecord:HybridModelvs.“Translation”31
This appendix illustrates examples, based on the data from a real clinical record, of two alternatives for the final appearance of the H&P record that the EHR can compile.
The first approach maintains the appearance of an optimal data entry interface, applying a combination of graphic elements (i.e., check boxes) to record quantitative elements and narrative (i.e., free text) sections to record qualitative elements required for both compliance and detailed indi-vidualized description of each encounter.
The second approach automatically “translates” this hybrid data entry appearance into the appearance of a traditional dictated record; i.e., a “pseudo-dictation,” where all ele-ments appear as narrative paragraphs.
These two alternatives will appear side-by-side to illustrate their differences in readability, searchability, and usabil-ity for purposes of E/M coding, liability protection, and clinical integrity. These comparative images may provide software designers and clinicians with a starting point for developing screens and forms that fulfill usability and efficiency measures, while also meeting E/M compliance requirements.
For the purpose of these illustrations, the narrative para-graphs precisely reproduce the exact wording that appears on the data collection screen. Reviewers should be aware, however, that in most current EHRs this adherence to exact translation is not present.
For example, a majority of these systems will translate a check box that says only “lungs normal” by expanding this content with a pre-loaded generic macro; the resultant translated paragraph would then automatically state, “The lungs have normal excursions with normal respiratory effort. They are also clear to percussion and palpation, with no evidence of rales, rhonchi, or wheezing.” Because this macro is not visible to the clinician at the time of recording that the lung findings are “normal,” there can be a significant disconnect between what the clinician actu-ally examined and observed and what the software auto-matically records.
This translated record also appears “cloned,” with unverifi-able identical wording in medical records of visit after visit and patient after patient.
The following paired pages illustrate the hybrid and trans-lated formats for the following sections of the medical His-tory and Physical
z Illustrations 1 and 2: Appearance for initial outpatient visit, chief complaint, past medical history, social his-tory, and family history (CC and PFSH)
z Illustrations 3 and 4: Appearance for initial outpatient visit, review of systems (ROS)
z Illustrations 5 and 6: Appearance for history of present illness (HPI) and physical examination
z Illustrations 7 and 8: Appearance for initial outpatient visit, medical decision making (MDM)
{ (note: the hybrid format also includes the rarely docu-mented qualitative E/M elements of complexity of data, three levels of risk, and nature of the presenting problem(s))
The following paired pages show, on the left, the documentation as generated through the EHR by the physician, and on the right, how the EHR interprets and writes the documentation to reflect the physician’s notes. As part of the classroom exercise, you will dissect the notes as created by the EHR to determine which elements are compliant and what the proper E/M coding levels should be. These are presented as points of discussion and are open to interpretation.
Attendees should examine these examples to determine if any of the noncompliant elements shown are present in their workplace EHRs or in the EHRs they are considering for adoption. The ASA Audit tools can be used to assist in the evaluation of these charts.


1
Appearance Options for the H&P Record: Hybrid Model vs. “Translation”1
This appendix illustrates examples, based on the data from a real clinical record, of two alternatives for the final appearance of the H&P record that the EHR can compile. The first approach maintains the appearance of an optimal data entry interface, applying a combination of graphic elements (i.e., check boxes) to record quantitative elements and narrative (i.e., free text) sections to record qualitative elements required for both compliance and detailed individualized description of each encounter. The second approach automatically “translates” this hybrid data entry appearance into the appearance of a traditional dictated record; i.e., a “pseduo dictation, where all elements appear as narrative paragraphs. These two alternatives will appear side-by-side to illustrate their differences in readability, searchability, and usability for purposes of E/M coding, liability protection, and clinical integrity. These comparative images should hopefully provide software designers and clinicians with a starting point for developing screens and forms that fulfill usability and efficiency measures while also meeting E/M compliance requirements.
For the purpose of these illustrations, the narrative paragraphs precisely reproduce the exact wording that appears on the data collection screen. Reviewers should, however, be aware that in most current EHRs this adherence to exact translation is not present. A majority of these systems will translate a check box that says only “lungs normal” by expanding this content with a pre-loaded generic macro; the resultant translated paragraph would then automatically state “The lungs have normal excursions with normal respiratory effort. They are also clear to percussion and palpation, with no evidence of rales, rhonchi, or wheezing.” Since this macro is not visible to the clinician at the time of recording that the lung findings are “normal,” there can be a significant disconnect between what the clinician actually examined and observed and what the software automatically records. This translated record also appears “cloned,” with unverifiable identical wording in medical records of visit after visit and patient after patient.
The following paired pages illustrate the hybrid and translated formats for the following sections of the medical History and Physical
• Illustrations 1 & 2: Appearance for initial outpatient visit, chief complaint, past medical history, social history, and family history (CC & PFSH)
• Illustrations 3 & 4: Appearance for initial outpatient visit, review of systems (ROS)
• Illustrations 5 & 6: Appearance for history of present illness (HPI) and physical examination
• Illustrations 7 & 8: Appearance for initial outpatient visit, medical decision making (MDM)
o (note: the hybrid format also includes the rarely documented qualitativeE/M elements of complexity of data, three levels of risk, and nature of the presenting problem(s))
1 This section is derived, with minor modifications, directly from Appendix F of “Practical E/M: Documentation and Coding Solutions for Quality Patient Care,” second edition, Chicago, AMA Press, 2008, pages 353 - 363

Patient Name: Account No. DOB: ____/____/____
Patient Medical History Form (p. 1): Please provide the following medical information to the best of your ability:
Date: January 10, 2002 Age: 47 List any ALLERGIES TO MEDICATIONS:
What problems are you here for today?
Ears clogged Codeine - causes nausea
Past Medical History:
1) Please check the "Yes" or "No" box to indicate if you have any of the following illnesses; for "Yes" answers, please explain
Yes No Yes No
Diabetes ������������ Stomach or intestinal problems ������������
Hypertension (high blood press) ������������ Allergy problems/therapy ������������ seasonal
Thyroid problems ������������ Kidney problems ������������
Heart Disease/cholesterol probs ������������ elevated cholesterol Neurological problems ������������
Respiratory problems ������������ occasional asthma Cancer ������������
Bleeding Disorder ������������ Other Medical Diagnosis ������������
Cholesterol of 230 diagnosed 3 years ago, dropped to 170 on medication, followed by Dr. X
Occasional mild asthma symptoms, has not required regular medication; inhaler prn
Mild seasonal allergy symptoms in the spring, with frequent sneezing and watery eyes
2) Please list any operations (and dates) you have ever had (including tonsils & adenoids) :
Right knee surgery 1999 - repair lateral cruciate ligament
3) Please list any current medications (and amounts, times per day);
������������������������������������������������ �� ����������������������� ��� ��������������������������������������� �����������������������
Ibuprofen, 400 mg as needed for pain; antihistamine X prn allergy Sx, atorvastatin 10 mg. per day; inhaler Y prn
Social History: Yes No Please list details below:
Do you use tobacco? ������������ List type and how much:
If no, did you use it previously? ������������ List type and how much: 1/2 pack per day for 1 year When did you quit? age 19
Do you drink alcohol? ������������ List type and how much: 4 - 5 beers per week
Do you drink caffeine? ������������ List type and how much: 2 - 3 cups coffee per day
What is your occupation? Electrician
Family History:
Please check the "Yes" or "No" box to indicate whether any relatives have any of the following illnesses:
If yes, please indicate which relative(s) have the problem
Yes No
Hearing problems ������������
Heart problems / murmurs ������������ Father died of heart attack, had high cholesterol
Allergy ������������ Mother has spring and fall allergies
Diabetes ������������
Cancer ������������ Mother had breast cancer - cured with surgery and radiation
Bleeding disorder ������������
Anesthesia problems ������������ Mother has nausea following general anesthesia
Reviewed by: XXX
Copyright 2006 by ASA, LLC ENT New Patient Form page 1

5
J.2 PFSH: transcription model
Patient is a 49-year old male who presents with
Chief complaint: clogged ears
Past Medical History: Medical Illnesses: Patient reports no history of diabetes, hypertension, thyroid
problems. There is a history of heart disease/cholesterol problems - elevated
cholesterol. There is a history of respiratory problems - occasional asthma. There is
no history of bleeding disorders, stomach or intestinal problems. There is a history
of allergy problem – seasonal. There is no history of diagnoses of kidney problems,
neurological problems, cancer, or other medical diagnoses
Operations: Right knee surgery 1999 – repair lateral cruciate ligament
Medications: Ibuprofen, 400 mg as needed for pain; decongestant X prn allergy;
atorvastatin 10 mg. daily; inhaler Y prn
Social History: The patient does not smoke. He previously smoked ½ pack per day for
one year, stopping at age 19. He drinks 4-5 beers per week. He drinks 2-3 cups of
coffee per day. He is an electrician
Family History: There is no family history of hearing loss, diabetes, or bleeding
disorders. His father had high cholesterol and died of a heart attack. His mother has
spring and fall allergies. His mother had breast cancer, cured with surgery and
radiation. His mother reports nausea following general anesthesia

Date____/____/____
Patient Name: Account No. DOB: ____/____/____
Patient Medical History Form (p. 2): Please provide the following medical information to the best of your ability:
Review of Systems:
1) Please check the "Yes" or "No" box to indicate whether you presently have any of the following symptoms:
2) For any "yes" responses, please check the "current" box if this symptom relates to the reason for your visit today
Yes No Current Yes No Current
GENERAL chills ������������ �������� weight loss or gain ������������ ��������
fatigue ������������ �������� daytime sleepiness ������������ ��������
ALLERGY environmental allergy ������������ �������� sneezing fits ������������ ��������
post-nasal drip ������������ ��������
NEURO headache ������������ �������� weakness ������������ ��������
passing out ������������ �������� numbness, tingling ������������ ��������
EYES eye pain / pressure ������������ �������� vision changes ������������ ��������
watery or itchy eyes ������������ ��������
ENT ear pain or itch ������������ �������� ear drainage ������������ ��������
hearing loss ������������ �������� ear noises ������������ ��������
dizziness ������������ �������� lightheadedness ������������ ��������
nasal congestion ������������ �������� sinus pressure or pain ������������ ��������
sense of smell problem ������������ �������� problem snoring, apnea ������������ ��������
hoarseness ������������ �������� throat pain ������������ ��������
throat clearing ������������ �������� throat dryness/itching ������������ ��������
RESPIR. cough ������������ �������� coughing blood ������������ ��������
wheezing ������������ �������� shortness of breath ������������ ��������
CARDIAC chest pain ������������ �������� palpitations ������������ ��������
wake short of breath ������������ �������� ankle swelling ������������ ��������
GI difficulty swallowing ������������ �������� heartburn ������������ ��������
abdominal pain ������������ �������� nausea/vomiting ������������ ��������
bowel irregularity ������������ �������� rectal bleeding ������������ ��������
GU frequent urination ������������ �������� painful urination ������������ ��������
blood in urine ������������ �������� prostate problems ������������ ��������
HEME/LYM swollen glands ������������ �������� sweating at night ������������ ��������
bleeding problems ������������ �������� easy bruising ������������ ��������
ENDO feel warmer than others ������������ �������� feel cooler than others ������������ ��������
MSK joint aches ������������ �������� muscle aches ������������ ��������
SKIN rash ������������ �������� hives ������������ ��������
itching ������������ �������� skin or hair changes ������������ ��������
PSYCH depression ������������ �������� anxiety or panic ������������ ��������
does use QQQ nasal spray prn. The patient reports A.M. nasal congestion; he also has forced air heat in his bedroom (note: I have advised use
of a bedroom humidifier from October thru April). He has occasional mild left frontal pain
GI: Moderate heartburn over the last six months. He also reports occasional throat clearing and post nasal drip sensation.
Resp: Patient reports a long-term history of episodic wheezing, which was significant , approximately six months ago. Pulmonary function testing
in the past has indicated presence of asthma
Snoring: Patient reports loud snoring at night, plus occasional episodes of waking up gasping for breath. He commonly wakes feeling tired and
also has frequent daytime fatigue, despite getting approximately seven hours sleep per night (the patient denies nocturnal medications or alcohol
ingestion). Has not fallen asleep while driving
Weight gain: Patient reports gaining thirty pounds over the last several years.
Reviewed by: XXX
Allergy: History of allergy testing and treatment, both as a child and as an adult. He does not report significant sneezing or ocular symptoms. He
Copyright 2006 by ASA, LLC ENT New Patient Form page 2

7
[SRL: this image should appear on the right-facing page when the book is open]
Review of Systems: General: patient reports gaining 30 pounds over the last several years. He commonly
wakes feeling tired and also has frequent daytime fatigue, despite getting
approximately seven hours sleep per night (the patient denies nocturnal
medications or alcohol ingestion). Has not fallen asleep while driving. He has no
chills
Allergy: patient complains of sneezing fits and post-nasal drip when symptomatic.
History of allergy testing and treatment, both as a child and as an adult. He does not
report significant sneezing or ocular symptoms. He does use QQQ nasal spray prn.
Neuro: there is no history of headache, passing out, weakness, numbness, or tingling
sensations
Eyes: patient has itchy eyes seasonally in the Spring. He denies vision changes or eye
pain/pressure
ENT: The patient notes that his ears itch at times and have small amounts of waxy
drainage. There is no history of tinnitus, dizziness, or lightheadedness. He reports
A.M. nasal congestion; he also has forced air heat in his bedroom (note: I have
advised use of a bedroom humidifier from October thru April). There is occasional
mild left frontal pain. There is no difficulty with the sense of smell. The patient
reports loud snoring at night, plus occasional episodes of waking up gasping for
breath. Patient denies hoarseness or throat pain, but does complain of occasional
throat clearing, post-nasal drip sensation, and throat dryness or itching
Respiratory: Patient reports a long-term history of episodic wheezing, which was
significant approximately six months ago. Pulmonary function testing in the past
has indicated presence of asthma. He has episodes of coughing and shortness of
breath, but no history of coughing blood
Cardiovascular: There is no history of chest pain, palpitations, or ankle swelling
GI: Moderate heartburn over the last six months. There is no history of difficulty
swallowing, abdominal pain, nausea or vomiting, bowel irregularity, or rectal
bleeding
GU: There is no history of frequent urination, painful urination, blood in the urine, or
prostate problems
Heme/Lymph: There is no history of swollen glands, sweating at nigh, bleeding
problems, or easy bruising
Endo: There is no history of feeling warmer than others or feeling cooler than others
Musculoskeletal: The patient has joint aches in his knees. There is no history of
muscle aches
Skin: There is no history of rash, hives, itching, or skin or hair changes
Psych: There is no history of depression or panic/anxiety symptoms

Date____/____/____ Patient States Consultation Requested By__________________________
Patient Name: Account No. DOB: ____/____/____
PRESENT ILLNESS Chronology with: 1. one to three elements [level 2] 2. four to eight elements; OR status of 3 chronic or inactive conditions [level 3, 4 or 5]
(1) duration (2) timing (3) severity; (4) location (5) quality (6) context (7) modifying factors (8) assoc. signs & symptoms
The patient reports both ears feeling intermittently clogged for approximately two weeks; the clogged sensation seems to have increased in the last several
days, with diminished hearing bilaterally and a sense of pressure in the left ear. There is no history of drainage from the ears. Of note, the patient
reports a history of problems with wax, and he cleans his ears with Q-tips on a daily basis.
The patient also reports ear pressure problems in airplanes during landing. He is also concerned that he may have hearing loss related to noise
exposure, since he plays drums in a rock band.
PHYSICAL EXAMINATION: Ear Nose & Throat
GENERAL (at least 3 measurements of vital signs) HT_5_ft_7__in WT__205___lbs
BP sitting-standing _124_/_78 mm Hg BP supine____/____mm Hg
PULSE _68__/min regular - irregular RESP _16_/min TEMP ______o (F-C)
Normal/AB Normal/AB
GENERAL APPEARANCE Stature, nutrition ������������ NECK MASSES & TRACHEA Symmetry, masses ������������
COMMUNICATION & VOICE Pitch, clarity ������������ THYROID Size, nodules ������������
HEAD/ INSPECTION Lesions, masses ������������ EYES OCULAR MOTILITY & GAZE EOMs, nystagmus ������������
FACE PALPATION / PERCUSSION Skeleton, sinuses ������������ RESP. RESPIRATORY EFFORT Inspiratory-expiratory ������������
SALIVARY GLANDS Masses, tenderness ������������ AUSCULTATION Lung sounds ������������
FACIAL STRENGTH Symmetry ������������ CVS HEART AUSCULTATION rhythm, heart sounds ������������
ENT PNEUMO-OTOSCOPY EACs; TMs mobile ������������ PERIPH VASC SYSTEM Edema, color ������������
HEARING ASSESSMENT Gross; Weber/Rinne ������������ LYMPH. NECK/AXILLAE/GROIN/ETC. Adenopathy ������������
EXTERNAL EAR & NOSE Appearance ������������ NEURO/ CRANIAL NERVES II - XII ������������
INTERNAL NOSE Mucosa, turbinates ������������ PSYCH. ORIENTATION Person, place, time ������������
*AFTER DECONGESTANT Septum, OMCs ������������ MOOD & AFFECT Comments ������������
LIPS,TEETH & GUMS Mucosa, dentition ������������ ������������
ORAL CAVITY, OROPHARYNX Mucosa, tonsils, palate ������������ ������������
HYPOPHARYNX Mucosa, pyriforms ����NV���� ������������
LARYNX (mirror: adults) Anatomy, vocal cord mobility ����NV���� ���� See attached dictation
NASOPHAR. (mirror: adults) Mucosa, choanae ����NV����
Hypopharynx, larynx, and nasopharyx not visualized due to 4+ hyperactive gag reflex
Ears: Impacted cerumen was cleaned from the left external auditory canal, revealing mild thickening of the posterior portion of the TM and mild positive
pressure on pneumo-otoscopy (note: the patient was performing Valsalva maneuvers prior to the examination). The right tympanic membrane has normal
appearance and mobility. Weber is midline; air conduction is greater than bone conduction bilaterally.
Nose: Mild inferior turbinate congestion bilaterally. Following spray, there is a mild septal deviation high to the right, and there is a large
middle meatal polyp visible on the left.
Mouth: Enlarged soft palate and uvula
1. problem focused = 1-5 elements [level 1] 2. expanded = 6-11 elements [level 2] 3. detailed = 12 or more elements [level 3]
4. comprehensive = document every element in basic areas AND at least 1 element in each optional area [level 4 or 5] *optional
*PAST POINTING
*ROMBERG
*TANDEM ROMBERG
Copyright 2006 by ASA, LLC ENT New Patient Form page 3

9
J.6 History of Present Illness and Physical Examination: transcription model
History of Present Illness: The patient reports both ears feeling intermittently clogged for
approximately two weeks; the clogged sensation seems to have increased in the last several
days, with diminished hearing bilaterally and a sense of pressure in the left ear. There is no
history of drainage from the ears. Of note, the patient reports a history of problems with wax,
and he cleans his ears with Q-tips on a daily basis. The patient also reports ear pressure
problems in airplanes during landing. He is also concerned that he may have hearing loss
related to noise exposure, since he plays drums in a rock band.
Physical Examination: General:
Vital Signs: Height 5 foot 7 inches; weight 205 pounds; pulse 68; blood pressure 124/78
General appearance: normal stature and appearance
Communication and voice: normal pitch and clarity
Head/Face:
Inspection: no lesions or masses
Palpation / percussion: normal skeleton and sinus palpation
Salivary glands: normal without masses or tenderness
Facial strength: normal symmetry
ENT:
Pneumo-otoscopy: Impacted cerumen was cleaned from the left external auditory canal,
revealing mild thickening of the posterior portion of the TM and mild positive pressure
on pneumo-otoscopy (note: the patient was performing Valsalva maneuvers prior to the
examination). The right tympanic membrane has normal appearance and mobility.
Hearing assessment: grossly normal; Weber is midline; air conduction is greater than bone
conduction bilaterally
External ear and nose: normal appearance
Internal nose: Mild inferior turbinate congestion bilaterally. Following spray, there is a
mild septal deviation high to the right, and there is a large middle meatal polyp visible
on the left
Lips, teeth, and gums: normal mucosa and dentition
Oral cavity, oropharynx: Enlarged soft palate and uvula
Hypopharynx (mirror exam): not visualized due to 4+ hyperactive gag reflex
Larynx (mirror exam): not visualized due to 4+ hyperactive gag reflex
Nasopharynx (mirror exam): not visualized due to 4+ hyperactive gag reflex
Neck:
Masses and trachea: normal symmetry and absence of masses
Thyroid: normal size and absence of nodules
Eyes:
Ocular motility and gaze: normal extra-ocular movements, no nystagmus
Respiratory:
Respiratory effort: normal inspiratory and expiratory effort
Cardiovascular:
Peripheral vascular system: no edema, normal color
Lymphatic:
Neck: no adenopathy
Neuro/psych:
Cranial nerves: normal nerves 2 – 12
Mood and affect: normal comments

Date____/____/____
Patient Name: Account No. DOB: ____/____/____
MEDICAL DECISION MAKING 2 of the 3 sections (a vs a' vs a", b vs b', c vs c' vs c") must meet or exceed indicated level of care
DATA REVIEWED (a): 1. Minimal (level 2) 2. Limited (level 3) 3. Moderate (level 4) 4. Extensive (level 5)
Audio Bilateral symmetrical sloping sensori-neural hearing loss (compatible with history of noise exposure)
Tympanometry Type A bilaterally
IMPRESSIONS / DIFFERENTIAL DIAGNOSES (b): PLANS / MANAGEMENT OPTIONS (b')
1. Minimal (level 2) 2. Limited (level 3) 3. Multiple (level 4) 4. Extensive (level 5)
1) Cerumen impaction left ear Cleaned; D/C Q-tips
2) High frequency sensori-neural hearing loss, likely secondary to noise exp. Consider hearing aid evaluation
3) History of barotrauma with flights Use ventilating ear plus with flights
4) Obstructive sleep apnea with snoring, nocturnal waking, daytime fatigue
5) Laryngo-pharyngeal reflux Proton pump inhibitor, elevate HOB, diet modification
6) Chronic polypoid rhinosinusitis with left middle meatal polyp Steroid nasal spray
7) History of allergic rhinitis
8) History of asthma
DATA ORDERED (a'): 1. Minimal or none (level 2) 2. Limited (level 3) 3. Moderate (level 4) 4. Extensive (level 5)
���� Audiological �������� ENG ���� ABR ���� Allergy evaluation ���� MRI / CT
1) Sleep study
2) Return 2 weeks for fiberoptic examination of larynx and pharynx
3) Future evaluation for extent of sinus pathology
Information Sheets Given: ���� Ear Care ���� Balance ����Hearing ���� Vestib Exercises ���� Throat eval ���� Gerd F/U ���� Voice
���� Nose&Sinus ���� Nose Care ���� URI info ���� Childhood Airway Obstrct ���� GERD ���� APNEA
COMPLEXITY OF DATA REVIEWED OR ORDERED (a")
1. Minimal (level 2) 2. Low (level 3) 3. Moderate (level 4) 4. Extensive (level 5)
���� min ���� limited ���� mod ���� extensive
RISK OF COMPLICATIONS &/OR MORBIDITY OR MORTALITY (see examples in Table of Risk)
1. Minimal (level 2) 2. Low (level 3) 3. Moderate (level 4) 4. High (level 5)
risk of presenting problem(s) (c): ���� min ���� low ���� mod ���� high
risk of diagnostic procedure(s) ordered or reviewed (c'): ���� min ���� low ���� mod ���� high
risk of management option(s) selected (c"): ���� min ���� low ���� mod ���� high
NATURE OF PRESENTING PROBLEM(S)
���� 1. minor (level 1) Problem runs definite and prescribed course, is transient in nature, and is not likely to permanently
alter health status; OR, has a good prognosis with management and compliance.
���� 2. low (level 1) Problem where the risk of morbidity without treatment is low; there is little to no risk of mortality
without treatment; full recovery without functional impairment is expected.
���� 3.low - mod (level 2) Problem where the risk of morbidity without treatment is low to moderate; there is low to moderate
risk of mortality without treatment; full recovery without functional impairment is expected
in most cases, with low probability of prolonged functional impairment
���� 4. moderate (level 3) Problem where the risk of morbidity without treatment is moderate; there is moderate risk of
mortality without treatment; prognosis is uncertain, or there is an increased probability
of prolonged functional impairment.
���� 5. mod - high (level 4,5) (level 4,5) Problem where the risk of morbidity without treatment is moderate to high; there is moderate risk
of mortality without treatment; uncertain prognosis or increased probability of
prolonged functional impairment
���� 6. high (level 4,5) Problem where the risk of morbidity without treatment is high to extreme; there is moderate to
high risk of mortality without treatment, or high probability of severe prolonged
functional impairment.
Complete this section only if documented below >50% of visit time involved counseling and/or coordinating care.
TIME: _____________ minutes ���� > 50% of visit time involved counseling and/or coordination of care
Clinician's signature: XXX
Copyright 2006 by ASA, LLC ENT New Patient Form page 4

11
J.8 Medical Decision Making: transcription model
Data reviewed:
Audiometry: Bilateral symmetrical sloping sensori-neural hearing loss (compatible
with history of noise exposure)
Tympanometry: Type A bilaterally
Impressions:
1) Cerumen impaction left ear
2) High frequency sensori-neural hearing loss, likely secondary to noise exp.
3) Obstructive sleep apnea with snoring, nocturnal waking, daytime fatigue
4) History of barotrauma with flights
5) Laryngo-pharyngeal reflux
6) Chronic polypoid rhinosinusitis with left middle meatal polyp
7) History of allergic rhinitis
8) History of asthma
Plans / Management Options / Data Ordered:
1) Cerumen cleaned; counseled patient on aural hygiene (including discontinuation of
use of Q-tips)
2) Consider hearing aid evaluation
3) Use ventilating ear plugs with flights
4) Overnight sleep study
5) Proton pump inhibitor, elevate HOB, diet modification
6) Steroid nasal spray
7) Return to office in two weeks for fiberoptic flexible laryngoscopy to assess larynx
and hypopharynx
8) Sinus assessment in the future (including radiographs, nasal endoscopy)
{Note: this presentation fails to provide documentation of complexity of data reviewed
and ordered, the risk of the presenting problems, the risk of diagnostic procedures
ordered, the risk of management options selected, and the nature of the presenting
problem(s).}

Advanced E/M Coding for EHRs
42 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Notes1 S Levinson, D Grider, R Linker, and S Thurston, “The Perfect Storm,” Medical Economics, (cover article), April 3, 2009, pages 20-21, http://www.modernmedicine.com/modernmedicine/Modern+Medicine+Now/The-problem-with-EHRs-and-coding/ArticleStandard/Article/detail/590411 2 Wendy Vogenitz, “EMR and E/M: Beware of Software’s Potential to Upcode, “ Part B News, May 01, 2006 Volume 20, Issue 183 Trailblazer Medicare Carrier’s Bulletin, Sept. 30, 20024 Eugene J. Winter, M.D., Medical Director for First Coast Service Options, Inc., 2007
www.hscj.ufl.edu/medicine/pbc/docs/medical_director_article.pdf (see page 3 of article)
5 Office of the National Coordinator for Health Information Technology, U.S. Department of Health and Human Services, “Recommended Requirements for Enhancing Data Quality in Electronic Health Records,” May 2007, page 46 http://www.rti.org/pubs/enhancing_data_quality_in_ehrs.pdf6 CMS Manual System, Pub 100-08 Medicare Program Integrity, Transmittal 438, Change Request 8033, November 9, 2012, http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R438PI.pdf {see replacement document, transmittal 455, http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R455PI.pdf }7 Medicare Claims Processing Manual, Chapter 12, section 30.6.1, http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf8 Medicare Claims Processing Manual, Chapter 12, Section 30.6.1, http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf 9 Levinson, Stephen R., M.D., Practical E/M: Docu-mentation and Coding Solutions for Quality Patient Care, second edition, Chicago: AMA Press, 2008, p. 14110 Ibid, page 141
11 American Medical Association, Current Procedural Terminology (CPT) 2013, Professional Edition, Chi-cago: AMA Press, 2012, page 712 Levinson, Stephen R., M.D., Practical E/M: Docu-mentation and Coding Solutions for Quality Patient Care, second edition, Chicago: AMA Press, 2008, Introduction, page xx13 American Medical Association, Current Procedural Terminology (CPT) 2013, Professional Edition, Chi-cago: AMA Press, 2012, page 814 American Medical Association and Health Care Financing Administration, “Documentation Guide-lines for Evaluation and Management Coding,” 1997, page 215 Ibid, page 5 16 Ibid, page 1017 Levinson, Stephen R., M.D., Practical E/M: Docu-mentation and Coding Solutions for Quality Patient Care, AMA Press, 2005 (first edition) and 2008 (second edition)18 American Medical Association and Health Care Financing Administration, “Documentation Guidelines for Evaluation and Management Coding,” 1995, http://www.uthouston.edu/dotAsset/2260096.pdf19 American Medical Association and Health Care Financing Administration, “Documentation Guidelines for Evaluation and Management Coding,” 1997, http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/referenceII.pdf20 Center for Medicare and Medicare Services, “Medicare Learning Network: Evaluation and Management Services Guide,” December 2010, http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/eval_mgmt_serv_guide-ICN006764.pdf 21 Medicare Claims Processing Manual, Chapter 12, Section 30.6.1, http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf

Advanced E/M Coding for EHRs
AdvancedE/MCodingforEHRs www.aapc.com 43
22 Eugene Winter MD, Medical Director First Coast Service Options Inc, “Requirements for the Payment of Medicare Claims-A Selection of Some Important Criteria,” 2007, page 2 “Cloning of Medical Notes,” http://www.cbhc.org/news/wp-content/uploads/2010/07/Session-2002-2.pdf23 S. Levinson, Practical EHR: Electronic Record Solutions for Compliance and Quality Care, Chicago, AMA Press, 2008, Chapter 7, page 99.24 American Medical Association, Current Procedural Terminology (CPT) 2013, Professional Edition, AMA Press, 2012, page 1025 American Medical Association and Health Care Financing Administration, “Documentation Guide-lines for Evaluation and Management Coding,” 1997, page 4726 Dr. William Osler, nhttp://www.brainyquote.com/quotes/authors/w/william_osler.html 27 Ibid28 Ibid29 Dr. Larry Weed, Medicine in Denial, Amazon pub-lishing, 2011, p. 2330 S. Levinson, Practical EHR: Electronic Record Solutions for Compliance and Quality Care, Chicago, AMA Press, 2008, Chapter 7, page 11331 This section is derived, with minor modifications, directly from Appendix F of “Practical E/M: Docu-mentation and Coding Solutions for Quality Patient Care,” second edition, Chicago, AMA Press, 2008, pages 353-363


AdvancedE/MCodingforEHRs www.aapc.com 45
Appendix A
May 3, 2013 Statement by American Medical
The following pages include a statement by American Medical Association (AMA) Chair Steven Stack to a federal hearing on Meaningful Use presented as this workshop was going to press. We provide it as additional information and perspective to this workshop.

46 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
1
StatementAttributabletoStevenJ.Stack,MD,Chair
AmericanMedicalAssociationMay3,2013
OpeningGoodMorning.MynameisStevenStackandIamanemergencyphysicianfromLexington,Kentucky,andtheChairmanoftheAmericanMedicalAssociation.
OnbehalfoftheAMA,Iampleasedtobeheretodiscusstheimpactofelectronichealthrecordsonclinicaldocumentation,codingandbilling.
TheAMAbelievesthathealthITandhealthinformationexchange,donewell,areessentialtooureffortstoadvancethetripleaim–betterhealth,bettercare,andlowercosts.
ThatweareheretodayistestamentbothtothesuccessesandshortcomingsoftheMeaningfulUseProgram.
Inthepositive,MeaningfulUsehasspurredrapidadoptionofhealthIT.Withouttheincentivesprovidedandcollaborationsfosteredbythisprogram,itisunlikelyourhealthsystemwouldbeadoptingthesenecessarytoolsasrapidlyasitisnow.
Therehavealsobeenundesiredconsequences.Attemptingtotransformtheentirehealthsysteminsucharapidandproscriptivemannerhascompelledproviderstopurchasetoolsnotyetoptimizedtotheend‐user’sneedsandthatoftenimpede,ratherthanenable,efficientclinicalcare.
Forthesereasons,andasageneralobservation,theAMAisgratefulthatStage3rulemakinghasbeenpostponedtoallowhealthcareprovidersandEHRvendorsmuchneededtimetoworktogethertoaddresstheseshortcomings.Additionally,webelievethatmoreflexibilityisneededforproviderstomeetStage2MeaningfulUserequirementsinordertobetteraccommodatethediversityofclinicalsettingsandvariationinworkflows.
Otherpresenterstodayarediscussingtheimpactsoftheincreasingprevalenceofdisease,therapidevolutioninnewtechnologies,andinterventionsthatenableustohelppatientsnowfarmorethaneverbefore.Hopingtocomplimentratherthan

AdvancedE/MCodingforEHRs www.aapc.com 47
2
reiteratetheirpoints,Ihavechosentoshareperspectivesonhowphysiciansdocumentclinicalencounters,theimpactofEHRsonthisdocumentation,andcommonfrustrationsassociatedwiththeEHRs.
Physicians,Technology,andEHRs
Tobegin,Inotethatphysiciansareprolifictechnologyadopters.Theyquicklyincorporateandmakeuseofallsortsofnewpatientmonitoringdevices,diagnosticimagingequipment,advancedsurgicaltools,andinnovativemedications.Incentiveprogramsandmandateshavenotbeennecessaryforphysicianstovoluntarilyembracethesetechnologiesthathaveimprovedtheirpatientcareandefficiency.
EHRs,however,areuniqueinthattheyhaverequiredadedicatedfederalstimulusprogramtocompeltheiruptakebythehealthcarecommunityatlarge.Thishasbeennecessary,innosmallpart,becausetheyarestillatanimmaturestageofdevelopment.EHRshavebeenandlargelyremainclunky,confusing,andcomplex.Thoughan18month‐oldchildcanoperateaniPhone,physicianswith7to10yearsofpost‐collegiateeducationarebroughttotheirkneesbytheirEHRs.
WhenanEHRisdeployedinadoctor’sofficeorhospital,physicianproductivitypredictably,consistentlyandmarkedlydeclines.Evenaftermonthsofuse,manyphysiciansareunabletoreturntotheirpre‐EHRlevelofproductivity–thereisasustainednegativeimpactresultinginthephysicianspendingmoretimeonclericaltasksrelatedtotheEHRandlesstimedirectlycaringforpatients.Inaway,itensuresthephysicianpracticesatthebottomofhisdegree.
Itisnosurprise,then,thatarecentsurveybyAmericanEHRPartnersdemonstratescontinuedescalationinphysiciandissatisfactionwiththeirEHRs.Infact,between2010to2012,thepercentageofdoctorswhowouldnotrecommendtheirEHRtoacolleagueincreasedfrom24%to39%andapproximately1/3rdofallsurveyedsaidtheywere“verydissatisfied”withtheirEHRandthatitisbecomingmoredifficulttoreturntopre‐EHRproductivitylevels.Simplystated,manyEHRsarenotfriendlytotheuserandratherthanimprovingphysicianefficiency,theyareawidespreadsourceoffrustration.Clinicaldocumentation,thoughonlyonefacetoftheproblem,isanillustrativeexample.
ClinicalDocumentationInthenowdistantpast,themedicalrecordwasprimarilyatoolusedbyphysicianstorecordtheirfindingsanddecision‐makingprocessfortheirpersonalfuturereferenceandasacommunicationtoolwithotherphysicians.Anidealnoteforaphysician’sneedsmightreadlikethis:

48 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
3
24y/ohealthymale.Slippedoniceandlandedonrighthand.Closed,angulateddistalradiusfracture.Nootherinjuries.SplintnowandtoO.R.ina.m.forORIF.
18y/ohealthyfemale.Feverandexudativepharyngitisfor2days.Examotherwiseunremarkable.Streptest+.Rx.Amoxil
Thesenotesarebrief,direct,andlacksuperfluousdetail.Overtime,however,themedicalrecordhasbecomeprogressivelymoreatoolforcoding,billing,compensation,compliance,andlitigation.Inparticular,tofulfilltherequirementsofprivateandgovernmentpayers,adetailedevaluationandmanagement(E/M)documentationparadigmwascreatedin1995asameanstotranslatethecognitiveworkperformedbyaphysicianintoastandardizedcollectionofdatatoassigneconomicvaluetotheserviceprovided.TheseE/Mguidelines,despiteacknowledgedlimitationsandmultipleeffortstorevisethem,remaininusetodayastheprinciplemeansofdocumentingandcompensatingforindividuallyperformedphysicianwork.BeforeEHRs,physicianscommonlyhand‐wroteordictatedtheirnotes.Theyreliedupontheirownmemoryplusvariousassistivetoolssuchasreferencecards,standardizedforms,andotherclinicalstafftohelpthemtocomplywiththeE/Mguidelines.Ittooktimetodocumentproperlybuteachchartlookeduniqueandthecontentlargelyhadtobecreatedfromscratch.WidespreadadoptionofEHRs,however,incombinationwithaprogressiveshifttowardsteam‐basedcareisagainrapidlyanddramaticallychangingcliniciandocumentation.EHRImpactonClinicalDocumentation
DocumentingafullclinicalencounterinanEHR,fromscratchandasingledatapointatatimecanbepuretorment.Thefullchartdoesn’tfitonthecomputerscreen.Eachelementisselectedbyaseriesofclicks,doubleclicks,oreventripleclicksofamousebutton.Standardizedlanguage,notnecessarilyintuitiveorideal,ispresentedforallitemsbeingdocumented.Hunting,clicking,andscrollingjusttocompleteasimplehistoryandphysicalexamisatediousandtime‐wastingexperience.Typingfree‐text,whilemoreindividualized,takesadditionaltimeandintroducesunstructureddatathatcreatesadditionalissues.
Toaddresstheseglaringinefficiencies,variousshortcutsandtoolsareusedintheEHR.Themostcommonofthesearetemplates,macros,andcut&paste.Noneoftheseareinherentlybadbuteachofthemcanbemisapplied,accidentallyorintentionally.
Templatesarepre‐formattedportionsofachart.Foraphysicalexam,forinstance,theremaybealistof12organsystemseachwithspecificterminologypresented

AdvancedE/MCodingforEHRs www.aapc.com 49
4
withineachorgantodescribenormalorabnormalfindings.Allthewordsarealreadyonthepage,butnothinghasyetbeendocumented.Thephysicianthenchecksboxes,circleswords,orslashesthroughwordstoindicatethepresenceorabsenceofeachdiscreteitem.Thisisusuallydonethroughmouseclicksandscrollingupanddownalonglistofitemsonacomputerscreen.Aslongasthephysiciandocumentsonlythosethingsheactuallydidanddocumentsaccuratelythisresultsinanaccurate,thoughveryhomogenous‐looking,physicalexamrecord.Additionally,templatescanpromptorremindphysicianstocheckordothingstheymightotherwisehaveforgottentodoand,inthismanner,canprovidesomedegreeofclinicaldecisionsupport.Unfortunately,selectingeverysingleitemindividuallytakesafairlylongtimesoaseconddocumentationtoolisoftenusedtostreamlinethisprocess.
Amacroisessentiallyacompletedtemplatewithanswerspreviouslydeterminedandautomaticallyentered.Forthesakeofexample,imaginethataphysicianhasabasicandacomprehensiveexaminationwithspecifiedelementsthatshedoeseachandeverytimeshedoesthattypeofexam.Inthisscenario,shemaypre‐enterthefindingsforbothanormalbasicexamandanormalcomprehensiveexamandsavetheseinasimilarlynamedmacro.Now,eachtimesheperformsoneoftheseexamsandfindsittobenormal,ratherthanre‐recreatingtheentireexamfromscratch,shecanselectandimporthernormalmacrofortherelevantexaminationandtheEHRwillautomaticallypopulatetheexambasedonherpreviouslyenteredselections.Again,aswiththeuseoftheblanktemplate,aslongshehasactuallyperformedtheworkdocumented,theuseofthismacroisanefficientandeffectivemeanstostreamlinethedataentryprocess.Additionally,ifthereareminorvariations,shecanimportthemacroandthenonlyalterthosedatapointsthatdifferforaspecificpatient.
Macroscanbeaproblem,however,whenaphysicianeitherthroughinnocenthumanoversightoractiveintent,importsamacrocontaininginformationthehedidnotactuallyverify.Inthisinstance,extracareandattentionisrequiredbecausethetechnologytoolcanmakeitalarminglyeasytoaccidentallyintroduceinaccurateinformationintothemedicalrecord.
Cut&paste,carryforward,andimportingaredifferingwaystodescribeathirdconceptthatarisesuniquelywithEHRdocumentation.Inthisinstance,theclinicianreusesinformationpreviouslydocumented.Forstaticinformation,thisisalogicalandbeneficialuseoftheEHR.IfMrs.Joneshadherappendixremovedin1977thatdatawillnotchangefortherestofherlife.Additionally,ifshelearnedthatshewasallergictopenicillinin1977whenshehadthatappendectomy,thatinformationwillalsofollowherfortherestofherlife.Solongastheseitemsareaccurate,itmakesgoodsensetocarrythemforwardthroughtheelectronicrecordsoeveryclinicianhasthisinformation.Thereisnovalueaddedbyaclinicianre‐askingallthesequestionsand,infact,thereisriskthatthepatientorphysicianwilloverlooksomeimportanthistoricaldataandanotherwiseavoidableerrorcouldoccur.

50 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
5
Cut&pastebecomesbadandisappropriatelycriticizedas“cloning”whencliniciansreproduceinformationcreatedbythemselvesorotherseitherwithoutattributionorwithoutattentiontoitsaccuracy.Itisnotappropriateforacliniciantocopyanotherprofessional’shistory,verbatim,andpresentitasifhehadobtaineditfromthepatienthimself.Itisoftenappropriate,however,foracliniciantodocumentthatshehasreviewedthenoteofanotherprofessionalandtosummarizethekeyelementsinherownnotewithattributiontoitssource.Makinguseofanotherexample,errorsinchartingremainerrorsinchartingwhetherdoneinanEHRoronpaper.RegardlessofthefrustrationsassociatedwiththeEHRs,physiciansandothercliniciansstillhavetheobligationtoreviewtheirowndocumentationtoensurethattheinformationisaccurate.EHRscanmakethisprocessinfuriatinglydifficultattimes.Evenso,thoughitismaynotbefraud,glaringinaccuraciescreatedbycarryingforwardpriornoteswithobviouserrorsaresimplynotacceptable.
Allthreeoftheaboveconcepts,i.e.templates,macros,andcut&paste,createanotherperilforphysicians.Inlargemeasure,everyclinicianusingthesameEHRwillcreatechartsthatlookremarkablysimilartoeveryotherclinicianusingthatsameEHRsystem.Manyinpayerandcompliancecommunitieshavelongbemoanedtheinconsistenciesandvariationinphysiciandocumentation.Now,EHRshaveshiftedthecriticismtooneofoverwhelminghomogeny.Eveniftheclinicianaccuratelyselectstheindividualdatapointsonatemplate,everysinglechartcontainingthatdocumentationtemplatewilllookessentiallythesameandmakeuseoftheexactsamewords.Inthiscase,itlooksasthougheveryclinicianhasplagiarizedthewordsotherofeveryotherclinician.
Infact,manylargeEHRsenableuserstoaccessthetemplatesandmacroscreatedbyanyuserinthesystem.Ifonephysicianhasaparticularlypithy,erudite,orprecisewayofdescribingacertainfindingorconditionandsavesitasa“favorite,”shemaylaterfindthatherownwordsbegintoappearinthenotescreatedbyotherclinicianswholikedherdescriptionsomuchtheyadopteditthemselves.Imitationis,afterall,thesincerestformofflattery!Again,aslongasthedescriptionaccuratelydescribestheworkdonebythephysicianandtheconditionofthepatienttheyaretreating,thisisnotfraudbutitcertainlyis“cloning.”Sincewearenottalkingaboutacollegethesis,theconceptofplagiarismismootbutwearestillleftwithlotsofclinicalchartsthatalllookremarkablyalike.
Alarmingly,someMedicarecarriershavealreadydisseminatedrulesthatifchartslooktoomuchaliketheywilldenypaymentforthem.Inthisinstance,evenwhencliniciansareappropriatelyusingtheEHR,atoolwithwhichtheyarefrustratedandtheuseofwhichthefederalgovernmenthasmandatedunderthreatoffinancialpenalty,theyarenowbeingaccusedofinappropriatebehavior,beingeconomicallypenalized,andbeinginstructed‘defacto’tore‐engineernon‐value‐addedvariationintotheirclinicalnotes.ThisisanappallingCatch‐22forphysicians.

AdvancedE/MCodingforEHRs www.aapc.com 51
6
AdditionalConsiderationsIwouldberemissifIdidn’talsomentionsomeoftheotherchallengesassociatedwiththeimpactofEHRsonclinicaldocumentation,coding,andbilling:
Governmentandprivatepayersarerequiringmoreandmorespecific
data,qualityreportingelements,andspecializedreportingbecollectedintheEHR.Capturingandenteringallthisdatatakestimeandcanelevatetheintensityofservice.
Becausesomanypeopleandsomanydevicescollectsomuch
information,themedicalrecordisbecomingsolargeandunwieldyastobeindecipherable.Simplepatientencountersnowroutinelygeneratescoresofpagesofdocumentationandcanbenearlyimpossibletoidentifythetrulyimportantdataamidstalltheclutter.
Vendorscreatestandardized,stockEHRproductsfortheirclients.
Attemptingtochangethesestandardizedproductsiseitherrefused,resistedorcomesatsubstantialexpense.Asaresult,mostcliniciansarecompelledtomakeuseofwhatevertheyhavebeenprovided.Thephysiciansknowthereareproblemsbutarepowerlesstofixthem.
Becauseeveryentryistimedandallentriesandordersendureinthe
EHR,itcanbenearlyimpossibletoactuallyunderstandwhatreallyhappenedandwhy.Canceledordersshowupalongwithexecutedorders.Ifanorderisenteredincorrectly,canceled,andre‐enteredcorrectly,thereare3separateordersdisplayedforalltheseactionsratherthansimplywhatwasfinallydoneforthepatient.
Temporal,ortime‐based,chartingalsocreatesaconfusingmorassof
documentationthatgivesafalseimpressionofhowthecareandworkwasactuallydone.Iwon’texplorethistopicatlengthtoday,butsomeverybizarredescriptionsofEHR“time‐warp”havebeenelsewheredescribed.
Inlightofallthesechallenges,itisevenmoreunsettlingthatONCrecentlyannouncedthatithasrevokedthecertificationoftwoEHRsystemsandsaidthatproviderscannotusethoseEHRstosatisfymeaningfuluserequirements.Whatabouttheproviderswhoalreadypurchasedthosecertifiedsystems?Whatprotectionisthisforthem?WillONCreimbursethemthecostoftheirpreviouslycertified,nowde‐certifiedEHR?Thissortofperiltoprovidersandindividualclinicianswhootherwisefollowedalltherulestheyweregivenishorriblyunfair.

52 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
7
MypurposeingivingtheseexamplesisnotdenigrateEHRs.IreiteratethattheAMAandmostphysiciansbelievethat,donewell,EHRshavethepotentialtoimprovepatientcare.Atpresent,however,theseEHRspresentsubstantialchallengestothephysiciansandothercliniciansnowrequiredtousethem.Underthesecircumstances,itiscertainlynotreasonabletobeoverlycriticalofphysiciansforstrugglingtocomplywiththeinadequaciesofmandatedEHRadoption,particularlywhenthephysiciancommunityhasvocallyandrepeatedlyraisedmanyoftheseconcernsfromtheverystart.ConclusionTheAMAoffersthefollowingsuggestionstoaddresstheconcernsidentifiedabove:
ONCshouldimmediatelyaddressEHRusabilityconcernsraisedbyphysiciansandtakepromptactiontoaddusabilitycriteriatotheEHRcertificationprocess.
CMSshouldprovideclearanddirectguidancetophysiciansconcerningthepermissibleuseofEHRclinicaldocumentationforthepurposesofcodingandbilling.Giventheexamplesdescribedabove,thecreationofthisguidanceclearlyrequiresactivedialoguewiththephysiciancommunitysoasnottofurtherhinderpatientcareorfurthererodephysicianproductivity.
Stage2oftheMeaningfulUseprogramshouldbereconsideredtoallowmore
flexibilitytoproviderstomeettheserequirementswhiletheEHRsarebetteradaptedtoaccommodatethediversityofclinicalsettingsandappropriatevariationinworkflows.
IagainthankyoufortakingthetimetocarefullyconsidertheimpactofEHRsonclinicaldocumentation,codingandbilling.OnbehalfoftheAMA,welookforwardtoworkingwithyoutorealizethefullpotentialofEHRstoadvancethetripleaimofbetterhealth,bettercare,andlowercost.

AdvancedE/MCodingforEHRs www.aapc.com 53
Presentation
Advanced E/M Coding for EHRs
Stephen R. Levinson, MD, CHCA www.PracticalEM.com
• This presentation is designed to provide accurate and authoritative information in regard to the subject matter covered
• The information includes both reporting and interpretation of materials in various publications, as well as interpretation of policies of various organizations. This information is subject to individual interpretation and to changes over time
• Author has personal interests in consulting, presenting, writing about, and developing software in order to help physicians achieve compliant medical records and to help them facilitate quality patient care
General Disclaimer

54 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• Proactive approach to EHRs – We need & want EHRs, but only high quality EHRs – Must be ‘operable as well as interoperable’
• Usable, e�cient, E/M compliant, trustworthy, and assist in promoting high quality patient care
• About a lot of things, but #1 is quality healthcare! – For us as patients – Care MDs should want to provide
Overview
• The workshop o�ers the author’s in depth analysis, of compliance and quality care issues encountered with EHRs – Analyses are based on sanctioned primary & secondary compliance resources wherever possible
(i.e., AMA & CMS) – When 1o or 2o resources not available for speci�c topics, author’s personal assessment will be
labeled (ask if uncertain) – Describes an optimal approach for coders, including advocating for 1) correction (or work-
arounds) of �awed EHR designs, & 2) enhanced clinician E/M education - during training as well as for EHR utilization
• Workshop attendees are encouraged to: – Critically evaluate these analyses and the potential solutions discussed – Share your thoughts and/or concerns during the workshop – Add these approaches to your “tool kit” for E/M documentation and coding. Apply them as you
judge to be indicated & appropriate!
Workshop Philosophy

AdvancedE/MCodingforEHRs www.aapc.com 55
Presentation
• E/M Coding? E/M auditing? • Outpatient? Inpatient? • Workplace Context? – Medical practice – Hospital / academic center – Medicare or insurer – Consultant
Attendee Demographics
• Coding standard (& tools) you currently use? – CPT® compliant (CPT & Doc Guidelines) – Marsh�eld tool (“score sheet”) – Trailblazer tool – Other
• Practice currently working with an EHR? • Practice currently evaluating EHRs?
Attendee Demographics

56 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• EHRs with compliant E/M ? – That actively consider medical necessity? – Is it possible to have a compliant coding engine if it doesn’t consider
medical necessity???
• Physicians’ response to their EHR? – Divorced – Living together in misery – Happy fast and non-compliant – Other
Attendee Demographics (For those currently working with EHRs)
Missing E/M features you would like to have added
1) 2)
What are YOUR Burning EHR Issues?
EHR features you would like �xed or turned o�
1) 2) 3)

AdvancedE/MCodingforEHRs www.aapc.com 57
Presentation
Current EHR Landscape - 1: the Promised Positives & Incentives
• Interconnectivity * • Interoperability * • Clinical decision support
– Preventive care services – Care protocols for diagnosed conditions
• Data mining • PQRI reporting • Health information exchange *
* = not yet standard with EHRs
Electronic Health Records Needed To Bene�t Health Care
(The marketing case) • Access to patient info. • Increased Patient Safety ** • Increased Quality Care ** • Eliminate duplicate tests and services ** • Cost savings to health system **
** = No evidence to support & no valid trials

58 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• HiTECH legislation • ARRA /CMS incentives for Meaningful Use – $44,000 per MD over �ve years – (about $35 per day; = one 99212; = 8 minutes per day)
• CMS penalties for non-use – 1-2% reduction in Medicare payments starting in 2016
(approx. $500/yr per MD)
Huge Demand for EHRs Today
Current EHR Landscape 2: the Undesired Consequences

AdvancedE/MCodingforEHRs www.aapc.com 59
Presentation
Certi�cation Includes No Criteria for Software to be E/M Compliant
• “We will review the extent of potentially inappropriate payments for E&M services…. Medicare contractors have noted an increased frequency of medical records with identical documentation across services.
• We will also review multiple E&M services for the same providers and bene�ciaries to identify electronic health records (EHR) documentation practices associated with potentially improper payments.” – http://oig.hhs.gov/publications/workplan/2011/FY11_WorkPlan-All.pdf
2011-2013 OIG Work Plans
See Section 2 of workbook for selected government EHR concerns

60 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• May: OIG repts 48% for E/M 2001-2010 – Especially F/U o�ce, F/U hospital, & E.D.
• 9/17, Wall Street Journal: “EHR savings little more than hype” – “Software generally clunky, frustrating, user-unfriendly”
• 9/17, Center for Public Integrity: upcoding by docs and hospitals – Getting worse “with proliferation of EMRs, which critics say
can facilitate abuse”
Electronic Health Records Ups & Downs On the HOT SEAT!
• 9/21, NY Times: MC bills rise w Elect Records – OIG warned that E/M “vulnerable to fraud & abuse” – “move to elect records may billions in higher billing, whether or not they provide
additional care”
• 9/25, NY Times: Abuse of EHRs – Obama admin warns against fraudulent use of EHRs to in�ate billings to Medicare (Atty
General Holder & HHS Secretary Sibelius) • {Author’s note: reviews show that overbilling is not as much the result of “fraudulent
use” as it is the result of using intrinsically non-compliant systems as they are designed to be used
Electronic Health Records Ups & Downs On the HOT SEAT!

AdvancedE/MCodingforEHRs www.aapc.com 61
Presentation
• 10/4 NY Times: Lawmakers urge halt on MU payments – Hold payments until clearly de�ne (and achieve) interoperability standards
• 9/25, NY Times: EHR Ups & Downs – A MAC (NGS) says will deny payment for treatments using “cloned
documentation” (EHRs) rather than individualized notes…to show medical necessity” – ** “Dr. Monteith said electronic systems were ‘disrupting traditional medical records
and, beyond that, how we think – the process of arriving at a diagnosis”
See Section 1 of workbook for details of these articles
Electronic Health Records Ups & Downs On the HOT SEAT!
Physicians Feel Trapped in a Vice
Decreasing net income Reporting demands
Decreasing time for care
oversight MACs, RACs, CERT, ZPICs Inadequate doc. tools
No compl. training
Non-funded mandates
doc. requirement

62 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
Setting the Table: Sources of EHR Challenges
• Physicians expect EHR developers to create programs with compliant documentation and coding of E/M services
• There are no certi�cation criteria mandating that EHR software programs meet these E/M compliance standards
Why is the EHR Environment So Challenging?

AdvancedE/MCodingforEHRs www.aapc.com 63
Presentation
• EHR developers expect clinicians to be e�ectively trained in the principles of E/M compliance and in the use of compliant medical record tools
• There are no standards established by the American Association of Medical Colleges (AAMC), residency training guidelines, or CMS mandating that physician training institutions meet these E/M compliance standards
Why is the EHR Environment So Challenging?
• Absence of compliance training during medical education – (it is therefore a “foreign language”)
• Absence of usable, e�cient, compliant documentation forms that promote compliant care and documentation – (it is therefore not possible to complete the intended task in
the time available) • Loss of physician role models in training for
comprehensive care and documentation – Mentors are no longer doing comprehensive H&Ps or
monitoring the documentation of students & residents
Why is E/M So Challenging for Physicians?

64 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• Most EHRs have incorporated the ‘scoring sheet’ as an automated coding engine – Facilitates code levels with documentation volume
• Most programmers build their screens on ful�lling needs of coding engines, so screens guide incomplete & non-compliant documentation
• Most EHRs compound problems by providing data entry shortcuts for “fast” documentation
• Most coders are using incomplete coding tools, making it di�cult to identify EHR documentation shortcomings
Why is EHR Coding So Challenging for Coders?
Where Does CPT’s E/M System Come From?

AdvancedE/MCodingforEHRs www.aapc.com 65
Presentation
• E/M is based on the standard reference text used to teach physicians the optimal approach to diagnosis & care
E/M Compliance is about Quality Care, Data Integrity
“Bates Guide to the H&P” • 7 Elements of the HPI: p. 3
– 8th: “timing” incl. “duration”
• 16 ROS Systems: p. 5–8 • PFSH: p. 4–5 • Physical Exam: p. 9 • MDM: p. 36–38
– Data review, Dx, plans
• Nature of Patient’s Problem: p. 37 – When to consider NPP: p. 36
E/M is Based on Bates’ Guide to the H&P “CPT & 1997 Doc. Guidelines” • 8 Elements of the HPI: p. 7 • 14 Systems of the ROS: p. 8
– Combines M&F GU, skin/breast
• PFSH: p. 9 • Physical Exam: p. 13-16 • MDM: p. 43
– Data review, Dx, plans, risks
• Nature of Presenting Problem: CPT p. 2-3 – When to consider NPP: Practical E/M, p. 119

66 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• CPT’s E/M Section & Doc. Guidelines match concept for concept with “Bates Guide to the Physical Exam and Medical History”
• Therefore E/M is not just a coding system. It can be used as a blueprint for medical record forms or screens that guide and facilitate quality patient care
• When done well, this approach also incorporates requirements for usability & e�ciency
E/M is Based on Bates’ Guide to the H&P
High Quality H&P Presents a Three-Sided Bene�t for Clinicians
• Ful�lls Compliance Needs • Promotes Quality Care • Provides Liability Protection
E/M Compliance is the key to unlocking this inter-relationship

AdvancedE/MCodingforEHRs www.aapc.com 67
Presentation
• “Medical necessity of a service is the overarching criterion for payment in addition to the individual requirements of a CPT code” – Medicare Claims Processing Manual, Chapter 12, section
30.6.1
• In accordance with the Social Security Law, Medicare will not pay for services that are not medically necessary (Soc.Sec. section 1862)
Medical Necessity: Foundation for Reliable & Authoritative E/M Coding
• Synopsis of the comprehensive de�nition applied in the HMO class action lawsuit settlements: – Health care services that a Physician, exercising prudent clinical judgment, would
provide to a patient for the purpose of evaluating, diagnosing or treating an illness, injury, disease or its symptoms, and that are
– (a) in accord with generally accepted standards of practice*; – (b) clinically appropriate, in terms of type, frequency, extent, site and duration – (c) considered e�ective for the patient’s illness, injury or disease; – (d) not primarily for the convenience of the patient or Physician – (e) {not more costly than an alternative service that is at least as likely to produce
equivalent therapeutic or diagnostic results}
*Medical Necessity De�nition (1)

68 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• “For these purposes, ‘generally accepted standards of medical practice’ means – Standards that are based on credible scienti�c evidence published in peer-reviewed
medical literature generally recognized by the relevant medical community
– Physician Specialty Society recommendations
– The view of Physicians practicing in relevant clinical areas
– And any other relevant factors”
• Preventive care may be Medically Necessary, but coverage for Medically Necessary preventive care is governed by the terms of the applicable Plan Documents”
Medical Necessity De�nition (2)
• Medical History – Chief Complaint; HPI; PFSH; ROS
• Physical Examination • Medical Decision Making (MDM)
– Data reviewed &/or ordered – # of diagnoses &/or treatment options – Risk of problems, tests, treatments
• Nature of the presenting problem (NPP) • Counseling • Coordination of Care • Time
Which of the 7 Elements of E/M Directly Relates to Medical Necessity?

AdvancedE/MCodingforEHRs www.aapc.com 69
Presentation
• Nature of the Presenting Problem is the key to correct coding (see Appendix C of CPT) – It sets the upper limit for level of care which is “medically
necessary” (i.e., “warranted”) – It also RAISES the bar to the level of care that is medically
indicated
The Key Practical E/M Insight: Medical Necessity (NPP)
• Most EHR software replicates physicians’ non-compliant paper records and adds non-compliant data entry shortcuts
• Many physicians using paper records have now mimicked and adopted non-compliant EHR features to increase speed of documentation
The Paper Record

70 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
Questions About Setting the Table?
EHR Analysis: Compliance Features Missing from Most EHRs

AdvancedE/MCodingforEHRs www.aapc.com 71
Presentation
• There are 7 components to E/M, not just 3 • Documentation Guidelines have both qualitative (medical
necessity) & quantitative (counting) guidelines, not just quantitative
• Many E/M coding and auditing challenges result from considering only selective portions of E/M and Documentation Guidelines
**E/M & EHR Coding Postulates – 1 (the E/M Impact)
• Clinicians’ EHR documentation challenges result from EHRs that have hard-wired quantitative portions of E/M and Documentation Guidelines into data entry screens and into automated coding engines – And selectively left out most of the qualitative portions
• Most EHRs compound this challenge with non-compliant automated data entry shortcuts that result in “cloned” pseudo-documentation
**E/M & EHR Coding Postulates – 2 (the EHR Impact)

72 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• EHRs’ selective misinterpretations of E/M guidelines and automated data entry shortcuts have cascaded down to the clinical care level
• This often results in disrupting and corrupting not only clinicians’ documentation, but also their diagnostic process
**E/M & EHR Coding Postulates – 3 (the Clinical Care Impact)
• Even the most experienced E/M coders are challenged to achieve reliable & trustworthy coding if using incomplete &/or non-compliant coding tools
• Most coders work with incomplete &/or non-compliant coding tools (e.g., “score sheet”)
• Using fully compliant E/M coding tools empowers reliable & trustworthy coding
**E/M & EHR Coding Postulates – 4 (Impact on Coders)

AdvancedE/MCodingforEHRs www.aapc.com 73
Presentation
Missing E/M features you would like to have added
1) Consideration of medical necessity for determining appropriate levels of care, documentation, & coding
2) Documentation of qualitative E/M features as well as quantitative
Source of EHR Documentation & Coding Issues
EHR features you would like �xed or turned o�
1) Automated data entry shortcuts that create “cloned” pseudo-documents
2) Incomplete and non-compliant coding engines
3) Billing codes used in MDM for indicating clinical diagnoses
• Medical History – Chief Complaint; HPI; PFSH; ROS
• Physical Examination • Medical Decision Making (MDM)
– Data reviewed &/or ordered – # of diagnoses &/or treatment options – Risk of problems, tests, treatments
• Nature of the presenting problem (E/M’s measure of medical necessity) • Counseling • Coordination of Care • Time
Participants: Prioritize the 3 Groups of E/M Components that Can Set Level of Care

74 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• Medical History – Chief Complaint; HPI; PFSH; ROS
• Physical Examination • Medical Decision Making (MDM)
– Data reviewed &/or ordered – # of diagnoses &/or treatment options – Risk of problems, tests, treatments
• Nature of the presenting problem (E/M’s measure of medical necessity) • Counseling • Coordination of Care • Time
Re-Prioritize the 3 Groups of E/M Components that Can Set Level of Care
• Therefore, while the overwhelming focus for physicians and for EHR programs has been on the three “key components,”
• The level of care determined by the key components is subordinate to: – The level of care warranted by Medical Necessity – The level of care indicated by time of counseling and coordination of
care, when circumstances are appropriately documented
Prioritizing the E/M Components

AdvancedE/MCodingforEHRs www.aapc.com 75
Presentation
Missing E/M features you would like to have added
1) Consideration of medical necessity for determining appropriate levels of care, documentation, & coding
2) Documentation of qualitative E/M features as well as quantitative
Source of EHR Documentation & Coding Issues EHR features you would like �xed or
turned o� 1) Automated data entry shortcuts
that create “cloned” pseudo-documents
2) Incomplete and non-compliant coding engines
3) Billing codes used in MDM for indicating clinical diagnoses
• Programmers work with zeroes and ones
• This allows ease of working with quantitative concepts
• But this also creates barriers in addressing qualitative features
Software Programming Challenges

76 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• Most currently certi�ed EHR systems incorporate the quantitative (i.e., objective or easily counted) guidelines, but leave out some or all of the qualitative (i.e., subjective) guidelines
• This selectivity results in coding gaps, or “loopholes,” that necessarily lead to non-compliant coding and billing practices by clinicians – When they use these systems as designed
Examining the Quantitative & Qualitative Aspects of E/M & Doc. Guidelines
See Section 3 of workbook for details quantitative & qualitative
• The 7 E/M components and types of guidelines: – Some E/M components rely solely on qualitative guidelines – Some E/M components rely on both qualitative & quantitative guidelines – There are no E/M components that rely solely on quantitative guidelines
• For E/M components that rely on both types of guidelines, the documentation must ful�ll qualitative guidelines as an absolute requirement to permit consideration (and “counting”) of the quantitative measures
• E/M components that rely solely on qualitative guidelines have equal importance in code determination with E/M components that rely on both qualitative and quantitative guidelines – In fact, the qualitative NPP is the overarching criterion for coding
• It would be optimal if clinicians documented their qualitative assessments (& if EHRs prompted this) – to facilitate optimal coding and optimal patient care
Foundation Principles of Quantitative & Qualitative Guidelines

AdvancedE/MCodingforEHRs www.aapc.com 77
Presentation
• Describe these aspects for: – PFSH & ROS – CC – HPI – Physical Exam – MDM – Medical Necessity (NPP)
Quantitative & Qualitative Aspects of E/M & Doc. Guidelines?
• DG: at least 1 speci�c item from any of the 3 history areas must be documented for pertinent PFSH
• DG: at least 1 speci�c item from any 2 of 3 history areas for complete PFSH (established patient visit)
• DG: at least 1 speci�c item from each of the 3 history areas for a complete PFSH (new patient visit)
PFSH 1: Quantitative Guidelines:

78 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• DG: PFSH may be recorded by sta� or on a form completed by the patient. – To document that the physician reviewed the information, there must
be a notation supplementing or con�rming the information recorded by others” • * Supplement = details of positives; con�rm = signature for negatives
• * Note: based on both clinical standards of care and logical interpretation of the Documentation Guidelines, it is equally apparent that there must be a notation supplementing (the positive �ndings) when recorded/documented by the physician himself or herself
PFSH 2: Qualitative Guidelines
* Indicates author’s interpretation
• Past history positive for diabetes, thyroid disorder, and obesity. There is no history of hypertension, heart disease, or cancer
• Social history reveals smoking, no alcohol or drugs • Family history positive for diabetes
Exercise: How should we code this PFSH?
• What is the level of PFSH by quantitative DGs? • Have the qualitative DGs been met by documentation? • Should we credit this as a pertinent PFSH, complete PFSH, or no PFSH at all?

AdvancedE/MCodingforEHRs www.aapc.com 79
Presentation
• PFSH section has both quantitative and qualitative DGs • There are no authoritative guidelines to justify addressing just the
quantitative features when qualitative DGs are not documented • If not documented, it wasn’t done, and if qualitative DGs not done, cannot
“count” the quantitative values • There is no PFSH at all
Discussion of PFSH Exercise
Consider the clinical implications of this documentation:
• We (and the M.D.) have no details of the diabetes, thyroid problem, or obesity; we don’t know how much smoking or for how long; we don’t know prevalence or severity of family problems with diabetes
• Would you want this kind of care???
Access your audit tool

80 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• Quantitative E/M measures are evaluated in color-coded sections (in conventional manner)
• Qualitative E/M measures are assessed in the check-box sections – Section 1: Qualitative criteria from Documentation Guidelines – Section 2: Identi�cation of non-compliant data entry shortcuts that
result in “cloned” pseudo-documentation (addressed later)
Using the Compliant E/M Coding Tool
• Fundamental principle: the qualitative criteria must be met as a pre-requisite for “counting” the quantitative – If one or more boxes checked as not meeting qualitative
requirements, coder should judge whether to reduce or to eliminate credit for quantitative work recorded
– This type of reduced credit can be documented by circling the reduced code level numbers on the left side of the sheet and/or circling the reduced level of history on the right column (arrows may be drawn to indicate this linkage)
Using the Compliant E/M Coding Tool

AdvancedE/MCodingforEHRs www.aapc.com 81
Presentation
Page 1: History (initial OP visit) How would you apply coding tool in PFSH example?
• DG: for problem pertinent ROS, “patient's positive responses and pertinent negatives for the system related to the problem should be documented”
• DG: for extended ROS, “patient's positive responses and pertinent negatives for two to nine systems should be documented ”
• DG: for complete ROS, “at least ten organ systems must be reviewed. Those systems with positive or pertinent negative responses must be individually documented”
ROS 1: Quantitative Guidelines:
* Note: concept of documenting all systems with positive & pertinent negative responses is also a qualitative guideline

82 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• DG: ROS may be recorded by sta� or on a form completed by the patient. – To document that the physician reviewed the information, there must
be a notation supplementing or con�rming the information recorded by others” • *Supplement = details of positives; con�rm = signature for negatives
• * Note: based on both clinical standards of care and logical interpretation of the Documentation Guidelines, it is equally apparent that there must be a notation supplementing (the positive �ndings) when recorded/documented by the physician himself or herself
ROS 2: Qualitative Guidelines
• Note: all 14 organ systems reviewed and documented this way
• Is this a problem pertinent, extended, or complete ROS; or no ROS at all?
– Why or why not?
• What is the critical qualitative ROS element that is missing?
Exercise: How should we code this ROS? (note: copied directly from a vendor’s web site)

AdvancedE/MCodingforEHRs www.aapc.com 83
Presentation
Page 1: History (initial OP visit) How would you apply coding tool in this ROS example?
• ROS section has both quantitative and qualitative DGs • There are no authoritative guidelines to justify addressing just the
quantitative features when qualitative DGs are not documented • If not documented, it wasn’t done, and if qualitative DGs not done, cannot
“count” the quantitative values • This is no ROS at all
Discussion of ROS Exercise
Consider the clinical implications of this documentation:
• We (and the M.D.) have no details of the patient’s headaches, cough, sputum production, or abdominal pain
• Any one of these symptoms could indicate a health-endangering or life-threatening condition, but we don’t know! Would you want this kind of care?

84 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• DG: For a brief HPI, “the medical record should describe one to three elements of the present illness”
• DG: For an extended HPI, “the medical record should describe at least four elements of the present illness (HPI), or the status of at least three chronic or inactive conditions”
HPI 1: Quantitative Guidelines:
* Note: concept of “status of” these 3 conditions is also a qualitative guideline
• De�nition in Documentation Guidelines and CPT: • “The HPI is a chronological description of the development of the patient's
present illness from the �rst sign and/or symptom or from the previous encounter to the present. It includes the following elements: location, quality, severity, duration, timing, context, modifying factors, and associated signs and symptoms”
• It is the “chronological description” of the course of the patient’s events that makes an HPI a history! This chronological description is the qualitative guideline for this critically important element of the medical history – Without this qualitative element, this section becomes an elaborate chief
complaint rather than a true history what has transpired during the course of the illness
• For 3 chronic conditions, the qualitative measure is ”status”
HPI 2: Qualitative Guidelines

AdvancedE/MCodingforEHRs www.aapc.com 85
Presentation
• CC: chest pain • Duration: 3 weeks • Timing: intermittent • Severity: moderate • Location: chest • Associated signs & symptoms: no SOB
Exercise: How should we code this HPI?
• What is the level of HPI by quantitative DGs? • Have the qualitative DGs been met by documentation? • Should we credit this as a brief HPI, extended HPI, or no HPI at all? (please vote by show of hands)
Page 1: History (initial OP visit) How would you apply coding tool in this HPI example?

86 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• HPI section has a de�nition that contains both quantitative and qualitative features
• There are no authoritative guidelines to justify addressing just the quantitative features when qualitative features are not documented
• If not documented, it wasn’t done, and if qualitative features not done, cannot “count” the quantitative values
• This is a CC, not an HPI
Discussion of HPI Exercise
Consider the clinical implications of this documentation: • We (and the M.D.) have no details of the patient’s course of the patient’s chest pain, how it began, how it progressed • This list of symptoms could represent cardiac, pulmonary, musculoskeletal, skin (e.g., Shingles), or GI cause • Would you want this kind of care?
• CC: scheduled follow-up visit • HPI: Patient has 3 chronic conditions – hypertension,
obesity, and diabetes. His last Hgb A1C was 6.8%
Exercise: How should we code this HPI?
• What is the level of HPI by quantitative DGs? • Has the qualitative feature (“status of”) been met by documentation? • Should we credit this as a brief HPI, extended HPI, or no HPI at all? (please vote by show of hands)

AdvancedE/MCodingforEHRs www.aapc.com 87
Presentation
Page 1: History (initial OP visit) How would you apply coding tool in this HPI example?
• HPI section has a de�nition that contains both quantitative (# of chronic conditions) and qualitative (status of ) features
• There are no authoritative guidelines to justify addressing just the quantitative features when qualitative features are not documented
• If not documented, it wasn’t done, and if qualitative features not done, cannot “count” the quantitative values
• This does not meet criteria for HPI
Discussion of HPI Exercise
Consider the clinical implications of this documentation:
• We (and the M.D.) have no details of the patient’s course of the patient’s health since the previous visit. Has weight changed? Has she had weakness, fainting, or headaches? Problems with vision or urination? How does she feel?
• Would you want this kind of care?

88 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• 1995 Guidelines • 1997 Guidelines
– General multi-system exam – Single organ system examinations
• Qualitative aspects of exam
Physical Examination Component
• Problem Focused exam involves only “the a�ected body area or organ system”; i.e., 1 organ system
• For a general multi-system Comprehensive examination, the medical record “should include �ndings about eight or more of the 12 organ systems”
• Therefore, by logical deduction, both expanded problem focused and detailed examinations will involve performing and documenting between two and seven organ systems
Exam 1(a): 1995 Quantitative Guidelines:

AdvancedE/MCodingforEHRs www.aapc.com 89
Presentation
• Problem Focused exam is a “limited examination of the a�ected body area or organ system”
• Expanded Problem Focused exam is a “limited examination of the a�ected body area or organ system and other symptomatic or related organ system(s)”
• Detailed exam is an “extended examination of the a�ected body area or organ system and other symptomatic or related organ system(s)”
• Comprehensive exam is a “general multi-system exam or complete examination of a single organ system”
Exam 2(a): 1995 Qualitative Guidelines
• The terms “limited exam” and “extended exam” are not de�ned – These are subjective terms
• How should we audit an extended (but < comprehensive) exam con�ned to a single a�ected organ system?
• Documentation of (all) related organ systems is often incomplete – How should this circumstance be coded?
• Many charts document extended exam of a�ected organ system but only limited examination of some or all of the related organ systems – How should this circumstance be coded?
• For comprehensive exam, the guidelines fail to state whether the >8 organ systems require an extended or a limited exam. However, a comprehensive exam should certainly be more complex than a detailed exam, therefore requiring an extended exam of 8 or more organ systems. – Unfortunately, we frequently �nd charts with limited exams of 8 organ systems where physicians believe they have
performed a comprehensive exam – How should this circumstance be coded?
1995 Qualitative Guidelines, Author’s Notes

90 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• DG: “Speci�c abnormal and relevant negative �ndings of the a�ected or symptomatic body area(s) or organ system(s) should be documented. A notation of ‘abnormal’ without elaboration is insu�cient” – Note: It is common that there is no doc of relevant negatives
• DG: “Abnormal or unexpected �ndings of the examination of any asymptomatic body area(s) or organ system(s) should be described”
• DG: “A brief statement or notation indicating ‘negative’ or ‘normal’ is su�cient to document normal �ndings related to una�ected area(s) or asymptomatic organ system(s)”
Qualitative Exam Requirements (in both ’95 & ’97 Doc Guidelines)
Coding Tool, Page 1: 1995 Exam Guidelines

AdvancedE/MCodingforEHRs www.aapc.com 91
Presentation
• The 1997 Documentation Guidelines provide speci�c examination templates for a general multi-system examination and for eleven di�erent single organ system examinations
• The Guidelines manual lists numbers of examination elements to be performed and documented speci�c for each of these types of examinations in order to ful�ll requirements for Problem Focused, Expanded Problem Focused, Detailed, and Comprehensive examinations
Exam: 1997 Quantitative Guidelines:
• DG: “Speci�c abnormal and **relevant negative �ndings of the a�ected or symptomatic body area(s) or organ system(s) should be documented. A notation of ‘abnormal’ without elaboration is insu�cient” – Note: It is common that there is no doc of relevant negatives
• DG: “Abnormal or unexpected �ndings of the examination of any asymptomatic body area(s) or organ system(s) should be described”
• DG: “A brief statement or notation indicating ‘negative’ or ‘normal’ is su�cient to document normal �ndings related to una�ected area(s) or asymptomatic organ system(s)”
Exam: 1997 Qualitative Guidelines

92 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
Coding Tool, Page 1: 1997 Exam Guidelines
• MDM challenges – Qualitative elements that call for quantitative measures
• Number of diagnoses/management options • Amount of data reviewed or ordered
– Qualitative elements that should be documented, but EHRs do not provide • The three types of risk • Complexity of data ordered or reviewed • Separation documentation sections for data ordered & management
options
Medical Decision Making Component

AdvancedE/MCodingforEHRs www.aapc.com 93
Presentation
• Neither CPT nor either edition of Documentation Guidelines provides quantitative values for the qualitative descriptors for “Number of diagnoses and/or management options”
• AMA publications “Practical E/M” and “Practical EHR" suggest the following quantitative values, and these suggestions were approved for the publication by the AMA’s CPT section
MDM 1: Quantitative Guidelines:
CPT Description Numerical Value
Minimal 1
Limited 2
Multiple 3
Extensive 4 or more
MDM : Quantitative Guidelines: • CPT & Doc Guidelines provide only quantitative values for the qualitative descriptors for “Number of diagnoses and/or management options” • “Practical E/M” and “Practical EHR" suggest the following quantitative values, which were approved for the publication by the AMA’s CPT section.

94 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
CPT Description Numerical Value
Minimal 1
Limited 2
Moderate 3
Extensive 4 or more
MDM : Quantitative Guidelines: • CPT & Doc Guidelines provide only quantitative values for the qualitative descriptors for “Amount of data ordered and/or reviewed” • “Practical E/M” and “Practical EHR" suggest the following quantitative values, which were approved for the publication by the AMA’s CPT section
• Complexity of data is a subjective (qualitative measure) • The Table of Risk: – Doc Guidelines advises “Because the determination of risk
is complex and not readily quanti�able, the table of risk includes common examples rather than absolute measures of risk”
MDM : Qualitative Guidelines:

AdvancedE/MCodingforEHRs www.aapc.com 95
Presentation
• Documentation recommended for the levels of risk: – It is clear that assessment of the three levels of risk is best accomplished by
the clinician at the point of care – However, the Documentation Guidelines fail to suggest that clinicians
should document their professional assessment of these three levels of risk (although it is, after all, a guideline for “documentation”)
– The additional documentation of this qualitative measure through well-designed EHR screens is e�ective for promoting compliant E/M coding and providing audit protection
– In the absence of such clinician documentation, the coder is compelled either to make this determination without clinical guidance or to seek the assistance of an authoritative clinician
MDM Qualitative Notes
Coding Tool, Page 2: MDM

96 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
Compliant Coding Tools for Coders
Primary resources – CPT – Documentation Guidelines
• Secondary sanctioned resources – Core CPT compliance rules – “Practical EHR” – ICD9
Coders’ Compliant Tool Kit for Reviewing EHR Documentation

AdvancedE/MCodingforEHRs www.aapc.com 97
Presentation
Missing E/M features you would like to have added
1) Consideration of medical necessity for determining appropriate levels of care, documentation,& coding
2) Documentation of qualitative E/M features as well as quantitative
Source of EHR Documentation & Coding Issues
EHR features you would like �xed or turned o�
1) Automated data entry shortcuts that create “cloned” pseudo-documents
2) Incomplete and non-compliant coding engines
3) Billing codes used in MDM for indicating clinical diagnoses
• The “Score Sheet” �rst appeared in 1995, along with Documentation Guidelines, as a shortcut tool for coders
• This tool has not been sanctioned by CMS or AMA • This non-sanctioned approach has (unfortunately) been adopted
as the basis for the automated coding engines in most EHRs – Since programmers are inclined to design entry screens to ful�ll the
needs of their coding engines, the compliance shortcomings of the score sheet are the basis for many EHR compliance issues
Critical Analysis of Incomplete and Non-Compliant Tools (Score Sheet)

98 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
Score Sheet: Medical History What is the critical compliance problem?
It is incomplete. There is no consideration of the qualitative E/M history guidelines
Score Sheet: Physical Exam What are the critical compliance problems?
It is incomplete. It includes only the problematic 1995 Guidelines There is no consideration of the qualitative E/M exam guidelines

AdvancedE/MCodingforEHRs www.aapc.com 99
Presentation
MDM: Number of Diagnoses/Managements What are the critical compliance problems?
• Incomplete: – No consideration of
management options – This undervalues a worsening
established problem (e.g. metastatic cancer with symptoms)
• Non-compliant – Counting formula not in DGs – DGs don’t give credit to new
problems – Overvalues mild new problems – Supports level 4 – 5 for all new
pts – Di�erent results than CPT
compliant
EHR Coding Engine: Level 4 for Minor Illness (Screen shot from Vendor Web Site)

100 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• Nature of the Presenting Problem is not considered at all on this non-compliant score sheet
• “Medical Necessity is the overarching criterion for payment” (and coding)
• Is it possible to have a compliant coding engine without consideration of medical necessity?
Score Sheet: Medical Necessity
• Comprehensive history (automated) – New Pt: pre-loaded macro, or doc by exception – Established Pt: copy forward old history
• Detailed or comprehensive exam (automated) – Copy/paste pre-loaded macro, or doc by exception – Or copy forward old exam
• Score Sheet MDM – # diagnoses: 1 new problem = moderate – Moderate Risk on Table of Risk:
• 1 new problem with uncertain prognosis • 2 stable chronic illnesses • **Manage one prescription medication
• Ignore NPP (medical necessity) • Time of visit & doc = 90 seconds
EHR Score Sheet Engines Level 4
Results:
audit = “false claims”;
liability = catastrophe;
quality

AdvancedE/MCodingforEHRs www.aapc.com 101
Presentation
Questions About Score Sheets and EHR Coding Engines?
• Quality E/M coding tools should be: – Comprehensive (include all E/M elements) – Usable – E�cient – Compliant with primary & secondary resources – Trustworthy – E�ective for clinician E/M education
Thoughtful & E�ective Coding Tools to Consider
See Sections 6 & 7 of workbook for analysis coding forms

102 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
Page 1: History (initial OP visit)
Page 1: 1997 Exam Guidelines

AdvancedE/MCodingforEHRs www.aapc.com 103
Presentation
Page 1: 1995 Exam Guidelines
Page 2: MDM

104 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• Challenge #1: Number of diagnoses and/or management options – Count only actively addressed diagnoses – Use minimal = 1, limited = 2, multiple = 3, extensive > 4 – Circle both the # of diagnoses & # of management options – Select level of the higher of these two choices – Notes on counting management options:
• Use of multiple meds to treat 1 or more conditions = only one option – e.g., to treat sinusitis with amoxicillin + decongestant = 1 option
• Must document alternative treatments to count >1 management option – e.g., treat sinusitis with amoxicillin, if not improved, change to Cefzil = 2 – e.g., treatment options for stage 1 localized lymphoma, “discussed surgery,
radiation therapy, chemotherapy, and combination therapy with radiation + chemo = 4
Coding Tool Exercise: Coding the MDM
• Challenge #2: amount of data – Use minimal = 1, limited = 2, moderate = 3, ext > 4
• Challenge #3: complexity of data ordered or reviewed – Not commonly documented by clinician (however, this would be helpful) – Conventional interpretations of data complexity:
• Ordering data requires relatively limited complexity decision making • Reviewing written reports from others is considered minimal or limited
complexity • Physician performing own readings of radiographs and other test results, or
reviewing outside records, usually credited as moderate or extensive complexity
Coding Tool Exercise: Coding the MDM

AdvancedE/MCodingforEHRs www.aapc.com 105
Presentation
• Challenge #4: three levels of risk – Risks of presenting problems, diagnostic procedures ordered, and
management options selected – Based on examples provided in “Table of Risk” – Not commonly documented by clinician (however, this would be
helpful). If questions arise, request MD assistance – Conditions warranting “moderate” level of risk are not uncommonly
encountered
Coding Tool Exercise: Coding the MDM
Page 3: NPP

106 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• Challenge #5: assessing the Nature of the Presenting Problem(s) – De�ned in CPT in terms of relative risks of morbidity or mortality without
treatment, uncertainty of prognosis, or probability of prolonged functional impairment
– In clinical terms, this is commonly described as natural course of an illness (without intervention)
– NPP is not commonly documented by clinician (however, this would be extremely helpful)
– Clinician’s measure of NPP can often be cross-checked by intensity of services ordered and type of follow-up
– If questions arise, request MD assistance for clinical judgment
Coding Tool Exercise: Coding the NPP
Page 4: Time

AdvancedE/MCodingforEHRs www.aapc.com 107
Presentation
99203 99204 99202
• First step: compare documentation to code submitted – Unable to judge if chart is over-coded or under-documented – e.g.: code submitted 99204; history level detailed, exam detailed, MDM low
complexity • 2nd step: consider medical necessity (only) if documentation supports
code submitted (otherwise NPP not addressed) – Medical necessity applied only to show “over-coding” • e.g., : 99214 submitted with detailed history and mod complexity
MDM documented, but patient’s diagnosis is only an acute bladder infection
Conventional Approach to E/M Coding, E/M Audits, and Clinician Education

108 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• First step: compare code submitted to care level warranted by the NPP – Code submitted > warranted by NPP = over coding – Code submitted < warranted by NPP = under coding – Code submitted = warranted by NPP = medically indicated
code • 2nd step: compare documentation to code submitted – Level of documentation < code submitted (and/or
warranted by NPP) = under documentation
Practical E/M Method for E/M Coding, E/M Audits, and Clinician Education
• Basic philosophy of this approach: – Code level driven by clinician’s judgment (of NPP), not by a
“coding game” – Sometimes need a little more care to rule out serious
illness; such e�ort does NOT change the medically indicated level of care!
Practical E/M Method for E/M Coding, E/M Audits, and Clinician Education

AdvancedE/MCodingforEHRs www.aapc.com 109
Presentation
• Is E/M selected (coded) appropriate for severity of NPP?
• Apply “Goldilocks” rule: – Not to high (no overcoding) – Not too low (no undercoding) – Always just right – This resolves question of “overcoding” vs. “under-
documenting” • Note on the coding form whether NPP was
documented by MD or had to be inferred by reviewer • Attendees: apply this approach to �nal page of
coding form
This is E/M Coding by the Goldilocks Principle
• From review on �nal page of audit report, was chart – Undercoded, overcoded, or correctly coded by MD? – Under documented or adequately documented?
• Answers: – Undercoded – Underdocumented
Questions About Compliant Tools for Coders?

110 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
EHR Analysis: Non-Compliant Features You Want Fixed or Turned O�
Note: Incomplete & non-compliant coding engines addressed above
Missing E/M features you would like to have added
1) Consideration of medical necessity for determining appropriate levels of care, documentation, & coding
2) Documentation of qualitative E/M features as well as quantitative
Source of EHR Documentation & Coding Issues
EHR features you would like �xed or turned o�
1) Automated data entry shortcuts that create “cloned” pseudo-documents
2) Incomplete and non-compliant coding engines
3) Billing codes used in MDM for indicating clinical diagnoses

AdvancedE/MCodingforEHRs www.aapc.com 111
Presentation
• Introduced to address the (unacceptable) problems of clinicians being forced to type at point of care
• Challenges of generic pseudo-documentation – Clinical: lack of ability for patient speci�c / visit speci�c documentation
impairs ability for individualized care – Medico-legal: fails to support indications for speci�c care – Compliance: automatic data entry is not individualized & fails to support
medical necessity (i.e., *“automation is not documentation”)
Cloned Documentation
* author’s interpretation; see workbook section 5 page 5
• Templates – Pre-loaded information to be completed – Contains only headings, lists of questions to be asked, or lists of physical
areas to be examined
• Macros – Pre-loaded information to be completed plus pre-loaded default to
negative or normal �ndings – Automatically, or with a single click, loads a completed clinical
document before the patient has even been evaluated
Possible Building Blocks for Structured Records: Templates vs. Macros

112 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
Template Example: Physical Exam (1997, Multi-System)
Macro Example: Physical Exam (1997, Multi-System)

AdvancedE/MCodingforEHRs www.aapc.com 113
Presentation
• Automated and semi-automated documentation tools Generic pick lists – Documentation by exception – Copy forward – Copy/paste
• Pre-loaded generic macros • Copy from other charts
– Translation
Clones: Non-individualized records
• Limited selection list of vocabulary words and phrases, compiled by point and shoot into a pseudo-narrative
• This shortcut data entry tool fails to provide su�cient depth or breadth to encompass individual nuances and variations, which are: – Required for narrative sections – Required to facilitate patient-speci�c & visit-speci�c care
& documentation
Generic Pick Lists

114 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• Pre-�lled graphic forms, or descriptive narratives, that physician is required to erase (if not performed) or change (from negative to positive or from normal to abnormal)
• Note: it takes more time and e�ort to correctly document REAL CARE with this approach than to work from a blank check-box template, free text dictation, or writing
Documentation by Exception
• This ROS macro appears with all the check boxes for “no” responses automatically entered – Either with no action by clinician
– Or with a single click
• In theory, clinician will un-document us asked questions & change to “yes” any positive responses from patient – This rarely happens; usually, the only
changes made relate solely to questions for the organ system related to presenting problem
• What is the critical qualitative ROS element that is missing here?
Example #1: Documentation by Exception Using a Graphic Interface (check boxes)

AdvancedE/MCodingforEHRs www.aapc.com 115
Presentation
• This ROS free text macro appears as a ‘pseudo-dictation, with all supposedly-asked questions automatically entered with “no” responses, without any action by clinician
• In theory, clinician will un-document any usasked questions & remove “no” for any + responses from patient – This rarely happens; usually, the only
changes made relate solely to questions for the organ system related to presenting problem
• What is the critical qualitative ROS element that is missing here?
Example #2: Documentation by Exception Using a Narrative Interface (pseudo-dictation)
• Moving entire blocks of history, exam, and/or MDM forward from one visit to the next
• Sequential charts appear (mostly) word-for-word identical (usually with only several words modi�ed)
• This functionality results in pseudo documentation that conveys a patient’s status from long ago, not what has transpired since last visit
• Clinical consequences: Often leads to attempts at “diagnosis by lab & radiology tests” rather than individualized patient-speci�c and visit-speci�c diagnosis and treatment
Copy Forward

116 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• Moving entire blocks of history, exam, and/or MDM forward from one patient to the next, or from centrally stored macros
• Not reliable, individualized, or compliant for history or exam sections
– Documentation almost always reveals all aspects of history and physical completely normal except for one area related to CC & HPI (how this is created)
– This creates problem-focused care disguised as comprehensive care
Copy/Paste Functionality
• Potential valid uses in MDM section: – Copy laboratory or X-ray results from lab section to data reviewed
section of MDM – Transfer commonly used pre-loaded set of diagnostic tests for a given
symptom or possible diagnosis – Transfer commonly used pre-loaded set of treatments for a given
symptom or possible diagnosis • Recommend the use of at least 2 clicks in all such situations: 1
click to bring up the pre-loaded information for review and possible patient-speci�c modi�cation before 2nd click to insert the modi�ed information into the MDM section
Copy/Paste Functionality

AdvancedE/MCodingforEHRs www.aapc.com 117
Presentation
• Documentation appears in the medical record that supports everything I do (or that I would like to get paid for)..right?
• The danger zones: – History and exam
• Resultant medical records (& the patients) lose their individuality – These records are not-patient speci�c and visit-speci�c!
Macros, copy-paste, & copy forward, documentation by exception
• Every patient tends to look the same…
• Every ROS tends to read the same… – All negative except for system related to
HPI – What question(s) did the MD actually
ask? • Every exam tends to read the same
– All normal except for system related to HPI
• Every visit’s code level tends to be the same (when combined with non-compliant coding engine)
EHR Macros Create Ducks in a Row

118 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
Dilbert’s Analysis of Copy & Paste
• Leads to approaching each patient identically to every other patient in a similar diagnostic category
• Cloned (limited) diagnoses • Cloned evaluations • Cloned treatments • Changes how physicians approach their patients • Linear thinking rather than global or holistic thinking • Physician tends to delegate decisions to the EHR • Charts lose integrity with copied information inappropriate for speci�c
patient or on repeated visits
Quality Care & Liability Dangers of Cloned Documentation

AdvancedE/MCodingforEHRs www.aapc.com 119
Presentation
• Abdomen: soft, nondistended, nontender, no hepatosplenomegaly
• Genital: prostate is nontender, no masses, negative enlargement
EHR Example, Female Patient
• Female genital exam reveals-non tender, no bulging, dimpling or lumps, normal skin and nipples.
• Pap done by GYN
EHR Example, Male Patient

120 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• “Last Tuesday, patient tripped on curb in front of her house and sprained her right ankle”
• According to her chart, she did this right before every visit, for 10 months in a row
EHR Example, Monthly Follow-up Visits
• EHR record of exam of an ENT visit for an 8 year old with possible nasal congestion; otherwise normal child whose actual height is 4 ft 4 inches and who weighs 75 lbs: – “Constitutional: Height 5 ft 9 inches. Weight 180 lbs – Appearance: well developed well nourished; easily responsive
to visual, verbal and tactile stimulation; oriented x 4; well groomed
– Eyes: no arcus senilis (corneal clouding seen in old people)
EHR Example: Inappropriate Information Copied and Pasted

AdvancedE/MCodingforEHRs www.aapc.com 121
Presentation
• Right ear - External auditory canal normal. Tympanic membrane red, injected, brownish-yellow, meniscus level behind the tympanic membrane.
• Left ear - same as the right. ** • Nasal Interior: Septum - deviated to the right 2+ (1-4 Scale). • Turbinates and middle meati - inferior turbinates hypertrophied +3. Middle
turbinates normal Nasal airway obstructed on the right side estimated 30 %. Rhinorrhea - bilateral, moderate, mucoid, yellow.
• Mucosa - pale; congested; no nasal polyps.
EHR Example: Macro with identical information copied for every patient; only changes made all appear as di�erent fonts
• Optimal Paradigm: Good Medical History Guides the development of a di�erential diagnosis
• Automation Paradigm: Diagnosis creates the history – Tentative diagnosis (based on chief complaint) generates insertion of a
pre-loaded non-speci�c history for that diagnosis, leading to a pre-determined work-up and management
Clinical Impact of Automation on the Diagnostic Paradigm

122 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• As a result, the record for every patient with a given (presumed) diagnosis reads similar to record for every other patient with that disease (and 2nd visit reads same as the 1st) – In other words: “GIGO” – “Since we got our EHR, every chart reads vanilla”
• Non-speci�c history is insu�cient for precise and reliable diagnoses
Clinical Impact of Automation on the Diagnostic Paradigm
• Clinical information is collected in an easily read graphic format that would (or would not) pass an audit,
• But it is then automatically converted to a pseudo-narrative format that is confounding and is commonly unable to pass an E/M audit
Observations on Translation

AdvancedE/MCodingforEHRs www.aapc.com 123
Presentation
• Translation document is cumbersome to read and to identify the positive responses (which also are not supplemented)
• This creates the “Where’s Waldo” e�ect
Translation Example (internet)
• Compliance danger is that even compliant graphic documentation appears as if it were a pre-loaded macro with documentation by exception (i.e., “cloned”)
• The “Where’s Waldo” e�ect! • Why would a physician want to transform an easy-to-read and
understand graphic interface into a 1960s style extensive transcription model record that requires more time to read and to understand ?
Observations on Translation

124 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
vs.
• Combining translation with copy/paste: – ROS information collected simply by checking a box labeled with an
organ system (e.g., “GI normal”) – EHR automatically translates this message by copy/pasting a pre-loaded
macro of detailed questions with negative responses that were never documented as being asked or answered
• Similar issues for physical exam of each individual organ system • Potential for false claims!
Recent Observation on Translation

AdvancedE/MCodingforEHRs www.aapc.com 125
Presentation
CMS & OIG Assessments of Cloned Documentation
• 2007 HHS & ONCHIT white paper: “These tools [defaults, templates, copying] can be extremely helpful if used correctly; however, the tools can also open the EHR-S up to fraud or abuse.” * – Note: this comment uses the word “template” to refer to the improper
templates we have labeled as “macros”
– *ONCHIT & HHS, “Recommended Requirements for Enhancing Data Quality in Electronic Health Record Systems,” 2007, page 46 http://www.rti.org/pubs.enhancing_data_quality_in_ehrs.pdf
Publications about Compliance Problems

126 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
“Guidelines should be developed for both vendors and users of EHRs regarding the appropriate use of documentation techniques to ensure complete, accurate, and quality documentation”
Recommendation from the 2007 HHS & ONC White Paper
Medical Economics, April 09 – 4 practices audited after implementing EHRs and using them as
instructed and intended
– Audit failures ranged from 20% to 95% of charts
– Fines ranged from $50,000 to $175,000+ per physician
– “Non-compliant documentation is also a ‘canary in the coal mine’ to report problems with usability, data integrity, quality of care, & liability protection”
“The Perfect Storm” Federal Audits of Practices with EHRs

AdvancedE/MCodingforEHRs www.aapc.com 127
Presentation
• “Stakeholders must structure an environment where: – Physicians receive appropriate training with e�ective and compliant
documentation tools – Software systems should provide only compliant designs and protect against
improper documentation – Government agencies eliminate non-compliant E/M practices in their own
organizations – Government agencies mandate compliant designs in the software systems
they are advocating and promoting”
• “EHRs must be operable as well as interoperable” • “Automation is not Documentation”
Recommendations
• “Cloned documentation does not meet medical necessity requirements for coverage of services rendered due to the lack of speci�c, individual information.
• All documentation in the medical record must be speci�c to the patient and her/his situation at the time of the encounter
• Cloning of documentation is considered a misrepresentation of the medical necessity requirement for coverage of services. Identi�cation of this type of documentation will lead to denial of services for lack of medical necessity and recoupment of all overpayments made.” – Eugene J. Winter, M.D., Medical Director for First Coast Service
Options, Inc., 2007 – http://medicare.fcso.com/Publications_A/2006/138374.pdf
EHRs, Cloned Documents, & Medical Necessity (MAC Analysis)
No Rubber Stamp

128 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• “Limited Space Templates (i.e., “macros”) … do NOT constitute su�cient documentation of a face-to-face visit and medical examination.”
• “Limited space templates (i.e., “macros”) often fail to capture su�cient detailed clinical information to demonstrate that all coverage and coding requirements are met.”
• “Templates (i.e., “macros”) designed to gather selected information focused primarily for reimbursement purposes are often insu�cient to demonstrate that all coverage and coding requirements are met. This is often because these documents generally do not provide su�cient information to adequately show that the medical necessity criteria for the item/service are met.”
EHRs, Cloned Documents, & Medical Necessity (CMS Analysis, 2012 - 2013)
EHR Analysis: Non-Compliant Features You Want Fixed or Turned O�
Replacing MDM Diagnoses with ICD-9 Codes

AdvancedE/MCodingforEHRs www.aapc.com 129
Presentation
Missing E/M features you would like to have added
1) Consideration of medical necessity for determining appropriate levels of care, documentation, & coding
2) Documentation of qualitative E/M features as well as quantitative
Source of EHR Documentation & Coding Issues
EHR features you would like �xed or turned o�
1) Automated data entry shortcuts that create “cloned” pseudo-documents
2) Incomplete and non-compliant coding engines
3) Billing codes used in MDM for indicating clinical diagnoses
• The purpose of coding is to summarize the rich narrative descriptions (and di�erential diagnoses) of the clinician’s MDM thought process, not to replace it!
Coding is NOT documentation

130 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• Codi�cation of medical records creates shorthand descriptions needed for payment process or generalized data collection
• Such shorthand descriptions are inadequate to characterize the breadth, depth, and/or degree of speci�city required to describe the characteristics of individual patients
• Neither ICD-9 diagnosis codes nor ICD-10 diagnosis codes provide this required degree of speci�city
Coding is NOT documentation
• EHR vendor goals (as marketed): – Make it “easier” on clinicians – Speed the process of selecting diagnosis codes for billing – Saves time of data entry for the billing o�ce personnel? – Eliminate need for coders?
Narrative Documentation of Clinical Impressions Replaced by ICD-9 Billing Codes

AdvancedE/MCodingforEHRs www.aapc.com 131
Presentation
• Issue results from combination of three other non-compliant EHR processes: – 1) Cloning functionality – selection limited by narrow number of choices on a pre-
loaded pick list – Absence of qualitative E/M features required for compliance
• DG: “For a presenting problem without an established diagnosis, the assessment or clinical impression may be stated in the form of di�erential diagnoses or as a "possible", "probable", or "rule out“ (R/O) diagnosis
• However, billing processes prohibit use of all but certain diagnoses
– Non-compliant coding engine, which “counts” one new problem as the equivalent of “multiple” problems • Thereby allowing moderate level MDM (which supports level 4) without requiring clinician
to document his or her thought process through a di�erential diagnosis
When coding replaces documentation
• Unintended Consequences for Patient Care – Inability to document “possible” or “rule out” diagnoses
truncates clinicians’ ability to document their decision making process
– When it is no longer (possible to be) documented, often times it is no longer done • i.e., clinician may cease applying diagnostic skills based on history and physical,
defaulting to “diagnosis by testing” • Diagnosis by testing is more costly, and what happens to patient when tests are all
normal?
Diagnosis by ICD-9 Codes

132 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• Loss of di�erential diagnosis eliminates nuances that individualize a patient’s problem, convey the NPP, and allow clinician to individualize a patient’s treatment – Relative probability of each possible diagnosis; e.g., “unlikely,” “possible,” “probable,” etc – Relative severity of each possible diagnosis; e.g., “mild,” “moderate,” “severe,” “life-
threatening,” etc. – Relative timing of each possible diagnosis; e.g., “constant,” “intermittent,” “occasional,”
“rare,” “�uctuating,” “unpredictable,” etc – Special di�erentiating features of each possible diagnosis; e.g., “unusual,” “atypical,”
“paradoxical,” “well-di�erentiated (tumor),” “poorly-di�erentiated (tumor),” “undi�erentiated (tumor),” etc
Unintended Consequences for Patient Care
• Dr. William Osler: – “It is much more important to know what sort of a patient has a disease than what sort
of a disease a patient has” – “The good physician treats the disease; the great physician treats the patient who has
the disease”
• Practical EHR: – “It is often even more important to �nd and address the di�erences among patients
with similar clinical manifestations than it is to recognize their similarities” – Practical EHR, Chapter 7, page 113
Principles of Real Quality Patient Care

AdvancedE/MCodingforEHRs www.aapc.com 133
Presentation
• EHR programming that non-compliantly requires the use of diagnosis codes to document clinical impressions both distorts the purpose of coding and interferes with the purpose of MDM documentation
Thoughts on Replacing MDM with ICD-9
• From our coders’ perspective, the solution to this three-part issue requires a three-part solution: – Turn o� the non-compliant coding engine – Turn o� the pick list menu of drop-down ICD codes
• This approach then requires a solution to provide diagnosis codes to the practice management system (e.g., a separate screen with selection of compliant CPT and ICD codes)
– Clinician review regarding individualized, in-depth narrative documentation, including di�erential diagnoses • Note: this review can logically be combined with clinician training for compliant
documentation for ICD-10 coding
Thoughts on Replacing MDM with ICD-9

134 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• From both a clinician’s and a patient’s perspective, the impact of this non-compliant process is signi�cant: – It discourages the medical diagnostic process, which uses the di�erential diagnosis to drive
patient-speci�c questions in the medical history and concentration on patient-speci�c areas of the physical examination
– It encourages reliance on diagnostic test results in lieu of the thought process described in Evidence Based Medicine: combining evidence with clinical expertise in the context of individualized patient evaluation
Thoughts on Replacing MDM with ICD-9
Summary Thought on EHR Designs “Our goal should NOT be to design EHRs that compel physicians to
‘think’ like computers. Our goal should be to design EHRs that help physicians think like physicians.”
SRL, 2011

AdvancedE/MCodingforEHRs www.aapc.com 135
Presentation
Coders’ Final EHR Obstacles
• HITECH and CMS have subsidized EHR adoption at least partially on the economic premise that this will reduce medical costs
• EHR vendors have, at least partially, marketed EHRs for their potential to increase E/M code levels
• Clinicians have committed to EHRs, at least partially, because of this promised increase in E/M code levels
Surveying the Stakeholder Landscape

136 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• OIG has identi�ed signi�cant increases in E/M code levels, at least partially related to EHR adoption. It has also identi�ed that these E/M increases are signi�cantly due to improper documentation and coding
• Congressmen have voiced displeasure that EHRs are being used to increase rather than decrease costs
Surveying the Stakeholder Landscape
• Now that we have the tools to provide consistent, reliable, trustworthy, and compliant E/M coding in the EHR environment,
• How happy and willing will our EHR stakeholders be to make the necessary improvements that enhance compliance & quality care?
• Clinicians? • CFOs? • Vendors?
Our Final Challenges

AdvancedE/MCodingforEHRs www.aapc.com 137
Presentation
• With existing EHRs, when we identify the presence of ongoing improper billing and coding, how do we address compliance requirements for self reporting of previous over-coding and over-billing?
• These are not easy questions !
Our Final Challenges
• Using new coding tools to promote dialogue and positive interaction with clinicians because of relationship of E/M (especially qualitative features) with clinical excellence
• Involvement with practice’s EHR evaluations, including E/M criteria and benchmarks for RFP documents and review of EHR products
• Help set standards for EHRs’ E/M design and functionality • Involvement with practice’s EHR implementation,
including physician training
Our New Opportunities

138 AAPC 1-800-626-CODE(2633) CPT®copyright2012AmericanMedicalAssociation.Allrightsreserved.
Presentation
• Inform and then mobilize your allies – Director of coding – Director of compliance – Physician champion(s) – Health care attorney
• Identify areas of risk within your EHR or the EHRs that you are considering for purchase
• Document Document Document! – Document recommendations, phone calls, conversations, emails,
EVERYTHING! • Create and implement a plan to bring your practice /facility into
compliance with E/M coding in your EHR
Rising to the Challenge
Thank you for your participation
CEU Code: AAPC0401131202A


Lowest Prices Anywhere
Pre-order Today!www.aapc.com/2014codebooks1-800-626-CODE (2633)
Physician Bundle 3 ICD-9 1 & 2 • HCPCS • Procedural Coding Expert
$269.95$99.95
Physician Bundle 1 ICD-9 1 & 2 • CPT® • HCPCS Level II
$299.95$159.95
Hospital Bundle 1 ICD-9 1-3 • CPT® • HCPCS Level II
$309.95$169.95
Physician Bundle 2 ICD-9 1 & 2 • HCPCS • CPT® • Procedural Coding Expert
$399.95$199.95
Hospital Bundle 2 ICD-9 1-3 • HCPCS • CPT® • Procedural Coding Expert
$409.95$209.95
Our Best Value!
Individual Books
Bundles
AMA’s CPT® Professional
$114.95$89.95
ICD-9-CM Vol. 1-2
$99.95$44.95
HCPCS Level II
$99.95$44.95
ICD-9-CMVol. 1-3
$103.95$54.95
Procedural Coding Expert
$99.95$54.95
ICD-10-CM
$99.95$59.95
ICD-10-PCS
$99.95$59.95
2014 CodE BooksPre-Order Sale Ends June 30th